
Towards Value Awareness in the Medical Field
Manel Rodriguez-Soto
1
, Nardine Osman
1
, Carles Sierra
1
, Paula S
´
anchez Veja
2
, Rocio Cintas Garcia
2
,
Cristina Farriols Danes
2
, Montserrat Garcia Retortillo
2
and Silvia Minguez Maso
2
1
Artificial Intelligence Research Institute (IIIA-CSIC), Barcelona, Spain
2
Hospital del Mar Research Institute (IMIM), Barcelona, Spain
{psanchezveja, rncintasgarcia, cfarriols, mgarciaretortillo, sminguez}@psmar.cat
Keywords:
Value Awareness, Value Alignment, Medical Protocols, Medical Corpus.
Abstract:
This position paper aims to illustrate how models and mechanisms can be designed to support value-aware
decision-making in the medical field. Such models and mechanisms allow for assessing the alignment of spe-
cific behaviours with human values, which could help medical personnel decide when to follow or break a
protocol and help relevant boards decide when and how to update existing protocols. AI supporting decision-
making in medicine is not new. Yet, AI that raises awareness about the alignment of medical decisions con-
cerning human values is novel despite the vital importance of bioethics in the field. This paper presents a
proposal for the formalisation of values and the design of models and mechanisms that raise value awareness
in the medical field.
1 INTRODUCTION
With the growing risks and fears of AI, developing
ethical AI has become a top objective of many gov-
ernmental bodies, organisations, and AI scientists.
One approach for achieving ethical AI is ensuring
AI that aligns with human values. Stuart Russell
argues that we should change the overarching goal
of AI from “intelligence” to “intelligence provably
aligned with human values” (Russell, 2019), a topic
now known as the value alignment problem.
The ultimate goal of this research is to develop
models and mechanisms for value-aware situation
analysis and decision-making. The objective is to
have AI systems that are aware of our value sys-
tems and can explain their behaviour or understand
the behaviour of others in terms of those value sys-
tems. In other words, in addition to AI being aware
of human values and reasoning with them, it can help
humans become aware of the alignment of their be-
haviour with different values. The latter is what this
paper is working towards, using AI to support medical
decision-making by raising value awareness.
The Hippocratic Oath is still considered today to
be a cornerstone and foundation of the medical pro-
fession across the world. It reflects the moral values
that define the medical profession, and some (Aski-
topoulou and Vgontzas, 2018) considered it to have
exemplified some of the fundamental modern ethi-
cal principles (such as beneficence, non-maleficence
and confidentiality) that have developed since 1970
and have been incorporated into the undergraduate
and postgraduate medical curriculum, residency train-
ing, and continuous professional education across the
Anglo-European world (Ngan and Sim, 2021). How-
ever, despite the extensive AI tools that support med-
ical decision-making today, there is a complete lack
of tools that analyse decisions from the perspective of
their alignment with human values.
The objective of this position paper is to develop
AI that is capable of explaining the alignment of
certain medical decisions with values. Such an AI
will help medical personnel decide when to follow or
break a protocol and help relevant boards decide when
and how to update existing protocols.
Given the current background in developing
value-aligned AI (Sierra et al., 2021; Montes and
Sierra, 2021; Rodriguez-Soto et al., 2022; Montes
and Sierra, 2022; Rodriguez-Soto et al., 2023), we
set out to develop tools that are application-driven, al-
lowing us to address real-life problems. This paper
opens with Section 2 by presenting the chosen med-
ical protocol of our use case, followed by Section 3
which introduces the construction of the corpus that
our AI tools will build upon. Section 4 then presents
our plan for the formal specification of values and the
Rodriguez-Soto, M., Osman, N., Sierra, C., Sánchez Veja, P., Cintas Garcia, R., Farriols Danes, C., Garcia Retortillo, M. and Minguez Maso, S.
Towards Value Awareness in the Medical Field.
DOI: 10.5220/0012588600003636
In Proceedings of the 16th International Conference on Agents and Artificial Intelligence (ICAART 2024) - Volume 3, pages 1391-1398
ISBN: 978-989-758-680-4; ISSN: 2184-433X
Copyright © 2024 by Paper published under CC license (CC BY-NC-ND 4.0)
1391

development of a moral reasoner, before concluding
with Section 5.
2 THE MEDICAL PROTOCOL
2.1 Medical Protocols
Clinical guidelines are an agreed framework outlin-
ing the care that will be provided to patients in a
designated area of practice. These documents pro-
vide information and recommendations about ther-
apeutic interventions, specify procedures to be fol-
lowed in defined situations, and are based on an as-
sessment of the current best evidence of clinical and
cost-effectiveness. Their purpose is to support a clini-
cian in the management of a specific clinical problem
but also they can assist patients in making informed
decisions and enhance the communication between
the patient and the healthcare professional.
Medical protocols consist of a written set of in-
structions that describes the approved and recom-
mended steps of a particular act or sequence of clini-
cal events. They are more explicit and specific in their
detail than guidelines because they specify who does
‘what’, ‘when’ and ‘how’ once a clinical management
decision has been made.
The medical protocols of Hospital del Mar are
documents that are elaborated by the professionals
involved in the healthcare process and validated by
the head of the service. The hospital has more than
1,600 healthcare protocols, of which more than 800
are medical protocols and more than 550 are nurs-
ing protocols. To identify a wide number of medi-
cal protocols in which ethical conflicts may appear,
some examples were analysed and we decided to fo-
cus on Hospital del Mar’s Therapy Intensity Level
Scale, which we describe next, as an example to iden-
tify possible bioethical dilemmas.
2.2 The NIT Protocol
Between 2019–2020, a working group led by the
Mortality Commission of Hospital del Mar initiated
a project to adapt guidelines from the geriatric field
that could provide support in those cases where there
was a general ethical conflict between patients, fam-
ily members and healthcare professionals. The work-
ing group resulted in designing a Therapy Intensity
Level scale (NIT scale), a classification system that
was adapted from the Rogers Memorial Veterans Hos-
pital and consists of 5 levels. This dynamic tool al-
lows professionals to update information throughout
patient care and helps resolve therapeutic decision as-
pects quickly. The classification is based on a shared
decision-making process agreed upon with the health-
care professionals and the patients (or their represen-
tatives) to guarantee adequate coherence between the
patient’s wishes, values and preferences and treatment
intensity. The NIT scale is used to identify which
actions are susceptible to be adopted depending on
the therapeutic objective (prolong patient’s life ex-
pectancy, enhance patient’s comfort or increase their
independence, ...).
The NIT level categorises treatments into 5 levels:
• NIT 1: This is the no-limitation treatments level.
All measures and efforts that prolong a patient’s
survival are accepted.
• NIT 2: This is the intensive treatment. The long-
term survival is the main objective.
– NIT 2A: This accepts all measures except CPR.
– NIT 2B: This does not accept CPR but con-
templates semi-criticals unit and some inten-
sive therapies.
• NIT 3: This is an intermediate level that accepts
complementary examinations and non-invasive
treatments. CPR, ICU and semi-criticals unit are
excluded.
• NIT 4: This is the conservative treatment: symp-
tom control and palliative care. Only symptomatic
and empirical treatments are included. Comple-
mentary explorations are prevented. CPR, ICU or
Semi-criticals unit must be avoided.
• NIT 5: This is applied to end-of-life patients sit-
uation. Comfort care is the main purpose. Only
comfort measures and treatments focused on pro-
viding comfort, quality of life and dignity (instead
of extending life) must be taken.
2.2.1 Value Awareness and the NIT Protocol
As we saw above, each NIT level has a number of
norms built within it, like giving a recommendation
for or against some actions (such as moving the pa-
tient to an ICU unit, or applying CPR). As such, an
AI system can check whether potential actions fol-
low or not the NIT protocol. However, more in-
terestingly, we plan to develop an AI system that
can take into consideration important values (such as
those that we present shortly in Table 3) and evalu-
ate each potential action with respect to those values.
We envision the medical professional to provide the
AI with a set of potential actions that they are con-
sidering to perform. These are selected from a pre-
defined list of actions (such as those presented in Ta-
ble 2). The system can then provide information on
AWAI 2024 - Special Session on AI with Awareness Inside
1392

the alignment of each action with the NIT protocol
along with its alignment with important values. Some
of the important values, which we discuss shortly in
Section 3, are the basic values of autonomy, benefi-
cence, non-maleficence and justice, along with addi-
tional values that are deemed important to the hospi-
tal (e.g. cost efficiency) or the patient (e.g. no pain).
In other words, an AI can raise value awareness for
the medical professional’s decision-making process
by analysing which values would a given potential ac-
tion promote or demote, and to what degree.
Furthermore, as we illustrate in Section 4, we can
deduce the alignment of medical protocols from the
alignment of actions. As such, an AI system will also
be capable of providing feedback on the alignment of
medical protocols, like the NIT protocol, with certain
values. This helps raise value awareness at the man-
agement level to help with decisions on when and how
should medical protocols evolve.
3 BUILDING THE CORPUS
One of the main challenges faced in this medical use
case is that the necessary data needed for reasoning
about values is not currently available. It either exists
in a non-digitised form or as part of the medical per-
sonnels’ know-how. To this end, the first step was to
work on building a corpus that can later on be used
(as we show in Section 4) for reasoning about values.
We commenced this line of work by compiling a
few entries of medical cases, with each entry consist-
ing of four main parts:
1. The criteria that describe a patient’s medical state,
such as their age and pathology, as described in
Table 1. We note that we decided to focus on gen-
eral criteria that could be deduced from the med-
ical files and that would help with value-based
analysis and decision-making.
2. The actions available for the medical personnel
to choose from, indicating which action was per-
formed or not, whether it was effective or not,
and whether it is aligned with the NIT protocol
or not. The set of actions is pre-defined, and it is
presented in Table 2.
3. The criteria that change as a result of taking an
action, such as the change in expected survival,
if any. Those are marked in Table 1 under the
‘Changes with actions’ column.
4. The relevant values that the AI reasoner must
consider in this medical use case, and whether
each action promotes, demotes, or does not af-
fect that value. The selected values are the basic
four bioethical values that the medical personnel
are trained to respect (Beauchamp and Childress,
1979), plus additional values, such as values that
are deemed important to the hospital (e.g. cost ef-
ficiency) or values that are deemed important to
the patient (e.g. suffer no pain, better quality of
life). All of these values, presented in Table 3,
have been provided by the medical doctors of the
NIT unit. We acknowledge an overlap between
basic values and patient values, which requires
further analysis.
In addition to the above four main parts, each case has
an anonymised case number, a date, and the assigned
NIT level.
As an example, we provide the details of one en-
try from our corpus, that of Case #4. Case #4 en-
tered the hospital under NIT level 4. The patient was
73 years old, with complex chronic disease, short-
term survival with an expected survival of less than 6
months, high Frail-VIG, without social support, with
a slight functional independence (with a Barthel In-
dex of 91–99), and a slight-moderate cognitive dete-
rioration. The action ‘Mild: TC/Transf/Picc/Enteral
Nutrition/others’ (in this case, it was a catheter peri-
toneal insertion) was considered not useful but was
taken by the medical doctor to improve patient com-
fort. According to the analysis of the medical doctors
populating the corpus, the result of taking this action
promoted the values ‘autonomy’ and ‘beneficence’,
but demoted the values ‘non-malificience’ and ‘jus-
tice’. It also demoted the value ‘cost-efficiency’, but
promoted the values ‘symptoms controlled (no pain)’
and ‘better quality of life’. We note that the action
was not aligned with the assigned NIT level, which
should have been NIT 3.
4 REASONING ABOUT VALUES
IN THE MEDICAL USE CASE
In what follows, we present how models and mech-
anisms can be developed to make use of the above
corpus for reasoning about values. The first step will
consist of representing biomedical values as formal
objects. Such a formalisation will allow us to have
a transparent, precise and computational definition
of values to determine which behaviours are aligned
with them. Then, as a second step, we foresee two
different approaches that will be explored further in
future work to determine value alignment. The first
uses machine learning (Murphy, 2022; Jordan and
Mitchell, 2015) to learn from the compiled corpus
data, while the second uses symbolic reasoning (Mc-
Carthy, 1999; Montes and Sierra, 2021; Curto et al.,
Towards Value Awareness in the Medical Field
1393

Table 1: Patient criteria.
Criteria Description Changes
with
actions
Criterion 1: Age (S) Patient’s age
Criterion 2: Patient with Com-
plex Chronic Diseases (CCD)
Measures if the patient has one or more chronic diseases with at least one
being permanent, leaving lingering disability, being non-reversible, or co-
existing with a psychological illness.
Criterion 3a: Short-term sur-
vival
Measures if the patient has an advanced chronic disease with a expected
survival rate of less than 12-18 months that requires palliative care.
✓
Criterion 3b: Expected survival It is an estimation, in months, of the expected survival of the patient.
Criterion 4: Frail-VIG [Scale:
Spict]
Fragility Index validated in the geriatric population. Based on different
variables, it offers a frailty evaluation tool for rapid assessment. Frail-
VIG establishes the degree of frailty of the patient. This criterion has a
reliable mortality predictive capacity.
✓
Criterion 5: Clinical Risk
Groups (CRG)
A categorical classification system that uses administrative data to identify
patients with chronic health conditions. Stratifies the population accord-
ing to morbidity groups in four different levels: (0) Promotion & Preven-
tion of diseases. (1) Self-management support: between 70–80% of pa-
tients are able to look after their own health efficiently and conveniently
(selfcare). (2) Illness management: high risk patients that need illness
management coordinated with the professionals. (3) Case management:
the patient needs a case manager to coordinate the medical care.
Criterion 6: Social support
(NS)
It considers if the patient has social support (family, friends) to offer sup-
port functions (emotional, instrumental, ...)
Criterion 7: Functional in-
dependence (Barthel Index)
[Scale: Berthel]
The Barthel Index is a 10-item instrument used in the evaluation of func-
tional independence in personal activities of daily living (ADL). It mea-
sures the capacity of a person for the execution of basic activities in daily
life (feeding, bathing, ambulation, bladder and bowel control, ...).
✓
Criterion 8: Patient’s advanced
directives (written or oral)
For patients who have decision-making capacity. Referred if there is a
signed document or the patient has mentioned their desires regarding treat-
ment decisions. It includes when the patients identify whom they want to
make decisions on their behalf when they cannot do so themselves.
Criterion 10: Cognitive deterio-
ration
When the patient suffers cognitive impairment (confusion, memory loss,
difficulty understanding or speaking, problems with concentration. . . )
Criteria 11: Comfort A dynamic state characterised by absence of pain, emotional and physical
distress and symptom control.
✓
2022) to reason about actions and protocols and their
alignment with values.
4.1 Value Representation
Regardless of which approach we follow for reason-
ing about values, we will need to have a formal rep-
resentation of values to enable this computational
reasoning. We commence with the four biomedi-
cal values of Beauchamp and Childress’ principialism
(Beauchamp and Childress, 1979) (Values 1–4 in Ta-
ble 3). As agreed upon by the biomedical community,
at least these four values provide the best framework
for ethical analysis in biomedical scenarios (Veatch,
2020).
Our first step towards formalising the four
biomedical values is first to categorise them follow-
ing the proposed outline by Veatch in (Veatch, 2020).
Veatch states that biomedical ethics’ four main val-
ues can be divided into two categories: consequence-
based values and duty-based values. To behave in
alignment with a given value has a separate definition
for each category, as we show next.
• Consequence-based values: An action is aligned
with a consequence-based value if its conse-
quences are aligned with that value. In a biomedi-
cal context, the degree of alignment with such val-
ues is measured by the amount of utility a given
action provides to the patient. This category in-
cludes the values of beneficence (measuring pos-
itive utility, goods) and non-maleficence (measur-
ing negative utility, harm).
• Duty-based values: An action is aligned with a
duty-based value if and only if it is morally ac-
ceptable according to that value, regardless of its
consequences. In a biomedical context, actions
such as “cheating” or “killing a patient” would
not be morally acceptable under any circumstance
with respect to the duty-based value of autonomy.
AWAI 2024 - Special Session on AI with Awareness Inside
1394
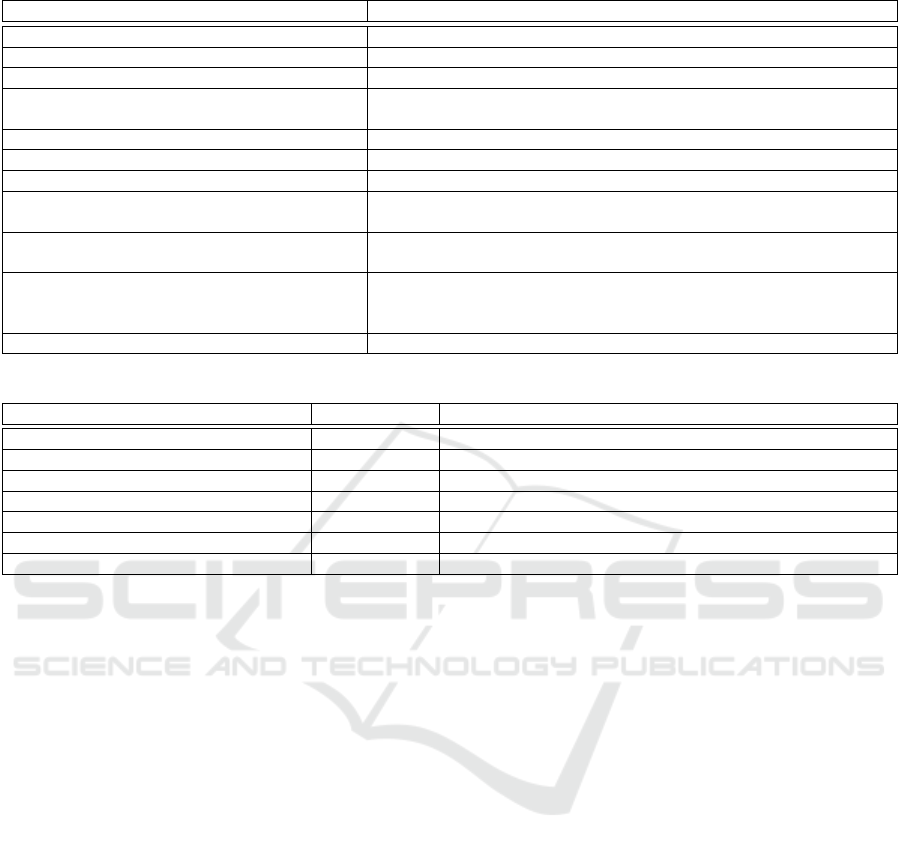
Table 2: Doctors’ actions.
Action Description
Action 1: RCP Cardiopulmonary Resuscitation (CPR)
Action 2: Transplant Transplant
Action 3: UCI Intensive Care Unit (ICU)
Action 4: VMNI Non invasive respiratory support. Any form of ventilation support
without tracheal intubation (includes oxigenotherapy)
Action 5: DVA Vasoactive drugs (noradrenaline, epinefrine, dopamine...)
Action 6: Dialysis Dialysis
Action 7: Simple: RX / Anal / Culture / AB X-ray, blood analysis, cell or urine culture
Action 8: Mild: TC / Transf / Picc / Enteral
nutrition
CAT Scan (computed tomography) / Blood transfusion / PICC: Periph-
eral Inserted Central Catheter / Enteral Nutrition
Action 9: ADV: RNM / Endoscopy / Parenteral
nutrition
Nuclear Magnetic Resonance / Endoscopy / Parenteral nutrition
Action 10: Palliative surgery Surgery designed to remedy the discomfort of and pain symptoms of
incurable diseases. Palliative surgical procedures are intended to re-
duce suffering or support quality of life.
Action 11: Curative surgery Are intended to prolong life or cure disease.
Table 3: Important values (some patient values are related to basic values).
Value Value type Description
Value 1: Autonomy Basic value patient’s ability to make informed decisions over themselves
Value 2: Beneficence Basic value patient’s benefit ensured
Value 3: Non-maleficence Basic value no harm being inflicted on the patient
Value 4: Justice Basic value fair, equitable, and appropriate treatment of all patients
Value 5: Cost efficiency Hospital value Cost minimisation
Value 6: Symptoms control (no pain) Patient value Minimising patients’ suffering from pain
Value 7: Better quality of life Patient value Improving the quality life of patients
This category also includes the value of justice.
We can formalise alignment with a consequence-
based value by considering a patient’s medical con-
ditions C before performing a medical action and
comparing them with their medical conditions C
′
af-
ter the action is performed. Formally, let V be a
consequence-based value, then:
align(a, ⟨C,C
′
⟩,V ) = f
V
(C,C
′
),
where a is the medical action taken, and f
V
is a func-
tion comparing the two medical conditions.
There are two implications from this equation.
The first one is that the action taken is irrelevant to the
formula since we only care about the consequences.
Moreover, this function is taking into account that the
outcome of an action is non-deterministic in a medi-
cal context, and for that reason we must focus on its
consequences.
The second implication is that we can obtain a for-
mal definition of f
V
(and thus, of the value) by explic-
itly listing which and how patient criteria in Table 1
are considered relevant. Assume that we have already
agreed on the subset of criteria C
V
associated with a
given value V . Then, a possible formula for f
V
could
be:
f
V
(C
V
,C
′
V
) = G
V
(
|C
V
|
∑
i=1
g
i
V
(c
i
, c
′
i
)),
where c
i
∈ C
V
and c
′
i
∈ C
′
V
are the conditions of the
patient for each criterion i before and after the ac-
tion, and functions g
i
v
and G
V
could be for instance
g
i
v
(x, y) = x − y and G
V
(x) = x. A formal definition
of them would allow us to obtain a representation of
beneficence and non-maleficence.
Finally, further research must be conducted for the
other two values to assess which is the set of accept-
able actions associated with each duty-based value.
4.2 Machine Learning
4.2.1 Value-Alignment of Actions in Context
One approach that we will investigate is to develop
learning mechanisms that would use the corpus being
built to help us learn and predict the relations between
an action A, context C (defined through the patient
criteria) and value V . In other words, we want to learn
to answer the following question: In a given context
C, does an action A promote, demote, or not-affect a
given value V ?
Towards Value Awareness in the Medical Field
1395

Formally, we specify these relations as the degree
of alignment that the action A in context C has with
the value V , which we represent as align(A,C,V ).
We want the range of alignment to be [−1, 1], so that
positive alignment would represent the action promot-
ing the value, negative alignment would represent the
action demoting the value, and an alignment of zero
would represent the action not to affect the value. Fur-
thermore, the use of a range helps us describe varying
degrees of (mis)alignment.
We expect the model to predict the degree of
(mis)alignment of an action with a value in a given
context by learning from the past alignments pre-
sented in the corpus we are building. That is, the
model learns from the past judgements of the medi-
cal personnel populating the corpus. Naturally, one
of the main challenges of this approach will be the
scarcity of the data.
4.2.2 Value-Alignment of Norms
We follow the traditional approach of defining norms
through deontic operators over actions in context (An-
drighetto et al., 2013;
˚
Agotnes et al., 2009). Some
examples of norms are:
• It is prohibited to perform action A (or action ¬A)
in context C.
• It is permitted to perform action A (or action ¬A)
in context C.
• It is obligatory to perform action A (or action ¬A)
in context C.
These examples make use of three deontic opera-
tors: prohibitions, permissions, and obligations. We
note that there are other deontic operators that one
may consider, such as gratuitousness (permission to
not perform an action) or indifference (permission to
perform as well as to not perform an action), to name
a few. We choose the above three operators for their
common usage. Furthermore, it is well established
that any deontic operator can be chosen as a basic op-
erator, and then all other deontic operators can be de-
fined in terms of the chosen basic operator. For ex-
ample, a permission to perform an action can be spec-
ified as the negation of an obligation to not perform
that action. As such, we say other deontic operators
may easily be added, if the need arises, as they can be
defined in terms of any of those three operators above.
Formally, we say let N = D(A,C) specify a norm
describing a deontic operator D ∈ {F, P, O} (where F
describes what is forbidden, P what is permitted, and
O what is obligatory) over an action A when the con-
text C is satisfied (or holds).
We then argue that if we can learn the align-
ment of an action A in context C with a value V ,
then we can deduce whether a norm N = D(A,C) is
aligned or not with that value V , which we represent
as alignN(N,V).
Examples of the properties that should hold when
deducing the alignment of norms from the alignment
of actions are presented in Figure 1. For example, we
say that if an action A in a given context C is aligned
with a value V (alignment is positive), and the norm
states that this action A is permitted or obligatory in
the context C, then this norm is aligned with that value
because it permits (in the case of the deontic operator
P) or obliges (in the case of the deontic operator O)
the action A that promotes that value V . Furthermore,
the alignment of the obligation may be greater than
the alignment of the permission, since obligations are
stronger than permissions in bringing about a given
action. Similarly, if the norm prohibits the action A
in context C (alignment is negative), then the norm
is not aligned with the value V . Similar reasoning is
followed in the remaining cases.
Finally, we note that we can also compute the
alignment of one norm N with a set of values V by
aggregating the alignment of that norm N with each
of the values V ∈ V :
alignN(N, V ) =
M
V ∈V
alignN(N,V)
where
L
is an aggregation operator to be designed.
4.2.3 Value-Alignment of Protocols
Since we understand protocols as sets of norms, we
say let P = N specify a protocol composed by the set
of norms N . We note that as our work progresses,
we may need to modify our specification of protocols
in such a way that allows us to address conflicting
norms. For example, we may attach a priority mea-
sure to each norm, so that norms with higher prior-
ity can override norms with lower priority when con-
flicts arise. However, this requires further collabora-
tion with the medical personnel at Hospital del Mar to
confirm that whatever specification we use for proto-
cols is consistent with their definition of protocols and
how they deal with conflicting norms. For the time
being, we keep things simple by defining protocols as
sets of norms.
We then argue that if we can assess the alignment
of norms with values, then we may deduce from that
the alignment of protocols with values, which we rep-
resent as alignP(P,V ).
For example, by aggregating the alignment of
each norm N in the set of norms N with value V ,
we get the alignment of the protocol P = N :
alignP(P,V ) =
M
N∈N
alignN(N,V)
AWAI 2024 - Special Session on AI with Awareness Inside
1396

IF align(A,C,V ) > 0
T HEN alignN(O(A,C),V ) ≥ alignN(P(A,C),V) > 0 ∧
alignN(F(A,C),V ) < 0
IF align(A,C,V ) < 0
T HEN alignN(O(A,C),V ) ≤ alignN(P(A,C),V) < 0 ∧
alignN(F(A,C),V ) > 0
IF align(A,C,V ) = 0
T HEN alignN(O(A,C),V ) = alignN(P(A,C),V) = alignN(F(A,C),V) = 0
Figure 1: Properties of deducing the value-alignment of norms from the value-alignment of actions in context.
Similarly, we can also compute the alignment of
a protocol P with a set of values V by aggregating
the alignment of that protocol with each of the values
V ∈ V :
alignP(P, V ) =
M
V ∈V
alignP(P,V )
Again, the design of the aggregation operator
L
will be carried out in future work.
4.3 Symbolic Reasoning
The alternative approach to learning that we will in-
vestigate is providing a symbolic representation of ac-
tions and values similar to (Montes and Sierra, 2022;
Sierra et al., 2021; Osman and d’Inverno, 2023), and
using that symbolic representation to reason about the
alignment of actions in context with values. We de-
scribe next the requirements for the symbolic repre-
sentations.
First, the symbolic representation of actions must
define what are the outcomes of actions. That is, how
do they change the current state of the world. In the
NIT use case, actions change some of the patients’
criteria, such as their expected survival, their comfort
(for example, if an action lowers the fever of a pa-
tient), etc.
The symbolic representation of values, on the
other hand, essentially defines how a value may be
evaluated in a given context to assess whether it is be-
ing promoted or not. Section 4.1 has presented our
initial approach.
For example, to evaluate whether the value ‘non-
maleficience’ is promoted, which is understood as no
harm is inflicted on the patient, the medical person-
nel try to confirm whether the patient has no pain,
improved quality of life, and improved expected sur-
vival, to name a few. Those are all deduced from the
criteria, such as the ‘expected survival (in months)’
and the ‘Frail-VIG’ value. As such, when populat-
ing the corpus and deciding whether a given action
promotes or not a given value, the medical personnel
are in fact analysing the impact of that action on those
specific criteria, and deciding accordingly whether the
value ‘non-maleficience’ is being promoted, demoted,
or unaffected by that action.
Given the symbolic representations of actions and
values, we can then develop a model that could anal-
yse the changes that an action brings about (in our use
case, that would be changes in patients criteria), and
whether those changes result in promoting, demoting
or not affecting a given value (as value evaluation is
based on analysing patient criteria).
Similar to the machine learning approach, we ar-
gue that if we can reason about actions’ alignment
with values per context, then we can deduce norms
alignment with values as well as the alignment of en-
tire protocols with values, following the approaches
presented in Sections 4.2.3 and 4.2.2.
4.4 Impact of Value Based Analysis
In both the machine learning approach and the sym-
bolic reasoning approach, we can analyse the align-
ment of actions in context, norms, and even entire
medical protocols with values. But what is the ac-
tual impact of this work? We argue that this can sup-
port value-aware decision-making for both the medi-
cal personnel and the management teams at hospitals
as follows:
• By analysing the alignment of actions in con-
text, the machine can inform a medical personnel
whether the action they have decided to carry out
is aligned or not with certain values, or whether
this action prefers one value over another, and to
what degree. We stress that we do not make state-
ments about what is right and wrong. The model
simply analyses the degree of (mis)alignment
with values, and it is up to the medical person-
nel to evaluate such alignments as well as asses
the importance of different values and make their
decisions accordingly. In summary, this line of
work promotes value-aware decision making by
Towards Value Awareness in the Medical Field
1397

medical personnel.
• By analysing the alignment of norms and pro-
tocols, the machine can inform the management
team (whether at the NIT level, or hospital level),
when certain norms or protocols are aligned with
certain values, or whether they give preference to
one value over another, and to what degree. This
helps the management team decide when, and un-
der what condition, should norms and protocols
change and evolve. Again, we do not make state-
ments about what is right and wrong, but we pro-
mote value-aware protocol design and specifica-
tion.
5 CONCLUSIONS
In this position paper, we have described the initial
work on developing value aware AI and applying it to
the medical field. We have described the process of
selecting an appropriate and illustrative medical pro-
tocol to work with, the ongoing building of the rel-
evant corpus, and the plans on how to develop mod-
els and mechanisms that would promote value-aware
decision-making and value-aware protocol design and
specification.
Our ongoing work continues to build the corpus
in collaboration with Hospital del Mar. We will also
continue with the formal specification of values, and
commence the development of models and mech-
anisms that reason about the alignment of actions,
norms, and protocols with values according to the
plans presented in Section 4.
ACKNOWLEDGEMENTS
This work has been supported by the EU funded
VALAWAI (# 101070930) project and the Spanish
funded VAE (# TED2021-131295B-C31) and Rhy-
mas (# PID2020-113594RB-100) projects. Further-
more, partial financial support was received from
project 2021 SGR 00754.
REFERENCES
˚
Agotnes, T., van der Hoek, W., Rodr
´
ıguez-Aguilar, J. A.,
Sierra, C., and Wooldridge, M. J. (2009). A temporal
logic of normative systems. In Makinson, D., Mali-
nowski, J., and Wansing, H., editors, Towards Math-
ematical Philosophy, volume 28 of Trends in logic,
pages 69–106. Springer.
Andrighetto, G., Governatori, G., Noriega, P., and van der
Torre, L. W. N., editors (2013). Normative Multi-
Agent Systems, volume 4 of Dagstuhl Follow-Ups.
Schloss Dagstuhl - Leibniz-Zentrum f
¨
ur Informatik.
Askitopoulou, H. and Vgontzas, A. N. (2018). The rele-
vance of the hippocratic oath to the ethical and moral
values of contemporary medicine. part i: The hippo-
cratic oath from antiquity to modern times. European
spine journal, 27(7):1481–1490.
Beauchamp, T. and Childress, J. (1979). Principles of
Biomedical Ethics. Oxford University Press.
Curto, G., Montes, N., Sierra, C., Osman, N., and Comim,
F. (2022). A norm optimisation approach to sdgs:
tackling poverty by acting on discrimination. In
Raedt, L. D., editor, Proceedings of the Thirty-First
International Joint Conference on Artificial Intelli-
gence, IJCAI 2022, Vienna, Austria, 23-29 July 2022,
pages 5228–5235. ijcai.org.
Jordan, M. I. and Mitchell, T. M. (2015). Machine learn-
ing: Trends, perspectives, and prospects. Science,
349(6245):255–260.
McCarthy, J. (1999). Making robots conscious of their
mental states. In Machine Intelligence 15, Intelligent
Agents [St. Catherine’s College, Oxford, July 1995],
page 3–17, GBR. Oxford University.
Montes, N. and Sierra, C. (2021). Value-guided synthesis of
parametric normative systems. In Dignum, F., Lomus-
cio, A., Endriss, U., and Now
´
e, A., editors, AAMAS
’21: 20th International Conference on Autonomous
Agents and Multiagent Systems, Virtual Event, United
Kingdom, May 3-7, 2021, pages 907–915. ACM.
Montes, N. and Sierra, C. (2022). Synthesis and properties
of optimally value-aligned normative systems. J. Artif.
Intell. Res., 74:1739–1774.
Murphy, K. P. (2022). Probabilistic machine learning: an
introduction. MIT press.
Ngan, O. M. Y. and Sim, J. H. (2021). Evolution of
bioethics education in the medical programme: a tale
of two medical schools. International Journal of
Ethics Education, 6(1):37–50.
Osman, N. and d’Inverno, M. (2023). A computational
framework of human values for ethical ai.
Rodriguez-Soto, M., Serramia, M., Lopez-Sanchez, M.,
and Rodriguez-Aguilar, J. A. (2022). Instilling moral
value alignment by means of multi-objective rein-
forcement learning. Ethics and Information Technol-
ogy, 24.
Rodriguez-Soto, M., Serramia, M., L
´
opez-S
´
anchez, M.,
Rodriguez-Aguilar, J. A., Bistaffa, F., Boddington, P.,
Wooldridge, M., and Ansotegui, C. (2023). Encoding
ethics to compute value-aligned norms. Minds and
Machines.
Russell, S. (2019). Human Compatible: Artificial Intelli-
gence and the Problem of Control. Penguin Publish-
ing Group.
Sierra, C., Osman, N., Noriega, P., Sabater-Mir, J., and
Perell
´
o, A. (2021). Value alignment: a formal ap-
proach. CoRR, abs/2110.09240.
Veatch, R. M. (2020). Reconciling Lists of Principles in
Bioethics. The Journal of Medicine and Philosophy:
A Forum for Bioethics and Philosophy of Medicine,
45(4-5):540–559.
AWAI 2024 - Special Session on AI with Awareness Inside
1398
