
Towards a Systemic Approach to Knowledge Integration in Learning
Health Ecosystems: AI and DLT Perspectives
Nabil Georges Badr
a
Higher Institute of Public Health, Faculty of Medicine, Saint Joseph University of Beirut, Beirut, Lebanon
Keywords: Learning Healthcare Systems, Distributed Ledger Technology, Artificial Intelligence.
Abstract: A Learning Health System (LHS) is an essential paradigm for addressing the evolving complexities of
healthcare systems, fostering continuous improvement, adaptability, and stakeholder collaboration. By
integrating knowledge management with technological advancements, LHS enhances data-driven decision-
making and the responsiveness of healthcare interventions. Artificial Intelligence (AI) has emerged as a
powerful tool within Learning Health Systems, yet its evolving nature presents challenges related to ethical,
traceable, and trustworthy data management. Distributed Ledger Technology (DLT) offers immutable and
transparent data governance, yet its full potential remains unrealized due to the absence of integrated
frameworks that could reinforce accountability and reliability in AI-driven processes. Addressing this gap is
critical for developing robust, ethical, and efficient healthcare solutions. This paper examines the synergistic
potential of AI and DLT within LHS, proposing a framework that leverages systematic knowledge integration,
predictive analytics, and proactive interventions. By harnessing AI-driven automation, IoT-enabled data
collection, and the secure, decentralized architecture of DLT, LHS can advance evidence-based healthcare,
mitigate disparities, and promote equitable access to high-quality care.
1 INTRODUCTION
A Learning Health System (LHS) is a vital approach
for addressing the evolving complexities of
contemporary healthcare systems. It emphasizes
continuous enhancement, adaptability, and
cooperation among stakeholders, including
healthcare providers, policymakers, researchers, and
community members. The effectiveness of an LHS
relies on the integration and management of
knowledge. By systematically generating, sharing,
and applying insights, the LHS supports evidence-
based practices, advances predictive analytics, and
drives proactive interventions. Utilizing data-driven
insights and fostering innovation, an LHS strives to
improve health outcomes, reduce disparities, and
ensure equitable access to quality care. Technological
advancements, like Internet of Things (IoT) and
Artificial Intelligence (AI), play a crucial role in this
integration. Using technology and automation
artifacts, data elements are organized, then
transformed into information. Closing the cycle,
newly acquired explicit knowledge converts to tacit,
a
https://orcid.org/0000-0001-7110-3718
restarting the cycle of renewable knowledge, thus
growing the skills and capabilities of the stakeholder
actors through knowledge integration. For instance,
integrated knowledge can inform predictive models
for disease outbreaks or environmental hazards,
empowering smart cities to proactively address public
health challenges while promoting equity,
sustainability, and improved health outcomes. Smart
sensors can monitor environmental conditions, detect
emergencies, and provide real-time data to both
public health and safety agencies. Predictive analytics
can identify trends and potential risks, enabling
coordinated responses. This interconnected approach
not only improves individual and community safety
but also fosters resilience and sustainability (Badr et
al., 2023).
We investigate the possible value creation of
joining AI to Distributed Ledger Technology (DLT)
as applied to the complex health service ecosystem.
DLT might track an immutable attribute for
preserving identity of sources of truth, without
maintaining an inherent level or trust in the
information collected and managed by AI (Pandl et
332
Badr, N. G.
Towards a Systemic Approach to Knowledge Integration in Learning Health Ecosystems: AI and DLT Perspectives.
DOI: 10.5220/0013657100004000
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Knowledge Discovery, Knowledge Engineering and Knowledge Management (IC3K 2025) - Volume 2: KEOD and KMIS, pages
332-339
ISBN: 978-989-758-769-6; ISSN: 2184-3228
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
al., 2020). Through this synthesis, we aim to advance
the discourse on intelligent health systems capable of
co-creating value, fostering systemic learning, and
responding effectively to present and future public
health challenges. We treat our concept of LHS as an
ecosystem with interconnected and adaptive
elements, decentralized and diverse components that
evolve based on interaction and feedback.
2 BACKGROUND
2.1 Visions of a Learning Health System
Public health relies on service intelligence to
transform data into knowledge integration to power
learning healthcare systems. In general, knowledge
management focuses on the collection, storage,
dissemination, and utilization of knowledge within an
organization or system, enabling informed decision-
making and continuous learning. For instance, in a
public health ecosystem, knowledge management
facilitates the integration of patient data, research
findings, and operational insights across healthcare
networks. This allows service providers to tailor
interventions, improve service delivery, and address
population-specific needs effectively.
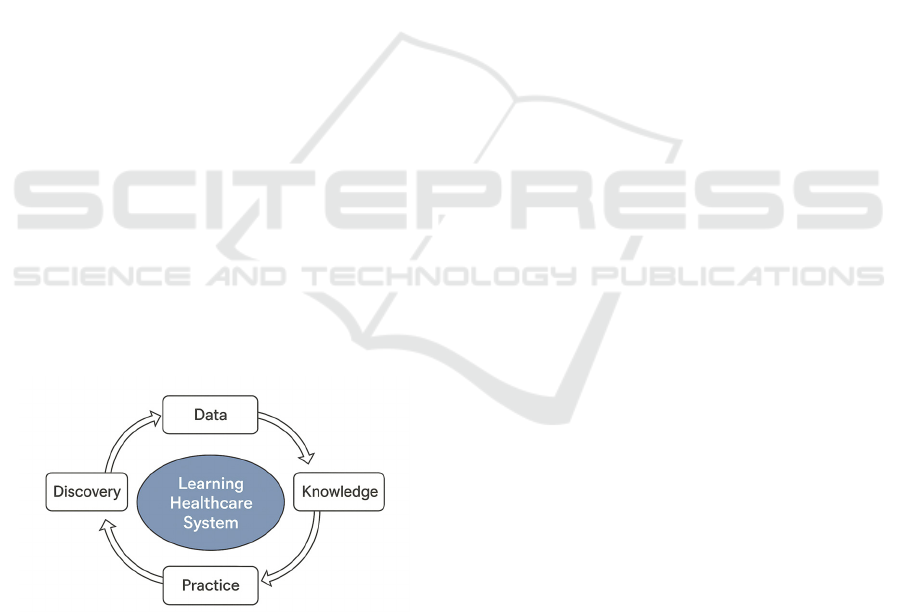
A Learning Health System integrates diverse data
sources to drive knowledge creation, inform policy
decisions, and enhance operational processes
(Easterling et al., 2022). The concept of a Learning
Health System revolves around creating a continuous
cycle of learning and improvement in healthcare
(Figure 1).
Figure 1: Conceptual Representation of Knowledge Cycles
Learning Health System.
It integrates data collection, analysis, and application
to enhance patient outcomes and system efficiency
(Yano et al., 2021). The LHS operates through
iterative cycles, often described as "Practice to
Data," "Data to Knowledge," and "Knowledge to
Practice." This means that real-world healthcare
practices generate data, which is analysed to produce
actionable knowledge, and this knowledge is then
applied back into practice.
The implementation of an LHS offers significant
benefits, including strengthened disease prevention
efforts, evidence-based policy formulation, and
improved health outcomes for populations.
Introducing an LHS has the potential to revolutionize
public health practices. To unlock this potential,
stakeholders across the public health ecosystem must
take coordinated action. Essential steps include
investing in advanced informatics infrastructure,
prioritizing the development of a skilled workforce,
establishing comprehensive data governance
frameworks, and creating incentives to support LHS
implementation and growth. By addressing these
critical areas, public health systems can evolve to
become more adaptive, efficient, and impactful in
achieving better health outcomes for all (Tenenbaum,
2024). Therefore, the production of useful, renewable
knowledge (Badr et al., 2020) that is required for
timely and effective decision-making. In context,
knowledge management in the healthcare sector
exhibits the full lifecycle of knowledge production
from knowledge creation, acquisition and storage
(Florio, 2019) for sharing, decision-making and
application of ethically sound knowledge translation
(Mutashar, 2024). The latter must be manifested
through measures of knowledge protection that drive
equity (Badr et al., 2023) and intellectual property
safeguards (Zhang et al., 2024).
To accelerate learning within a Healthcare
system, envisioning a closed-loop process is key. This
approach ensures the integration of truthful
information to enable timely decision-making,
enhance stakeholder collaboration, and foster
interoperability. Crucially, it also maintains
transparency and trust in the shared knowledge.
Potential elements of acceleration include integrated
data systems, creating platforms where diverse data
sources—like patient records, environmental health
data, and research findings—are unified and
accessible for analysis. Advanced analytics leverage
2.2 Potential of DLT in Healthcare KM
Distributed Ledger Technology (DLT) refers to a
decentralized system of electronic records that
enables independent entities to reach consensus on a
shared ledger without relying on a central authority
(Rauchs et al., 2018). Unlike traditional databases,
DLT systems maintains data across multiple nodes.
These systems typically employ cryptographic
techniques, consensus algorithms, and immutable
data structures to validate and secure transactions
Towards a Systemic Approach to Knowledge Integration in Learning Health Ecosystems: AI and DLT Perspectives
333

(Zheng et al., 2017). DLT systems serve as
“consensus machines” that facilitate secure,
transparent, and tamper-resistant data exchange
across distributed environments (König & Neumaier,
2023). Key functionalities include decentralized data
validation, whereby, transactions are verified through
consensus mechanisms eliminating the need for
centralized oversight. Once recorded, data entries are
cryptographically linked and cannot be altered
retroactively, ensuring auditability and trust
(Immutable Recordkeeping). Programmable logic
(Smart Contracts) is embedded in the ledger to
automate processes such as access control, asset
transfers, and compliance enforcement (Christidis &
Devetsikiotis, 2016).
Despite its challenges in scalability,
interoperability, and regulatory uncertainty ongoing
research and hybrid architectures—such as
combining DLT with federated learning or semantic
ontologies are improving the potential in enhancing
data integrity, provenance, and accessibility across
sectors such as healthcare, finance, and supply chain
management (Antal et al., 2021; König & Neumaier,
2023). Its effectiveness in knowledge management is
particularly evident by maintaining a tamper-proof
history of transactions, DLT ensures that knowledge
assets remain authentic and verifiable (Ferraiolo et
al., 2021). Attribute-based access models integrated
with DLT allow for granular, policy-driven sharing of
sensitive data across organizational boundaries
(DeFranco et al., 2024). Emerging frameworks
leverage DLT to construct distributed knowledge
graphs, enabling consistent and trustworthy
knowledge sharing in decentralized systems (Zaarour
et al., 2024).
2.3 AI in Healthcare KM
Artificial Intelligence (AI) refers to the design and
development of computational systems capable of
performing tasks that typically require human
intelligence, such as learning, reasoning, perception,
and decision-making (Russell & Norvig, 2021). AI
systems operate through algorithms that enable
machines to analyze data, recognize patterns, and
adapt to new information.
AI significantly enhances both data management
and knowledge management (KM) by automating
processes, improving accuracy, and enabling
intelligent decision support. AI systems naturally
excel in processing structured and unstructured data,
extracting relevant insights from diverse sources such
as documents, images, and speech (Sterne &
Davenport, 2024). Natural language processing
(NLP) and machine learning (ML) algorithms play a
critical role in generating metadata and organizing
data assets to improve discoverability (Taherdoost &
Madanchian, 2023). Despite its transformative
impact on knowledge management (KM), AI faces
persistent challenges, including issues with data
quality, integration, user trust, and ethical concerns
such as algorithmic bias and privacy. These barriers
can hinder adoption and system reliability.
Nevertheless, AI continues to advance as a core
component of KM systems, offering scalable,
intelligent, and adaptive solutions tailored to the
demands of complex, data-driven environments.
Empirical studies and industry applications
demonstrate that AI is highly effective in
transforming knowledge management (KM)
practices. AI was reported to enhance the speed and
precision of knowledge discovery, substantially
reducing time spent searching for information and
enabling more informed decision-making (Davenport
& Kirby, 2016). By automating routine KM tasks, AI
liberates human resources to focus on strategic and
creative work (Vadari & Desik, 2021).
The advancement of AI and its integration within
Learning Health Systems (LHS) present significant
opportunities for rapid learning cycles and value
creation. However, the inherently probabilistic and
evolving nature of AI poses challenges to ensuring
ethical, traceable, and trustworthy information
handling. AI and machine learning to process
information rapidly, uncover patterns, and predict
outcomes. Collaborative networks encourage
partnerships across disciplines and institutions to
share knowledge and resources effectively.
3 TOWARDS ACCELERATING
LEARNING HEALTH SYSTEMS
In a learning healthcare system, there must be a clear
cycle of information exchange between practice and
research. The system capitalizes on advancements in
health information technology and the expanding
health data infrastructure to access and utilize
evidence in real time. Simultaneously, it extracts
insights from real-world care delivery processes,
fostering innovation in care practices and driving
health system transformation through rigorous
research.
3.1 Adaptability and Scalability
Artificial Intelligence (AI) empowers data-driven
decision-making in healthcare by transforming vast,
KMIS 2025 - 17th International Conference on Knowledge Management and Information Systems
334

complex datasets into actionable insights that
enhance clinical, operational, and strategic outcomes.
Integrating consolidated and amalgamated
information from different sources in a decentralized
infrastructure may introduce ambiguity and lack the
transparency necessary to instil trust in the decisions.
Through advanced machine learning algorithms,
AI systems analyse structured and unstructured
data—from electronic health records and sensor
inputs to genomic sequences and social
determinants—to uncover patterns, predict trends,
and recommend interventions with speed and
precision. This analytical capability supports real-
time decision support, personalized treatment plans,
and resource optimization, facilitating a shift from
reactive care to anticipatory and adaptive health
management.
AI continuously learns from emerging data, it
strengthens feedback loops and enhances the agility
of decision-making across the Learning Health
System, paving the way for more responsive,
equitable, and evidence-informed healthcare
delivery. Such LHS must be designed to operate at
various levels, from individual organizations to
national healthcare systems, ensuring adaptability
and scalability.
3.2 Collaboration and Interoperability
We expect AI to enhance systems interoperability by
enabling communication and data exchange across
diverse platforms and applications. Advanced
techniques like data mapping and transformation
allow AI algorithms to convert information into
formats compatible with different systems,
addressing challenges like data silos and inconsistent
standards (Nilsson et al., 2024). Natural Language
Processing (NLP) further supports interoperability by
extracting structured data from unstructured sources,
such as clinical notes, making integration across
systems more efficient (Dennehy et al., 2023).
Additionally, AI facilitates predictive analytics,
identifying patterns and trends that improve
coordination and decision-making across
interconnected systems. By leveraging these
capabilities, AI drives more cohesive interoperability,
ultimately enhancing outcomes in industries like
healthcare.
3.3 Transparency and Trust
Illustrative to the complexity of knowledge
production and management, numerous attributes of
trustworthy AI, including privacy, interpretability,
bias, and fairness, are closely linked. Explainable AI
has the potential to overcome this issue and can be a
step towards trustworthy AI (Markus et al., 2021).
Building trustworthy and explainable AI (XAI) in
healthcare systems is still in its early stages (Albahri
et al., 2023). Where explainability is the process by
which the AI model derives its output can be
presented so that users can understand it (Samek et
al., 2017). Explainable AI (XAI) for example is a set
of tools and frameworks to help the user understand
and interpret predictions made by machine learning
models. Explainable AI (XAI) is a growing field that
aims to make AI models more understandable. In
Healthcare, XAI aims to make AI system decision-
making processes more transparent, allowing users to
trust, understand, and manage AI. AI-driven models
used in diagnosing diseases or suggesting treatment
options often leverage XAI to help physicians
understand the basis of their recommendations.
Hospitals can use explainable AI for cancer detection
and treatment, where algorithms show the reasoning.
This is done by providing clear explanations of how
AI models make decisions or predictions.
3.4 Automation and Efficiency
Healthcare providers may now increase operational
efficiency, precision, and the fundamental building
blocks of decision-making processes thanks to the
combination of AI algorithms, machine learning
paradigms, and deep learning methodologies. AI is
assisting medical professionals and life sciences
organizations in improving early illness detection and
intervention. AI technology (with machine learning
capabilities) can identify disparities (e.g., housing
conditions, food insecurity, transportation issues) that
negatively impact the ability to find the right patients
for the right trials and assist them in participating
successfully by sifting through unstructured data and
narrative notes. On the other hand, DLT significantly
enhances automation and efficiency within a learning
Healthcare system (Badr, 2019).
3.5 Ethical and Secure Learning
Ethical manipulation of data components would
involve user engagement, full disclosure and
feedback on justifiable use of information (Badr et al.,
2021). By using AI technologies, healthcare
professionals and academics may more effectively
assess unfair inequities and assist communities and
providers in creating solutions that improve health
equality by connecting them to community resources,
treatment alternatives, and access to care. When
Towards a Systemic Approach to Knowledge Integration in Learning Health Ecosystems: AI and DLT Perspectives
335

maintained, the trustworthy nature of AI systems is
complemented by their responsible use and
application. AI systems are not intrinsically
dangerous or harmful; rather, their potential for harm
depends largely on the context in which they are used.
In simpler terms, we must be able to trust the
accuracy, veracity and accuracy of the data feeding
the knowledge production cycle, entering the cycle at
any point.
3.6 Continuous Feedback for
Improvement
Closing the cycle, newly acquired explicit knowledge
converts to tacit, restarting the cycle of renewable
knowledge, thus growing the skills and capabilities of
the stakeholder actors through knowledge integration
(Badr et al., 2020). Parenthetically, the evolution of
knowledge in public health is a model where two
principles collide: the need to have integral
information for decision-making and the necessity to
maintain ethical boundaries of privacy (Badr et al.,
2021). Aside from the noble goal of public safety,
these tools must be ethically compliant to ensure that
no "harm is done" to fundamental ethical principles
that must protect individuals' autonomy, privacy, and
non-discrimination today (Badr et al., 2021).
3.7 AI – DLT Synergistic Advantage
The lack of a robust framework for maintaining
transparency, accountability, and immutability in AI-
driven data processes creates risks of compromised
data integrity and trust. DLT offers deterministic and
immutable capabilities that could address these
challenges, there is a need for effective integration of
DLT into AI-driven systems.
However, the absence of standardized pathways
for utilizing smart contracts and leveraging DLT's
capabilities to track sources of truth and ensure data
security further complicates the creation of ethical
and reliable Learning Health Systems. This gap
highlights the need for a framework that synergizes
DLT's transparency and AI's analytical power to
support ethical, efficient, and trustworthy healthcare
solutions.
Recent studies highlight the transformative
potential of DLT, particularly blockchain, in
healthcare and AI applications. For instance,
blockchain is being explored for enhancing data
security, interoperability, and patient privacy (Bundi
et al., 2023). It offers decentralized and immutable
data management, which is crucial for handling
sensitive health records and AI-driven analytics
(Drosatos & Kaldoudi, 2019). Key applications
include Secure Data Sharing, where Blockchain
facilitates secure and interoperable health data
exchange, enabling AI models to access reliable
datasets for training and predictions. On the other
hand, the regulatory requirements of Patient Consent
Management can be addressed through DLT’s Smart
contracts ensure transparent and automated consent
processes (Plenk et al., 2019).
By ensuring secure, decentralized, and tamper-
proof data management, DLT minimizes the need for
manual interventions, streamlining processes like
patient record updates and medical supply tracking.
Smart contracts, a feature of DLT, automate complex
workflows such as insurance claims processing,
reducing administrative burdens and accelerating
operations. Its interoperability enables data sharing
across healthcare providers, researchers, and patients,
eliminating redundancies and fostering collaboration.
Furthermore, DLT offers transparent traceability for
clinical trials and treatments, ensuring accountability
and improving trust. With reduced operational costs
and enhanced data handling efficiency, DLT plays a
pivotal role in enabling real-time analytics and
personalized care, driving better patient outcomes and
operational excellence.
Continuous feedback and improvement in a
learning healthcare system can be revolutionized by
the synergy of DLT and AI. DLT ensures that
healthcare data is securely stored and transparently
shared, enabling stakeholders to access immutable
records for analysis and collaboration. This
decentralized data structure allows real-time feedback
loops between researchers, providers, and patients,
ensuring that insights are consistently integrated into
practice. AI enhances this process by analysing large
datasets, identifying patterns, and generating
actionable recommendations for care improvement.
Together, DLT and AI enable dynamic updates to
protocols, personalized treatment plans, and efficient
resource allocation, fostering an ecosystem that
adapts and evolves in response to new evidence,
ultimately driving better health outcomes and
operational efficiency.
4 PUTTING IT ALL TOGETHER
A learning health system is designed to detect,
validate, and respond to public health threats while
continuously improving through feedback and
analytics. This enables proactive responses to health
emergencies, such as outbreaks or contamination
events. A LHS is structured to detect, validate, and
KMIS 2025 - 17th International Conference on Knowledge Management and Information Systems
336
respond to health threats such as outbreaks or
contamination, while continuously refining its
processes through feedback and analytics. This
proactive approach integrates systematic workflows
centred on monitoring, validation, decision-making,
and adaptive learning (Gheibi et al., 2021).
In the healthcare system, the integration of these
workflows enables rapid advancements in clinical
outcomes and operational efficiency. For example,
the use of AI and big data in disease outbreak
monitoring can expand into broader applications like
personalized medicine, predictive diagnostics, and
real-time hospital resource management. The
continuous feedback loops and analytics-driven
adjustments ensure that the system learns from every
case, refining its processes to deliver better care over
time. By integrating AI and DLT, healthcare systems
can accelerate learning, enhance efficiency, and
improve patient outcomes. Therefore, accelerating
learning within a healthcare system involves applying
principles that enhance the speed and effectiveness of
knowledge acquisition, decision-making, and system
improvement.
DLT and AI are transformative forces in
accelerating Learning Healthcare Systems (LHS).
DLT, such as blockchain, ensures secure, transparent,
and decentralized data sharing across healthcare
networks. This technology addresses critical
challenges like data integrity, privacy, and
interoperability, enabling collaboration among
stakeholders, including healthcare providers,
researchers, and patients. By creating immutable
records, DLT fosters trust and accountability, which
are essential for advancing LHS. AI complements
DLT by analysing vast datasets to uncover patterns,
predict outcomes, and optimize decision-making
processes. In LHS, AI-powered tools enhance
diagnostics, personalize treatments, and streamline
administrative tasks. For example, machine learning
algorithms can identify trends in patient data,
enabling proactive interventions and improving
population health management. AI also supports real-
time monitoring through wearable devices and
telemedicine platforms, enhancing patient
engagement and accessibility. The integration of DLT
and AI creates a synergistic ecosystem where data-
driven insights and secure information exchange
drive continuous learning and improvement. DLT
ensures that data shared across the system remains
tamper-proof and accessible, while AI transforms this
data into actionable knowledge. Together, they
enable LHS to adapt to emerging challenges, innovate
care delivery, and reduce inefficiencies.
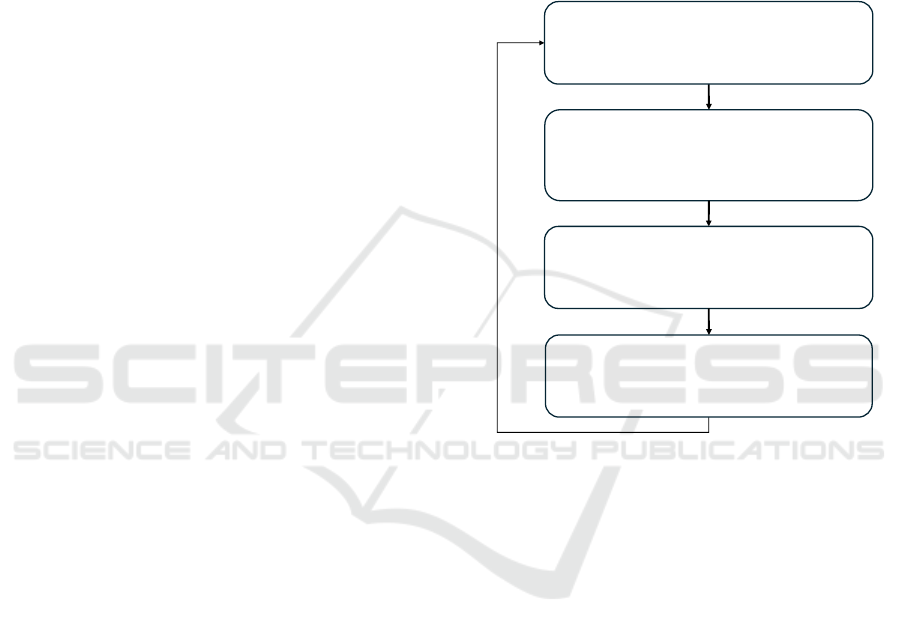
We can therefore exemplify our model in a
simple, practical, and comprehensive knowledge
management life cycle model (KMC). Building on
the harmonization concept from Heisig, P. (2009) and
following the example of Evans and Ali’s (2013), we
suggest a model for Conceptual KMC Integration in
Learning Health Systems. Each stage is powered by
technologies such AI and DLT. We further explain
essential principles for accelerating learning
healthcare systems (Figure 2).
Figure 2: Conceptual KMC Integration in Learning Health
Systems (By author inspired by Evans and Ali’s (2013).
We envision the following: In the Identify/Create
phase, AI facilitates real-time analytics and predictive
modeling, enabling timely insights, while DLT
ensures data integrity and origin traceability,
reinforcing trust in the foundational data layer. The
Store & Share stage emphasizes interoperability and
collaboration; AI offers transparent insights and
process automation, whereas DLT provides
decentralized data governance and transparency,
securing seamless and accountable data exchange. As
knowledge is Used/Applied, ethical considerations
come to the forefront—AI systems are designed to
minimize bias and enhance fairness, and DLT ensures
compliance and auditability, safeguarding ethical
data use across stakeholders. Before the cyclical
iteration, in the phase Learn & Improve, AI analyzes
outcomes and feedback to refine predictions and
actions, while DLT maintains a transparent history of
interactions, enabling robust traceability and systemic
evaluation. Together, these stages exemplify a
dynamic learning cycle, where AI and DLT operate
Identify / Create
Data-Driven Decision Making
(AI) Real-time analytics & predictive modelling
(DLT) Ensure the integrity & security of data used in AI models
Store / Share
Collaboration / Interoperability / Transparency
Trust / Automation / Efficiency
(AI) Transparent insights & automation of processes
(DLT) Enhance interoperability; Transparency and Accountability
.
Use / Apply
Ethical and Secure
(AI) Prioritize ethical use (fairness and bias reduction)
(DLT) Ensures compliance & Ethical use
Learn & Improve
Continuous Feedback and Improvement
(AI) Analyse feedback from outcomes and experiences
(DLT) Provide transparent record of all interactions and outcomes
Towards a Systemic Approach to Knowledge Integration in Learning Health Ecosystems: AI and DLT Perspectives
337

in synergy to support adaptive decision-making,
ethical data stewardship, and sustainable innovation
in healthcare systems.
5 CONTRIBUTION AND FUTURE
RESEARCH
This paper advances the discourse on systemic
knowledge integration in Learning Health Systems by
proposing a novel framework that synergizes
Artificial Intelligence (AI) and Distributed Ledger
Technology (DLT). It contributes to the field by
conceptualizing an approach that addresses the dual
challenges of data governance and dynamic
knowledge generation within healthcare
environments. Specifically, the integration of
immutable DLT architectures with predictive and
adaptive AI workflows offers a blueprint for
designing transparent, interoperable, and responsive
health systems. The framework operationalizes
foundational principles of trust, collaboration, and
continual learning—core tenets of sustainable
LHSs—while aligning with broader goals of
equitable care and system resilience.
DLT and AI are pivotal in fostering collaboration
within a Learning Healthcare system (LHS). Several
applications of AI in healthcare are focused on
enabling caregivers to better care for patients in order
to improve the quality of care (Badr, 2022). DLT
provides secure, transparent, and decentralized data-
sharing capabilities, which create a trusted
environment for stakeholders such as healthcare
providers, researchers, and patients to exchange
information without compromising data privacy or
integrity. This secure framework is complemented by
AI, which processes vast amounts of data to uncover
patterns, predict outcomes, and personalize
interventions, thereby enhancing decision-making
(Badr, 2022). Together, DLT and AI promote
continuous learning through knowledge integration
and feedback loops, enabling dynamic responses to
emerging health challenges. Their synergy fuels co-
creation and innovation in healthcare delivery,
ultimately building a more resilient and patient-
centred ecosystem (Badr et al., 2021).
Future research ought to focus on operationalizing
this conceptual model within real-world healthcare
settings and diverse sociotechnical ecosystems.
Exploratory studies are needed to evaluate the
model’s scalability, performance, and regulatory
compliance across heterogeneous infrastructures and
stakeholder groups. Empirical investigations into the
implementation of AI-DLT synergy in patient
consent management, adaptive diagnostics, and inter-
organizational knowledge exchange will help
validate its practical utility. Additionally,
interdisciplinary inquiry into behavioral,
organizational, and systemic barriers to adoption can
inform strategies for stakeholder engagement, trust-
building, and ethical design. Expanding this model to
encompass Smart Cities and global health networks
may further uncover its potential for promoting
equity, sustainability, and personalized “care at
scale”.
Disclosure of Interests. Author has no competing
interests to declare that are relevant to the content of
this article.
REFERENCES
Albahri, A. S., Duhaim, A. M., Fadhel, M. A., Alnoor, A.,
Baqer, N. S., Alzubaidi, L., Albahri, O. S., Alamoodi,
A. H., Bai, J., Salhi, A., & others. (2023). A systematic
review of trustworthy and explainable artificial
intelligence in healthcare: Assessment of quality, bias
risk, and data fusion. Information Fusion, 96, 156–191.
Antal, C., Cioara, T., Anghel, I., Antal, M., & Salomie, I.
(2021). Distributed Ledger Technology Review and
Decentralized Applications Development Guidelines.
Future Internet, 13(3), 62. https://doi.org/10.3390/fi1
3030062
Badr, G. N., Carrubbo, L., Baldi, G., & others. (2023).
Engaging our Digital Technology Actors in Learning
HealthCare Ecosystems for Sustainability and Equity.
In Managing Knowledge for Sustainability (pp. 2141–
2162). Institute of Knowledge Asset Management
(IKAM).
Badr, N., Drăgoicea, M., Walletzkỳ, L., Carrubbo, L., &
Toli, A. M. (2021). Modelling for ethical concerns for
traceability in time of pandemic “do no harm” or “better
safe than sorry!” Proceedings of the 54th Hawaii
International Conference on System Sciences, 1779.
Badr, N. G. (2019). Blockchain or distributed ledger
technology what is in it for the healthcare industry?
KMIS, 277–284.
Badr, N. G. (2022). Learning Healthcare Ecosystems for
Equity in Health Service Provisioning and Delivery:
Smart Cities and the Quintuple Aim. The Proceedings
of the International Conference on Smart City
Applications, 237–251.
Badr, N. G., Carrubbo, L., Ruberto, M., & others. (2021).
Responding to COVID-19: Potential Hospital-at-Home
Solutions to Re-configure the Healthcare Service
Ecosystem. HEALTHINF, 344–351.
Badr, N. G., Dragoicea, M., & Crihana, I. (2020). What do
we know about renewable knowledge and sustainable
societal growth? A scoping review. 17th Conference of
KMIS 2025 - 17th International Conference on Knowledge Management and Information Systems
338

the Italian Chapter of AIS (Association for Information
Systems).
Bundi, D. G., Mutua, S., & Karume, S. (2023). A review of
distributed ledger technologies application in medical
systems interoperability. African Journal of Science,
Technology and Social Sciences, 2(2), 1–11.
Christidis, K., & Devetsikiotis, M. (2016). Blockchains and
Smart Contracts for the Internet of Things. IEEE
Access, 4, 2292–2303. https://doi.org/10.1109/access.
2016.2566339
Davenport, T. H., & Kirby, J. (2016). Only humans need
apply: Winners and losers in the age of smart machines
(Vol. 1). Harper Business New York.
DeFranco, J. F., Roberts, J., Ferraiolo, D., & Compton, D.
C. (2024). An infrastructure for secure data sharing: A
clinical data implementation. JAMIA Open, 7(2),
ooae040.
Dennehy, D., Griva, A., Pouloudi, N., Dwivedi, Y. K.,
Mäntymäki, M., & Pappas, I. O. (2023). Artificial
intelligence (AI) and information systems: Perspectives
to responsible AI. Information Systems Frontiers,
25(1), 1–7.
Drosatos, G., & Kaldoudi, E. (2019). Blockchain
applications in the biomedical domain: A scoping
review. Computational and Structural Biotechnology
Journal, 17, 229–240.
Easterling, D., Perry, A. C., Woodside, R., Patel, T., &
Gesell, S. B. (2022). Clarifying the concept of a
learning health system for healthcare delivery
organizations: Implications from a qualitative analysis
of the scientific literature. Learning Health Systems,
6(2), e10287.
Ferraiolo, D. F., Defranco, J. F., Kuhn, D. R., & Roberts, J.
(2021). A New Approach to Data Sharing and
Distributed Ledger Technology: A Clinical Trial Use
Case. IEEE Netw., 35(1), 4–5.
Florio, M. (2019). Investing in science: Social cost-benefit
analysis of research infrastructures. Mit Press.
Gheibi, O., Weyns, D., & Quin, F. (2021). Applying
machine learning in self-adaptive systems: A
systematic literature review. ACM Transactions on
Autonomous and Adaptive Systems (TAAS), 15(3), 1–
37.
König, L., & Neumaier, S. (2023). Building a Knowledge
Graph of Distributed Ledger Technologies. arXiv
Preprint arXiv:2303.16528.
Markus, A. F., Kors, J. A., & Rijnbeek, P. R. (2021). The
role of explainability in creating trustworthy artificial
intelligence for health care: A comprehensive survey of
the terminology, design choices, and evaluation
strategies. Journal of Biomedical Informatics, 113,
103655.
Mutashar, M. K. (2024). Navigating ethics in AI-driven
translation for a human-centric future. Academia Open,
9(2), 10–21070.
Nilsson, J., Javed, S., Albertsson, K., Delsing, J., Liwicki,
M., & Sandin, F. (2024). Ai concepts for system of
systems dynamic interoperability. Sensors, 24(9), 2921.
Pandl, K. D., Thiebes, S., Schmidt-Kraepelin, M., &
Sunyaev, A. (2020). On the Convergence of Artificial
Intelligence and Distributed Ledger Technology: A
Scoping Review and Future Research Agenda (No.
arXiv:2001.11017). arXiv. https://doi.org/10.48550/
arXiv.2001.11017
Plenk, M., Levant, I., & Bellon, N. (2019). How technology
(or distributed ledger technology and algorithms like
deep learning and machine learning) can help to comply
with regulatory requirements. In The impact of digital
transformation and FinTech on the finance
professional (pp. 241–258). Springer.
Rauchs, M., Glidden, A., Gordon, B., Pieters, G. C.,
Recanatini, M., Rostand, F., Vagneur, K., & Zhang, B.
Z. (2018). Distributed ledger technology systems: A
conceptual framework. Available at SSRN 3230013.
Russell, S. J., & Norvig, P. (2021). Artificial Intelligence:
A Modern Approach, Global Edition 4e.
Samek, W., Wiegand, T., & Müller, K.-R. (2017).
Explainable artificial intelligence: Understanding,
visualizing and interpreting deep learning models.
arXiv Preprint arXiv:1708.08296.
Sterne, J., & Davenport, T. H. (2024). A brief history and
the future of customer data. Applied Marketing
Analytics, 10(3), 194–204.
Taherdoost, H., & Madanchian, M. (2023). Artificial
intelligence and knowledge management: Impacts,
benefits, and implementation. Computers, 12(4), 72.
Tenenbaum, J. D. (2024). Accelerating a learning public
health system: Opportunities, obstacles, and a call to
action. Learning Health Systems, 8(4), e10449.
Vadari, S., & Desik, P. A. (2021). The role of AI/ML in
enhancing knowledge management systems. IUP
Journal of Knowledge Management, 19(2), 7–31.
Yano, E. M., Resnick, A., Gluck, M., Kwon, H., & Mistry,
K. B. (2021). Accelerating learning healthcare system
development through embedded research: Career
trajectories, training needs, and strategies for managing
and supporting embedded researchers. Healthcare,
8,
100479.
Zaarour, T., Khalid, A., Pradeep, P., & Zahran, A. (2024).
Using Distributed Ledgers To Build Knowledge
Graphs For Decentralized Computing Ecosystems.
Proceedings of the 33rd ACM International Conference
on Information and Knowledge Management, 3083–
3092.
Zhang, D., Xia, B., Liu, Y., Xu, X., Hoang, T., Xing, Z.,
Staples, M., Lu, Q., & Zhu, L. (2024). Privacy and
copyright protection in generative AI: A lifecycle
perspective. Proceedings of the IEEE/ACM 3rd
International Conference on AI Engineering-Software
Engineering for AI, 92–97.
Zheng, Z., Xie, S., Dai, H., Chen, X., & Wang, H. (2017).
An overview of blockchain technology: Architecture,
consensus, and future trends. 2017 IEEE International
Congress on Big Data (BigData Congress), 557–564.
Towards a Systemic Approach to Knowledge Integration in Learning Health Ecosystems: AI and DLT Perspectives
339
