
Traumatic Rescue Experiences and Post-Traumatic Stress Disorder in
Firefighters: The Moderating Roles of Inhibitory Control and
Cognitive Flexibility
Zhong Xia and Wang Jingyi
Shanghai Fire Research Institute of MEM, Shanghai, China
Keywords: Firefighters, PTSD, Traumatic Stress Exposure, Inhibitory Control, Cognitive Flexibility.
Abstract: OBJECTIVES: This study aimed to analyze the correlation between traumatic stress exposure and PTSD
symptoms in Chinese firefighters using questionnaire and test methods, and to examine the moderating
effects of inhibitory control and cognitive flexibility of executive functions.
METHODS: A total of 263 frontline firefighters from China participated in this study. The self-developed
"20-item Firefighter Stress Trauma Exposure Experience Inventory" was employed to investigate the
subjects' experiences of traumatic events related to firefighting and rescue tasks since their recruitment. The
Post-Traumatic Stress Disorder Scale (PCL-5) was used to assess the presence and severity of PTSD-related
symptoms. Inhibitory control and cognitive flexibility were evaluated using the Stroop test and the number
manipulation test, respectively. A moderating model was constructed through path analysis.
RESULTS: Linear regression analysis revealed that traumatic stress exposure significantly and positively
predicted the severity of PTSD symptoms in firefighters (p < 0.05). The moderating effect of inhibitory
control was significant (p < 0.05), with simple slope analysis indicating that firefighters with strong
inhibitory control were less adversely affected by traumatic stress exposure. Although the moderating effect
of cognitive flexibility was not significant (p > 0.05), the simple slope analysis exhibited a trend similar to
that of inhibitory control.
CONCLUSION: Inhibitory control and cognitive flexibility can moderate the development of PTSD in
firefighters to some extent. The findings underscore the potential value of utilizing executive function and
other cognitive training to enhance firefighters’ resilience to PTSD.
1 INTRODUCTION
As an unique occupational group, firefighters are
entrusted with the critical tasks of fire prevention,
fire suppression, and emergency rescue, all of which
entail significant danger, complexity, and
uncertainty. Firefighters are frequently exposed to
various hazards, intense auditory and visual stimuli,
traumatic scenes, and the experience or witnessing of
casualties among themselves and others during
rescue missions. Such exposures can easily lead to
traumatic experiences and, consequently, to various
psychological disorders (Smith, Goldstein, & Grant,
2016). Post-Traumatic Stress Disorder (PTSD) is
characterized by the delayed onset and persistence of
intense fear, anxiety, helplessness, distress, and other
mental disorders resulting from exceptionally
threatening or catastrophic psychological trauma
(Goldstein et al., 2016). PTSD is one of the most
common mental disorders among firefighters,
significantly impairing their occupational health.
Numerous studies have investigated the prevalence of
PTSD in firefighters, with lifetime prevalence rates
ranging from 1.9% to 57% across different countries,
depending on sample sources and assessment methods
(Obuobi-Donkor, Oluwasina, Nkire, & Agyapong,
2022). Overall, firefighters have a higher risk of
developing PTSD and experience more severe
symptoms than the general population.
Various traumatic task experiences are often
considered the primary triggers of PTSD in
firefighters (Serrano-Ibanez, Corras, Del Prado, Diz,
& Varela, 2022). Due to the nature of their work,
firefighters are more frequently exposed to traumatic
events than the general population, including
witnessing gruesome and bloody scenes,
experiencing or witnessing severe injuries, facing
death directly, and encountering various shocking
disaster scenarios (Wagner et al., 2021). In addition
to task experiences, numerous studies have identified
other variables that influence the development of
Xia, Z. and Jingyi, W.
Traumatic Rescue Experiences and Post-Traumatic Stress Disorder in Firefighters: The Moderating Roles of Inhibitory Control and Cognitive Flexibility.
DOI: 10.5220/0013036700003938
In Proceedings of the 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health (ICT4AWE 2025), pages 155-164
ISBN: 978-989-758-743-6; ISSN: 2184-4984
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)
155

PTSD, such as age (Chung, Lee, Jung, & Nam,
2015), marital status (Chen et al., 2007), level of
burnout (Meyer et al., 2012), work climate (Jo et al.,
2018), social support (Jin et al., 2022; Shi, Chen, Li,
& An, 2021), history of psychological and
psychiatric disorders (Kim, Park, & Kim, 2018;
Noor, Pao, Dragomir-Davis, Tran, & Arbona, 2019),
and cognitive factors (Wild & Gur, 2008). The
development of PTSD is thus a multifactorial
process, with traumatic experiences being one of the
most critical causal factors.
Typical symptoms of PTSD include recurrent
intrusive traumatic experiences (such as flashbacks
and nightmares), persistent avoidance, negative
alterations in cognition and mood, and heightened
arousal (Pietrzak et al., 2015). These symptoms
make it difficult for firefighters with PTSD to fully
engage in rescue missions, potentially leading to
mission hindrance or failure. PTSD has also been
associated with cognitive impairments (Qureshi et
al., 2011; Schuitevoerder et al., 2013). Patients with
PTSD often exhibit varying degrees of cognitive
deficits, such as impairments in memory and
learning (Johnsen & Asbjornsen, 2008; Mattson,
Nelson, Sponheim, & Disner, 2019), visuospatial
processing (Kunimatsu, Yasaka, Akai, Kunimatsu, &
Abe, 2020), and central executive functions
(Jagger-Rickels et al., 2021; Li et al., 2019; Polak,
Witteveen, Reitsma, & Olff, 2012), such as
inhibitory control and cognitive flexibility.
Inhibitory control refers to the mental process by
which individuals regulate their attention, thoughts,
behaviors, or emotions to overcome strong internal
tendencies or external temptations, while cognitive
flexibility refers to the ability to shift cognitive
resources across multiple tasks (Diamond, 2012).
Studies have shown that these executive functions
are related to PTSD symptoms such as flashbacks,
nightmares, persistent anxiety, depression, and
heightened arousal (Fitzgerald, DiGangi, & Phan,
2018). Some researchers even suggest that deficits in
executive functions, particularly inhibitory control,
make it difficult for PTSD patients to suppress
memories and thoughts related to traumatic
experiences, leading to recurrent intrusive memories
and persistent negative emotions (Cavicchioli et al.,
2020; Philippot & Agrigoroaei, 2017).
Therefore, researchers have explored the
application of systematic cognitive training in the
treatment and rehabilitation of PTSD, achieving
positive results with interventions such as Eye
Movement Desensitization and Reprocessing
(EMDR) (Jeffries & Davis, 2013) and Cognitive
Processing Therapy (CPT) (Asmundson et al., 2019;
Resick, Suvak, Johnides, Mitchell, & Iverson, 2012).
Based on these findings, it is reasonable to
hypothesize that the chain of PTSD triggered by
traumatic events is moderated by individual
cognitive abilities, such as executive functions.
In this study, frontline firefighters from eastern
and central China were selected to investigate the
pathways by which traumatic task experiences affect
PTSD symptoms and to examine the moderating
effect of higher cognitive abilities, particularly
central executive functions, on this relationship.
2 MATERIALS AND METHODS
2.1 Research Design
This retrospective study involved frontline
firefighters (defined as those serving in basic fire
rescue stations) from Anhui and Shanghai province,
China. We assessed their exposure to traumatic
events related to firefighting and rescue duties since
their recruitment and evaluated their current PTSD
symptoms using questionnaires. Additionally, we
measured the participants' inhibitory control and
cognitive flexibility using a set of executive function
tests administered on handheld PDA devices. All
assessments were conducted at the fire rescue
stations where the subjects were employed, with
participants gathered in a conference room to
complete the tests and questionnaires. Informed
consent was obtained from all station officers
(station chiefs or instructors) prior to the study.
The specific procedures for administering the
tests were as follows: First, permission was obtained
from the chief officers of each fire station to conduct
the study. Before administering the tests, these
officers collected demographic information on all
station members, including gender, age, length of
service, marital status, and educational background.
The fire station officers then organized the subjects
to take the tests in the conference room, ensuring
they were seated at intervals to avoid interruptions.
Once all subjects were ready, the researcher guided
them through the completion of the questionnaires
and tests.
2.2 Tools
2.2.1 Traumatic Rescue Experiences
The "20-item Firefighters ’ Stress Trauma
Exposure Experience Inventory," a self-compiled
tool, was used to investigate subjects' exposure to
traumatic events related to firefighting and rescue
missions since their recruitment. The questionnaire
includes 20 items representing typical stress trauma
experiences, such as life-threatening situations for
oneself and comrades, witnessing brutal scenes,
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
156
handling dead bodies or severely injured individuals,
and being present at disaster scenes. Each item is
scored on a 3-point scale: 0 (never), 1 (once), and 2
(twice or more). Higher scores indicate more
extensive exposure to stress trauma. The Cronbach's
alpha coefficient of the scale was 0.914, indicating
good reliability. Specific inventory items are
presented in Appendix.
2.2.2 PTSD Symptoms
The Post-Traumatic Stress Disorder Scale (PCL-5)
was used to assess the presence and severity of
PTSD-related symptoms. The scale consists of 20
items that meet the diagnostic criteria for PTSD
according to the American Psychiatric Association’
s Diagnostic and Statistical Manual of Mental
Disorders, Fifth Edition (DSM-5) (Blevins,
Weathers, Davis, Witte, & Domino, 2015). Although
the PCL-5 is not a stand-alone diagnostic tool for
PTSD, it can be used for initial assessment and
monitoring of potential PTSD-related symptoms
(Wortmann et al., 2016). The Cronbach's alpha
coefficient of the scale was above 0.9, indicating
good reliability (Cheng et al., 2020). Specific
inventory items are presented in Appendix.
2.2.3 Inhibitory Control and Cognitive
Flexibility
A classic Stroop test was used to assess subjects’
inhibitory control, where color words were presented
randomly, and the task was to respond to the font
color of the word with a keystroke. The test included
two conditions: congruent (the word meaning matches
the font color, e.g., "red" in red) and incongruent (the
word meaning does not match the font color, e.g.,
"yellow" in red). The test comprised 36 trials, with
half in the congruent condition and half in the
incongruent condition. Higher accuracy and shorter
response times indicate better inhibitory control.
A number manipulation test was designed to
assess cognitive flexibility. In this test, a pair of
numbers (both within 10) was presented randomly,
and the task was to quickly determine the size
relationship between the two numbers. If the left
number was greater, subtraction was performed (left
minus right); if the right number was greater,
addition was performed. Results were entered via a
numeric keyboard. The test consisted of 20 trials,
requiring 10 conversion processes (switching from
subtraction to addition or vice versa). All subjects
completed a general numerical ability test before this
test to control for differences in mathematical ability.
Higher accuracy and shorter completion times
indicated better cognitive flexibility, assuming
consistent general numerical ability among subjects.
2.3 Subjects
The study involved administering scales and tests in
20 fire rescue stations (the most basic firefighting
units) in Anhui and Shanghai province, China. All
subjects met the following criteria: (1) informed
consent and voluntary participation; (2) completion
of all induction training and formal enrollment in
service; (3) participation in at least one rescue
mission. Subjects were excluded if they: (1) were
absent or left midway through the test due to
vacation, duty, or rescue tasks; (2) had a history of
mental illness or a family history of hereditary
mental illness; (3) had never participated in a fire
rescue mission since recruitment; (4) did not wish to
participate for other reasons.
2.4 Data Analysis
All scale and test data were analyzed using IBM
SPSS 22.0 and IBM SPSS AMOS 22.0.
Demographic data were described using frequency,
percentage, mean, and standard deviation. Linear
regression was employed to model the pathway
linking traumatic rescue experiences to PTSD
symptom severity. Pathway analysis was conducted
to examine the moderating effects of inhibitory
control and cognitive flexibility on this relationship.
3 RESULTS
3.1 Sociodemographic Characteristics
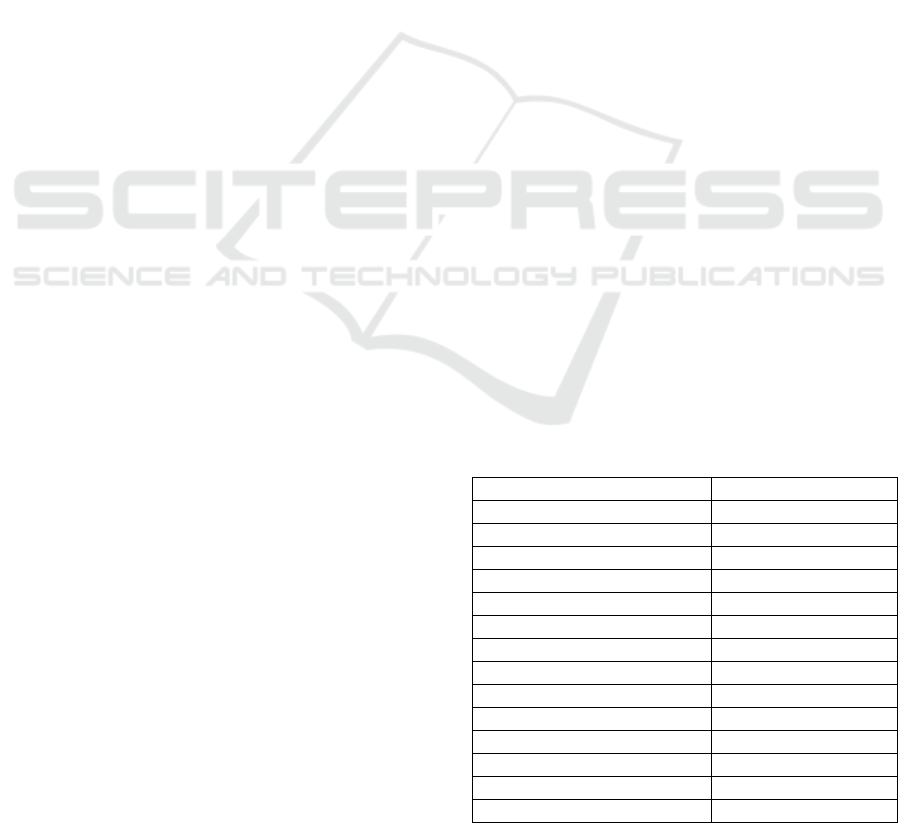
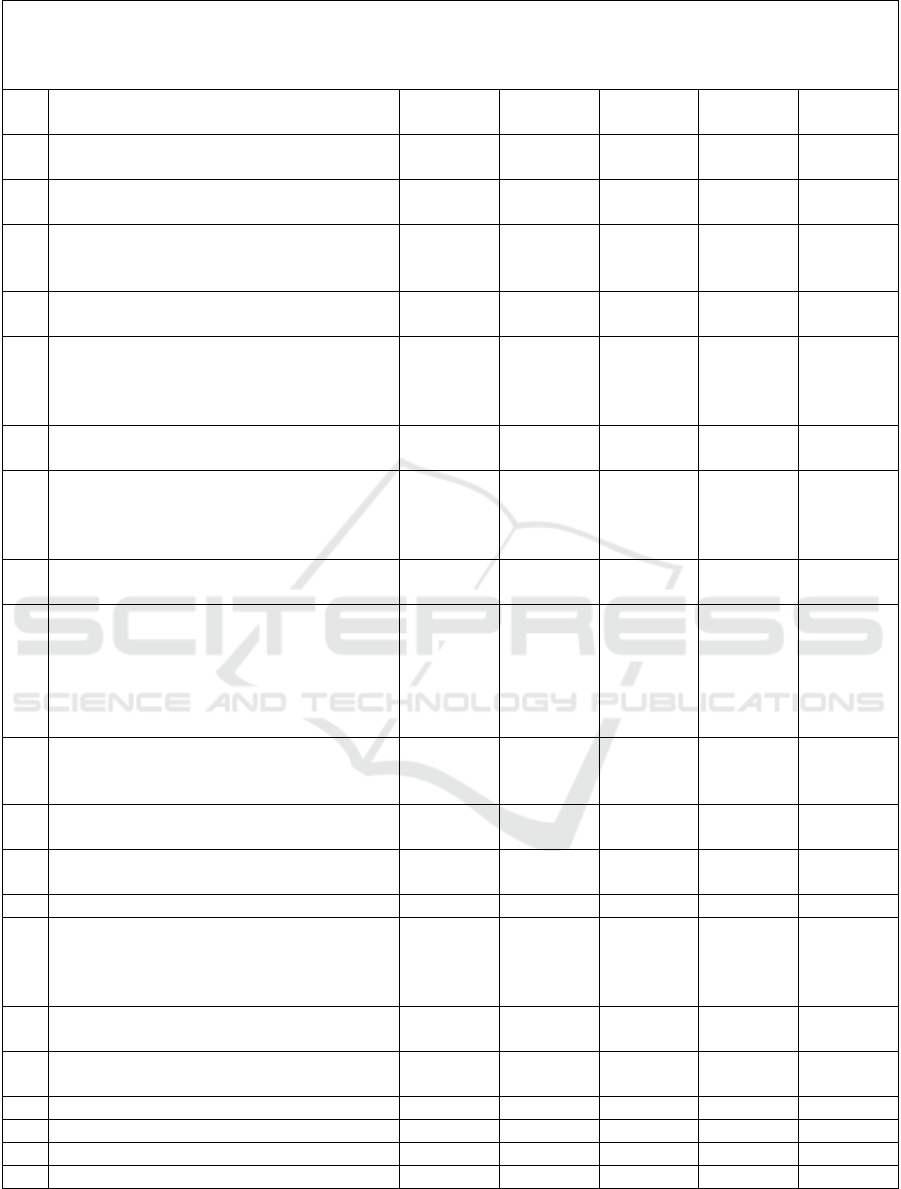
Table 1 presents the sociodemographic information
of all subjects. Data from 263 valid subjects were
collected, all male. Ages ranged from 20 to 44 years,
Table 1: Sociodemographic characteristics(n=263).
items frequency(%)
age
≤25 123(46.8)
26~30 104 (39.5)
>30 36 (13.7)
Enlistment duration
≤3 142 (54)
4~8 76 (28.8)
>8 45 (17.2)
Marital status
married 72 (27.4)
unmarried 191 (72.6)
Educational background
Below university degree 210 (79.9)
University degree or above 53 (20.1)
Traumatic Rescue Experiences and Post-Traumatic Stress Disorder in Firefighters: The Moderating Roles of Inhibitory Control and
Cognitive Flexibility
157
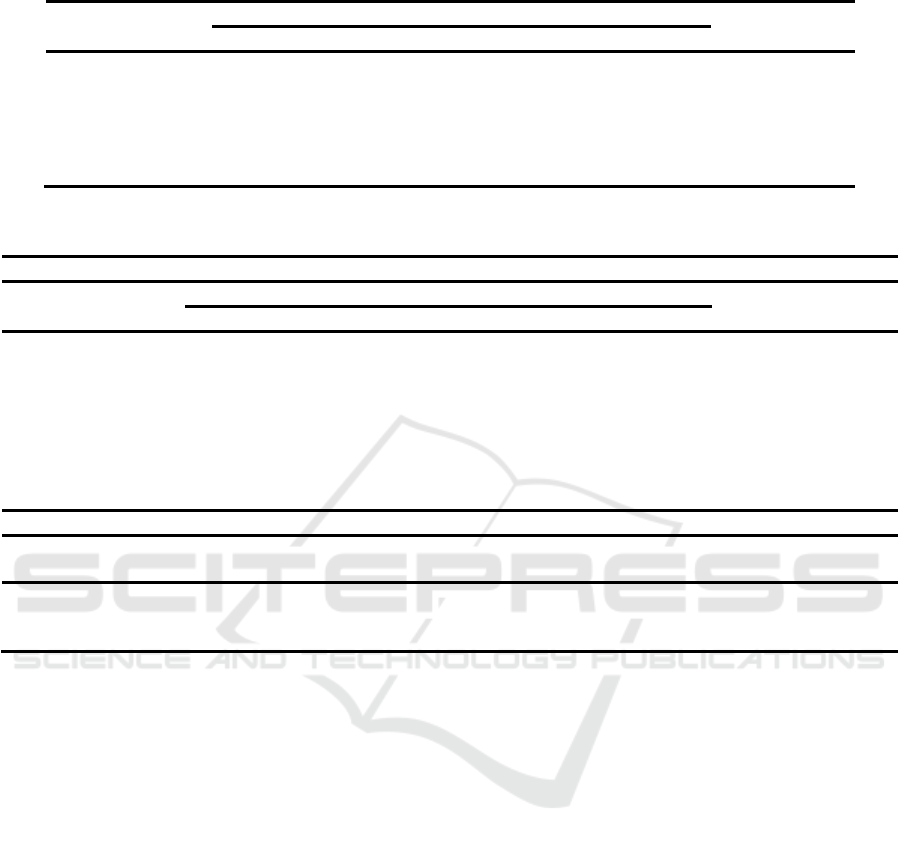
Table 2: Linear regression model of PTSD symptoms on TRAUMA scores.
Unstandardized coefficients Standardized coefficients
t P value
B Standard error Beta
Constant 7.095 1.032 - 6.872 0.000**
TRAUMA scores 0.260 0.071 0.221 3.655 0.000**
R
2
0.049
Adjusted R
2
0.045
F F (1, 261) =13.356, p=0.000
D-W 1.710
Table 3: Mediating model of Stroop test scores.
Model summary
Unstandardized coefficients Standardized coefficients
t P value
B Standard error Beta
constant 0.048 0.059 - 0.802 0.423
TRAUMA scores 0.209 0.060 0.209 3.494 0.001**
Stroop scores -0.115 0.060 -0.115 -1.929 0.055
TRAUMA*Stroop -0.097 0.042 -0.140 -2.341 0.020*
R
2
0.084
R
2
changes 0.019
F value F (3,259)=7.882,p=0.000
F value changes F(1,259)=5.482,p=0.020
simple slope analysis
Levels of moderating variable
Regression
coefficients
Standard error t P value 95% CI
average 0.209 0.060 3.494 0.001 [0.092,0.327]
High level(+1SD) 0.112 0.076 1.465 0.144 [-0.038,0.262]
Low level(-1SD) 0.307 0.069 4.435 0.000 [0.171,0.442]
with a mean age of 26.51 ± 4.18 years (M ± SD).
The shortest length of service was less than 1 year,
and the longest was 25 years, with a mean of 4.44 ±
4.29 years (M ± SD). There were 191 unmarried
subjects (72.6%) and 72 married subjects (27.4%).
Educational levels were as follows: 1 junior high
school graduate (0.4%), 86 high school graduates
(32.7%), 123 college degree holders (46.8%), 48
university degree holders (18.3%), and 5 with a
bachelor’s degree or higher (1.9%).
3.2 The Effect of Traumatic Rescue
Experiences on PTSD Symptoms
A linear regression model was constructed with the
subjects' scores on the PCL-5 as the dependent
variable and their scores on the '20-item Firefighters’
Stress Trauma Exposure Experience Inventory'
(hereafter referred to as the TRAUMA Inventory) as
the independent variable. Table 2 presents the model
fit with R
2
=0.049, indicating that this independent
variable explains 4.9% of the variance in the
dependent variable. The model passed the F-test
(F=13.356, p=0.000<0.05). The regression
coefficient for the independent variable was 0.260
(p=0.000<0.05), indicating that the independent
variable had a significant positive effect on the
dependent variable. This result suggests that
firefighters who scored high on the TRAUMA
Inventory may exhibit a higher propensity for PTSD
symptoms.
3.3 Moderating Effects of Inhibitory
Control and Cognitive Flexibility
To explore the moderating effects of subjects'
inhibitory control and cognitive flexibility on PTSD
symptoms, all variables involved in the analysis
were converted to standard Z scores. The subjects'
scores on the Stroop test and the number
manipulation test (hereafter referred to as the NT)
were added to the model constructed in section 3.2.
Table 3 presents the model with Stroop test scores as
a moderating variable. In this model, the number of
correct responses (ranging from 0 to 36) was used as
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
158
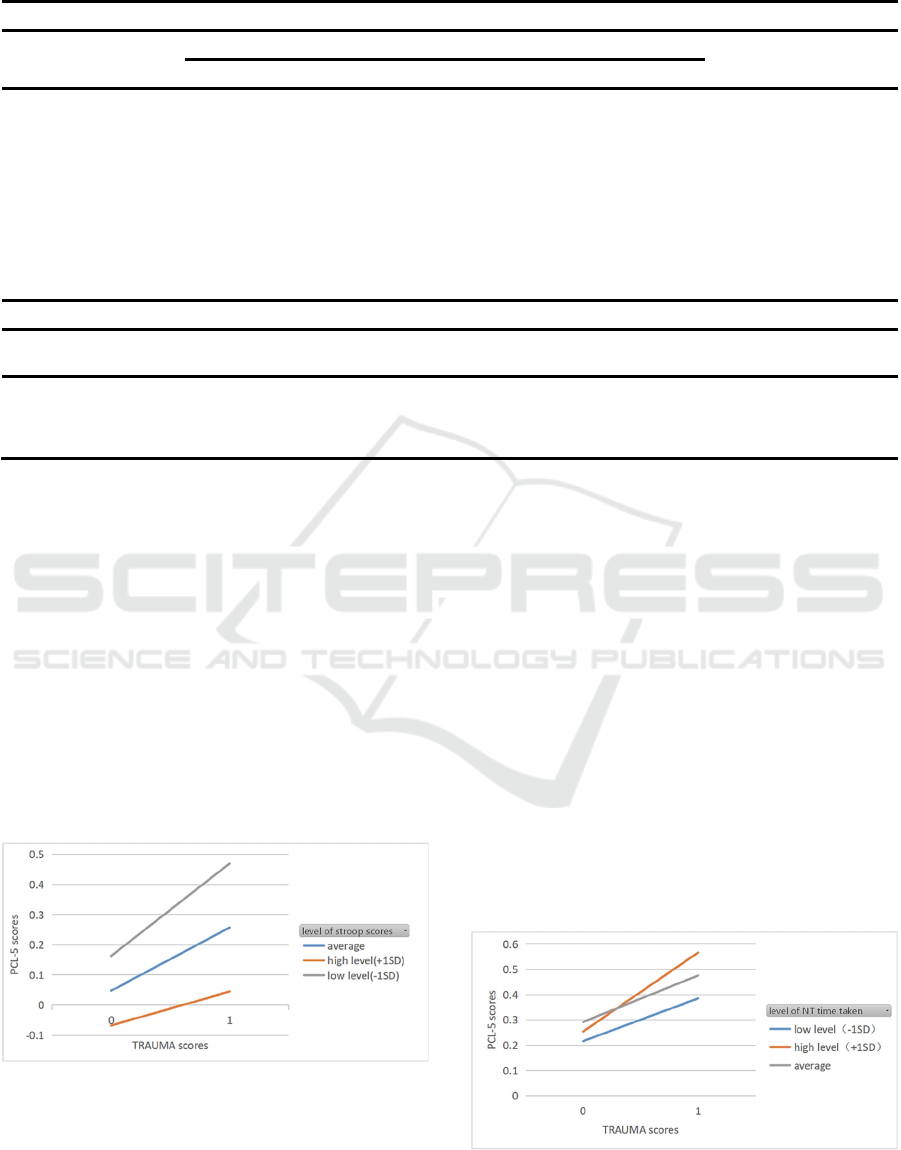
Table 4: Mediating model of NT time taken.
Model summary
Unstandardized coefficients Standardized coefficients
t P value
B Standard error Beta
constant 0.254 0.418 - 0.608 0.544
TRAUMA scores 0.222 0.061 0.222 3.626 0.000**
NT time taken 0.038 0.065 0.038 0.581 0.562
TRAUMA*NT 0.053 0.067 0.048 0.793 0.429
R
2
0.057
R
2
changes 0.002
F value F (3, 257) = 3.110, p=0.010
F value changes F (1,257) = 0.628,p=0.429
simple slope analysis
Levels of moderating variable
Regression
coefficients
Standard error t P value 95% CI
average 0.222 0.061 3.626 0.000 [0.102,0.342]
High level(+1SD) 0.275 0.093 2.941 0.004 [0.092,0.458]
Low level(-1SD) 0.169 0.087 1.931 0.055 [-0.002,0.340]
an indicator of test performance. The interaction
regression coefficient for TRAUMA scores and
Stroop scores was −0.097(p=0.020<0.05), indicating
a significant moderating effect. Further simple slope
analysis showed that when the moderating variable
(Stroop scores) was at a low or average level, there
was a significant positive effect of TRAUMA scores
on PTSD symptoms (B=0.307,p=0.000<0.05;
B=0.209,p=0.001<0.05), while at a high level, this
effect was not significant (B=0.112,p=0.144>0.05),
as shown in Figure 1 and Table 3. This suggests that
subjects with greater inhibitory control are somewhat
able to withstand the impact of traumatic rescue
experiences, as evidenced by the lesser effect on
PTSD symptoms.
Figure 1: Simple slope diagram for different Stroop scores
levels.
Table 4 presents the model with NT scores as a
moderating variable. Due to the low difficulty of the
test items (addition and subtraction within 10), the
vast majority of subjects achieved nearly 100%
accuracy. Therefore, the time taken by subjects to
complete the test was used as an indicator of
performance, with longer times indicating worse
cognitive flexibility. To avoid confounding general
numerical ability with cognitive flexibility, subjects'
time on the General Numerical Ability Test
(completed before the formal test) was added as a
covariate. The model fit indicated that the interaction
term's regression coefficient was
0.053(p=0.429>0.05), suggesting that the
moderating effect of NT was not significant. Despite
the poor model fit, simple slope analysis was
performed, as shown in Figure 2. Results indicated
that TRAUMA scores had a significant positive
effect on PTSD symptoms when NT time was at
average or high levels (B=0.222, p=0.000 < 0.05;
B=0.275, p=0.004 < 0.05), but not at low levels
(B=0.169, p=0.055 > 0.05).
Figure 2: Simple slope diagram for different NT levels.
Traumatic Rescue Experiences and Post-Traumatic Stress Disorder in Firefighters: The Moderating Roles of Inhibitory Control and
Cognitive Flexibility
159

4 DISCUSSION
This study constructed a pathway model to examine
the effect of stress trauma exposure on the
development of PTSD symptoms in firefighters.
Findings indicate that the extent of stress trauma
exposure significantly positively affects the severity
of PTSD symptoms in firefighters, meaning those
who experience more traumatic rescue events tend to
exhibit more PTSD symptoms. Traumatic events and
scenarios are inevitable for firefighters. The majority
of firefighters face shocking events including injury,
illness, death, heat, noise, and explosions, making
them more susceptible to PTSD compared to the
general population. Studies in the United States,
Canada, and the United Kingdom show that
firefighters have a much higher prevalence of PTSD
than the general population, as well as military
personnel and first responders (Obuobi-Donkor et
al., 2022). Additionally, PTSD can coexist with
other psychological disorders, and firefighters are
often at risk for other mental health problems such as
anxiety and depression due to their work
environment (Alghamdi, Hunt, & Thomas, 2015),
complicating the screening, diagnosis, and
intervention processes for PTSD.
For PTSD prevention, avoiding stressors is an
effective option (Kyron, Rikkers, LaMontagne,
Bartlett, & Lawrence, 2022). However, for
firefighters, this is difficult to achieve since exposure
to various stressors is inherent to their job. Even
retired firefighters may have a high prevalence of
PTSD (McFarlane & Bryant, 2007). Thus,
preemptive approaches to reduce PTSD incidence in
firefighters are challenging.
In recent years, cognitive therapy has been
widely used for treating various psychological
disorders, such as autism (Wass & Porayska-Pomsta,
2014), Alzheimer's disease (Vecchio et al., 2022),
and PTSD (Ehlers & Clark, 2000). Executive
function, a core aspect of higher cognitive abilities,
has been linked to PTSD development and recovery
(Olff, Polak, Witteveen, & Denys, 2014; Smits,
Geuze, Schutter, van Honk, & Gladwin, 2021). This
study tested the moderating effects of inhibitory
control and cognitive flexibility. Results indicated
that inhibitory control significantly moderates PTSD
symptoms, with stronger inhibitory control
associated with fewer PTSD symptoms. Although
the moderating effect of cognitive flexibility was not
significant, slope analysis suggested a potential
effect. Inhibitory control allows individuals to
suppress dominant responses detrimental to current
activities (Ullsperger & Danielmeier, 2022), helping
control intrusive traumatic experiences and negative
thinking in PTSD. Cognitive flexibility enables
individuals to transfer cognitive resources between
tasks, potentially reducing hypervigilance, a
common PTSD symptom, by shifting attention and
adjusting mental states.
Firefighters' occupational characteristics make
them vulnerable to various hazards and traumatic
events, and their management practices may increase
susceptibility to anxiety, depression, and stress
disorders, impacting performance and increasing
separation and suicide risks (Davidson, Stein,
Shalev, & Yehuda, 2004). Effective treatment or
alleviation of PTSD symptoms is crucial for
maintaining firefighters' occupational health.
However, many PTSD treatments are not suitable for
firefighters due to the long duration and systematic
interventions required, often necessitating time away
from duty, which is not feasible. Moreover, the fire
department's militaristic and masculine culture can
stigmatize mental health treatment, leading to
condition concealment or negative treatment. Given
these factors, enhancing firefighters' resilience to
traumatic stress through cognitive training to reduce
PTSD probability or alleviate symptoms appears to
be a prudent intervention.
5 CONCLUSION
In conclusion, this study verified the moderating
effects of inhibitory control and cognitive flexibility
on PTSD morbidity and symptom severity in
firefighters. Firefighters with greater inhibitory
control and cognitive flexibility under the influence
of traumatic rescue experiences are less likely to
develop PTSD symptoms. Enhancing executive
functioning in firefighters to prevent PTSD onset or
reduce symptom severity is a viable strategy for
improving their occupational mental health.
REFERENCES
Alghamdi, M., Hunt, N., Thomas, S. (2015). The
effectiveness of narrative exposure therapy with
traumatised firefighters in Saudi Arabia: A randomized
controlled study. Behaviour Research and Therapy,
66, 64-71. https://doi.org/10.1016/ j.brat.2015.01.008.
Asmundson, G. J. G., Thorisdottir, A. S., Roden-Foreman,
J. W., Baird, S. O., Witcraft, S. M., Stein, A. T.,
Powers, M. B. (2019). A meta-analytic review of
cognitive processing therapy for adults with
posttraumatic stress disorder. Cognitive Behaviour
Therapy, 48(1), 1-14. https://doi.org/10.1080/165060
73.2018.1522371.
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
160

Blevins, C. A., Weathers, F. W., Davis, M. T., Witte, T.
K., Domino, J. L. (2015). The posttraumatic stress
disorder checklist for DSM-5 (PCL-5): Development
and initial psychometric evaluation. Journal of
Traumatic Stress, 28(6), 489-498. https://doi.org/
10.1002/jts.22059.
Cavicchioli, M., Ramella, P., Vassena, G., Simone, G.,
Prudenziati, F., Sirtori, F., Maffei, C. (2020). Mindful
self-regulation of attention is a key protective factor
for emotional dysregulation and addictive behaviors
among individuals with alcohol use disorder. Addictive
Behaviors, 105, 106317. https://doi.org/
10.1016/j.addbeh.2020.106317.
Chen, Y. S., Chen, M. C., Chou, F. H., Sun, F. C., Chen, P.
C., Tsai, K. Y., Chao, S. S. (2007). The relationship
between quality of life and posttraumatic stress
disorder or major depression for firefighters in
Kaohsiung, Taiwan. Quality of Life Research, 16(8),
1289-1297. https://doi.org/10.1007/s11136-007-9248
-7.
Cheng, P., Xu, L. Z., Zheng, W. H., Ng, R. M. K., Zhang,
L., Li, L. J., Li, W. H. (2020). Psychometric property
study of the posttraumatic stress disorder checklist for
DSM-5 (PCL-5) in Chinese healthcare workers during
the outbreak of corona virus disease 2019. Journal of
Affective Disorders, 277, 368-374.
https://doi.org/10.1016/j.jad.2020.08.038.
Chung, I. S., Lee, M. Y., Jung, S. W., Nam, C. W. (2015).
Minnesota multiphasic personality inventory as related
factor for posttraumatic stress disorder symptoms
according to job stress level in experienced
firefighters: 5-year study. Annals of Occupational and
Environmental Medicine, 27, 16. https://doi.org/
10.1186/s40557-015-0067-y.
Davidson, J. R., Stein, D. J., Shalev, A. Y., Yehuda, R.
(2004). Posttraumatic stress disorder: Acquisition,
recognition, course, and treatment. The Journal of
Neuropsychiatry and Clinical Neurosciences, 16(2),
135-147. https://doi.org/10.1176/jnp.16.2.135.
Diamond, A. (2012). Activities and programs that improve
children's executive functions. Current Directions in
Psychological Science, 21(5), 335-341.
https://doi.org/10.1177/0963721412453722.
Ehlers, A., Clark, D. M. (2000). A cognitive model of
posttraumatic stress disorder. Behaviour Research and
Therapy, 38(4), 319-345. https://doi.org/10.1016/
s0005-7967(99)00123-0.
Fitzgerald, J. M., DiGangi, J. A., Phan, K. L. (2018).
Functional neuroanatomy of emotion and its regulation
in PTSD. Harvard Review of Psychiatry, 26(3),
116-128. https://doi.org/10.1097/HRP.0000000
000000185.
Goldstein, R. B., Smith, S. M., Chou, S. P., Saha, T. D.,
Jung, J., Zhang, H., Grant, B. F. (2016). The
epidemiology of DSM-5 posttraumatic stress disorder
in the United States: Results from the National
Epidemiologic Survey on Alcohol and Related
Conditions-III. Social Psychiatry and Psychiatric
Epidemiology, 51(8), 1137-1148. https://doi.org/
10.1007/s00127-016-1208-5.
Jagger-Rickels, A., Stumps, A., Rothlein, D., Park, H.,
Fortenbaugh, F., Zuberer, A., Esterman, M. (2021).
Impaired executive function exacerbates neural
markers of posttraumatic stress disorder.
Psychological Medicine, 1-14. https://doi.org/10.10
17/S0033291721000842.
Jeffries, F. W., Davis, P. (2013). What is the role of eye
movements in eye movement desensitization and
reprocessing (EMDR) for post-traumatic stress
disorder (PTSD)? A review. Behavioural and
Cognitive Psychotherapy, 41(3), 290-300.
https://doi.org/10.1017/S1352465812000793.
Jin, F., Ashraf, A. A., Ul Din, S. M., Farooq, U., Zheng,
K., Shaukat, G. (2022). Organisational caring ethical
climate and its relationship with workplace bullying
and post-traumatic stress disorder: The role of type
A/B behavioural patterns. Frontiers in Psychology, 13,
1042297. https://doi.org/10.3389/fpsyg.2022.10
42297.
Jo, I., Lee, S., Sung, G., Kim, M., Lee, S., Park, J., Lee, K.
(2018). Relationship between burnout and PTSD
symptoms in firefighters: The moderating effects of a
sense of calling to firefighting. International Archives
of Occupational and Environmental Health, 91(1),
117-123. https://doi.org/10.1007/s00420-017-1263-6.
Johnsen, G. E., Asbjornsen, A. E. (2008). Consistent
impaired verbal memory in PTSD: A meta-analysis.
Journal of Affective Disorders, 111(1), 74-82.
https://doi.org/10.1016/j.jad.2008.02.007.
Kim, J. I., Park, H., Kim, J. H. (2018). Alcohol use
disorders and insomnia mediate the association
between PTSD symptoms and suicidal ideation in
Korean firefighters. Depression and Anxiety, 35(11),
1095-1103. https://doi.org/10.1002/da.22803.
Kunimatsu, A., Yasaka, K., Akai, H., Kunimatsu, N., Abe,
O. (2020). MRI findings in posttraumatic stress
disorder. Journal of Magnetic Resonance Imaging,
52(2), 380-396. https://doi.org/10.1002/jmri.26929.
Kyron, M. J., Rikkers, W., LaMontagne, A., Bartlett, J.,
Lawrence, D. (2022). Work-related and nonwork
stressors, PTSD, and psychological distress:
Prevalence and attributable burden among Australian
police and emergency services employees.
Psychological Trauma: Theory, Research, Practice,
and Policy, 14(7), 1124-1133. https://doi.org/10.10
37/tra0000536.
Li, G., Wang, L., Cao, C., Fang, R., Cao, X., Chen, C.,
Hall, B. J. (2019). Posttraumatic stress disorder and
executive dysfunction among children and
adolescents: A latent profile analysis. International
Journal of Clinical and Health Psychology, 19(3),
228-236. https://doi.org/10.1016/j.ijchp.2019.07.001.
Mattson, E. K., Nelson, N. W., Sponheim, S. R., Disner, S.
G. (2019). The impact of PTSD and mTBI on the
Traumatic Rescue Experiences and Post-Traumatic Stress Disorder in Firefighters: The Moderating Roles of Inhibitory Control and
Cognitive Flexibility
161

relationship between subjective and objective
cognitive deficits in combat-exposed veterans.
Neuropsychology, 33(7), 913-921. https://doi.org/
10.1037/neu0000560.
McFarlane, A. C., Bryant, R. A. (2007). Post-traumatic
stress disorder in occupational settings: Anticipating
and managing the risk. Occupational Medicine, 57(6),
404-410. https://doi.org/10.1093/occmed/kqm070.
Meyer, E. C., Zimering, R., Daly, E., Knight, J., Kamholz,
B. W., Gulliver, S. B. (2012). Predictors of
posttraumatic stress disorder and other psychological
symptoms in trauma-exposed firefighters.
Psychological Services, 9(1), 1-15. https://doi.org/
10.1037/a0026414.
Noor, N., Pao, C., Dragomir-Davis, M., Tran, J., Arbona,
C. (2019). PTSD symptoms and suicidal ideation in
US female firefighters. Occupational Medicine,
69(8-9), 577-585. https://doi.org/10.1093/occmed/
kqz057.
Obuobi-Donkor, G., Oluwasina, F., Nkire, N., Agyapong,
V. I. O. (2022). A scoping review on the prevalence
and determinants of post-traumatic stress disorder
among military personnel and firefighters:
Implications for public policy and practice.
International Journal of Environmental Research and
Public Health, 19(3), 1565. https://doi.org/10.3390/
ijerph19031565.
Olff, M., Polak, A. R., Witteveen, A. B., Denys, D. (2014).
Executive function in posttraumatic stress disorder
(PTSD) and the influence of comorbid depression.
Neurobiology of Learning and Memory, 112, 114-121.
https://doi.org/10.1016/j.nlm.2014.01.003.
Philippot, P., Agrigoroaei, S. (2017). Repetitive thinking,
executive functioning, and depressive mood in the
elderly. Aging & Mental Health, 21(11), 1192-1196.
https://doi.org/10.1080/13607863.2016.1211619.
Pietrzak, R. H., Tsai, J., Armour, C., Mota, N.,
Harpaz-Rotem, I., Southwick, S. M. (2015).
Functional significance of a novel 7-factor model of
DSM-5 PTSD symptoms: Results from the National
Health and Resilience in Veterans study. Journal of
Affective Disorders, 174, 522-526. https://doi.org/
10.1016/j.jad.2014.12.007.
Polak, A. R., Witteveen, A. B., Reitsma, J. B., Olff, M.
(2012). The role of executive function in posttraumatic
stress disorder: A systematic review. Journal of
Affective Disorders, 141(1), 11-21.
https://doi.org/10.1016/j.jad.2012.01.001.
Qureshi, S. U., Long, M. E., Bradshaw, M. R., Pyne, J. M.,
Magruder, K. M., Kimbrell, T., Kunik, M. E. (2011).
Does PTSD impair cognition beyond the effect of
trauma? Journal of Neuropsychiatry and Clinical
Neurosciences, 23(1), 16-28. https://doi.org/10.1176/
jnp.23.1.jnp16.
Resick, P. A., Suvak, M. K., Johnides, B. D., Mitchell, K.
S., Iverson, K. M. (2012). The impact of dissociation
on PTSD treatment with cognitive processing therapy.
Depression and Anxiety, 29(8), 718-730.
https://doi.org/10.1002/da.21938.
Schuitevoerder, S., Rosen, J. W., Twamley, E. W., Ayers,
C. R., Sones, H., Lohr, J. B., Thorp, S. R. (2013). A
meta-analysis of cognitive functioning in older adults
with PTSD. Journal of Anxiety Disorders, 27(6),
550-558. https://doi.org/10.1016/j.janxdis.2013.01.0
01.
Serrano-Ibanez, E. R., Corras, T., Del Prado, M., Diz, J.,
Varela, C. (2022). Psychological variables associated
with post-traumatic stress disorder in firefighters: A
systematic review. Trauma, Violence, & Abuse,
15248380221082944. https://doi.org/10.1177/152483
80221082944.
Shi, J., Chen, Y., Li, X., An, Y. (2021). Predicting
posttraumatic stress and depression symptoms among
frontline firefighters in China. Journal of Nervous and
Mental Disease, 209(1), 23-27. https://doi.org/
10.1097/NMD.0000000000001250.
Smith, S. M., Goldstein, R. B., Grant, B. F. (2016). The
association between post-traumatic stress disorder and
lifetime DSM-5 psychiatric disorders among veterans:
Data from the National Epidemiologic Survey on
Alcohol and Related Conditions-III (NESARC-III).
Journal of Psychiatric Research, 82, 16-22.
https://doi.org/10.1016/j.jpsychires.2016.06.0 22.
Smits, F. M., Geuze, E., Schutter, D., van Honk, J.,
Gladwin, T. E. (2021). Effects of tDCS during
inhibitory control training on performance and PTSD,
aggression and anxiety symptoms: A
randomized-controlled trial in a military sample.
Psychological Medicine, 52(16), 1-11. https://doi.org/
10.1017/S0033291721000817.
Ullsperger, M., Danielmeier, C. (2022). Motivational and
cognitive control: From motor inhibition to social
decision making. Neuroscience & Biobehavioral
Reviews, 136, 104600. https://doi.org/10.1016/j.neu
biorev.2022.104600.
Vecchio, F., Quaranta, D., Miraglia, F., Pappalettera, C.,
Di Iorio, R., L'Abbate, F., Rossini, P. M. (2022).
Neuronavigated magnetic stimulation combined with
cognitive training for Alzheimer's patients: An EEG
graph study. Geroscience, 44(1), 159-172.
https://doi.org/10.1007/s11357-021-00508-w.
Wagner, S. L., White, N., Randall, C., Regehr, C., White,
M., Alden, L. E., Krutop, E. (2021). Mental disorders
in firefighters following large-scale disaster. Disaster
Medicine and Public Health Preparedness, 15(4),
504-517. https://doi.org/10.1017/dmp.2020.61.
Wass, S. V., Porayska-Pomsta, K. (2014). The uses of
cognitive training technologies in the treatment of
autism spectrum disorders. Autism, 18(8), 851-871.
https://doi.org/10.1177/1362361313499827.
Wild, J., Gur, R. C. (2008). Verbal memory and treatment
response in post-traumatic stress disorder. The British
Journal of Psychiatry, 193(3), 254-255.
https://doi.org/10.1192/bjp.bp.107.045922.
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
162
Wolffe, T. A. M., Robinson, A., Clinton, A., Turrell, L.,
Stec, A. A. (2023). Mental health of UK firefighters.
Scientific Reports, 13(1), 62. https://doi.org/10.1038/
s41598-022-24834-x.
Wortmann, J. H., Jordan, A. H., Weathers, F. W., Resick,
P. A., Dondanville, K. A., Hall-Clark, B., Litz, B. T.
(2016). Psychometric analysis of the PTSD checklist-5
(PCL-5) among treatment-seeking military service
members. Psychological Assessment, 28(11),
1392-1403. https://doi.org/10.1037/pas0000260.
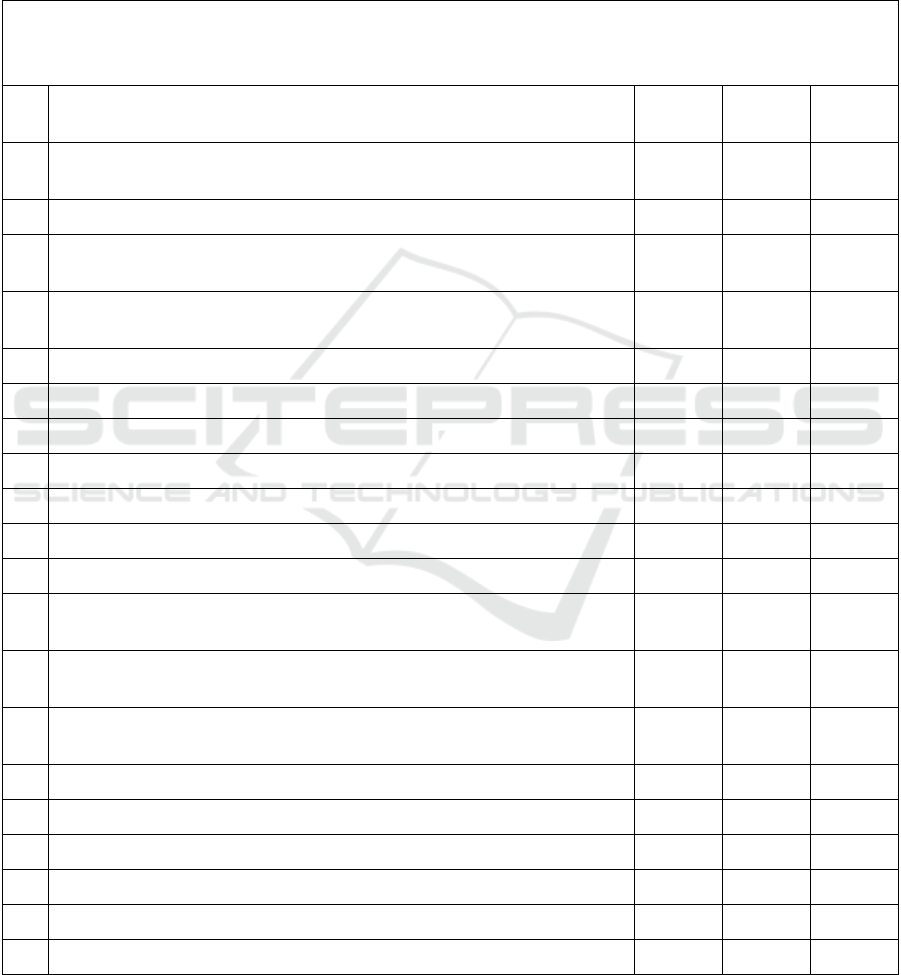
APPENDIX
the 20-item Firefighters’ Stress Trauma Exposure Experience Inventory
Instructions: Please select the number of times you have experienced the following events since your enlistment based on
your actual situation.
items 0 1 time
2 times or
more
1
Minor injuries sustained during training or missions (requiring medical
treatment but not hospitalization)
2 Seriously injured in training or missions (requiring hospitalization)
3
Witnessing a comrade slightly injured during training or mission (requiring
medical treatment but not hospitalization)
4
Witnessing a comrade seriously injured during training or mission (requiring
hospitalization for treatment)
5 Witnessing the death of a comrade in training or during a mission
6 Hearing the death of a comrade in training or during a mission
7 Participate in fire extinguishing with injuries or fatalities
8 Participate in flood, typhoon and other weather disaster rescues
9 Participate in earthquake, mudslide and other geological disaster rescues
10 Participate in traffic accident rescues
11 Rescue of suicides
12
Participate in the building (structure) and facilities and equipment collapse
accident disposals
13
Participate in the disposals of hazardous materials leaks, explosions and
poisoning
14
Participate in the disposals of pressure vessels, pipelines and other equipment
leaks and explosions
15 Rescues of burned or mutilated people
16 Rescues of seriously injured people
17 Rescues of minors
18 Witnessing the death of a minor during a mission
19 Witness/search/contact/carry bodies during the mission
20 Witness the fragmented bodies during the mission
Traumatic Rescue Experiences and Post-Traumatic Stress Disorder in Firefighters: The Moderating Roles of Inhibitory Control and
Cognitive Flexibility
163
The Post-traumatic Stress Disorder Scale (PCL-5)
Instructions: below is a list of problems that people sometimes have in response to a very stressful experience. Keeping
your worst event in mind, please read each problem carefully and then circle one of the numbers to the right to indicate
how much you have been bothered by that problem in the past month.
In the past month, how much were you
bothered by:
Not at all A little bit Moderately Quite a bit extremely
1 Repeated, disturbing, and unwanted
memories of the stressful experience?
0 1 2 3 4
2 Repeated, disturbing dreams of the stressful
experience?
0 1 2 3 4
3 Suddenly feeling or acting as if the stressful
experience were actually happening again (as
if you were actually back there reliving it)?
0 1 2 3 4
4 Feeling very upset when something reminded
you of the stressful experience?
0 1 2 3 4
5 Having strong physical reactions when
something reminded you of the stressful
experience (for example, heart pounding,
trouble breathing, sweating)?
0 1 2 3 4
6 Avoiding memories, thoughts, or feelings
related to the stressful experience?
0 1 2 3 4
7 Avoiding external reminders of the stressful
experience (for example, people, places,
conversations, activities, objects, or
situations)?
0 1 2 3 4
8 Trouble remembering important parts of the
stressful experience?
0 1 2 3 4
9 Having strong negative beliefs about
yourself, other people, or the world (for
example, having thoughts such as: I am bad,
there is something seriously wrong with me,
no one can be trusted, the world is
completely dangerous)?
0 1 2 3 4
10 Blaming yourself or someone else for the
stressful experience or what happened after
it?
0 1 2 3 4
11 Having strong negative feelings such as fear,
horror, anger, guilt, or shame?
0 1 2 3 4
12 Loss of interest in activities that you used to
enjoy?
0 1 2 3 4
13 Feeling distant or cut off from other people? 0 1 2 3 4
14 Trouble experiencing positive feelings (for
example, being unable to feel happiness or
have loving feelings for people close to
you)?
0 1 2 3 4
15 Irritable behavior, angry outbursts, or acting
aggressively?
0 1 2 3 4
16 Taking too many risks or doing things that
could cause you harm?
0 1 2 3 4
17 Being “superalert” or watchful or on guard? 0 1 2 3 4
18 Feeling jumpy or easily startled? 0 1 2 3 4
19 Having difficulty concentrating? 0 1 2 3 4
20 Trouble falling or staying asleep? 0 1 2 3 4
ICT4AWE 2025 - 11th International Conference on Information and Communication Technologies for Ageing Well and e-Health
164
