
Research Progress of Ebola Live Vector Vaccine
Jiaqi Mi
The High School Affiliated to Renmin University of China, Beijing, China
Keywords: Ebola Virus, Live Vector Vaccine, rVSV‑ZEBOV.
Abstract: Ebola virus is a highly lethal virus belonging to the Filoviridae family. The virus is mainly transmitted through
the patient's body fluids and may cause Ebola hemorrhagic fever, with a mortality rate of up to 25% to 90%.
The early manifestations of Ebola hemorrhagic fever commonly involve fever and muscle pain, followed by
severe symptoms such as vomiting, diarrhea, internal and external bleeding, which may eventually lead to
organ failure and death. Live vector vaccines created an innovative class of immunization. It employs
attenuated viruses or bacteria as delivery vehicles. These carriers transport specific pathogen antigens into
host cells, thereby stimulating the body's immune system to generate a protective response. With the
advancement of genetic engineering, this vaccine has been widely used in the prevention and treatment of
various diseases. Among them, the Ebola vaccine (Ervebo) has been widely used in many African countries.
This article reviews the current status and progress of Ebola live vector vaccines by combing and analyzing
relevant domestic and foreign literature. Focuses on the therapeutic mechanism of the Ebola vaccine and the
drug production process. By comparing drugs currently on the market or in the clinical stage, this article found
that there are some difficulties in the current Ebola vaccine research field, mainly in terms of vaccine
specificity and storage technology. In the end, this paper comprehensively reviews the existing research,
points out the shortcomings of current research, and predicts future development trends, aiming to provide a
reference for researchers for further exploration in the field of Ebola live vector vaccines and provide some
ideas and suggestions for subsequent research.
1 INTRODUCTION
The Ebola outbreak will bring about negative impacts
such as restricted transportation, economic damage,
collapse of the medical system, and social disorder in
the epidemic area. These impacts will last for a long
time. In the past few years, the Ebola outbreak caused
serious economic damage to African countries such
as Liberia, Sierra Leone, and Guinea.
The Ebola virus mainly invades the human body
by infecting epithelial cells of the skin and mucous
membranes. The virus enters the dendritic cells or
macrophages by binding to receptors on the surface
of host cells, damaging these immune cells and thus
weakening the body's immune capacity. Once inside
the host cell, the virus uses the host cell's mechanism
to replicate itself and produce a large number of virus
particles. These newly produced viruses will further
spread to various parts of the body through blood
circulation. Early symptoms include fever, fatigue,
muscle pain and sore throat. As the virus attacks
endothelial cells, ruptures the blood vessel walls,
causing bleeding and edema in the body, severe
patients may suffer from multiple organ failure and
die. This virus was first discovered in Sudan and the
Democratic Republic of the Congo in Central Africa
in 1976. Since then, the virus has broken out several
times in central and western Africa (Selvaraj et
al.,2018), and in 2014 it caused the largest Ebola
outbreak in history, resulted in more than 28,000
confirmed cases and 11,000 deaths (Malvy et
al.,2019), triggering global panic. In response to the
threat posed by the epidemic, scientists began to study
the treatment and prevention of Ebola hemorrhagic
fever. In 2015, the World Health Organization
declared that the outbreak had been largely contained.
Although breakthroughs have been made in the
development of Ebola vaccines and prevention and
control of the epidemic, the Ebola virus remains a
major challenge facing the public health field because
the vaccine is still not widely used in remote
mountainous areas.
At present, with the accumulation of clinical
experience, supportive treatment (such as fluid
supplementation, electrolyte balance, complication
128
Mi, J.
Research Progress of Ebola Live Vector Vaccine.
DOI: 10.5220/0014436600004933
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Biomedical Engineer ing and Food Science (BEFS 2025), pages 128-133
ISBN: 978-989-758-789-4
Proceedings Copyright © 2026 by SCITEPRESS – Science and Technology Publications, Lda.

management, etc.) has become the main treatment for
Ebola virus through Fluid replacement by intravenous
injection to maintain electrolyte balance, this method
can significantly improve the survival rate of Ebola
patients in high-incidence areas. In addition,
monoclonal antibodies such as REGN-EB3 and
mAb114 have shown significant effects in controlling
viral replication and reducing mortality, becoming
one of the most effective ways to treat Ebola
(Mulangu et al.,2019). On the other hand, although
vaccines are not a treatment method, they play a key
role in disease prevention and control and minimize
the risk of infection to individuals exposed to the
strain in the early stages of an epidemic. For example,
the approval and widespread use of the Ervebo
vaccine marks an important progress in prevention
and control work and enhances the ability of countries
to respond to the epidemic. However, there are still
challenges in treating Ebola: many areas with limited
resources lack sufficient medical facilities and expert
guidance, which is not conducive to early
intervention of the epidemic. From the perspective of
disease prevention, the lack of universality of
vaccines against virus strains and storage issues in
tropical regions are also difficult problems that need
to be overcome.
This article will focus on the mechanism and
production process of rVSV-ZEBOV Ebola vaccines
and provide some feasible solutions to the difficulties
encountered in the development of this field.
With the development of genetic engineering
technology, live vector vaccines in various countries
play an increasingly important role in disease
prevention. However, there are still some technical
problems in Ebola vaccine in terms of specific
immunity and storage. To solve these problems, this
article aims to explore and propose solutions through
literature research to promote the sustainable
development of live vector vaccine technology in the
field of Ebola prevention and control.
2 EBOLA VACCINE
The Ebola virus is wrapped into an endosome, it
enters the host cell by binding to a receptor which
triggers endocytosis of the cell membrane: The
surface glycoprotein of virus undergoes proteolytic
processing in the endosome so that it is able to interact
with the cellular receptor cholesterol transporter
Niemann-Pick C1 (NPC1) protein in order to fuse
with the endosomal membrane, and to release the
ribonucleoprotein into the cytoplasm (Baseler et al.,
2017). After the negative-strand RNA genome of the
virus enters the cytoplasm, it uses the host cell's
machinery for transcription and replication. The RNA
polymerase on the viral RNA will replicate the viral
RNA in the cell, generate a large amount of positive-
strand RNA as a template to produce new negative-
strand RNA. The proteins encoded by the viral genes
(such as glycoproteins, nucleocapsid proteins, etc.)
are synthesized on the ribosomes of the host cell and
transported to the cell membrane or corresponding
parts of the cell. The newly synthesized viral RNA
and proteins are assembled into new virus particles in
the cytoplasm of the host cell and released outside the
host cell to further infect other cells. By this process,
EBOV spreads from the infection site via monocytes
to regional lymph nodes, and to liver and spleen via
blood (Geisbert et al., 2003). When the virus spreads
in the body, it attacks the host's endothelial cells,
especially the vascular endothelial cells, causing
damage to the blood vessel walls and increased
vascular permeability. Blood components will leak
into the tissues, causing massive bleeding. As the
virus spreads, it will cause multiple organ failures,
including the liver and heart.
There are many challenges in treating the Ebola
virus, with the biggest one being the lack of specific
drugs. Treatment mainly relies on symptomatic
support such as fluid replacement, blood pressure
maintenance and oxygen supply. Although some
antiviral drugs are under development, there is still no
completely effective treatment plan. At the same
time, Ebola outbreaks mostly occur in resource-
scarce areas in Africa. Incomplete medical conditions
and citizens' lack of awareness of disease prevention
due to lack of education have further accelerated the
spread of the virus.
3 EXISTING TREATMENTS
There are currently three main response methods to
the Ebola epidemic: supportive therapy , Drug
treatment and vaccination. Supportive therapy such as
fluid replacement Massive internal bleeding caused
by Ebola virus destroying blood vessel walls. Related
research shows that this intervention can increase the
chance of survival efficiently during the early phase
of the disease (Goeijenbier et al., 2014). This will
reduce the harm caused by the epidemic in the early
stages. On the other aspect, drugs are also widely used
in disease treatment by the support of governments.
Scientists injected the triple monoclonal antibody
ZMapp as the control group, in contrast to antiviral
Research Progress of Ebola Live Vector Vaccine
129

agent remdesivir (MAb114). The experimental
results indicate that the mortality rate in the Mab114
group was 35.1%, slightly lower than that of the
ZMapp group, which had a mortality rate of 49.7%
(Sabue et al., 2019). However, the aforementioned
data further indicate that pharmacological
interventions are ineffective in lowering the mortality
rate associated with the Ebola virus. Therefore,
improving the resistance of susceptible people in
Ebola-affected areas to the virus and promoting
universal immunity became one of the important
tasks for scientists, and the Ebola live vector vaccine
came into being. The mechanism of this vaccine is
inserting the protective antigen gene of other
pathogens into the non-essential region gene of the
vector genome to form a new recombinant virus. This
new virus is going to be implanted into human body
and triggering an immune response. The immune
system will produce specific antibodies and immune
cells by recording the information of the viral
genome. When a real virus invades the human body,
the immune system is able to produce a large number
of corresponding antibodies to respond to the virus in
a short period of time. This vaccine has advantages
such as simple production, applicability to a variety
of pathogens and long immunity.
4 THE rVSV-ZEBOV EBOLA
VACCINE
4.1 Treatment Principle
Scientists use the genetically modified vesicular
stomatitis virus (VSV) as an Ebola vaccine vector.
The reason why VSV is able to become the vector is
that it can be classified as a single-stranded negative-
sense RNA virus so that it lacks a complex cleavage
mechanism or segmented genome, making it
amenable to insert foreign genes. Besides, this virus
primarily impacts livestock and the infection is meek
and asymptomatic in humans. Human infections have
been reported only in a small number of cases,
primarily among animal handlers and laboratory
researchers (Bishnoi et al. 2018). That means it is
almost harmless to humans and can be engrafted in
the human body.
To begin with, people will remove the
glycoprotein gene of VSV. This process would render
VSV unable to infect other cells and ensure that it
cannot replicate within the human body for an
extended period for safety reason. After that, insert
the glycoprotein(GP) gene of the Ebola virus to
enable its expression in the VSV vector. Finally, by
using reverse transcription technology, a stable
recombinant vesicular stomatitis virus–Zaire Ebola
virus(rVSV-ZEBOV) strain expressing the Ebola
glycoprotein gene is constructed.
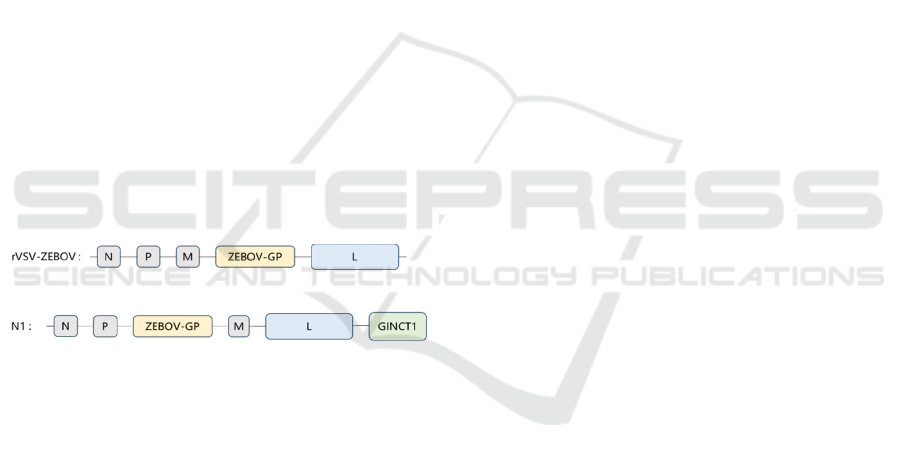
Figure 1: Example of Insert the Ebola Virus Glycoprotein
Gene.
As Figure 1 shows, GP gene of VSV has been
removed, in favor of GP gene of Ebola virus to form
a rVSV-ZEBOV. When this recombinant virus enters
the human body, the immune system will produce
corresponding antibodies based on the ZEBOV
genome, thereby having the ability to prevent the true
virus.
4.2 Development and Production
Process
After obtaining the recombinant virus, the researchers
used serum albumin and buffers to prepare the
vaccine, and by adjusting and maintaining the pH
value of the vaccine, they ensured that the vaccine
would not lose its activity due to changes in pH
during storage and use, thereby maintaining the
effectiveness of the vaccine and reducing the
stimulation of the drug to the human body during
injection. The rVSV-ZEBOV vaccine was produced
using recombinant human serum albumin and a tris
aminomethane buffer, with each vial containing a
concentration of 100 million plaque-forming units
(PFU) per milliliter. Pharmacists utilized normal
saline as a diluent to prepare the vaccine doses,
achieving concentrations of either 3 million PFU or
20 million PFU (Regules et al.,2017).
Once a candidate vaccine is developed, it must
first be tested in rodents and non-human primates to
ensure the safety and effectiveness of the vaccine. In
2007, researchers used three animal models: mice,
guinea pigs, and rhesus monkeys to consider the post-
exposure therapeutic effect of rVSV-ZEBOV
BEFS 2025 - International Conference on Biomedical Engineering and Food Science
130

vaccine. They found that mice and guinea pigs
immunized 24 hours after ZEBOV infection could
obtain 100% and 50% protection respectively; while
rhesus monkeys immunized within 20 to 30 minutes
after infection could obtain 4/8 protection (Feldmann
et al.,2007). This research result confirms the rVSV-
ZEBOV vaccine's protective effect on mammals by
producing an immune response in the test subject and
provides a theoretical basis for subsequent human
experiments.
After passing mammal experiments, the vaccine
will be administered to human volunteers on a small
scale for Phase I-III clinical trials. In 2014, two Phase
I clinical trials of the vaccine were conducted in the
United States. These two studies verified for the first
time the safety and immunogenicity of the rVSV-
ZEBOV vaccine in humans. An immune response can
be produced about 6 days after a single intramuscular
injection (Regules et al.,2017). After a double dose,
the body produces a secondary immunity, and the
antibody immune effect is enhanced, confirming the
effectiveness of the vaccine in humans.
Subsequently, a phase II clinical trial conducted in
Liberia showed data on the immune effect of 2.0×107
PFU rVSV-ZEBOV. One month after immunization,
the geometric mean of GP antibodies in the rVSV-
ZEBOV group was 1000 EU/ml, with a positive rate
of 83.7%; 12 months after immunization, the
geometric mean of GP antibodies in the rVSV-
ZEBOV group was 818 EU/ml, with a positive rate of
79.5%(Kennedy et al.,2017). This suggests that the
rVSV-ZEBOV vaccine maintains high antibody
levels and has a strong immune effect for a long
period of time after vaccination. During the Phase
III study stage, the sample size needs to be further
expanded to ensure the universal applicability of the
vaccine. In experiments conducted by the Canadian
Center for Vaccinology and other institutions in
2019,1197 healthy adults were randomized 2:2:2:2:1
to receive 1 of 3 consistency lots of rVSV-
ZEBOV(2× 10
7
plaque-forming units [pfu]), high-
dose 1×10
8
pfu, or placebo. At 28 days, more than
94% of vaccine recipients seroresponded, with
responses persisting at 24 months in over
91%(Halperin et al.,2019). This result confirms that
the vaccine has a wider audience and has immune
efficacy for a longer period of time. Since then, the
rVSV-ZEBOV vaccine has been officially put into
large-scale production.
4.3 Drugs Currently on the Market or
in Clinical Stages
The vaccines currently available on the market can be
divided into three categories: DNA vaccines, mRNA
vaccines and viral vector vaccines. DNA vaccines,
such as the Ebola vaccine INO-4212 developed by
Inovio Pharmaceuticals and GeneOne Life Science,
are used to express plasmids that are immunogenic
antigens. DNA vaccine production mainly relies on
large-scale fermentation and purification of plasmid
DNA, without the need for complex cell culture or
virus inactivation, and the steps are relatively simple,
with low production costs. However, due to the need
to encode different Ebola virus subtypes, it has the
disadvantages of complex immunization procedures
and has a long production cycle.
Unlike DNA vaccines, which deliver DNA
encoding antigenic proteins to the cell nucleus,
mRNA vaccines deliver mRNA encoding antigenic
proteins directly to the cytoplasm. After entering the
cell, the lipid nanoparticles encapsulating the viral
antigen protein mRNA fuse with the cell membrane,
releasing the internal substances into the cytoplasm.
The cell ribosomes will read the mRNA sequence,
synthesize the viral antigen protein, activate the
immune system to produce a specific immune
response, and then form immune memory to provide
long-term protection. Scientists vaccinate guinea pigs
with Ebola mRNA vaccine to induce EBOV-specific
IgG and neutralizing antibody responses. The
experiment result indicated that 100% of guinea pigs
survived after EBOV infection (Meyer et al.,2017).
This confirms the effectiveness of the Ebola mRNA
vaccine in mammals. However, mRNA has poor
stability and needs to be stored at low temperatures.
It also requires a complex lipid nanoparticle delivery
system, which also greatly increases the cost of
vaccine production.
Viral vector vaccines such as rVSV-ZEBOV use
modified viruses as vectors to deliver the antigen
genes of target pathogens into host cells, thereby
stimulating an immune response. The vaccine was
developed by the Public Health Agency of Canada
and then licensed to Merck (product name V920) for
later development of the vaccine. In May 2018,
Merck and its partners provided a large number of
vaccines to WHO during a new round of Ebola
outbreaks in the Democratic Republic of the Congo
and other places for ring vaccination (forming a
circular population around each contact of a new
Ebola case, with an immediate vaccination group and
a delayed vaccination group) to prevent further spread
Research Progress of Ebola Live Vector Vaccine
131
of the epidemic. According to statistics, a total of
300,000 residents in epidemic areas were vaccinated
from 2018 to 2020(Wolf et al.,2020). Despite the
modification, viral vectors may still trigger an
immune response in the human body, bringing
potential risks. Therefore, the safety of viral vector
vaccines will still be an issue that needs to be paid
attention to in the future.
4.4 Challenges and Prospects
Although the rVSV-ZEBOV vaccine is currently the
most effective vaccine against Ebola virus, its safety
still needs to be improved: In clinical trials conducted
in Africa and Europe, 103 out of 110 subjects (94%)
who received an immunization dose exceeding
3.0×10⁶ PFU (plaque-forming units) still exhibited
vaccine viremia three days after immunization.
(Agnandji et al.,2016). This finding highlights the
persistence of the vaccine virus in the bloodstream
shortly after administration, causing some potential
side effects and needs further optimization of the
vaccine's safety profile. Researchers used systems
vaccinology to deeply analyze vaccine clinical trial
data and interpret the causes of adverse reactions to
guide further optimization of vaccine design and
reduce drug side effects. As a result,
rVSVN1CT1GP3 (N1) was successfully developed.
Figure 2: Comparision Between Gene Structure of the First
Generation Vaccine and N1 Vaccine.
As Figure 2 shows, compared with the first-
generation rVSV-ZEBOV vaccine, the N1 vaccine
swaps the positions of the ZEBOV-GP gene and the
M gene, and adds the gene sequence (GINCT1) with
a reduced length of the cytoplasmic tail of the VSIV
glycoprotein after the L gene.
The above optimization steps for the vaccine
genome can effectively reduce the side effects of
vaccines. People found through animal experiments
that the probability of viremia in crab-eating
macaques after a single immunization with the
modified vaccine was 10 times lower than that of the
first-generation rVSV-ZEBOV vaccine (Mire er
al.,2015), which proved that this modification can
effectively improve the safety of the vaccine. In the
future, based on further understanding of rVSV-
ZEBOV vaccine clinical data, the safety of the
vaccine will be greatly improved.
Besides, rVSV-ZEBOV only targets the Zaire
Ebola virus (EBOV-Z), but there are still different
Ebola virus strains such as Sudan (SUDV) and
Bundibugyo (BDBV). Scientists are actively
developing multivalent vaccines designed to target
multiple strains, including the Ebola Sudan vaccine
(rVSV-EBOV-SUD), which is built on the rVSV
platform and is currently undergoing clinical trials.
5 CONCLUSION
Ebola vaccines are of great significance in public
health security. The development of Ebola vaccines
can control the epidemic and reduce the mortality rate
of patients in poor areas. At the same time, it can
prevent possible Ebola outbreaks in the future and
protect people in high-risk areas. Current vaccine
research focuses on developing multivalent vaccines
that can target multiple Ebola virus strains and
reducing dependence on the cold chain to facilitate
promotion in areas with limited resources.
This article deeply explores the relevant literature
in the field of Ebola live vector vaccines and uses the
method of literature research to deeply analyze this
technology. However, in terms of vaccine safety and
broad spectrum, the development speed of Ebola live
vector vaccines has been restricted to a certain extent.
In order to promote further development in this field
and mitigate the adverse impact of the Ebola outbreak
in West Africa, it is particularly urgent to solve the
above problems and promote the comprehensive
construction of Ebola live vector vaccine.
Ebola live vector vaccines will continue to play an
important role in the future, providing stronger
protection for global public health security through
technological innovation and multi-field cooperation:
With the advancement of genetic engineering and
viral vector technology, future Ebola live vector
vaccines will be safer and more efficient, and
vaccines for different Ebola strains will also be
produced. In addition, by improving the vaccine
formula or using more stable vectors, it may be
possible to reduce dependence on the cold chain in
the future, reduce storage and transportation costs,
make it more suitable for promotion in resource-
limited areas, and meet the vaccine needs of the vast
poor areas of Africa.
BEFS 2025 - International Conference on Biomedical Engineering and Food Science
132

REFERENCES
Agnandji, S. T. 2016. Phase 1 Trials of rVSV Ebola
Vaccine in Africa and Europe. The New England
journal of medicine, 374(17), 1647–1660.
Baseler, L. 2017. The Pathogenesis of Ebola Virus Disease.
Annual review of pathology, 12, 387–418.
Bishnoi, S. 2018. Oncotargeting by Vesicular Stomatitis
Virus (VSV): Advances in Cancer Therapy. Viruses,
10(2), 90.
Feldmann, H. 2007. Effective post-exposure treatment of
Ebola infection. PLoS pathogens, 3(1), e2.
Geisbert, T. W. 2003. Pathogenesis of Ebola hemorrhagic
fever in cynomolgus macaques: evidence that dendritic
cells are early and sustained targets of infection. The
American journal of pathology, 163(6), 2347–2370.
Goeijenbier, M. 2014. Ebola virus disease: a review on
epidemiology, symptoms, treatment and pathogenesis.
The Netherlands journal of medicine, 72(9), 442–448.
Halperin, S. A. 2017. Six-Month Safety Data of
Recombinant Vesicular Stomatitis Virus-Zaire Ebola
Virus Envelope Glycoprotein Vaccine in a Phase 3
Double-Blind, Placebo-Controlled Randomized Study
in Healthy Adults. The Journal of infectious diseases,
215(12), 1789–1798.
Kennedy, S. B. 2017. Phase 2 Placebo-Controlled Trial of
Two Vaccines to Prevent Ebola in Liberia. The New
England journal of medicine, 377(15), 1438–1447.
Malvy, D. (2019). Ebola virus disease. Lancet (London,
England), 393(10174), 936–948.
Meyer, M. 2018. Modified mRNA-Based Vaccines Elicit
Robust Immune Responses and Protect Guinea Pigs
From Ebola Virus Disease. The Journal of infectious
diseases, 217(3), 451–455.
Mire, C. E. 2015. Single-dose attenuated Vesiculovax
vaccines protect primates against Ebola Makona virus.
Nature, 520(7549), 688–691.
Mulangu, S. 2019. A Randomized, Controlled Trial of
Ebola Virus Disease Therapeutics. The New England
journal of medicine, 381(24), 2293–2303.
Regules, J. A. 2017. A Recombinant Vesicular Stomatitis
Virus Ebola Vaccine. The New England journal of
medicine, 376(4), 330–341.
Selvaraj, S. A. 2018. Infection Rates and Risk Factors for
Infection Among Health Workers During Ebola and
Marburg Virus Outbreaks: A Systematic Review. The
Journal of infectious diseases, 218(suppl_5), S679–
S689.
Wolf, J. 2020. Applying lessons from the Ebola vaccine
experience for SARS-CoV-2 and other epidemic
pathogens. NPJ vaccines, 5(1), 51.
Research Progress of Ebola Live Vector Vaccine
133
