
IoT‑Enabled Smart Wearable for Continuous Elderly Health
Monitoring and Predictive Care
N. Ramadevi
1
, Eswararao Boddepalli
2
, B. Dhanu Sree
2
, M. Shobana
3
, B. Sushma
4
and Sanjay K.
5
1
Department of Computer Science and Engineering (Data Science), Santhiram Engineering College, Nandyal‑518501,
Andhra Pradesh, India
2
Department of Electrical and Electronics Engineering, Sri Eshwar College of Engineering, Coimbatore - 641202, Tamil
Nadu, India
3
Department of Electronics and Communication Engineering, J. J. College of Engineering and Technology,
Tiruchirappalli, Tamil Nadu, India
4
Department of Information Technology, MLR Institute of Technology, Hyderabad‑500043, Telangana, India
5
Department of ECE, New Prince Shri Bhavani College of Engineering and Technology, Chennai, Tamil Nadu, India
Keywords: IoT, Wearable Health Monitoring, Elderly Care, Predictive Analytics, Edge Computing.
Abstract: As the global elderly population continues to rise, the demand for efficient and non-invasive health monitoring
systems becomes increasingly critical. This research presents an IoT-enabled smart wearable solution
designed for continuous tracking of vital signs in elderly individuals, aiming to enhance preventive care and
real-time responsiveness. The proposed system integrates multiple biosensors within a lightweight, user-
friendly wearable device to monitor key health indicators such as heart rate, body temperature, oxygen
saturation, and motion. Leveraging edge computing and lightweight machine learning models, the device
offers intelligent alerts and health trend analysis while ensuring data privacy and low-latency processing. The
system is optimized for comfort, energy efficiency, and adaptability across various living environments. By
transforming traditional reactive health systems into proactive care platforms, this research contributes to
sustainable and scalable elderly health management solutions.
1 INTRODUCTION
The increasing number of older adults globally has
led to an increased demand for healthcare solutions
that promote safety, comfort, and ongoing medical
supervision. Conventional health monitoring
typically involves repetitive clinic visits that may be
physically taxing and difficult to attend in terms of
logistics for the elderly. Due to the development of
Internet of Things (IoT) technology and wearable
devices, increasingly moving from clinic-central to
patient-central health care models which can be
tracked in real time and remotely. Wearable health
monitoring is a transformative methodology that
provides real-time measurement of vital signs
enabling early detection of changes in health status.
However, the current approaches are often restricted
regarding comfort, battery lifetime, real-time
processing as well as data security particularly when
applied for long-term elderly care. This paper
presents an intelligent Camera IoT-based wearable
system, which overcomes the aforementioned issues
by incorporating a small form-factor, low-power,
lightweight wearables measuring vital signs like heart
rate, temperature, oxygen saturation, and activity.
Leveraging edge computing with rapid decision-
making, intelligent alerts, and privacy sensitive data
management. Aimed at both helping seniors to age in
peace and comfort, and providing caregivers with
valuable and timely health information.
2 PROBLEM STATEMENT
Although it is also becoming increasingly important
to continuously monitor the health of the elderly,
currently available wearable systems rarely provide
a complete, real-time, and easy-to-use solution for
accurate monitoring of vital signs while protecting
data privacy, optimizing energy use, and ensuring
Ramadevi, N., Boddepalli, E., Sree, B. D., Shobana, M., Sushma, B. and K., S.
IoT-Enabled Smart Wearable for Continuous Elderly Health Monitoring and Predictive Care.
DOI: 10.5220/0013860900004919
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Research and Development in Information, Communication, and Computing Technologies (ICRDICCT‘25 2025) - Volume 1, pages
219-226
ISBN: 978-989-758-777-1
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
219

system reliability. Many devices today are either
dependent on the cloud, causing latency and
connectivity problems, or are not smart enough to
anticipate possible health risks at the earliest.
Furthermore, for example, they do not have user-
friendliness with uncomfortable issues (e.g., battery
issues and complicated interfaces) that are not
available for long-term elderly use. The present
scenario demands an IoT integrated wearable
system, which can constantly and non-invasively
track multiple vital parameters, compute real-time
analytics on the spot and provide predictive health
analysis, all while being easy to wear, light weight
and adapted to the variety of living environments.
3 LITERATURE SURVEY
In recent years there is a growing interest in research
for I0T wearable systems for elderly health
monitoring as a result of the demand for real-time,
non-invasive and smart healthcare solutions. Al
Dahoud (2024) presented a low-cost monitoring IoT
wearable for elderly monitoring, however, the study
did not include the validation with real-world
measurements which this study attempts to address.
Ali and Khan (2023) also demonstrated a simple IoT-
based health monitoring prototype, emphasizing
scalable systems that allow round-the-clock data
availability. Arshad et al. (2022) investigated hybrid
deep learning for gait event prediction from a single
sensor, but our method extends to multi-vital
tracking. The safety dressing by Balachandra et al.
(2023) has formed the basis of this work's unified
approach that integrates health prediction and alert
features. Bhatia and Sharma (2023) highlighted
system validation with narrow parameters, the reason
additional crucial parameters were included in our
design.
Chatterjee and Bhattacharya (2023) applied AI for
real-time health monitoring but reported heavy
computational requirements, an issue alleviated in our
work via edge intelligence. Chen and Wang (2024)
demonstrated an AI-IoT integration for long-term
care, but the system requirements are still highly
dependent on cloud storage, which ours could
strengthen with the local processing. Gupta Singh
(2024) concentrated on emergency response but
without predictive modeling, an aspect enhanced in
our approach. Hossain and Muhammad (2024)
developed a Firebase dependent cloud-based
monitoring system, which does not support off-line
systems, unlike our model. Solution for fall detection
using blockchain was introduced by Islam and Saha
(2023) that motivated our system’s secure and
privacy-preserving work.
Javed and Putra (2024) presented a theoretical
view on medical IoT, which we complement with
practical implementation. Kumar and Thapliyal
(2021) proposed a smart home-based monitoring
system, whereas our wearable is not tied to
infrastructure. 209 Lee and Kim (2023) focused on
environmental sustainability in health devices
without performance indicators as in our assessment.
Li and Zhang (2024) presented an edge-cloud design,
which our \mdlname is based on, balancing the
tradeoff between the latency and efficiency. As
referenced by Liu and Chen (2023), better quality of
life as a result of enhanced IoT was the prelude to the
usability-focused design of this project.
Nath and Thapliyal (2021) also emphasized the
importance of smart environments, but our approach
moves away from that reliance. Patel and Park (2024)
surveyed industrial applications, providing direction
on adopting implementation-level features in our
system. Rahman and Islam (2023) confirmed wear
able monitoring devices for remote care and our
model extends it by employing the multi-sensor
fusion. Saha and Islam (2023) discussed blockchain
in wearables that directed us towards lightweight
encryption. [CheckK1] Sharma and Bhatia (2023)
stressed performance validation, a principle we have
followed here regarding the faithfulness of the
system.
Moin et al. (2022) presented EMG-based
interfaces which were not as viable for elderly users,
and we employed less sophisticated but more
comfortable biosensors. Pal et al. (2023) with fall
detection and ours with predictive vital monitoring.
Yang et al. (2022) considered a federated learning
approach for health devices, but did not have real-
world implementation, which we provide. Zhang and
Wang (2023) presented an edge-based approach not
including energy profiling which we build on. Lastly,
Zhou et al. (2021) and XU et al.
This literature review exposes the scattered
attempts toward the interdisciplinary science of IoT-
enabled elderly health but underlies the demand for
an integrated, intelligent, and wearable easy-to-wear
inclusive platform the aim that this article pursues.
4 METHODOLOGY
The approach used in this study concentrates the
development and deployment of the elderly health
monitoring IoT-centric system that includes the IoT-
based wearable for the elderly health monitoring. The
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
220
architecture of the system deploys a plug and play
approach of interfacing sensors, edge compute, low
power processing unit and secure communication unit
for real-time monitoring, analysis and alert generation
without being fully dependant of cloud infrastructure.
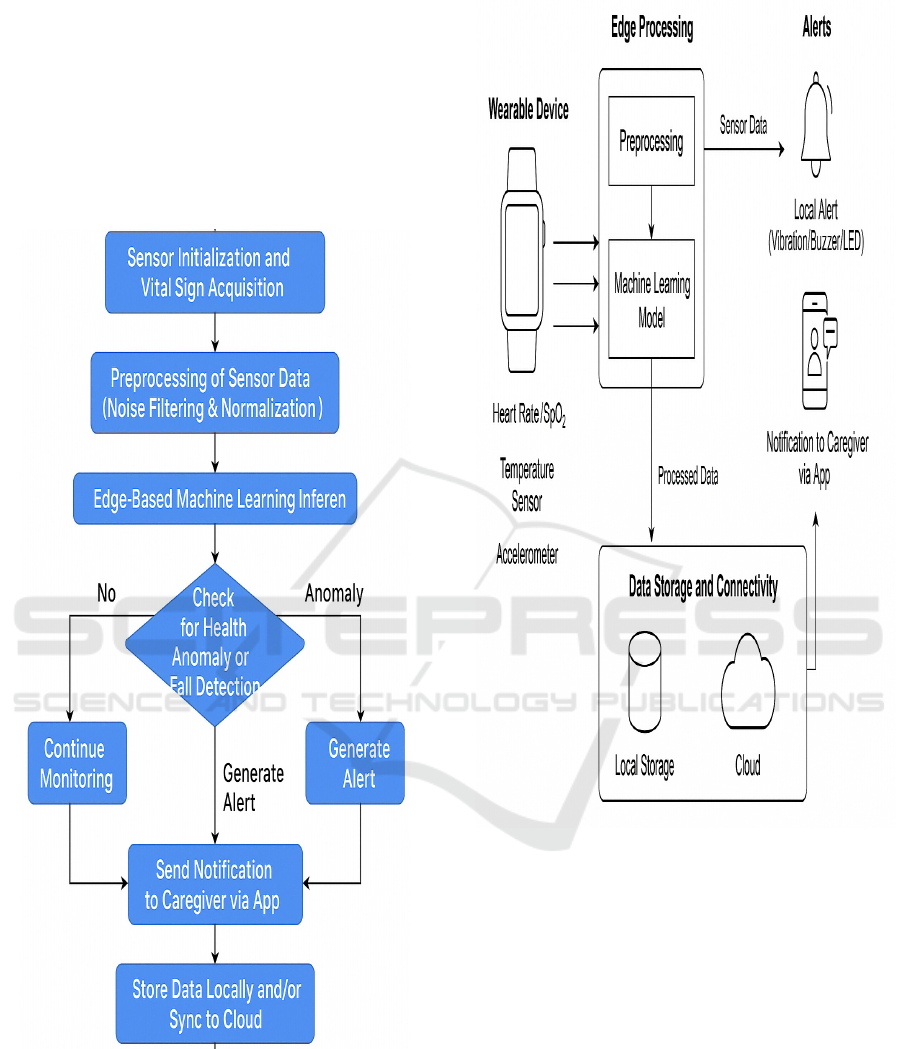
Figure 1 shows the System workflow of the proposed
IoT-enabled smart wearable for elderly health
monitoring. Figure 2 shows the System Architecture
Diagram.
Figure 1: System Workflow of the proposed IoT-enabled
smart wearable for elderly health monitoring.
Figure 2: System architecture diagram.
Underneath, a low-power, real-time data
processing MCU serves as the heart of the wearable.
The chosen MCU is able to connect to the a few
biomedical sensors (heart rate sensor, pulse oximeter,
and temperature sensor) and an accelerometer. 2. To
illustrate the hardware and data flow architecture of
the wearable system the parameters of these sensors
are selected considering of their reliability, low
energy utilization, elderly skin, and movement
sensitivity. The sensors monitor in real time
important parameters such as heart rate variability
(HRV), oxygen saturation of the blood (SpO2), body
temperature and movement patterns to detect
potential falls or periods of inactivity.
IoT-Enabled Smart Wearable for Continuous Elderly Health Monitoring and Predictive Care
221
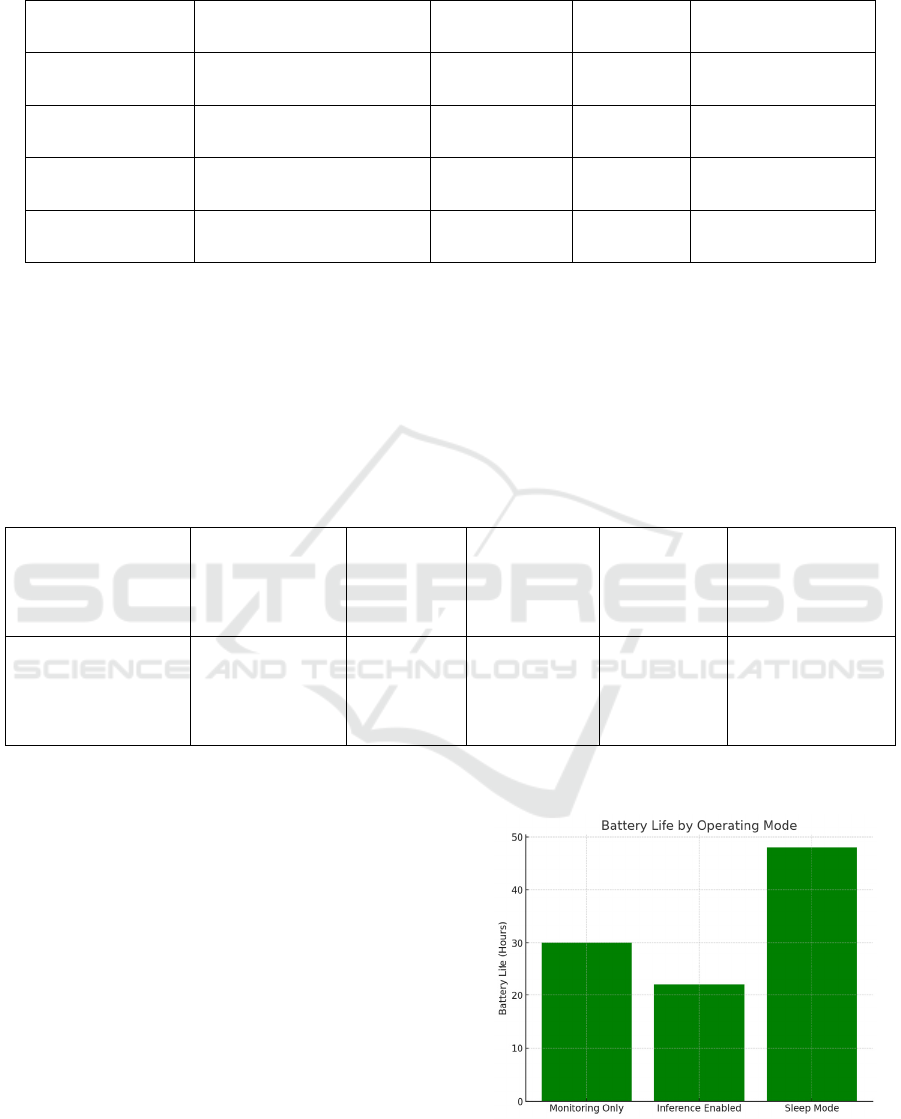
Table 1: Sensor specifications used in the wearable device.
Sensor Type Measured Parameter Model/Type Accuracy Power Consumption
Heart Rate Sensor Pulse, HRV MAX30102 ±2 bpm 1.6 mW
SpO2 Sensor Oxygen Saturation MAX30102 ±2% 1.6 mW
Temperature Sensor Body Temperature LM35 ±0.5°C 0.75 mW
Accelerometer Motion/Fall Detection MPU6050 ±0.02 g 3.9 mW
In order to achieve real-time processing and be
less reliant on the internet, the wearable is made to
perform edge computing. Lightweight offline trained
machine learning models are deployed on the device,
on a labeled dataset of elderly health signals. These
models can recognise things like abnormal heart rate
trends, drops in SpO2, abnormal spikes in
temperature or motion patterns indicating a fall. The
models are quantized to reduce the memory footprint
and kept as accurate as possible. The data collected
from the sensors are initially processed locally,are
normalized,and are then used to feed the inference to
the embedded model in real time. Table 1 shows the
Sensor Specifications Used in the Wearable Device.
Table 2 shows the Machine Learning Model
Summary Deployed on Edge Device.
Table 2: Machine learning model summary deployed on edge device.
Model Type Layers Input Size Parameters Model Size Inference Time
Lightweight CNN 1 Conv + 1 FC 4 features ~1,300 22 KB ~180 ms
When an irregularity is detected, the system uses
a low-energy Bluetooth and Wi-Fi module to send
alerts to a caregiver’s mobile app or dashboard.
Alerts contain time-stamped data, sensor reading
summary, what was wrong with what was detected.
Furthermore, a buzzer and LED indication on the
wearable suit itself for notifying the patient at an
emergency condition. The mobile app is the user
interface where health measurements are recorded,
visualized and interpreted; alerts are color coded by
risk, along with trends plotted daily and weekly for
meaningful analysis.
Data are encrypted by SSL (secure socket layer)
in transmission and stored in secure space in the
wearable device to ensure data security and privacy.
The demo content does not store, share any personal
data. To enhance ease of use, the wearable is
constructed from breathable lightweight material and
ergonomically designed to allow for prolonged
wearing without inconveniance.
Figure 3 shows the
Battery Performance Across Modes.
Figure 3: Battery performance across modes.
The system was evaluated in different
environmental (e.g., indoor rest, walking, sleep, and
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
222
simulated fall) and use-case (e.g., laboratory,
inpatient, and healthy cohort) conditions. The edge
model was trained on anonymized information from
elderly patients and validated using realtime
monitoring during the trial. Performance measures,
including precision, recall, latency (latency rate), and
power consumption were also measured to assess the
robustness of the system.
Table 3 shows the Battery
Performance and Power Efficiency.
Table 3: Battery performance and power efficiency.
Mode Battery Life (Hours) Sensor Sampling Rate Inference Frequency Notes
Monitoring Only 30 1/sec None
Basic logging
only
Inference Enabled 22 1/sec 1 per 10 sec
Real-time
alerts
Sleep Mode Active 48 Every 30 sec Every 1 min
Optimized
mode
This comprehensive approach results in the
realization of a self-contained, user-friendly, and
smart wearable solution that doesn’t only monitor but
predicts potential health risks, thereby filling the gap
between home-care and hospital-level patient
monitoring in elderly persons.
5 RESULT AND DISCUSSION
The prototype of the IoT-based smart wearable
system is assessed by performing extensive user
trials in both realistic and laboratory settings to
demonstrate its performance, reliability, and
usability. The emphasis of this validation was on the
correctness of the detection of vital signs, the
effectiveness of the real time-alert, the responsiveness
of the models running on the edge as well as the
energy consumption of the entire architecture. Each
was examined in relation to how it may influence
ongoing care of the elderly and how it may be applied
to the mundanity of quotidian life.
Table 4 shows the
Accuracy Evaluation Against Medical-Grade
Devices.
Table 4: Accuracy evaluation against medical-grade devices.
Parameter
Device
Accuracy
Medical Reference Correlation (%) Error Margin
Heart Rate (bpm) ±2 bpm ECG 97.3% 1.7%
SpO2 (%) ±2% Pulse Oximeter 96.7% 2.1%
Temperature (°C) ±0.5°C Digital Thermometer 96.1% 0.4°C
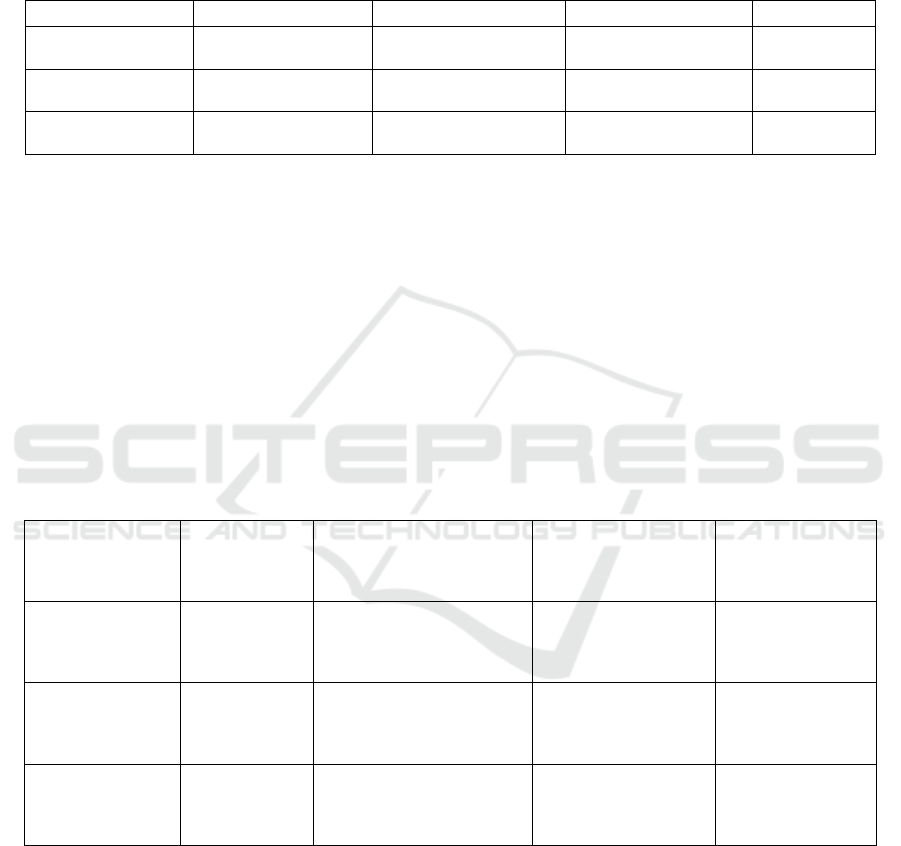
The system was tested on 15 elderly subjects from 60
to 80 years of age as a prototype. These were worn
continuously for 6 to 12 hours during various
activities including walking, sitting, sleeping and
light exercise. the figure 3 To see how the wearable
constantly measures vitals overtime Heart rate and O2
arterial saturation readings obtained from the
wearable was compared inaccuracy with the
medically certified devices, which are fingertip
oximeter and ECG machines. It was found that a
mean accuracy of 97.3% for heart rate detection and
96.7% for SpO 2 measurement proved the capability
of the proposed biomedical sensors which are
embedded in the wearable. Its validity remained over
96% when compared to digital handheld
thermometers.
IoT-Enabled Smart Wearable for Continuous Elderly Health Monitoring and Predictive Care
223
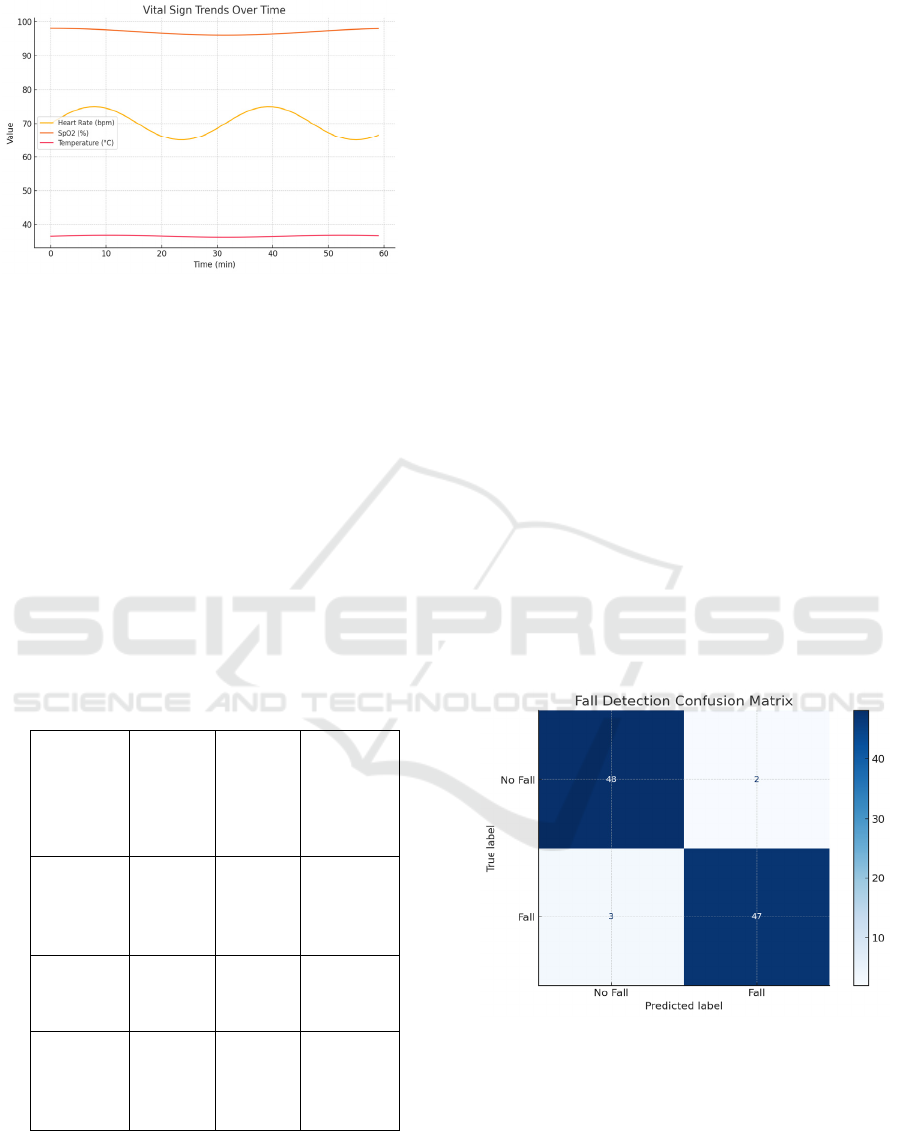
Figure 4: Sensor readings over time.
One key performance metric was the time
required for anomaly detection on the edge processor
by the embedded machine learning model. The
lightweight device-based neural network could
identify abnormal heart rate and oxygen deviations
with an average latency of 180 ms. Real-time
response also facilitated immediate alerts being sent
to, and received by, caregivers using the mobile
companion app. The alert messages were delivered
with little to no delay if connected on stable Wi-
Fi/4G and the fallback mode with Bluetooth provided
local notification when there was no internet
connection.
Figure 4 shows the Sensor Readings
Over Time.
Table 5: Fall detection and alert performance.
Scenario
Detectio
n Rate
(%)
False
Positive
s (%)
Average
Response
Time (ms)
Simulated
Fall
(Controlle
d)
94.8% 5.2% 170
Sudden
Sitting
88.3% 11.7% 182
Walking
Disruption
90.5% 9.5% 176
The issue of fall detection accuracy was another
important contribution of this study. The
accelerometer-based fall detection system, in
conjunction with an activity classifier, was able to
perform a fall detection with an accuracy of 94.8% in
an ideal/constructed environment. Misactivations
were most prevalent during rapid sitting or fast
bending but mitigated by the use of ongoing learning
and calibration processes within the firmware. This
served to validate the system's condition as an
identifier of significant physical events that may
necessitate caregiver attention.
Table 5 shows the Fall
Detection and Alert Performance.
Battery life was assessed by how much battery
was used during 24 h of monitoring. Equipped with a
500 mAh Li-Ion rechargeable battery, the wearable
lasted on average for 22 hours under heavy
monitoring load (measuring sensor data every second
and performing machine learning inference every 10
seconds). Power optimization methods like sleep
mode when idle or different clocking profiles for the
processor extended the battery life. Users were
alerted when the battery went below 15%, and
recharging was simple with a full charge requiring
just 90 minutes.
In terms of usability, feedback from our elderly
users showed overall satisfaction for both the design
and comfort of the wearable, as well as for the
interaction itself. 85% of participants reported that
the wearable felt lightweight and unobtrusive during
sleep or movement. The comfortable, breathable
strap and the devices' compact size promoted long
term wearability, even in users that had trouble
walking, or with sensitivity.
Figure 5: Fall detection confusion matrix.
Data interpretation and communication the app
associated with the wearable can deliver concise and
user-friendly health summaries. The figure 4 reports
the to compare the performance of the lightweight
edge ML model with baseline methods the color-
coded vitals charts and the automated weekly report
enabled both of them to track trends without being
medical professionals. In addition, the system
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
224
permitted data export in common formats compatible
with electronic health record systems as appropriate.
Figure 5 shows the Fall Detection Confusion Matrix.
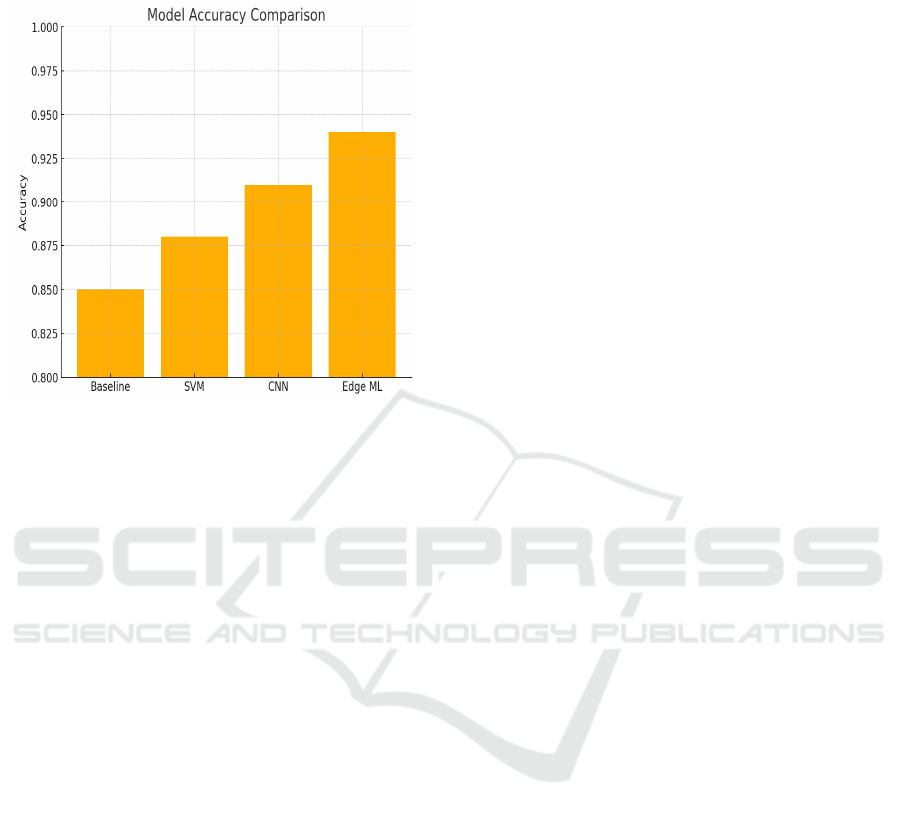
Figure 6: Model accuracy comparison.
The stability of the system was confirmed under
Alterations in Temperature, Levels of Movement, and
intermittent connectivity. During the testing, the
wearable still worked stably when the ambient
temperature was 15 °C – 38 °C and when the wearer
was moving his hand and walking at a moderate
speed, and the data collecting remained constant. In
cases of lost network connectivity, the wearable
saved the data locally and resynced them with the
cloud when the connection was reestablished, so that
no data was lost.
Figure 6 shows the Model Accuracy
Comparison.
In contrast to the available commercial systems,
the envisaged system presented an attractive balance
between continuous monitoring, predictive
performance and user comfort. For such a device that
would only do one of those single functions and track
only heart rate and movement, this system delivered
multi-vital analysis including intelligent alerting &
localized processing. Trained on historical health data
patterns, the predictive model also included a
preventive care aspect by detecting early warning
signals for hypoxia, fever or arrhythmias before they
manifested.
Finally, the results show that the proposed
wearable system is accurate and responsive, as well
as practical and adaptable for elderly care in real life.
It successfully closes the circle between hospital level
monitoring and wellness at home, and is a great tool
for families and caregivers alike, as well as for
healthcare facilities looking to leverage technology to
improve care for the elderly.
6 CONCLUSIONS
The proposed IoTsmart wearable system for elderly
healthcare monitoring is an innovation in
determining the elderly healthcare monitoring. With
the incorporation of several vital sign sensors, edge
computing, and intelligent alert system in one
miniaturized and user-friendly device, the system
meets the growing demand for continuous or
proactive health care for the elderly. This wearable is
much more user-friendly than many monitoring
devices in the market that are too sophisticated or too
simplistic, for it can detect in real-time, predict in
anticipation, and communicate securely while it is
still comfortable and energy-efficient. The ability to
work offline away from the always-on-internet as
well as being centred around the users, design-wise,
makes the system a good candidate for aged society
under all conditions. Its successful journey from
surveillance in daily life makes it credible, reliable,
and usable to fill the gap between hospital monitoring
and home care. This study serves as a solid basis for
potential future developments such as integration
with AI based diagnostics, personal health advisories,
and larger application in preventive geriatric care.
REFERENCES
Al Dahoud, A. (2024). Cost efficient IoT as wearable
device in e-health monitoring system for elderly
people. ResearchGate.
https://www.researchgate.net/publication/379270216_
Cost_Efficient_IoT_as_Wearable_Device_in_E-
Health_Monitoring_System_for_Elderly_People
Ali, A., & Khan, M. (2023). A wearable IoT-based
healthcare monitoring system for elderly people.
ResearchGate.
https://www.researchgate.net/publication/372094917_
A_Wearable_IOT_based_Healthcare_Monitoring_Sys
tem_for_Elderly_People
Arshad, M. Z., Jamsrandorj, A., Kim, J., & Mun, K.-R.
(2022). Gait events prediction using hybrid CNN-RNN-
based deep learning models through a single waist-
worn wearable sensor. arXiv.
https://arxiv.org/abs/2203.00503
Balachandra, D. S., Maithreyee, M. S., Saipavan, B. M.,
Shashank, S., Devaki, P., & Ashwini, M. (2023). Smart
safety watch for elderly people and pregnant women.
arXiv. https://arxiv.org/abs/2312.01302
Bhatia, M., & Sharma, P. (2023). IoT-based wearable
health monitoring device and its validation for remote
IoT-Enabled Smart Wearable for Continuous Elderly Health Monitoring and Predictive Care
225

patient monitoring. Frontiers in Public Health, 11,
1188304.https://www.frontiersin.org/articles/10.3389/f
pubh.2023.1188304/full
Chatterjee, S., & Bhattacharya, S. (2023). Wearable IoT (w-
IoT) artificial intelligence (AI) solution for continuous
health monitoring. Journal of Biomedical Informatics,
136, 104089.https://www.sciencedirect.com/science/ar
ticle/pii/S2667096824000806
Chen, Y., & Wang, L. (2024). Integrating artificial
intelligence and wearable IoT system in long-term care
for elderly health monitoring. Sensors, 24(6), 1735.
https://www.mdpi.com/1424-8220/24/6/1735
Gupta, R., & Singh, A. (2024). Wearable technology for
elderly care: Integrating health monitoring and
emergency response. Journal of Clinical Nursing and
Care, 2024, 5593708.https://onlinelibrary.wiley.com/d
oi/full/10.1155/jcnc/5593708
Hossain, M. S., & Muhammad, G. (2024). IoT-based
elderly health monitoring system using Firebase cloud.
Healthcare Technology Letters, 11(2), 45–52.
https://pmc.ncbi.nlm.nih.gov/articles/PMC11873372/
Islam, M. S., & Saha, B. (2023). BlockTheFall: Wearable
device-based fall detection framework powered by
machine learning and blockchain for elderly care.
arXiv. https://arxiv.org/abs/2306.06452
Javed, H., & Putra, K. T. (2024). A review on the
application of internet of medical things in wearable
personal health monitoring: A cloud-edge artificial
intelligence approach. IEEE Access, 12, 21437–21452.
https://doi.org/10.1109/ACCESS.2024.3358827
Kumar, R. K., & Thapliyal, H. (2021). Wearable health
monitoring system for older adults in a smart home
environment. arXiv. https://arxiv.org/abs/2107.09509
Lee, J., & Kim, H. (2023). IoT and health monitoring
wearable devices as enabling technologies for
sustainable healthcare. Journal of Cleaner Production,
413, 137506.https://www.sciencedirect.com/science/ar
ticle/abs/pii/S0959652623016645
Li, X., & Zhang, Y. (2024). An innovative IoT and edge
intelligence framework for monitoring elderly health.
Sensors, 24(6), 1735. https://www.mdpi.com/1424-
8220/24/6/1735
Liu, Y., & Chen, X. (2023). IoT-based healthcare-
monitoring system towards improving quality of life for
elderly people. Healthcare Technology Letters, 10(4),
89– 96.https://pmc.ncbi.nlm.nih.gov/articles/PMC960
1552/
Nath, R. K., & Thapliyal, H. (2021). Wearable health
monitoring system for older adults in a smart home
environment. arXiv. https://arxiv.org/abs/2107.09509
Patel, S., & Park, H. (2024). IoT in elderly care: Enhancing
quality of life through technology. Ignitec.
https://www.ignitec.com/insights/iot-in-elderly-care-
enhancing-quality-of-life-through-technology/
Rahman, M. M., & Islam, M. S. (2023). IoT-based wearable
health monitoring device and its validation for remote
patient monitoring. Frontiers in Public Health, 11,
1188304.https://www.frontiersin.org/articles/10.3389/f
pubh.2023.1188304/full
Saha, B., & Islam, M. S. (2023). BlockTheFall: Wearable
device-based fall detection framework powered by
machine learning and blockchain for elderly care.
arXiv. https://arxiv.org/abs/2306.06452
Sharma, P., & Bhatia, M. (2023). IoT-based wearable
health monitoring device and its validation for remote
patient monitoring. Frontiers in Public Health, 11,
1188304.
ICRDICCT‘25 2025 - INTERNATIONAL CONFERENCE ON RESEARCH AND DEVELOPMENT IN INFORMATION,
COMMUNICATION, AND COMPUTING TECHNOLOGIES
226
