
DRLPARTO: A Machine Learning Based Partograph for Fetal
Monitoring System
Deepa J., Nandhyala Geetha Reddy, P. Sai Kiran and P. V. Sai Ram Reddy
Department of Information Technology, Vel Tech Rangarajan Dr. Sagunthala R&D Institute of Science and Technology,
Avadi, Chennai, Tamil Nadu, India
Keywords: Partograph, Labor, Fetal, Delivery, Prediction, Amniotic Fluid, Cervix Dilation.
Abstract: The review focuses on predicting the mode of delivery using machine learning techniques. Our approach
involves developing a machine learning model that evaluates partograph data to anticipate possible
complications or the necessity for medical interventions. Although various perspectives exist on the
application of partographs, a comprehensive understanding of their implementation remains unclear. The
proposed model assesses multiple parameters, considering the mother’s health status, fetal condition, and the
ongoing labor progression. The primary goal is to identify the most effective algorithms for predicting
delivery outcomes, specifically distinguishing the types of delivery i.e, normal or cesarean deliveries using
machine learning techniques. Supervised learning algorithms such as Decision Trees, Random Forest, and
Logistic Regression were employed with the proposed method DRLPARTO achieving 93% accuracy and
consistently high precision, recall, and F1 score (92-93%), demonstrating its robustness and effectiveness in
the given task.
1 INTRODUCTION
A partograph is a tool used to track labor progress and
monitor the health of both the mother and baby. It
records data in a graphical format, helping doctors
make decisions if complications arise during
childbirth. To predict delivery outcomes, we develop
machine learning models using parto- graph data.
According to the Government of India, around 1.3
million Indian women have died during childbirth in
the past two decades due to various reasons. The
partograph plays a crucial role in understanding the
health of the mother and baby, identifying
complications early, and making labor safer. It also
helps healthcare workers better understand labor
patterns.
Partographs have been the subject of extensive
research, but because of a lack of standardized
implementation, their practical application is still
restricted. The goal is to close the gap between data-
driven insights and practical clinical decision-making
by incorporating machine learning into partograph
analysis. The results demonstrate artificial
intelligence's potential.
If we can predict the type of delivery (normal or
C-section), we can prevent unnecessary medical
complications, ensuring the safety of both the mother
and baby. This also reduces risks during childbirth
and helps lower death rates. The World Health
Organization (WHO) supports monitoring active
labor and encourages new approaches during this
phase. The main goal of this project is to analyze
health conditions during labor and predict the
delivery type using machine learning. To understand
why partographs are important, we must look at their
history. The idea of recording labor progress in a
graph started in 1952 when Dr. Emanuel Friedman
couldn’t be present for his first child’s birth due to
work. He contacted the hospital frequently and
recorded his wife’s cervical dilation on a graph. He
continued observing all women in the maternity ward
throughout the night. Though contraction frequency
wasn’t very informative, he noticed that cervical
dilation followed an S-shaped curve, now called the
“sigmoid curve.” Since his first recording happened
on the day his child was born, the concept of the curve
is believed to have started in 1952.
Friedman later decided to divide labor into two
phases: latent and active, published a study analyzing
100 women, recording cervical dilation and
contractions per centimeter. This graph became
known as the “Friedman Curve” or “cardiograph”. In
J., D., Reddy, N. G., Kiran, P. S. and Reddy, P. V. S. R.
DRLPARTO: A Machine Learning Based Partograph for Fetal Monitoring System.
DOI: 10.5220/0013932800004919
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Research and Development in Information, Communication, and Computing Technologies (ICRDICCT‘25 2025) - Volume 5, pages
553-558
ISBN: 978-989-758-777-1
Proceedings Copyright © 2026 by SCITEPRESS – Science and Technology Publications, Lda.
553
1955, this study expanded to 500 women and
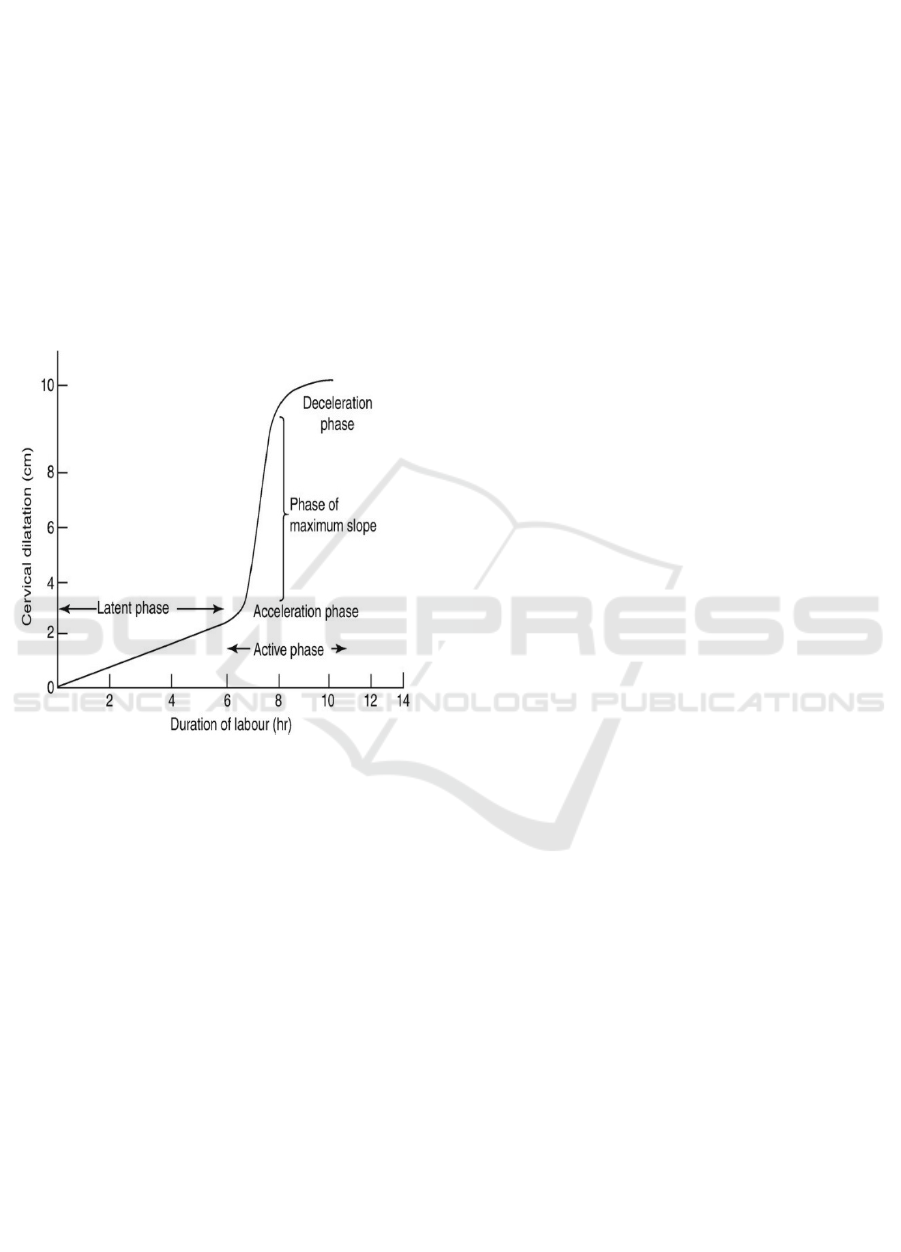
published another research paper. Figure 1 shows
Phases of Labour representation.
Friedman divided labor into four phases based on
cervical dilation as in Figure 1:
• Latent phase - Slow dilation (up to 2.5 cm).
• Acceleration phase - Rapid dilation with a
change in speed.
• Maximum slope - The cervix dilates steadily
in a straight- line pattern.
• Deceleration phase - The cervix is fully
dilated, and the rate of dilation slows down.
Later, Dr. Philpott developed a partograph
based on Friedman’s curve. He introduced
two lines:
Figure 1: Phases of labor representation.
The alert line, which acts as a warning. The action
line, which signals the need for medical intervention
if crossed. This system was later introduced in
England, where British gynecologist John Studd
made modifications. He replaced the alert and action
lines with a nomogram that used cervical dilation at
the time of admission as a reference.
In 1994, the World Health Organization (WHO)
officially approved the partograph. They
recommended its use in all labor wards to ensure safer
deliveries. This recommendation was based on a
study involving over 35,000 women. The use of
partographs significantly reduced maternal and infant
deaths and lowered the risks of prolonged labor. The
WHO also introduced an updated version called the
labor scale, which helps study labor conditions in
more detail. This is how the partograph has evolved
and developed over the years, becoming a vital tool
in maternal healthcare.
Section 2 provides an overview of related work,
while Section 3 outlines the proposed methodology.
The results and findings are discussed in Section 4,
and the conclusion is presented in Section 5.
2 RELATED WORKS
Khali et al. (2022) evaluated a digital version of the
partograph for labor management. The goal was to
enhance labor quality and prevent complications by
ensuring accurate monitoring. The study, which
involved 800 women, found that the average delivery
duration was 3.5 hours for first-time mothers and 3.3
hours for those who had given birth before. The
average participant age was 25.6 years, with an
average parity of 2. The findings showed that the
digital partograph effectively improved labor
management and newborn health outcomes.
Ashour E.S. et al. (2023) conducted a study in
Egypt to compare digital and paper-based
partographs. They found that digital partographs
improved maternity nurses’ performance, ensuring
better documentation and timely interventions.
Additionally, digital tools led to better maternal and
neonatal outcomes, reducing cesarean sections and
newborn intensive care admissions. The study
suggested that adopting digital partographs in labor
wards could enhance maternal and newborn health in
other regions.
Bedwell et al. (2017) analyzed the effectiveness
of the partograph in labor monitoring. Their review
followed five steps: defining the research scope,
gathering evidence, evaluating primary studies,
synthesizing findings, and sharing results. They
reviewed 95 sources, including research papers,
policies, audits, and expert opinions. The findings
showed that while the partograph is useful for
tracking labor, its effectiveness depends on factors
like healthcare worker competency and acceptance.
GJ Hofmeyr et al. (2021) introduced a new
approach to labor monitoring called the next-
generation partograph. This tool aims to offer
personalized care, focusing on respectful maternity
services. Key features include considering individual
differences in labor progression and setting
intervention triggers based on the health of the mother
and baby. The model promotes better communication
between healthcare providers and laboring women.
The study argues that adopting this advanced
partograph could improve health outcomes and
patient satisfaction.
Melese et al. (2020) studied the use of the
partograph in Southern Ethiopia. The research
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
554

assessed healthcare workers’ knowledge, attitudes,
and usage of the tool in obstetric care. While most
participants were aware of the partograph, their
willingness to use it was inconsistent. The study
found that factors such as equipment availability,
workload, and training influenced its use. The authors
emphasized the need to promote partograph use in
healthcare facilities to improve childbirth outcomes.
Lavender T et al. (2020) examined the role of the
partograph in labor management. Their study
discussed the history of the partograph, its challenges,
and its effectiveness in improving childbirth
outcomes. They explored different versions of the
partograph and the factors that affect its success. The
paper also suggested best practices and future
research directions to enhance labor monitoring tools.
The authors supported their conclusions with
references to multiple studies.
Xiaoqing He et al. (2023) reviewed 62 studies to
gain new insights into labor patterns. Their research
challenged traditional labor curves and definitions of
abnormal labor. The review emphasized that recent
studies suggest abnormal labor cannot always be
determined based on a standard labor curve. This has
significant implications for global childbirth care
practices.
Yeliz Dog˘an Merih et al. (2023) developed the
Electronic Touch and Partograph Device, an
innovation that combines vaginal examination with
digital labor monitoring. This device can track up to
50 patients simultaneously, ensuring real-time data
collection. Developed between 2016 and 2020, the
device underwent extensive research and ethical
reviews. It improves safety for both healthcare
workers and pregnant women, offering a promising
advancement in labor monitoring technology.
Singh et al. (2022) conducted a quality
improvement initiative to increase the use of the
modified WHO partograph in labor rooms. The aim
was to improve maternal and neonatal outcomes by
ensuring regular labor monitoring. The team
identified reasons for low partograph usage and
introduced solutions such as allocating triage rooms,
training staff, involving interns and nurses, setting
clear policies, and designating supervisory roles. As
a result, partograph usage increased from 25 Percent
to 95 Percent. Despite challenges like printer
malfunctions and misplaced documents, the initiative
successfully improved labor care quality.
Shivani Sharma et al. (2022) focused on
improving maternal health through a new partograph
model. The study aimed to reduce preventable
maternal deaths by identifying abnormal labor early
and providing timely interventions. Researchers
developed and validated a reliable partograph, which
proved effective in improving childbirth outcomes.
The study recommended widespread adoption of
partographs in labor monitoring to enhance maternal
and newborn safety.
3 PROPOSED SYSTEM
The traditional approach to labor monitoring
primarily relies on manual partograph recording to
track the progress of labor and ensure maternal and
fetal well-being. A partograph is a standardized tool
used by healthcare providers to document key
parameters such as cervical dilation, fetal heart rate,
uterine contractions, and maternal vital signs at
regular intervals. In conventional systems, paper-
based partographs are widely used in hospitals and
maternity wards. Healthcare professionals manually
record observations and assess labor progression
based on predefined thresholds. If abnormal labor
patterns are detected, appropriate clinical
interventions are initiated. However, this manual
process is prone to human errors, inconsistencies in
data recording, and delays in decision making.
Despite its importance, the adoption and effective
utilization of partographs remain limited due to
several challenges. These include insufficient
training, high workload on healthcare staff, and a lack
of standardized monitoring protocols. Additionally,
paper-based partographs lack real-time analysis and
do not provide predictive insights that could help
anticipate complications in labor.
Furthermore, while some digital partograph
solutions have been introduced, their adoption is still
in early stages. Many healthcare facilities continue to
rely on traditional manual methods, which may not
provide the level of efficiency required for modern
obstetric care. Thus, the existing labor monitoring
system heavily depends on manual data entry and
fixed threshold-based decision making, making it less
adaptable to variations in labor progression and real
time clinical needs. There is a growing necessity for
intelligent, automated, and predictive solutions that
can enhance the accuracy and efficiency of labor
monitoring, ultimately improving maternal and
neonatal outcomes.
The primary objective of this work is to develop a
machine learning model that analyzes partograph data
to predict potential complications during labor and
determine the need for medical interventions. The
model evaluates various maternal and fetal
parameters, including maternal status, fetal condition,
and labor progression, to classify the delivery type as
DRLPARTO: A Machine Learning Based Partograph for Fetal Monitoring System
555

either normal or cesarean. To achieve this, the study
leverages advanced machine learning techniques to
process and interpret partograph data effectively. The
system is designed to identify crucial patterns that
indicate deviations from normal labor, enabling
timely medical decisions. Various machine learning
algorithms are assessed to determine the most
accurate model for delivery type prediction.
This research aims to bridge the gap between
theoretical understanding and practical
implementation of partographs in clinical settings. By
integrating machine learning into obstetric care, the
system enhances decision-making, improves
maternal and fetal health outcomes, and reduces risks
associated with labor. Through extensive
experimentation and validation, this study contributes
to the advancement of intelligent healthcare solutions
for maternity care.
3.1 Methodology
Upon analyzing the reviewed research papers, it is
evident that multiple methodologies and techniques
have been applied to understand and implement the
partograph. However, despite numerous studies and
recorded data, the actual implementation remains
limited. To improve the effectiveness and accuracy of
labor monitoring, certain machine learning models
have been identified as optimal solutions. The
algorithms employed in this study include Decision
Trees, Random Forest, and Logistic Regression.
These models fall under the category of supervised
machine learning algorithms, which are utilized to
make accurate predictions based on historical data.
The functioning of each algorithm is elaborated
below:
3.1.1 Supervised Machine Learning
Algorithms
Supervised learning is a branch of machine learning
where models are trained on labeled datasets,
meaning the input data is associated with known
output values. By leveraging these pre-labeled
examples, the model learns patterns and makes
predictions when new, unseen data is introduced.
3.1.2 Decision Tree Classifier
A decision tree is a rule-based model that facilitates
decision-making by structuring the data into a
hierarchical tree format. It consists of decision nodes
and leaf nodes, where decision nodes represent
different choices based on feature values, and leaf
nodes signify the final output. This algorithm
effectively categorizes data through a sequence of
binary decisions, ultimately arriving at a conclusion
based on conditions such as yes/no or true/false
responses.
3.1.3 Random Forest
Random Forest is an ensemble learning technique
that enhances the performance of individual decision
trees by generating multiple trees and aggregating
their predictions. Each tree is built using a subset of
the training data, and the final prediction is obtained
by averaging (for regression) or voting (for
classification) among all trees. This method improves
accuracy, reduces overfitting, and ensures robust
predictions, making it highly effective in labor
monitoring applications.
3.1.4 Logistic Regression
Logistic regression is a statistical model used for
classification tasks, where the output is a discrete
value (such as 0 or 1, yes or no, or true or false). It
applies a sigmoid function to transform input values
into probability scores, determining the likelihood of
an event occurring. When the probability surpasses a
certain threshold, the outcome is classified as 1
(positive class); otherwise, it is classified as 0
(negative class). This algorithm is particularly useful
for predicting binary outcomes in medical and
healthcare applications.
By integrating these algorithms, we can achieve
reliable and efficient labor monitoring solutions,
overcoming some of the challenges and limitations
identified in prior research.
Figure 2: DRLPARTO: A partogragh tracer architecture.
The figure 2 shows the workflow of the machine
learning-based classification system. The process
starts with collecting datasets containing FHR,
contractions, pulse, amniotic fluid, BP, temperature,
and cervix length. The data undergoes processing and
cleaning to remove inconsistencies. The cleaned data
is then split into training data and testing data. The
training data is used to train machine learning
algorithms, including Decision Tree Classifier,
Random Forest, and Logistic Regression. After
training, a classification model is generated, which is
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
556

then used to make predictions based on new input
data.
4 RESULTS AND DISCUSSION
Figure 3 indicates that the cervix length increases
sharply at the beginning and then stabilizes over time.
This suggests that initial changes occur rapidly, but
further progression is minimal or steady.
Figure 3: Cervix dilation.
Phase-wise analysis of a process, where each
phase is categorized as either “Normal” or requiring
“Consult” as shown in figure 4. While most phases
are marked as “Normal,” Phase 4 and Phase 7
indicate” Consult,” suggesting potential concerns in
those stages. However, the final result is marked as
“Normal,” implying that despite some irregularities,
the overall outcome is within acceptable limits.
Figure 4: Delivery prediction.
Figure 5: Comparison of the proposed model with
individual models.
The table 1 presents a comparative analysis of
different machine learning algorithms based on four
key performance metrics: accuracy, precision, recall,
and F1 score. It is also shown graphically in figure 5.
The Decision Tree model achieved 85% accuracy,
with balanced precision, recall, and F1 scores around
83-84%. Random Forest performed better, attaining
89% accuracy and an F1 score of 91%, indicating
improved overall performance. Logistic Regression
showed similar effectiveness with 88% accuracy and
slightly lower recall. The proposed method
outperformed all models, achieving 93% accuracy
and consistently high precision, recall, and F1 score
(92-93%), demonstrating its robustness and
effectiveness in the given task.
Table 1: State of art comparison.
algorithm accuracy precision recall f1
score
decision
tree
85 83 84 83
random
forest
89 90 87 91
logistic
regression
88 87 86 86
proposed
metho
d
93 92 92 93
5 CONCLUSION AND FUTURE
WORK
Predicting the type of delivery a few hours before
labor begins can help ensure a safe childbirth.
Whether a woman delivers vaginally or through a
cesarean section can impact both her health and the
baby’s well-being. Therefore, making the right
decision is crucial. This can be done using a par-
tograph, a tool that is widely recognized and
DRLPARTO: A Machine Learning Based Partograph for Fetal Monitoring System
557

recommended by the World Health Organization
(WHO), highlighting its importance in labor
management. From our review of various studies, we
found that machine learning and artificial intelligence
can be used to implement this prediction system.
Many researchers have explored different ways to
apply these technologies to improve labor
monitoring. In our approach, we focus on supervised
machine learning algorithms such as decision trees,
random forests, and logistic regression. Using these
methods can help predict delivery outcomes with high
accuracy, ultimately improving maternal and
newborn care. The partograph plays a crucial role in
monitoring health conditions during labor. Since its
introduction, it has undergone several modifications
to improve its effectiveness. Various factors help
assess the mother’s health and the environment
necessary for a safe delivery, and these have been
refined over time. As seen from the analysis of
different studies, the partograph is highly beneficial
for healthcare providers, mothers, and newborns.
While many researchers have explored its theoretical
aspects and case studies, only a few have discussed
using machine learning algorithms for predicting
delivery outcomes. Some studies have highlighted
important parameters for labor monitoring, but
practical implementation is still lacking.In the future,
further advancements can be made by integrating
machine learning techniques and improving
implementation strategies. Through continuous
research, experimentation, and technological
innovation, the medical field can enhance labor
monitoring and improve maternal and neonatal health
outcomes.
REFERENCES
Bedwell, Carol, Karen Levin, Celia Pett, and Dame Tina
Lavender.” A realist review of the partograph: when
and how does it work for labor monitoring” BMC
pregnancy and childbirth 17 (2017): 1-11.
ES, Ashour, Tahany El-Sayed El-Sayed Amr, Gehan
Ahmed Mohmed Elbahlowan, and Samah Mohamed
Elhomosy.” Effect of Implementing Intrapartum
Digital versus Paper Partographs on Maternity Nurses’
Performance and Birth Outcomes.” Egyptian Journal of
Health Care 14, no. 1 (2023): 430-445.
He, Xiaoqing, Xiaojing Zeng, James Troendle, Maria
Ahlberg, Ellen L. Tilden, Joa˜o Paulo Souza, Stine
Bernitz et al.” New insights on labor progression: a
systematic review.” American Journal of Obstetrics and
Gynecology (2023).
Hofmeyr, G. Justus, Stine Bernitz, Mercedes Bonet,
Maurice Bucagu, Blami Dao, Soo Downe, Hadiza
Galadanci et al.” WHO next-generation partograph:
revolutionary steps towards individualized labor care.”
Bjog 128, no. 10 (2021): 1658.
Khalil, Abu Bakr, Sayed A. Mostafa, and Ayman D.
Mohamed.” Revaluation of Paperless Partograph in the
Management of Labor.” Suez Canal University Medical
Journal 25, no. 1 (2022): 35- 41.
Lavender, tina, and stine bernitz.” use of the partograph-
current thinking.” best practice research clinical
obstetrics gynaecology 67 (2020): 33-43.
Melese, Kidest Getu, Bedilu Girma Weji, Tezera Moshago
Berheto, and Eyasu Tamru Berkus.” Utilization of
partograph during labour: A case of Wolaita Zone,
Southern Ethiopia.” Heliyon 6, no. 12 (2020).
Merih, Yeliz Dog˘an.” An Artificial Intelligence-Assisted
Innovative Product in Labor Follow-Up: The Electronic
Touch and Partograph Device.” Journal of Education
Research in Nursing/Hems¸irelikte Eg˘itim ve
Aras¸tırma Dergisi 20, no. 2 (2023).
Sharma, Shivani, Saroj Parwez, Kiran Batra, and Bharat
Pareek.” Enhancing safe motherhood: Effect of novel
partograph on labor outcomes and its utility: An Indian
perspective.” Journal of Family Medicine and Primary
Care 11, no. 11 (2022): 7226.
Singh, Ritu, Mukta Agarwal, Sudwita Sinha, Hemali H.
Sinha, Monika Anant,” Modified WHO Partograph in
Labour Room: A Quality Improvement Initiative to
Find Out Concerns, Challenges and Solutions.” Cureus
14, no. 10 (2022).
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
558
