
A Review of the New Rural Cooperative Medical Scheme Under the
Background of Urban and Rural Medical Insurance Integration
Qingchuan Xu
School of Government Administration, Shenzhen University, Shenzhen, Guangdong, 518060, China
Keywords: New Rural Cooperative Medical Scheme, Integration of Medical Insurance, Health Equity.
Abstract: TAs the core system of China’s rural medical security system, the New Rural Co-operative Medical Scheme
has acted significantly in narrowing the urban-rural medical gap. With the ongoing unification of healthcare
coverage for urban and rural populations gaining momentum, contradictions such as regional imbalance and
reverse redistribution have gradually become prominent. This analysis collated the relevant literatures and
summarized the existing research on the practice of the NCMS from multiple dimensions. The research finds
that through practice and integration into medical insurance, although the NCMS has effectively improved
the supply of medical services through various means, there are still fundamental contradictions of regional
differences and group differences. The research conclusion indicates that future reforms need to be fairness
oriented. Only by establishing a differentiated mechanism and a better collaborative network can more
effective support be provided for the improvement of medical insurance efficiency.
1 INTRODUCTION
The policy of the New Rural Cooperative Medical
Scheme (hereinafter referred to as ‘the NCMS’)
originated from the social development problems in
China in the 1980s. With the disintegration of the
traditional rural health care system, a series of social
problems, such as farmers’ medical difficulties and
the disparity of healthcare resources between urban
and rural places, have become increasingly serious. In
2003, the General Office of the State Council of the
People’s Republic of China forwarded ‘the Opinions
on Establishing New Rural Cooperative Medical
Scheme’ (Guobanfa [2003] No. 3), launching the
national pilot of the NCMS (General Office of the
State Council of China, 2003). By 2010, the NCMS
had basically improved coverage in rural areas across
the country, with a participation rate of up to 95%.
However, the numerous differences in medical
resources between urban and rural zones remain a
major concern (Office of the People’s Government of
Lanzhou City, 2011; State Council of China, 2016).
As China continues to promote modernization and
development, more and more attention has begun to
focus on the deficiencies of the health care system for
achieving universal medical insurance and promoting
social equity. In 2016, the State Council of China
announced ‘the Opinions on integrating the Basic
Medical Insurance System for Urban and Rural
Residents (Guofa [2016] No. 3), marking the launch
of the health care integration (State Council of China,
2016). Medical insurance integration refers to the
integration of the Urban and Rural Resident Basic
Medical Insurance (hereinafter referred to as ‘the
URRBMI’) with the Urban Resident Basic Medical
Insurance (hereinafter referred to as ‘the URBMI’)
and the NCMS. It is also one of the core issues of
China’s medical security system reform in recent
years (see Table 1).
Against the backdrop of health coverage merger
policy implementation, the NCMS faces various
challenges, such as regional development imbalance,
reverse redistribution effect and other practical
problems. It is necessary to optimize the system effect
through more refined policy design, which provides
space for discussion and analysis in this explore.
The core goal of the URRBMI is to eliminate
urban and rural differences through system
integration. Practical measures include unified
financing mechanism, unified reimbursement
catalog, unified fund management and analysis and
treatment support. In particular, the objective calls for
government financial subsidies to rise concurrently
and for urban and rural populations to pay according
to
the same levels, integrate the original drug and
Xu, Q.
A Review of the New Rural Cooperative Medical Scheme Under the Background of Urban and Rural Medical Insurance Integration.
DOI: 10.5220/0014391500004859
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Politics, Law, and Social Science (ICPLSS 2025), pages 583-592
ISBN: 978-989-758-785-6
Proceedings Copyright © 2026 by SCITEPRESS – Science and Technology Publications, Lda.
583

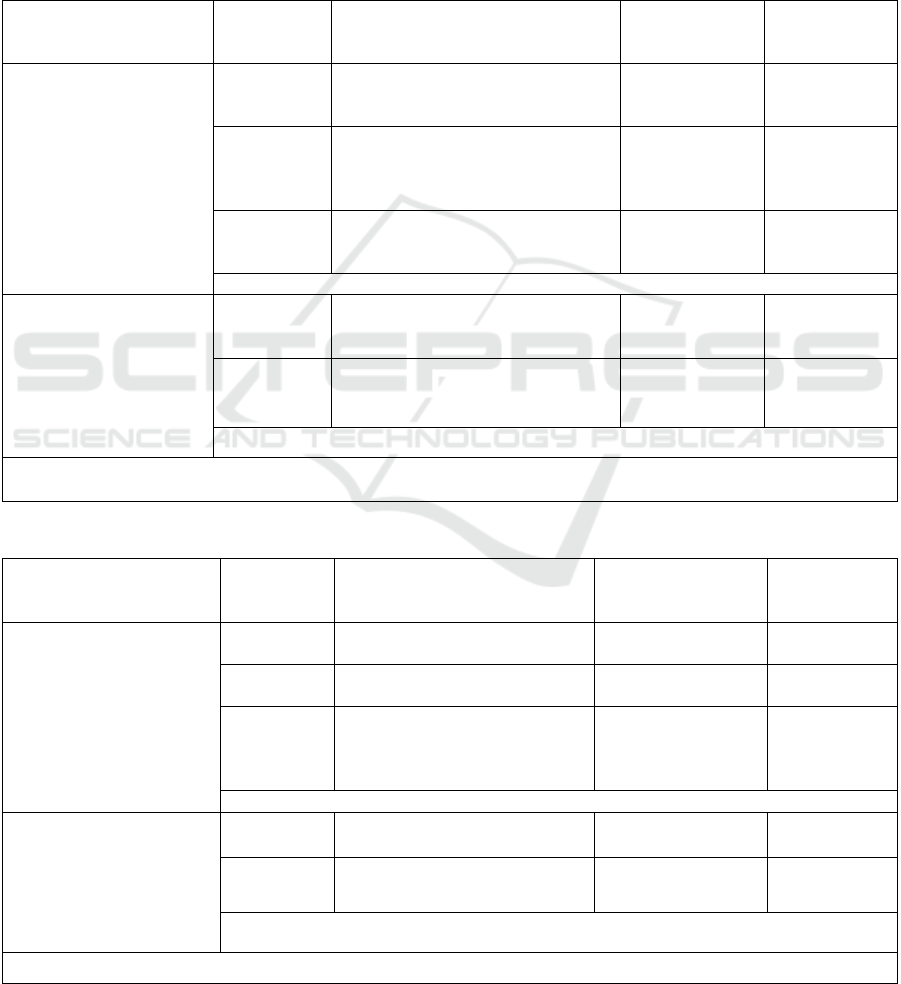
Table 1. The Construction Process of Primary Medical Insurance.
Yea
r
Polic
y
and practice Sta
g
e of developmen
t
2002
The CPC Central Committee and the State
Council of China announced ‘the Decision on
Further Strengthening Rural Health Work’,
suggesting the creation of a new health program
for rural places
The framework of the NCMS was clarified at
the national level for the first time
2003
The General Office of the State Council forwarded
‘the Opinions on Establishing the NCMS’ and
launched a nationwide pilot program
The programmatic document had emerged that
marked the transition from theory to practice of
the NCMS, and began to build a rural medical
securit
y
s
y
stem coverin
g
the whole countr
y
.
2007
The pilot program of the URBMI was launched,
covering non-employed urban residents
For the first time, a medical insurance system
was established for non-employee groups in
urban areas, forming an urban-rural division
with the NCMS.
2010 The NCMS had basically realized nationwide rural coverage, with a participation rate of over 95%.
2008-
2013
Eight provinces have taken the lead in piloting the integration
2013
The State Council of China issued ‘the Opinions
on Integrating the Basic Medical Insurance
S
y
stem for Urban and Rural Residents’
As an authoritative policy document, it clarifies
the relevant practical principles
2016
The health insurance programs of both rural and
urban residents have been integrated in 31
provinces across the country, and the National
Medical Insurance Administration is in charge of
unified mana
g
ement.
Achieved complete system, management, and
service unification and worked to end the dual
division among urban and rural zones.
service catalog in the URBMI and the NCMS. Then,
by utilizing different payout percentages to alleviate
the issue of resource crowding out of large hospitals,
the provincial level will coordinate the medical
insurance funds of suburban as well as rural medical
funds, increasing the amount that rural residents can
be reimbursed. This will improve the efficiency of
fund use and encourage patients to seek appropriate
medical care.
The policy design reflects the transition logic from
formal integration to substantive fairness. In reality,
however, the NCMS’s unity has regional economic
level disparities, primarily in vast agricultural regions,
local fiscal capacity and uneven management
efficiency, resulting in significant spatial
differentiation in the integration effect.
This article systematically reviewed the existing
literatures on the current status of the NCMS,
examines how health equity in the combining program
of medical insurance for rural and urban dwellers
affect the allocation of medical resources and financial
burden, while proposing the contributions and
shortcomings of existing exploration. It is hoped that,
based on the existing exploration, the findings can
provide policymakers with operational suggestions
such as regional differentiated adjustments and a
dynamic monitoring mechanism design.
2 ANALYZE METHODS AND
PROCESS
Literature searched for this exploration comes from
CNKI and Web of Science.
The keywords for searching in CNKI was ‘the
New Rural Cooperative Medical Scheme’/‘the
NCMS’, and specific screening was performed
through the search commands ‘Academic Journals’,
‘Peking University Core’/‘CSSCI’, and the literature
in the past five years/the top ten most cited literature.
A total of 69 studies were screened in the first
screening. In the second screening, literature that was
not related to the analysis topic (like emphasizing the
NCMS’s influence on consumption/pension/job
choice/fertility intention, etc.) was screened, and a
total of 32 literatures remained. The third screening
screened literatures that were related to the analysis
topic but had too narrow a focus and were not
valuable in the analysis of this explore or had
ICPLSS 2025 - International Conference on Politics, Law, and Social Science
584
different analysis perspectives from this explore
(such as limited to a single disease: heart disease,
gastric cancer, cardiovascular and cerebrovascular
diseases, etc., a single group: lonely elderly people,
left-behind children, etc., a single region: the specific
situation of a certain district in a certain city or a
certain county, etc.), and finally 14 literatures were
left as references for this explore (see Table 2).
In addition, the keyword ‘the Urban and Rural
Residents Basic Medical Insurance (the URRBMI)’
was included, and the search instructions were
‘Academic Journals’, ‘Peking University
Core’/‘CSSCI’, documents from the past five years,
and the top 20 most cited documents. Among the
basic 11 documents, after screening out documents
that were not related to the analysis topic of this
exploration, a total of 4 documents remained (see
Table 2).
Table 2. Illustration of CNKI Literature Search.
Keywords Steps Instructions
The number of
remaining
documents
Notes
The NCMS/ the New
Rural Cooperative
Medical Scheme
Primary
screening
Academic journals, Peking
University core/CSSCI, top 10 most
cited in the
p
ast 5
y
ears
69
Secondary
screening
Exclude literatures irrelevant to the
topic (such as consumption, elderly
care, fertility and other fields with
weak correlation
)
32
Elimination of
37 articles
Tertiary
screening
Exclude literatures with too narrow a
perspective (such as single disease,
g
rou
p
, or re
g
ional ex
p
lores, etc.
)
13
Elimination of
18 articles
13 articles in total
The Urban and Rural
Residents Basic Medical
Insurance/the URRBMI
Primary
screening
Academic journals, Peking
University core/CSSCI, top 20 most
cited in the past 5 years
11
Secondary
screening
Exclude literatures irrelevant to the
topic
4
Elimination of
7 articles
4 articles in total
17 articles in total
Table 3. Illustration of Web of Science Literature Search.
Keywords Steps Instructions
The number of
remaining
documents
Notes
The New Rural
Cooperative Medical
Scheme/the
NCMS
Primary
Screenin
g
Article, Top 20 in the past 5
y
ears/Hi
g
hl
y
Cite
d
140
Secondary
Screenin
g
Exclude non-Q1 partition and
low-im
p
act-factor literatures
36
Elimination of
104 articles
Tertiary
Screening
Exclude low-relevance
literatures (such as labor supply,
single population/disease
explores, etc.)
12
Elimination of
24 articles
12 articles in total
The Urban and Rural
Residents Basic Medical
Insurance/the URRBMI
Primary
Screening
Article、Q1、Top 20 in the past
5 years/Highly Cite
d
16
Secondary
Screening
Exclude literatures irrelevant to
the topic
3
Elimination of
13 articles
3 articles in total
15 articles in total
A Review of the New Rural Cooperative Medical Scheme Under the Background of Urban and Rural Medical Insurance Integration
585

The keywords for the search in Web of Science
were ‘the New Rural Cooperative Medical
Scheme’/‘the NCMS’, and the search instructions
were ‘Article’, the literature in the past five years/the
top 20 most cited literatures. The first screening
resulted in a total of 140 literature. In the second
screening, the literature that was not in the Q1
partition and had a relatively small impact factor was
screened, and a total of 36 articles remained. The third
screening screened various types of literature that
were less relevant to the analysis topic of this explore
and had different perspectives (such as the impact of
labor supply, a single social group, the treatment of a
single disease, the impact of population mobility,
etc.), and finally a total of 12 literatures remained (see
Table 3).
In addition, the keywords was included: ‘the Urban
and Rural Residents Basic Medical Insurance’/‘the
URRBMI’, and the search instructions were ‘Article’,
Q1 partition, literatures in the past five years, and the
top 20 most cited literatures. Among the basic 16
literatures, after screening out investigate questions
that were not related to the analysis topic of this
exploration, a total of 3 literatures remained.
Finally, a total of 33 documents were found by
combining the literatures searched by CNKI and Web
of Science (see Table 3).
3 LITERATURE REVIEW
3.1 Literature Induction Logic
Based on an extensive review of literatures, an
inductive structure is established as shown in the table
4, using a systematic overall framework to analyze
the progressive inductive logic from institutional
input to policy processing, then to effect output, and
finally focusing on feedback regulation (see Table 4).
Table 4: Literature summary structure.
Structural level Core conten
t
Institutional input
level
The necessity, path, and results of combining health insurance in agricultural
re
g
ions as well as urban zones
Challenges and coping strategies of regional heterogeneity to policy
implementation
Policy processing
level
Policy design optimization (such as tiered mechanism reform, payment method
innovation)
Supporting mechanism innovation (fund coordination, information platform
construction, etc.)
Effect output level
Health performance and economic performance
Povert
y
reduction results and income distribution effects
Feedback adjustment
level
Re-examination of group heterogeneity and regional heterogeneity
3.2 System Input Level
3.2.1 Urban-Rural Medical Insurance
Pooling and System Integration
The necessity, progression, and evaluation of the
melding of both metropolitan and rural medical
coverage systems are the main topics of this section.
It highlights the importance of unified finance
standards, reimbursement ratios, and other methods
in reducing the disparity between urban and rural
areas. In this part, some literatures explore that in the
process of integrating the NCMS with the URBMI,
the rate at which rural populations use medical
services has considerably increased by unifying
financing standards, reimbursement ratios and
medical catalogs.
Some scholars have found in their explorations
that from 2008 to 2018, the NCMS significantly
increased the hospitalization rate of rural residents;
and after the integration of medical insurance in areas
where the NCMS was implemented, the
hospitalization reimbursement rate and
reimbursement ratio were also significantly improved
(Yan et al, 2022; Huang & Wu, 2020). The
integration of medical insurance based on the NCMS
has effectively targeted the situation of poverty
generated by illness and has significantly reduced the
incidence of poverty caused by illness among rural
residents by 6.57%. In addition, the targeting effect is
more obvious for groups with poor health, chronic
diseases, low-to-medium consumption, and high
medical expenses (Li et al.,2021).
ICPLSS 2025 - International Conference on Politics, Law, and Social Science
586

The disparity in poverty between urban and rural
regions must still be reduced, nevertheless, by
medical insurance integration using strategies like
uniform finance standards and broadened
reimbursement scope, because the economic factor is
still the key hindering the realization of fairness (Ren
et al, 2022). At the same time, regional heterogeneity
has also affected the specific results. For instance,
compared to eastern China, the degree of
improvement in health levels in central and western
China is far greater (Meng et al, 2024). To avoid
compromising the true impact of medical insurance
integration, the NCMS should keep concentrating on
the predicament of families with limited assets having
to pay for the medical treatment of wealthier areas
because of an unequal distribution of resources (Peng
& Yue et al, 2020).
Through empirical analysis, Qiu et al. discovered
that the degree of economic growth must be the basis
for integrating medical insurance in urban as well as
rural regions. Taking Dongguan, Taicang and other
relatively economically developed regions in China
as examples, in addition to lowering the proportion of
individual expenses for rural people, the integration
model can raise the outpatient benefit rate and
standardize financing criteria and benefits. They
pointed out that the integration needs to be promoted
in stages: developed regions can promote the
integration in one step, and underdeveloped regions
should adopt a layered integration approach to
balance fiscal pressure and insurance demand.
Although the integration has alleviated the imbalance
of health care resources, a more notable rise has been
caused by geographical heterogeneity in
hospitalization utilization in the western region in
China, and we need to be vigilant about reverse
subsidy issues, such as the urban-rural cost gap. Qiu
et al. emphasized fair financing and equal benefits in
the integration practice, and suggested reducing the
cost of institutional separation through unified
management and information platforms (Qiu et al,
2011). Other scholars also pointed out that in addition
to platform unification and phased promotion,
institutional integration should shift from payment for
services to payment for disease type, prepayment of
total amount or per capita payment to control
excessive medical treatment, and alleviate financing
fairness through payment by income tiers (Liu &
Vortherms, 2017; Luo et al, 2021).
3.2.2 Addressing Regional Heterogeneity
Some scholars focus on the differences in policy
effects between regions in China. From the practice
of the NCMS to its integration, they propose a
discussion on how to deal with the uneven regional
resource distribution and structural differences in the
degree of benefit.
In the practice of the NCMS, regional
heterogeneity has long been reflected. The NCMS’s
major disease insurance has decreased the frequency
of poverty vulnerability in the center and western
family units in China despite the health care system’s
influence on poverty reduction is more noticeable in
the central and westernmost fields, as was previously
indicated, and the degree of advantage is much
greater than it is in the eastern zone (Gao & Ding,
2021). In such economically underdeveloped regions,
although the policy tilt effect is more obvious, due to
the absolute disadvantages in per capita income and
medical service utilization, the potential migration of
medical resources from countryside to metropolitan
regions (also known as the reverse subsidy dilemma)
presents a problem for medical fairness in central and
western agricultural regions (Ren et al, 2022; Peng &
Yue, 2020).
Taking the study of Gao & Ding as an example, the
empirical results show that in the western and central
portions of the state, the NCMS’s major disease
insurance has a much deeper effect on poverty
reduction than in the eastern area. Additionally, the
central and western areas have seen a greater decline
in the incidence of poverty vulnerability, but the
eastern region has seen a somewhat limited effect.
This difference is due to the weak economic
foundation and medical resource scarcity in the
western and central areas, and the higher marginal
utility brought by policy bias (Gao & Ding, 2021).
Some academics stress that actively expanding health
care coverage, reducing economic inequities, and
optimizing regional resource allocation are necessary
to address regional heterogeneity and attain the full
inclusivity of medical cover system (Ren et al, 2022;
Meng, 2024).
3.3 Policy Operation and Processing
Level
3.3.1 Policy Design Optimization
This subsection mainly refers to the investigative
perspective that focuses on the defects of medical
insurance, such as the tiering mechanism and the
adverse selection while proposing optimization and
reform suggestions. From this perspective, it is
mainly reflected in the further expansion and
improvement based on the practical results of the
NCMS.
A Review of the New Rural Cooperative Medical Scheme Under the Background of Urban and Rural Medical Insurance Integration
587

The deviations in informal systems and
understandings of insured persons, such as
interpersonal relationships and information quality,
have led to problems such as insufficient transparency
of medical insurance policies and adverse distribution
(Office of the People’s Government of Lanzhou City,
2011; Yuan et al, 2020; Xiong, 2022). Based on the
empirical analysis of the NCMS, Yip & Hsiao
concluded that the previous approach disregards
outpatient costs for chronic diseases and was overly
preoccupied with hospitalization prevention,
resulting in limited poverty reduction effects.
Through the comparison of the experimental rural
mutual medical care model (RMHC), they confirmed
that the strategy of covering outpatient services,
canceling deductibles and integrating funding pools
can reduce the poverty gap by 17%-18.5%,
significantly reducing the risk of medical poverty.
Yip Winnie also advocated the abolition of the
Medical Savings Accounts (MSA) and the transfer of
resources to outpatient and chronic disease
protection, emphasizing that policy design needs to
adapt to the epidemiological characteristics of the
disease burden (Yip & Hsiao, 2009).
3.3.2 Innovation of Supporting Mechanisms
As scholar Yu reported, from 2003 to 2010, the
NCMS rapidly increased the participation rate and the
utilization rate of inpatient services for rural residents
by implementing a strategy of low payment
thresholds and high fiscal subsidies, but there are still
fundamental problems such as low welfare levels,
adverse distribution, and regional imbalances.
Through analysis, Yu suggested that a dynamic
adjustment mechanism and differentiated subsidies
linked to farmers’ income should be established, and
that the reform and optimization of mechanisms,
including cross-departmental collaboration of fund
advances, risk warning mechanisms, and insurance
incentives for welfare supplements, should be
promoted (Yu, 2015). At the same time, according to
the decline in individual disease prevention rates
generated by the increase in insurance participation
rates, health risks can be classified and multi-level
insurance contracts can be designed to alleviate the
corresponding ex-ante moral risks (Guo & Zhou,
2021). Based on the practical measures of city
Beijing’s medical insurance, its system can be
actively refined and medical service needs can be met
by refining payment methods and establishing a
national unified data monitoring and dynamic
evaluation system (Liu & Vortherms, 2017).
In short, policy design needs to balance efficiency
and fairness, and adapt to disease burden and group
needs through benefit measures such as weakening
individual power differences and promoting
coordination and integration (Zhai, 2021).
3.4 Effect Output Level
3.4.1 Health Performance and Economic
Performance
This component focuses on assessing the primary
consequences of the NCMS on medical resource
consumption (hospitalization rate, total cost) and
health level (expressed health, mental health, and
objective health), while paying attention to changes
in economic burden.
Based on the national health service survey data
from 2003 to 2013, according to Zhang et al., the
NCMS considerably raised rural residents’ inpatient
service usage rates (from 2.7% to 7.7%) and
eliminated the urban-rural income gap in service
utilization, but the risk of catastrophic medical
expenditures for low-income groups still remained
high (for example, in 2013, the proportion of medical
expenditures of the lowest-income households
exceeding 40% reached 24.7%, while that of the
highest-income households was only 2.5%). Even
though middle-class and upper-class families now
bear less medical expense, the contradiction between
health needs and the payment ability of low-income
groups has intensified, and the economic risks have
not been effectively alleviated. They emphasized that
although the NCMS has implemented remarkable
results in health equity, financial protection for low-
income families still needs to be strengthened (Zhang
et al, 2021).
During the healthcare system integration phase,
empirical studies reveal that unifying urban-rural
medical coverage effectively improves beneficiaries’
self-assessed wellness, psychological conditions, and
clinical health indicators, while simultaneously
narrowing urban-rural health outcome gaps and
mitigating disparities across socioeconomic groups
(Zheng et al, 2021).
In terms of economic performance, out-of-pocket
medical expenses fell from 60 percent in 2001 to 35
percent in 2011, raising per capita income of farmers
participating in the NCMS by about 4 percent. The
rate of medical service usage, overall medical care,
and out-of-pocket medical costs all rise with the
incorporation of medical insurance (Yu, 2015; Qi,
2011; Ma & Li, 2021). Although the integration of
health care has improved health coverage, it has
exacerbated overall health inequalities, which tend to
ICPLSS 2025 - International Conference on Politics, Law, and Social Science
588

increase over time (He & Shen, 2021).
Cheng & Zhang pointed out that, taking the elderly
as an example, the NCMS has raised the rate of
medical care usage and considerably improved the
health of those who are insured by reducing the
phenomenon of abandoning medical care due to
poverty. However, actual medical expenditures have
not decreased significantly and the incidence of major
disease expenditures has not improved either. The
demand for medical services is relatively elastic,
resulting in price subsidies stimulating consumer
demand, offsetting the cost control effect, and limited
economic performance. The compensation
mechanism needs to be optimized to balance health
improvement and economic burden (Cheng & Zhang,
2012).
In summary, although the practice and integration
of the NCMS have accomplished remarkable results
in improving health, the insurance mechanism needs
to be further optimized to alleviate the outpatient
burden of insured farmers and to realize the
effectiveness of medical insurance through policy
publicity and resource coordination (Bei et al, 2024;
Zhang et al, 2024).
3.4.2 Poverty Reduction and Income
Distribution Effects
The NCMS’s regulatory implications for poverty
rates, catastrophic medical costs, economic
disparities, and the likelihood of unequal distribution
are made clear.
Qi systematically evaluated the poverty reduction
and income distribution effects of the NCMS based
on micro panel data from 30 provinces and regions
across the country from 2003 to 2006. His analysis
found that the NCMS significantly reduced the
probability of poverty at the farmer level and
contributed favorably to the decrease of poverty. By
reducing the economic disparity inside the village, the
NCMS simultaneously decreased the hamlet’s Gini
coefficient by 6.4%; nevertheless, this had no obvious
impact on the province’s overall income distribution.
Agriculturalists with low and intermediate earnings
are the primary beneficiaries of the NCMS’s income-
increasing effect, and they need to count on the
external economic climate for assistance, while high-
income farmers have limited benefits. This shows that
although the NCMS has effectively alleviated local
poverty and inequality within the village, higher-level
income distribution regulation still needs institutional
optimization and coordinated policy support (Qi,
2011).
Income redistribution is harmed by the basic
medical insurance system, even while medical
coverage helps to bridge the income gap caused by
growing medical expenditures. Additionally, rising
medical costs reduce the real impact of poverty
reduction. The effect varies from system to system
(Liao & Yu, 2021; Li et al, 2020).
In addition to the effectiveness of the NCMS, the
problem of reverse distribution among different
income groups is particularly prominent. For
instance, high-income groups benefit more from the
NCMS’s ability to reduce poverty, the introduction of
critical sickness insurance indirectly widens the
income gap, and the likelihood of catastrophic
medical expenses is negatively correlated with group
income (Luo & Yan, 2022; Zhao, 2021). In addition,
the program offers those with limited incomes only a
restricted degree of economic protection. In 2013,
China’s National Health Service Survey indicated
that 24.7% of the lowest-income families had medical
costs that accounted for more than 40% of their
income (while the highest-income families only had
2.5%) (Zhang et al, 2021). From this perspective, the
academic community is concerned that although the
NCMS has alleviated some poverty, the overall
catastrophic expenditure has not been improved well,
and it is necessary to balance the fairness of
distribution by strengthening the monitoring of
medical insurance integration, optimizing the
reimbursement ratio, improving the financing
mechanism and improving the level of protection for
low-income groups (Liu & Vortherms, 2017; Wang
et al, 2020; Jin et al, 2020).
3.5 Feedback Adjustment Level
Mainly includes analyzing the differentiated impact
of policies on urban and rural areas, income, age,
health behavior and other groups, highlighting the
problem of unequal benefits for vulnerable groups.
The policy effect of the NCMS also needs to focus
on the challenges of resource allocation and benefit
fairness. Since the high-income group’s poverty
vulnerability is effectively reduced while the low-
income group’s poverty is not, income stratification
has made the poverty reduction effect more
pronounced in this group. Beyond that, the earnings
growth of the wealthy individual class was much
more than that of those with reduced incomes (this is
referred to as the economically disadvantaged class
only rises by 5%, while the high-income group
increases by 10-15%) (Luo & Yan, 2022; Zhao,
2021). At the same time, differences in gender,
chronic diseases, age and other aspects also lead to
different poverty reduction effects, and the elderly
A Review of the New Rural Cooperative Medical Scheme Under the Background of Urban and Rural Medical Insurance Integration
589

group has a higher hospitalization rate, and the
outpatient rate of male insured persons is significantly
higher than that of female insured persons (Luo et al,
2021; Ding et al, 2023).
Taking Peng & Yue’s analysis as an example, they
focus on the group differences and structural equity
in the integration of the NCMS. Its primary
conclusion is that because of the significant
difference in the cost and use rate of inpatient
treatments throughout urban and agricultural areas,
there is a chance that reverse subsidies from rural to
urban medical insurance funds will occur after
medical insurance unification. Similarly, inequalities
in the risk-sharing system are exacerbated by the
differences in income and medical resources between
villages and towns. Therefore, they pointed out that
the integration of medical insurance must be careful,
by strengthening the system design and rural health
construction to promote the effectiveness of
integration (Peng & Yue, 2020).
To put it briefly, because of the regional and group
variations in the medical insurance system, distinct
security measures must be incorporated into the
policy design for various groups in order to integrate
the NCMS into medical security and further
encourage integration, such as vulnerable groups and
low-income groups, to accomplish the overall
equality of medical services (Huang & Wu, 2020;
Zhang et al, 2021; Zheng et al, 2021; Ma & Li, 2021).
4 MAIN CONTRIBUTIONS AND
DEFICIENCIES OF EXISTING
EXPLORES
4.1 Contributions
Existing exploration in the field of practice and
integration of the NCMS mainly reflects the
following important contributions:
Research confirms the beneficial effects of the
NCMS on rural inhabitants’ health and services,
while confirming that medical insurance integration
has effectively narrowed the urban-rural health
inequality. In addition, some explores have
accomplished the visualization of policy effects in the
population and spatial dimensions by constructing
policy transmission paths and analysis models. At the
level of constructing integration theory, some
literatures innovatively proposed different gradual
reform paths, systematically demonstrated the core
mechanisms such as the unification of the overall
coordination mechanism and the standardization of
management services, and provided theoretical
support for practical operations.
4.2 Limitations and Shortcomings
Although the existing investigations have made
significant progress, there are still the following
limitations and deficiencies:
The existing investigations appear insufficient on
regional links. Existing results mostly adopt the
macro-division method of the east, middle and west,
or analyze and investigate specific concentrated
areas, lack of systematic analysis on the adaptability
of policy tools to realize links between different
regions, and less attention to national-level plans and
actions to achieve transition based on distinct
principles.
Enhancement of the strategy’s outcome evaluation
mechanism is expected. Most explores are limited to
cross-sectional data analysis, and the long-term
effects of the integration of the NCMS are not tracked
enough. A standardized indicator system has not yet
been formed in terms of fund sustainability
assessment and service quality monitoring.
There is a gap in the analysis on micro-
mechanisms. Although existing literatures focus on
theoretical propositions of moral hazard, such as
induced medical demand, empirical investigations on
the behavioral decision-making patterns of insured
subjects and their policy awareness is still weak.
4.3 Explore Prospects
In view of some of the shortcomings shown in the
analysis, future investigations can pay additional
attention to the following aspects:
Quantitative investigation on regional
heterogeneity. In the view of the practical problem of
regional resource allocation differences as mentioned
above, the exploration should be based on the
traditional division of east, middle and west, and
explore a regional classification system that is more
in line with the needs of medical insurance policies.
That is, pay more attention to core indicators such as
economic level (per capita disposable
income/financial self-sufficiency rate), medical
resource density (number of beds per thousand
people/primary hospital coverage rate) and
population structure (aging rate/proportion of floating
population) at the county level, realize the spatial
division formulated according to different demand
levels to provide more accurate analysis for
differentiated compensation policies.
ICPLSS 2025 - International Conference on Politics, Law, and Social Science
590

Focus on cross-domain policy transmission
exploration. Exploration should pay more attention to
the balance of policy effects among regions. The
lagging of medical insurance policies in some regions
is not entirely due to financial capacity, but also
includes policy cognition gaps and administrative
coordination costs. The primary role of non-economic
issues in the progressive merger route and the health
care insurance system’s operation must be actively
investigated, and solutions and analysis must be
offered to make collaborative management a reality.
5 CONCLUSION
The relationship between integration and the
NCMS’s practical impact may be summed up as
follows, based on the aforementioned literature
overview, system integration analysis, and policy
impacts analysis:
The system integration reform focuses on overall
coordination and regional dynamic optimization,
which has significantly improved the health
performance and poverty reduction effects, but there
are conflicts in the reverse distribution of policy
effects and regional resource allocation differences,
that is, the overall efficiency and fairness
measurement problem.
The overall optimization design of the policy has
improved the overall situation in each region to a
certain extent, but the group differences within each
region, urban-rural differences, and differences in
resource allocation between regions are difficult to
effectively solve in a short period of time.
The accuracy of the medical insurance system
(involving various groups) and the reimbursement
mechanism must be considered in the real
optimization of the aforementioned issues; the
balance of policy effects between the east and the
west in regional coordination management; and to
discover benefit measures to deal with adverse
selection and social capital dependence.
In summary, institutional integration has driven
the optimization of policy effects through unified
standards, regional inclination, and dynamic
optimization, but its design flaws, such as insufficient
inclusiveness and low transparency, have generated
an imbalance in the distribution of health and
economic benefits. Future reforms need to be guided
by fairness while realizing two-way optimization of
institutional integration and policy effects through
precision, regional coordination, and transparency
measures.
REFERENCES
Bie, F., Yan, X., Qiu, W., Mao, A., Meng, Y., Cai, M.,
Yang, R., Zhang, Y. 2024. Does supplemental private
health insurance impact health care utilization and
seeking behavior of residents covered by social health
insurance? Evidence from China National Health
Services Survey. International Journal for Equity in
Health 23(1).
Cheng, L., Zhang, Y. 2012. The New Rural Cooperative
Medical Scheme: economic performance or health
performance? Economic Explore 47(01):120-133.
Ding, J., Zhang, B., Kang, Z. 2023. Can medical insurance
alleviate the poverty vulnerability of rural residents? --
From the Perspective of the Income and Expenditure
Effect of the New Rural Cooperative Medical Scheme.
Nankai Economic Research (07):49-69.
Gao, J., Ding, J. 2021. Can the New Rural Cooperative
Medical Scheme for Major Diseases Alleviate Long-
term Rural Poverty?—An Examination from the
Perspective of Poverty Vulnerability. Lanzhou Journal
(04):170-181.
General Office of the State Council of China. 2003. Notice
of the General Office of the State Council on
forwarding the opinions of the Ministry of Health and
other departments on establishing a new rural
cooperative medical system.
https://www.gov.cn/gongbao/content/2003/content_62
600.htm, last accessed 2025-3-20.
Gu, X., Zhou, Y. 2021. New Rural Cooperative Medical
Scheme: Adverse Selection and Moral Hazard.
Shanghai Financial Finance (02):15-25.
He, W., Shen, S. 2021. Does the integrated urban and rural
medical insurance policy alleviate health inequality? —
—Empirical evidence from a quasi-natural experiment
in prefecture-level cities in China. China Rural
Observation (03):67-85.
Huang, X., Wu, B. 2020. Impact of urban-rural health
insurance integration on health care: Evidence from
rural China. South China Economic Review 64.
Jin, S., Yu, J., Tian, R. 2020. Does China's basic medical
insurance system promote fair benefits? -- Empirical
Analysis Based on the Survey of Chinese Household
Finance. Quarterly Journal of Economics 19(04):1291-
1314.
Li, F., Wu, Y., Yuan, Q., Zou, K., Yang, M., Chen, D. 2020.
Do health insurances reduce catastrophic health
expenditure in China? A systematic evidence synthesis.
PLOS ONE 15(9).
Li, H., Li, Z. 2021. Does the integration of urban and rural
residents' medical insurance alleviate the poverty
caused by illness in rural areas? Modern Economic
Discussion (07):31-39.
Liao, Z., Yu, J. 2021. Explore on the income redistribution
effect of China's basic medical insurance system -
empirical analysis based on China's household financial
survey data. Explore on Financial Issues (07):57-65.
Liu, G.G., Vortherms, S.A., Hong, X. 2017. China's Health
Reform Update. Annual Review of Public Health
38:431-448.
A Review of the New Rural Cooperative Medical Scheme Under the Background of Urban and Rural Medical Insurance Integration
591

Luo, D., Deng, J., Becker, E.R. 2021. Urban-rural
differences in healthcare utilization among
beneficiaries in China's new cooperative medical
scheme. BMC Public Health 21(1).
Luo, D., Yan, S. 2022. New Rural Cooperative Medical
Scheme, catastrophic medical expenditure and poverty
vulnerability. Taxation and Economy (01):69-76.
Ma, W., Li, H. 2021. From the New Rural Cooperative
Medical Scheme to the basic medical insurance for
urban and rural residents: an analysis of the policy
effects of urban and rural medical insurance integration.
Chinese Economic Issues (04):146-157.
Meng, Y., Yu, R., Bai, H., Han, J. 2024. Evidence From the
China Family Panel Studies Survey on the Effect of
Integrating the Basic Medical Insurance System for
Urban and Rural Residents on the Health Equity of
Residents: Difference-in-Differences Analysis. JMIR
Public Health and Surveillance 10.
Office of the People's Government of Lanzhou City. 2011.
Statistical Communiqué of the People's Republic of
China on the National Economic and Social
Development in 2010(3).
https://tjj.lanzhou.gov.cn/art/2011/12/12/art_4850_311
628.html, last accessed 2025-3-20.
Peng, H., Yue, J. 2020. Integration of China's basic medical
insurance system: theoretical debate, practical progress
and future prospects. Academic Monthly 52(11):55-65.
Qi, L. 2011. Explore on the poverty reduction, income
increase and redistribution effects of the New Rural
Cooperative Medical Scheme. Explore on Quantitative
and Technical Economics 28(08):35-52.
Qiu, Y., Zhai, S., Hao, J. 2011. Explore on the coordinated
development of urban and rural medical insurance:
theory, empirical evidence and countermeasures. China
Soft Science (04):75-87.
Ren, Y., Zhou, Z., Cao, D., Ma, B., Shen, C., Lai, S., Chen,
G. 2022. Did the Integrated Urban and Rural Resident
Basic Medical Insurance Improve Benefit Equity in
China? Value in Health 25(9):1548-1558.
State Council of China. 2016. Opinions of the State Council
on integrating the basic medical insurance system for
urban and rural residents.
https://www.gov.cn/zhengce/zhengceku/2016-
01/12/content_10582.htm, last accessed 2025-3-22.
Wang, J., Zhu, H., Liu, H., Wu, K., Zhang, X., Zhao, M.,
Yin, H., Qi, X., Hao, Y., Li, Y., Liang, L., Jiao, M., Xu,
J., Liu, B., Wu, Q., Shan, L. 2020. Can the reform of
integrating health insurance reduce inequity in
catastrophic health expenditure? Evidence from China.
International Journal for Equity in Health 19(1).
Xiong, J. 2022. Competitive Allocation of Welfare Benefits
of New Rural Cooperative Medical System
Participants. Agricultural Technology and Economy
(10):40-52.
Yan, X., Liu, Y., Cai, M., Liu, Q., Xie, X., Rao, K. 2022.
Trends in disparities in healthcare utilisation between
and within health insurances in China between 2008
and 2018: a repeated cross-sectional study.
International Journal for Equity in Health 21(1).
Yip, W., Hsiao, W.C. 2009. Non-evidence-based policy:
How effective is China's new cooperative medical
scheme in reducing medical impoverishment? Social
Science & Medicine 68(2):201-209.
Yu, H. 2015. Universal health insurance coverage for 1.3
billion people: What accounts for China's success?
Health Policy 119(9):1145-1152.
Yuan, B., Jian, W., Martinez-Alvarez, M., McKee, M.,
Balabanova, D. 2020. Health system reforms in China
a half century apart: Continuity but adaptation. Social
Science & Medicine 265.
Zhai, F. 2021. Divergence and Choice: The Basic Principles
of my country's Integrated Universal Health Insurance
System. Medicine and Philosophy 42(05):45-50.
Zhang, J., Luo, J., Chen, G., Zhang, C., Wang, J., Li, L.
2024. High-quality Development of Public Health in
Guizhou Province, China. Journal of Resources and
Ecology 15(4):925-936.
Zhang, Y., Dong, D., Xu, L., Miao, Z., Mao, W., Sloan, F.,
Tang, S. 2021. Ten-year impacts of China's rural health
scheme: lessons for universal health coverage. Global
Health 6(4).
Zhao, W. 2021. The impact effect and transmission
mechanism of social medical insurance on rural
residents' income - empirical evidence from the New
Rural Cooperative Medical Scheme for serious
illnesses. Financial Forum (06):56-66.
Zheng, C., Wang, X., Sun, Q. 2021. Explore on urban and
rural medical insurance pooling policy, residents' health
and health inequality. Nankai Economic Explore
(04):234-256.
ICPLSS 2025 - International Conference on Politics, Law, and Social Science
592
