
Enhancing Data Quality and Semantic Annotation by Combining
Medical Ontology and Machine Learning Techniques
Zina Nakhla
1,*
and Manel Sliti
2,†
1
Université de Tunis, Institut Supérieur de Gestion, BESTMOD Laboratory, Tunis, Tunisia
2
Université de Manouba, Institut Supérieur des Arts et Multimedia de Manouba, Manouba, Tunisia
Keywords: Interoperability, Ehr, Ontology, Machine Learning, NLP.
Abstract: Effective management of electronic health records (EHR) is a major challenge in the modern healthcare
sector. Despite technological advances, the interoperability of medical data remains a crucial challenge. This
complex problem is manifested by the diversity of data formats, the presence of multiple standards and the
heterogeneity of Information Technology (IT) systems used in health- care establishments. However, the
diversity of IT systems and the complexity of medical terminologies often make data interoperability and
semantic annotation in the healthcare domain difficult. To address this challenge, our study proposes an
innovative approach to standardize the representation of medical concepts, to automate the detection of
medical abbreviations and to improve the contextual understanding of medical terms. We developed an
ontological model to harmonize the representation of medical data, thus facilitating their exchange and
integration between different health systems. In parallel, we used advanced machine learning techniques for
automatic detection of medical abbreviations in medical texts, and applied Natural Language Processing to
improve contextual understanding of medical terms. The results of our study demonstrate the effectiveness of
our approach in solving challenges related to medical data management. By combining different advanced
techniques, our approach helps overcome barriers to medical data interoperability and paves the way for better
healthcare system integration and improved patient care.
1 INTRODUCTION
An Electronic Health Record (EHR) is a digital
version of a patient’s paper chart (Sachdeva and
Bhalla, 2022). EHR systems facilitate the collection,
storage, and sharing of patient information in a
structured manner to enhance healthcare delivery and
clinical decision-making. They are designed to
provide real-time, centralized, and secure medical
information accessible to authorized users. While an
EHR contains a patient’s medical history, diagnoses,
prescriptions, and other clinical data, its role goes
beyond mere data archiving. It allows access to
evidence-based tools that help healthcare
professionals optimize their medical decisions
(Fennelly and Moroney, 2024).
One of the key features of an EHR is that health
information can be created and managed by
authorized providers in a digital format capable of
*
Corresponding author
†
Contributing author
being shared with other providers across more than
one health care organization. EHRs are built to share
information with other health care providers and
organizations such as laboratories, specialists,
medical imaging facilities, pharmacies, emergency
facilities, and workplace clinics so they contain
information from all clinicians involved in a patient’s
care. However, sharing the information needed is a
very complicated problem.
Doctors and specialists are suffering from
collecting distributed data spread over different
locations, and lack of the interoperability among all
the healthcare information systems. Also, the domain
of healthcare produces a huge quantity of data from
various disparate sources. The single patient’s data
can be dispersed over diverse EHRs with various
representation ways (Begoyan, 2007).
Data in EHRs could be presented in many
different types of formats: structured data as
140
Nakhla, Z. and Sliti, M.
Enhancing Data Quality and Semantic Annotation by Combining Medical Ontology and Machine Learning Techniques.
DOI: 10.5220/0013750200004000
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Knowledge Discovery, Knowledge Engineering and Knowledge Management (IC3K 2025) - Volume 2: KEOD and KMIS, pages
140-150
ISBN: 978-989-758-769-6; ISSN: 2184-3228
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.

(database) (Schloeffel et al, 2006) unstructured data
such as (documents, images,...) (Kiourtis et al, 2017),
and semi-structured data (XML files) (Mylka et al,
2012).
The EHR interoperability problem refers to the
ability of different systems to seamlessly exchange,
interpret, and utilize patient data across various
healthcare providers and settings. This challenge
arises from differences in data formats, adopted
standards, and proprietary systems, leading to
inefficiencies, medical errors, and fragmented care.
Interoperability can be categorized into three levels,
firstly Technical interoperability, which ensures the
physical connection between systems and data
transfer. Secondly Syntactic interoperability, which
enables data exchange through standardized formats
(HL7, XML), (Sartipi and Dehmoobad ,2008).
Thirdly Semantic interoperability, which ensures a
uniform understanding of exchanged data by using
standardized medical terminologies. Semantic
interoperability is essential for improving clinical
decision-making, enhancing care coordination, and
ensuring that all healthcare professionals have access
to consistent and reliable medical information. To
address these challenges, several standards and
terminologies have been developed. Among the
standards enabling structured clinical content
exchange are Health Level Seven (HL7) Digital
Imaging and Communications in Medicine
Structured Reporting (DICOM SR), (Begoyan, 2007)
, ISO EN 13606 (Costa et al, 2011) , openEHR
[(Kalra, 2006), (Schloeffel et al, 2006),( Da Costa,
2019),( Roehrs et al, 2018), (Begoyan, 2007)], GEHR
(Celesti et al, 2016). Nonetheless,semantic
interoperability cannot be achieved without the
adoption of standardized medical terminologies, such
as the Systematized Nomenclature of Medicine
Terms (SNOMED CT), which is the most
comprehensive medical terminology system used
worldwide. SNOMED CT enables precise encoding
of clinical information, facilitating medical document
annotation, clinical decision support, and EHR
interoperability.
Despite continuous efforts, limitations persist,
particularly concerning the variety of medical data
formats, variability of collection protocols,
confidentiality concerns, and the absence of uniform
standards for semantic tagging. These challenges
hinder the automatic understanding of medical data,
slowing down interoperability advancements. To
overcome these limitations, this study proposes an
innovative approach that integrates ontologies,
machine learning, and Natural Language Processing
(NLP). This combination allows for standardizing
medical concept representation, automatically
detecting medical abbreviations, and improving the
contextual understanding of medical terms.
Unlike previous approaches, our method
introduces a novel integration of structured ontology-
based representations with advanced machine
learning and NLP models, enhancing data
standardization, medical entity recognition, and
abbreviation expansion. This paper details each phase
of our proposed approach, demonstrating how it helps
overcome barriers to medical data interoperability
and facilitates seamless integration within healthcare
systems, ultimately improving patient care.
This paper presents an integrated approach to
solving challenges related to medical data
interoperability by combining ontology, machine
learning and NLP. We discuss in detail the different
phases of our approach by combining different
advanced techniques, our approach helps overcome
barriers to medical data interoperability and paves the
way for better healthcare system integration and
improved patient care. The rest of this paper is
structured as follows. Section 2 presents the related
work and previous studies. Section 3 describes the
used dataset. The proposed architecture with its
internal phases are described in Section 4. Section 5
contains the results of experiments, and we discuss
our evaluation of the proposed solution. Section 6
presents a comparison study. Finally, the conclusion
and future work.
2 RELATED WORK
One of the most consistent themes across the
literature is the potential of EHR to revolutionize
multiple aspects of healthcare. Many of these papers
describe how an EHR system can improve how
patients are diagnosed, treated and improve
healthcare (Gunter et al , 2005). McClanahan
describes how quick access to patient information
through a universal EHR system can save the lives of
thousands of emergency room patients each year by
reducing medical errors (McClanahan, 2008).
Santos et al. explained the importance of EHR due
to its ability to integrate various user interfaces and
programs. While their findings are promising, they do
not fully address the significant infrastructural and
financial challenges of integrating diverse systems at
a national or international level. Many of the
proposed solutions are theoretical and lack real-world
validation, which raises questions about their
scalability and long-term feasibility (Santos et al,
2010).
Enhancing Data Quality and Semantic Annotation by Combining Medical Ontology and Machine Learning Techniques
141

Berges et al. explore the use of ontologies in
improving interoperability in heterogeneous EHR
systems. First, they used a reasonable ontology that
EHR-related concepts focus on meanings and
perspectives. Second, they tracked modules that
enable the acquisition of rich ontological descriptions
of EHR data guided by constraint models of medical
knowledge frameworks. Third, it considers necessary
mapping maxims between the concepts that mappings
update. While their model demonstrates the potential
for more structured and accurate data representation,
it overlooks the practical challenges of implementing
such models across diverse healthcare environments.
The author’s approach to aligning heterogeneous
EHR descriptions is promising but requires further
exploration into how these mappings can be
dynamically updated in real-time across various
clinical settings (Berges et al, 2011).
Ferrer et al. represented and integrated patient
data from many different heterogeneous data sources
and encouraged the integration of patient data into a
rule-based Clinical Decision Support System
(CDSS). Their work represents a significant step in
bridging standards such as ISO/CEN 13606 and HL7
through OpenEHR approach. They proposed a
Personal Health Records (PHR) combining
OpenEHR and HL7 supported by a service-oriented
information exchange system (González-Ferrer et al,
2012).
Liyanage et al proposed a method for improving
semantic interoperability in healthcare by using
ontologies. They present an ontology toolkit that
facilitates the development of ontologies for chronic
disease management using heterogeneous health data.
Nevertheless this approach is useful but limited by its
focus on specific diseases and may not be easily
generalized to other domains (Liyanage et al, 2015).
Also, Kiourtis et al. proposed a generic ontology-
based semantic architecture to solve EHR
interopability problem. This architecture used an
ontology language to transform heterogeneous
medical data into a generic schema, called CHL that
can be used to represent health data in a way that is
consistent and understandable to machines. The CHL
also makes it possible to merge different medical
ontologies with similar relationships. The authors
also pointed out that this method is not lossless, as
data transformation can lead to loss of information.
This is a significant limitation, as the loss of data
could compromise patient care and treatment
decisions (Kiourtis et al, 2017).
Futhermore, Hajjamy et al. developed a
semiautomatic approach to integrate classical data
sources into an ontological database. Their method
involves transforming data sources into ontologies
using measures of syntactic, semantic, and structural
similarity, to generate a global ontology. The authors
suggested that their approach could be enhanced by
incorporating other information retrieval techniques
and big data methods to handle larger ontologies.
Although their method is promising, its reliance on
traditional data fusion methods may hinder its ability
to handle the large and complex datasets common in
modern healthcare (El Hajjamy et al,2018).
In 2019, Li Chen et al. developed an ontology to
represent knowledge and relationships in the field of
diabetes and used this ontology to build a reasoning
model for medical decision making. Their method
involved collecting data from various sources,
defining Semantic Web Rule Language (SWRL)
rules to define the reasoning rules of the ontology,
and implementing the SWRL rules in an inference
engine to create a help system for decision called
Ontology-based Medical Diagnostic and Treatment
Platform (OMDP). OMDP used OWL ontology and
SWRL rules to analyse patient’s symptoms, make
diagnosis and recommend treatment by integrating
different types of diabetes knowledge. Despite this,
the limited scope of their model focused only on
diabetes raises concerns about its broader
applicability across other medical conditions.
Furthermore, while the integration of different
knowledge sources is valuable, the lack of real-time
data integration limits its practical utility (Li Chen et
al, 2019).
In 2020, Sreenivasan and chacko. proposed an
approach to map heterogeneous EHR data to
ontologies, to create a semantically annotated
knowledge base that can be queried. The approach
involved semantically annotating the data using an
ontology, building a new of knowledge and the use of
a semantic inference module to infer knowledge from
data. The proof of concept showed that health data
mapped into a relational database using ontologies
can be used for inference and for rapid decision
making by healthcare professionals. The proof of
concept is promising but remains at a pilot stage, and
further validation is required before it can be widely
adopted in clinical practice (Sreenivasan and Chacko,
2020).
In 2022, Adel et al. proposed an ontological model
to integrate patient health data from heterogeneous
data sources at a centralized point to improve the
quality of care. The authors unified five different
healthcare data formats into an unified ontology. The
results showed that the proposed model made it
possible to integrate and collect all patient data from
heterogeneous data sources, improving the quality of
KEOD 2025 - 17th International Conference on Knowledge Engineering and Ontology Development
142

care and reducing medical errors. However, there are
limits to the model, including its specificity to a
particular area, the use of limited test data, the need
for close collaboration between health professionals
and computer scientists, and the need for more in-
depth validation on a larger population in real clinical
environments ( Adel et al, 2022).
Overall, most of the existing approaches faced
limitations, especially the variety of medical data
formats, the variability of collection protocols, the
problem of confidentiality of medical data, and the
lack of uniform standards for semantic tagging, which
have hindered the automatic understanding of data.
These challenges have hindered the implementation
of comprehensive solutions and highlighted the need
for innovative approaches to overcome these
limitations.
3 DATASET DESCRIPTION
This section details the data sources and the
construction of the patient file, outlining the process
used to gather and structure the datasets necessary for
our study. The Web offers access to an enormous
quantity of documents, in several forms (texts,
images, videos, sounds) and in different languages.
Most of these documents are freely available, easy to
access, and in electronic format. To identify relevant
resources, we used the Google search engine with
targeted queries such as “medical dataset Excel”,
“EHR data sample xls”, and “clinical records
spreadsheet». From the search results, we first
considered the most popular web pages (the top-
ranked pages in the results list). These pages were
then filtered according to qualitative criteria:
Representativeness of the medical domain,
Audience targeted by the site (general public or
healthcare professional),
Author of the page (health professional or not),
Language used (easily understandable or
specialized terminology).
Based on these criteria, we selected web pages that
hosted structured datasets and, more specifically,
Excel files. While Excel is not a standard format for
EHR representation, its tabular structure makes it an
accessible, modifiable, and easily shareable medium
for organizing medical information. These files
provided a practical way to compile representative
terms used by healthcare mediators while maintaining
data consistency.
Thus, the dataset consists of Excel files retrieved
from public health websites and open research
portals, each containing structured medical records in
English and French.
The Excel model is organized into five main classes:
1. Patient ID: an anonymized identifier assigned
to each patient.
2. Healthcare Professional: the physician, nurse,
or medical specialist associated with the
patient record.
3. Disease: the main diagnosis for the patient.
4. Medicine: the prescribed drug or treatment.
5. Symptom: the clinical signs reported by the
patient or observed by the healthcare
professional.
In addition to these core classes, the dataset also
contains supplementary attributes such as medical
exams, therapeutic procedures, and allergies, which
are linked to the five main classes. This structure
ensures both flexibility and consistency in
representing patient-related information
We started with data cleansing which is a crucial
step in the process of managing healthcare data,
including EHR. This phase aims to guarantee the
quality, consistency and reliability of medical
information. During data cleansing, several aspects
are taken into account including the detection and
removal of duplicates, errors, and missing data. In
general, data cleansing plays a major role in creating
high-quality EHRs, ensuring that medical
information is accurate, complete and consistent,
which contributes to better quality healthcare and
efficient management of health data.
4 THE PROPOSED
ARCHITECTURE
Our proposed approach combines the structuring
power of a medical ontology with the flexibility of
machine learning and NLP. The motivation for this
approach is based on identifying the greatest
challenges to medical knowledge. This information is
the cornerstone of clinical decision-making,
biomedical research, and health management.
However, medical data is often unstructured,
heterogeneous, and subject to semantic ambiguity,
creating significant obstacles for healthcare
professionals and researchers who need to extract
relevant insights. To address these challenges, our
method integrates ontology-based structuring with
advanced machine learning techniques and Natural
Language Processing (NLP) to enhance semantic
annotation and interoperability.
Enhancing Data Quality and Semantic Annotation by Combining Medical Ontology and Machine Learning Techniques
143
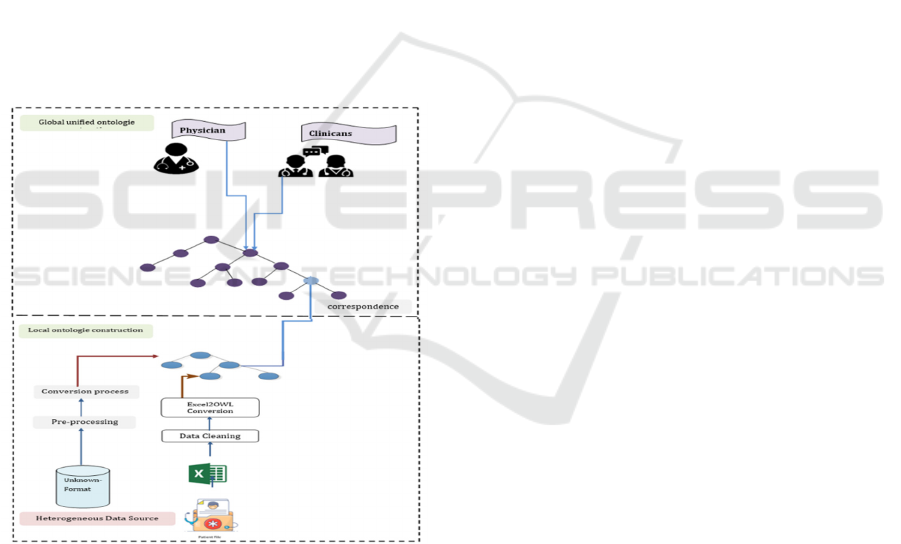
The architecture of this approach is shown in
Figure 1. It consists of two main layers: the
construction of local ontologies and the unification
into a global ontology.
1. In the first layer: Local Ontology Construction
A local ontology is generated for each data
source, and then converted into an OWL
ontology representation.
The input EHR data sources used in this
process are Excel files.
The output of this layer is a structured local
ontology in OWL format.
2. In the second layer: Global Ontology
Construction
The objective of this layer is to generate a
unified global ontology that consolidates
heterogeneous data sources into a single
structured representation.
This step provides semantic alignment and
ensures consistency across different
healthcare information systems.
Figure 1: Architecture of the proposed approach.
4.1 Local Ontologies Construction
Converting an Excel file into an ontology is a
fundamental process for transforming tabular data
into a rich and interpretable semantic structure. This
process is essential when we want to create a formal
and structured representation of the concepts and
relationships present in the data. Excel files are
commonly used to store and manage data in tabular
form, making them easy to use but less suitable for in-
depth semantic analysis. In contrast, an ontology is a
formal representation of concepts and relationships
providing rich semantics for data. The conversion
process begins with defining an appropriate ontology
structure for the data domain. This involves identi-
fying the classes, properties and relationships that
characterize the data. For example, in an Excel file
containing patient information, an ontology could
define classes such as ‘‘Patient‘‘,‘‘Disease‘‘,
‘‘Treatment‘‘, etc., and specify properties. Then, each
row in the Excel file is transformed into a class
instance in the ontology, and the values of the table
cells are associated with the corresponding properties.
4.2 Global Ontologies Construction
Ontology integration is a key step for ensuring
semantic interoperability across heterogeneous
medical datasets. One of the main challenges is that
ontologies may be developed under different
conceptual frameworks, which complicates their
integration. In our approach, we focused on domain-
specific ontologies that provide complementary
coverage of structural, administrative, and semantic
aspects of medical data. We selected three ontologies
for integration: EHR EXTRACT RM.owl, which
provides a formal representation of electronic health
record structures; RIMV3OWL.owl, which models
the HL7 Reference Information Model (RIM) and its
use in clinical systems; and OGMS.owl (Ontology for
General Medical Science), which defines core
concepts of medical science such as disease,
symptom, and diagnosis. The choice of these
ontologies was motivated by their complementary
scope: EHR EXTRACT RM and RIMV3OWL
address the structural and administrative aspects of
patient records, while OGMS provides the semantic
layer for core medical concepts.
Although BFO (Basic Formal Ontology) is a well-
known top-level ontology, we did not explicitly adopt
it in this work. Integrating BFO would have required
substantial re-engineering of the selected ontologies,
which was beyond the scope of our study. Instead, we
aimed to construct a unified mid-level ontology that
bridges EHR structures and medical semantics in a
pragmatic way, directly addressing interoperability
challenges. It is also worth noting that OGMS is itself
grounded in BFO, which indirectly provides our
integration with a degree of top-level alignment.
Furthermore, during the integration process we
identified a lack of sufficient information on medical
abbreviations within the existing ontologies. To
address this gap, we introduced a dedicated Medical
Abbreviations class, in which each abbreviation
KEOD 2025 - 17th International Conference on Knowledge Engineering and Ontology Development
144
instance is systematically organized in alphabetical
order and explicitly linked to its full meaning. This
addition enhances accessibility and improves the
semantic clarity of medical records for healthcare
professionals, researchers, and practitioners.
The use of abbreviations is frequent, users of the
global ontology could thus quickly access detailed
information on medical abbreviations, thereby
strengthening the quality and accuracy of medical
research and data analysis.
4.3 Machine Learning to Ensure
Correspondence
Faced with the complexity of medical terminologies
and the diversity of standards, semantic annotation is
essential for a precise understanding of medical
information. Nevertheless, applying this annotation at
scale requires a scalable approach, which is where
machine learning comes in. By leveraging machine
learning models, our solution aims to automate the
semantic annotation process, thus allowing precise
identification of medical terms and their contexts
within the data. At the same time, machine learning
helps overcome interoperability barriers by enabling
systems to dynamically adapt to different standards
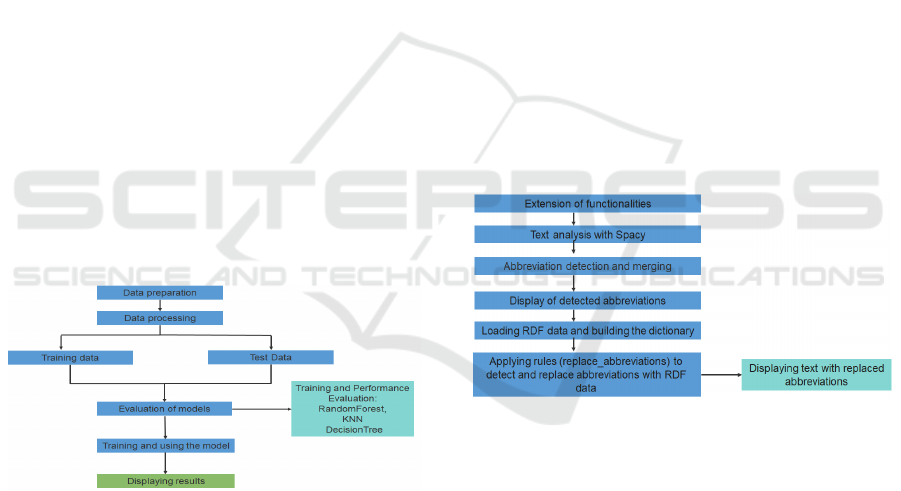
and data formats. The following steps in Figure 2
illustrate a comprehensive approach to solving the
automatic abbreviation detection problem.
Figure 2: Abbreviation detection model using ML.
4.4 Natural Language Processing to
Ensure Correspondence
The use of NLP and the SpaCy library represent an
essential dimension of our approach for semantic
annotation in the context of EHR. While machine
learning offers powerful solutions, NLP stands out as
a complementary method, exploiting advanced
understanding of human language to extract rich
semantic information. By integrating SpaCy, a
modern NLP library, our research aims to go beyond
the traditional limits of semantic annotation. The NLP
techniques and SpaCy significantly contribute to our
goal of semantically enriching medical data, thereby
improving the understanding of complex medical
concepts and supporting informed decision-making
in healthcare. Unlike standard implementations, we
enhance SpaCy capabilities by integrating domain-
specific medical ontologies, custom rule-based
phrase matchers, and pre-trained transformer models
to improve entity recognition. This enhancement
allows for high precision annotation and a better
contextual understanding of medical texts, making it
more adaptable to the complexities of EHR systems.
To validate our approach, we conduct quantitative
performance evaluations, including:
Precision, Recall, and F1-score for entity
recognition and abbreviation expansion.
Comparative analysis with alternative
NLP libraries to justify model selection.
Error analysis to refine NLP-based entity
resolution
This method’s approach performs several steps to
detect and process abbreviations in text using SpaCy,
the steps of this method are illustrated in the
following Figure 3.
Figure 3: Model using NLP (SpaCy).
5 EXPERIMENTATION AND
RESULTS
This section discusses the gathered results for each
phase of the proposed system.
5.1 Result of Data Cleansing
Figure 4 shows the missing values in all columns, the
1st column ’class’ shows that it has the highest
number of values displaying NaN with a number of
NaN is equal to 34, on the other hand the column
’properties’ has no NaN missing values, and the other
two columns ’subclass’ and ’instances’ have almost
Enhancing Data Quality and Semantic Annotation by Combining Medical Ontology and Machine Learning Techniques
145
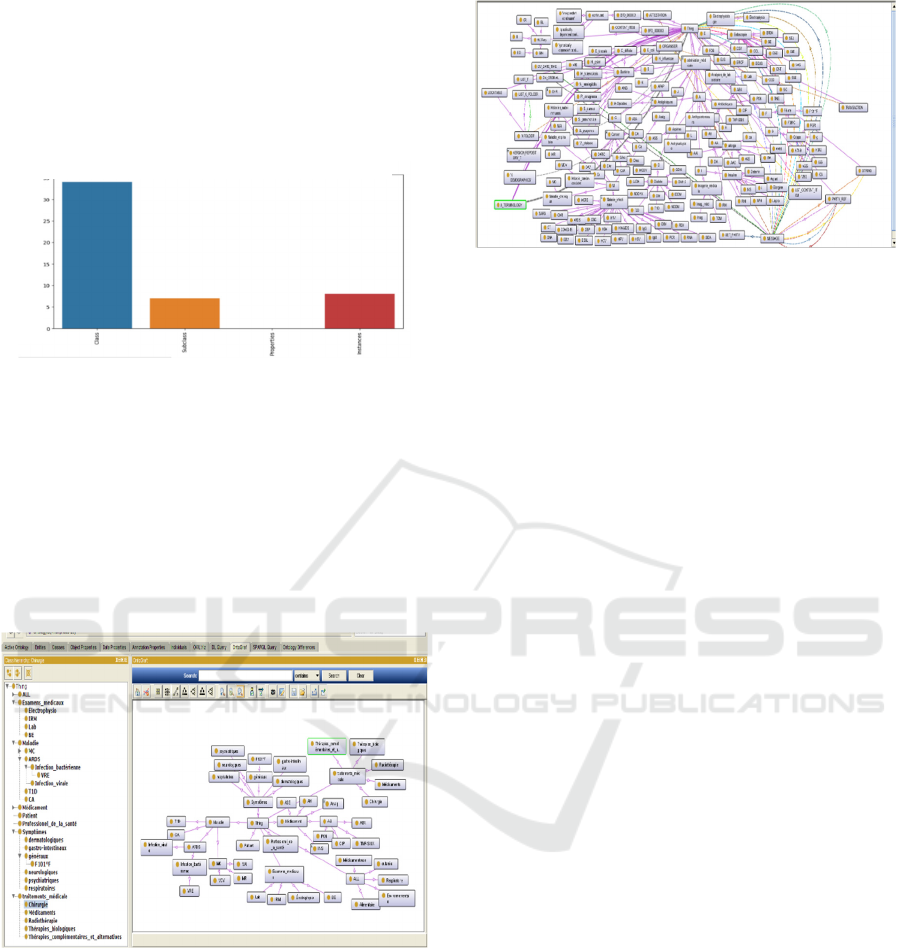
the same number of missing values with a NaN count
less than 10. Figure 4 illustrates the distribution of
missing NaN values in all columns before the
cleansing data. Then we replaced the NaNs with
zeros, and then we replaced with a specific chain
under the name ’Inconnu’.
Figure 4: Screenshot of the distribution of missing NaN
values in all columns before the cleansing data.
5.2 Results of Ontologies Construction
In this section we discuss the results of converting
data from Excel to our local ontology. This phase
constitutes the foundation of our approach, giving our
medical data a rich and precise semantic
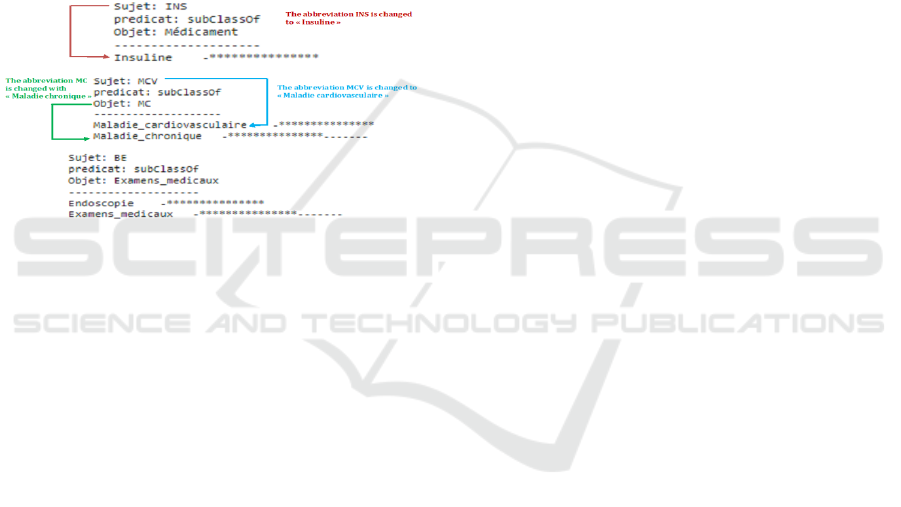
representation. Figures 5 and 6 show an extract of the
constructed ontology.
Figure 5: Ontology generated from Excel file
Figures 5 illustrate the ontology generated from an
Excel dataset, showing how tabular attributes are
transformed into semantic classes and organized
hierarchically. Some classes are instantiated with
terms in French, while others appear in English,
reflecting the multilingual nature of the source data.
This bilingual alignment allows the ontology to
support annotation in both languages, enabling health
records to be processed without ambiguity and
ensuring interoperability across multilingual datasets.
Figure 6: OntoGraf of the global ontology constructed.
Figure 6 OntoGraf of the global ontology constructed
from integrated sources (EHR EXTRACT RM.owl,
RIMV3OWL.owl, OGMS.owl) presents the graph of
the unified ontology produced by merging local
ontologies with domain ontologies. It highlights
aligned classes, merged properties, and the extensions
introduced (notably the Medical Abbreviations class
and its links to full forms). This mid-level ontology
acts as a semantic bridge between EHR structural
schemas and medical domain concepts.
5.3 Abbreviation Detection Using
Machine Learning
The following steps illustrate a comprehensive
approach to solving the automatic abbreviation
detection problem:
Data preparation: Begins loading data
containing phrases, abbreviations, meanings
and binary functions. Then created the
abbreviation to id dictionary to map the
abbreviations to unique numeric indexes and
added the abbreviation encoded column to
encode the abbreviations and use them for the
subsequent machine learning model.
Data processing: For data processing, we have
used scikit-learn to create a word vector using
CountVectorizer. These word vectors are then
combined using hstack with other properties
such as uppercase letters, alphanumeric letters,
and dot endings. The dataset is divided into a
training and a test set to evaluate the
performance of the models.
Evaluation of the model: Several classification
models such as RandomForest, KNN and
DecisionTree are trained on the data. The
performance of each model is evaluated using
various metrics such as accuracy, mean absolute
error, mean squared error and confusion matrix.
These estimates are then visualized using Plotly
Express to facilitate model operation.
Distribution of missing values (NAN) by column
number of missing values (NAN)
KEOD 2025 - 17th International Conference on Knowledge Engineering and Ontology Development
146
The comparison shows that the Decision Tree
classifier achieved the best performance, with an
accuracy of 1.0 and average absolute and squared
errors of 0.00. In second place, the Random Forest
model obtained an accuracy of 0.93, an average
absolute error of 0.06, and an average squared error
of 0.26. Finally, the K-Nearest Neighbors (KNN)
model achieved an accuracy of 0.83, an average
absolute error of 0.17, and an average squared error
of 0.41.
Although Decision Tree reached perfect accuracy
on the dataset, accuracy alone is not always a
sufficient metric for evaluating classifiers in the
medical domain, where robustness and generalization
are critical. For this reason, we also considered
complementary metrics such as precision, recall, and
F1-score, which provide a more balanced view of
performance. Based on these metrics, Decision Tree
remained highly effective, but Random Forest offered
more stable generalization results.
The final choice of Random Forest as the selected
model was motivated by several factors. First, unlike
a single Decision Tree, Random Forest aggregates
multiple trees, which reduces overfitting and
improves robustness on unseen data. Second, in
practice, the implementation of a Decision Tree with
high complexity required more computational
resources than were available in our environment, as
well as additional expertise in fine-tuning and
optimization. In contrast, Random Forest required
less fine-tuning, was easier to implement, and offered
strong performance while maintaining computational
feasibility.
5.3.1 Training and Using the Model
The implementation of the Random Forest model for
abbreviation detection involves a structured approach
comprising several key steps. Initially, a pipeline is
established, integrating a transformer
(CountVectorizer) and a RandomForestClassifier
model, facilitating efficient data preprocessing by
converting text into word vectors. Subsequently, the
dataset is partitioned into training and test sets, and
the RandomForest model is trained on the training set.
Following training, the model generates predictions
on the test set, and its performance is evaluated based
on accuracy. Additionally, the model is applied to
new sentences to detect abbreviations, assigning
labels to indicate their presence. This systematic
approach showcases the integration of Random
Forest into a natural language processing pipeline for
abbreviation detection, emphasizing its role in data
preparation, training, and prediction
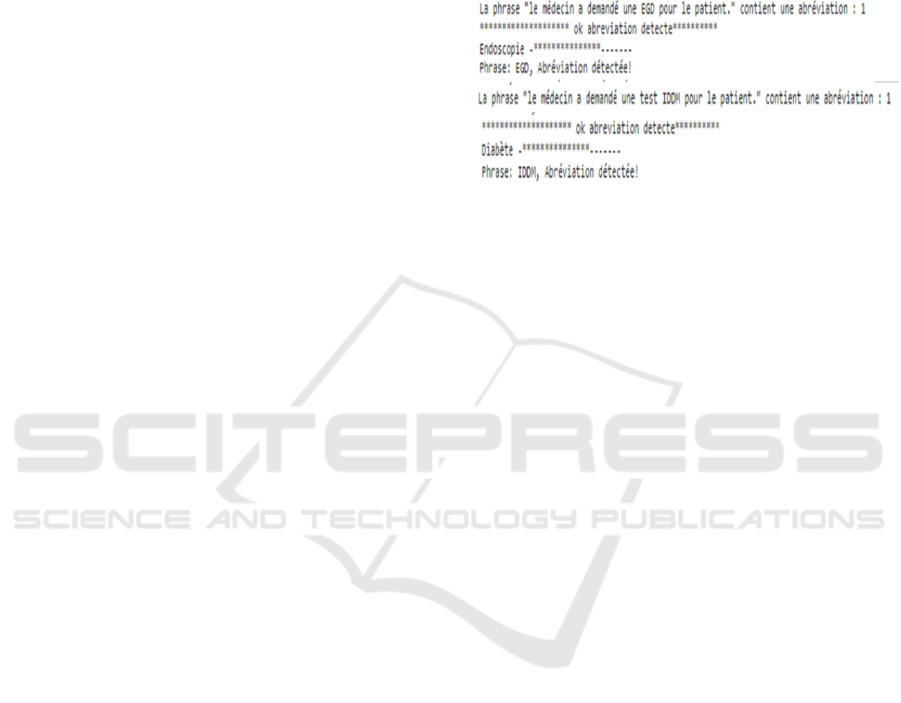
5.3.2 Displaying Results
We indicated whether an abbreviation was detected in
the new sentence and also displayed information
about the detected abbreviation by replacing the
abbreviation with its meaning using the replace
abbreviations function.
Figure 9: The results given by the Random Forest model.
Figure 9 shows our result given by the Random Forest
model trained to predict if there is an abbreviation. If
detected, the result displays the detected abbreviation
and its meaning. Take as an example the first
screenshot which shows that the abbreviation ’EGD’
is detected and changes with their meaning. which is
endoscopy. This section shows the resolution of the
automatic abbreviation detection problem,
integrating text processing, feature creation, model
training and performance evaluation. It offers a
complete and extensible solution for detecting
abbreviations in similar contexts.
5.4 Method of Abbreviation Detection
Using SpaCy a NLP Library
The method of automatic abbreviation detection was
implemented using SpaCy, a natural language
processing (NLP) library, combined with rule-based
heuristics and semantic enrichment.
SpaCy was applied for text preprocessing and
linguistic analysis, including tokenization, part-of-
speech tagging, and dependency parsing.
Abbreviation candidates were then identified through
regular expression–based rules, focusing on patterns
such as:
• uppercase sequences of up to five characters,
• contextual forms like “long form (short form)”
(e.g., Blood Pressure (BP)),
• and co-occurrence of potential abbreviations
with their expansions within the same text
window.
To improve accuracy, the system performed
frequency analysis of abbreviation–expansion pairs
and validated them against ontology concepts. When
Enhancing Data Quality and Semantic Annotation by Combining Medical Ontology and Machine Learning Techniques
147
multiple expansions were possible, the one
corresponding to an existing ontology class was
selected.
Furthermore, we used RDF data to enrich the
abbreviation dictionary. Each abbreviation was
annotated with semantic information such as domain,
synonyms, and related ontology class.
In the final step, abbreviations were automatically
replaced by their expanded forms, improving both
readability and semantic clarity. This process is
particularly beneficial for medical record analysis,
clinical reporting, and advanced biomedical research.
Figures 10 illustrate the overall workflow,
showing how SpaCy, regular expressions, and RDF-
based enrichment were combined to detect, expand,
annotate, and replace abbreviations in the corpus.
Figure 10: Screenshot of some abbreviations with their text
replaced given by SpaCy.
6 COMPARISON STUDY
We have done a comparison between the proposed
framework and other previous frameworks.
The machine learning-based approach is more
suited to complex tasks requiring generalization from
labeled data, while the NLP approach with SpaCy is
more transparent, easily adaptable, and well suited to
specific tasks like abbreviation detection. We have
done a comparison between the proposed framework
and other previous frameworks. Table 1 summaries
that comparison. This comparison highlights the
different approaches, their strengths and weaknesses,
allowing a comparative assessment of the
methodologies adopted for medical data
interoperability and semantic annotation. Our
approach stands out significantly from others on
several fronts, attesting to its reliability and
effectiveness. In terms of semantic annotation, our
methodology relies on advanced NLP and machine
learning techniques, thus surpassing the competing
approach which does not offer similar semantic
functionalities. The flexibility of our system is
demonstrated by its ability to adapt to the nuances
inherent in medical data, thus surpassing the average
flexibility offered by other approaches. Regarding
model training, our approach excels by integrating a
robust process, unlike the other method which
neglects this crucial dimension. In terms of
ontological interoperability, our approach confirms
its advantage by guaranteeing semantic consistency
between different data sources. And in terms of
complexity, our approach maintains a careful balance
between sophistication and practicality, thus
positioning itself favorably compared to other
approaches, characterized by high complexity.
Finally, from the performance point of view, our
approach excels with a high evaluation, while the
other approaches show moderate performance. These
substantial differences illustrate the increased
reliability and overall superiority of our approach.
Although the proposed approach achieves
syntactic interoperability in distributed EHRs, it
contains many perspectives. First, integration of new
data sources, we are expanding our approach to
include a variety of medical data sources, such as
medical images, imaging reports and genomic data.
This would contribute to a more complete
presentation of medical information. Second, much of
the knowledge in the field of medicine is unclear, so
we have to deal with incomplete and unclear
problems in the field. Therefore, the presence of a
specialist in this field is a plus.
7 CONCLUSIONS
The complex terminology used by specialists in the
medical field often creates a barrier for anyone
seeking to understand health-related information.
Health users need to decipher this ‘‘jargon‘‘to better
manage their situation. In the context of EHR,
hospitals and physicians face major challenges in
effectively sharing the information needed for
quality, timely, and costeffective care. In this
approach, we set out to solve the complex challenge
of EHR interoperability by combining approaches
based on machine learning and NLP. Our main
objective was to improve the semantic annotation of
medical data, thus facilitating interoperability
between different healthcare systems. To achieve this
goal, we followed an integrated approach, which built
a local and global ontology that helped improve
interoperability by standardizing the representation of
medical concepts. Our approach demonstrated
notable
efficiency in semantic annotation, providing
KEOD 2025 - 17th International Conference on Knowledge Engineering and Ontology Development
148
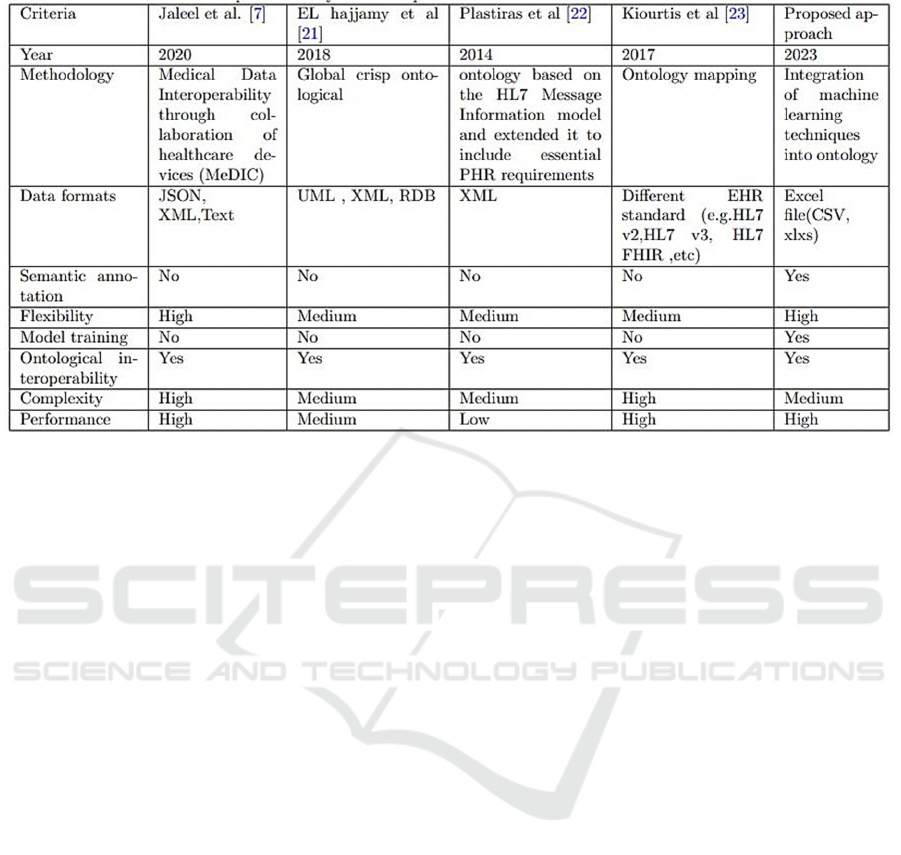
Table 1: A Comparison Study of the Proposed Framework and Other Previous Ones.
increased flexibility and better adaptation to
variations in medical data. Machine learning models
helped with accurate abbreviation detection, while the
use of SpaCy enhanced contextual understanding of
medical terms. The results show that Our proposed
ontological model offers a significant contribution to
understanding and resolving the challenges
surrounding semantic annotation of electronic health
records. Also it showed significant benefits in data
cleansing and medical data interoperability. By
combining robust ontological elements, machine
learning and NLP approaches, our approach aspires
to improve the efficiency and accuracy of health
systems through smarter management of medical
data, paving the way for significant advances in
understanding and management medical data,
reducing medical errors and guaranteed
interoperability. For future work, we need to create a
graphical user interface to easily use the implemented
framework and Further development of the
framework will concentrate on the limitations of this
work, as discussed previously.
REFERENCES
Adel, E., El-Sappagh, S., Barakat, S., Kwak, K., Elmogy,
M. (2022). Semantic architecture for interoperability in
distributed healthcare systems. IEEE Access, 10,
126161–126179.
Begoyan, A. (2007). An overview of interoperability
standards for electronic health records. Society for
Design and Process Science, USA.
Berges, I., Bermúdez, J., Illarramendi, A. (2011). Toward
semantic interoperability of electronic health records.
IEEE Transactions on Information Technology in
Biomedicine, 16, 424–431.
Celesti, A., Fazio, M., Romano, A., Villari, M. (2016). A
hospital cloud-based archival information system for
the efficient management of HL7 big data. In 2016 39th
International Convention on Information and
Communication Technology, Electronics and
Microelectronics (MIPRO), pp. 406–411.
Chen, L. Li, Lu, D., Zhu, M., Muzammal, M., Samuel, O.,
Huang, G., Li, W., Wu, H. (2019). OMDP: An
ontology-based model for diagnosis and treatment of
diabetes patients in remote healthcare systems.
International Journal of Distributed Sensor Networks,
15, 1550147719847112.
Costa, C., Menárguez-Tortosa, M., Fernández-Breis, J.
(2011). Clinical data interoperability based on
archetype transformation. Journal of Biomedical
Informatics, 44, 869–880.
Costa, C. Da, Wichman, M., Rosa Righi, R., Yamin, A.
(2019). Ontology-based model for interoperability
between openEHR and HL7 health applications. In
Proceedings of the International Conference in Health.
Fennelly, O., Moroney, D., Doyle, M., Eustace-Cook, J.,
Hughes, M. (2024). Key interoperability factors for
patient portals and electronic health records: A scoping
review. International Journal of Medical Informatics,
105335.
González-Ferrer, A., Peleg, M., Verhees, B., Verlinden, J.,
Marcos, C. (2012). Data integration for clinical
decision support based on openEHR archetypes and
HL7 virtual medical record. In International Workshop
on Process-oriented Information Systems in
Healthcare, pp. 71–84.
Gunter, T., Terry, N. (2005). The emergence of national
electronic health record architectures in the United
Enhancing Data Quality and Semantic Annotation by Combining Medical Ontology and Machine Learning Techniques
149

States and Australia: models, costs, and questions.
Journal of Medical Internet Research, 7, e383.
Hajjamy, O. El, Alaoui, L., Bahaj, M. (2018). Integration of
heterogeneous classical data sources in an ontological
database. In Big Data, Cloud and Applications: Third
International Conference, BDCA 2018, Kenitra,
Morocco, pp. 417–432.
Kalra, D. (2006). Electronic health record standards.
Schattauer GMBH-Verlag.
Kiourtis, A., Mavrogiorgou, A., Kyriazis, D. (2017).
Aggregating heterogeneous health data through an
ontological common health language. In 2017 10th
International Conference on Developments in eSystems
Engineering (DeSE), pp. 175–181.
Liyanage, H., Krause, P., De Lusignan, S. (2015). Using
ontologies to improve semantic interoperability in
health data. BMJ Health & Care Informatics, 22.
McClanahan, K. (2008). Balancing good intentions:
protecting the privacy of electronic health information.
Bulletin of Science, Technology & Society, 28, 69–79.
Mylka, A., Kryza, B., Kitowski, J. (2012). Integration of
heterogeneous data sources in an ontological
knowledge base. Computing & Informatics, 31.
Roehrs, A., Costa, C., Rosa Righi, R., Rigo, S., Wichman,
M. (2018). Toward a model for personal health record
interoperability. IEEE Journal of Biomedical and
Health Informatics, 23, 867–873.
Santos, M., Bax, M., Kalra, D. (2010). Building a logical
EHR architecture based on ISO 13606 standard and
semantic web technologies. In MEDINFO 2010, pp.
161–165.
Sartipi, K., Dehmoobad, A. (2008). Cross-domain
information and service interoperability. In
Proceedings of the 10th International Conference on
Information Integration and Web-based Applications &
Services, pp. 25–32.
Sachdeva, S., Bhalla, S. (2022). Using knowledge graph
structures for semantic interoperability in electronic
health records data exchanges. Information, 13, 52.
Schloeffel, P., Beale, T., Hayworth, G., Heard, S., Leslie,
H., et al. (2006). The relationship between CEN 13606,
HL7, and openEHR. In HIC 2006 and HINZ 2006:
Proceedings, p. 24.
Sreenivasan, M., Chacko, A. (2020). A case for semantic
annotation of EHR. In 2020 IEEE 44th Annual
Computers, Software, and Applications Conference
(COMPSAC), pp. 1363–1367.
Plastiras, P., O’Sullivan, D., Weller, P. (2014). An
ontology-driven information model for interoperability
of personal and electronic health records
KEOD 2025 - 17th International Conference on Knowledge Engineering and Ontology Development
150
