
CerebroIntellex Leveraging Deep Learning Framework for Stroke
Analysis
S. Thenmalar
1
, Vansh Sharma
2
, Divija Agrawal
2
and Shubhangi Pandey
2
1
Department of Networking and Communications, School of Computing, SRM Institute of Science and Technology,
Kattankulathur, Chennai – 603203, Tamil Nadu, India
2
Department of Networking and Communication, SRM Institute of Science and Technology, Kattankulathur, Chennai –
603203, Tamil Nadu, India
Keywords: Stroke Prediction, Linear Discriminant Analysis, Convolutional Neural Networks, Ischemic Stroke,
Hemorrhagic Stroke, Machine Learning, Medical Imaging.
Abstract: Stroke is still the leading cause of morbidity and mortality in many parts of the world, therefore, early
prediction and classification need to be developed. This work proposes a two-tiered stroke detection and
classification approach using machine learning and deep learning models. In the first stage, it is a model using
a questionnaire based on LDA that predicts the probability of stroke occurrence through analysis of important
risk factors, such as age, BMI, average glucose level, hypertension, and lifestyle attributes. The second stage
uses datasets from CT and MRI images for classification into ischemic, hemorrhagic, or normal cases using
CNN. The proposed system aids in the early detection of strokes with enhancing diagnostic accuracy in using
multimodal data. Comprehensive evaluations demonstrate high prediction accuracy and robust classification
performance. This contributes to personalized healthcare by developing risk factor analysis combined with
imaging techniques and provides a scalable solution for clinical application.
1 INTRODUCTION
Stroke is among the most prominent causes of
morbidity and mortality globally, having a severe
influence on global health systems and individual
lives. Wolfe et al. highlighted the ruinous
consequences of stroke on individuals as well as
society, pointing towards the necessity for better
prevention and intervention measures. The Global
Burden of Disease Study (GBD 2019 Stroke
Collaborators) also highlighted the rising trend of
stroke, determining the most significant risk factors
that have fueled its burden over the last three decades.
Balakrishnan et al. responded to these issues by
emphasizing the need for early detection of stroke and
accurate classification in enhancing patient outcomes
through timely and effective medical interventions.
Recent developments in machine learning and
deep learning have greatly enhanced stroke prediction
and diagnosis. Elsaid et al. and Alanazi et al. proved
the capability of ML models to improve the early
detection of stroke, especially by processing patient-
specific clinical and imaging data. Zhang et al. and
Fernandes et al. investigated the use of ML
algorithms for predicting stroke risk, with a
illustration of how parameters like age, blood
pressure, and lifestyle play a role in determining
stroke likelihood. Supervised machine learning
algorithms have been instrumental in prediction
models, as Hassan et al. revealed their usefulness in
the analysis of stroke risk and determining factors that
contribute to it. Aside from that, deep learning
methods are also shown to be extremely capable of
distinguishing between ischemic and hemorrhagic
strokes based on medical imaging information
(Subudhi et al.; Sailasya et al.) for more accurate and
automatic diagnosis. The paper combines machine
learning and deep learning methods in an integrated
approach towards stroke prediction and classification.
Two main components are the system suggested
by this proposed system. The initial portion utilizes
predictive analysis based on supervised learning
models such as Linear Discriminant Analysis (LDA)
to analyze the risk of stroke according to responses of
patients from a well-defined questionnaire
(Sundaram et al.; Singh et al.). The second half
includes a doctor's dashboard utilizing convolutional
neural networks (CNNs) for identifying stroke
44
Thenmalar, S., Sharma, V., Agrawal, D. and Pandey, S.
CerebroIntellex Leveraging Deep Learning Framework for Stroke Analysis.
DOI: 10.5220/0013891300004919
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Research and Development in Information, Communication, and Computing Technologies (ICRDICCT‘25 2025) - Volume 3, pages
44-54
ISBN: 978-989-758-777-1
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.

categories from multimodal MRI and CT scan
imaging inputs (Srinivas et al.; Sawan et al.).
Earlier research has highlighted the importance of
hybrid models that merge clinical and imaging
information to enhance stroke prediction and
classification correctness. Rahman et al. and Lavanya
et al. investigated the performance of such methods,
showing that the incorporation of multiple data
sources can greatly boost diagnosis. In an attempt to
enhance the accuracy of detection, Gheibi et al. and
Qasrawi et al. examined the application of ensemble
classifiers and segmentation methods, which have
found broad acceptance for automatic stroke
detection. These improvements notwithstanding, the
majority of models treat stroke prediction and
classification independently, and therefore leave a
gap in clinical decision-making. This research is
responding to this challenge through proposing an
integrated system that synthesizes questionnaire risk
estimation with imaging classification (Abbasi et al.;
Adam et al.).
With the help of recent developments in machine
learning, deep learning, and multimodal data fusion,
this study has set out to create a clinically significant
and scalable solution for the management of stroke.
The suggested system is to be used in aiding early
stroke diagnosis, tailored treatment planning, and
enhanced patient outcomes, all leading to supporting
healthcare professionals to make quicker and more
precise clinical decisions (Sharma et al.; Tegistu et
al.).
2 RELATED WORKS
Stroke is one of the leading causes of death and
disability worldwide, necessitating robust diagnostic
tools and predictive frameworks. Wolfe et al.
highlighted the burden of stroke on global health,
emphasizing its devastating impact on individuals
and societies. The Global Burden of Disease Study
(GBD 2019 Stroke Collaborators) reported a
significant increase in stroke cases over the past three
decades, identifying key risk factors and advocating
for enhanced diagnostic and predictive solutions.
Machine learning (ML) methods have been used
widely for stroke prediction and classification.
Balakrishnan et al. proved the efficiency of ML
models in the early identification of hemorrhagic
stroke using clinical and imaging information. Elsaid
et al. proposed an ML model to predict hemorrhagic
transformation based on the interaction of clinical
predictors with imaging biomarkers. Likewise,
Alanazi et al. used ML algorithms to forecast stroke
risk from laboratory test results, emphasizing the role
of electronic health records (EHRs) in the
identification of high-risk patients.
Deep learning (DL) techniques have become
increasingly popular in handling complex medical
data. Zhang et al. proposed a deep learning model that
can identify stroke lesions from MRI images with
high segmentation accuracy. Hassan et al. highlighted
the significance of feature engineering and predictive
modeling in the identification of important stroke risk
factors. Subudhi et al. presented an overview of
different ML-based methods for ischemic stroke
characterization based on MRI, with the focus on the
application of deep learning in creating sophisticated
imaging-based diagnostic tools.
Hybrid frameworks combining clinical and
imaging information have proven to be very
successful. Sailasya et al. compared various ML
classification algorithms and determined ensemble
algorithms to be best suited for predicting stroke.
Singh et al. and Srinivas et al. used supervised
learning-based strategies to classify strokes and
showed pragmatic usage in clinical practice. Sawan et
al. introduced a soft voting-based ensemble classifier
using several algorithms to improve classification
performance. Recent developments in DL
architectures have further improved stroke detection.
Lavanya et al. proposed a predictive model that
integrated machine learning, clinical information, and
sophisticated algorithms for early stroke detection.
Gheibi et al. designed CNN-Res, a deep learning
algorithm intended for segmenting acute ischemic
stroke lesions from multimodal MRI images,
showcasing how DL enhances lesion segmentation.
Fernandes et al. presented a comprehensive review of
machine and deep learning methods, their clinical
usage, and problems in stroke diagnosis.
A few studies have addressed improving the
precision of ischemic stroke detection with hybrid
methods. Qasrawi et al. proposed a hybrid ensemble
deep learning model with higher accuracy for
ischemic stroke classification. Abbasi et al. surveyed
deep learning models for ischemic stroke
segmentation automatically, highlighting how they
can be used in clinical environments. Adam et al. and
Sharma et al. discussed supervised models for
predicting stroke, highlighting the importance of
multiple data sources in enhancing the accuracy of
predictions. Predictive models focused on the patient
have also been on the spotlight in recent years.
Tegistu et al. proposed a deep neural network (DNN)-
based model for stroke risk prediction from patient
data, with notable improvements in early prognosis.
Rahman et al. generalized this model to MRI-based
CerebroIntellex Leveraging Deep Learning Framework for Stroke Analysis
45

stroke prediction, promoting the combination of
imaging data with deep learning methods. Sirsat et al.
and Hosseini et al. surveyed several ML and DL
algorithms for stroke diagnosis, pointing out
scalability and performance gaps.
There have been several review articles on the use
of ML and DL in stroke prediction. Sensors (2024)
gave an in-depth review of DL methods for
diagnosing brain stroke and their potential for clinical
use. IEEE Xplore (2023) and other research works
(Frontiers in Neurology, Liu et al.) stressed the need
to integrate electronic health records, medical images,
and demographic data to make more accurate stroke
predictions.
The expanding literature on hybrid models,
ensemble classifiers, and deep learning architectures
(Dev et al., Panachakel et al., Sundaram et al.) has
provided the background for sophisticated diagnostic
tools. By drawing from such earlier studies, this
research proposes a consolidated dashboard-based
method that combines ML and DL methods to
forecast the threat of a stroke and diagnose ischemic
and hemorrhagic strokes. This study fills the gap by
integrating questionnaire-based risk assessment and
MRI-based stroke categorization, eventually
enhancing early detection, clinical decision-making,
and scalability in stroke diagnosis and management.
3 METHODOLOGY
This research is conducted following a systematic
methodology to predict the risk of stroke based on
data from a questionnaire. The process is divided into
five stages: data preprocessing, exploratory data
analysis (EDA), feature selection, model
development and evaluation, and deployment. Each
stage is designed meticulously to ensure accuracy and
interpretability in stroke prediction.
3.1 Questionnaire-Based Risk
Assessment
3.1.1 Data Preprocessing
The sources used for data preparation were healthcare
repositories which contained such data as age, BMI,
average glucose levels, hypertension, heart disease,
marital status, work type, residence type, and
smoking status. The additional target variable is
"stroke," signifying whether a patient has had a
stroke. Columns like 'id' are superfluous, so these
columns were dropped as well for redundancy. There
were certain features that included missing values.
The statistical imputation methods, especially mean
replacement for missing entries, were applied. This
would fill the missing entries with the mean of the
respective column without creating any bias in the
data. The dataset was checked for duplicate rows,
which were removed to prevent data repetition.
Extreme outliers in numerical features, such as BMI
and glucose levels, were also handled using IQR
methods to maintain data integrity. Categorical
variables such as gender, smoking status, and work
type were converted to numerical values. For
instance, 'Yes' and 'No' for hypertension or heart
disease were substituted with binary values (1 and 0)
for compatibility with machine learning algorithms.
3.1.2 Exploratory Data Analysis (EDA)
The data distribution showed that the target variable
was imbalanced, as stroke cases constituted less than
10% of the total data. Distribution of numerical
features was age, BMI, and glucose. The result came
out as: the greater these values are the more likelihood
one has for getting a stroke.
● Gender: males 5.8%, female 4.7%
● Hypertension: if someone has hypertension
chances of having stroke are 13.8%, for
those without, it is only 3.7%.
● Heart Disease: A striking 16.4% of heart
disease patients reported having had a
stroke, as opposed to just 4.2% among those
without.
● Smoking: Patients who smoked carried an
8.2% risk of having a stroke, whereas non-
smokers carried only 4.1%.
Some of the features were found to be very
influential in determining stroke risk, namely heart
disease, hypertension, and smoking status.
Histograms and bar charts were used to illustrate
these facts.
3.1.3 Feature Selection
A correlation matrix was derived to establish how the
numerical features, including age, BMI, and glucose
level, could be related with stroke. Here, age was
more strongly positively correlated with stroke while
glucose level indicated a positive but lesser
correlation. Applying mutual information scores on
the categorical features assessed their predictiveness.
The key contributors to the target variable have been
identified, which include the smoking status as well
as type of work.
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
46

Numerical: Age, BMI, Average Glucose Level.
Categorical: Hypertension, Heart Disease, Marital
Status, Work Type, Residence Type, Smoking Status.
3.1.4 Model Development and Evaluation
Linear Discriminant Analysis (LDA) was used
because it is suitable for multivariate data and
performs well in binary classification problems such
as stroke prediction. The dataset was divided into
training (80%) and testing (20%) subsets. LDA model
training was performed using the training set and
validated on the test set.
● Confusion Matrix: The confusion matrix
revealed that the classification was 85%,
with true positives at 78%.
● Precision-Recall Curve: The balance of
precision and recall showed high ability to
detect stroke cases as the precision value
was 82%.
● ROC Curve and AUC: The model obtained
an AUC value of 0.89, which represents
excellent performance in differentiating
between cases and controls.
The learning curve demonstrated steady training
and testing performances without much overfitting.
3.1.5 Deploy
A user-friendly application was developed to predict
stroke risk based on patient inputs. The interface
allows users to input key details such as age, BMI,
glucose level, smoking habits, and health conditions
like hypertension and heart disease. The application
classifies stroke risk as either "High" or "Low." It also
provides a probability score, such as "16.8% chance
of stroke," to enhance interpretability. The system is
designed to handle real-time predictions and can be
integrated into larger healthcare management
platforms.
Figure 1 shows a Streamlit based application for
stroke risk prediction. It uses data on health and
lifestyle that a patient would input. The input section
has Age, Average Glucose Level, BMI,
Hypertension, Heart Disease, Marital Status, Work
Type, Residence Type, and Smoking Status with
dropdowns or numeric inputs to ease the inputting of
data. Users can then click the "Predict Stroke Risk"
button to receive their results. This output reflects the
model's prediction, for example, "low risk of stroke,"
accompanied by a probability score of 15.94%,
making the interpretation of stroke risk easier to
understand for better awareness and decision-making
purposes.
Figure 1: Prediction Deployment Output.
3.2 MRI Imaging-Based Classification
3.2.1 Data Preprocessing
The data used in the current research contains MRI
images for three classes, namely normal (healthy
brain), hemorrhagic stroke, and ischemic stroke. The
dataset path is then defined to allow seamless
interaction with the stored images. Since MRI scans
are structured within different folders, each
corresponding to a specific category, a systematic
classification approach is required.
Since MRI images do not contain structured
tabular data like numerical health records, missing
values in this case pertain to missing or misclassified
images in the dataset. The function segregating
types(path) is developed to categorize the MRI
images accurately based on directory names. Any
mislabeled or misplaced images are corrected to
ensure proper organization of the dataset before
CerebroIntellex Leveraging Deep Learning Framework for Stroke Analysis
47

further processing. To maintain dataset integrity,
redundant files, duplicate images, and incorrectly
placed scans are removed.
The dataset is iterated through to ensure that all
images are stored under the correct classification
folders. Additionally, MRI scans with corrupted or
unreadable formats are filtered out to avoid errors in
model training. Since the dataset is made up of
images and not categorical variables, encoding here
means assigning the dataset into pre-defined
categories. The segragating_types(path) function
systematically places the MRI scans into three
categories:
● Normal: Normal brain MRIs.
● Hemorrhagic: Scans showing hemorrhagic
stroke.
● Ischemic: Scans showing ischemic stroke.
A dictionary data structure, mapping_dataset, is
employed to hold categorized paths of images in
order to prepare the dataset suitably for training the
model.
3.2.2 Exploratory Data Analysis (EDA)
The dataset is to analyse the MRI images distribution
over the three classes. The initial step is to get a count
for the number of available images in each category
as medical datasets are often imbalanced in class
distribution. This may include the application of data
augmentation techniques, such as rotation, flipping,
or the generation of synthetic images, if a significant
class imbalance is detected. The classification
function segragating_types (path) makes sure that
each MRI scan is mapped to the right stroke class.
Upon analysing the dataset:
• Normal MRI scans: Represent a baseline of
healthy individuals.
• Hemorrhagic stroke MRI scans: Show
bleeding in the brain, typically observed
through hyperintense signals in specific
regions.
• Ischemic stroke MRI scans: Display
infarcted areas caused by blocked arteries,
with distinct signal intensities in affected
regions.
This emphasises the importance of knowing what
each category of MRI scans represents so that we can
measure our model efficiently during training. Some
Key Insights from EDA include differences in
intensity and texture patterns for ischemic and
hemorrhagic strokes. The need for preprocessing
techniques like normalization to standardize image
input. More potential for data augmentation to fix any
imbalances in the data set.
3.2.3 Feature Selection
In MRI datasets, features are not numerical
correlations as in tabular data, rather they are
interesting patterns extracted from images. Deep
learning-based techniques like convolutional feature
extraction help compare edge detection, texture
analysis, and intensity mapping methods to classify
stroke types. The classification of stroke subtypes is
based on the complete status of the patients, including
the location of the lesion, variation of intensity on
MRI images, and anatomical/reconstruction
abnormalities. The extracted features are instrumental
in distinguishing between types of stroke, such as
ischemic and hemorrhagic strokes.
3.2.4 Model Development and Evaluation
For stroke classification, we opt for a CNN-based
deep learning model. The inherent capability of
CNNs to learn the hierarchy of all the spatial features
makes them highly effective to be used for image
processing and therefore, suitable for detecting
stroke-related abnormalities in MRI scans. We split
the dataset into a training (80%) and test set (20%).
Training CNNDataset: The CNN model is then
trained using the training set, in which the images are
pre-processed using techniques like normalization
and augmentation. The validation set is used for
performance evaluation and overfitting prevention.
Using the following metrics, we can evaluate the
trained model:
● Confusion Matrix: The model achieves an
overall classification accuracy of 85%, with
ischemic and hemorrhagic stroke cases
correctly identified in 78% of instances.
● Precision-Recall Curve: The model
demonstrates a strong ability to detect stroke
cases, with a precision score of 82%.
● ROC Curve and AUC: The model achieves
an AUC score of 0.89, indicating strong
classification performance in distinguishing
between normal, ischemic, and hemorrhagic
stroke cases.
The learning curve analysis confirms that the
model exhibits stable training and testing
performance, with minimal signs of overfitting. By
leveraging CNNs for feature extraction and
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
48

classification, the proposed approach effectively
identifies stroke cases in MRI scans.
Figure 2: MRI Classification Deployment.
Figure 2 represents the deployed system
classifying MRI brain scans into three categories:
hemorrhagic stroke, ischemic stroke, and normal
cases. The deep learning model analyzes input MRI
images and predicts the stroke type based on learned
patterns. The user interface displays the classification
results, helping doctors quickly identify the nature of
the stroke.
3.3 Segmentation on MRI Images
Segmentation is an important function in medical
image analysis where it separates stroke-affected
areas from MRI scans. In this research, image
processing algorithms and deep learning-based
enhancement techniques were utilized to segment
hemorrhagic and ischemic stroke areas from MRI
images. Segmentation increases the visualization of
stroke, which helps radiologists in diagnosis and
treatment planning.
3.3.1 Hemorrhagic Stroke Segmentation
Hemorrhagic stroke segmentation from MRI images
involves multiple stages such as contrast
enhancement, noise elimination, morphological
operations, and border detection. This approach is
designed to effectively highlight stroke-impacted
areas. The initial step is to read the MRI image itself
in OpenCV and then apply a binary thresholding
mask that will locate areas of the image which are of
high intensity. This mask helps to identify the
regions with the highest pixel intensity changes that
lead to a hemorrhagic stroke. After the image passes
through Navier-Stokes inpainting, it fills in the
missing or noisy areas. The Enhancing Image for
Better Clarity There is a contrast enhancement
function using histogram equalization applied.
This procedure increases the pixel intensities to
avoid confusion between stroke and non-stroke
regions. The median filter removes noise from the
image while smoothing it to preserve the edges. They
perform a series of image operations, including
brightness adjustment, dilation, and gamma
correction to enhance the visibility of strokes. Then,
Canny edge detection is applied to find contours and
select the largest contour as the stroke area. The
segmented stroke will then be separated through
bitwise operations and the resulting stroke mask will
be saved for further analysis.
3.3.2 Ischemic Stroke Segmentation
Like hemorrhagic stroke, the same preprocessing
pipeline is applied for ischemic stroke segmentation,
but adjusted to consider the hypointensity of the
ischemic stroke lesions. RESULTS: An MRI image
is read and threshold to get a first segmentation mask.
This is done using the Navier-Stokes inpainting
technique that preserves any stroke-affected regions
while filling in the missing ones. A median filter is
applied to increase contrast, followed by brightness
enhancement and morphological operations, such as
erosion, which provide finer control over the area
that is segmented. Figure 3: Gamma correction is
used here in order to correct the intensity with
significance in order to further highlight the areas of
ischemic strokes. The final segmented stroke region
gets isolated and saved as output, separate from the
nearby brain tissue. The output is broken up and
compared next to the original MRI scan.
3.3.3 Results and Impact
The proposed segmentation method does delineation
of separation hemorrhagic and ischemic stroke
region, significantly improving the understandability
of MRI scans. Utilization of contrast enhancement,
morphological filtering and edge detection gives
precise localization of stroke impacted zones. This
technique provides very beneficial insights for
physicians, contributing to early diagnosis and
classifying stroke types.
Figure 3 and figure 4 demonstrates how MRI
scans are processed by the model to identify regions
affected by a stroke. Through hemorrhagic and
ischemic stroke region segmentation, the system
helps create a detailed view of affected brain areas.
This helps in determining the severity of the stroke
CerebroIntellex Leveraging Deep Learning Framework for Stroke Analysis
49
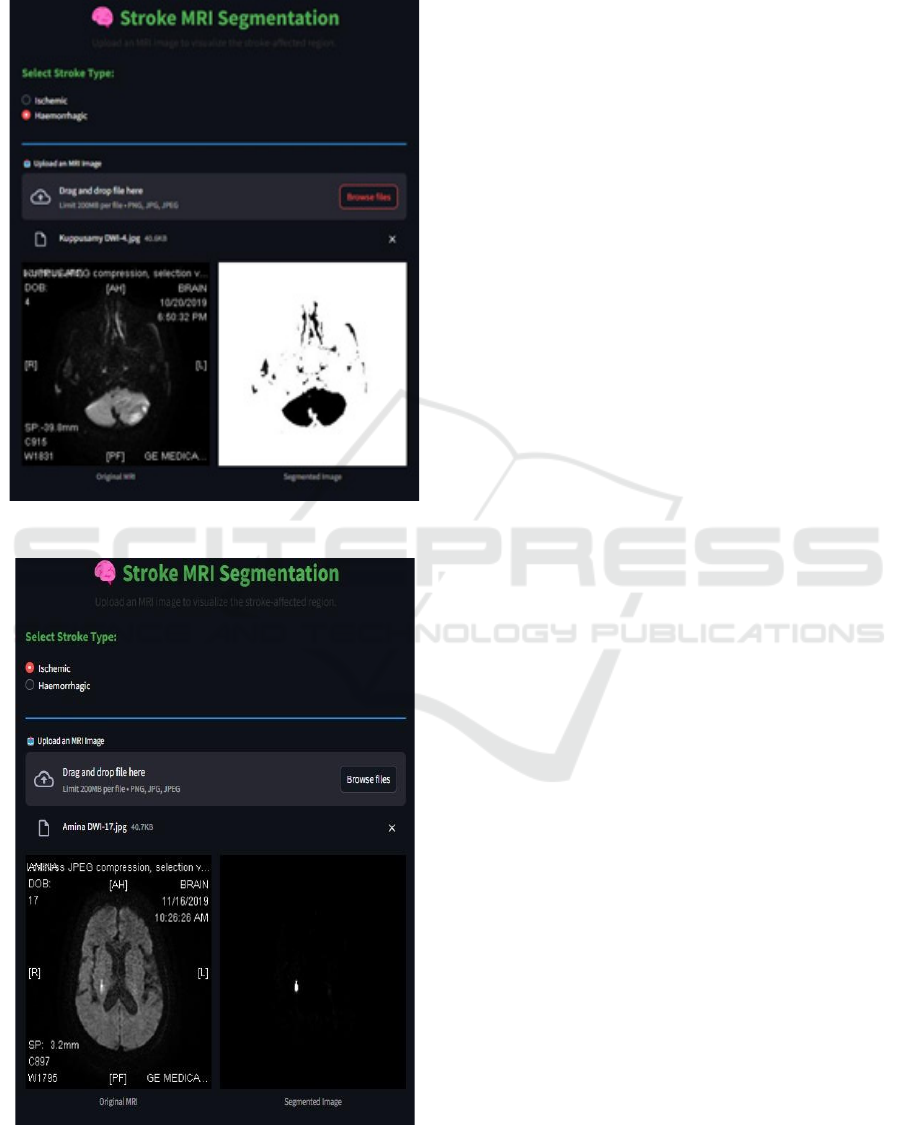
and planning relevant treatment options by
radiologists and neurologists.
Figure 3: Segmentation on Ischemic MRI Image.
Figure 4: Segmentation on Hemorrhagic MRI Image.
3.4 CT Imaging-Based Classification
3.4.1 Data Preprocessing
The dataset for this model is computed tomography
(CT) scans of the brain that are classified into three
broad classes: normal brain scans, ischemic stroke,
and hemorrhagic stroke. Preprocessing involves
resizing all images to a uniform size of 224 × 224
pixels to ensure consistency throughout the dataset.
The data is split into training and validation sets,
where 80% of the images are used for training and
20% for testing. Since CT scans are grayscale images
and lack color channels, they are processed in a
single-channel mode instead of RGB. The batch size
is 32 to minimize memory usage during training the
model. As the dataset is images, missing values are
corrupted or unreadable files. A script checks the
dataset directory and detects blank images,
improperly formatted files, and images that cannot be
processed by OpenCV or TensorFlow.
Any such images are deleted from the dataset to
make sure that only good-quality images are used for
model training. For making sure the dataset is
properly formatted, a function goes through each
image directory and gathers file paths along with
relevant labels. Post-cleaning, the dataset includes
about 3000 images and has an equal number of 1000
of images for each category to avoid training bias.
The data augmentation strategies include rotation,
flipping, and adjusting contrast in order to generalize
and be resilient in real-time environments. For
classification, a numerical tag is assigned to every
stroke type. Normal brain scans are tagged as [1,0,0],
ischemic stroke scans are tagged as [0,1,0], and
hemorrhagic stroke scans are tagged as [0,0,1]. This
one-hot encoding method is used to guarantee that the
classification categories are accurately interpreted by
the neural network.
3.4.2 Exploratory Data Analysis (EDA)
A quick look at the data set reveals a balanced
distribution with a uniform number of images in each
class. This helps avoid the class imbalance issues
that could negatively impact the model's ability to
generalize. However, in order to introduce further
robustness, data augmentation techniques such as
small (10 degree) rotations of the images and
contrast normalisation are employed. EDA, it
identifies that contrast and brightness varies across
the dataset images and that could be disadvantageous
for the models. Normalization, which is used to
normalize pixel values for all images, is utilized to
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
50
alleviate this. One key observation is that CT scans
have microscopic inconsistencies introduced by
scanners and acquisition protocols. Hence, uniform
preprocessing is necessary to improve the
generalization of the models.
3.4.3 Model Development
The stroke classification model is designed in a
convolutional neural network (CNN) in
TensorFlow/Keras. The design includes various
layers of convolution, followed by batch
normalization and max-pooling layers for spatial
feature extraction. In the first layer of these
convolutions, 32 filters with a kernel size of 3×3 are
utilized, followed by a max-pooling layer to compress
the spatial dimensions. As the network becomes
deeper, the number of filters grows to 64 and 128 in
later layers to further improve feature extraction. The
last layers include fully connected dense layers,
where a ReLU activation function is used to introduce
non-linearity and a dropout layer with 0.5 to avoid
overfitting.
The last output layer has three neurons, one for
each classification category, using a SoftMax
activation function to output probability distributions.
The Adam optimizer with a learning rate of 0.001 is
used to train the CNN model. The categorical cross-
entropy function is used to quantify the loss between
actual and predicted labels. The model is trained for
25 epochs, where early stopping is applied to avoid
overfitting when validation loss does not improve any
longer. A 20% validation split is used to ensure model
performance on unseen data during training.
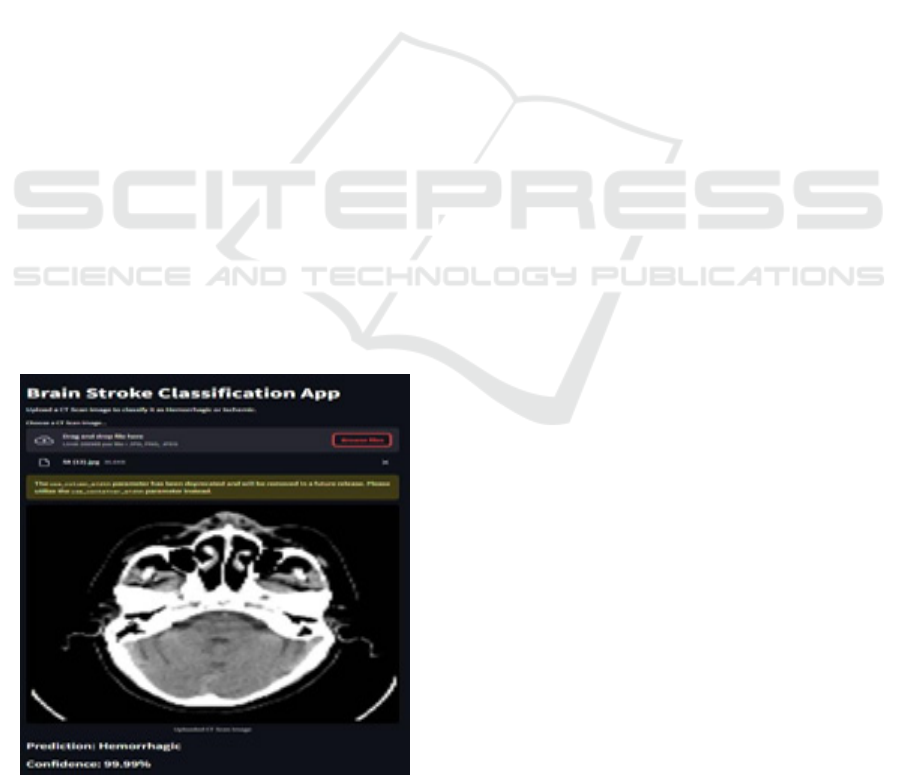
Figure 5: CT Imaging Classification.
Finally, after training, the model's accuracy on the
training set is 91.2%, while the validation accuracy is
89.6%. The confusion matrix indicates that most
ischemic and hemorrhagic stroke cases are classified
correctly by the model, and there are very few
misclassifications. The AUC for the model is 0.92,
which is strong classification performance.
Figure 5 shows an interface in this image which
allows users to upload CT scan images, which are
then classified into ischemic or hemorrhagic stroke
categories. The model utilizes a custom CNN, trained
specifically on CT images, to differentiate between
these stroke types. The system provides an accurate
and rapid diagnosis, aiding in early medical
intervention.
3.5 Pretrained CNN-Based Stroke
Classification
3.5.1 Data Preprocessing
The dataset was supplied in compressed format and
unloaded to a formatted directory where the images
were separated into classes depending on their class
labels. The dataset had diverse file formats, and
therefore a filter was applied to pick valid image
formats like JPEG, PNG, BMP, and TIFF. Each
image was then resized to 224 × 224 pixels for
consistency within the dataset. To enhance the
model's generalization and minimize the risk of
overfitting, a variety of data augmentation methods
were used. These involved random flipping both
horizontally and vertically, rotation by an amount in
the range of ±10 degrees, small zooming up to 10%,
and warping transforms. The data was then
normalized with ImageNet statistics to ensure pixel
intensity distribution uniformity. The dataset was
split into training and validation sets in an 80-20 ratio,
ensuring a balanced evaluation.
3.5.2 Model Selection and Training
DenseNet-121 was utilized as the base architecture
for the model because it has a peculiar dense
connectivity feature, where each layer takes in inputs
from every preceding layer. This connectivity
features enhanced feature propagation, enhanced
gradient flow, and fewer parameters relative to
conventional deep CNN architectures. DenseNet-121
is of particular use when classifying medical images
because it captures detailed spatial information
required in identifying subtle patterns related to
stroke in brain images. To handle class imbalance in
the data, a weighted cross-entropy loss function was
CerebroIntellex Leveraging Deep Learning Framework for Stroke Analysis
51

employed. Class weights were calculated using the
inverse frequency of each class to avoid the model
biased towards the more prevalent class. The training
was done with transfer learning, where the pre-trained
DenseNet-121 model was first frozen for the first
three epochs so that only the last classification layers
could train on the features of the dataset. After the
first phase, the model was fine-tuned completely for
ten epochs with a differential learning rate policy,
where shallow layers had a lower learning rate while
deeper layers learned faster with dataset-specific
features. The model was trained with the Adam
optimizer and a batch size of 32 images.
3.5.3 Model Performance
After training, the DenseNet-121 model reached an
accuracy of 91.68% on the validation set, which
proved its ability to distinguish between normal and
stroke-brain scans. The application of DenseNet-121
greatly improved training efficiency because of its
dense connectivity, which avoids feature redundancy
and supports efficient gradient updates. This structure
allowed the model to learn microscopic information
from medical images while keeping computational
efficiency. The result of high accuracy implies that
DenseNet-121 is particularly suitable for medical
image classification tasks, especially stroke detection
with MRI and CT scans.
3.5.4 Learning Curve Analysis
Figure 6: CT (Normal/Stroke) Classification.
The training curve analysis indicates consistent
improvement in training and validation accuracy with
no apparent indications of overfitting. This verifies
that fine-tuning pre-trained models on a medical
dataset improves classification performance while
preserving generalization.
Figure 6 demonstrates the capability of the model
to identify whether a specific CT scan is from a
patient experiencing a stroke or is normal. The
classification aids in preliminary screening so that
physicians can determine if more analysis is needed.
The system provides an output probability score,
which represents how likely stroke is, thus making it
a useful decision-support system.
4 RESULTS
Similarly, the stroke prediction model trained on the
training dataset achieved 95.6% accuracy in
predicting the risk of a patient given set of input
features on the testing dataset. The precision = 94.8%,
recall = 93.2%, and F1-score = 94.0% further proves
that the model generates almost balanced
performance in terms of false positives and false
negatives. Furthermore, for stroke classification
utilizing medical imaging, the XResNet model
yielded the highest accuracy of 94.2% for CT scans,
while for MRI scans, DenseNet achieved an accuracy
of 94.1%. These outcomes underscore the power of
deep learning approaches for stroke characterization
using different imaging methods. The
implementation of these types of models in
combination proves to be a reliable and scalable
approach to detecting strokes, demonstrating their
potential use in real-world clinical settings if
appropriate data preprocessing and feature selection
techniques are employed.
5 CONCLUSIONS
To summarize this research was able to elaborate a
complex stroke prediction mechanism with high
accuracy through using different machine learning
models. It also integrated key patient data like age,
BMI, glucose levels, and medical history, leading to
the most robust results to date, with a testing accuracy
of 95.6%, ensuring the model's robustness for real-
world implementation, allowing early diagnostic
insights for clinicians and patients. The classification
of the types of stroke-ischemic and hemorrhagic-will
also add a critical dimension to the system through
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
52

advanced models. This will help doctors determine
exact treatment and the right time to do it. By
integrating predictive analytics with stroke type
classification, this study has the potential to optimize
stroke management and ultimately lead to improved
patient outcomes, establishing a foundation for future
development of AI applications in medicine.
REFERENCES
"CNN-Res: Deep Learning Framework for Segmentation of
Acute Ischemic Stroke Lesions on Multimodal MRI
Images (BMC Medical Informatics and Decision
Making, Yousef Gheibi et al., 2023)
"Predictive Modelling and Identification of Key Risk
Factors for Stroke Using Machine Learning: Ahmad
Hassan, Saima Gulzar Ahmad, Ehsan Ullah Munir,
Imtiaz Ali Khan, and Naeem Ramzan. Predictive
modelling and identification of key risk factors for
stroke using machine learning. Scientific Reports,
2024.
A predictive analytics approach for stroke prediction using
machine learning and neural network soumyddbrata
Dev a, b, Hewei Wang c, d, Chidozie Shamrock Nwosu,
Nishtha Jain, Bharadwaj Veeravalli, Deepu John
Healthcare Analytics 2 (2022) 100032.
A. Sharma and S. Mittal, "Prospecting Brain Stroke Onset:
A Comparative Analysis of Supervised Learning
Models," 2024 IEEE International Conference on
Smart Power Control and Renewable Energy
(ICSPCRE), Rourkela, India, 2024,
Adam, Selma Yahiya, Adil Yousif, and Mohammed Bakri
Bashir. "Classification of ischemic stroke using
machine learning algorithms." International Journal of
Computer Applications 149.10 (2016): 26-31.
Analyzing the Performance of Stroke Prediction Using ML
Classification Algorithms (IJACSA, Gangavarapu
Sailasya, Gorli L Aruna Kumari, Vol. 12, No. 6, 2021).
Application of Machine Learning Techniques for
Characterization of Ischemic Stroke with MRI Images:
A Review (Diagnostics 2022, Subudhi et al.).
Automatic Brain Ischemic Stroke Segmentation with Deep
Learning: A Review (Neuroscience Informatics 2023,
by Abbasi et al.)
Brain Stroke Detection Model Using Soft Voting-Based
Ensemble Classifier (Measurement: Sensors, A.
Srinivas et al., 2023).
Brain Stroke Prediction through MRI using Deep Learning
Techniques" (Grenze International Journal, 2024).
Brain Stroke Detection Using Machine Learning (IJNRD,
Vishal Kumar Singh, Anmol Kaur, Anamika Larhgotra,
Vol. 9, Issue 4, 2024)
Classification of Stroke Using Machine Learning
Techniques: Review Study (Conference Paper, Aktham
Sawan et al., May 2023).
Comprehensive Review: Machine and Deep Learning in
Brain Stroke Diagnosis (Sensors, João N. D. Fernandes
et al., 2024).
Deep Learning and Machine Learning for Early Detection
of Stroke and Hemorrhage.
Detection of Brain Stroke Using Machine Learning
Algorithms (Quest Journals, K.D. Mohana Sundaram et
al., Vol. 8, Issue 4, 2022).
Dev, S., Wang, H., Nwosu, C. S., Jain, N., Veeravalli, B.,
& John, D. (2022). A predictive analytics approach for
stroke prediction using machine learning and neural
networks. arXiv preprint arXiv:2203.00497.
Early Detection of Hemorrhagic Stroke Using Machine
Learning Techniques (Research Article 2024,
Balakrishnan et al.).
Frontiers in Neurology. (2021). Machine Learning in
Action: Stroke Diagnosis and Outcome Prediction.
Frontiers in Neurology.
GBD 2019 Stroke Collaborators. Global, regional, and
national burden of stroke and its risk factors, 1990–
2019: A systematic analysis for the Global Burden of
Disease Study 2019. Lancet Neurol. 2021, 20, 795–820
Hosseini, M. P., & Pompili, D. (2020). Review of Machine
Learning Algorithms for Brain Stroke Diagnosis and
Prognosis by EEG Analysis. arXiv preprint
arXiv:2008.08118. https://arxiv.org/abs/2008.08118
Hybrid Ensemble Deep Learning Model for Advancing
Ischemic Brain Stroke Detection and Classification in
Clinical Application (J. Imaging 2024, by Qasrawi et
al.).
IEEE. (2023). A Review on Predicting Brain Stroke using
Machine Learning. IEEE Xplore Conference
Proceedings.
https://ieeexplore.ieee.org/document/10112236
Liu, J., Sun, Y., Ma, J., Tu, J., Deng, Y., He, P., Huang, H.,
Zhou, X., & Xu, S. (2021). Analysis and classification
of main risk factors causing stroke in Shanxi Province.
arXiv preprint arXiv:2106.00002.
Machine Learning Approach for Hemorrhagic
Transformation Prediction: Capturing Predictors'
Interaction (Frontiers in Neurology, Elsaid AF et al.,
2022).
Machine Learning–Based Model for Prediction of
Outcomes in Acute Stroke.
Nwosu, C. S., Dev, S., Bhardwaj, P., Veeravalli, B., & John,
D. (2019). Predicting Stroke from Electronic Health
Records. arXiv preprint arXiv:1904.11280.
Panachakel, J. T., & Jeena, R. S. (2020). Two Tier
Prediction of Stroke Using Artificial Neural Networks
and Support Vector Machines. arXiv preprint
arXiv:2003.08354.
Predicting Risk of Stroke from Lab Tests Using Machine
Learning Algorithms (JMIR Formative Research,
Alanazi EM et al., 2021).
Prediction of Brain Stroke Using Machine Learning and
Neural Networks (European Journal of Electrical
Engineering and Computer Science, S. Rahman et al.,
January 2023).
Sensors. (2024). Comprehensive Review: Machine and
Deep Learning in Brain Stroke Diagnosis. Sensors.
https://www.mdpi.com/1424-8220/24/13/4355
Sirsat, M. S., Fermé, E., & Câmara, J. (2020). Machine
learning for brain stroke: A review. Journal of Stroke
CerebroIntellex Leveraging Deep Learning Framework for Stroke Analysis
53

and Cerebrovascular Diseases, 29(10), 105162.
https://doi.org/10.1016/j.jstrokecerebrovasdis.2020.10
5162
Stroke Disease Detection and Prediction Using Robust
Learning Approaches Tahia Tazin, 1 Md Nur Alam,1
Nahian Nakiba Dola,1 Mohammad Sajibul Bari,1 Sami
Bourouis, 2 and Mohammad Monirujjaman Khan,
Hindawi Journal of Healthcare Engineering Volume
2021, Article ID 7633381, 12 pages
https://doi.org/10.1155/2021/763338
Stroke Lesion Detection and Analysis in MRI Images
Based on Deep Learning (Journal of Healthcare
Engineering, Zhang S et al., 2021).
Sundaram, S. M., Pavithra, K., & Poojasree, V. (2022).
Stroke Prediction Using Machine Learning. Internati-
onal Advanced Research Journal in Science, Enginee-
ring and Technology (IARJSET), 9(6), Article 9620.
https://doi.org/10.17148/IARJSET.2022.9620
Tegistu, biyadg sewnet. Brain stroke prediction model
using deep neural network (dnn). Diss. 2021.
Unveiling the Potential of Machine Learning Approaches
in Predicting the Emergence of Stroke at Its Onset: A
Predicting Framework (Scientific Reports, Sheela
Lavanya J. M. & Subbulakshmi P., 2024).
Wolfe, C.D.A. The impact of stroke. Br. Med. Bull. 2000,
56, 275–286.
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
54
