
The Impact of Stigmatization of Mental Disorders on the Public's
Self-Perception
Zixuan Liu
College of Traditional Chinese Medicine, Faculty of Chinese Medicine Science Guangxi University of Chinese Medicine,
Nanning, 530000, China
Keywords: Stigma, Stigmatization, Depression.
Abstract: Objective: This research endeavours to explore whether the public's stigmatization of mental disorders exerts
an influence on the public's evaluation of their own mental states. Methods: A questionaire was designed, and
223 subjects will be recruited via convenience sampling on the Internet as the research participants. The
Perceived Devaluation-Discrimination Scale (PDDS), adapted by Zuo Bin from Link's original, will be
employed. Based on the scores obtained, the subjects will be categorized into a high group and a low group.
Subsequently, the Self-Rating Depression Scale (SDS) will be utilized to analyze the participants' perception
of their own mental states within the two groups. Results: In this study, 167 questionnaires were screened for
analysis. The mean score of the subjects on the Public Stigmatization Scale was (28.74 ± 5.84), and that on
the Self-Rating Depression Scale was (46.14 ± 10.33). The average score of the SDS scale for the subjects in
the low group was (48.53 ± 1.24), while that for the subjects in the high group was (44.15 ± 1.00). Conclusion:
Groups that are more perceptive of the stigmatization of mental disorder patients in society tend to experience
greater psychological stress as a consequence.
1 INTRODUCTION
Mental disorders constitute a prevalent and life-
threatening ailment (Askelund et al., 2019). Research
indicates that the lifetime prevalence rate of
depression in China reaches 6.9% (Huang et al.,
2019). Additionally, due to the exorbitant costs
associated with hospitalization, medication, and
nursing care for mental disorder patients, it imposes a
substantial burden on both families and society
(König et al., 2020). The World Health Organization
(WHO) reported in 2022 that mental disorders
currently represent the primary cause of disability-
adjusted life years, accounting for approximately one-
sixth of the global disability-adjusted life years.
Concurrently, the stigma prevalent in the mental
health domain is perturbing the public's perception of
their own mental states (Shi & Jiang, 2023). The
negative emotional experience engendered by this
stigmatization phenomenon induces certain
individuals to endure greater mental stress, and may
even impede potential mental disorder patients from
seeking assistance (Makowski & Knesebeck, 2023,
Zhang et al., 2020, Colizzi et al., 2020).
In 1963, Erving Goffman initially introduced the
concept of stigmatization. He explicitly defined
stigmatization as the act of affixing negative labels to
an entire group, thereby fostering a negative
stereotype (Goffman).
Prior research on group emotions has
demonstrated that negative emotions can proliferate
directly within groups and progressively shape the
collective perception of various matters (Barsade &
Gibson, 1998). The stigmatization of certain
phenomena emerges during this process (Zeng & Li,
2020). With the advancement of psychology,
although the public's cognizance of psychological
phenomena has witnessed an increment, the public's
stigmatization of mental disorders persists (Maharjan
& Panthee, 2019). This pervasive stigmatization
phenomenon has given rise to the emergence of
stigma among relevant patients, and has also
compelled individuals with mild psychological issues
to withstand greater psychological pressure
(Mukhopadhyay & Mukherjee, 2018).
The concept of stigma was proposed by Corrigan.
Corrigan's research bifurcated stigma into public
stigma, stemming from the stigmatization
phenomenon induced by external negative
impressions, and self-stigma, which patients develop
towards themselves due to their affliction with
diseases (Corrigan, 2004). This study is designed to
430
Liu, Z.
The Impact of Stigmatization of Mental Disorders on the Public’s Self-Perception.
DOI: 10.5220/0014120500004942
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 2nd International Conference on Applied Psychology and Marketing Management (APMM 2025), pages 430-434
ISBN: 978-989-758-791-7
Proceedings Copyright © 2026 by SCITEPRESS – Science and Technology Publications, Lda.

investigate the current public awareness regarding the
stigmatization of mental disorders and to explore
whether public stigma impacts individuals' perception
of their own mental states.
2 METHODS
2.1 Sample
The present research employed a questionnaire-based
survey approach, whereby subjects were randomly
recruited as research participants on the Chinese
Internet through convenience sampling. The inclusion
criteria were stipulated as follows: (1) Absence of any
prior history of mental disorders; (2) Attainment of an
educational level at least equivalent to primary
school; (3) Absence of overt intellectual impairments
and possession of the capacity to comprehend the
scale content. A total of 223 questionnaires were
amassed in the course of this study, among which 167
valid responses, characterized by earnest completion,
were screened out, yielding an efficacy rate of 75%
(rounded to two decimal places).
2.2 Tools
2.2.1 Perceived Devaluation-Discrimination
Scale, (PDDS)
In this investigation, the Public Stigmatization Scale
was utilized to explore the subjects’ perception of
the degree of stigmatization associated with mental
disorders (Zuo & Ai, 2011). This scale was modified
by Zuo Bin from the Perceived Devaluation-
Discrimination Scale devised by Link et al. (Link et
al., 1987) The entire scale adopts a 4-level scoring
system and comprises 12 items, with 6 of them being
reverse-scored.
2.2.2 Self-Rating Depression Scale, (SDS)
The SDS was deployed in this study to dissect the
subjects’ perception of their own mental states. This
scale is constituted of 20 straightforward
interrogatives and employs a 4-level scoring regimen,
principally aiming to evaluate the frequency and
severity of symptomatology (Xin et al., 2012). Each
entry is scored in accordance with the sequence of 1,
2, 3, and 4, such that a greater score corresponds to a
higher frequency and severity of symptom
manifestation. Among these, 10 questions necessitate
reverse scoring, and the average score is adopted for
statistical outcomes. It has been empirically validated
that this scale exhibits sound reliability and validity,
with a Cronbach’s α coefficient of 0.842 and a test-
retest reliability correlation coefficient of 0.809 (Liu
et al., 2021).
2.3 Statistical Analysis
SPSS 29.0 statistical software was harnessed for data
analysis in this study. Quantitative data were
expressed in the form of mean ± standard deviation.
The t-test was implemented for comparisons between
the two groups, while multiple linear regression
analysis was employed for multivariate exploration,
with p < 0.05 serving as the benchmark for statistical
significance.
3 RESULTS
3.1 Basic Information
A total of 167 subjects were screened out. Among
them, the age range of the subjects was from 18 to 49
years old, with a mean age of (23.04 ± 3.64) years.
In terms of gender distribution, there were 100 male
cases and 67 female cases.
3.2 Grouping Information
Through the analysis of statistical data, the mean
PDDS score of all subjects was ascertained as (28.74
± 5.84). In the current study, based on the PDDS
scores of the subjects, 76 datasets with scores below
the average were incorporated into the low group, and
91 datasets with scores above the average were
incorporated into the high group. According to the
scores on the Public Stigmatization Scale, it was
revealed that the low group exhibited a more
pronounced perception of the stigmatization of
mental disorders, whereas the high group manifested
a relatively milder perception.
3.3 Data Comparison
The average score per item on the SDS scale for the
subjects in the low group was (2.43 ± 0.54), and that
for the subjects in the high group was (2.21 ± 0.48).
The results are presented in the following table.
The Impact of Stigmatization of Mental Disorders on the Public’s Self-Perception
431
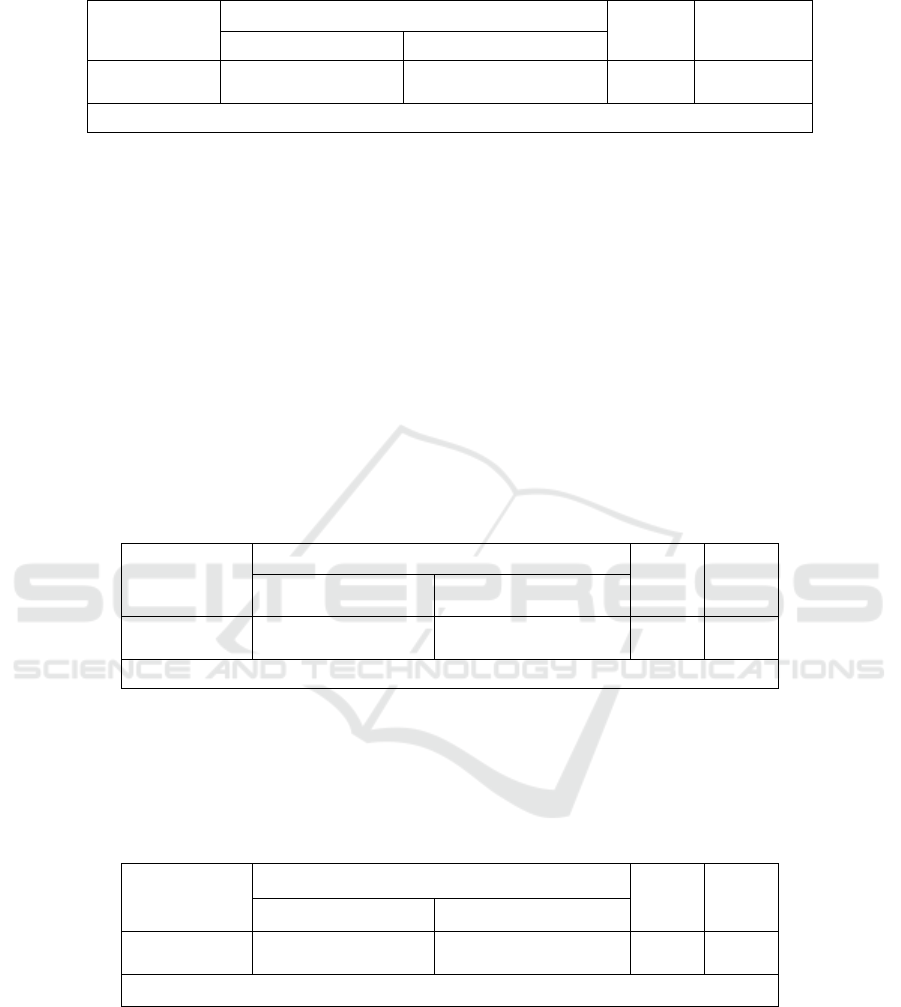
Table 1: T-test analysis results.
PDDS (Mean ± Standard Deviation) t p
low group (n = 76) high group (n = 91)
SDS Average
Score
2.43±0.54 2.21±0.48 2.78 0.01**
* p<0.05 ** p<0.01
From the above Table 1, the independent samples
t-test was employed to explore the disparity in the
average SDS score among different PDDS average
score groups. It can be discerned from the table that a
significant difference (p < 0.05) was observed in the
average SDS score among different PDDS average
score groups. More specifically, a highly significant
difference at the 0.01 level (t = 2.778, p = 0.006) was
detected in the average SDS score among different
PDDS average score groups. Furthermore, upon
detailed comparison, it was evident that the average
score per item on the SDS scale for the low group
(2.43) was markedly higher than that for the high
group (2.21).
3.4 Analysis of Factors Influencing
Subjects' Perception of Their Own
Mental States
3.4.1 Univariate Analysis
The subjects were categorized by age (Li et al., 2024).
Employing the independent samples t-test, an
exploration was conducted into the disparity in the
average SDS score for a single item among diverse
age cohorts. It could be deduced that no significant
divergence (p > 0.05) was manifested in the average
SDS score across different age groups. The specific
details are presented as shown in Table 2:
Table 2: T-test analysis results.
Age (Mean ± Standard Deviation) t p
Above 25 years old (n
= 41
)
Below 25 years old (n =
126
)
SDS Average
Score
2.35±0.47 2.29±0.53 0.61 0.54
* p<0.05 ** p<0.01
Subsequently, the independent samples t-test was
utilized to scrutinize the difference in the average
SDS score for one item between disparate genders.
The resultant data indicated that a significant
discrepancy (p < 0.05) prevailed in the average SDS
score among samples of different genders. The
outcomes are tabulated below:
Table 3: T-test analysis results.
Gender (Mean ± Standard Deviation) t p
Female (n = 67) Male (n = 100)
SDS Average
Score
2.48±0.50 2.19±0.50 3.67 0.00**
* p<0.05 ** p<0.01
It is discernible from the above Table 3 that gender
exhibited a significance at the 0.01 level with respect
to the average SDS score (t = 3.665, p = 0.000).
Through meticulous comparison, it was ascertained
that the average value for females (2.48) was
conspicuously higher than that for males (2.19).
3.4.2 Multivariate Analysis
Gender, age, and the average PDDS score were
designated as independent variables, while the
average SDS score served as the dependent variable
for the purpose of conducting a linear regression
analysis. The particulars are expounded as shown in
Table 4:
APMM 2025 - International Conference on Applied Psychology and Marketing Management
432
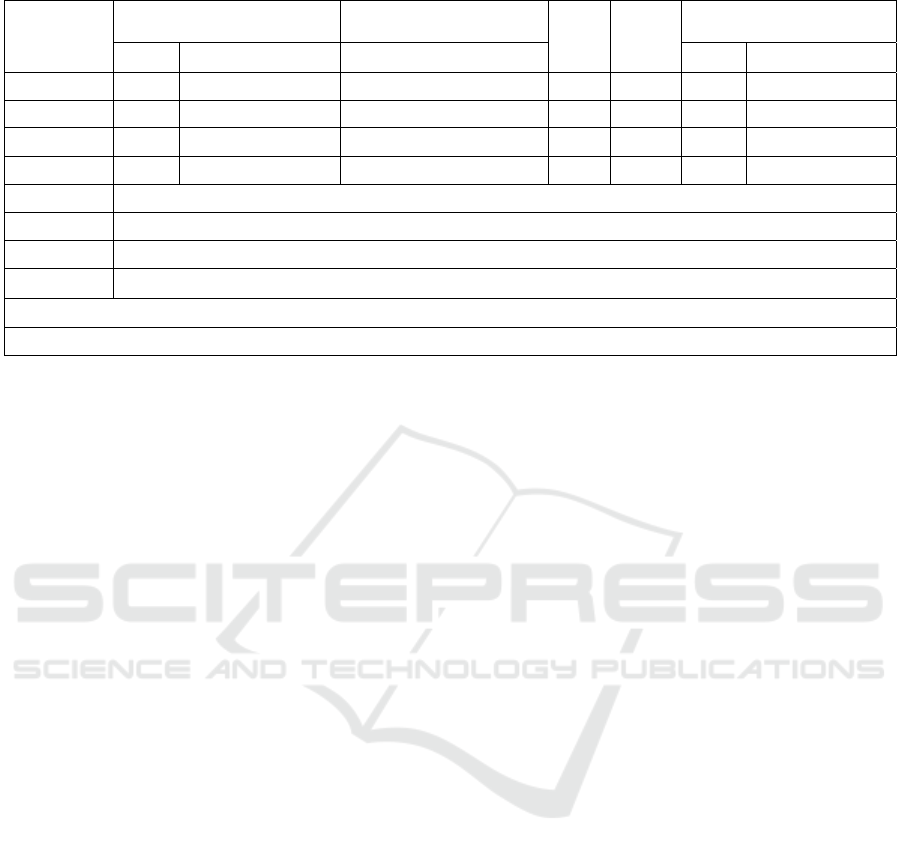
Table 4: Linear regression analysis results (n = 167).
Unstandardized Coefficients Standardized Coefficients
t p
Collinearity Diagnosis
B
Standard Error
Beta VIF
Tolerance
Constant
3.78 0.34 - 10.99 0.00** - -
Gender
-0.28 0.08 -0.27 -3.62 0.00** 1.04 0.96
Age
-0.02 0.01 -0.11 -1.46 0.14 1.03 0.97
PDDS -0.28 0.08 -0.26 -3.64 0.00** 1.01 0.99
R 2
0.15
Adjusted R²
0.14
F F (3,163)=9.80,p=0.00
D-W Value
1.78
Note: Dependent Variable = SDS
* p<0.05 ** p<0.01
It can be gleaned from the above table that the
model formula is: SDS average score = 3.776 - 0.280
* gender - 0.015 * age - 0.280 * PDDS average
score.R² = 0.153, signifying that gender, age, and the
average PDDS score can elucidate 15.3% of the
variance in the average SDS score. Upon subjecting
the model to a multicollinearity test, it was
ascertained that all VIF values within the model were
less than 5, intimating the absence of a collinearity
issue. Moreover, the D-W value hovered around 2,
thereby suggesting that the model was devoid of
autocorrelation and that no correlation subsisted
among the sample data, rendering the model
satisfactory.
In summary, gender and PDDS score have a
significant negative bearing on the SDS score of the
subjects, whereas age does not have an impact on the
SDS score of the subjects.
4 DISCUSSION
Mental disorders, being ailments that imperil human
life and safety, give rise to crucial inquiries regarding
how to mitigate the morbidity risk among the general
populace and augment the prospects of recovery for
individuals afflicted with such disorders. These
inquiries warrant profound exploration. The
stigmatization of mental disorders, manifesting as a
phenomenon with the potential to impinge upon the
public's self-perceptual faculties and attenuate
patients' self-esteem as well as their inclination to
seek medical recourse, merits earnest consideration
(Li et al., 2023).
In the present study, questionnaires were
disseminated with the objective of probing into the
influence of the stigmatization phenomenon on the
public's self-perception. Subsequently, 167
questionnaire responses were amassed and
meticulously screened. Thereafter, predicated on the
PDDS scores of the subjects, they were bifurcated
into a high group and a low group. Notably, the mean
score per item on the SDS for the low group (2.43)
was markedly superior to that of the high group
(2.21).
The independent samples t-test was enlisted to
authenticate the disparities, and the resultant
deduction was that a statistically significant
difference (p < 0.05) was evinced in the average SDS
score among the subject samples of diverse
experimental cohorts. It is posited that groups that
exhibit a heightened awareness of the stigmatization
of mental disorder patients within society are
predisposed to endure more pronounced
psychological duress when engaged in self-
assessment of their mental states.
When the t-test was deployed to dissect gender-
based variances, a significance at the 0.01 level was
manifested for the average SDS score (t = 3.665, p =
0.000). Through comparative analysis, it becomes
evident that the mean value for females (2.48) was
conspicuously greater than that for males (2.19).
Antecedent research has unequivocally established
that women are characteristically more prone to detect
stigma and the stigmatization of mental disorders, a
finding that dovetails with and corroborates the
conclusion derived from this study (Feng et al., 2022).
The Impact of Stigmatization of Mental Disorders on the Public’s Self-Perception
433

5 CONCLUSION
In conclusion, data were collected and analyzed
through questionnaire surveys and convenience
sampling in this study. The designed survey proved
that the stigmatization phenomenon has a negative
influence on the self-perception of the public.
Furthermore, in the collected research samples,
gender has become one of the factors influencing the
self-perception of the subjects. It is necessary to call
on society to reduce the prejudice and discrimination
against mental illness through education, publicity
and policy advocacy. By doing so, the incidence rate
of mental disorders can be curtailed, and the self-
efficacy and propensity of patients with mental
disorders to seek medical attention can be enhanced.
REFERENCES
A. D. Askelund, S. Schweizer, I. M. Goodyer, & others.
Positive memory specificity is associated with reduced
vulnerability to depression. Nat. Hum. Behav., 3(3),
265–273. (2019)
Y. Huang, Y. Wang, H. Wang, Z. Liu, X. Yu, J. Yan, … Y.
Wu. Prevalence of mental disorders in China: A cross-
sectional epidemiological study. Lancet. Psychiatry,
6(3), 211–224. (2019)
H. König, H.-H. König, & A. Konnopka. The excess costs
of depression: A systematic review and meta-analysis.
Epidemiol. Psychiatr. Sci., 29, e30. (2020)
S. Shi, & Y. Jiang. Research progress on stigma in patients
with depression. Chin. J. Health. Educ., 11(11), 1023–
1026. (2023)
A. C. Makowski, & O. von dem Knesebeck. Public
depression stigma does not vary by symptom severity.
J. Ment. Health., 32(2), 434–442. (2023)
Z. Zhang, K. Sun, C. Jatchavala, J. Koh, Y. Chia, J. Bose,
… R. Ho. Overview of stigma against psychiatric
illnesses and advancements of anti-stigma activities in
six Asian societies. Int. J. Environ. Res. Public. Health.,
17(1), 280. (2020)
M. Colizzi, M. Ruggeri, & A. Lasalvia. Should we be
concerned about stigma and discrimination in people at
risk for psychosis? A systematic review. Psychol. Med.,
50(5), 705–726. (2020)
E. Goffman. Stigma: Notes on the management of spoiled
identity. Postgrad. Med. J., 47(542), 642–642. (n.d.)
S. G. Barsade, & D. R. Gibson. Group emotion: A view
from top and bottom. Unpublished manuscript. (1998)
X. Zeng, & L. Li. Stigma and stigmatization in international
relations. Int. Political. Sci., 3, 78–111. (2020)
S. Maharjan, & B. Panthee. Prevalence of self-stigma and
its association with self-esteem among psychiatric
patients in a Nepalese teaching hospital: A cross-
sectional study. BMC. Psychiatry, 19(1), Article 347.
(2019)
D. Mukhopadhyay, & S. Mukherjee. Stigma towards mental
illness: A hospital-based cross-sectional study among
caregivers in West Bengal. Indian. J. Public. Health.,
62(1), 15. (2018)
P. Corrigan. How stigma interferes with mental health care.
Am. Psychol., 59(7), 614–625. (2004)
B. Zuo, & C. Ai. The relationship between group identity,
self-esteem, and mental illness stigma. Chin. J. Appl.
Psychol., 17(4), 299–303. (2011)
B. G. Link, F. T. Cullen, I. Frank, & J. F. Wozniak. The
social rejection of former mental patients:
Understanding why labels matter. Am. J. Sociol., 92(6),
1461–1500. (1987)
L. Y. Xin, C. L. Hou, R. M. Wang, R. L. Lan, & M. Y. Lü.
Factor structure analysis of the Self-Rating Depression
Scale and its influencing factors. Chin. J. Health.
Psychol., 20(10), 1521–1523. (2012)
B. Y. Liu, J. Zhao, & D. Zheng. Study on the accuracy of
HAMD and SDS in distinguishing the severity of
depression. Chongqing. Med., 50(18), 3174–3177,
3181. (2021)
H. Y. Li, S. Y. Wen, X. M. Chen, J. M. Qiu, X. Y. Song, X.
L. Kuang, & L. Q. Gu. Analysis of the current status and
related influencing factors of stigma levels in patients
with depression. China. Mod. Med., 31(8), 118–121.
(2024)
L. Li, Z. Zhang, & F. Li. Correlation analysis of
stigmatization and help-seeking behavior in patients
with depression. Psychol. Monthly, 16, 119–122.
(2023)
L. Feng, Y. P. Huang, & G. B. Zheng. Current status and
influencing factors of stigma among patients with
depression. China. Med. Innov., 19(33), 90–93. (2022)
APMM 2025 - International Conference on Applied Psychology and Marketing Management
434
