
A Predictive Approach for Healthcare Expenditure Using Ensemble
Techniques
Syed Musharaf, Sripathi Srujan Kumar, B Maruthi Reddy and Bidyutlata Sahoo
Department of CSE(AI&ML), Institute of Aeronautical Engineering, Dundigal, Hyderabad, Telangana, India
Keywords: Healthcare, Ensemble Techniques, Regression Algorithms, Decision Making, XBG Regressor.
Abstract: Accurate estimates of healthcare expenses are necessary due to the rising cost of healthcare brought on by the
advent of new viruses and other health issues. These forecasts are essential for individuals and insurance
providers to make educated decisions and plan for future medical requirements. Because of the exponential
expansion of data and the complexity of computations involved, traditional methods of evaluating health
insurance prices have become increasingly insufficient and frequently inaccurate. The objectives of this
research are to determine the most accurate ensemble technique for forecasting changes in healthcare
spending, assess the effectiveness of ensemble approaches in comparison to traditional models, and help
prospective purchasers of medical insurance choose plans that best suit their individual requirements.Through
rigorous experimentation and analysis, several regression algorithms, including KNN Regressor, Linear
Regressor, Random Forest, Decision Tree, and XGB Regressor, were assessed for their predictive
performance. Among these, the most successful performance was XGB Regressor, with an astounding
accuracy of 89.7%. This result highlights the algorithm's robustness and effectiveness in handling the
complexity inherent in healthcare expenditure prediction.
1 INTRODUCTION
Digital health is a field that is expanding rapidly on a
worldwide scale. (Sudhir, Biswajit , Dolly, &
Manomitha, 2022) Internationally, the number of
digital health businesses has increased during the
previous five years. In developed countries, there are
two major challenges to health insurance: rising
health care costs and a rise in the uninsured
population. Medical insurance is a vital part of the
medical sector. On the other hand, because patients
with uncommon illnesses account for most of the
medical cost, it is difficult to forecast spending.
Numerous ML algorithms and deep learning
approaches are used for data prediction. The factors
of training time and accuracy are looked at. The bulk
of machine learning algorithms only require a brief
time of training. However, the prediction results from
these techniques are not particularly accurate.
Deep learning models can also find hidden
patterns, but their usage in real-time is constrained by
the training period. (Nithya & Dr. V. Ilango, 2017)
Regression models such as Linear Regression,
XGBoost Regression, Random Forest Regression,
Decision Tree Regression, KNN Model, Support
Vector Regression, and Gradient Boosting
Regression can all be used and used in this study. This
study's main goal is to present a novel approach for
accurately forecasting healthcare expenses.
2 LITERATURE SURVEY
Numerous research in various contexts on the
estimation of healthcare costs have been published in
the medical domain. While there are numerous likely
assumptions in machine learning, its effectiveness
depends on selecting an almost exact method for the
given problem domain and adhering to the right
protocols for model construction, training, and
deployment.(Sudhir, Biswajit , Dolly, & Manomitha,
2022) In order to predict health insurance prices based
on certain attribute values observed in the dataset, a
number of machine learning regression models were
used in this study.
As part of the technique, a dataset containing
pertinent characteristics like age, BMI, and smoking
status is gathered. Missing value management, feature
normalization, and categorical variable encoding are
examples of preprocessing procedures. Training and
Musharaf, S., Kumar, S. S., Reddy, B. M. and Sahoo, B.
A Predictive Approach for Healthcare Expenditure Using Ensemble Techniques.
DOI: 10.5220/0013586300004664
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 3rd International Conference on Futuristic Technology (INCOFT 2025) - Volume 2, pages 41-48
ISBN: 978-989-758-763-4
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
41

testing sets of the data are created, with noteworthy
features selected. After training several regression
models, Polynomial Regression reduces residual error
by fitting a curve to the data, resulting in the best
accuracy of 80.97%. (Nithya & Dr. V. Ilango, 2017)
Six different classification algorithms were used in
combination to predict which beneficiaries' inpatient
claim amounts increased in 2008 and 2009.
Using the test dataset, the results showed 80%
sensitivity, 77.56% overall accuracy, and 76.46%
precision, the model proved to be useful in helping
high-risk patients select the best insurance plan and in
properly estimating cost and revenue for insurance
providers.(A. Tike & S. Tavarageri, 2017) Utilizing
Medicare payment data, a medical price prediction
system was developed to help patients identify less
expensive medical providers. The authors present a
brand-new hierarchical decision tree method for
estimating prices.
Several experiments are conducted to compare
this method against several machine learning
techniques, including linear regression, Random
Forests, and gradient-boosted trees, and the results
demonstrate that the hierarchical decision tree
achieves a high accuracy. (M Mohammed Hanafy &
Omar M.A. Mahmoud, 2021)This study demonstrates
how insurance premiums can be predicted using a
variety of regression models. They also compared the
results of several other models, such as the DNN,
Random Forest Regressor, Support Vector Machine,
XGBoost, CART, Randomized Additive Model, and
k-Nearest Neighbors.
The stochastic gradient boosting model, which
produces an R-squared value of 84.8295, an MAE of
0.17448, and an RMSE of 0.38018, is found to be the
most successful model. (Hossen, 2023) In this
research, they anticipate insurance amounts for
different groups of people using both individual and
local health data. The effectiveness of these
techniques was investigated using nine regression
models: Linear Regression, XGBoost Regression,
Gradient Boosting, KNN Model, Random Forest
Regression, Ridge Regression, Lasso Regression,
Decision Tree Regression, and Support Vector
Regression. (Lahiri & N. Agarwal, 2014) They use
about 114,000 beneficiaries and over 12,400
attributes in publicly available Medicare data. It
solved the problem of accurately predicting which
customers' inpatient claim amounts increased
between 2008 and 2009 by using six different
classification algorithms.
The study predicts which beneficiaries inpatient
claim amounts grew from 2008 to 2009 using publicly
available Medicare data with over 114,000
beneficiaries and 12,400 attributes. Employing an
ensemble of six classification techniques, it obtains an
overall accuracy of 77.56%, a precision of 76.46%,
and a sensitivity of 80% with the test dataset.
(Gregori, et al., 2011) After being introduced,
regression techniques suitable for healthcare cost
analysis were applied in two experimental settings:
hospital care for diabetes and cardiovascular
treatment (the COSTAMI trial). The study presents
regression approaches created especially for
healthcare cost analysis.
These techniques are applied in observational
settings (diabetes hospital care) as well as
experimental ones (the COSTAMI trial in
cardiovascular treatment). (Bertsimas, et al., 2008)
This study investigates data mining techniques, which
are a potent tool for estimating health-care expenses
and offer precise estimates of medical costs.
In order to predict medical costs, the study used
data-mining techniques. It evaluates their accuracy in
two contexts: observational (diabetic hospital care)
and experimental (COSTAMI research in
cardiovascular medicine). The study looks at the
value of medical data in predicting costs, especially
for high-priced members, and emphasizes the
predictive ability of past cost trends. (Mukund
Kulkarni, et al., 2022) This work uses a range of
machine learning regression models on a personal
medical cost dataset to anticipate health insurance
costs based on certain features.
Regression models including gradient boosting,
polynomial, decision tree, random forest, multiple
linear, and other regression models are studied in this
work. All the models are trained on a subset of the
dataset, and their performance is evaluated using
metrics such as root mean square error (RMSE), mean
absolute error (MAE), and accuracy. (Sahu Ajay,
Sharma Gopal, Kaushik Janvi, Agarwal Kajal, &
Singh Devendra, 2023) “With a score of 85.776%, it
was discovered that Gradient Boosting Decision Tree
Regression had the best accuracy rate for estimating
the amount. Although around 80% of the time, both
random forest and linear regression could produce
accurate forecasts.
3 DESIGN AND PRINCIPLE OF
MODEL
3.1 METHODOLOGY
Using ensemble learning approaches, we created a
predictive model for healthcare spending in this study. To
INCOFT 2025 - International Conference on Futuristic Technology
42
improve prediction accuracy, we used the XGB Regressor,
Decision Tree, Random Forest, KNN Regressor, and Linear
Regression algorithms. This was a reliable and scalable
approach. In order to maximize model performance, our
method included preprocessing the dataset, which included
addressing missing values and scaling features, and then
hyperparameter tweaking. To ensure generalizability, cross-
validation techniques were used during the model's training
and evaluation process on historical healthcare expenditure
data. Important performance indicators including RMSE
and MAE were used to evaluate how well the model
predicted future healthcare expenses.
3.1.1 Data Source Description
The healthcare expenditure dataset that is used is
sourced from KAGGLE’s repository. (Medical Cost
Personal Datasets, 2018) There are 1338 rows and
seven properties or features in the collected data set;
Three of the seven characteristics or traits have
categorical values, and the remaining four have
numerical values. Next, the data set is split into two
parts. Subsequently, the dataset is divided in half. For
the first and second components, respectively, the
words "training data" and "test data" are used.
Predictions made by the model will be more accurate
the more data it obtains throughout its training process
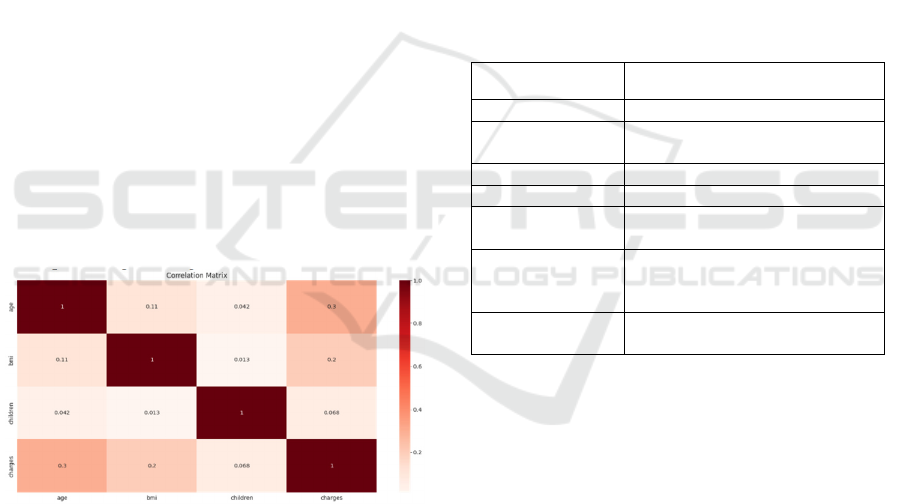
on unknown data. Figure 1 displays the dataset's
correlation matrix. Models are evaluated using test
sets, while health insurance cost prediction models are
developed using training datasets.
Figure 1: Correlation Matrix of Dataset.
A few fields in the dataset had missing values.
Examining the distributions led to the conclusion that
new attributes should be used to replace the missing
variables, which implies that some data may be
missing. The missing data mechanism must first
choose the best approach to analyse the data because
this is only possible if the data is lost completely at
random.
3.1.2 Exploratory Data Analysis(EDA)
Using EDA, the dataset is quickly analysed to look for
any hidden patterns, spot abnormalities, confirm
assumptions, and test ideas. The data obtained from
EDA aids in selecting suitable machine learning
techniques to address the required challenge. Several
kinds of columns that are present in the data are
discovered after conducting an exploratory data
analysis on the entire data set.
3.1.3 Preprocessing and Feature
Engineering
The dataset has seven variables, as (Sudhir, Biswajit ,
Dolly, & Manomitha, 2022) Table 1 illustrates. The
objective variable, the cost of a customer's charges, is
determined by taking into consideration the values of
the remaining six variables.
Table 1: Dataset.
Name Description
Age Customer’s age
BMI Body mass index of the
custome
r
Number of kids Total number of children
Gende
r
Male/Female
Smoker Whether the customer is smoker
or not.
Region Where the person lives:
southwest, southeast, northeast,
northwest
Charges (target
variable
)
Medical charges the customer
has to
p
a
y
Reviewing the data, accurately rebuilding it, and
using machine learning techniques are all part of this
step. The dataset was first checked for any missing
values. It was found that the dataset contained missing
values in the BMI and charges columns. The missing
values were imputed using the relevant attribute
values' mean values.
One-Hot encoder is used to encode the categorical
columns and impute the null values. This process
involves preparing the training, testing, and validation
sets.
3.1.4 Machine Learning Model Selection
KNN Regressor
To forecast a person's healthcare expenses, one
machine learning technique used is the K-Nearest
Neighbors (KNN) Regressor. After the dataset is
prepared, this is trained on the pre-made training set
A Predictive Approach for Healthcare Expenditure Using Ensemble Techniques
43

to encode categorical variables and normalize
numerical features. The best 'k' value is found by
averaging the costs of the nearest neighbors in the
feature space, and this value is used by the model to
anticipate healthcare spending using cross-validation.
Utilizing the KNN Regressor's ability to spot
minute patterns and relationships in the data, this
technique provides a benchmark to be utilized in
conjunction with other ensemble approaches like
XGBoost and Random Forest Regressor. Prior to
hyperparameter change, the KNN model's loss
function is ascertained by performance metrics such
as Mean Absolute Error, Mean Square Error, and
Root Mean Squared Error. We saw that after
calculating these measures, the model's loss for
testing data was roughly 8494, but its RMSE for
validation data was roughly 9862. This means that by
adjusting the hyperparameters, we may make our
model better.
The following hyperparameters were tuned for the
KNN model:
• n neighbors
• weights
• leaf size
Upon finalizing the hyperparameter for leaf size,
the minimum RMSE training error is 9734.15 at leaf
size of 50, whereas the minimum RMSE validation
error is 9789.20 at leaf size of 10. Thus, we adjusted
our model so that the leaf size is 10. Consequently,
after adjusting the hyperparameter, we obtained the
following values: leaf size = 10, weights = "uniform,"
and n neighbors = 11. This contributes to the KNN
regressor's optimal performance.
The estimated RMSE is incredibly high,
indicating that the model performs horribly on the test
data. Thus, in order to improve accuracy and lower
loss/error, we will train our model using various
regression models.
Linear Regressor.
The cost of individual healthcare is predicted using the
Linear Regression model. Once the training dataset
has been processed through a series of data
preprocessing steps, such as normalizing numerical
features and encoding categorical variables, the
trained linear regression model is used. The objective
of this model is to create a linear relationship between
the goal variable (healthcare costs) and the input
parameters (such as age, BMI, smoking status, and
region).
The Linear Regression model fits a straight line to
the data that minimizes the sum of squared errors to
get an easy-to-understand estimate of healthcare
expenditures. This model can be used as a benchmark
for more intricate ensemble techniques such as
XGBoost and Random Forest Regressor.
When we calculated the linear regression model's
loss function, we found that it had a far lower RMSE
than the KNN model for both training and validation
data. To see if it performs any better, we adjusted its
hyperparameters.The following hyperparameter were
tuned for Linear Regression Model:
• normalize
• fit intercept
We left the hyperparameters at their default values
because, even after fine-tuning them, the model is not
influenced by the adjustments. This model performs
noticeably better than the Knn Model, as evidenced
by the noticeably greater RMSE of the Knn Model on
the testing data.
Decision Tree.
In order to forecast healthcare expenses based on
different individual attributes, the Decision Tree
Regressor is used. The Decision Tree model is trained
on the training data after the data has been pre-
processed to allow for categorical variables and scale
numerical features. This model iteratively splits the
data into subsets based on the characteristic that
decreases variance the maximum, resulting in a
structure that resembles a tree. The decisions made
based on attributes are represented by each node in the
tree, while the expected expenses of healthcare are
represented by the leaves. The decision tree model has
been found to be entirely overfit to the training set. In
order to lessen overfitting on our model, we thus
carried out hyperparameter adjustment in the
following stage.
The following hyperparameters were tuned for the
Decision tree model:
• max-depth
• max-leaf-nodes
When max-leaf-nodes = 8, the training and
validation sets produce the greatest results when the
max leaf node's hyperparameters are tweaked. This is
the way the model is adjusted.
Because of this, the decision tree regression model
has outperformed the linear regression model. To
explore whether we may obtain better outcomes, we
nevertheless evaluated our data using two more
models.
Random Forest Regressor.
One essential technique for predictive modelling is
Random Forest. First off, it makes reliable data
preprocessing easier by handling missing values and
categorical variables well, which expedites the
production of the dataset. In the modelling stage,
INCOFT 2025 - International Conference on Futuristic Technology
44
Random Forest's intrinsic capacity to compute feature
relevance helps it find critical features that impact
healthcare forecasts, like patient demographics and
medical history. The group of decision trees in
Random Forest then uses the combined predictive
capability of several trees to improve accuracy and
robustness when predicting healthcare outcomes,
such as patient costs or illness progression.
In addition to enhancing prediction stability, this
ensemble approach allows for thorough model
evaluation, guaranteeing that the forecasts are
accurate and suitably in line with the demands of
healthcare planning and resource allocation. It is
highly likely that the training data will cause this
model to overfit. Hyperparameter tunning is thus
carried out.
The following hyperparameters were tuned for the
random forest regressor:
• n-estimators
• max-depth
• max-leaf-nodes
Max-Leaf-Nodes is set to None by default,
meaning that there can be an infinite number of nodes.
As a result, when max leaf nodes = 16, the model's
training and validation RMSE is at its lowest. We thus
adjusted our model in that manner. In comparison to
the decision tree model, this has done even better. To
check if we could make any more accurate
predictions, however, we tested our data using an
XGBRegressor.
Gradient Boosting Machines (XGBRegressor).
In order to handle complicated interactions in
healthcare data and improve predictive accuracy, the
XGBRegressor (Extreme Gradient Boosting
Regressor) is essential. XGBoost is used because of
its capacity to create a sequence of decision trees one
after the other. These trees learn from each other's
mistakes and improve predictions one iteratively.
First, by determining and ranking the most important
variables for healthcare predictions—such as patient
demographics, medical history, and environmental
factors—XGBoost performs exceptionally well in
feature selection and dimensionality reduction.
Gradient boosting, in which each new tree
concentrates on the residual mistakes of the preceding
ones, successfully increases predictive precision, is
how it enhances the performance of the model during
training.
Furthermore, because of its robustness against
overfitting and capacity to handle big datasets with
high dimensionality, XGBoost is particularly well-
suited for projecting healthcare costs and illness
outcomes. This guarantees that the model not only
produces accurate predictions but also improves
decision-making processes in healthcare planning and
resource allocation. Looking at the RMSE of training
and validation data suggests that the model may have
been overfit using the training set. Therefore, we
adjusted the model's hyperparameters to lessen
overfitting.
The following hyperparameters were tuned for the
Gradient Boosting Machine:
• max-depth
• max-leaf-nodes
• n-estimators
• booster
• min-child-weight
When the max depth hyperparameter is set to 2,
the model operates at its peak efficiency. Changing
the value of the hyperparameter max-leaf-nodes has
no effect on the model when it comes to tuning. In
contrast, the model performs best on both the training
and validation sets when n estimators equal 100 when
tuned with n-estimator hyperparameters. Finally,
when max-child-weight = 94 is selected as the
hyperparameter for minimum child weight, the model
performs best on the training and validation sets. We
thus adjusted our model in that manner.
Thus, we observed that XGBRegressor model
has the best performance on the testing data.
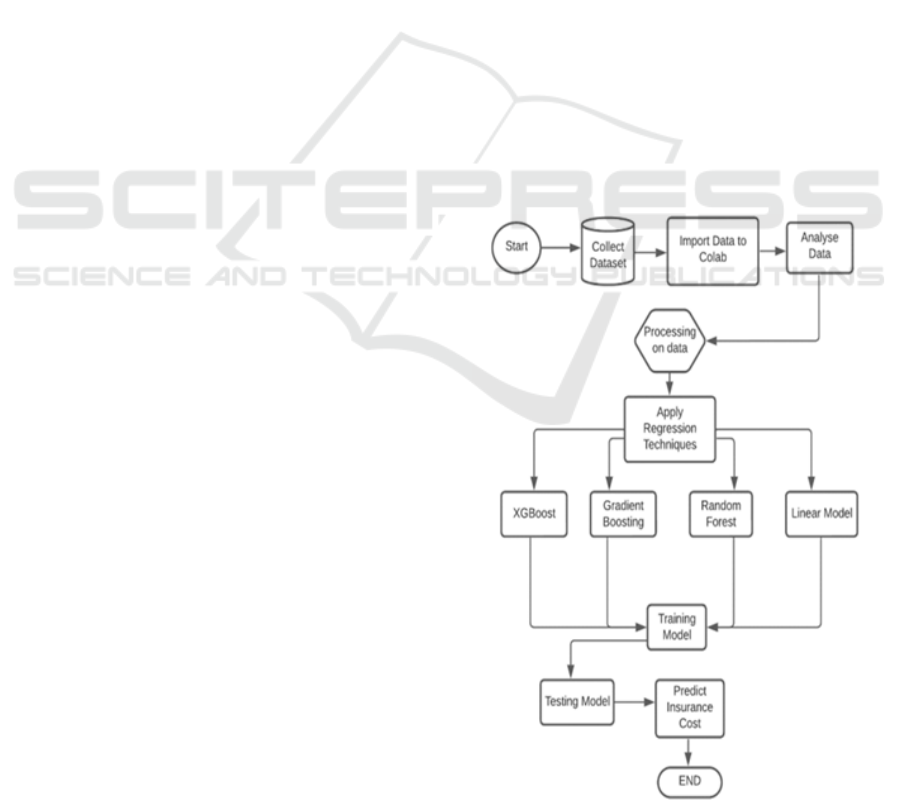
Figure 2: Flowchart of Model.
A Predictive Approach for Healthcare Expenditure Using Ensemble Techniques
45
4 RESULTS AND DISCUSSION
4.1 Experimentation Results
The performance of the model is evaluated using
the following metrics:
𝑅
Score
Root Mean Square Error (RMSE)
𝑅
Score: It is a useful indicator to evaluate the
fitness of the model. The R-squared number ranges
from 0% to 100%, or 0 to 1. A greater number denotes
a better match.
𝑅
=1 − 𝑆𝑆𝐸/𝑆𝑆𝑇
The total squared residuals, or squared deviations
from each observation's predicted value, is known as
the SSE (Squared Sum of Error).
∑
(𝑦
−𝑦
∗
)
.
Sum of Squared Total, or SST, is the squared
deviations of each observation from the mean for the
whole sample.
∑
(𝑦
−ŷ)
.
RMSE: The Root Mean Square error is a
commonly used method to estimate a model's
prediction error. It shows the model's absolute fit to
the data points and shows how close the observed data
points are to the model's projected values. A better
match is indicated by lower RMSE values. The
accuracy of the basis paper model as calculated using
these metrics is shown in (Sudhir, Biswajit , Dolly, &
Manomitha, 2022) Table 2.
RMSE =
∑
(
∗
)
Table 2: Base Paper Results.
Model R2_Score RMSE Accuracy(in
%)
Simple
Linear
Regression
0.62 7523.98 62.86
Multiple
Linear
Regression
0.75 7523.98 75.86
Polynomial
Regression
0.80 5100.53 80.97
Ridge
Regression
0.75 6070.80 75.82
Lasso
Regression
0.75 6066.31 75.86
Table 3: Calculated Results.
Model R2_Score RMSE Accuracy(in
%)
KNN
Re
g
resso
r
0.1966 12150.10 19.66
Linear
Regresso
r
0.8057 5975.16 80.57
Decision
Tree
Re
g
resso
r
0.8905 4485.31 89.05
Random
Forest
Re
g
resso
r
0.8995 4297.03 89.95
XGB
Re
g
resso
r
0.89.72 4345.61 89.72
Following model testing on the test dataset, the
results of the previously stated models were recorded.
Table 3 shows the accuracy, RSME, and R² metrics
for the model that has been covered thus far. Figure.
2 depicts how this model operates.
4.2 Observations
When compared to other models, the KNN
Regressor performs noticeably worse. The R2 value
of 0.1966 indicates a weak link between the input
features and anticipated healthcare spending,
explaining only 19.66% of the dataset's variation.
Since there appears to be a significant mistake in the
forecasts, the RMSE of 12,150.10 renders it
unreliable for precise forecasting. The model's
19.66% accuracy shows its limitations, which are
probably brought on by the dataset's high
dimensionality and complexity, which the KNN
algorithm finds difficult to handle. KNN is not
appropriate for forecasting healthcare spending in this
situation due to its subpar performance.
With a R² value of 0.8057, the Linear Regression
model shows a considerable improvement over the
KNN, accounting for around 80.57% of the data's
variance. The model successfully captures important
patterns between characteristics and the target
variable, as evidenced by this strong linear
relationship. With a reduced error and an RMSE of
5975.16, it is evident that it can produce predictions
that are more dependable than KNN. Although it still
lacks the predictive precision and adaptability of more
complex models like Decision Trees and Random
Forests, the model's 80.57% accuracy makes it a
useful baseline for comparison.
With an R² score of 0.8905, the Decision Tree
Regressor outperforms the other models, accounting
for 89.05% of the variance and indicating that it can
handle more intricate, non-linear interactions in the
INCOFT 2025 - International Conference on Futuristic Technology
46

dataset. The RMSE of 4485.31, which is significantly
less than that of linear regression, indicates improved
prediction accuracy. The Decision Tree model is
highly competitive with an accuracy of 89.05%.
The highest performance is the Random Forest
Regressor, which explains 89.95% of the variation in
the data with an R² value of 0.8995. With the lowest
RMSE of 4297.03 out of all the models, this one
makes the most accurate forecasts. With an accuracy
of 89.95%, Random Forest is clearly the best model
in terms of precision and generalization. This is partly
because Random Forest is an ensemble model, which
minimizes overfitting and increases robustness across
various data patterns.
Strong performance is also obtained by the
XGBoost Regressor, which rivals Random Forest
closely with an R2 score of 0.8972, explaining
89.72% of the variance. Although it has a little larger
RMSE of 4345.61 than Random Forest, it
nevertheless exhibits very excellent prediction
accuracy. The 89.72% accuracy rate confirms
XGBoost's potency as a prediction model especially
for intricate datasets. It is almost as good as Random
Forest in this situation because it can reduce bias and
variation using gradient boosting techniques.
The best models for forecasting healthcare costs
are Random Forest and XGBoost, which have the
lowest error and the highest accuracy. While KNN
performs poorly, Linear Regression provides a solid
baseline but lacks the accuracy of the ensemble
models. Although it may be prone to overfitting, the
Decision Tree Regressor produces results that are
competitive. In general, the best methods for this
forecasting task are ensemble models such as Random
Forest and XGBoost.
With an accuracy rate of 89.7%, XGBoost's
exceptional performance highlights its applicability
for challenging predictive tasks in the analysis of
healthcare spending. It differs from conventional
regression techniques in that it can handle big datasets
with high dimensionality, find important predictors,
and improve model performance through repeated
refining. Accurate spending forecasts are essential for
optimizing budget allocation, boosting operational
efficiency, and improving patient care in healthcare
planning and resource allocation. Healthcare
providers can improve overall healthcare
management and service delivery by using ensemble
approaches like XGBoost to make well-informed
decisions based on dependable prediction insights.
5 CONCLUSIONS
This study set out to precisely forecast healthcare
costs through the application of multiple ensemble
learning strategies. Several algorithms, such as the
KNN Regressor, Linear Regressor, Random Forest,
Decision Tree, and XGBRegressor, were assessed
based on their prediction accuracy through thorough
testing and analysis. XGBRegressor stood up as the
best performance among all, attaining an astounding
accuracy of 89.7%. This outcome demonstrates how
well the algorithm handles the complexity involved in
predicting healthcare expenses.
The ability of ensemble learning methods, in
particular Random Forest and XGBoost, to estimate
healthcare costs with low error margins and high
accuracy. These models perform better than more
straightforward algorithms like KNN and Linear
Regression, which are helpful as baselines but fall
short in capturing the intricacy of the data. Because
ensemble approaches reduce variation and bias, they
are essential for producing accurate forecasts. This
method offers a strong foundation for predicting
healthcare expenditures, which is essential for
budgeting, resource allocation, and policy planning in
the healthcare industry. It does this by utilizing
historical data and cutting-edge machine learning
algorithms. Predictive healthcare analytics can
benefit greatly from additional improvements made
through feature engineering, deep learning
integration, and real-time data application, which can
result in even more accurate and flexible models.
Future research can go in a number of ways to
improve the machine learning models' ability to
anticipate healthcare costs. First, the accuracy of the
forecasts could be increased by adding more features,
like lifestyle indicators, geographic location, and
socioeconomic aspects. In order to capture patterns
and seasonality in healthcare expenses over time,
time-series analysis could be used to enhance the
present model to include temporal elements.
Investigating deep learning methods like neural
networks, which have the potential to identify more
intricate patterns in the data that conventional
machine learning models might overlook, is another
exciting direction. To strike a compromise between
interpretability and accuracy, hybrid models that use
both machine learning and deep learning techniques
could potentially be investigated.
To further enhance performance, automatic
hyperparameter tuning utilizing methods like grid
search or Bayesian optimization might be applied to
the present models. Better understanding model
decisions would also benefit from the application of
A Predictive Approach for Healthcare Expenditure Using Ensemble Techniques
47

explainable AI (XAI) techniques, particularly in a
delicate industry like healthcare where openness is
essential.
Furthermore, moving to real-time predictive
analytics may provide managers of healthcare
organizations with timely insights on spending
patterns, allowing them to make responsive changes
to their resource allocation plans. Maintaining the
model's applicability and efficacy in changing
healthcare environments requires ongoing validation
against fresh datasets and collaboration with
healthcare professionals. By seizing these chances,
the initiative can improve patient outcomes, cost
effectiveness, and healthcare management by
advancing predictive analytics in healthcare spending
forecasting.
REFERENCES
A. Tike & S. Tavarageri. (2017). A Medical Pricce
Prediction System using Hierarchical Decision Trees.
IEEE Big Data Conference
Bertsimas, M. V. Bjarnadottir, M. A. Kanre, J. C. Kryder,
R. Pandey, S. Vempala, & G. Wang. (2008).
Algorithmic prediction of healthcare costs. Operations
Research, 56.
Gregori, M. Petrinco, S. Bo, A. Desideri, F. Merletti, & E.
Pagano. (2011). Regression Model for Analyzing costs
and their determinants in healthcare : an introductory
review. International Journal for Quality in Healthcare,
23.
Hossen, S. (2023). Medical Insurance Cost Prediction
Using Machine Learning. Dhaka, Bangladesh.
Lahiri, & N. Agarwal. (2014). Predicting Healthcare
Expenditure Increase for an Individual from Medicare
Data. ACM SIGKDD Workshop on Health Informatics.
M Mohammed Hanafy, & Omar M.A. Mahmoud. (2021).
Predict Health Insurance Cost by using Machine
Learning and DNN Regression Models. International
Journal of Innovative Technology and Exploring
Engineering(IJITEE), 10(3, January).
(2018). Medical Cost Personal Datasets. Kaggle Inc.
Mukund Kulkarni, Dhammadeep D. Meshram, Bhagyesh
Patil, Rahul More, Mridul Sharma, & Pravin Patange.
(2022). Medical Insurance Cost Prediction Using
Machine Learning. International Journal for Research
in Applied Science & Engineering Technology
(IJRASET), 10.
Nithya, B., & Dr. V. Ilango. (2017). Predictive Analytics in
Healthcare Using Machine Learning Tools and
Techniques. International Conference on Intelligent
Computing and Control Systems ICICCS.
Sahu Ajay, Sharma Gopal, Kaushik Janvi, Agarwal Kajal,
& Singh Devendra. (2023). Healtch Insurance Cost
Prediction by Using Machine Learning . International
Conference on Innovation Computing &
Communication (ICICC).
Sudhir, P., Biswajit , P., Dolly, D., & Manomitha, C. (2022).
Health Insurance Cost Prediction Using Regression
Models. Conference on Machine Learning, Big Data,
Cloud and Parallel Computing (COM-IT-CON), May.
INCOFT 2025 - International Conference on Futuristic Technology
48
