
SINONA (Ready to Deliver Your Medicine) Service for Outpatients
at Health Service Center
Haedar Akib
1 a
, Andi Selvi Kartini Wonsu
2
, Didin
1 b
, Andi Muhammad Rivai
1 c
and
Khairil
Asnan Haedar
3 d
1
Department of Administration Science, Universitas Negeri Makassar, Makassar City, South Sulawesi, Indonesia
2
La Mappapenning Regional Hospital, Bone Regency, South Sulawesi, Indonesia
3
Department of Biological Sciences, Khon Kaen University, Mueang Khon Kaen, Khon Kaen, Thailand
Keywords: SINONA, Medicine Delivery Service, Outpatients, Healthcare Innovation, Public Service Evaluation.
Abstract: This study aims to evaluate the feasibility, effectiveness, and user perceptions of SINONA in enhancing
healthcare service delivery at La Mappapenning Regional Hospital, Bone, Indonesia. A qualitative-
phenomenological approach was employed, involving semi-structured interviews with 12 patients and 3
employees, supported by observational data. The study analyzed user awareness, perceptions, and service
quality using Rogers' innovation diffusion theory as a conceptual framework. Findings reveal that SINONA
improves accessibility and patient satisfaction, particularly for those with time constraints or mobility
challenges, by delivering medications safely and promptly. Despite these benefits, challenges such as delivery
delays and limited interaction with pharmacists were identified, reflecting variability in user perceptions. The
study highlights the service's potential to enhance healthcare equity and efficiency through innovative
logistics and technology integration while recommending continuous user education, inclusivity, and system
optimization. SINONA exemplifies the modernization of healthcare services aligned with social justice and
contemporary public health needs.
1 INTRODUCTION
Outpatient medicine delivery is a response to
challenges faced in traditional health systems, such as
long queues at pharmacies, limited physical access,
and geographical disparities. This innovation not only
increases efficiency but also encourages better quality
of health services, with a more personalized approach
based on patient needs. Through the analysis of the
philosophical, theoretical, and normative
perspectives cited in this article, outpatient medicine
delivery innovation is not just a technical change, but
also a real manifestation of efforts to create social
justice, improve community welfare, respond to the
challenges of the times with adaptive and inclusive
technology-based solutions. Therefore, innovation in
public services in the health sector, especially in
medicine delivery, is one of the strategic steps to
a
https://orcid.org/0000-0003-3821-0583
b
https://orcid.org/0009-0004-1664-1395
c
https://orcid.org/0009-0000-8458-5787
d
https://orcid.org/0000-0001-6695-5422
increase the accessibility and efficiency of health
services for the community. This innovation can
ensure that patients receive medicines quickly, safely,
and on time, especially in times of emergency or for
patients living in remote areas. Nevertheless, the
results of preliminary research on the benefits,
suitability, complexity, replication intensity, and
testing of the results of the SINONA (Siap Antar Obat
Anda / Ready to Deliver Your Medicine) service
innovation are perceived differently by each patient
because of their different characteristics (gender, age,
type of work, perception of disease, time, place,
behavioral ethics, and standards of service quality
received). Therefore, this study explains the urgency
and perspective of implementing Sinona service
innovation in health service center. The concept of
innovation according to Rogers (2002) is applied in
this normative research which includes dimensions,
Akib, H., Wonsu, A. S. K., Didin, , Rivai, A. M. and Haedar, K. A.
SINONA (Ready to Deliver Your Medicine) Service for Outpatients at Health Service Center.
DOI: 10.5220/0013421000004654
In Proceedings of the 4th International Conference on Humanities Education, Law, and Social Science (ICHELS 2024), pages 753-760
ISBN: 978-989-758-752-8
Copyright © 2025 by Paper published under CC license (CC BY-NC-ND 4.0)
753
namely: 1) Relative Advantage: Innovation has
advantages compared to old solutions; 2)
Compatibility: Innovation is by the values, norms,
and practices of the social environment; 3)
Complexity: The level of difficulty or complexity in
adopting innovation; 4) Trialability: The ability to test
innovation before deciding to adopt it permanently;
5) Observability: The ability to see the results of the
use of innovation by others. These indicators help
researchers see a picture of innovation that is
understood and accepted by the community and
ultimately shows the level of success of the
dissemination of innovation at a certain level, context,
and locus.
The results of this normative (literature) research are
expected to provide benefits to various interested
parties both theoretically and practically.
Theoretically, it enriches the scope of public
administration and administrative development as a
focus of scientific study in the form of medicine
delivery innovations based on the use of new
technology, logistics, and processes that ease the
medicine distribution from healthcare facilities (such
as hospitals, pharmacies, or health center) to the
patient. Likewise, this innovation revitalizes the
function of application-based delivery services
through collaboration (actor collaborative
partnerships) with local delivery services or even the
use of drones in hard-to-reach areas.
Practically, the results of this study provide benefits
for both service providers and recipients to ameliorate
both accessibility and acceptability, particularly for
those living in distant places or with limited mobility,
find it difficult to acquire medicine swiftly and
directly. Additionally, it help promotes satisfaction
among patients by saving their time, energy, and
minimizes queue at medical facilities.
2 METHOD
Qualitative-phenomenological study employed at
The Regional Hospital La Mappapenning in Bone,
Indonesia (-4.731807, 120.056417), targeting about
30 random patients queued at the pharmacy section of
the hospital. Sociodemographic (domicile,
occupation, sex, and transport type), awareness, and
perception to the Sinona service were collected by
semi-administered interview. The interview and
observation guidelines developed according to
Balanced Score Card (BSC) at Peel Memorial
Hospital in Vancouver Canada, and Mayo Clinic in
the United States (Griffith et al., 2002; Riwu &
Wibowo, 2021; Sharma, 2009; A. R. Taufik, 2018),
which emphasized the managerial aspects, user
perspective, and sustainable organizational processes
(see Table 1).
Data collecting process conducted on July 8
th
to 15
th
,
2024 (6 respondents per day). Interview notes were
evaluated to identify biases. Finally, about 12
responses analyzed using interactive model (Miles et
al., 2014) which includes data collection, data
condensation, data presentation, verification, and
drawing conclusions, consecutively. The remaining
18 responses were excluded due to possible bias in
the response. Among the responses, 8 quoted as the
Sinona user. Moreover, another response obtained
from 3 employees from the pharmacy section
(collected from 3 different shifts), which elucidated
the managerial aspects of Sinona service. All
interview were scheduled with the interviewees
outside the hospital to ensure confidentiality.
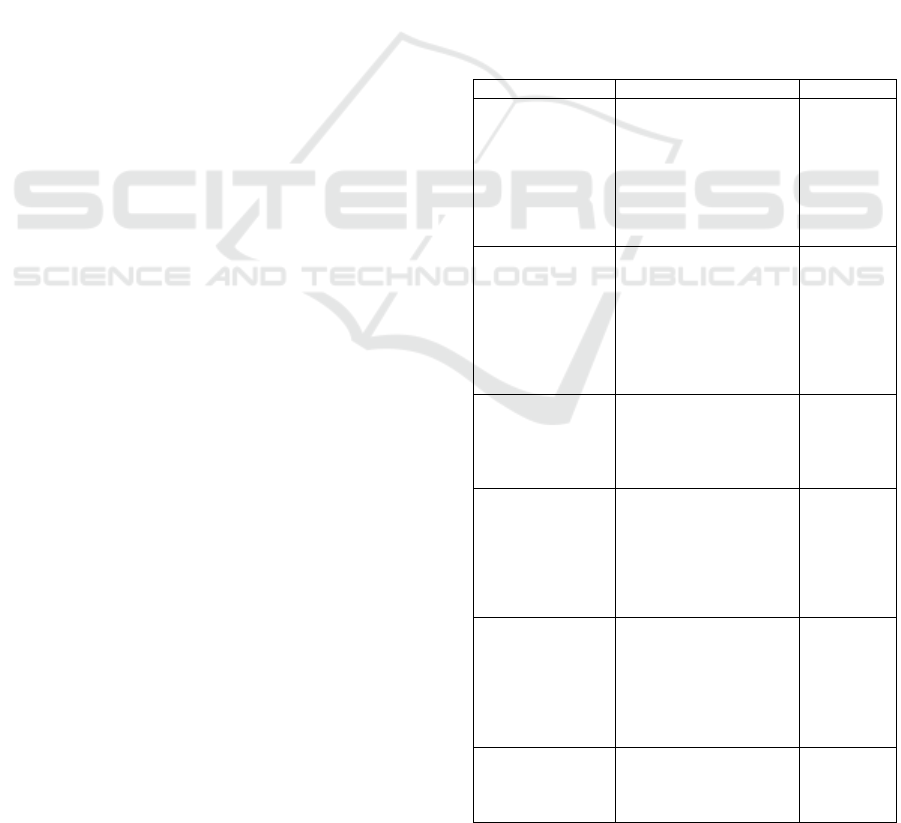
Table 1. Interview guidelines for patients and employees
Dimension
Question [item coding]
Purpose
Sociodemographic
What is your current
occupation? [Sc1]
To gather
backgroun
d
informatio
n on the
respondent'
s work
profile.
What is your mode of
transportation when
accessing health
facilities? [Sc2]
To
understand
logistical
constraints
related to
accessing
health
services.
How far is your
residence from the
hospital (in kilometers or
minutes of travel)? [Sc3]
To assess
geographic
al
accessibilit
y.
How busy do you
acknowledge yourself to
wait and follow all the
process here? [Sc4]
To
consider
whether
the users
are
workaholic
or not
Awareness
Have you heard of the
Sinona service before
this interview? [Aw1]
To
determine
awareness
levels
about the
Sinona
service.
If yes, how did you learn
about the Sinona
service? [Aw2]
To identify
the
communica
tion
ICHELS 2024 - The International Conference on Humanities Education, Law, and Social Science
754
channels
effectively
used for
awareness.
Perception of
Service
What do you think are
the advantages of using
the Sinona service?
[Pc1]
To explore
perceived
benefits.
What challenges do you
associate with using the
Sinona service? [ Pc2]
To
understand
barriers to
adoption.
Do you feel the Sinona
service aligns with your
health and lifestyle
needs? Why or why not?
[Pc3]
To assess
compatibili
ty with
personal
values and
practices.
Service Quality
Have you faced any
issues with the safety or
packaging of the
medicines delivered?
[Sq1]
To assess
the quality
and safety
measures
of the
service.
Would you recommend
the Sinona service to
others? Why or why not?
[Sq2]
To
understand
overall
satisfaction
and
likelihood
of positive
word-of-
mouth.
Does the payment
worth? [Sq3]
To
understand
why they
choose the
service
rather than
to wait at
the hospital
Managerial
Aspects (*)
What role do pharmacy
staff play in ensuring the
success of the Sinona
service? [Mg1]
To explore
operational
dependenci
es and
bottlenecks
.
How are the delivery
schedules determined
and coordinated? [Mg2]
To
understand
the
logistics
and
manageme
nt of the
service.
What measures are in
place to ensure
confidentiality and safety
of patient information?
[Mg3]
To assess
compliance
with
privacy
and data
protection
standards.
*only for employees
Furthermore, normative study employed by
observation. Several key points observed regarding
the implementation of Sinona service, related to it’s
compliance with the Law and public service
perspective (see below).
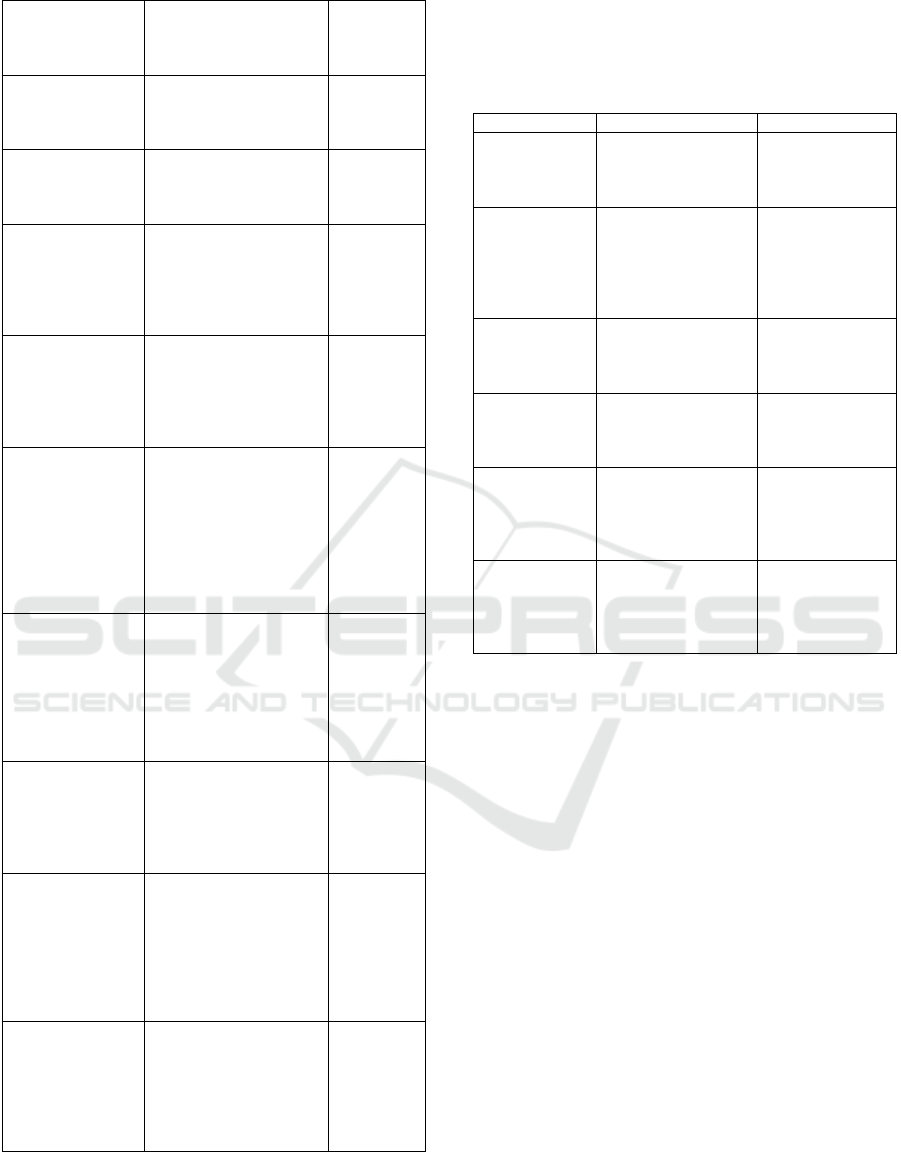
Table 2. Observational card
Category
Aspect to Observe
Das Sollen
Legal
Framework
Compliance with
Law Number 17 of
2023 concerning
Health. [Comp1]
Required to obey
the law
Compliance with
Minister of Health
Regulation Number
72 of 2016 on
Pharmaceutical
Standards. [Comp2]
Meet all delivery
timelines and
service standards.
Implementation
Mechanisms
ensuring quality and
safety of medicine
delivery. [Imp1]
Medicine
handling for
special cases
Delivery timelines
and adherence to
service standards.
[Imp2]
Medicine
handling for
special cases
Innovative
Practices
Collaboration with
third-party delivery
services or adoption
of new technologies
(e.g., drones). [Ivp1]
Ensure inclusivity
in the term of
business
Feedback
mechanisms for
ensuring continuous
service improvement.
[Ivp2]
Personal
confidentality
3 RESULT AND DISCUSSION
3.1 Awareness
About 8 of 12 respondents were Sinona user, which
access the hospital either by bike or car (n = 6 / 2).
Respondents were lived more than 5 to more than 10
kilometers or about 15 to 30 minutes of travel to the
hospital. All respondents occupation were time
consuming (need to work from office/field), which
generally elaborated in their response to Sc4 as, “… i
need to go home quickly to rest … waiting here just
make me sore …” We found that the hospital has only
been operating for 1 year, so majority of the patients
were not from the local community.
3.2 Perception
Sinona were presented as an additional service by the
new operated hospital. As a flagship program, all
employee are responsible to promote the service.
Respondent revealed that they easily found posters
advertising Sinona. Moreover, employees will tell
SINONA (Ready to Deliver Your Medicine) Service for Outpatients at Health Service Center
755

them at the time they handed the receipt. Patient tell,
“… they told us that if we do not wish to wait for the
medicine, we could use the service and pay later at
home …” Philosophically, innovation in health
services in outpatient medicine delivery refers to the
"principle of utilitarianism" (collective welfare),
social justice, and humanism in public service. In
utilitarian ethical theory, it is taught that the right
action produces the greatest benefit for the greatest
number of people. Innovation in medicine delivery
allows more patients, especially those who do not
have time or are unable to come to health facilities, to
get access to the medicines they need (Abu-Farha et
al., 2022; Damaralam, 2020).
The Sinona service provides significant benefits for
individuals seeking convenience and time-saving
solutions when it comes to medication delivery. One
of the main advantages mentioned by users is the ease
of receiving prescriptions without having to visit the
hospital or pharmacy in person. As one respondent
shared, "… i no longer need to wait in long queues at
the pharmacy or hospital, which saves me both time
and energy …" Additionally, users appreciate the
comfort of having their medications delivered
directly to their homes, especially those with mobility
issues or busy schedules. "… being able to have my
medicine delivered right to my doorstep means, i
don't have to take time off work or arrange for
transportation …" one individual noted. This added
level of convenience significantly enhances users'
experience, as it removes barriers like transportation,
long waiting times, and accessibility challenges. The
urgency of this innovation is based on Rawls' (2020)
view that a good social system must ensure an
equitable allocation of resources, particularly for the
most disadvantaged populations, as a reflection of
moral principles. Medicine delivery for outpatients is
a form of distributive justice in which health care are
readily available to everybody, regardless of
geographic location or socioeconomic status, which
also reflects to the "principle of humanism," which
emphasizes the need of honoring human dignity while
satisfying fundamental requirements.
Theoretically, innovation in public health services in
the case of medicine delivery is important because it
teaches changes designed to improve individual and
institutional performance and the effectiveness of
government service delivery, as stated “ … as
someone with a chronic illness, i often find it difficult
to leave the house. Sinona's service allows me to
manage my health without the added stress of going
to the pharmacy …" According to experts (Bloch &
Bugge, 2013; Gow, 2014; Misuraca & Viscusi, 2015),
innovation occurs through the use of technology,
organizational change, and the development of new
service models. The mechanism of digital-based
medicine delivery through applications and virtual or
Internet of Things regulatory systems (Sopyan et al.,
2023) is one example of the application of public
service innovation theory. This method not only
increases the effectiveness of services but also makes
services more responsive to community needs.
3.3 Service Quality
According to experts (Denhardt et al., 2018;
Gruening, 2001), the efficiency, effectiveness, and
responsiveness of services are carried out by adapting
private sector management practices based on the
theory of New Public Management (NPM) or the
theory of New Public Service (NPS) based on the
theory of democracy. In the context of SINONA (Siap
Antar Obat Anda/ Ready to Deliver Your Medicine)
service innovation, the use of technology and an
organized delivery system is expected to increase the
efficiency of the distribution process, accelerate
services, reduce the administrative burden on health
facilities, increase accountability and transparency in
public services, and satisfy service recipients. Users
appreciate the ability to bypass long queues at
pharmacies and have medications delivered directly
to their homes, a feature especially valuable for those
with mobility challenges or chronic conditions.
However, the service faces skepticism from non-
users, who express concerns about reliability, such as
timely delivery and medication safety, as stated “… i
would consider using the service if i could be sure the
medication would arrive safely and on time …” This
suggests that while the service offers substantial
convenience, it may not yet have gained the trust of
everyone, particularly those unfamiliar with the
platform or who have concerns about delivery
logistics.
Despite its benefits, the Sinona service is not without
challenges. Delivery delays and the lack of personal
interaction with pharmacists are common criticisms
among users, with some finding the absence of in-
person advice a drawback, as mentioned by the
respondent “ … once, i needed a prescription
urgently, but the delivery took longer than expected,
which was stressful …” Moreover, “… i miss the
personal interaction with my pharmacist when
getting advice about my medication …”
The urgency of this new public service is based on the
theory of digital public services (Bertot et al., 2016)
which teaches that public services are modernized
ICHELS 2024 - The International Conference on Humanities Education, Law, and Social Science
756

through the use of digital technology. Medicine
delivery through online platforms or mobile
applications reflects the trend of digitalization of
public services which aims to accelerate access,
reduce disparities, and provide more efficient and
transparent services. As per today, ease of access is
necessary and demanded. Respondent states that, “ …
the service fits perfectly with my lifestyle because i
work long hours and don't have time to visit a
pharmacy …”. However, concern to the inclusivity
on the hospital emphasized by the non-user, “… we
don’t want that the service will only be good for those
who pays more for the service …”. Subsequently, “…
the service should be fast, because it is their
responsibility and indeed their evaluation criteria.
Offering delivery service should be the second option
when they are overloaded or something urgent …”.
3.4 Legal Compliance
The normative basis for medicine delivery services
for hospital patients in Indonesia is Law Number 17
of 2023 concerning Health. This law regulates the
right of everyone to obtain health services, including
access to medicines. It also regulates the distribution
of medicines by health service standards.
Furthermore, it stipulates that hospitals must provide
comprehensive services, including pharmaceutical
services. Hospitals are required to provide safe,
quality, anti-discriminatory, and effective health
services, including medicine delivery.
On the administrative side, not all medicine can
delivered by Sinona service. Some medicine required
special handling, such as narcotics or psychotropic
containing drugs, as mentioned by the employees, “
… we need to ensure that the medicine delivered only
for generic purposes and does not require special
handling …”, additionally, “ … pharmacy staff
double-check my prescriptions, which gives me
confidence that I'm receiving the right medication
every time …”. Checking the right medicine as
written on the receipt is necessary in the process. That
is aligned with the Regulation of the Minister of
Health Number 72 of 2016 concerning Standards of
Pharmaceutical Services in Hospitals emphasized
that psychotropics need special handling. It also
regulates the standards for medicine distribution from
hospital pharmacy installations, including the
mechanism for delivering medicines to patients.
Moreover, as per Regulation of the Minister of Health
Number 9 of 2017 concerning Pharmacies. It is
stipulated that pharmacies can provide medicine
delivery services to patients with procedures that
must guarantee medicine quality and speed of service.
One of the key responsibilities of the pharmacists is
verifying prescriptions to ensure they are valid and
legally authorized, in compliance with both national
and international pharmaceutical regulations, as
stated "… the pharmacy staff ensures that my
prescription is valid before sending it out for delivery,
which reassures me that everything is being done
legally and safely …". Additionally, pharmacy staff
are required to maintain accurate records of all
transactions, as mandated by law, ensuring proper
documentation and traceability of every prescription.
This legal oversight helps ensure that the service
operates within the boundaries of the law, preventing
the misuse or mishandling of medications, while also
protecting patients from potential legal and health
risks. The regulation is a strong legal basis to support
and regulate medicine delivery services to patients in
Indonesia.
Experts and researchers (Kaplan & Norton, 2001;
Riwu & Wibowo, 2021; Sharma, 2009; A. R. Taufik,
2018; Vitezić et al., 2019) previously understood that
innovation as one of the dimensions to measure
organizational (institutional) performance.
Furthermore, it is stated that efficient and effective
public health service performance-innovation
measurement should be able to translate the
organization's mission, vision, and strategy into
operational goals and performance measures, both
financial and non-financial performance measures.
2.2 Discussion
As a developing nation, Indonesia always struggles
with the issue of limited public access to high-quality,
reasonably priced healthcare. Even though there have
been numerous approaches and initiatives up to this
point, including public health services, increased
investment in health services, improved service
quality, and decentralization of the health system. The
awareness of Sinona among users and non-users
indicates that the service has been effectively
promoted, leveraging tools such as posters and direct
communication by hospital staff. Despite being a
relatively new initiative from a newly established
hospital, the majority of respondents were aware of
the service. Expert studies (Ruliansyah, 2017; Siti et
al., 2019; Zulu et al., 2015) revealed that the main
cause of all these health problems lies in the limited
access of the community to a reliable social-health
security system. This aligns with the utilitarian
philosophy of maximizing collective welfare and
improving access to healthcare services. Nonetheless,
some non-users remain hesitant due to concerns over
reliability, delivery timeliness, and medication safety.
SINONA (Ready to Deliver Your Medicine) Service for Outpatients at Health Service Center
757

This skepticism underscores the need for the service
to build greater trust and address these concerns
comprehensively.
Data reveals mixed feedback regarding the quality of
service provided by Sinona. Users appreciated the
convenience and accessibility offered by the service,
they also raised concerns about delivery delays and
the lack of personal interaction with pharmacists. For
many patients, particularly those with chronic
illnesses, the ability to receive medications without
leaving their homes significantly enhances their
healthcare experience. However, the absence of
personalized consultations with pharmacists
diminishes the service’s perceived value. Non-users
also echoed concerns about medication accuracy and
quality assurance. Those concerns aligned with the
facts that health and social security are the main
instruments and prerequisites for overcoming
poverty, economic growth, and development, which
requires coherent and effective policies (Rahman,
2018; Rosyadi, 2015; Setiawan, 2017).
Health service innovation is a future investment to
improve the quality of human resources (HR),
support sustainable development in the health sector,
and play an important role in poverty alleviation
efforts (Arsyad et al., 2020; Dwiyanto & Jemadi,
2013). Health sector development is directed at
improving the quality, equity, and affordability of
health services for the public. Public health services
in the current digital era are characterized by
competition, independence, and innovation in various
fields and levels of the organization (Lavoie ‐
Tremblay et al., 2017; Lee et al., 2018; A. Putra et al.,
2017; R. M. D. Putra, 2018; Zulu et al., 2015). Health
services do not only rely on accessibility,
acceptability, and patient satisfaction (Ali, 2016;
Faezipour & Ferreira, 2013; Hsieh & Kagle, 1991;
Prasojo, 2017; Raivio et al., 2014; Ruliansyah, 2017;
M. Taufik et al., 2017), but also involve
responsiveness to demands for quality health services
which are the main needs for most of the population
or citizens. Likewise, the increasingly fierce
competition between public service providers
requires innovative ideas to be able to meet shared
expectations in all aspects of life.
Innovation in public health services is one form of
effort to improve the quality of people's lives. This
innovation is understood as the application of the
concept of social justice, efficiency, and state
responsibility in realizing general welfare. Thus,
medicine delivery for outpatients is a form of
creativity-based innovation that reflects a change in
the paradigm of health services towards a more
inclusive, responsive, and technology-based system.
Based on the understanding of experts and
researchers, research on innovation in public health
services in medicine delivery for outpatients is
approached through various perspectives of
innovation theory. Innovation according to (Rogers,
2002) can be applied in public services at certain loci,
including in the health sector by carrying out five
stages in its dissemination, namely: 1) awareness
stage, 2) understanding stage, 3) evaluation stage, 4)
adoption stage, and 5) consolidation stage.
Meanwhile, its application in health services includes
efforts to: 1) ensure that health professionals
understand the innovation and its benefits, 2)
facilitate evaluation by health professionals of the
effectiveness and safety of the innovation, 3) ensure
that the innovation is easy to use and practice by
health professionals, and 4) help health professionals
to integrate the innovation effectively into their work
practices at health service centers (hospitals, health
centers).
According to experts and researchers (Gani et al.,
2021; Hafizh, 2016; Purwanto et al., 2020; Syam et
al., 2018) hospitals are service centers that have
greater value-added service for patients, customers,
employees, and the community that support local,
regional, and national economic growth when their
management is based on creativity and innovation
that is valuable to the public. Therefore, to assess the
success of the service innovation being implemented,
it is necessary to conduct research at the locus of the
Regional Technical Implementation Unit (UPTD) of
the La Mappapenning Regional General Hospital
(RSUD) in Bone Regency, because some consider
that several hospitals with the status of public service
agencies (BLU) still only focus on the success of their
service programs on financial aspects and equal
distribution of services alone.
Experts and researchers (Abu-Farha et al., 2022;
Damaralam, 2020; Lavoie‐Tremblay et al., 2017;
Nolte & Organization, 2018; A. Putra et al., 2017; R.
M. D. Putra, 2018; Suwarno, 2008; Zulu et al., 2015)
stated that innovation in public sector services,
including medicine delivery services for hospital
patients, is a breakthrough in overcoming the
pathology of public administration and health
services in certain loci, including at the Regional
Hospital La Mappapenning. Bertucci (2004), stated
that the importance of innovation in public sector
services is based on considerations of
democratization of services, international
agreements, the occurrence of imbalances in the
ICHELS 2024 - The International Conference on Humanities Education, Law, and Social Science
758

distribution of superior human resources, better
bureaucratic order, privatization, and outsourcing in
organizations (institutions). Furthermore, innovation
in public health services is implemented to increase
efficiency and effectiveness and reduce waste of
budget spending because public sector organizations
are faced with a scarcity of resources and budget
constraints (Mochammad, 2019; Muluk, 2015).
4 CONCLUSIONS
The findings of this study emphasize the significant
potential of the SINONA innovation in transforming
healthcare service delivery through enhanced
accessibility and efficiency. SINONA offers clear
advantages over traditional methods, aligning with
community values while addressing challenges such
as geographic and logistical barriers. Despite varying
perceptions based on patient characteristics,
SINONA demonstrates its feasibility and
effectiveness in ensuring timely, safe, and equitable
medicine delivery. This innovation not only
contributes to improving public health outcomes but
also represents a critical step toward advancing
inclusive, adaptive, and collaborative health service
innovations that align with contemporary
technological advancements and social justice goals.
Further improvements also require to address the
complexities and challenges associated with the
adoption and implementation of SINONA. These
include enhancing user education to improve
understanding and acceptance, streamlining
technology to ensure ease of use, and promoting
inclusive partnerships with delivery services to
expand reach, particularly in remote or underserved
areas. Moreover, continuous evaluation and feedback
mechanisms should be integrated to adapt the service
to diverse patient needs and ensure equitable access.
ACKNOWLEDGEMENTS
Special thanks to UPTD RSUD La Mappapenning
Hospital for data collection and technical assistance.
Their extraordinary contributions have greatly
improved the quality of this thesis paper.
REFERENCES
Abu-Farha, R., Alzoubi, K. H., Rizik, M., Karout, S., Itani,
R., Mukattash, T., & Alefishat, E. (2022). Public
perceptions about home delivery of medication service
and factors associated with the utilization of this
service. Patient Preference and Adherence, 2259–
2269. https://doi.org/10.2147/PPA.S377558
Ali, D. A. (2016). Patient satisfaction in dental healthcare
centers. European Journal of Dentistry, 10(03), 309–
314.
Arsyad, M., Pulubuhu, D. A. T., Kawamura, Y., Maria, I.
L., Dirpan, A., Unde, A. A., Nuddin, A., & Yusuf, S.
(2020). The role of public health services (PHS) in
agricultural poverty alleviation. Enfermeria Clinica,
30, 194–197.
Bertot, J., Estevez, E., & Janowski, T. (2016). Universal
and contextualized public services: Digital public
service innovation framework. Elsevier.
Bertucci, G. (2004). The UNDESA/IASIA initiative for
public sector leadership capacity enhancement.
International Review of Administrative Sciences,
70(4), 685–691.
Bloch, C., & Bugge, M. M. (2013). Public sector
innovation - From theory to measurement. Structural
Change and Economic Dynamics, 27, 133–145.
Damaralam, F. (2020). Analisis Niat Penggunaan Layanan
Antar Obat Online: Studi Kasus Halodoc. Universitas
Teknologi Sepuluh November.
Denhardt, R. B., Denhardt, J. V, Aristigueta, M. P., &
Rawlings, K. C. (2018). Managing human behavior in
public and nonprofit organizations. Cq Press.
Dwiyanto, B. S., & Jemadi, J. (2013). Pemberdayaan
masyarakat dan pengembangan kapasitas dalam
penanggulangan kemiskinan melalui PNPM mandiri
perkotaan. Jurnal Maksipreneur: Manajemen,
Koperasi, Dan Entrepreneurship, 3(1), 36–62.
Faezipour, M., & Ferreira, S. (2013). A system dynamics
perspective of patient satisfaction in healthcare.
Procedia Computer Science, 16, 148–156.
Gani, H. A., Akib, H., Mukmin, A., & Bare, R. R. (2021).
Public Entrepreneurship.
Gow, J. I. (2014). Public sector innovation theory
revisited1. The Innovation Journal, 19(2), 1.
Gruening, G. (2001). Origin and theoretical basis of New
Public Management. International Public
Management Journal, 4(1), 1–25.
Hafizh, D. A. (2016). Inovasi Pelayanan Publik; Studi
Deskriptif tentang Penerapan Layanan e-Health dalam
meningkatkan Kualitas Pelayanan Kesehatan di
Puskesmas Pucangsewu Kota Surabaya. Kebijakan
Dan Manajemen Publik, 4(3).
Hsieh, M., & Kagle, J. D. (1991). Understanding patient
satisfaction and dissatisfaction with health care. Health
& Social Work, 16(4), 281–290.
Kaplan, R. S., & Norton, D. P. (2001). Transforming the
balanced scorecard from performance measurement to
strategic management: Part 1. Accounting Horizons,
15(1), 87–104.
SINONA (Ready to Deliver Your Medicine) Service for Outpatients at Health Service Center
759

Lavoie‐Tremblay, M., Aubry, M., Cyr, G., Richer, M.,
Fortin‐Verreault, J., Fortin, C., & Marchionni, C.
(2017). Innovation in health service management:
Adoption of project management offices to support
major health care transformation. Journal of Nursing
Management, 25(8), 657–665.
Lee, E., Hamelin, T., & Daugherty, J. (2018).
Globalization of health service: sharing of best
practices in perianesthesia nursing care, a case study of
cross-border institutional collaboration. Journal of
PeriAnesthesia Nursing, 33(2), 209–219.
Miles, M. B., Huberman, A. M., & Saldana, J. (2014).
Qualitative data analysis: A methods sourcebook.
Thousand Oaks, CA: Sage.
Misuraca, G., & Viscusi, G. (2015). Shaping public sector
innovation theory: an interpretative framework for
ICT-enabled governance innovation. Electronic
Commerce Research, 15, 303–322.
Mochammad, R. (2019). Inovasi Pelayanan Publik.
KEMUDI: Jurnal Ilmu Pemerintahan, 4(1), 1–20.
Muluk, M. R. K. (2015). Budaya Organisasi Pelayanan
Publik. Jurnal Manajemen Pelayanan Kesehatan,
8(1), 8–20.
Nolte, E., & Organization, W. H. (2018). How do we
ensure that innovation in health service delivery and
organization is implemented, sustained and spread?
Prasojo, A. (2017). Pengaruh Fasilitas, Kualitas Pelayanan,
dan Aksesibilitas Terhadap Kepuasan Pasien di Rumah
Sakit Gigi dan Mulut Institut Ilmu Kesehatan Bhakti
Wiyata Kediri. Simki-Economic, 1(11), 2–6.
Purwanto, A., Asbari, M., Prameswari, M., Ramdan, M.,
& Setiawan, S. (2020). Dampak Kepemimpinan,
Budaya Organisasi dan Perilaku Kerja Inovatif
Terhadap Kinerja Pegawai Puskesmas. Jurnal Ilmu
Kesehatan Masyarakat, 9(01), 19–27.
Putra, A., Usman, J., & Abdi, A. (2017). Inovasi Pelayanan
Publik Bidang Kesehatan Berbasis Home Care Di Kota
Makassar. Kolaborasi: Jurnal Administrasi Publik,
3(3), 294–309.
Putra, R. M. D. (2018). Inovasi Pelayanan Publik Di Era
Disrupsi (Studi Tentang Keberlanjutan Inovasi E-
Health Di Kota Surabaya). Universitas Airlangga.
Rahman, H. (2018). Potret Pertumbuhan Ekonomi,
Kesenjangan Dan Kemiskinan Di Indonesia Dalam
Tinjauan Ekonomi Politik Pembangunan. Jurnal Ilmu
Dan Budaya, 40(55).
Raivio, R., Jääskeläinen, J., Holmberg-Marttila, D., &
Mattila, K. J. (2014). Decreasing trends in patient
satisfaction, accessibility and continuity of care in
Finnish primary health care–a 14-year follow-up
questionnaire study. BMC Family Practice, 15(1), 1–
7.
Rawls, J. (2020). Political liberalism. In The New Social
Theory Reader (pp. 123–128). Routledge.
Riwu, S. L., & Wibowo, A. (2021). Penilaian Kinerja
Rumah Sakit Dengan Menggunakan Pendekatan
Balanced Scorecard: Systematic Review. Jurnal
Manajemen Kesehatan Yayasan RS. Dr. Soetomo,
7(2), 267–283.
Rogers, E. M. (2002). Diffusion of preventive innovations.
Addictive Behaviors, 27(6), 989–993.
https://doi.org/10.1016/s0306-4603(02)00300-3
Rosyadi, K. (2015). Islam, Modal Sosial, Pembangunan
dan Pengentasan Kemiskinan. DIMENSI-Journal of
Sociology, 8(1).
Ruliansyah. (2017). Pengaruh Tingkat Kualitas Pelayanan
dan Aksesibilitas Fasilitas Pelayanan Kesehatan
Puskesmas Terhadap Kepuasan Pasien (Studi Pada
Puskesmas II Purwokerto Utara). Universitas Jenderal
Soedirman.
Setiawan, H. H. (2017). Penanggulangan Kemiskinan
Melalui Pusat Kesejahteraan Sosial. Sosio Informa:
Kajian Permasalahan Sosial Dan Usaha
Kesejahteraan Sosial, 3(3).
Sharma, A. (2009). Implementing balance scorecard for
performance measurement. ICFAI Journal of Business
Strategy, 6(1), 7–16.
Siti, I., Siahaan, S., Wanggae, G., Widyasari, R.,
Kurniawan, A., Aryastami, N. K., & Pratiwi, N. L.
(2019). Dinamika jender terhadap akses pelayanan
kesehatan maternal sembilan etnis di Indonesia.
Buletin Penelitian Sistem Kesehatan, 22(1), 1–9.
Sopyan, E., Suarna, D., & Ashar, M. H. (2023). Rancang
Bangun Robot Pengantar Obat dan Makanan Pasien
Berbasis Internet of Things. Bulletin of Information
Technology (BIT), 4(3), 344–352.
Suwarno, Y. (2008). Inovasi di Sektor Publik. STIA-LAN
Jakarta.
Syam, H., Akib, H., Patonangi, A. A., & Guntur, M.
(2018). Principal Entrepreneurship Competence Based
on Creativity and Innovation at the Context of
Learning Organizations in Indonesia. Journal of
Entrepreneurship Education, 21(3), 1–13.
Taufik, A. R. (2018). Pengukuran Kinerja Melalui
Balanced Scorecard (Bsc)(Studi Kasus Pada Tiga
Rumah Sakit Di Pasuruan). Universitas Brawijaya.
Taufik, M., Susilastuti, D. H., & Kurniawan, A. (2017).
Perbandingan Kepuasan Pasien terhadap Pelayanan
Kesehatan Menurut Aksesbilitas Wilayah (Kasus
Kecamatan Sungai Lilin Dan Kecamatan Tungkal Jaya
Kabupaten Musi Banyuasin, Sumatera Selatan).
Majalah Geografi Indonesia, 29(2), 154–162.
Vitezić, N., Setnikar Cankar, S., & Linšak, Ž. (2019).
Effectiveness measurement using DEA & BSC
methods in public health services. The NISPAcee
Journal of Public Administration and Policy, 12(1),
199–216.
Zulu, J. M., Hurtig, A.-K., Kinsman, J., & Michelo, C.
(2015). Innovation in health service delivery:
integrating community health assistants into the health
system at district level in Zambia. BMC Health
Services Research, 15(1), 1–12.
ICHELS 2024 - The International Conference on Humanities Education, Law, and Social Science
760
