
The Research on the Key Pathogenic Factors of Depression
Shaozong Liang
a
Oriental College of International Trade and Foreign Languages, Haikou University of Economics,
Haikou, Hainan, 571127, China
Keywords: Depression, Depression Factors, Depression Causes, Random Forest.
Abstract: Depression is a significant public health concern, posing critical risks such as suicide. This study investigates
the key pathogenic factors of depression using clinical data sourced from the Kaggle website, comprising
413768 instances with 15 variables, including socioeconomic, lifestyle, and medical factors. The Random
Forest algorithm is employed to analyze the correlation between these variables and chronic medical
conditions (depression). The model identified income as the most critical predictor of depression, with an
importance score of 0.668, followed by the number of children and history of substance abuse. Descriptive
analysis further revealed that low-income groups, individuals with lower education levels, and non-smokers
exhibited higher rates of chronic medical conditions. These findings underscore the pivotal role of
socioeconomic and lifestyle factors in the prevalence of depression, offering valuable insights for targeted
healthcare interventions and preventive strategies. While the current model demonstrates moderate predictive
accuracy, future research should focus on expanding the dataset, incorporating additional clinical variables,
and comparing results across multiple machine learning models to enhance predictive performance and
generalizability. The approach holds promise for advancing the understanding of depression and improving
mental health outcomes globally.
1 INTRODUCTION
Depression has emerged as a public health concern in
contemporary society, affecting millions of
individuals worldwide. As a chronic and recurrent
disease, depression is one of the most critical risk
factors for suicide. Nearly one billion people
worldwide are affected by mental health issues, and
the diagnosis rate of depression among teenagers
surges (Nguyen, T.-L. & Lee, 2025). The suicide rate
among elderly patients with depression accounts for
27.2% of global suicide deaths (Szücs, Cohen &
Reynolds, 2025). The incidence of depression is
increasing in recent years. Epidemiological studies
show that among the 25 major causes of the total
burden of disease, depression ranks 13th in the
disability adjusted life year and 2nd in the disability
adjusted life year (Ao et al., 2024). A number of
depression patient can be treated with drugs, but there
are still 15%~33% of patients who are ineffective
after drug treatments (Fei, Cheng & Shen, 2024).
Depression is a common mental disorder in clinic at
a
https://orcid.org/0009-0004-4901-1584
present. The main clinical manifestations of
depression are depression, slow thinking, weakened
will activity and decreased interest. The latest
research shows that the prevalence of depression is
about 27.6%, and the number of patients with
depression in the world has reached 350 million, and
is increasing year by year. The recurrence rate of
depression is high, and people are prone to self injury
or suicidal behavior, which has brought serious
damage to individuals, families and society (Ma,
2024). In the United States, the lifetime prevalence of
major depression is 21% in women and 11% -13% in
men. It is the main cause of suicide. Among the top
10 deaths in the United States, it is reported that
nearly 50000 people commit suicide every year. The
morbidity and mortality associated with depression
make it the number one cause of disability in the
world and cause a huge economic burden on society
in terms of productivity loss (Kuerban, 2024).
Depression is a genetic disease, the probability of
depression in relatives of patients with depression,
First-Degree Relatives, is higher than that of the
Liang, S.
The Research on the Key Pathogenic Factors of Depression.
DOI: 10.5220/0013834000004708
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 2nd International Conference on Innovations in Applied Mathematics, Physics, and Astronomy (IAMPA 2025), pages 605-609
ISBN: 978-989-758-774-0
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
605

general population. Wang’s et al. (2024) study also
shows that the incidence of depression in families
with depression, alcohol dependence or antisocial
personality is significantly higher than that in the
control population, indicating that the interaction
between gene and environment play a significant role
in the pathogenesis of depression. People with high
frequency of interaction with patients with depression
have higher recognition of biogenetic interpretation
and childhood adversity interpretation (Zhang, 2024).
The onset of depression lasts for more than 2 weeks
each time, even for 1 year or several years, and
depression is easy to relapse (Chen et al., 2024). The
survey shows that the incidence of sleep disorders in
patients with depression is 55.00%, indicating that
more than half of patients with depression are
accompanied by sleep disorders, and once
accompanied by insomnia, the incidence and severity
of the remaining physical symptoms of patients
would also increase (Li, Shi & Zhang, 2023).
Depression patients may have suicidal ideation of
different intensities, and even suicidal behavior, the
suicide rate of depression patients is about 10%~15%.
Projections indicate that by 2030, depression will
account for the highest proportion of disability-
adjusted life years (DALYs) lost globally (Zhong,
2024). Therefore, it is of significance to study the key
pathogenic factors of depression for the prevention of
depression.
The study aims to leverage clinical data to
investigate depression, with all patient data sourced
from the Kaggle website. Using the Random Forest
algorithm to explore the correlation between various
risk factors and chronic medical conditions, focusing
on depression. By analyzing key determinants of
depression, the research seeks to provide insights for
targeted interventions and preventive strategies,
ultimately contributing to improved mental health
outcomes.
2 METHODS
2.1 Data Source
The data utilized in this paper for predicting
depression were obtained from clinical cases on the
Kaggle website (Sasaki, 2024). The dataset provides
the basis for correlations between factors and
depression. It contains 413768 sample cases and 15
variables, including age, marital status, number of
children, smoking status, physical activity level,
employment status, alcohol consumption, dietary
habits, sleep patterns, education level, income,
history of mental illness, history of substance abuse,
family history of depression, and chronic medical
conditions, determined through medical diagnostic
records.
92% of the 413768 instances were randomly
selected as samples with no missing values. Using the
Random Forest algorithm, which employs all
available clinical features, to judge the samples as
having chronic medical conditions or not having
chronic medical conditions.
2.2 Method Introduction
The method used in this study is the Random Forest
algorithm. The Random Forest model operates on
ensemble learning principles, constructing multiple
decision trees through dual randomization: bootstrap
sampling and random feature subsets during node
splitting. Predictions are aggregated via majority
voting, reducing overfitting risks. Its advantages are
tolerance for missing values and interpretable feature
importance rankings. The model excels in handling
heterogeneous variables without manual
preprocessing, while maintaining computational
efficiency through parallelized tree training.
Chronic medical conditions are classified as target
variables and the other 14 factors are divided into
feature columns, which explores the correlation
between various variables in the table and chronic
medical conditions (depression), calculates the
importance of the characteristics of each variable, and
predicts whether a person has depression.
3 RESULTS
3.1 Descriptive Analysis
Extract 3 variables: education level, income, and
smoking status. Figures 1, 2 and 3 ordinates represent
the number of abscissas.
Figure 1 , whose abscissas represent 5 education
levels from high school to phD, shows whether the
variable Education level has the number of Chronic
Medical Conditions. The sample with Bachelor’s
degree and high school education had the highest
number of chronic medical conditions.
IAMPA 2025 - The International Conference on Innovations in Applied Mathematics, Physics, and Astronomy
606
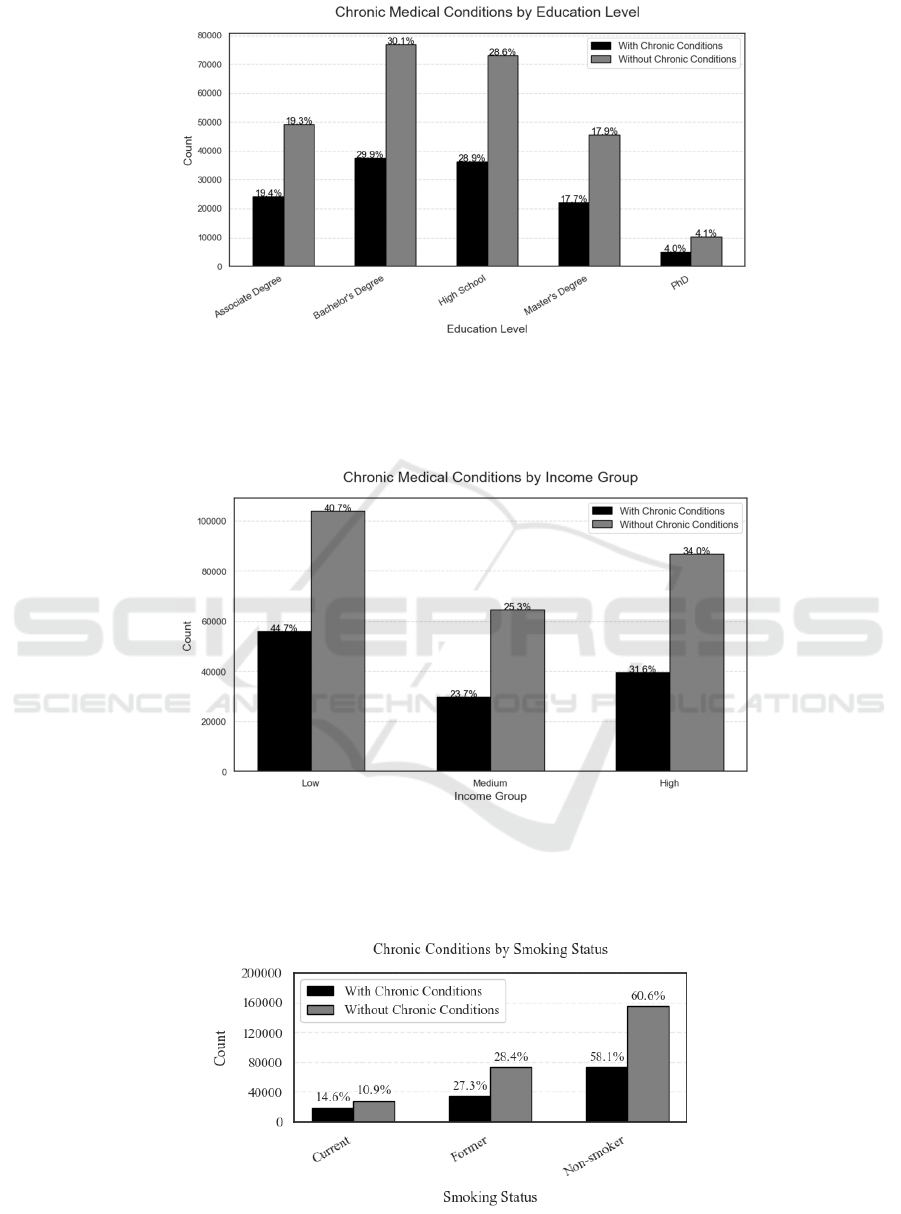
Figure 1: Education levels has the number of Chronic Medical Conditions (Photo/Picture credit: Original).
The Figure 2, whose abscissas represent 3 income
levels from low to high, shows whether the variable
Income has the number of chronic medical conditions,
with the low-income group having the highest
number of chronic medical conditions.
Figure 2: Income groups has the number of chronic medical conditions (Photo/Picture credit: Original).
Figure 3, whose abscissas represent 3 smoking
conditions, shows whether the variable Smoking
Status has the number of chronic medical conditions,
with the non-smoking group having the highest
number of chronic medical conditions.
Figure 3: Smoking Status has the number of chronic medical conditions (Photo/Picture credit: Original).
The Research on the Key Pathogenic Factors of Depression
607
3.2 Random Forest Results
Table 1: Model Evaluation
Precisio
n
Recall
F1-
score
Suppor
t
0
67.36% 74.35% 70.68% 70664
1
33.04% 25.99% 29.10% 34401
accurac
y
58.52% 105065
macro
avg
50.20% 50.17% 49.89% 105065
weighte
d avg
56.12% 58.52% 57.07% 105065
0 = No chronic medical conditions, 1 = Having
chronic medical conditions. For 0, precision is
67.36%, recall is 74.35%, and the F1-score is 70.68%.
For 1, precision is 33.04%, recall is 25.99%, and the
F1-score is 29.10%. The macro-average precision is
50.20%, recall is 50.17%, and F1-score is 49.89%.
The weighted-average precision is 56.12%, recall is
58.52%, and F1-score is 57.07%. The accuracy of the
model is 58.52% , indicating that the model is reliable.
Train the model using a Random Forest Classifier
and calculate the importance score for each feature.
Table 2 shows all feature importance scores in
descending order.
Table 2: Importance Score
Feature Importance
Income 0.668
Number of Children 0.071
History of Substance Abuse (Yes) 0.027
Family History of Depression (Yes) 0.025
History of Mental Illness (Yes) 0.025
Alcohol Consumption (Moderate) 0.016
Sleep Patterns (Poor) 0.016
Alcohol Consumption (Low) 0.015
Sleep Patterns (Good) 0.013
Dietary Habits (Moderate) 0.013
Education Level (High School) 0.013
Marital Status (Married) 0.012
Physical Activity Level (Moderate) 0.012
Education Level (Bachelor's Degree) 0.011
Education Level (Master's Degree) 0.009
Marital Status (Widowed) 0.009
Physical Activity Level (Sedentary) 0.008
Dietary Habits (Unhealthy) 0.008
Smoking Status (Non-smoker) 0.007
Smoking Status (Former) 0.007
Employment Status (Unemployed) 0.006
Marital Status (Single) 0.005
Education Level (PhD) 0.005
The importance score of Income is 0.668, the
highest. The most important feature for predicting
depression is: Income.
4 DISCUSSION
The Random Forest model demonstrated strengths in
this study, including its capability to handle high-
dimensional data with mixed feature types while
maintaining robustness against missing values and
outliers (Breiman, 2001). The disadvantage is limited
model interpretability, struggling to quantify the
specific impact direction of individual features on
prediction outcomes. It is sensitive to class imbalance,
it may affect the prediction accuracy of minority
classes if the target variable "chronic medical
conditions" is severely imbalanced (Zhang, Liu, &
Wang, 2020).
Introducing a weighted iterative mechanism to
further enhance classification performance in
XGBoost, or incorporating external datasets (such as
public health databases) to expand sample diversity
and avoid sampling bias, can optimize the model
(Zhang et al., 2020; Zhang, Chen, & Li, 2021). The
limitations of this study's design are reliance on self-
reported questionnaires and samples drawn from a
single database, which affect the model's
generalizability (Wong et al., 2022).
In the future, electronic health records, wearable
device data, and genomic information can be
integrated to develop a multidimensional predictive
model (Topol, 2019).
5 CONCLUSION
This study demonstrates the reliability of predicting
whether an individual has depression based on a
comprehensive set of factors, including marital status,
number of children, smoking status, physical activity
level, employment status, alcohol consumption,
dietary habits, sleep patterns, education level, income,
history of mental illness, history of substance abuse,
family history of depression, and chronic medical
conditions. Using the Random Forest algorithm,
income is identified as the most important predictor
of depression, with the importance score of 0.668,
followed by the number of children and history of
substance abuse. Descriptive analysis further
revealed that low-income groups, individuals with
lower education levels, and non-smokers exhibited
higher rates of chronic medical conditions. These
findings emphasize the critical role of socioeconomic
IAMPA 2025 - The International Conference on Innovations in Applied Mathematics, Physics, and Astronomy
608

and lifestyle factors in the development of depression,
providing valuable insights for targeted healthcare
interventions and preventive strategies. Significant
differences in the distribution between the new data
and the training data (such as the lifestyle habits of
different populations in different regions) will
decreases the performance of the model. Not
considering key variables in medical diagnosis,
relying solely on questionnaire data limits clinical
practicality. While the current model achieves
moderate predictive accuracy, future research should
focus on expanding the dataset, incorporating
additional clinical variables, and comparing results
across multiple machine learning models to improve
predictive performance and generalizability. The
approach holds promise for advancing our
understanding of depression.
REFERENCES
Ao, Y., Guo, Y. Q., Guo, R. J., et al., 2024. Analysis of
traditional Chinese medicine syndrome elements,
accompanying symptoms, and their correlations in
1063 patients with depression. Global Traditional
Chinese Medicine, 17(11), 2250–2256.
Breiman, L., 2001. Random forests. In Machine Learning,
45, 5-32.
Chen, J., Li, X., Zhang, T., et al., 2024. The impact of early
trauma experiences in patients with depression. In
Psychology Monthly, 19(06), 19-21. DOI:
10.19738/j.cnki.psy.2024.06.006
Fei, Y. X., Cheng, S. F., & Shen, Y. P., 2024. Changes and
influencing factors of cognitive function in patients
with depression during modified electroconvulsive
therapy. Zhejiang Clinical Medicine, 26(6), 837–839.
Kuerban, K., 2024. Differences in clinical characteristics
and influencing factors between melancholic and non-
melancholic depression patients [Master ’ s thesis,
Xinjiang Medical University].
CNKI.
https://kns.cnki.net/kcms2/article/abstract?v=5ykJdPm
CibI82sUyBIyincZu8P6NPZVvct7NlmKGXWGBJlC
eKs7s4IPBKHloWPyhGCj5caFHr-b-
alfMbqFbAVgImDtI719jlC8FVJGWlXVBs3bXdHcx
xQRhtBHx0ITB1uGG8xKoQsPxSM_8s9Cles3DNwv
wsEUutFDxCQAN2BrYgn_H9xZPBw==&uniplatfor
m=NZKPT&language=CHS
Li, S., Shi, L., Zhang, W., 2023. Sleep disorder incidence
and its influencing factors in patients with depression.
In World Journal of Sleep Medicine, 10(06), 1302-1305.
Ma, B. X., 2024. Analysis of related factors of anhedonia in
patients with depression and research on traditional
Chinese medicine prescriptions and
syndromes [Doctoral dissertation, Tianjin University of
Traditional Chinese Medicine].
Nguyen, T.-L., & Lee, J.-Y., 2025. Kindness as a public
health action. Communications Medicine, 5(4), 112–
125.
Sasaki, T. 2024. What causes depression? Causal inferenc.
Kaggle.
https://www.kaggle.com/code/sasakitetsuya/what-
causes-depression-causal-inference
Szücs, A., Cohen, R., & Reynolds, C. F., 2025.
Investigating direct and moderating effects of social
connectedness and perceived social support on suicidal
ideation in depressed aging adults: A prospective study.
In Biological Psychiatry Global Open Science, 4(2),
102–115.
Topol, E. J., 2019. High-performance medicine: the
convergence of human and artificial intelligence. In
Nature Medicine, 25(1), 44-56.
Wang, X., Xiao, C., Li, L. L., et al., 2024. Prevalence and
influencing factors of depression in Heilongjiang
Province. Journal of Qiqihar Medical College, 45(11),
1060–1064.
Wong, K. C., Luo, X., & Zhang, Q., 2022. Cross-cultural
validation of machine learning models in healthcare: A
systematic review. In The Lancet Digital Health, 4,
e158–e167.
Zhang, J., 2024. The mechanism and intervention of causal
explanations affecting the stigma of
depression [Doctoral dissertation, Southwest
University]. https://doi.org/10.27684/d.cnki.gxndx.202
4.002253
Zhang, L., Chen, H., & Li, M., 2021. Enhancing model
generalizability through multi-source health data
integration. In Journal of Biomedical Informatics, 123,
104567.
Zhang, Y., Liu, Y., & Wang, J., 2020. Boosting ensemble
learning for imbalanced data classification: A hybrid
approach. In IEEE Transactions on Knowledge and
Data Engineering, 33, 4567–4581.
Zhong, W. S., 2024. Analysis of living conditions of
college students with depression. Health Education and
Health Promotion, 19(4), 430 – 433.
https://doi.org/10.16117/j.cnki.31-1974/r.202404430
The Research on the Key Pathogenic Factors of Depression
609
