
Healthcare Bias in AI: A Systematic Literature Review
Andrada-Mihaela-Nicoleta Moldovan
1 a
, Andreea Vescan
1 b
and Crina Grosan
2 c
1
Babes¸-Bolyai University, Faculty of Mathematics and Computer Science, Computer Science Department, Cluj-Napoca,
Romania
2
Applied Technologies for Clinical Care, Kings College London, London, U.K.
Keywords:
Systematic Literature Review, Algorithmic Bias, Fairness, Health Disparities.
Abstract:
The adoption of Artificial Intelligence (AI) in healthcare is transforming the field by enhancing patient care,
advancing diagnostic precision, and optimizing clinical flows. Despite its promise, algorithmic bias remains a
pressing challenge, raising critical concerns about fairness, equity, and the reliability of AI systems in diverse
healthcare settings. This Systematic Literature Review (SLR) investigates how bias manifests across the AI
lifecycle—spanning data collection, model training, and real-world application and examines its implications
for healthcare outcomes. By rigorously analyzing peer-reviewed studies based on inclusion and exclusion
criteria, this review identifies the populations most impacted by bias and explores the diversity of existing mit-
igation strategies, fairness metrics, and ethical frameworks. Our findings reveal persistent gaps in addressing
health inequities and underscore the need for targeted interventions to ensure AI systems serve as tools for
equitable and ethical care. This work aims to guide future research and inform policy development, in order
to prioritize both technological progress and social responsibility in healthcare AI.
1 INTRODUCTION
Artificial Intelligence (AI) is transforming health-
care by improving diagnostic accuracy, personaliz-
ing treatment, and optimizing patient outcomes. Bias
in medical environments is defined by Panch et al.
(Panch et al., 2019) as “the instances when the appli-
cation of an algorithm compounds existing inequities
in socioeconomic status, race, ethnic background, re-
ligion, gender, disability or sexual orientation to am-
plify them and adversely impact inequities in health
systems”. Although it does not always happen, bias
usually can lead to discrimination.
In recent years, the academic community has
given the problem of algorithmic bias in Machine
Learning (ML) systems (van Assen et al., 2024) used
in the healthcare industry a lot of attention. Given
their significant effects on healthcare outcomes and
decision-making processes, researchers have directed
more of their attention to comprehending and resolv-
ing possible biases that may exist in these systems.
In an Action Plan published in January 2021
(Clark et al., 2023), the Food and Drug Administra-
a
https://orcid.org/0009-0006-6289-9869
b
https://orcid.org/0000-0002-9049-5726
c
https://orcid.org/0000-0003-1049-2136
tion (FDA) highlighted the importance of detecting
and mitigating bias in machine learning-based medi-
cal systems. The WHO (World Health Organization)
Guidance on Ethics and Governance of AI for Health
(Guidance, 2021) also acknowledges the possibility
of prejudice being ingrained in AI technology. In Oc-
tober 2023, WHO adopted a plan of guiding princi-
ples which are: autonomy, safety, transparency, re-
sponsibility, equity, and sustainability (Bouderhem,
2024).
Burema et al. (Burema et al., 2023) have compiled
a collection of situations to highlight the prevalence
of ethical issues in medical systems. Some incidents
that occurred from algorithmic bias and discrimina-
tion within the healthcare sector include a case that in-
volved the distribution of care work (i.e., the number
of hours a caregiver should spend with their patient)
(Lecher, 2020), and another that reffers to the distri-
bution of Covid-19 vaccinations (Wiggers, 2020a).
Researchers raise awareness of racial algorithmic
bias in medical settings (Ledford, 2019), (Jain et al.,
2023). Black patients were shown to have inferior
diagnostic accuracy when using neural network algo-
rithms trained to categorize skin lesions (Kamulegeya
et al., 2023). It has also been discovered that health
sensors exhibit racial bias (Sjoding et al., 2020).
Covid-19 prediction models with flaws (Thomp-
Moldovan, A.-M.-N., Vescan, A. and Grosan, C.
Healthcare Bias in AI: A Systematic Literature Review.
DOI: 10.5220/0013480300003928
In Proceedings of the 20th International Conference on Evaluation of Novel Approaches to Software Engineering (ENASE 2025), pages 835-842
ISBN: 978-989-758-742-9; ISSN: 2184-4895
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)
835

son, 2020), as well as electronic symptom checks
(Fraser et al., 2018) reveal problems with the AI ac-
curacy. When assessing kidney function, prejudice or
discrimination against specific populations was dis-
covered in AI (Simonite, 2020). Even Google’s lack
of openness in their AI for breast cancer prediction
was questioned by experts (Wiggers, 2020b).
We conducted a Systematic Literature Review
(SLR) in accordance with the guidelines proposed by
Kitchenham and Charters (Kitchenham and Charters,
2007). The SLR assesses and synthesizes the state-
of-the-art concerning healthcare bias in Artificial In-
telligence (AI) systems. The focus is on existing lit-
erature regarding various aspects related to healthcare
bias, specifically concerning algorithm bias.
The contributions in this paper are the following:
• Conducting an SLR regarding healthcare bias in
AI systems that included a set of 97 articles from
six database publication sources;
• Providing answers to five research questions re-
garding algorithm bias in AI systems, consider-
ing various aspects such as: algorithmic bias cat-
egories, sources of bias in healthcare algorithms,
generated risks due to lack of algorithmic fairness,
bias mitigation strategies, and metrics for identifi-
cation of fairness in healthcare algorithms.
• Gaps, challenges, and open issues are discussed,
with proposed opportunities/recommendations.
The remainder of this paper is structured as fol-
lows: Section 2 covers related work, Section 3 out-
lines the methodology, Section 4 details the review
process, Section 5 presents the results, Section 6 dis-
cusses the findings, Section 7 addresses threats to va-
lidity, and Section 8 concludes the paper.
2 RELATED WORK
Yfantidou et al. (Yfantidou et al., 2023) presents a
comprehensive study on bias in personal informatics,
which includes the identification of bias types and the
proposal of guidelines for mitigating discrimination.
However, their research is specifically centered on
personal informatics, focusing exclusively on systems
implemented in devices (watches, wearables) rather
than addressing bias within the healthcare domain.
While existing surveys and reviews (Mienye et al.,
2024), (Kumar et al., 2024) define bias types and
sources, propose frameworks, or offer critical per-
spectives, our SLR takes a complementary approach.
Instead of focusing on fixed statements about bias
types and sources, we aim to consolidate diverse per-
spectives from the literature, drawing parallels and
highlighting variations in how bias is understood. Our
goal is not to establish conclusions, but to present a
comprehensive overview of existing knowledge, serv-
ing as a resource for researchers in AI healthcare.
There are qualitative surveys and systematic re-
views on AI ethics in healthcare (Singh et al., 2023),
(Williamson and Prybutok, 2024), however, our ap-
proach focuses strictly on algorithmic fairness.
3 METHODOLOGY
This section contains the details of the performed re-
search, research questions, and protocol definition.
3.1 Review Need Identification
The literature on AI bias in healthcare is divided be-
tween technical studies on algorithm improvement
and social science research on ethical and cultural im-
plications, however, a combined approach is needed.
Addressing both technical and societal biases in AI
will lead to more effective and equitable healthcare
solutions (Belenguer, 2022).
3.2 Research Questions Definition
We outline the research questions in our investigation:
RQ1: Which are the main algorithmic bias cate-
gories in healthcare?
RQ2: What are the most common sources of bias
in healthcare algorithms?
RQ3: What risks are generated by the lack of
algorithmic fairness in healthcare and who is most
likely to be affected?
RQ4: Which bias mitigation strategies are pro-
posed to reduce algorithmic disparities in AI for
healthcare?
RQ5: How is bias assessed and which metrics
have been proposed for identifying fairness in health-
care algorithms?
3.3 Protocol Definition
The steps of the conducted SLR protocol are the fol-
lowing: the search and selection process with the in-
cluded and excluded criteria; the data extraction strat-
egy; the synthesis of the extracted data with the re-
sponses to the research questions; and the discussion
of the results, identified gaps and open issues, oppor-
tunities and recommendations. The next sections pro-
vide detailed descriptions of each step of the protocol.
ENASE 2025 - 20th International Conference on Evaluation of Novel Approaches to Software Engineering
836
4 CONDUCTING THE SLR
The SLR related activities are provided next, includ-
ing the selection process that contains the database
search and the specification of the selection criteria,
followed by the data extraction.
4.1 Search and Selection Process
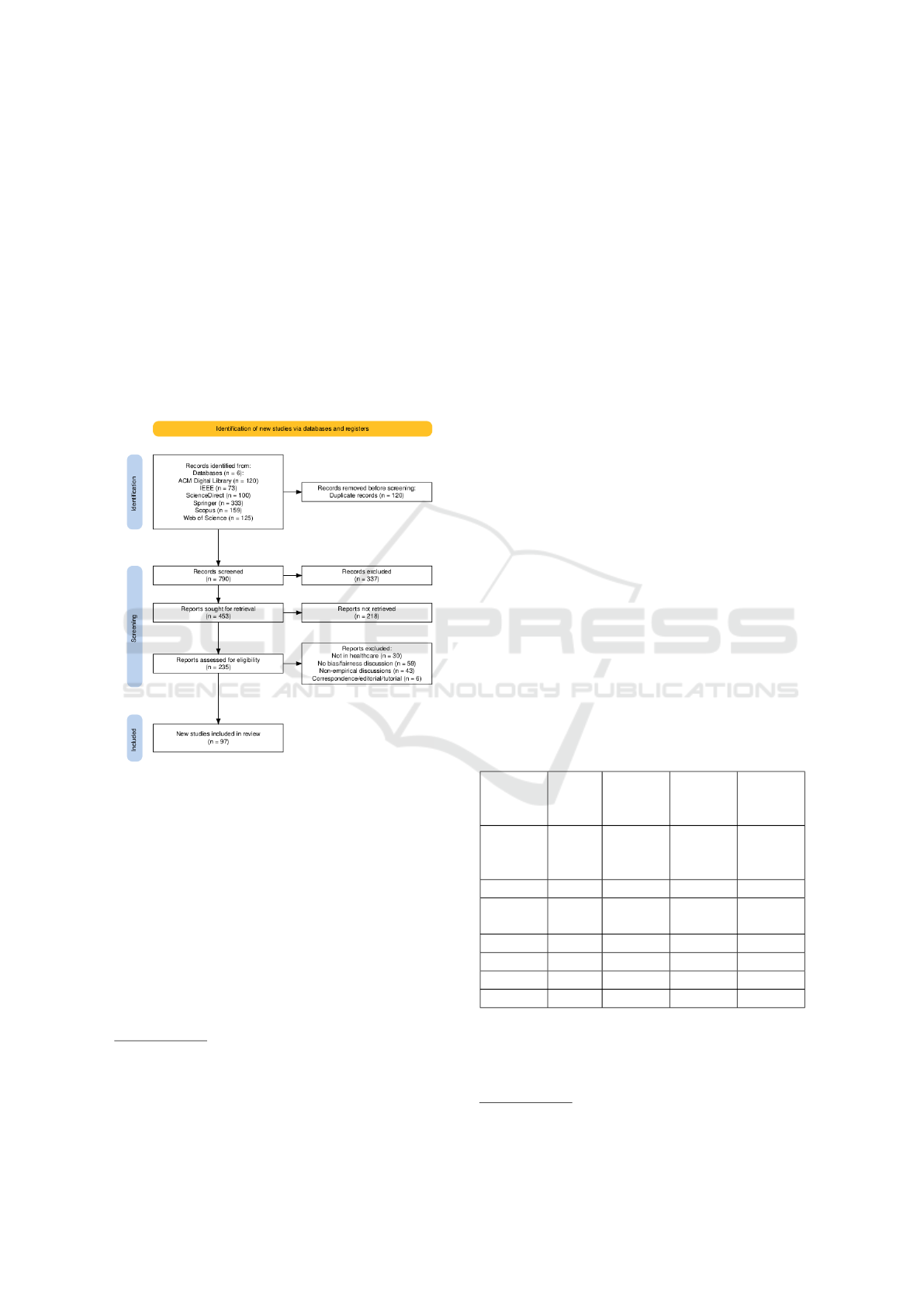
For our literature review, we followed the PRISMA
2020 statement (Page et al., 2021), which ensures a
transparent, unbiased, and reproducible process. Fig-
ure 1 shows the filtering stages, resulting in the selec-
tion of 97 papers from the databases.
Figure 1: Diagram of the Scoping Review Flow in accor-
dance with the PRISMA 2020 declaration (Haddaway et al.,
2022).
4.1.1 Database Search
To ensure the inclusion of the most pertinent re-
search on the topic (Kitchenham and Charters, 2007),
a manual search was conducted across six prominent
databases: ACM Digital Library, IEEE Xplore, Sci-
enceDirect, Scopus, Springer, and Web of Science
(WOS)
1
. Three researchers were assigned databases
for the October 2024 search using ”AI algorithmic
bias in healthcare”, applying filters for publication
1
ACM: https://dl.acm.org, IEEE Xplore:
https://ieeexplore.ieee.org, ScienceDirect: https://www.
sciencedirect.com, Scopus: https://www.scopus.com,
Springer: https://link.springer.com, WOS: https:
//www.webofscience.com
year or domain to manage excessive results and sort-
ing by relevance.
4.1.2 Merging, and Duplicates and Impurity
Removal
Upon completing the search of each database, we uti-
lized Zotero software
2
to extract the BibTeX files
containing the citations of all retrieved papers as the
first filtering stage. These files were subsequently
parsed for the automatic removal of duplicate entries.
4.1.3 Application of the Selection Criteria
The main objective was to identify a selection of ap-
proximately 100 papers that provided the most sub-
stantial insights into the topic of AI algorithmic bias
in healthcare. These papers were assessed on whether
they include answers to the research questions and on
inclusion and exclusion criteria (Meline, 2006).
The inclusion and exclusion criteria that guided
the evaluation of each article to determine its applica-
bility to the research topics.
4.2 Data Extraction
The review protocol produced the initial findings (Ta-
ble 1). After retrieving articles, removing duplicates,
and excluding papers based on relevance and lack of
access, 235 articles were re-evaluated for eligibility in
a detailed third review and 97 papers were identified
as relevant to AI algorithmic bias in healthcare.
Table 1: Table showing the search and review statistics
across various sources.
Source DB
search
Sought
for re-
trieval
Assessed
for eli-
gibility
Selected
ACM
Digital-
Library
120 91 15 10
IEEE 73 93 93 14
Science
Direct
100 13 13 8
Springer 333 212 90 42
Scopus 159 25 11 9
WOS 125 19 13 14
Total 910 453 235 97
To filter out papers on unrelated topics, we man-
ually assessed a set of keywords before identifying
the main ideas, using keyword-based initial screen-
ing (Kitchenham and Charters, 2007). Our selection
2
Zotero: https://www.zotero.org
Healthcare Bias in AI: A Systematic Literature Review
837

of terms included AI, ML, healthcare, bias, fairness,
correctness, metrics, discrimination, clinic or medi-
cal. We recorded occurrences for each term found in
a document, and documented the main ideas of the
papers that scored positively on most terms.
Figure 2 shows the final selection of papers, with
a six-fold increase in publications from 2022 to 2024.
Figure 2: Final database selection: distribution by year of
publication.
A replication package is available containing the
list of all the selected articles from this study (Au-
thor(s), 2025). Further, in this paper, we will refer to
the selected papers with S1 to S97.
5 RESULTS
The following section presents the findings for the
key RQs, addressing the main categories of algorith-
mic bias in healthcare (RQ1), their sources (RQ2), the
risks stemming from unfair algorithms (RQ3), mitiga-
tion strategies to reduce disparities (RQ4), and met-
rics to assess fairness (RQ5). We provide examples
from the selected literature for all answers.
5.1 RQ1: Main Algorithmic Bias
Categories in Healtcare
Seven distinct types of algorithmic bias were identi-
fied in medical settings (S6): historical bias, which
mirrors existing societal prejudices against specific
groups (S15, S16, S79); representation bias, arising
from sampling methods that under-represent certain
population segments (S57, S64, S66, S74, S75); mea-
surement bias, resulting from poorly fitted ML mod-
els (S78); aggregation bias, occurring when univer-
sal models fail to account for variations among sub-
groups; learning bias, where modeling decisions ex-
acerbate disparities in performance; evaluation bias,
which emerges when benchmark datasets do not ac-
curately reflect the intended target population; and
deployment biases (S25) when a model is applied in
ways that diverge from its intended purpose. Many
researchers agree on similar types of bias (S27, S36,
S48, S49, S83) but use varying terms: ’representa-
tion bias’ is also called ’sample bias’ or ’selection
bias’; ’aggregation bias’ overlaps with ’linking bias’;
and ’deployment bias’ is sometimes termed ’feedback
bias’ (S23).
Investigating the selected publications, we ex-
tracted information regarding only mention of the bias
and/or containing in depth investigation regarding al-
gorithmic bias. The algorithmic biases that are most
mentioned in the articles are those related to historical
bias and representation/sampling/selection bias, the
same being also in the case of in-depth investigation
as seen in Figure 3. When considering what database
publications investigated in-depth the algorithmic bi-
ases, the data indicated that Springer and ACM have
the largest number of such papers.
Figure 3: In-depth study investigation of algorithmic biases
in database publications.
Other studies (S46, S82) categorize bias into: ge-
netic variations, intra-observer labeling variability,
data acquisition processes. When classified by cause,
similar issues are stated as prevalence-, presentation-,
and annotation-sourced disparities (S70).
Keeling (S93) outlines how typical clinical ML
models are limited and task-specific, and that their bi-
ases are frequently caused by the under-representation
of certain demographics in training data. On the other
hand, whereas generalist models are wide-ranging,
they also incorporate more intricate biases like stereo-
type associations. Ustymenko and Phadke (S3) intro-
duce some guidelines that aim to be useful in a future
framework addressing bias in LLMs for healthcare.
5.2 RQ2: Sources of Bias in Healthcare
Algorithms
Several sources of bias are identified in the inves-
tigated approaches, Figure 4 depicts the main ones
from label bias and target specification bias to cogni-
tive biases in decision-making and domain shifts dur-
ENASE 2025 - 20th International Conference on Evaluation of Novel Approaches to Software Engineering
838
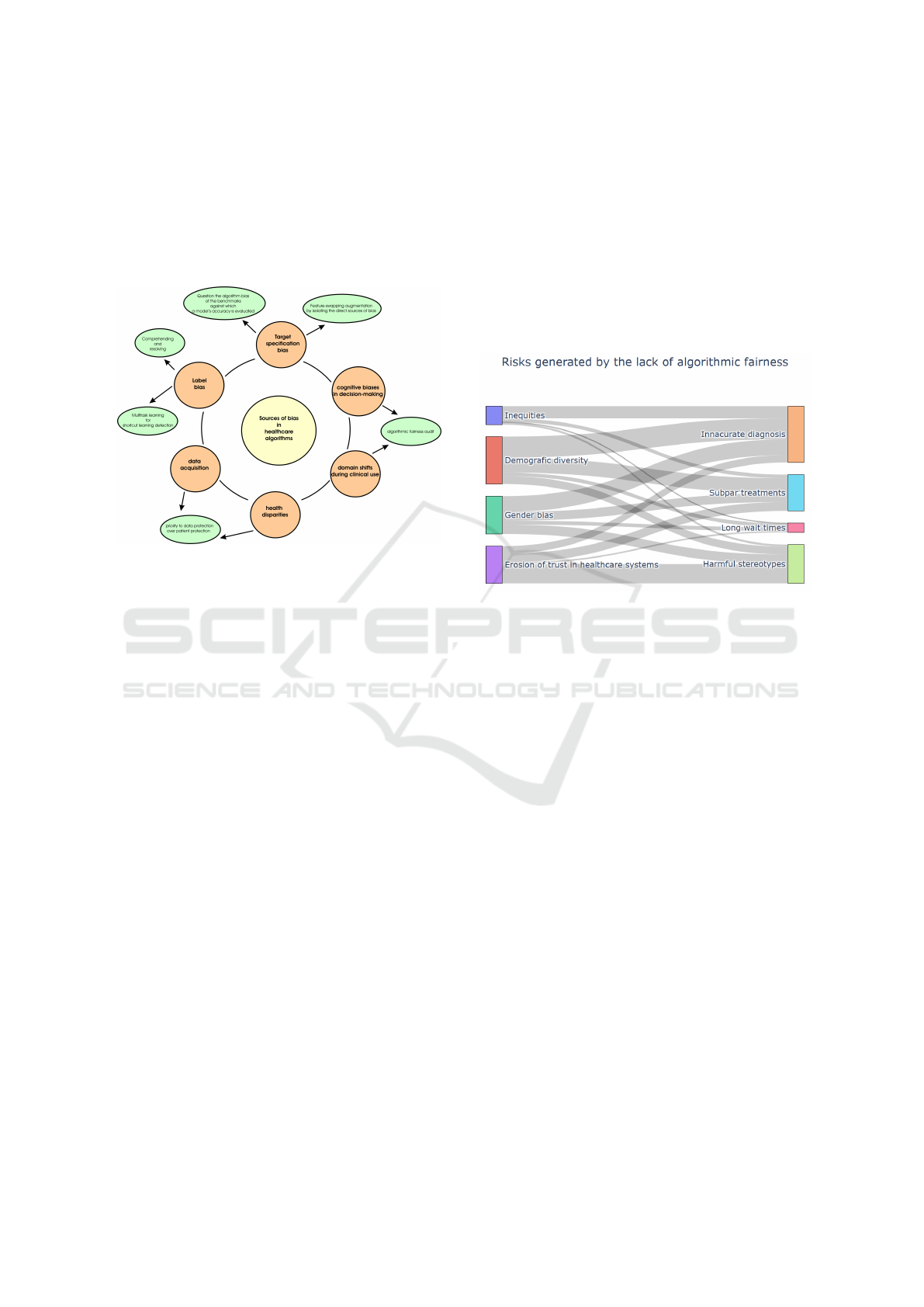
ing clinical use. Specific biases are related to data:
data acquisition and health disparities. For each of
such biases, several solutions were proposed from
multitask learning (S67, S76) and feature-swapping
augmentation to algorithmic fairness audit frame-
works (S80). In the next paragraphs, we provide de-
tails about the sources of biases and some solutions.
Figure 4: Sources of bias in healthcare algorithms.
The types and sources of bias are highly related.
Sources of bias in Clinical Decision Support Sys-
tems (CDSS) were identified as cognitive biases in
decision-making, in domain transitions during clini-
cal usage, as health inequities, and during data gath-
ering (S33).
According to Mhasawade et al. (S2), label bias in
healthcare algorithms occurs when proxy labels, used
instead of actual labels, vary in their connection to
true health status across subgroups. Another simi-
lar approach employs multitask learning for the de-
tection of shortcut learning (S76). Similarly, QP-Net
uses multitask learning alongside a domain adaptation
module (S67), aligning feature distributions across
subgroups to improve less-frequent subgroup fitting.
Questioning the bias in benchmarks used to evalu-
ate model accuracy is crucial. The authors (S1) argue
that label-matching accuracy may bias foreign data
and should be avoided in high-stakes medical con-
texts.
The debiased Survival Prediction solution pro-
posed by Zhong et.al. (S18) reduces the effect of
biases on model performance by isolating the direct
source of bias. By detaching identification informa-
tion, researchers have proven that disentanglement
learning produces more equitable survival estimates
free from population biases (S18). This approach was
also empirically assessed in combination with feder-
ated learning for healthcare equity (S46, S50, S69).
5.3 RQ3: Generated Risks by the Lack
of Algorithmic Fairness in
Healthcare
The lack of algorithmic fairness generates several
risks from inaccurate diagnoses and harmful stereo-
types to the erosion of trust in the healthcare systems.
In Figure 5 several elements as source of risks are
identified: inequities, demographic diversity, gender
bias, and lack of confidence in the healthcare system.
Figure 5: Risks generated by the lack of algorithmic fair-
ness in healthcare.
Children and young people (CYP) under 18 are
particularly underrepresented in research (S42). A
study on Covid-19 diagnosis data (S32) revealed sig-
nificant age disparities, with only 10% of data rep-
resenting individuals under 20, while 50% pertained
to those over 70. Another study on diabetic read-
missions (S12) found that Naive Bayes performed
well for patients under 40, but scored weak non-
discrimination metrics for younger populations. The
ACCEPT-AI framework highlights key ethical con-
siderations for using pediatric data in AI/ML research
(S72).
Healthcare AI systems can inadvertently sustain
xenophobic biases, worsening health inequalities for
migrants and ethnic minorities (S85). For example,
using proxies for sensitive traits can intensify ex-
clusion and link foreignness with disease (S76). A
case study (S38) on a skin color detection algorithm
showed a 16% error in detecting skin tone and a 4%
error in recognizing white faces.
Literature on AI fairness in healthcare highlights
how real-world gender biases are reinforced (S60)
(S42), (S9). Women have been historically underrep-
resented in health data, limiting AI’s impact on their
healthcare (S43). A skin color detection case study
(S38) found a 6% error in recognizing women over
men, while Cardiovascular AI research (S23) shows
Healthcare Bias in AI: A Systematic Literature Review
839
women receive less care.
5.4 RQ4: Mitigation Strategies to
Reduce Algorithmic Disparities in
AI for Healthcare
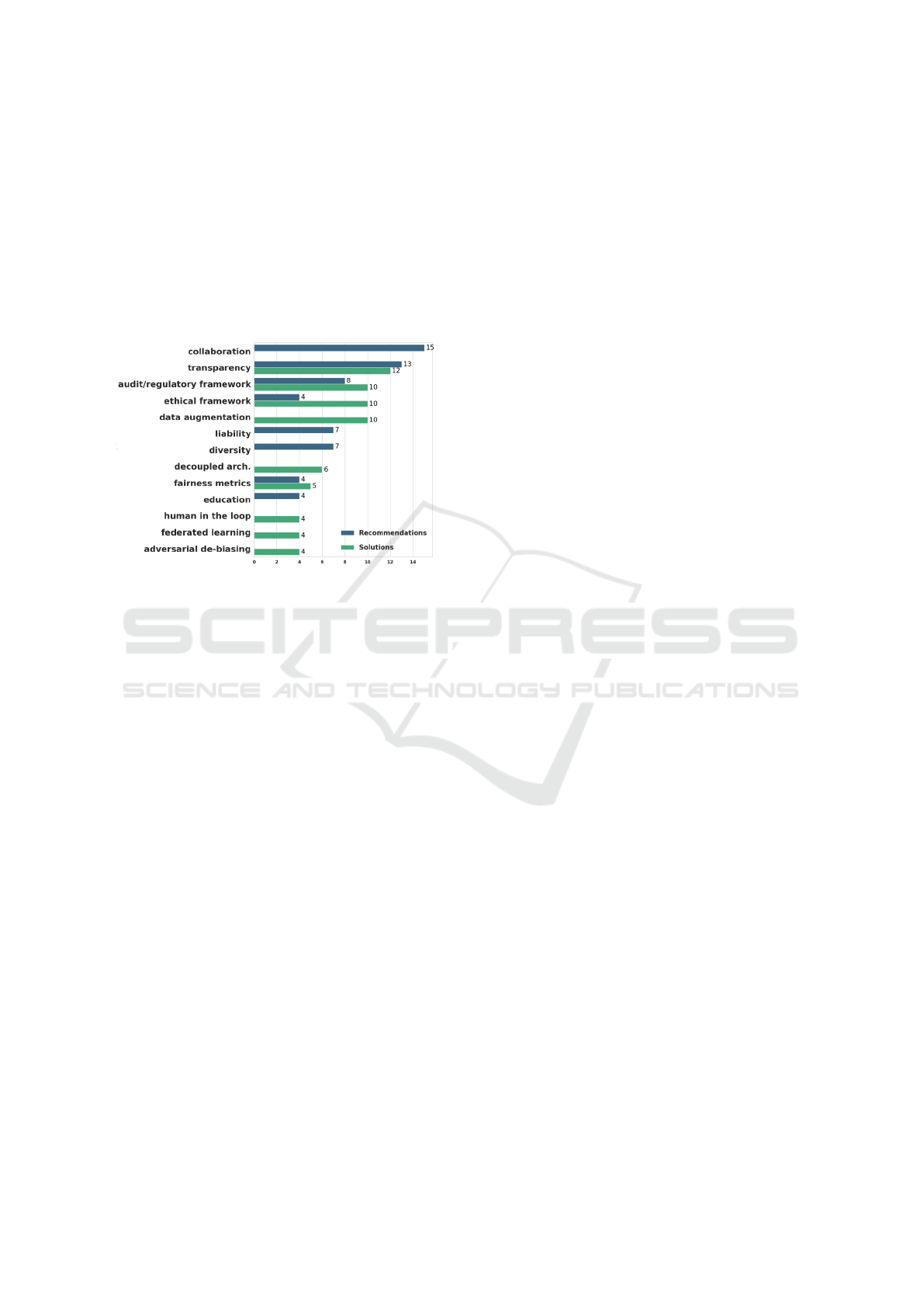
The most frequently proposed mitigation solutions
and recommendations from the selected papers are
displayed in Figure 6.
Figure 6: Distribution of mitigation strategies.
Ethical principles. Distinct approaches to
fair AI include borrowing ethical principles from
fields where they are successfully applied. Amu-
gongo et al. (S10) suggest incorporating Ubuntu
ethics—principles. Belenguer (S83) advocates apply-
ing ethics systems from the pharmaceutical industry,
while Younas and Zeng (S95) propose using Central
Asian ethics. Creating a perfect plan to address all
ethical issues is unlikely, and debates continue on bal-
ancing algorithm transparency with data protection,
as well as on certifying developers who meet ethical
standards (S53, S55).
Frameworks. The most encountered bias mitiga-
tion solution stands in the form of a framework (S14,
S24, S26, S47, S48, S46, S38, S4, S21, S52, S54, S49,
72, S81, S91). Iabkoff et al. (S52) introduced one of
the most comprehensive frameworks.
Transparency. Explainable AI (XAI) refers to AI
systems that aim to provide human-understandable
justifications for their decisions and predictions, en-
hancing transparency (S35, S20, S46, S80, S96, S28).
Procedural justice emphasizes the importance of the
decision-making plan (S35), while Gerdes (S96) and
Kumar (S41) argue that AI models must be explain-
able in healthcare for better understanding. Legal
constraints may enforce transparency (S84), and open
data for XAI enhances accessibility and clarity, aid-
ing informed decisions (S20). Yousefi (S8) suggests
sharing data for public interest. The TWIX tech-
nique (S73) mitigates bias in surgeon skill assess-
ments. Ziosi et al. (S80) evaluate XAI methods based
on their ability to address fairness and transparency
(S30).
Data handling. Although it is common practice to
generate synthetic datasets (S40, S58, S77, S32) for
drawing parallels between situations with balanced
and unbalanced data (S29), or to generate datasets
that are as diverse as possible, approaches for fair-
ness include real-data datasets, or a middle solution
that modifies existing data (S51, S65, S77). A pro-
posal is to exclude demographic data (S22), as models
achieve “locally optimal” fairness, but struggle in out-
of-distribution (OOD) settings, suggesting less demo-
graphic encoding promotes “globally optimal” fair-
ness (S56).
Human-in-the-Loop (HITL). The idea of HITL
is essential for challenging the function of human
knowledge and the interaction between algorithms
and people. A human-guided approach guarantees
that developments in technology are a reaction to real
clinical requests (S33, S34, S97). Iniesta (S71) in-
troduces a framework that emphasizes the HITL ap-
proach by several principles like accountability or pa-
tient education.
5.5 RQ5: Bias Assessment and Metrics
to Identify Fairness in Healthcare
Algorithms
Audit frameworks (S59, S17, S77, S83, S94, S71) aim
at adapting the development stage to be bias-aware
(S26), disparities to be acknowledged from data col-
lection to decision design (S46) through bias identi-
fication solutions (S38) for assessing datasets against
racial, age, or gender bias. Moghadasi et al. (S21) ar-
gue that identifying bias sources is key to mitigation.
In order to guarantee a more thorough, customized,
and impartial perspective, users should additionally
employ a variety of bias measures (S13, S31, S19,
S29).
Mienye et al. (S19) reviewed fairness metrics
(S62) and categorized them into six types: group fair-
ness, individual fairness, equality of opportunity, de-
mographic parity, equalized odds, and counterfac-
tual fairness, each with its own mathematical formula
(S61, S69, S32, S29, S56, S61).
A framework proposed for improved and ethical
patient outcomes (S17) implements fairness measures
to evaluate the impact of AI algorithms on different
demographic groups using the disparate impact met-
ric for assessing fairness (S69, S6, S29, S44, S56).
Bowtie analysis is used to assess risks and ensure
safety (S32). Similarly, Forward-Backward analysis
ENASE 2025 - 20th International Conference on Evaluation of Novel Approaches to Software Engineering
840

(S43) splits the process into forward (examining con-
sequences) and backward (tracing causes) steps.
6 FINDINGS AND DISCUSSIONS
This section outlines the findings of this investigation,
providing several perspectives regarding gaps, chal-
lenges, and open issues. Opportunities and recom-
mendations are detailed at the end of the section.
6.1 Discussions of Results
Although bias can also arise during data acquisition
by competent institutions or results interpretation by
clinicians, most frameworks (S14, S4, S26) and ap-
proaches (S20, S22, S37, S81, S83) assign the task
of working on bias mitigation to researchers and de-
velopers. Very few of them are addressed to medical
personnel (S48, S5). Some scholars and practitioners
posit that governance frameworks may serve as a vi-
able solution (S42, S90, S42). Combinations of legal
and audit frameworks are proposed as potential strate-
gies (S84), (S83).
Multiple studies consider fairness and even pro-
pose approaches for specific tasks or branches of
medicine (S7), such as ICU readmission (S11), dia-
betes (S12) (S92), lung ultrasound (S14), pulmonary
embolism (S18), critical care (S33), liver allocation
(S35, S87), cardiac sarcoidosis (S21), pain detection
(S45), medical imaging (radiology, dermatology, oph-
thalmology) (S56), S70), virology (S88) (with empha-
sis on Covid-19 (S61) (S82), oncology (S63) (S89),
cardiac imaging (S23), orthopedics (S65), thyroid ul-
trasound (S67), antibiotic prescription (S68), pedi-
atrics (S72), surgeon skill assessment (S73), health-
care time series (S77), neuroscience (S86), point-of-
care diagnostics (S39). Tandon et al. (S49) aim to pro-
vide help for developers to decide which AI-enabled
strategies to use for certain designs in the medical
field based on context-specific criteria.
6.2 Gaps, Challenges, Open Issues
Several gaps have been identified based on the inves-
tigated papers:
• Underrepresentation of minority groups in medi-
cal datasets.
• Many AI models are “black boxes”, making it
hard to identify and mitigate biases.
• Limited testing of AI systems on varied demo-
graphic and geographic populations.
• Insufficient collaboration between technologists,
clinicians, and patients.
• AI systems can perpetuate and magnify existing
systemic biases.
6.3 Opportunities and
Recommendations
Several Opportunities to address healthcare bias in
AI are identified and provided next: Enhanced data
diversity by incorporating diverse datasets, Person-
alized medicine advancements by having customiz-
able treatments, Collaborative multidisciplinary re-
search through multiple experts, Development of fair-
ness metrics that are tailored for healthcare applica-
tions, and Policy and regulation innovation.
The following Recommentations are provided to
address healthcare bias in AI: regular bias audits, di-
versify training datasets, stakeholder engagement, im-
plement eXplainable AI (XAI), and adopt fairness-
centric regulations.
7 THREATS TO VALIDITY
Despite being thorough, this literature study has a
limitation that should be noted, namely the speed at
which AI is developing, which may have resulted in
new discoveries after the research under considera-
tion. Publication bias may have skewed the findings,
as studies with positive results are more likely to be
published, while null or negative findings often go
unreported. To mitigate this, we aimed to include a
diverse range of studies and explicitly sought those
discussing limitations or failures.
8 CONCLUSIONS
Numerous ethical, political, and economic factors
have influenced the application of AI in healthcare,
improving the technology’s fairness in this area. By
taking these aspects into consideration, a suitable de-
gree of control over AI’s detrimental effects on the
healthcare industry has been demonstrated. Still,
many of the statements made in this study encourage
academics to identify additional useful implications
for practitioners and policymakers about the reliabil-
ity of AI applications in healthcare, which will en-
hance the literature in the future.
Healthcare Bias in AI: A Systematic Literature Review
841

ACKNOWLEDGEMENTS
The publication of this article was partially supported
by the 2024 Development Fund of the Babes-Bolyai
University.
REFERENCES
Author(s), A. (accessed January 2025). Healthcare
bias in ai: A systematic literature review. =
https://figshare.com/s/cc41c628a51a442181fd.
Belenguer, L. (2022). Ai bias: exploring discriminatory
algorithmic decision-making models and the appli-
cation of possible machine-centric solutions adapted
from the pharmaceutical industry. AI and Ethics,
2(4):771–787.
Bouderhem, R. (2024). Shaping the future of ai in health-
care through ethics and governance. Humanities and
Social Sciences Communications, 11(1):1–12.
Burema, D., Debowski-Weimann, N., von Janowski,
A., Grabowski, J., Maftei, M., Jacobs, M., Van
Der Smagt, P., and Benbouzid, D. (2023). A sector-
based approach to ai ethics: Understanding ethical is-
sues of ai-related incidents within their sectoral con-
text. In Proceedings of the 2023 AAAI/ACM Confer-
ence on AI, Ethics, and Society, pages 705–714.
Clark, P., Kim, J., and Aphinyanaphongs, Y. (2023). Mar-
keting and us food and drug administration clear-
ance of artificial intelligence and machine learning en-
abled software in and as medical devices: a system-
atic review. JAMA Network Open, 6(7):e2321792–
e2321792.
Fraser, H., Coiera, E., and Wong, D. (2018). Safety of
patient-facing digital symptom checkers. The Lancet,
392(10161):2263–2264.
Guidance, W. (2021). Ethics and governance of artificial
intelligence for health. World Health Organization.
Haddaway, N. R., Page, M. J., Pritchard, C. C., and
McGuinness, L. A. (2022). Prisma2020: An r package
and shiny app for producing prisma 2020-compliant
flow diagrams, with interactivity for optimised digital
transparency and open synthesis. Campbell systematic
reviews, 18(2):e1230.
Jain, A., Brooks, J. R., Alford, C. C., Chang, C. S., Mueller,
N. M., Umscheid, C. A., and Bierman, A. S. (2023).
Awareness of racial and ethnic bias and potential so-
lutions to address bias with use of health care algo-
rithms. In JAMA Health Forum, volume 4, pages
e231197–e231197. American Medical Association.
Kamulegeya, L., Bwanika, J., Okello, M., Rusoke, D., Nas-
siwa, F., Lubega, W., Musinguzi, D., and B
¨
orve, A.
(2023). Using artificial intelligence on dermatology
conditions in uganda: A case for diversity in training
data sets for machine learning. African Health Sci-
ences, 23(2):753–63.
Kitchenham, B. and Charters, S. (2007). Guidelines for per-
forming systematic literature reviews in software en-
gineering. 2.
Kumar, A., Aelgani, V., Vohra, R., Gupta, S. K., Bhagawati,
M., Paul, S., Saba, L., Suri, N., Khanna, N. N., Laird,
J. R., et al. (2024). Artificial intelligence bias in med-
ical system designs: A systematic review. Multimedia
Tools and Applications, 83(6):18005–18057.
Lecher, C. (2020). Can a robot decide my medical treat-
ment?
Ledford, H. (2019). Millions affected by racial bias in
health-care algorithm. Nature, 574(31):2.
Meline, T. (2006). Selecting studies for systemic re-
view: Inclusion and exclusion criteria. Contempo-
rary issues in communication science and disorders,
33(Spring):21–27.
Mienye, I. D., Obaido, G., Emmanuel, I. D., and Ajani,
A. A. (2024). A survey of bias and fairness in health-
care ai. In 2024 IEEE 12th International Confer-
ence on Healthcare Informatics (ICHI), pages 642–
650. IEEE.
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I.,
Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tet-
zlaff, J. M., Akl, E. A., Brennan, S. E., et al. (2021).
The prisma 2020 statement: an updated guideline for
reporting systematic reviews. bmj, 372.
Panch, T., Mattie, H., and Atun, R. (2019). Artificial intel-
ligence and algorithmic bias: implications for health
systems. Journal of global health, 9(2).
Simonite, T. (2020). How an algorithm blocked kidney
transplants to black patients— wired.
Singh, B., Rahim, M. A. B. U., Hussain, S., Rizwan, M. A.,
and Zhao, J. (2023). Ai ethics in healthcare-a sur-
vey. In 2023 IEEE 23rd International Conference on
Software Quality, Reliability, and Security Compan-
ion (QRS-C), pages 826–833. IEEE.
Sjoding, M. W., Dickson, R. P., Iwashyna, T. J., Gay, S. E.,
and Valley, T. S. (2020). Racial bias in pulse oxime-
try measurement. New England Journal of Medicine,
383(25):2477–2478.
Thompson, A. (2020). Coronavirus: Models pre-
dicting patient outcomes may be “flawed” and
“based on weak evidence. Yahoo! Retrieved from
https://sg.style.yahoo.com/style/coronavirus-covid19-
models-patientoutcomes-flawed-153227342.html.
van Assen, M., Beecy, A., Gershon, G., Newsome, J.,
Trivedi, H., and Gichoya, J. (2024). Implications
of bias in artificial intelligence: considerations for
cardiovascular imaging. Current Atherosclerosis Re-
ports, 26(4):91–102.
Wiggers, K. (2020a). Covid-19 vaccine distribution algo-
rithms may cement health care inequalities.
Wiggers, K. (2020b). Google’s breast cancer-predicting ai
research is useless without transparency, critics say.
Williamson, S. M. and Prybutok, V. (2024). Balanc-
ing privacy and progress: a review of privacy chal-
lenges, systemic oversight, and patient perceptions in
ai-driven healthcare. Applied Sciences, 14(2):675.
Yfantidou, S., Sermpezis, P., Vakali, A., and Baeza-Yates,
R. (2023). Uncovering bias in personal informatics.
Proceedings of the ACM on Interactive, Mobile, Wear-
able and Ubiquitous Technologies, 7(3):1–30.
ENASE 2025 - 20th International Conference on Evaluation of Novel Approaches to Software Engineering
842
