
A Proposed Framework for Integrating Digital Triage with 3D Human
Model for Intuitive Health Visualization and Monitoring
Md Jobayer Hossain Chowdhury
a
, Mohamed Mehfoud Bouh
b
, Abdullah Al Noman
c
,
Nadia Binte Rahman Peeya
d
, Shah Manan Vinod
e
, Syed Usama Hussain Shah Bukhari
f
,
Prajat Paul
g
, Forhad Hossain
h
and Ashir Ahmed
i
Faculty of Information Science and Electrical Engineering, Kyushu University, Fukuoka, Japan
Keywords:
Digital Triage, Human Digital Twin, Healthcare Informatics, Electronic Health Records, Health Visualization,
Patient Monitoring, Artificial Intelligence.
Abstract:
This paper presents a novel integration of digital triage protocols with three-dimensional human digital twin
models to enhance patient assessment and clinical decision-making in healthcare. We investigate how Elec-
tronic Health Record (EHR) data can be transformed into intuitive, anatomically-relevant visualizations that
map health parameters to specific body regions using color-coded indicators. Building upon the B-logic
framework from Portable Health Clinic systems, our approach creates personalized 3D patient models that
dynamically represent health status through targeted visual cues—from BMI and vital signs to biomarkers and
lifestyle factors. The system architecture incorporates anthropometric data and facial recognition to generate
individualized avatars, while large language models provide contextual healthcare suggestions based on de-
tected risk factors. This integration addresses limitations in current EHR-based triage systems, particularly
regarding alert effectiveness and protocol compliance. While the system shows potential for enhanced visual-
ization, practical implementation may face challenges in data availability, privacy, and clinical validation. The
proposed visualization methodology offers healthcare providers and patients an intuitive interface for health
monitoring, potentially improving engagement, comprehension, and clinical workflow in both emergency and
routine healthcare settings.
1 INTRODUCTION
Over the past decade, the adoption of Electronic
Health Record (EHR) systems has transformed mod-
ern healthcare delivery. As of 2021, 96% of non-
federal acute care hospitals in the United States had
implemented certified EHR systems, compared to
only 7.6% in 2008 (Office of the National Coordina-
tor for Health Information Technology (ONC), 2021;
a
https://orcid.org/0009-0008-5311-9191
b
https://orcid.org/0000-0002-7716-7007
c
https://orcid.org/0009-0002-5360-8667
d
https://orcid.org/0009-0008-8657-1651
e
https://orcid.org/0009-0004-2398-9795
f
https://orcid.org/0009-0003-2755-9568
g
https://orcid.org/0009-0002-2243-6078
h
https://orcid.org/0000-0002-3593-0860
i
https://orcid.org/0000-0002-8125-471X
Jiang et al., 2023). A global survey by the Organi-
sation for Economic Co-operation and Development
(OECD) across 27 countries revealed that only 15
had achieved nationally unified EHR systems, under-
scoring persistent challenges related to interoperabil-
ity and fragmentation (Slawomirski et al., 2023).
While developed nations are progressively inte-
grating EHR and Electronic Medical Record (EMR)
systems, adoption rates in developing countries re-
main low, ranging from 5% to 30%, primarily due
to limited infrastructure, financial constraints, and the
lack of standardized health data frameworks (Dere-
cho et al., 2024). One key advancement enabled by
EHR systems is digital triage—automated protocols
that prioritize patient care based on clinical urgency.
However, traditional EHR-based alert systems often
suffer from poor protocol compliance, alert fatigue,
and suboptimal visualization interfaces. For instance,
a randomized controlled study showed no significant
Chowdhury, M. J. H., Bouh, M. M., Al Noman, A., Peeya, N. B. R., Vinod, S. M., Bukhari, S. U. H. S., Paul, P., Hossain, F., Ahmed and A.
A Proposed Framework for Integrating Digital Triage with 3D Human Model for Intuitive Health Visualization and Monitoring.
DOI: 10.5220/0013567200003970
In Proceedings of the 15th International Conference on Simulation and Modeling Methodologies, Technologies and Applications (SIMULTECH 2025), pages 329-336
ISBN: 978-989-758-759-7; ISSN: 2184-2841
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)
329

Table 1: Triage System Categories in Healthcare.
Triage Category Implementation Con-
text
Representative Systems Key Characteristics
Emergency Depart-
ment Triage
Emergency Depart-
ments, Pre-Hospital
ESI(Emergency Severity
Index), CTAS(Canadian
Triage and Acuity Scale),
MTS(Manchester Triage Sys-
tem), ATS(Australasian Triage
Scale)
Traditional, rule-based methods that
help prioritize who gets care first.
AI Driven EHR Integration, Tele-
health, AI-Supported
Platforms
HopScore, SERT(System
for Emergency Risk Triage),
TriageGO
Uses AI and machine learning to predict
risk and suggest actions.
Disaster & Mass
Casualty
Emergency Situations,
Pandemic Response
START(Simple Triage and
Rapid Treatment), Jump-
START, Triage Sieve, SAVE
Helps in chaotic events by categorizing
patients.
Specialized Pediatric, Mental
Health
JumpSTART, MHTS ( Mental
Health Triage Scale)
Tailored for specific populations like
children or people with mental health
needs.
improvement in triage compliance through passive
EHR alerts, highlighting the need for more intuitive
and dynamic triage strategies (Holmes et al., 2015).
This paper proposes a framework integrating dig-
ital triage protocols with three-dimensional human
digital twin (HDT) models. By leveraging anthro-
pometric data, facial recognition, and color-coded vi-
sualizations, the system aims to transform structured
EHR data into an anatomically meaningful 3D repre-
sentation. This approach enables healthcare providers
and patients to monitor and understand health risks
more intuitively.
Research Question: How to integrate and visual-
ize medical triage with a 3D human model?
To address this question, the paper introduces
a framework that links B-Logic-based triage from
Portable Health Clinic (PHC) systems with AI-
generated digital avatars. The system also incorpo-
rates large language models (LLMs) to provide per-
sonalized health suggestions based on mapped risk
factors. The proposed methodology targets both
emergency and routine care, particularly in low-
resource settings, offering a potential pathway toward
more accessible and personalized healthcare monitor-
ing.
2 AVAILABLE TRIAGE SYSTEM
AND ITS LIMITATION
In an EHR-integrated triage workflow, clinicians
(often triage nurses) enter a patient’s initial in-
formation—vital signs, symptoms, and chief com-
plaint—directly into a module of the EHR. This dig-
ital form captures key data points and often enforces
required fields to ensure completeness (Aronsky et al.,
2008).
The integration of triage systems within Elec-
tronic Health Record (EHR) platforms represents a
significant advancement in healthcare informatics and
clinical decision support. Multiple triage frameworks
now operate within these digital environments and
can be categorized into four primary classifications
based on implementation context and clinical focus.
Emergency Department Triage systems, such
as the widely adopted Emergency Severity Index
(ESI) (Aronsky et al., 2008; Liu et al., 2022) and
Canadian Triage and Acuity Scale (CTAS) (Office
of the National Coordinator for Health Informa-
tion Technology (ONC), 2021), Australasian Triage
Scale(ATS) (Ebrahimi et al., 2015) , Manchester
Triage System (MTS) (Azeredo et al., 2015) offer
structured protocols used in emergency and urgent
care settings to prioritize treatment based on patient
acuity and resource requirements.
Mass Casualty Incident (MCI) Triage protocols
are specifically designed for disaster scenarios and
large-scale emergencies. Systems such as Simple
Triage and Rapid Treatment (START), JumpSTART
(for pediatric patients), and the Triage Sieve catego-
rize patients using a color-coded classification (im-
mediate/red, delayed/yellow, minor/green, and expec-
tant/black) to optimize resource allocation (Bazyar
et al., 2019; Wang et al., 2022).
Technology-Assisted Triage includes informatics-
driven systems like HopScore (Levin et al., 2018),
the SERT (System for Emergency Risk Triage), and
TriageGO (Johns Hopkins Medicine, 2022), which
utilize artificial intelligence and EHR integration to
predict clinical risk and suggest appropriate care path-
ways in real time.
Specialty Population Triage frameworks are de-
signed for specific groups such as pediatric or men-
SIMULTECH 2025 - 15th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
330

Table 2: B-logic triage system.
Parameter Lower Warning Green Yellow Orange Red Upper Warning
Height (cm) <100.0 >200.0
Weight (kg) <25 >100.0
BMI <25 ≥25 & <30 ≥30 & ≤35 >35
Waist (cm) Male <40.0 <90.0 ≥90.0 NA NA >120.0
Waist (cm) Female <40.0 <80.0 ≥80.0 NA NA >110.0
Hip (cm) <40.0 >120.0
Waist Hip Ratio Male <0.90 ≥0.90 NA NA -
Waist Hip Ratio Female <0.85 ≥0.85 NA NA -
Temperature (C) <33.0 ≥37.0 & <37.5 ≥37.5 NA NA >39.0
HBsAg negative positive
Smoking positive
Urine Sugar - +- Others
Urine Protin - +- Others
Urinary Urobilinogen +- Others
Oxygenation of Blood (%) >100 ≥96 ≥93 & ≤96 ≥90 & <93 <90 <92
Blood Pressure Systolic <70 <130 ≥130 & <140 ≥140 & <180 ≥180 >220
Blood Pressure Diastolic <50 ≤85 ≥85 & <90 ≥90 & <110 ≥110 >140
Blood Sugar (mmol/dl) PBS <3.0 <7.78 ≥7.78 & <11.11 ≥11.11 & <16.67 ≥16.67 >30.0
Blood Sugar (mmol/dl) FBS <3.0 <5.56 ≥5.56 & <7.0 ≥7.0 & <11.11 ≥11.11 >20.0
Blood Hemoglobin (g/dl) >18.0 ≥12.0 ≥10.0 & <12.0 ≥8.0 & <10.0 <8.0 <6.0
Pulse Rate (beats/min) <50 ≥60 & <100 ≥50 & <60 <50 OR ≥120 >130
Arrhythmia Normal Others
Blood Cholesterol (mg/dl) <120.0 ≤200.0 >200.0 & ≤225.0 ≥225.0 & <240.0 ≥240.0 >300.0
Blood Uric Acid (mg/dl) Male <2.5 ≥3.5 & ≤7.0 >7.0 & ≤8.0 ≥8.0 >12.0
Blood Uric Acid (mg/dl) Female <2.5 ≥2.4 & ≤6.0 >6.0 & ≤7.0 ≥7.0 >12.0
tal health patients. These include systems like Jump-
START (Bazyar et al., 2019; Wang et al., 2022)
and the Mental Health Triage Scale (MHTS) (Broad-
bent et al., 2007), which tailor triage protocols to the
unique needs of their respective populations.
The triage systems perform effectively within
their domains, offering structured support for clini-
cal decision-making. However, they face limitations
in patient engagement due to health literacy gaps.
Many patients struggle to interpret medical data and
triage outcomes presented in standard EHR inter-
faces. Moreover, the lack of intuitive, body-mapped
visualizations reduces clarity and makes it harder for
users to understand their health status. These issues
highlight the need for more accessible and patient-
friendly triage solutions.
3 PORTABLE HEALTH CLINIC
AND B-LOGIC
The Portable Health Clinic (PHC), developed by
Kyushu University and Grameen Communications,
delivers telehealth services to underserved rural ar-
eas using a portable briefcase with diagnostic tools.
Health data is sent to a remote call center, where
doctors review EHRs and provide consultations via
telemedicine. A color-coded triage system (green
to red) guides patient prioritization. Integrated
with the PHC, the B-Logic framework uses prede-
fined medical parameters to classify patients by risk
level, enabling efficient diagnosis and resource allo-
cation (Ahmed et al., 2013). table 2 shows the B-logic
triage system.
4 CONCEPT OF 3D
VISUALIZATION OF PHC
TRIAGE SYSTEM
The PHC system collects patient data and stores it in
a database, automatically assigning each patient to a
color-coded triage category. The new proposed sys-
tem will generate a ’patient digital twin’ and use these
data to provide customized suggestions and visual-
izations, allowing individuals to view and understand
their health status through a personalized digital rep-
resentation. In fig. 1, it shows the system architecture
of the proposed system.
4.1 Digital Twin with Real-Time Triage
To make the digital twin with a real-time triage sys-
tem, we need to break it down into two parts.
A Proposed Framework for Integrating Digital Triage with 3D Human Model for Intuitive Health Visualization and Monitoring
331
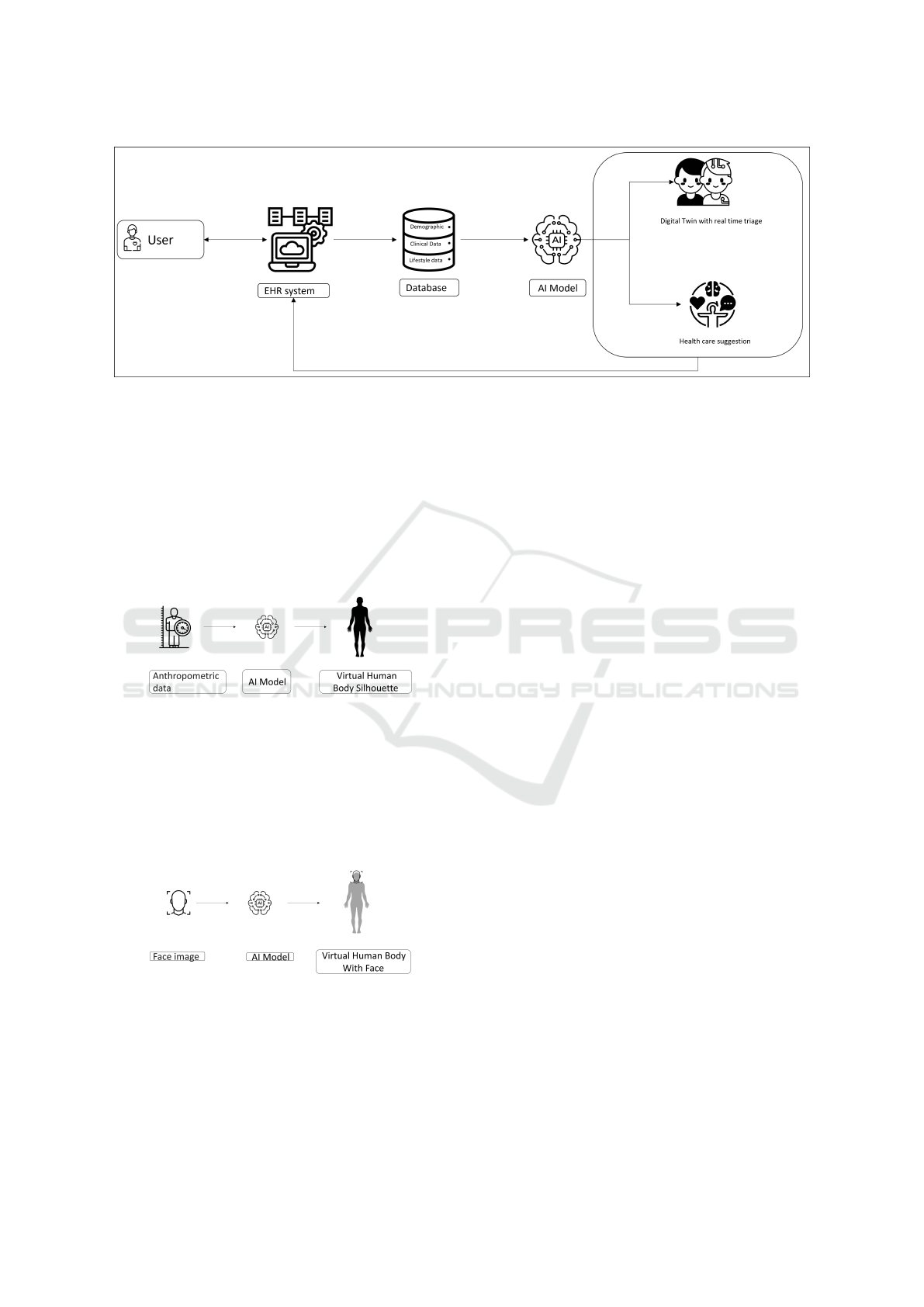
Figure 1: Proposed framework.
4.1.1 Silhouette Estimation from
Anthropometric Data
Almost every EHR system collects the anthropomet-
ric data of a patient, such as height, weight, etc. Also,
PHC has the patient’s anthropometric data. We will
use the data to generate a specific silhouette of the pa-
tient. In fig. 2, it shows how the anthropometric data
will be the input of an AI model that will make the
silhouette of the patient.
Figure 2: Anthropometric data to silhouette structure.
4.1.2 3D Face Construction from Image Data
EHR systems have patient images in their database.
As fig. 3 suggests, the AI model will create a 3D face
based on the image, and the face will merge with the
human silhouette to make a clone of the individual
patient.
Figure 3: User image to 3D face structure.
4.2 Mapping Health Parameters to
Body Parts
The system will map each key health parameter to
a specific body region on the 3D model, indicating
where the effect of that metric is most visible or rele-
vant. Here’s a breakdown of the parameters and how
to visualize them on the body
4.2.1 Height, Weight, BMI (Body Mass Index)
These relate to the overall body. A common approach
is to reflect BMI by the overall silhouette. For in-
stance, the entire figure could be outlined or filled
with a color representing whether the BMI is normal
or high. A green full-body glow for normal BMI, vs.
orange or red if BMI is in overweight/obese range,
immediately signals the category.
4.2.2 Waist, Hip Measurements, and Waist-Hip
Ratio
To emphasize the abdominal and hip region, a col-
ored band can be drawn around the waist or hips of
the model. For instance, a ring or outline at the waist
level may be displayed in green to indicate a healthy
circumference, while red can denote measurements
beyond the risk threshold. Since the waist-to-hip ra-
tio serves as a single risk indicator, the entire mid-
section, including the stomach and hip area, can be
color-coded to reflect risk levels. A high ratio, indica-
tive of central obesity, may be represented by a red-
colored region. This visual mapping enables users to
perceive an expanding red belly when waist size be-
comes a concern. Additionally, a subtle translucent
“slice” or disc around the waist can be incorporated to
display the numeric value of the ratio. A straightfor-
ward approach involves highlighting the torso, partic-
ularly the abdominal area, with severity-based color
coding for waist and hip metrics.
SIMULTECH 2025 - 15th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
332
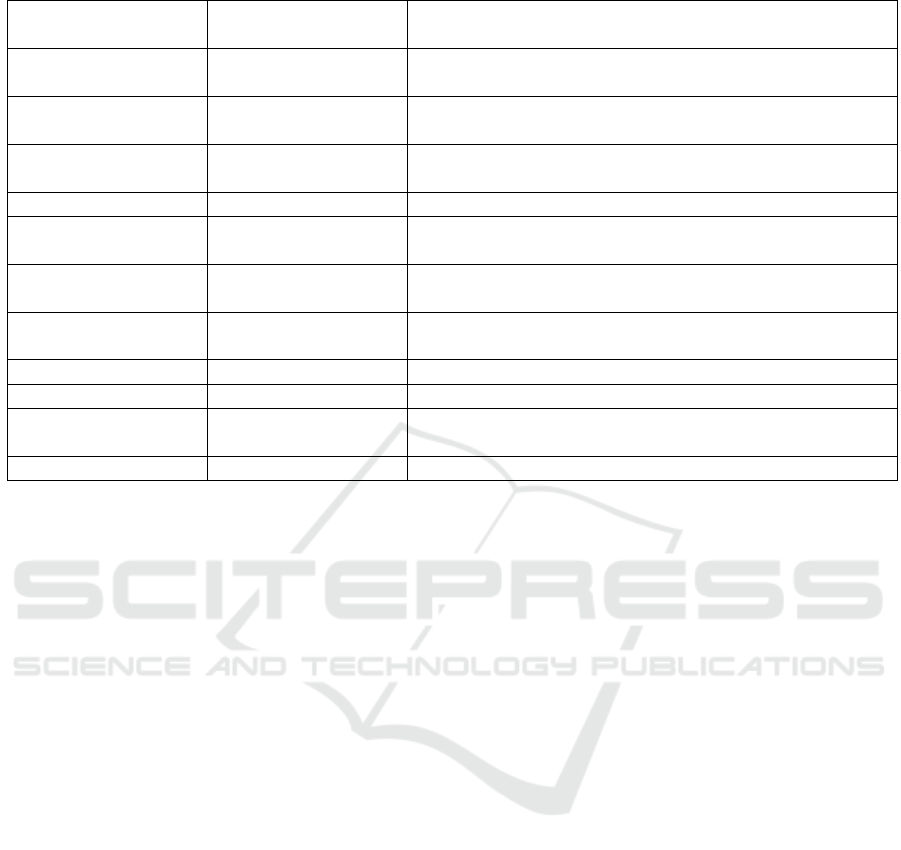
Table 3: Health Parameters Mapping.
Health Parameter Mapped Body Re-
gion
Visualization Approach
Height, Weight, BMI Overall body Color-coded whole body (green/yellow/red for BMI), nu-
meric values for height/weight
Waist, Hip Measure-
ments
Abdomen and hip re-
gion
Colored band around waist/hips, midsection highlighted
based on risk
Body Temperature Forehead, head,
whole body
Heatmap overlay (blue to red gradient), forehead glow
Blood Pressure Arms, chest highlighted arms for BP, heart icon on chest for pulse
Blood Oxygenation
(SpO
2
)
Fingertips,
lungs/chest
Glowing fingertip (green/yellow/red), lung overlay in
color
Blood Sugar (Glu-
cose)
Fingertip, hands,
veins
Hand highlight, blood droplet icon, color-coded veins
Hemoglobin (Hb) Circulatory system Blood vessels colored red (normal) or blue (anemic), pale
skin tone
Cholesterol Heart/chest Heart turns color for cholesterol risk, artery clog icons
Uric Acid Joints (feet, knees) Foot/knee highlights for uric acid buildup
Smoking Lungs, mouth Lungs overlaid with smoky texture or colored (yel-
low/red)
Urine Parameters Kidneys, bladder Kidneys and bladder highlighted, color-coded for risk
4.2.3 Body Temperature
Body temperature is commonly measured at the fore-
head or ear, but fever affects the entire body. An ef-
fective method for visual representation is a heatmap
overlay that spans the entire body. This can be im-
plemented using a gradient shader, where cooler tem-
peratures are represented in blue and elevated tem-
peratures in red. Given that the normal human body
temperature is approximately 37°C, a simplified ap-
proach could involve using green to denote normal
temperature ranges and red to indicate fever. To en-
hance clarity, specific regions, such as the forehead,
can be emphasized using a thermometer icon or a red
glow, aligning with the common practice of forehead-
based temperature checks. Alternatively, the model’s
facial or forehead region can dynamically change
color—retaining a normal skin tone when within the
healthy range and turning flushed red when fever is
detected. If a full-body heatmap is employed, care
should be taken to ensure it does not interfere with
other visual overlays. In such cases, a subtle overall
tint adjustment—such as a slight red hue when fever
is present—can effectively signal an elevated temper-
ature. Given that body temperature is represented as a
single numerical value, a minimalistic approach, such
as a small colored indicator (e.g., a red dot on the fore-
head), may also suffice while maintaining an intuitive
and informative visualization.
4.2.4 Blood Pressure and Pulse Rate
Blood pressure and pulse rate are critical indicators
of circulatory health, typically measured on the arm
and closely associated with cardiovascular function.
To effectively visualize these vitals, a model can
highlight specific anatomical regions where measure-
ments commonly occur. For instance, the upper arm
or wrist—locations used for blood pressure monitor-
ing—can be color-coded to indicate status, with green
representing normal levels and red signaling hyper-
tension. Additionally, an icon of a heart or artery
can be placed on the arm to reinforce the associa-
tion with circulatory health. For pulse rate visual-
ization, an intuitive approach is to use a heart sym-
bol on the chest that dynamically animates to mimic a
beating heart. This icon could change color to reflect
pulse rate abnormalities—red for tachycardia (ele-
vated heart rate) and blue for bradycardia (low heart
rate). Some avatar-based monitoring systems already
implement similar features, where heart icons adjust
color based on real-time vital signs. Since blood
pressure and pulse rate are interrelated, a dual rep-
resentation could enhance clarity: the heart symbol
on the chest can reflect pulse rate through animation
and color changes, while the arm region can indicate
blood pressure status. In cases of severe hypertension,
an extended visualization—such as highlighting the
blood vessel network in red—can effectively convey
cardiovascular strain. Conversely, hypotension or a
dangerously low pulse could be depicted using a blue
A Proposed Framework for Integrating Digital Triage with 3D Human Model for Intuitive Health Visualization and Monitoring
333

tint or a slow pulsating animation. For user interac-
tion, a clickable interface where selecting the arm or
heart symbol provides precise numerical readings of
blood pressure and pulse rate would enhance usabil-
ity. However, even without interaction, a color-coded
system ensures immediate recognition of circulatory
health status at a glance
4.2.5 Blood Oxygenation (SpO
2
)
Blood oxygen saturation (SpO
2
) is a vital parame-
ter typically measured at the fingertip using a pulse
oximeter or inferred from lung function. In a digital
twin, it can be visualized by highlighting the finger-
tip or lungs. A color-coded glow—green (normal),
yellow (moderate), red (low)—can indicate oxygen
levels, with pulsing effects enhancing visibility. For
anatomical context, the lungs may be tinted red to
signal respiratory distress. Combining fingertip and
lung highlights offers intuitive feedback. Interactive
elements, like clicking for exact values, can further
improve user engagement and health monitoring clar-
ity.
4.2.6 Blood Sugar (Glucose)
Blood glucose levels are typically monitored through
finger-prick tests or continuous glucose monitors
(CGMs) placed on the arm. While glucose
metabolism affects the entire body, an effective vi-
sual representation should focus on intuitive indica-
tors, such as the hands (where blood tests occur) or
a blood droplet symbol to signify sugar levels. A
simple and clear method is to highlight the finger-
tip, where traditional glucose tests are performed. A
small droplet icon can be placed on the fingertip,
changing color to reflect blood sugar status: Green for
normal glucose levels Yellow for moderate elevation
Red for high blood sugar (hyperglycemia) For a more
anatomical approach, a vein or artery overlay could
be used to signify blood sugar levels, though this is
a more abstract representation. If the model includes
visible veins, they could subtly change color based on
glucose concentration. However, to maintain clarity
and usability, a color-coded highlight on the hands is
a more direct and intuitive approach. User interac-
tion can be enhanced by allowing the glowing hand to
be clickable, displaying real-time blood sugar read-
ings. In some medical visualization systems, high
blood sugar is represented across multiple organs due
to its long-term effects on areas such as the kidneys,
eyes, and nerves, but this level of detail may be un-
necessary for general use. If an anatomical focus is
preferred, the pancreas (responsible for insulin pro-
duction) could be highlighted, though most lay users
may not immediately recognize its location. Alter-
natively, a small glucose meter icon placed near the
model could provide additional clarity. However, fol-
lowing the established visual scheme, a color-coded
hand region remains the most intuitive and immedi-
ately recognizable indicator of blood sugar status.
4.2.7 Hemoglobin
Hemoglobin (Hb) plays a crucial role in the blood’s
oxygen-carrying capacity, directly influencing cir-
culation and tissue oxygenation. A decrease in
hemoglobin levels, indicative of anemia, may be rep-
resented through visual changes in the circulatory sys-
tem. For instance, if a model includes arteries and
veins, normal hemoglobin levels could be depicted
with bright red vessels, while anemia might be illus-
trated using a dull blue or gray hue. In the absence
of detailed vascular representation, an alternative ap-
proach could involve using a blood drop icon over
the torso or adjusting the overall skin tone—rosy for
normal hemoglobin and pale or bluish for low lev-
els. Given hemoglobin’s impact on energy and oxy-
genation, visual cues such as highlighting the chest
(symbolizing the heart and circulation) or the arm
veins (where blood is commonly drawn for testing)
may enhance interpretability. Maintaining consis-
tency with oxygen-related indicators, such as linking
hemoglobin visualization to the chest or arterial path-
ways, can further reinforce its physiological signifi-
cance.
4.2.8 Cholesterol
Cholesterol and uric acid are distinct physiologi-
cal markers, each associated with specific body sys-
tems. Cholesterol is primarily linked to cardiovascu-
lar health, while uric acid is connected to joint func-
tion, particularly in conditions like gout. To visu-
alize cholesterol levels, the heart or arterial system
can serve as a focal point, with color-coded indi-
cators—such as a red or orange hue—to signify el-
evated cholesterol and potential cardiovascular risk.
Additional elements, such as an artery-clogging icon,
could further reinforce this association. For uric acid,
visualization can be centered on the joints, with a fo-
cus on areas most commonly affected by gout, such
as the big toe, knees, or hands. A practical approach
would be to highlight the foot or toe joint when uric
acid levels are high, as gout frequently manifests in
these areas first. Alternatively, a generic joint icon,
such as a knee, could be used to represent broader
joint-related risks. If highlighting multiple joints
becomes complex, selecting a single representative
joint—such as the knee or foot—provides clarity
SIMULTECH 2025 - 15th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
334

while maintaining effectiveness. A user-interactive
model could allow access to specific details by click-
ing on the heart for cholesterol-related data and the
foot or knee for uric acid levels, ensuring intuitive en-
gagement with the health metrics.
4.2.9 Smoking
Smoking significantly affects lung health and in-
creases disease risk. In the 3D model, this can be
visualized by highlighting the lungs—healthy lungs
appear normal, while smoker’s lungs are tinted gray
or black. A color gradient (green to red) can indicate
smoking intensity. Since it’s a lifestyle factor, a sim-
ple visual toggle or overlay can signal smoking status,
enhancing user awareness of its health impact.
4.2.10 Urine-Related Parameters
Urine-related parameters, such as urine sugar, ke-
tones, and kidney function markers, are closely tied
to the renal system, including the kidneys and blad-
der. A clear visualization of these metrics can be
achieved by mapping them to the anatomical loca-
tions of these organs. The kidneys, positioned in the
lower back, could be highlighted from either the rear
view or subtly shown from the front as faint outlines
on the sides. The bladder, located in the lower ab-
domen, can also serve as a visual indicator for urine-
related issues. Color-coded cues can effectively com-
municate abnormal findings. For instance, healthy
kidneys and bladder could be depicted in green, while
abnormal readings—such as proteinuria or elevated
creatinine—could prompt a shift to orange or red.
A more simplified approach might use a single uri-
nary tract icon, such as a kidney symbol on the ab-
domen, to consolidate renal health indicators. How-
ever, given the distinct roles of the kidneys and blad-
der, representing both individually enhances clarity.
If the model allows rotation, users could view the kid-
neys from the back, reinforcing anatomical accuracy.
By linking color changes to specific urine test abnor-
malities, this approach provides an intuitive and direct
way to visualize renal function concerns.
4.3 Healthcare Suggestion
The system will incorporate a triage-based approach
using a large language model (LLM) to provide per-
sonalized healthcare suggestions and motivate pa-
tients toward better health management. By analyzing
key health parameters, the model will assess risk lev-
els and generate tailored recommendations. For ex-
ample, if high cholesterol or elevated blood pressure
is detected, the system may suggest lifestyle changes
such as dietary modifications, increased physical ac-
tivity, or medical consultation. Beyond medical ad-
vice, the system will also focus on patient motivation.
Instead of merely presenting risk factors, it will use
positive reinforcement and actionable steps to encour-
age behavior change. If a patient shows early signs
of dehydration or kidney strain, the system might
prompt hydration reminders and explain the benefits
of maintaining optimal fluid balance. Similarly, for
smokers, it could offer quitting strategies, highlight
immediate health benefits, and suggest resources for
smoking cessation. The integration of an LLM al-
lows for a dynamic and engaging interaction, where
responses are not only medically relevant but also em-
pathetic and motivating. By adapting to patient needs
and health trends, the system can enhance patient en-
gagement, encourage proactive healthcare decisions,
and ultimately contribute to improved long-term well-
being.
5 DISCUSSION
This study presents a concept of integration digi-
tal triage system with human digital twin models to
improve healthcare visualization and patient moni-
toring. By mapping clinical parameters to specific
body regions on a 3D model, the system offers an
intuitive interface that enhances both patient under-
standing and clinician decision-making. It holds par-
ticular promise in underserved areas, supporting re-
mote assessments and low-resource healthcare deliv-
ery through the Portable Health Clinic model.
Despite its potential, the system has notable lim-
itations. Accurate avatar generation depends on reli-
able anthropometric and facial data, which may not
always be available, especially in rural or under-
resourced settings. The use of facial recognition also
raises ethical and privacy concerns, highlighting the
need for strict data protection and informed consent.
Additionally, reliance on AI for triage decisions
introduces risks, including algorithmic bias and mis-
interpretation of diverse clinical presentations. These
risks are especially relevant in global health contexts
where population data may be underrepresented in
training datasets.
Future work should include clinical validation,
user studies, and the integration of AI methods to en-
sure fairness and trust. Addressing these challenges is
critical for safe, effective, and ethical implementation
across diverse healthcare settings.
A Proposed Framework for Integrating Digital Triage with 3D Human Model for Intuitive Health Visualization and Monitoring
335

6 CONCLUSION
This paper has presented a conceptual framework for
integrating digital triage protocols with 3D human
digital twin models to enhance healthcare visualiza-
tion, patient monitoring, and decision-making. The
proposed system leverages anthropometric data and
facial recognition to create personalized 3D models
that visually represent health parameters in anatom-
ically relevant locations. By implementing a color-
coded visualization scheme based on the B-logic
triage framework, the system enables intuitive inter-
pretation of complex health data. The incorpora-
tion of LLM-based healthcare suggestions further en-
hances the system’s utility by providing personalized
recommendations and motivational prompts based on
detected risk factors. This combination of visual rep-
resentation and actionable guidance represents a sig-
nificant step toward more patient-centered healthcare
monitoring. The technology has particular promise
for remote healthcare delivery in underserved com-
munities, building upon the Portable Health Clinic
model. While technical challenges remain in imple-
mentation and integration with existing EHR systems,
the approach offers a promising path to improve pa-
tient engagement, enhance clinical decision-making,
and ultimately advance healthcare delivery through
more intuitive and accessible health information vi-
sualization.
REFERENCES
Ahmed, A., Inoue, S., Kai, E., Nakashima, N., and Nohara,
Y. (2013). Portable health clinic: A pervasive way to
serve the unreached community for preventive health-
care. In Distributed, Ambient, and Pervasive Inter-
actions: First International Conference, DAPI 2013,
Held as Part of HCI International 2013, Las Vegas,
NV, USA, July 21-26, 2013. Proceedings 1, pages 265–
274. Springer.
Aronsky, D., Jones, I., Raines, B., Hemphill, R., Mayberry,
S. R., Luther, M. A., and Slusser, T. (2008). An inte-
grated computerized triage system in the emergency
department. In AMIA Annual Symposium Proceed-
ings, volume 2008, page 16.
Azeredo, T. R. M., Guedes, H. M., de Almeida, R. A. R.,
Chianca, T. C. M., and Martins, J. C. A. (2015). Ef-
ficacy of the manchester triage system: a systematic
review. International emergency nursing, 23(2):47–
52.
Bazyar, J., Farrokhi, M., and Khankeh, H. (2019). Triage
systems in mass casualty incidents and disasters: a re-
view study with a worldwide approach. Open access
Macedonian journal of medical sciences, 7(3):482.
Broadbent, M., Moxham, L., and Dwyer, T. (2007). The
development and use of mental health triage scales in
australia. International journal of mental health nurs-
ing, 16(6):413–421.
Derecho, K. C., Cafino, R., Aquino-Cafino, S. L., Isla Jr,
A., Esencia, J. A., Lactuan, N. J., Maranda, J. A. G.,
and Velasco, L. C. P. (2024). Technology adoption of
electronic medical records in developing economies:
A systematic review on physicians’ perspective. Dig-
ital Health, 10:20552076231224605. Version A.
Ebrahimi, M., Heydari, A., Mazlom, R., and Mirhaghi,
A. (2015). The reliability of the australasian triage
scale: a meta-analysis. World journal of emergency
medicine, 6(2):94.
Holmes, J. F., Freilich, J., Taylor, S. L., and Buettner, D.
(2015). Electronic alerts for triage protocol com-
pliance among emergency department triage nurses:
a randomized controlled trial. Nursing research,
64(3):226–230.
Jiang, J., Qi, K., Bai, G., and Schulman, K. (2023). Pre-
pandemic assessment: a decade of progress in elec-
tronic health record adoption among us hospitals.
Health Affairs Scholar, 1(5):qxad056.
Johns Hopkins Medicine (2022). Tool developed to assist
with triage in the emergency department. Accessed:
March 10, 2025. https://www.hopkinsmedicine.org/
news/articles/2022/11/tool-developed-to-assist-with-
triage-in-the-emergency-department.
Levin, S., Dugas, A., Gurses, A., Kirsch, T., Kelen, G.,
Hinson, J., et al. (2018). Hopscore: An electronic
outcomes-based emergency triage system. Agency for
Healthcare Research and Quality.
Liu, N., Xie, F., Siddiqui, F. J., Ho, A. F. W., Chakraborty,
B., Nadarajan, G. D., Tan, K. B. K., Ong, M. E. H.,
et al. (2022). Leveraging large-scale electronic health
records and interpretable machine learning for clinical
decision making at the emergency department: pro-
tocol for system development and validation. JMIR
research protocols, 11(3):e34201.
Office of the National Coordinator for Health Information
Technology (ONC) (2021). Adoption of electronic
health records by hospital service type, 2019-2021.
Accessed: March 10, 2025.
Slawomirski, L., Lindner, L., de Bienassis, K., Haywood,
P., Hashiguchi, T. C. O., Steentjes, M., and Oderkirk,
J. (2023). Progress on implementing and using elec-
tronic health record systems: developments in oecd
countries as of 2021.
Wang, J., Lu, W., Hu, J., Xi, W., Xu, J., Wang, Z., and
Zhang, Y. (2022). The usage of triage systems in mass
casualty incident of developed countries. Open Jour-
nal of Emergency Medicine, 10(2):124–137.
SIMULTECH 2025 - 15th International Conference on Simulation and Modeling Methodologies, Technologies and Applications
336
