
Predictive Analytics for Multiple Diseases Using Machine Learning
Vijayalakshmi M., Shiva Subramanian and Harsh Jain
Department of Computing Technologies, SRM Institute of Science and Technology, Kattankulathur, India
Keywords: Chronic Diseases, Medicare, Health Care Management Data Analytics, Machine Learning, Supervised
Learning, Disease Prediction, Support Vector Machine (SVM), Logistic Regression, Early Detection, Patient
Outcomes, Predictive Analytics.
Abstract: The prevalence of chronic diseases is increasing among Medicare patients, and there is a need for innovative
ways of healthcare management. Medical practitioners are commonly swamped by the large quantities of
information involved in the analysis so that it becomes an uphill task to interpret symptoms and diseases
within time. Utilization of supervised ML algorithm has proved its effectiveness for diagnosis purposes to
diseases and enables medical professionals to detect risky conditions in an early stage. The goal of the project
is to predict the likelihood of a variety of diseases in the Medicare population using data analytics and machine
learning. We will identify patterns and risk factors associated with multiple diseases through preprocessing
and enhancement of available data. More advanced ML algorithms will be leveraged to create prediction
models: SVM for the prediction of both diabetes and Parkinson's disease and logistic regression for heart
disease. Feeding labeled input data into the algorithms during the training process will help learn correlations
between feature and disease correlations. When predicting, the models will then be tested on an independent
data set to establish how accurately they are able to predict outputs and call out potential issues for fine-tuning
if needed. Such insights help healthcare providers identify a patient issue earlier and intervene appropriately.
This, of course, improves patient outcomes while controlling health costs. This project depicts the promise of
predictive analytics with respect to improving patient care under Medicare through creating personalized and
proactive healthcare solutions.
1 INTRODUCTION
The prevalence of chronic disease in Medicare
patients has been on the rise and it has become a
challenge for healthcare management, thus calling for
new ways of facilitating improved detection and
management of such diseases. Health care
professionals deal with large amounts of information
related to patients. In that context, proper diagnosis
of symptoms and detection of diseases at an early
stage has become difficult. Traditional procedures fail
to meet the volume and complexity of this
information, so advanced techniques have to be
employed to make health care delivery effective. In
such a context, supervised machine learning
algorithms are becoming promising solutions in
improving disease diagnosis and early detection. The
algorithms rely heavily on datasets in recognizing
patterns and at-risk factors of various diseases,
thereby supporting medical practitioners to make
informed choices. This project is designed in a way to
utilize the strength of data analytics and machine
learning for predicting the onset of chronic diseases
in the Medicare population. The existing state-of-the-
art ML models for disease prediction have the issues
of poor data quality, limited generalizability,
overfitting, and strong feature selection that may lead
to nonreliable predictions, so this project is focused
on promoting better preprocessing of data,
application of multiple ML algorithms, and using
validation with the use of various datasets to improve
accuracy and generalizability together with better
interpretability. SVM algorithms will be used to
predict diabetes and Parkinson's disease, while
logistic regression will be used in predicting heart
disease. Once these models are put through training
with labeled patient data, the algorithms will have
learned to recognize patterns between features and
their corresponding disease. These models will then
be tested using another independent set of data and,
therefore, their accuracy will be checked for further
verification about potential problems. This manner,
the results that are going to come out would be
92
M., V., Subramanian, S. and Jain, H.
Predictive Analytics for Multiple Diseases Using Machine Learning.
DOI: 10.5220/0013923300004919
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Research and Development in Information, Communication, and Computing Technologies (ICRDICCT‘25 2025) - Volume 5, pages
92-99
ISBN: 978-989-758-777-1
Proceedings Copyright © 2026 by SCITEPRESS – Science and Technology Publications, Lda.

reliable enough to make necessary adjustments. The
results expected from this project are going to guide
the providers of healthcare into earlier identification
and intervention for chronic diseases with the aim of
rising patient outcomes and lowering health care costs
in facilities. This paper focuses on the integration of
predictive analytics in Medicare patient care. Thus, it
helps in giving personalized and proactive healthcare
solutions, transforming the management of chronic
diseases.
State-of-the-art machine learning-based disease
prediction systems face substantial challenges like
dependency on the quality of the dataset, challenges
in feature selection, and origination of bias through
the use of a single algorithm. These issues might lead
to false predictions and the defeat of precocity of
diseases. To counter these issues, this project aims at
designing a multi-algorithm machine learning system
that utilizes a variety of supervised learning models
in order to have an increased level of accuracy
pertaining to predictiveness and to take away the bias.
Data preprocessing along with advanced techniques
of feature selection is also crucial in order to improve
quality to a large extent. These need to be expanded
to include different demographics to make the models
more generalizable and less likely to overfit.
Evaluation of the learning models after training will
also increase the reliability of predictions. Lastly, it
will evaluate and compare the performance of
different machine learning models applied in
handling various diseases, including heart disease,
diabetes, and Parkinson's disease. By addressing
these objectives, the project aims to offer a strong
framework for more accurate and reliable disease
prediction.
2 LITERATURE SURVEY
The inclusion of machine learning (ML) in healthcare
for disease prediction has highlighted significant
challenges and limitations in current systems. A
major issue is the dependency on data quality. Poor
data, characterized by missing entries,
inconsistencies, and class imbalances, often results in
unreliable predictions. Kourentzes et al. and Lipton et
al. demonstrated how inadequate data quality
adversely impacts model accuracy, especially in
predicting cardiovascular disease mortality risks.
Beam and Kohane also emphasize that data
preprocessing is critical for healthcare applications to
address these issues effectively.
Another key challenge is effective feature
selection. Guyon and Elisseeff identified that
inefficient methods tend to overfit, capturing noise
rather than meaningful patterns. Prominent
techniques like Recursive Feature Elimination and
LASSO (Zou and Hastie) have proven useful but
often lack consistency across varied datasets. Miotto
et al. highlighted the need for dimensionality
reduction techniques to avoid overfitting while
preserving model effectiveness.
Algorithmic bias is another significant concern.
Obermeyer et al. observed that models trained on
homogeneous datasets struggle to generalize, thereby
exacerbating health disparities among demographic
groups. To address this, multi-algorithm systems
leveraging strengths from multiple supervised
learning models have emerged as a promising
solution. For instance, Hodge and Austin
demonstrated how ensemble methods could enhance
accuracy and reduce bias, particularly in predicting
diabetes and heart disease (Chakraborty et al.,).
Esteva et al. explored how deep learning models
could reduce bias by integrating diverse datasets.
Advanced preprocessing and feature engineering
techniques also play a critical role in improving
model performance. Sun et al. conducted systematic
reviews highlighting the importance of preprocessing
in enhancing generalization and minimizing
overfitting. Topol emphasized the importance of
high-quality preprocessing for AI-driven healthcare
solutions. Furthermore, Wang and Preininger stressed
the need for diverse datasets to ensure robust and
unbiased model training.
Model evaluation is equally crucial. Good post-
training evaluation techniques, such as cross-
validation, ensure performance optimization and
reliability (Varma & Simon). Liu et al. demonstrated
that systematic evaluations could match or
outperform human-level diagnostic accuracy in
certain medical domains.
Recent advances in machine learning have shown
immense potential for addressing these challenges.
Liang et al. applied AI to pediatric disease
diagnostics, achieving high accuracy and
interpretability. Shickel et al. highlighted the growing
role of deep learning in analyzing electronic health
records (EHRs), enabling better predictions for
chronic diseases. Rajkomar et al. explored how ML
could revolutionize patient care by integrating
precision medicine and scalable analytics.
Additionally, Esteva et al. and Litjens et al.
demonstrated how deep learning models, such as
convolutional neural networks, could achieve
dermatologist-level performance in detecting skin
conditions and medical imaging, respectively.
Advances in these areas pave the way for
Predictive Analytics for Multiple Diseases Using Machine Learning
93

implementing predictive analytics across diverse
healthcare domains.
Taken together, these insights underscore the need
for creative solutions to improve ML-based disease
prediction systems. They also highlight the
importance of data diversity, advanced
preprocessing, multi-algorithm approaches, and
rigorous model evaluation to ensure reliable and
generalizable predictions.
3 WORKING PRINCIPLE
The multi-algorithm approach shall use several
supervised machine learning models in order to
enhance the accuracy of disease prediction with
balancing the type of bias existing with single-
algorithm-based approaches. Advanced
preprocessing techniques come into effect initially for
cleansing and preparing the dataset while maintaining
the quality by determining such issues as missing
values and inconsistencies. Then feature selection
processes are integrated to identify and rank features
important to the predictive performance of the
models.
During training, cleaned and preprocessed data
are fed into sets of ML algorithms, which include
SVM for diabetes and Parkinson's disease prediction
models and logistic regression for the heart disease
prediction model. The models are trained with labeled
data such that it learns the pattern and correlation
between features of the patients and the outcome of
their diseases. Lastly, the trained models were
validated on separate sets of data that did not take part
during the training process. This validation would
help in establishing the correctness of the models
besides generalizing over other patient populations.
After validation, the models are integrated in user-
friendly interfaces based on Streamlit that enable
users to input a disease they want to check. The
application captures the input from the user performs
the needed validations and then processes it through
the appropriately trained model. As a result, the
returned prediction results along with their respective
confidence levels are returned to the user for enabling
decision making pertinent to the health area. This is a
structured approach that will target the provision of a
strong and reliable predictive analytics tool for
disease detection in early stage development to
improve patient outcome results while enhancing
healthcare delivery efficiencies
4 METHODOLOGY
4.1 System Design
In the system design, the choice of Streamlet
framework as a means of building the user interface
is what makes up the major elements of the software,
coupled with pre-trained models of machine learning
like Support Vector Machines and logistic regression,
as well as libraries for data manipulation and model
evaluation. Separation of frontend UI from backend
processing is clearly defined to allow one to take
advantage of modularity and maintainability.
4.2 Data Collection and Preprocessing
The data collection and preprocessing phase is filled
with a large dataset of Medicare patients gathered
together with rich demographic, clinical, and
historical health data. Techniques of preprocessing
are applied to ensure data quality that include the
cleaning process, handling missing values,
normalizing numerical features, and encoding
categorical variables.
4.3 Feature Selection
Feature selection primarily deals with the
identification of features that best predict the disease.
Some of the methods that can be applied in this
direction include correlation analysis, recursive
feature elimination, and others. Along with this, some
method of dimensionality reduction is also performed
so that the risk of overfitting is avoided but as much
effectiveness of the model as possible is preserved.
4.4 Building the Model
The approach used for the development of the model
is multi-algorithm. Support Vector Machines are used
for predicting diabetes and Parkinson's disease,
whereas logistic regression has been taken into
consideration for predicting heart diseases. These
models will learn the underlying patterns and
correlations between different features and diseases
by being trained with labeled input data.
4.5 Model Validation
All this is done by doing model validation against a
separate dataset while testing the trained models.
Metrics like accuracy, precision, recall, and F1-score
are measured in an effort to find out the level of
performance that the models have achieved. If the
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
94

initial performance fails to meet the required
thresholds, then the action of hyperparameter tuning
takes place for increasing the robustness of the model.
4.6 UI Development
The user interface will be designed as a friendly and
intuitive interface using Streamlet to permit doctors
to select disease types for inputting patient-specific
information. In real time, validation of the user input
is used in order to have reliable data, and, in case an
error is observed, the error messages will pop up in
real-time.
4.7 Integration and Testing with the
Model
Model integration integrates the trained machine
learning models into the Streamlet application to
make real-time predictions based on the inputs that a
user may give. Functional testing of the application
will be done afterward to confirm if indeed it gives a
correct prediction and an interface that is friendly to
use.
4.8 Deployment and Feedback
This will be the last stage, where the application goes
into live service, observed in practice with its
performance, and continuously accommodates
improvement by making sure that feedback from
users is taken. This would identify areas for
improvement, thus ensuring the predictive analytics
system would remain effective and relevant to clinical
practice.
5 IMPLEMENTATION PROCESS
5.1 Frontend Development Using
Streamlit
The development of the predictive analytics
application begins by setting up Streamlit in creating
a very intuitive user interface. The front-end model is
developed to enable the user to select which disease
to check, such as Diabetes, Heart Disease, or
Parkinson's. As per this disease selected, design a user
input form to collect necessary data such as age,
medical history, and any other information that may
be vital for prediction.
5.2 Input Validation
The application uses input validation to ensure that
the entries made by users will fall within legitimate
ranges and formats, like numeric ranges, such as age,
glucose levels, among others. The system also
employs error handling as it gives prompt feedback,
in case of entry errors or incompleteness, and directs
the user to correct the entries before processing.
5.3 Selecting Models According to User
Choices
Conditional logic will be used to determine which of
the disease models should be utilized based on a
choice selected by the user. Supervised learning
techniques are available within the application in
order to train models based on real-life samples of
data. Once chosen, the appropriate trained machine
learning model is loaded to conduct inference.
5.4 Model Inference
In the model inference, the application now
configures itself to format the inputted data from the
user into a form that fits the selected machine learning
model. The model proceeds to run its predictions
based on the formatted data. The outcome is then
interpreted to include probabilities or binary
classifications to show whether the user is likely to be
afflicted with the disease selected.
5.5 Display Results to User
The results of the model are actually shown to the
users through Streamlit's display feature. When the
model gives a high probability of having a disease,
the message will read as follows: "The prediction
shows that you have a high chance of having diabetes
from what you typed. End" Otherwise, in case the
prediction would indicate a low probability, the
message is also compliant with this by saying, "The
prediction indicates a low percent chance of having
diabetes based on your input." The application can
also return confidence levels or probabilities to help
make users better understand the accuracy of the
prediction.
5.6 Backend Integration, Testing, and
Validation
Backend integration needs to ensure that the trained
machine learning models are actually well-integrated
with the Streamlit interface; this can typically be done
Predictive Analytics for Multiple Diseases Using Machine Learning
95

by loading the models from saved files. Functional
testing is a rather complex process to ensure that the
application will execute the right work flow of user
inputs and selections to produce the correct
predictions. Model validation ensures that the
machine learning models behave consistently with
their off-line evaluations.
5.7 Code Breakdown
This code starts with import and setup, as is always
necessary in a Python program. This includes `os` for
interaction with the operating system and `pickle` to
load saved machine learning models. The backbone
of this web interface is created with `streamlit`. To
add the sidebar menu, the `streamlit_option_menu`
will be used.
The Streamlit app is setup as follows:
st.set_page_config(title='', layout='wide',
page_icon='') Here, title, layout, and icon of the app
are defined in order to create uniform visual
presentation. Working directory is identified using
os.path.dirname (os.path.abspath (__file__)) which
helps find saved model files. Pretrained models for
Diabetes, Heart Disease, and Parkinson's Disease are
loaded using pickle.load: preparing them for
inference. A sidebar created with the use of st.sidebar
enhances UX by offering clearer navigation to, for
example, Diabetes Prediction and Heart Disease
Prediction.
Figure 1 shows the Sample code for code
breakdown.
Figure 1: Sample code 1.
5.8 Model Loading
The working directory is set to determine the location
of the script. The `pickle` module is used to load pre-
trained models for Diabetes, Heart Disease, and
Parkinson's Disease from disk. Figure 2 shows
Sample code for model loading.
Figure 2: Sample code 2.
5.9 Sidebar Navigation
The application has a sidebar through which the user
can navigate to select the desired page for predicting
different diseases. Every page is designed differently
to take the required user input for the disease selected
and then process it accordingly.
Figure 3: Sample code 3.
In summary, all parts of the application-from frontend
development to data validation; models will infer the
result and then display it to users-so provides a fully
integrated experience of disease likelihood prediction
for users on the basis of their inputs. The figure 3
shows Sample code for sidebar navigation.
6 ADVANTAGES AND
DISADVANTAGES
6.1 Advantages
The key advantages of the proposed machine learning
approach in predictive analytics on multiple diseases
include improved early detection of disease. This
enables the health provider to identify high-risk
patients, followed by timely intervention and
ultimately better patient outcomes. Advanced
algorithms can be used, including large datasets. The
system can effectively analyze large datasets and
identify complex patterns that might not come into
view using traditional methods. Hence, this leads to
better and more accurate diagnoses as well as
personalized health care solutions for individualized
patients. The multi-algorithm also reduces biases
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
96
inherent in single-model evaluations, and it offers
greater generalizability and robustness in predictions
across different populations and healthcare settings.
6.2 Disadvantages
Although it has many advantages, the implementation
of predictive analytics in the health sector presents
several challenges. The first major challenge relates
to the quality of data required for effective predictive
analytics; low-quality data always affects prediction
accuracy, which has serious implications on patient
safety. Third, a problem will be the model complexity
while training and the issue of feature selection,
which can be challenging to make the model
interpretable by healthcare providers to grasp the
rationale behind the prediction. Another problem will
be overfitting, as such models are typically very well
trained on small, narrow datasets, and thus will
compromise their generalizability to larger patient
populations. Finally, the onset of these complex
analytics systems will probably be difficult to adjust
in working healthcare systems and will also pose
logistically challenging integration work by health
organizations.
7 SYSTEM ARCHITECTURE
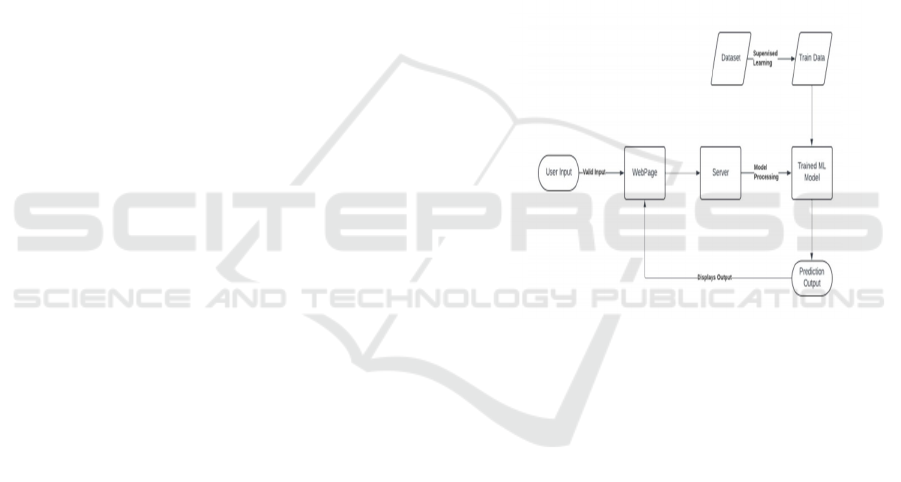
Pre-labeled data is used for training machine learning
models and supervised learning techniques. In case of
a labeled dataset being available, one approaches
supervised learning with the method of training a
model wherein each example is tied up with a known
outcome or label. For instance, in disease prediction
cases, the training data can be about patient
information with a disease or not.
Figure 4 shows
Workflow Diagram.
Training with Labeled Data: This software learns
the relationships of the data itself and hence analyzes
features like age and glucose level in relation to the
existence or non-existence of a disease
Model Training: It could be considered as model
training where the model looks for patterns and
correlations between the input, including features and
outcome, while scanning the labeled data.
Testing of the Model: Then, test the model against
unseen data, based on performance measures that
may be derived. All the training processes show how
models predicts real-time results.
Making Predictions: The model, after successful
train and test, can be applied to predict the chance of
developing a disease based on information being
provided by patients.
UI User Interface The frontend of this application is
implemented using Streamlit. It will be an interactive
environment where a user can be able to interact with
the application. Major components include:
Streamlit Application: This is the frontend; here is
where the user interacts with the app.
Sidebar Navigation: In this page, one would provide
the user with an option to choose the disease they
wish to predict.
Disease Prediction: Pages These would be different
pages in which Diabetes, Heart Disease, and
Parkinson's Disease would be predicted separately.
Figure 4: Workflow diagram.
Backend Components: This is where the features of
backend architecture hold the loading and making of
predictions via the model. Some of these include.
Load & Predict Diabetes Model: To load the
Diabetes pre-trained model so that it will make
prediction based on users' input
Load & Predict Heart Disease Model: The Heart
Disease model is loaded into such a system and run
with predictions
Load & Predict Parkinson's Model: Loads the
Parkinson's model and makes predictions.
D. Data Flow
The application has its data flow in three stages
User Interaction: Users wish to see a type of disease
predication by clicking it in the sidebar and then log
data correspondingly on the specific page it leads to.
Model Processing: The data submitted for the
Predictive Analytics for Multiple Diseases Using Machine Learning
97
building of the prediction is forwarded to the
concerned model of machine learning.
Results Display: On the same page of submission,
the user will get the results of the prediction,
displaying whether they are likely to have that disease
or not.
This structured architecture clearly differentiates the
user interface and backend processing, making the
application better in modularity and maintainability.
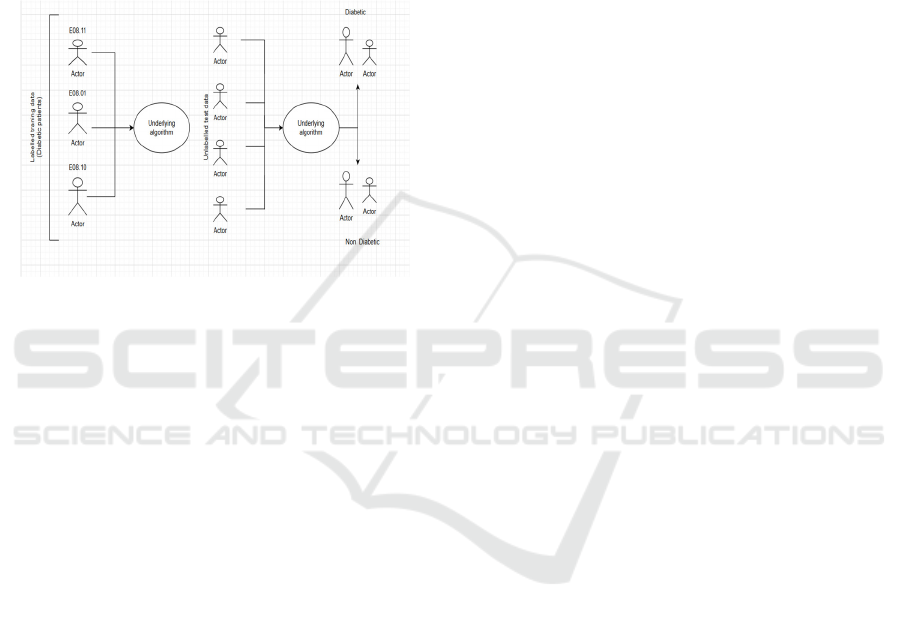
The
figure 5 shows Use case diagram.
Figure 5: Use case diagram.
8 RESULTS AND CONCLUSIONS
In our multiweapon machine learning application in
predictive analytics, we thus developed a multimode
system that has resulted in increased accuracy in
disease diagnostics with the Medicare patients. The
models were trained on SVM for diabetes and for
Parkinson's, while the best logistic regression
emerged with the further preprocessing and feature
selection of the diverse datasets. We found that, upon
validation, our models generally performed very well
and generalized well across demographics.
For example, in the multi-algorithm approach, it
integrated not only the minimization of the inherent
biases in the single-algorithm model but also
comprehensive assessment of diversity in various
techniques of prediction. Our system then ably
managed high-quality datasets and scaled the diverse
datasets so as to confront most common issues one
would face when deploying a model for disease
prediction: overfitting and data noise. The friendly
interface set up using Streamlit has made interaction
seamless and thus allows for real time prediction
based on users' input.
The general aim of this project is to be able to
show how predictive analytics may come to
revolutionize health care through the use of chronic
diseases.
Indeed, with the lessons learnt in the results from our
study, such machine learning technologies shall have
practical applications to offer timely and personalized
solutions to patients through their respective health
care providers. Work on such aspects provides initial
building blocks for future innovations in the usage of
machine learning within clinical applications,
therefore, healthcare professionals can base their
decisions on real data-driven revelations.
REFERENCES
A. Belle et al. (2015). "Big data analytics in healthcare,"
BioMed Research International, 2015.
A. Esteva et al. (2017). "Dermatologist-level classification
of skin cancer with deep neural networks," Nature,
542(7639), 115–118.
A. Rajkomar et al. (2019). "Machine learning in medicine,"
New England Journal of Medicine, 380(14), 1347–
1358.
A. Esteva et al. (2019). "A guide to deep learning in
healthcare," Nature Medicine, 25(1), 24–29.
B. Shickel et al. (2018). "Deep EHR: A survey of recent
advances in deep learning techniques for electronic
health record (EHR) analysis," IEEE Journal of
Biomedical and Health Informatics, 22(5), 1589–1604.
E. J. Topol (2019). "High-performance medicine: the
convergence of human and artificial intelligence,"
Nature Medicine, 25(1), 44–55.
F. Wang & A. Preininger (2019). "AI in health: state of the
art, challenges, and future directions," Yearbook of
Medical Informatics, 28(1), 16–26.
G. Huang et al. (2017). "Densely connected convolutional
networks," Proceedings of the IEEE Conference on
Computer Vision and Pattern Recognition, pp. 4700–
47.
G. Litjens et al. (2017). "A survey on deep learning in
medical image analysis," Medical Image Analysis, 42,
60–88.
H. C. Shin et al. (2016). "Deep convolutional neural
networks for computer-aided detection: CNN
architectures, dataset characteristics and transfer
learning," IEEE Transactions on Medical Imaging,
35(5), 1285–1296.
H. Liang et al. (2019). "Evaluation and accurate diagnoses
of pediatric diseases using artificial intelligence,"
Nature Medicine, 25(3), 433–448.
Hodge and Austin (2020). "Applications of ensemble
methods in diabetes and heart disease predictions,"
Journal of Medical Systems.
P. S. Kohli & S. Arora (2018). "Application of machine
learning in disease prediction," 4th International
Conference on Computing Communication and
Automation (ICCCA), pp. 1–4.
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
98

R. Miotto et al. (2018). "Deep learning for healthcare:
review, opportunities, and challenges," Briefings in
Bioinformatics, 19(6), 1236–1246.
S. Uddin, A. Khan, M. E. Hossain, & M. A. Moni (2019).
"Comparing different supervised machine learning
algorithms for disease prediction," BMC Medical
Informatics and Decision Making, Vol. 19, No. 1, pp.
1–16.
Sun et al. (2017). "Systematic review on preprocessing for
generalization in ML," Journal of AI in Medicine.
Varma & Simon (2006). "Cross-validation for
optimization," Statistical Models in Medicine.
X. Liu et al. (2019). "A comparison of deep learning
performance against health-care professionals in
detecting diseases from medical imaging: a systematic
review and meta-analysis," The Lancet Digital Health,
1(6), e271–e297.
Z. Zhang & L. Wang (2019). "Machine learning for clinical
trials in the era of precision medicine," Contemporary
Clinical Trials, 86, 105819.
Z. Obermeyer et al. (2019). "Dissecting racial bias in an
algorithm used to manage the health of populations,"
Science, 366(6464), 447–453.
Predictive Analytics for Multiple Diseases Using Machine Learning
99
