
Changes in the Number of Smokers by State Before and after the US
Epidemic
Yiyang Tian
1,*
and Ruoyu Ying
2
1
Department of Letters and Science, University of California, Davis, U.S.A.
2
Department of Computing, University of Technology Sydney, Sydney, Australia
*
Keywords: COVID-19 Pandemic, Tobacco Use Trends, Descriptive Statistical Analysis, Regression Analysis.
Abstract: Against the backdrop of the global COVID-19 pandemic, significant changes have occurred in people's
lifestyles and behavioral patterns, including variations in tobacco use. This study employs descriptive
statistical analysis and regression analysis to explore trends in tobacco use among different age groups in the
United States before and during the pandemic, as well as the influencing factors. The research covers
descriptive statistics on tobacco use rates among individuals aged 12 - 17, 18 - 25, and 26+ for the periods
2018 - 2019 and 2021 - 2022, comparing changes and disparities across states and age groups. Regression
models are constructed to analyze the impact of time dummy variables, state, and age on tobacco use rates.
The findings indicate a decline in tobacco use rates across all age groups during the pandemic, with varying
degrees of reduction and distinct influencing factors among different age groups. This study provides evidence
for understanding the pandemic's impact on tobacco use behavior and offers insights for formulating more
effective tobacco control policies.
1 INTRODUCTION
In the field of global public health, tobacco use has
long been a critical issue of concern. Smoking is
closely linked to the development of severe diseases
such as lung cancer and cardiovascular conditions,
posing a persistent threat to population health.
According to the World Health Organization,
smoking causes over 8 million deaths annually
worldwide, including approximately 1.2 million non-
smokers who die from secondhand smoke exposure.
With increasing public health awareness and the
implementation of tobacco control policies globally,
smoking rates have shown a gradual decline over the
past few decades. However, individual smoking
behavior remains dynamically influenced by complex
social and environmental factors.
The COVID-19 pandemic, which emerged in
early 2020 as one of the most severe global public
health crises of the century, has profoundly disrupted
societal production and daily life. During the
pandemic, measures such as social distancing,
economic shutdowns, fear of infection, and abrupt
changes in daily routines created a unique high-stress
environment. In this context, smoking - a complex
habit with both physiological dependence and
psychological regulation functions - inevitably
experiences multifaceted influences. From a
psychological perspective, pandemic-induced anxiety
and depression may have driven some individuals to
increase smoking frequency as a coping mechanism.
A 2020 survey by the American Psychological
Association found that 40% of respondents reported
increased smoking during the early pandemic, with
the 18 - 34 age group showing a 52% increase.
However, from a behavioral restriction standpoint,
measures such as the closure of public spaces,
tightened tobacco retail controls, and reduced social
smoking opportunities due to remote work
objectively constrained smoking behavior. This dual
dynamic of "stress-driven increase" and
"environmentally constrained decrease" led to
significant individual variability in smoking behavior
during the pandemic.
The United States, as one of the hardest-hit
countries, exhibits notable regional heterogeneity
among states in terms of pandemic response
strategies, economic structures, demographic
distributions, and tobacco control policy strictness.
For instance, New York implemented strict
lockdowns and closed all indoor public spaces as
early as March 2020, while Texas lifted restrictions
Tian, Y. and Ying, R.
Changes in the Number of Smokers by State Before and after the US Epidemic.
DOI: 10.5220/0013860800004719
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 2nd International Conference on E-commerce and Modern Logistics (ICEML 2025), pages 779-785
ISBN: 978-989-758-775-7
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
779

relatively early in 2021. Such differences resulted in
varying levels of pandemic pressure, economic
disruption, and behavioral constraints across states,
leading to complex and diverse patterns in smoking
behavior changes. Some industrial states saw 15% -
20 % fluctuations in smoking rates due to soaring
unemployment and the closure of social venues,
while states with a high concentration of tech
industries, such as California, experienced smaller
changes (around 5%) owing to widespread remote
work and a younger demographic. Given this
complexity, existing research lacks a systematic
explanatory framework, necessitating in-depth
comparative analysis.
This study addresses the dual mechanisms of
pandemic impact on smoking behavior and the
significant socioeconomic and policy differences
across U.S. states. It aims to comprehensively analyze
dynamic changes in smoking rates across states from
2018 - 2019 (pre-pandemic) to 2021 - 2022 (during
and post-pandemic). The research focuses on three
core dimensions: (1) using panel data models to
precisely depict smoking rate trends across states by
age, gender, and education level; (2) employing
spatial econometric methods to identify regional
clustering effects in smoking behavior changes; and
(3) constructing structural equation models to explore
the interaction mechanisms among pandemic control
intensity, economic fluctuations, demographic
characteristics, and pre-existing tobacco control
policies. The study seeks to answer: Which states
experienced significant changes in smoking rates
during the pandemic? How do these changes
quantitatively relate to state-level policy variables
and socioeconomic indicators? What lasting effects
did temporary environmental changes during the
pandemic have on long-term smoking behavior
patterns?
Theoretical contributions of this study include
expanding traditional smoking behavior research,
which primarily focuses on individual psychological
factors, by incorporating macro-level public health
events into the analytical framework. Through multi-
level data integration, the study reveals the complex
pathways through which major social crises influence
addictive behaviors. The proposed theory enriches the
situational factors theory in health behavior studies,
offering new analytical dimensions for understanding
individual decision-making during emergencies.
Practically, the findings will inform state-specific
tobacco control policies in the U.S. For states with
significant increases in smoking rates (e.g., Rust Belt
industrial states), targeted interventions such as
psychological support for the unemployed and
community-based cessation programs are
recommended. For states with notable declines (e.g.,
West Coast regions), successful strategies like
"remote work smoking control" and "health
communication for younger demographics" can be
replicated elsewhere. Importantly, the regional
difference analysis framework developed in this
study can serve as a methodological reference for
other countries assessing smoking behavior changes
during public health crises and formulating tailored
intervention strategies, thereby contributing to multi-
objective collaborative governance systems.
2 LITERATURE REVIEW
2.1 Domestic Literature Review
Research on smoking behavior in China has evolved
in stages, reflecting shifting public health priorities.
Early studies focused on establishing the link between
smoking and diseases, laying a scientific foundation
for understanding smoking hazards. Liu Xiaoyan's
(2018) 10-year cohort study in Xuanwei City
provided large-scale evidence that smokers' lung
cancer mortality was 3.2 times higher than non-
smokers, solidifying smoking as a primary risk factor.
Xiao Junling's (2020) cross-sectional survey of
10,000+ residents in Jiayuguan City further
demonstrated that smokers faced 47% higher
respiratory disease risks and 32% higher
cardiovascular risks, establishing dose-response
relationships between smoking and chronic diseases.
Post-2010, studies began examining
sociodemographic disparities. Kang Guorong et al.
(2015) revealed urban-rural divides in smoking rates
(28.7% rural vs. 21.3% urban) and health literacy
gaps (22 percentage points), incorporating
socioeconomic status into smoking behavior models.
Li Shanpeng and Qi Fei (2018) highlighted policy
effects, showing that smoking bans reduced daily
cigarette consumption from 16.2 to 13.5 in Qingdao.
Li Zhongyou et al. (2018) tracked gender disparities
over 25 years in Guangxi, with male smoking rates
declining from 58.3% (1991) to 52.7% (2015) while
female rates remained low (3.2% - 4.1%).
Recent studies emphasize targeted interventions.
Lei Chunping (2012) identified peer influence
(coefficient 0.63) and family environment (0.48) as
key factors for youth smoking. Wang Zhao et al.
(2011) classified college smokers into social (37.2%)
and stress-relief (28.9%) types, informing tailored
campus programs. Zheng Bao (2011) found policy
perception gaps: smokers' support for public smoking
ICEML 2025 - International Conference on E-commerce and Modern Logistics
780
bans (68%) lagged behind non-smokers' (89%), but
72% desired cessation services, guiding local policy
adjustments.
Domestically, research has progressed from
biological foundations (disease links) to sociological
explanations (group difference) to public health
applications (precision strategies). While establishing
an "individual-behavior-policy" framework, gaps
remain in studying pandemic impacts and emerging
products like e-cigarettes.
2.2 International Literature Review
Global research employs multidisciplinary
approaches. Van Gucht et al. (2010) used behavioral
diaries to show how social contexts and moods affect
smoking patterns. Stang et al. (2000) quantified
smoking's contribution to COPD. Noonan et al.
(2015) mapped woodsmoke exposure risks using
GIS, while Hall (2004) analyzed smoke hazards in
fire disasters.
Haenszel et al. (1956) pioneered U.S. smoking
pattern analyses. Shopland et al. (1996) identified
higher smoking rates in Southern/Midwestern states,
linking regional culture to behavior. Jamal et al.
(2015) tracked 2005 - 2014 trends, showing faster
declines among men and variations by
race/education.
2.3 Literature Critique
Existing studies lack dynamic cross-regional
comparisons, especially regarding pandemic impacts.
International work underanalyzes state-level
differences during COVID-19, neglecting policy-
economic-psychological interactions.
Methodologically, traditional surveys dominate, with
limited causal inference. This study addresses these
gaps by integrating multi-source data and causal
methods to examine U.S. state-level smoking
changes, offering theoretical and practical
advancements for tobacco control.
3 METHODOLOGY
This study combines descriptive statistics and
regression analysis to investigate pre-/post-pandemic
tobacco use trends among U.S. age groups.
Descriptive statistics- compare 2018 - 2019 and
2021 - 2022 tobacco use rates across ages (12 - 17, 18
- 25, 26+) and states, calculating changes to identify
pandemic effects.
Regression analysis -models tobacco use rates
(dependent variable) against time dummies (0=pre-
pandemic, 1=pandemic), controlling for state and
age. Coefficient significance tests determine
pandemic impacts, while R2 evaluates model fit. This
reveals underlying mechanisms behind trend shifts.
4 RESULTS
4.1 Descriptive Statistical Analyses
This section explores changes in tobacco use trends
before and after the epidemic with the help of
descriptive statistical analyses of data on tobacco use
rates by age from 2018 to 2019 and from 2021 to
2022.
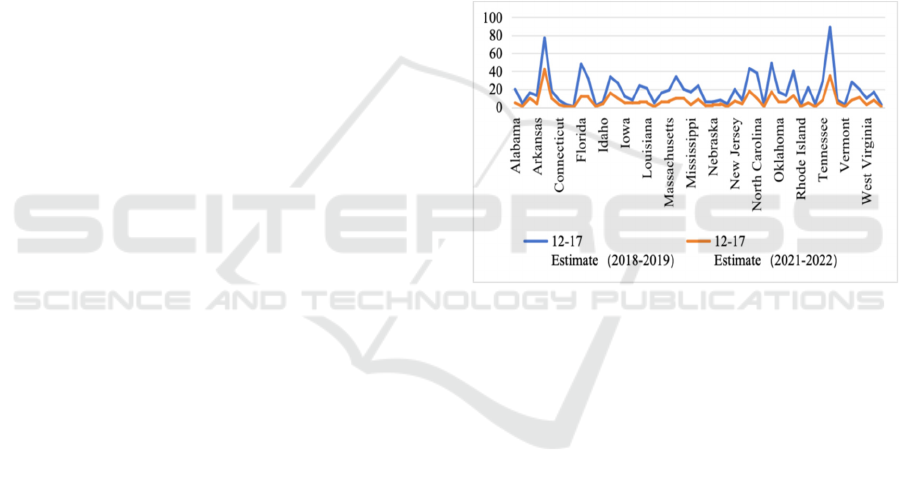
Figure 1: Changes in tobacco use among 12-17 year olds
before and after the epidemic
Figure 1 shows that in the 12- to 17-year-old age
group, the overall trend in the data shows a general
decline in tobacco use in this age group during the
epidemic, with estimates of tobacco use in Alabama
ranging from 20 in 2018-2019 to 5 in 2021-2022, a
decline of 15, and in California from 77 to 42, a
decline of 35. California, on the other hand, dropped
from 77 to 42, a decline of 35. Such a downward trend
was demonstrated in several states, suggesting that
tobacco use in this age group was controlled to some
extent during the epidemic. In terms of regional
distribution, there was a relatively large difference in
tobacco use rates between states, with several states
like Alaska having a relatively low estimated value of
tobacco use before the epidemic of only 4, while
California had a relatively high rate of 77. This
difference persisted during the epidemic, reflecting
the different foundations of youth tobacco prevention
and control, as well as their effectiveness, in different
regions.
Changes in the Number of Smokers by State Before and after the US Epidemic
781

Figure 2: Changes in tobacco use among 18-25 year 25-
year-olds before and after the epidemic
As can be seen in Figure 2, in the 18 to 25 age
group, tobacco use rates in this age group showed the
same decline during the epidemic, for example, in
Alabama, where the rate of tobacco use decreased by
96 from 155 in 2018-2019 to 59 in 2021-2022, and in
Texas, where the rate decreased from 756 to 299, a
decline of 457, with different There is some variation
in usage rates between states. Before the epidemic,
Florida had a tobacco use rate of 399 compared to 23
in Hawaii, and during the epidemic, it dropped to 164
in Florida and 17 in Hawaii, and this difference
between states has a key impact on the overall
tobacco use trend, with this age group experiencing
limited socialisation and lifestyle changes during the
epidemic, which may be a key factor contributing to
the decline in tobacco use rates.
Figure 3 shows that in the 26 and over age group,
there was a decline in tobacco use during the
epidemic for people aged 26 and over, for example,
Alabama dropped from 1012 to 762, a decrease of
250, and New York dropped from 2469 to 2183, a
decrease of 286, although the overall trend was
downward, although the differences in use between
different states were more striking, with states like
Texas had a high estimate of tobacco use of 4,015
before the epidemic, while Vermont had only 97, and
during the epidemic, Texas dropped to 3,293, and
Vermont dropped to 86, a difference that reflects the
impact of different states' social environments, levels
of economic development, and tobacco control
policies on the tobacco use behaviors of the adult
population.
Comparison of the three age groups shows that
tobacco use declined in all age groups during the
epidemic,
but the magnitude of the decline and the
Figure 3: Changes in tobacco use among people aged 26+
before and after the epidemic
trend of change varied, with a more pronounced
decline in the 12- to 17-year-old age group, which
may be related to the strengthening of health
promotion and education in schools during the
epidemic, and the restriction of the scope of activities
of students, etc., and a larger decline in the 18- to 25-
year-old age group, where changes in lifestyle and
social patterns had a greater impact on their tobacco
use behaviour. The decline in the 18-25 age group is
also relatively large, with changes in the pace of life
and socialisation patterns having a greater impact on
their tobacco use behaviour. 26 and older age groups,
although also declining, are experiencing a smaller
decline due to the relative stability of this group's
lifestyles. Economically developed regions may see
more pronounced declines in tobacco use because of
strict prevention and control measures and high levels
of health awareness, while states with higher levels of
tobacco industry dependence have seen relatively
smaller declines.
4.2 Regression Results
4.2.1 12-17 Year
Table 1: Tobacco use among 12-17 year olds
Regression Statistics Value
Multiple R 0.8417
R Square 0.7085
Adjusted R Square 0.6646
Standard Error 7.0690
Observations 56
ICEML 2025 - International Conference on E-commerce and Modern Logistics
782
Table 2: Estimated regression coefficients and test results for tobacco use among 12-17 year olds
Coefficients
Standard
Error
t Stat P-value
Lower 95
per cent
Upper 95
per cent
Lower 95.0
per cent
Upper 95.0
per cent
Intercept 3.7394 6.3194 1.0284 16.1349 31.1270 16.1349 31.1270
After 4.4763 -3.6222 0.0007 -25.2310 -7.1976 -25.2310 -7.1976
Treated 0.2400 -0.1377 0.8906 -0.5152 0.4491 -0.5152 0.4491
Interaction Term
(After*Treated)
0.2864 0.0208 0.9835 -0.5667 0.5786 -0.5667 0.5786
The results of the analyses in Table 1 and Table 2
show that, after controlling for the effects of the
different states, the coefficient of the time dummy
variable "After" in the 12 to 17 year olds shows a
specific characteristic, with a coefficient of -16.2143,
which means that in 2021 to 2022, the rate of tobacco
use in the 12 to 17 year olds declined in comparison
to the rate in 2018 to 2019. 2018 to 2019 is
decreasing, as can be seen from the p-value of 0.0007;
the coefficient is statistically significant, indicating
that the epidemic has had a relatively very prominent
effect on the use of tobacco in this age group. During
the epidemic, this age group's exposure to tobacco
may have been reduced due to the restriction of the
scope of activities of young people and the
strengthening of health education in schools, which
led to a decrease in the rate of tobacco use. Moreover,
Treated and Interaction Term are not significant in
Table 1 and Table 2, suggesting that "state" as a
control variable may have a weaker effect on tobacco
use, and the main effect is due to the time dummy
variable "After". After".
4.2.2 18-25 Years
Table 3: Tobacco use among 18-25 year olds
Regression Statistics Value
Multiple R 0.9733
R Square 0.9474
Adjusted R Square 0.9347
Standard Error 23.9077
Observations 56
Table 4: Estimated regression coefficients and test results for tobacco use among 18-25 year olds
Coefficients
Coefficient
Values
Standard
Error
t Stat P-value
Lower 95
per cent
Upper 95
per cent
Lower 95.0
per cent
Upper 95.0
per cent
Intercept 148.8768 10.8210 13.6836 2.1829 127.0232 170.7304 127.0232 170.7303
After -133.8214 12.9327 -10.3475 3.4105 -159.9722 -107.6706 -159.9723 -107.6705
Treated 0.369643 0.61817 0.5980 0.5523 -0.8662 1.6055 -0.8662 1.6055
Interaction Term
(After*Treated)
-0.5982 0.7380 -0.8106 0.4218 -2.0792 0.8828 -2.0792 0.8828
As can be seen from Table 3 and Table 4, the
coefficient of the time dummy variable "After" is -
133.8214 for the age group of 18 to 25 years old,
which indicates that during the epidemic period, the
tobacco use rate of this age group decreased
compared with that before the epidemic. In addition,
the p-value of this coefficient is 3.4105, which is
much smaller than the common level of 0.05, and this
change is statistically significant, which confirms that
the epidemic has had a strong impact on the tobacco
use behaviour of people aged 17 to 25. During the
epidemic, there was a significant change in the way
18-25 year olds socialised, with an increase in online
activities and a decrease in offline gatherings, which
may have led to a corresponding decrease in tobacco
use behaviours that were often seen in social
situations, resulting in a significant decrease in
tobacco use.
Changes in the Number of Smokers by State Before and after the US Epidemic
783
4.2.3 26 Years and Over
Table 5: Tobacco use among people aged 26 and over
Regression Statistics Value
Multiple R 0.9733
R Square 0.9474
Adjusted R Square 0.9347
Standard Error 23.9077
Observations 56
Table 6: Estimated regression coefficients and test results for tobacco use among 26-year-olds
Coefficients
Coefficient
Values
Standard
Error
t Stat P-value
Lower 95
per cent
Upper 95
per cent
Lower 95.0
per cent
Upper 95.0
per cent
Intercept 148.8769 10.8800 13.6836 2.1828 127.0232 170.7303 127.0232 170.7303
After -133.8214 12.9327 -10.3476 3.4105 -159.972 -107.6705 -159.972 -107.6706
Treated 0.3696 0.6181 0.5980 0.5523 -0.8662 1.6055 -0.8662 1.6055
Interaction Term
(After*Treated)
-0.5982 0.7380 -0.8106 0.4218 -2.0792 0.8827 -2.0792 0.8828
The analyses in Table 5 and Table 6 show that the
coefficient of the time dummy variable "After" is -
133.8214 for the age group of 26 and above, which
also shows a decrease in tobacco use during the
epidemic, and its p-value is 3.4105, which means that
the epidemic has also had a certain impact on this age
group. The coefficient of "After" is -133.8214, which
also shows a decrease in tobacco use during the
epidemic, with a p-value of 3.4105. During the
epidemic, people in this age group may have reduced
their tobacco consumption due to many factors such
as changes in their work patterns and the
implementation of controls in public places, which
led to a decrease in the rate of tobacco use. Although
the social and life patterns of people aged 26 and
above are relatively more stable, the changes in the
overall social environment brought about by the
epidemic still have an undeniable impact on their
tobacco use behaviour. Although the social and
lifestyle patterns of people aged 26 and over are more
stable, the changes in the social environment brought
about by the epidemic have had a significant impact
on their tobacco use behaviour.
Regression analyses clearly show that the
epidemic had a strong impact on tobacco use trends
in different age groups, and that tobacco use declined
in all age groups during the epidemic. Although the
magnitude of the decline and the factors influencing
it varied by age group, it is undeniable that the
epidemic, as a powerful external variable, reshaped
people's lives and consumption patterns, and
ultimately had a negligible effect on tobacco use
behaviour. use behaviours.
5 CONCLUSION
This study focuses on the changes in tobacco use
trends among different age groups before and after
the epidemic, using regression analyses to deeply
analyse the impact of time variables and factors such
as different states and ages on tobacco use, and the
results show that the epidemic had an impact on the
use of tobacco among people aged 12-17, 17-25, and
26 and older, and that tobacco use among all age
groups showed a declining trend during the epidemic.
The results show that the epidemic had an impact on
tobacco use among 12 to 17, 17 to 25, and 26-year-
olds and older, and that tobacco use among all age
groups decreased during the epidemic.
This result gives insights into many aspects. From
the perspective of public health, the preventive and
control measures implemented during the epidemic,
such as social restriction and control of public places,
have to a certain extent limited the access to and use
of tobacco, resulting in a reduction in the rate of
tobacco use among people of all ages, which provides
new ideas and references for the subsequent
formulation of tobacco control policies, such as
making reference to the effective control model
during the epidemic, strengthening the regulation of
youth smoking behaviour, and restricting smoking
ICEML 2025 - International Conference on E-commerce and Modern Logistics
784

behaviour in public places. This provides new ideas
and references for the subsequent formulation of
tobacco control policies, for example, by referring to
the control model that worked well during the
epidemic, strengthening the regulation of youth
smoking behaviour, and restricting smoking
behaviour in public places.
However, it is also important to note the
limitations of this study in that the model, although it
takes into account factors such as time and state, may
have an impact on tobacco use as well as other
variables that were not included, such as changes in
economic conditions, shifts in cultural attitudes, etc.,
and that the data from the study only covered two
specific periods, making it difficult to fully reflect
changes in tobacco use trends over time.
Future research can broaden the scope of data,
incorporate more influencing factors, and construct a
more complete model to gain a more comprehensive
understanding of the changing patterns of tobacco use
behaviours, provide a solid theoretical basis and data
support for the development of more effective
tobacco control strategies, and promote public health.
AUTHORS CONTRIBUTION
All the authors contributed equally and their names
were listed in alphabetical order.
REFERENCES
Fan, Z., Xiong, H., & Wang, Z., 2011. Survey and research
on smoking among university students in Kunming,
Yunnan Province. Social Sciences (New Theory),
26(03), 154-155.
Haenszel, W., Miller, H. P., & Shimkin, M. B., 1956.
Tobacco smoking patterns in the United States. US
Government Printing Office.
Hall, J. R., 2004. How many people are exposed to sublethal
fire smoke? Fire Technology, 40, 101-116.
He, X., 2021. Relationship between passive smoking and
respiratory symptoms among rural women in typical
counties and districts in the Huaihe River Basin and
analysis of influencing factors. Lanzhou University.
Jamal, A., Homa, D. M., O'Connor, E., et al., 2015. Current
cigarette smoking among adults-United States, 2005-
2014. MMWR Morb Mortal Wkly Rep, 64(44), 1233-
1240.
Kang, G., Lu, P., Qian, G., et al., 2015. Study on tobacco
prevalence among urban and rural residents aged 15-69
years in Gansu Province. China Health Education,
31(10), 919-924.
Lei, C., 2012. Study on the current situation of smoking
behaviour and influencing factors of students in a
medical college in Chongqing. Third Military Medical
University.
Li, S., & Qi, F., 2014. 2014 Qingdao Adult Tobacco
Epidemic Survey Report. People's Health Press, 169.
Li, Z., Tang, Z., Fang, Z., et al., 2018. Analysis of smoking
status and trend of change among residents aged 18
years and above in 6 cities (counties) of Guangxi from
1991 to 2015. China Health Education, 34(03), 195-
199.
Liu, X., 2018. Estimation of prevalence characteristics of
lung cancer deaths among smokers and non-smokers
aged 30-69 years in six townships of Xuanwei City,
2014-2016. Peking Union Medical College.
Noonan, C. W., Ward, T. J., & Semmens, E. O., 2015.
Estimating the number of vulnerable people in the
United States exposed to residential wood smoke.
Environmental Health Perspectives, 123(2), A30-A30.
Shopland, D. R., Hartman, A. M., Gibson, J. T., et al., 1996.
Cigarette smoking among US adults by state and
region: estimates from the current population survey.
JNCI: Journal of the National Cancer Institute, 88(23),
1748-1758.
Stang, P., Lydick, E., Silberman, C., et al., 2000. The
prevalence of COPD: using smoking rates to estimate
disease frequency in the general population. Chest,
117(5), 354S-359S.
Van Gucht, D., Van den Bergh, O., Beckers, T., et al., 2010.
Smoking behaviour in context: where and when do
people smoke? Journal of behaviour therapy and
experimental psychiatry, 41(2), 172-177.
Xiao, J., 2020. Survey and analysis of community residents'
hygiene and health status in Jiayuguan City. Lanzhou
University.
Xu, L., Liu, T., Li, L., et al., 2014. Study on the prevalence
of tobacco among adults in Guizhou Province. China
Chronic Disease Prevention and Control, 22(06), 675-
678. doi:10.16386/j.cjpccd.issn.1004-
6194.2014.06.008.
Zheng, B., 2011. A survey of smoking attitudes and related
behaviours among key populations for tobacco control
in Henan Province. Zhengzhou University.
Changes in the Number of Smokers by State Before and after the US Epidemic
785
