
Deep Learning‑Based Generative Al for Segmenting Necrotic Lung
Lesions in CT Images Using Self‑Supervised Contrastive Learning
G. Indumathi, Sudharsan T. S., Ashok I. and Tharunkumar M.
Department of Computer Science and Engineering, SRM Institute of Science and Technology, Ramapuram, Chennai, Tamil
Nadu, India
Keywords: Convolutional Neural Networks (CNNs), Necrotic Lung Lesions, CT Images, Pulmonary Diseases,
Segmentation, Variational Autoencoders (VAEs), Self‑Supervised Learning, Contrastive Learning, Feature
Representation, Annotated Datasets, Generalization, Lesion Morphology, Medical Image Processing, Clinical
Applications.
Abstract: Segmenting necrotic lung lesions in CT images plays a vital role in diagnosing and managing pulmonary
diseases. However, traditional methods often struggle with the complex shapes and varying appearances of
lesions while relying heavily on manually annotated datasets. To overcome these limitations, we introduce an
innovative framework that combines Variational Autoencoders (VAEs) and self-supervised contrastive
learning for more accurate and efficient segmentation. The VAE helps the model learn compact and
meaningful representations of CT images, while contrastive pretraining enhances these features using
unlabeled data, improving generalization across different datasets. This approach not only reduces
dependency on manual annotations but also excels in capturing fine lesion boundaries and handling diverse
lesion appearances. By advancing medical image segmentation, our method provides a robust, scalable, and
efficient solution to key clinical challenges, ultimately aiding in early detection and treatment planning for
lung diseases.
1 INTRODUCTION
Medical imaging, particularly computed tomography
(CT), plays a crucial role in diagnosing and managing
lung diseases. Identifying necrotic lung lesions which
may be associated with infections, cancer, or
inflammatory condition is essential for effective
treatment. However, manually detecting and
segmenting these lesions is challenging, time-
consuming, and often subjective, varying from one
radiologist to another. This highlights the urgent need
for automated and reliable segmentation methods to
improve accuracy and efficiency in clinical settings.
With recent advancements in deep learning, medical
image analysis has seen remarkable improvements.
Generative models like Variational Autoencoders
(VAEs) can effectively capture meaningful patterns
in complex medical data while preserving critical
diagnostic details. When combined with self-
supervised contrastive learning, these models
become even more powerful by learning from
1odelling1 medical images.
In this study, we present an innovative approach
that integrates VAE-based generative 1odelling with
self-supervised contrastive learning to segment
necrotic lung lesions in CT scans. The VAE extracts
compact, informative features, while contrastive
learning refines them by distinguishing between
similar and different patterns. This synergy improves
segmentation accuracy and enables the model to
generalize across diverse lung lesion types. By
automating lesion detection, our method provides a
scalable and efficient solution that enhances clinical
decision-making, ultimately leading to better patient
outcomes.
2 LITERATURE SURVEY
Medical image segmentation plays a vital role in
diagnosing and managing pulmonary diseases,
especially when identifying necrotic lung lesions in
CT scans. These lesions often have irregular shapes
and varying appearances, making them difficult to
segment using traditional techniques like
thresholding or region-growing methods. As a result,
512
Indumathi, G., S., S. T., I., A. and M., T.
Deep Learning-Based Generative Al for Segmenting Necrotic Lung Lesions in CT Images Using Self-Supervised Contrastive Learning.
DOI: 10.5220/0013932200004919
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Research and Development in Information, Communication, and Computing Technologies (ICRDICCT‘25 2025) - Volume 5, pages
512-518
ISBN: 978-989-758-777-1
Proceedings Copyright © 2026 by SCITEPRESS – Science and Technology Publications, Lda.

deep learning-based generative models have emerged
as more accurate and robust solutions for this task.
Deep learning architectures like Convolutional
Neural Networks (CNNs) and U-Net have shown
remarkable success in medical image segmentation.
However, these methods often require large
annotated datasets, which can be a major limitation
due to the time and expertise needed for manual
labeling. To overcome this, Variational
Autoencoders (VAEs) first introduced by Kingma
and Welling (2013) offer an effective alternative by
learning compact, meaningful representations of
high-dimensional data. This capability makes them
valuable for both segmentation and data
augmentation in medical imaging.
To further reduce reliance on labeled datasets,
Self-Supervised Learning (SSL) enables models to
learn from unlabeled data through pretext tasks like
image reconstruction. Contrastive learning, a subset
of SSL, enhances feature extraction by ensuring that
similar images (positive pairs) are grouped together
while distinct images (negative pairs) are kept apart.
Popular contrastive learning methods like SimCLR
(Chen et al., 2020) and MoCo (He et al., 2020) have
significantly improved the generalization and
robustness of deep learning models in medical image
analysis.
By combining VAEs with self-supervised
contrastive learning, we can develop a powerful and
efficient solution for necrotic lung lesion
segmentation. This approach reduces the need for
manual annotation, enhances segmentation accuracy,
and allows the model to adapt to diverse imaging
conditions. Moving forward, refining contrastive loss
functions and exploring hybrid deep learning models
could further improve segmentation performance,
making AI-driven medical imaging even more
reliable and effective for clinical applications.
3 PROBLEM STATEMENT
Segmenting necrotic lung lesions in CT scans is a
complex task due to their irregular shapes, low
contrast, and limited availability of annotated data.
Traditional deep learning models rely heavily on
manual labeling, which is time-consuming and labor-
intensive. To overcome these challenges, this
research introduces a generative AI framework that
combines Variational Autoencoders (VAEs) with
self-supervised contrastive learning. This approach
enhances segmentation accuracy, reduces the need for
manual annotations, and improves the model’s ability
to generalize across diverse datasets. By leveraging
unlabeled data and learning meaningful patterns, this
method offers a more efficient and scalable solution
for medical image analysis.
3.1 Thresholding Method
Thresholding is a basic technique for image
segmentation. It chooses a threshold value and
separates pixels into two classes: those that are above
the threshold and those that are below. This technique
can be applied to separate the objects of interest, such
as potential lung lesion regions, from the background
in an image.
How it applies to lung lesions identification
This method combines VAEs, contrastive learning,
and U-Net to enhance necrotic lung lesion
segmentation in CT images, achieving high accuracy
while minimizing the need for manual annotations.
Limitations
The system relies on high-quality CT scans, requires
extensive computational resources, may struggle
with extreme lesion variations, and needs clinical
validation.
3.2 K-Means Clustering
K-means clustering is an unsupervised
machinelearning algorithm. It attempts to partition 'n'
observations into 'k' clusters in which each
observation belongs to the cluster-1 with the nearest
mean, serving as a prototype of the cluster-2.
Manual Analysis:
This is the conventional method in which a trained
expert (such as a pulmonologist) visually studies the
medical images (MRI, CT scans) and manually marks
the region of the tumor.
3.2.1 Disadvantages
1. High Computational Cost: Training VAEs and
contrastive learning models demands high GPU
resources, making real-time clinical deployment
costly and technically challenging for
widespread medical use.
2. Limited Generalization: The model's
reliability may be affected by unseen data due to
variations in lesion shape, CT scan quality, and
diverse patient demographics.
3. Interpretability Issues: Generative AI models
operate like black boxes, making it hard for
clinicians to interpret predictions, which limits
trust in medical applications.
4. Clinical Validation Requirement: Extensive
Deep Learning-Based Generative Al for Segmenting Necrotic Lung Lesions in CT Images Using Self-Supervised Contrastive Learning
513
real-world validation is essential to confirm
accuracy, robustness, and compliance with
medical standards before this approach can be
widely adopted.
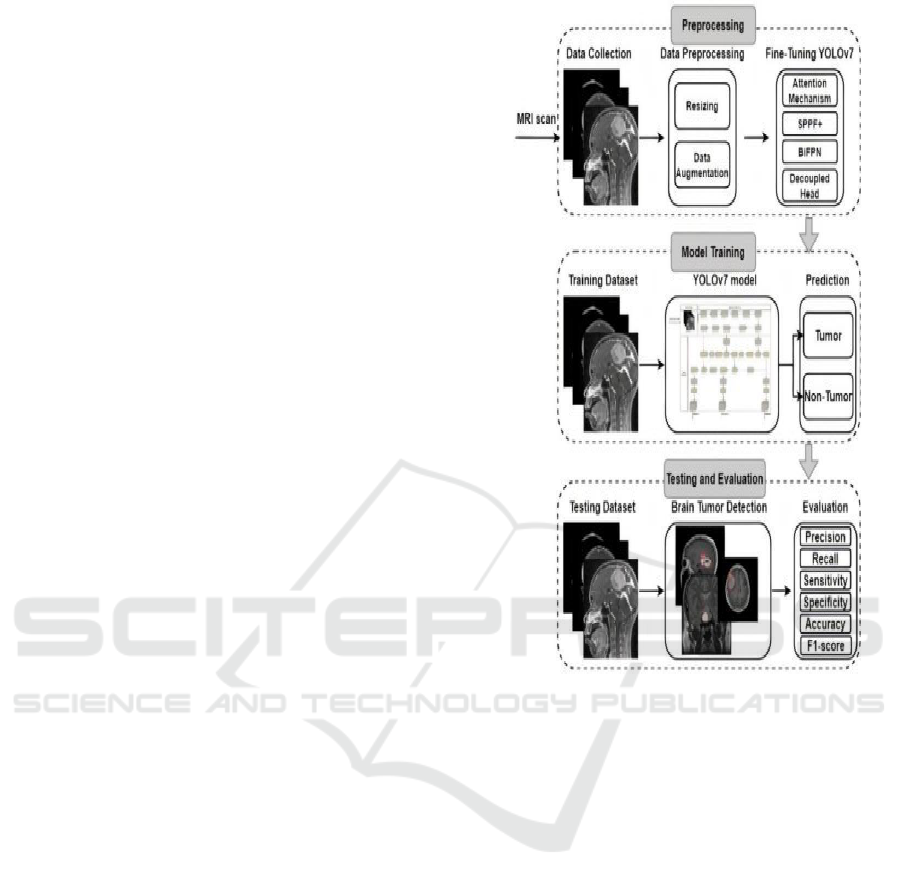
4 PROPOSED SYSTEM
Our system combines Variational Autoencoders
(VAEs) and Self-Supervised Contrastive Learning to
segment necrotic lung lesions in CT images. The
figure1 shows the Block diagram of the proposed
system VAEs extract meaningful latent features,
while contrastive learning refines these features
using unlabeled data. This method enhances
segmentation accuracy, minimizes reliance on
manual annotations, and improves generalization
across different datasets, making it a more efficient
and scalable solution for medical imaging.
4.1 Variational Autoencoders (VAEs)
1. Learning Data Distribution: VAEs are
generative models. They are not simply learning
how to classify images; they learn the
underlying probability distribution of data.
Think of learning the "essence" of what makes a
brain image be a brain image and what
variations are possible.
2. Image Enhancement: This learned knowledge
can be used to manipulate and improve images.
3. Noise Removal: VAEs can reconstruct images
to remove noise and artifacts, which could blur
important information, making images clearer
for further processing.
4. Detailed Representation: VAEs can also
produce a more detailed or improved
representation of images. It can be enhanced
through the feature representation by drawing
out subtle features and filling in gaps, which is
easier to see abnormalities.
5. Improved Classification Accuracy: Through
the enhancement of the quality and clarity of the
input images, VAEs indirectly help to improve
the performance of downstream tasks such as
diseaseclassification. The clearer the images
are, the easier it is for a model trying to detect a
tumor.
Figure 1: Block Diagram of the Proposed System.
4.2 Convolutional Neural Networks
(CNNs)
1. Image Classification: Image classification is
arguably the application field where CNNs are
most effectively used. Spatial hierarchies of
features for images are where they excel
particularly well. Therefore, in case of brain
tumors, they learned to classify one category of
the brain tissue different from another.
2. Labeled Dataset: This is a kind of supervised
learning model of CNNs, so it requires data to
be labeled. The paragraph refers to the dataset
of the labeled brain MRI or CT images, for
instance, benign tumor, malignant tumor, and
normal tissue.
3. Feature Extraction:The CNN learns to
automatically extract the features relevant
from images. Features are not pre-defined by
humans, but instead are learned by the
network. In the case of brain tumor detection,
the shape, size, texture, and other features about
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
514

the tumor would be examples.
4. Automation and Efficiency: The most
important advantage of CNNs is that they
automate the process of feature extraction and
classification. This makes the detection of brain
tumors faster, more objective, and potentially
more accurate than manual analysis.
5. Early Diagnosis and Better Outcomes: By
enabling rapid and precise identification of brain
tumors, CNNs contribute to earlier diagnosis,
which is crucial for improving treatment
outcomes and patient survival.
4.3 Advantages
1. Reduced Annotation Dependency: By
learning from unlabeled CT images, self-
supervised contrastive learning reduces the
reliance on large annotated datasets, making
model training more efficient.
2. Improved Segmentation Accuracy:
Combining Variational Autoencoders (VAEs)
with contrastive learning improves feature
extraction, resulting in more accurate detection
of lesion boundaries in CT images.
3. Better Generalization: The model effectively
adapts to diverse datasets, ensuring greater
robustness across various imaging conditions
and patient populations for more reliable
segmentation..
4. Enhanced Feature Representation: VAEs
extract meaningful latent features, effectively
capturing variations in lesion appearance and
structure for more accurate and reliable
segmentation.
5. Efficient Handling of Complex
Morphologies: The framework accurately
segments lesions with irregular shapes, low
contrast, and diverse textures, offering superior
performance compared to traditional methods.
6. Scalability: After training, the system can
process large datasets without extra
annotations, making it highly efficient and
practical for clinical applications.
7. Reduced Human Effort and Time:
Automating lesion segmentation accelerates
diagnosis and treatment planning, reducing
radiologists' workload and improving efficiency
in medical imaging analysis.
8. Robust Against Label Noise: Self-supervised
learning reduces errors caused by inconsistent
manual annotations, enhancing model
reliability and ensuring more accurate and
consistent lesion segmentation.
9. Potential for Transfer Learning: The learned
representations are highly adaptable, allowing
fine-tuning for other medical imaging tasks,
improving versatility and expanding clinical
applications.
10. Supports Early Disease Detection: Enhanced
segmentation enables early detection of necrotic
lung conditions, facilitating timely
interventions and improving patient outcomes
through more accurate diagnoses and treatment
planning.
5 MODULE DESCRIPTION
5.1 Convolutional Neural Networks
(CNNs)
Focus on CNNs as the primary architecture, with its
ability to excel in image analysis and feature
extraction.
Specific CNN Architectures: Discuss specific
architectures of CNNs used, such as ResNet,
VGG, Inception, and the reason for using them.
1. Hybrid Models: If applicable, discuss
hybrid models that combine CNNs with
other deep learning architectures, such as
Recurrent Neural Networks or Transformers.
5.2 Variational Autoencoder (VAE)
1. VAE for Data Augmentation: The VAE
learns the underlying distribution of healthy
brain images. It can then generate synthetic,
but realistic, healthy images to augment the
training data, thereby improving the
robustness of the model and reducing
overfitting, especially in cases where the data
is scarce.
2. VAE for Feature Extraction: The VAE's
latent space (the compressed representation)
can be used to extract features from the MRI
images. These features, combined with the
CNN's features, can improve the accuracy of
tumor classification.
3. VAE for Anomaly Detection: Train the
VAE on the healthy brain images to learn
their normal representation. Tumor
containing images will probably have a high
reconstruction error while passing through
the VAE since they are anomalous and can
be used for potential tumor detection.
Deep Learning-Based Generative Al for Segmenting Necrotic Lung Lesions in CT Images Using Self-Supervised Contrastive Learning
515

4. Hybrid Model: It should be explicitly stated
if the model is a hybrid, which case it
combines CNNs ,VAEs in some way,
followed by the interaction between the two
components.
5.3 Data Preprocessing and
Augmentation
1. Standard Preprocessing: Outline the
standard preprocessing steps for images
(noise reduction, contrast enhancement,
etc.).
2. VAE-Based Augmentation: Explain how
the VAE is used to generate synthetic data.
Mention specific techniques used to ensure
the generated images are realistic and
diverse.
5.4 Training and Evaluation
1. Training the VAE: Describe the training
process for the VAE, including the loss
function (typically a combination of
reconstruction loss and KL divergence) and
optimization techniques.
2. Training the CNN (with or without VAE
features): Describe how one trains the
CNN, potentially making use of VAE-
extracted features.
3. Evaluation Metrics: State standard
evaluation metrics (accuracy, sensitivity,
specificity, F1-score, AUC). If VAE is used
for anomaly detection, discuss the relevant
metrics.
5.5 Potential Applications
Figure 2: : Sample Lung Cancer Image.
Clinical Diagnosis and CAD: Discuss applications in
the clinical field, computer-aided diagnosis
5.6 Limitations
1. VAE Training Complexity: Recognize the
challenge in training VAEs effectively.
2. Interpretability: Explain the difficulties in
interpreting the latent space of the VAE and its
contribution to tumor detection.the figure 2
shows the sample lung cancer image .
6 IMPLEMENTATION
Segmenting necrotic lung lesions in CT images is
challenging, but deep learning-based generative AI
enhances both accuracy and efficiency. Our method
follows a structured pipeline, integrating data
preprocessing, model training, self-supervised
contrastive learning, and final segmentation to
achieve highly precise and reliable results.
6.1 Preparing the Data
Before training an AI model, obtaining high-quality
CT scan datasets is essential. We use publicly
available datasets like LIDC-IDRI or hospital-
acquired medical images. Raw CT scans often
contain noise and irrelevant details that can affect
model accuracy, so we apply preprocessing
techniques to improve data quality. Standardization
normalizes pixel intensities for consistency, while
lung isolation removes unnecessary regions using
thresholding and morphological operations. To
enhance adaptability, data augmentation introduces
variations like rotation, flipping, and contrast
adjustments. Since 3D CT scans are computationally
heavy, patch extraction breaks them into smaller 2D
sections, preserving lesion details. These steps
optimize segmentation accuracy and model
performance.
6.2 Learning Features with Variational
Autoencoders
Since medical image datasets are often limited,
Variational Autoencoders (VAEs) help the model
recognize meaningful patterns and generate realistic
representations of CT images. VAEs consist of three
key parts. First, the encoder compresses CT scans
into a compact feature space, capturing important
anatomical details. Instead of simply memorizing
images, latent space sampling allows the model to
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
516

learn underlying patterns, making it more adaptable
to new data. Finally, the decoder reconstructs images
from this compressed information while preserving
critical lesion details. To ensure accuracy, we use
Reconstruction Loss to keep generated images close
to the originals and KL Divergence Loss to prevent
overfitting and maintain a well-structured feature
space.
6.3 Enhancing Feature Learning with
Self-Supervised Contrastive
Learning
Since labeling medical images is time-consuming
and requires expert annotation, contrastive learning
helps the model differentiate between similar and
different lung lesions without relying on manual
labels. The process begins by creating positive pairs
(two slightly modified versions of the same CT scan)
and negative pairs (images from different patients).
These pairs are then processed through a Siamese
Network or SimCLR framework, which teaches the
model to pull similar images closer in the feature
space while pushing dissimilar ones apart. To refine
this learning, we use Contrastive Loss (NT-Xent
Loss), which strengthens feature representations.
This approach enhances the model’s ability to
accurately identify lung lesions, even in cases where
labeled data is scarce, improving segmentation
performance and generalization.
6.4 Performing Segmentation with U-
Net
For the final segmentation step, we integrate the
learned features into a U-Net model, a widely used
deep learning architecture for medical image
segmentation. The encoder (backbone) is initialized
with contrastive learning-pretrained weights,
allowing it to extract meaningful high-level features
from CT scans. The decoder then reconstructs a
pixel-wise segmentation mask, accurately outlining
necrotic lung lesions. To preserve fine details, skip
connections are used, ensuring that important spatial
information from the encoder is retained throughout
the network. To optimize segmentation accuracy, we
employ a combination of Dice Loss, which measures
overlap accuracy between the predicted mask and
actual lesion, and Binary Cross-Entropy (BCE) Loss,
which ensures accurate classification of lesion and
non-lesion regions, improving overall model
performance.
6.5 Evaluating Performance and
Testing on New Data
To ensure our model performs well across various
datasets, we evaluate it using key performance
metrics. The Dice Similarity Coefficient (DSC)
measures how accurately the predicted lesion mask
overlaps with the actual ground truth, ensuring
precise segmentation. Intersection over Union (IoU)
further assesses segmentation accuracy by comparing
the predicted and actual lesion areas. Additionally,
we analyze precision, recall, and F1-score to detect
false positives and false negatives, ensuring reliable
performance. To confirm the model’s robustness, we
test it on unseen external datasets, verifying its ability
to generalize across different imaging conditions,
scanner types, and patient variations for real-world
applicability.
7 CONCLUSIONS
The proposed deep learning-based generative AI
approach provides an effective solution for
segmenting necrotic lung lesions in CT images by
integrating Variational Autoencoders (VAEs), self-
supervised contrastive learning, and U-Net
segmentation. VAEs help extract meaningful features
from medical images, enabling the model to learn rich
representations of lung structures. Contrastive
learning, on the other hand, strengthens the model’s
ability to differentiate between healthy and diseased
lung tissue without relying on extensive manually
labeled data. This significantly enhances the model’s
generalization capability, making it more adaptable to
real-world clinical applications.
By incorporating U-Net, which is well-suited for
medical image segmentation, the framework ensures
highly accurate, pixel-level detection of necrotic lung
lesions. The encoder, pretrained with contrastive
learning, extracts high-level features, while the
decoder reconstructs precise segmentation masks. To
validate performance, we use key evaluation metrics
such as Dice Similarity Coefficient (DSC),
Intersection over Union (IoU), precision, and recall,
which confirm the model’s reliability.
By reducing dependence on large annotated
datasets, this scalable, automated, and highly accurate
approach offers an advanced tool for early diagnosis
and treatment planning, ultimately improving
healthcare outcomes for lung disease patients.
Deep Learning-Based Generative Al for Segmenting Necrotic Lung Lesions in CT Images Using Self-Supervised Contrastive Learning
517

REFERENCES
C. Peng, X. Zhang, G. Yu, G. Luo, and J. Sun, ‘‘Large
kernel matters Improve semantic segmentation by
global convolutional network,’’ inProc. IEEE Conf.
Comput. Vis. Pattern Recognit. (CVPR), Jul. 2017,pp.
4353–4361.
G. Litjens, T. Kooi, B. E. Bejnordi, A. A. A. Setio, F.
Ciompi,M. Ghafoorian, J. A. Van Der Laak, B. Van
Ginneken, and I. C. Sanchez,‘‘A survey on deep
learning in medical image analysis,’’ Med. Image
Anal.,vol. 42, pp. 60–88, Dec. 2017.
G. Pezzano, V. R. Ripoll, and P. Radeva, ‘‘CoLe-CNN:
Context-learningconvolutional neural network with
adaptive loss function for lungnodulesegmentation,’’
Comput. Methods Programs Biomed., vol. 198, Jan.
2021,Art. no. 105792.
H. Cao, H. Liu, E. Song, C.-C. Hung, G. Ma, X. Xu, R. Jin,
and J. Lu,‘‘Dual-branch residual network for lung
nodule segmentation,’’ Appl. SoftComput., vol. 86,
Jan. 2020, Art. no. 105934.
O. Ronneberger, P. Fischer, and T. Brox, ‘‘UNet:
Convolutional networksfor biomedical image
segmentation,’’ in Proc. Int. Conf. Med. ImageComput.
Comput.-Assist. Intervent. Cham, Switzerland:
Springer, 2015,pp. 234–241.
S. B. Knight, P. A. Crosbie, H. Balata, J. Chudziak, T.
Hussell, and C. Dive,‘‘Progress and prospects of early
detection in lung cancer,’’ Open Biol.,vol. 7, no. 9, Sep.
2017, Art. no. 170070.
S. Wang, M. Zhou, Z. Liu, Z. Liu, D. Gu, Y. Zang, D. Dong,
O. Gevaert,and J. Tian, ‘‘Central focused convolutional
neural networks: Developinga data-driven model for
lung nodule segmentation,’’ Med. Image Anal.,vol. 40,
pp. 172–183, Aug. 2017.
S. Luo, J. Zhang, N. Xiao, Y. Qiang, K. Li, J. Zhao, L.
Meng, and P. Song,‘‘DAS-Net: A lung nodule
segmentation method based on adaptivedualbranchatte
ntion and shadow mapping,’’ Appl. Intell., vol. 52, no.
13,pp. 15617–15631, 2022.
V. Badrinarayanan, A. Handa, and R. Cipolla, ‘‘SegNet: A
deep convolutionalencoder–decoder architecture for
robust semantic pixel-wiselabelling,’’ 2015,
arXiv:1505.07293.
X. Dong, S. Xu, Y. Liu, A.Wang, M. I. Saripan, L. Li, X.
Zhang, and L. Lu,‘‘Multi-view secondary input
collaborative deep learning for lung nodule3D
segmentation,’’ Cancer Imag., vol. 20, no. 1, pp. 1–13,
Dec. 2020.
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
518
