
Virtual Reality for Detailed Visualization and Generation of Proximal
and Distal Bone Fracture Patterns
J. J. Jim
´
enez-Delgado
1 a
, F. D. P
´
erez-Cano
1 b
, G. Parra-Cabrera
1 c
and I. Remolar-Quintana
2 d
1
Department of Computer Science, University of Ja
´
en, Ja
´
en, Spain
2
Institute of New Imaging Technologies, Universitat Jaume I, Castell
´
on, Spain
Keywords:
Bone, Fracture, Pattern, Virtual Reality, Usability, Interaction.
Abstract:
This paper articulates the application of virtual reality (VR) in facilitating the study of bone fractures, particu-
larly those affecting the proximal and distal end segments of long bones, areas of the bone in which there are a
large number of irregularities. With the increasing prevalence of bone fractures due to aging and increased life
expectancy, we present an innovative virtual reality system that meticulously generates and visualizes bone
fracture patterns in three dimensions. The system allows users, including healthcare professionals, to interact
with 3D bone models and delineate fracture patterns in a realistic environment. It features haptic feedback,
simulating the sensation of drawing on a real bone. The tool also provides an exporting functionality for the
drawn fractures, enabling the integration into other medical platforms. Experts have evaluated the interaction
and representation of the fracture patterns in a highly positive evaluation. The experts assessed the system
positively, emphasizing its potential towards enhancing surgical planning, improving patient outcomes, and
fostering educational advancements. Future work aims at improving the degree of realism within the VR en-
vironment and refining the precision of closing fracture lines.
1 INTRODUCTION
The increase in life expectancy has led to a higher in-
cidence of fractures, mainly due to the gradual wear
and tear associated with daily activities. This natu-
ral aging process often weakens bones, making them
more susceptible to fractures. A complicating fac-
tor in the treatment of fractures is the interference of
blood at the site of the injury, which can obscure the
surgeon’s view and make it difficult to align the bone
fragments. As a result, secondary surgeries are often
required to properly realign these fragments.
The elderly are particularly at risk for hip frac-
tures, an injury that poses significant health risks and
can lead to serious consequences such as reduced mo-
bility and increased dependency. These fractures are
particularly challenging due to the complex nature of
the hip joint and the essential role it plays in weight
bearing and movement. Therefore, in this work we
will focus on the use of long bones, with particular
a
https://orcid.org/0000-0003-3014-0496
b
https://orcid.org/0000-0002-8065-8173
c
https://orcid.org/0000-0003-0364-8657
d
https://orcid.org/0000-0002-7743-2579
emphasis on the use of the femur, as it is one of the
most common fractures and has the greatest impact
on people.
The study of bone fractures helps to understand
the nature and morphology of these injuries, which is
crucial for the development of effective and person-
alized therapeutic strategies. In this context, virtual
reality is emerging as an innovative tool that is revo-
lutionizing the study of bone fractures. The applica-
tion of virtual reality in the medical field allows health
care professionals to visualize the complex anatomy
of bone fractures in three dimensions. This facilitates
a deeper analysis of the unique characteristics of each
fracture, such as the orientation of the fracture lines,
the dispersion of the bone fragments, and the struc-
tural integrity of the affected bone, as well as improv-
ing the precision of surgical planning and patient out-
comes.
The proximal and distal segments of bones typi-
cally exhibit numerous irregularities, making it quite
complex to draw a fracture pattern in these areas. The
common approach involves creating a 2D design and
mapping or projecting it onto the bone model (Parra-
Cabrera et al., 2022). However, the traditional method
cannot be effectively applied in these bone regions,
300
Jiménez-Delgado, J., Pérez-Cano, F., Parra-Cabrera, G. and Remolar-Quintana, I.
Virtual Reality for Detailed Visualization and Generation of Proximal and Distal Bone Fracture Patterns.
DOI: 10.5220/0012446500003660
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 19th International Joint Conference on Computer Vision, Imaging and Computer Graphics Theory and Applications (VISIGRAPP 2024) - Volume 1: GRAPP, HUCAPP
and IVAPP, pages 300-306
ISBN: 978-989-758-679-8; ISSN: 2184-4321
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
often necessitating the use of 3D drawing devices,
such as haptic devices. This work presents a vir-
tual environment for drawing a wide range of frac-
ture patterns, including the most deformed areas of
human bones, for export and use in other medical
tools. The VR allows us to generate a three dimen-
sional interactive environment for detailed visualiza-
tion of fractures, including the orientation of fracture
lines and deformities on the bone surface. It is par-
ticularly useful for examining complex areas of bone
fractures, such as the proximal and distal end seg-
ments. The tool also allows healthcare profession-
als to export these fracture patterns for use in other
medical tools. It enables healthcare professionals to
meticulously examine the anatomical intricacies and
complexities of fractures within challenging anatomi-
cal regions, such as the proximal and distal ends of
bones. This precise, 3D visualization fosters com-
prehension of the specific fracture geometry, empow-
ering surgeons to devise tailored surgical strategies.
Moreover, it furnishes aspiring surgeons with an inter-
active tool for honing practical skills, enabling them
to practice fracture identification and treatment within
virtual environments prior to real clinical scenarios.
The outline of this work is as follows: In the next
section, we analyze the previous work on medical ap-
plications in virtual reality. After the background,
the materials used and the system developed are de-
scribed in detail. The following sections present and
discuss the results obtained in the process of using
the simulator. Finally, the conclusions summarize the
main advances and lines of work for the future.
2 RELATED WORK
Progress in bone fractures is essential for the diagno-
sis and recovery of the patients. These studies con-
tribute to improving practices and technologies for
treating fractures, including fixation methods, plates,
screws, and prostheses. The study of bone fractures
from a forensic and anthropological perspective re-
veals crucial information to determine the cause of
death or the lifestyle of the subject, as each bone and
fracture is unique and the anatomy of the fracture
varies according to various biological factors such
as age, bone density and diseases that affect bone
strength (Jones, 2010; Azar et al., 2020). Although
they are different, there are certain patterns in their
shape when they are produced under similar condi-
tions (P
´
erez-Cano et al., 2023). AO Trauma Inter-
national and Orthopaedic Trauma Association Rep-
resentatives (AO/OTA) presented a compendium for
the classification of bone fractures and dislocations
(Meinberg et al., 2018). The number of pieces of bone
detached, the angle and the shape of the fracture lines
are the elements that allow differentiating the differ-
ent types of bone fractures. However, the shape of
the bone is not uniform and the areas with the most
irregularities are those where it is most difficult to ex-
tract a fracture pattern for replication in another clin-
ical case. In the case of long bones, the irregularities
are usually found at the ends of the bone, that is, the
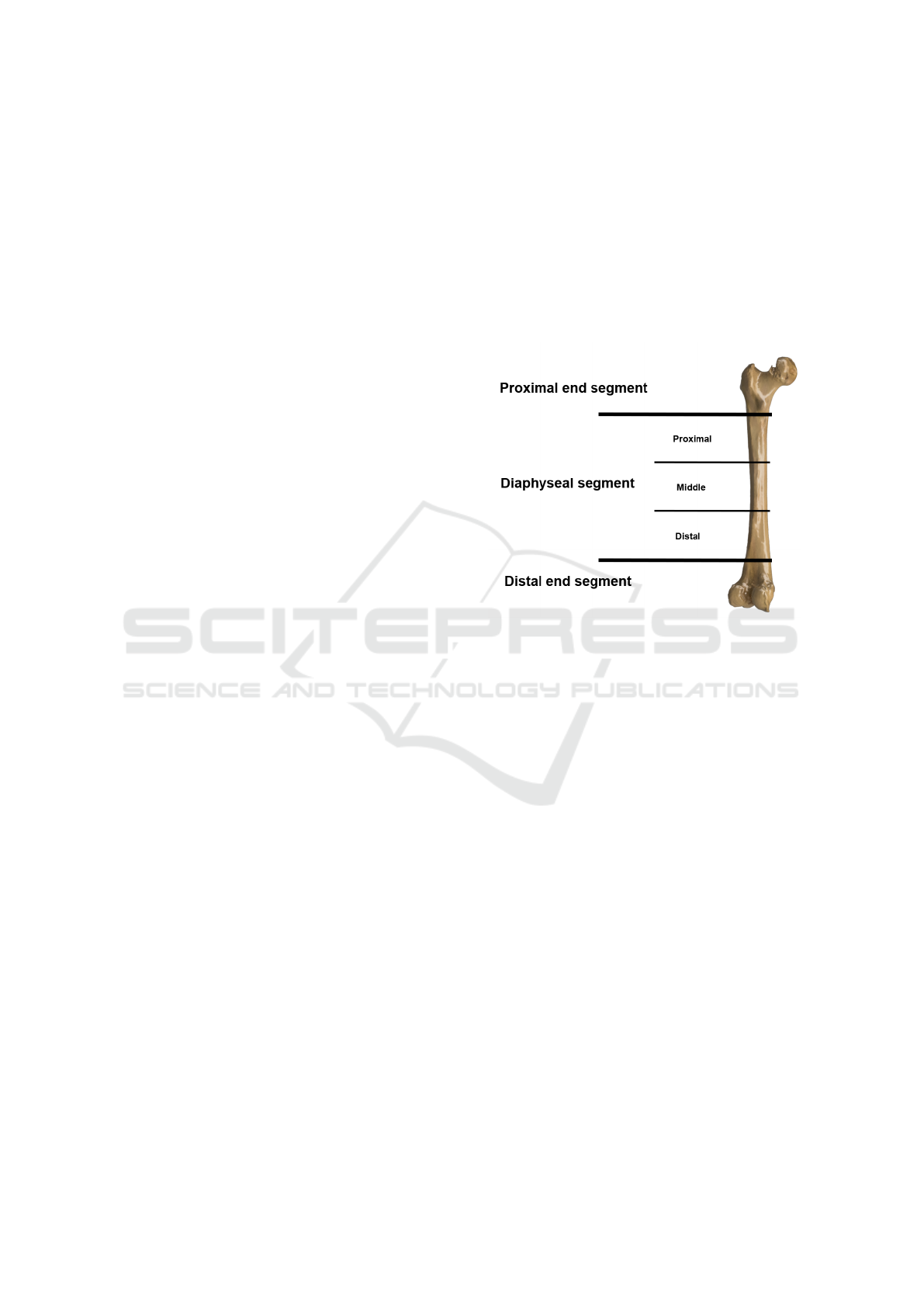
proximal and the distal end segments of the bone (Fig.
1).
Figure 1: The areas of a long bone in which a fracture is
likely to occur.
Several authors emphasize the importance of us-
ing new technologies to achieve realistic visualization
when conducting a medical simulation (Tsai et al.,
2001; Citak et al., 2008; Vaughan et al., 2016; Gu-
sai et al., 2017; Negrillo-C
´
ardenas et al., 2021; Fu
et al., 2022; Loetscher et al., 2023). Citak et al. (Citak
et al., 2008) concluded that the use of technology to
improve visualization and interaction allowed them to
improve the planning of a bone fracture reduction by
obtaining a more accurate result in the surgical pro-
cess. Tsai (Tsai et al., 2001) also concludes that simu-
lations in a virtual environment allow better planning,
mainly by improving the visualization of the fracture
area. Florence A
¨
ım et al. (A
¨
ım et al., 2016) have
demonstrated the effectiveness and advantages of us-
ing VR to train new surgeons. However, most virtual
reality based studies have focused on fracture reduc-
tion planning and training.
Some authors report that the use of VR also helps
participants to feel motivated and interested in partici-
pating in this type of projects (Herne et al., 2022; Reer
et al., 2022). Among other aspects, immersion, inter-
action and feedback are highlighted as fundamental
elements. Herne et al. (Herne et al., 2022) emphasize
the importance of feedback in providing a good expe-
Virtual Reality for Detailed Visualization and Generation of Proximal and Distal Bone Fracture Patterns
301

rience to the user who tries the tool. Gusay et al. (Gu-
sai et al., 2017) focused on analyzing the interaction
of a user in a realistic environment. In this work, they
analyze the different ways a user can interact with the
environment using different devices compatible with
the HTC Vive head-mounted display (HMD) to visu-
alize the scene.
Negrillo et al. (Negrillo-C
´
ardenas et al., 2021) de-
veloped a fracture reduction system based on VR us-
ing contralateral fractures as targets. They observed a
high learning rate when using the system and a reduc-
tion in simulation time as more trials were performed.
Vaughan et al. (Vaughan et al., 2016) reviewed the
main existing fracture reduction simulation environ-
ments, as well as the problems with some of them.
In this study, the authors also conclude that there is
strong evidence that the skill level of trainees in med-
ical procedures can be assessed using VR simulators.
Akhtar et al. (Akhtar et al., 2015) demonstrate the va-
lidity of a haptic VR trauma simulator, with surgeons
performing the procedure most often performing best
on the simulator. Homma et al. (Homma et al., 2019)
also worked along these lines and came to the same
conclusion.
Loetscher et al. (Loetscher et al., 2023) conducted
a recent study in which they concluded that there is
evidence that the integration of virtual reality in the
medical field is extremely beneficial and that it should
be used more often to take full advantage of its bene-
fits. Some companies, such as Meta, are moving in
this direction to provide ecosystems to support the
growth of virtual reality in the medical field. How-
ever, it is a process that will take some time before it
becomes a necessity for healthcare.
3 MATERIAL AND METHOD
The project was developed using the Unity engine, a
leading game engine known for its ability to support
interactive 3D content and broad cross-platform com-
patibility. The virtual reality experience was delivered
through the HTC Vive Pro Kit, chosen for its high-
resolution display and advanced tracking capabilities.
By using the advanced Lighthouse tracking system,
also known as base stations, we obtain a millimetric
accuracy for user positioning. This level of accuracy
makes this VR system ideal for simulating the intrica-
cies of an operating room environment. The immer-
sive experience is further enhanced by the wide range
of hardware sensors, including proximity sensors, gy-
roscopes, and infrared sensors. In addition, the con-
trollers are designed to provide seamless interaction
with the virtual environment. They incorporate tac-
tile feedback through vibration, allowing precise ma-
nipulation of three-dimensional objects, such as hu-
man bones in our simulation. The user can interact
with the environment using two controllers held in the
right and left hands. The equipment used to support
the virtual reality application consists of a computer
equipped with an i7 microprocessor, 8GB of RAM,
and an NVidia 1060 graphics card.
The virtual environment design consists of an op-
erating room (Fig. 2). A familiar space has been
recreated for the surgeons to increase the level of im-
mersion. The primary function of our tool is to allow
the user to delineate and examine fracture patterns on
highly detailed 3D models of long bones, focusing on
the complex and irregular areas such as the proximal
and distal end segments. The user can select between
different long bone models to draw a fracture using
the controllers.
Figure 2: Environment used to conduct the simulation.
The left controller allows the user to move around
the environment and move the model to improve the
viewing angle, while the right controller allows the
user to create the fracture pattern. To create a fracture
pattern, the controllers emit a laser beam in the direc-
tion they are pointed. When this laser intersects the
bone model, it creates a visible line on the bone sur-
face that represents the fracture line. The points form-
ing the fracture line are calculated by the intersection
between the mesh and the beam leaving the controller,
using the algorithm of M
¨
oller and Trumbore (M
¨
oller
and Trumbore, 1997). The user must hold down the
trigger to add points to the polyline that defines the
fracture line (Fig. 4). In addition, the fracture line
must be fully closed and connected for the fracture to
be valid and exported. It is not necessary to draw the
line in one go, the user can add points to the fracture
line one at a time and confirm when the fracture rep-
resentation is complete. This mechanism facilitates
the elimination of incorrect points marked by the user,
since a history of the various iterations with the model
and the points selected is stored, so that errors can
be corrected as the fracture line is drawn. Figure 3
GRAPP 2024 - 19th International Conference on Computer Graphics Theory and Applications
302

shows the graphical interface that can be used by the
user within the virtual environment when drawing the
fracture pattern on a human bone. Moreover, the user
defines the end of the representation of the model and
it is automatically validated by a study of the continu-
ity of the polyline. If the polyline is not closed, the
user is prompted to continue with the design of the
pattern.
Haptic feedback is integrated to enhance the tac-
tile experience, giving the user the sensation of draw-
ing on a real bone through small vibrations. This fea-
ture is particularly useful for medical professionals, as
it adds a layer of realism that is critical to understand-
ing the physical characteristics of bone fractures. The
intensity of the vibration is slightly increased when
the user is drawing the fracture line and it is in a hole
or a bump is found in the geometry of the model. The
vibrations are managed by assessing the distance vari-
ations between the position of the controller and the
specific point on the bone model where the laser beam
intersects during the drawing activity. When the user
move the laser over the bone’s surface, the occurrence
and intensity of vibrations depend on the difference in
distance between consecutive points along the frac-
ture line.
An essential feature of this tool is the ability to
export the drawn fracture lines. This functionality al-
lows the fracture patterns to be integrated into other
tools. For this purpose, we have exported the point
cloud drawn by the user. We are currently working
on the import of the fracture lines generated in this
tool, so that it will not only serve to generate fracture
patterns, but also to improve the visualization or the
lines of existing patterns obtained with this or other
medical tools.
4 RESULTS
The previous section has detailed the development of
a virtual reality application to delineate and examine
fracture patterns on highly detailed 3D models of long
bones, specifically focusing on the complex and irreg-
ular areas of the bone surface. In this section we show
the result obtained and we focus on the evaluation of
the results obtained and how to analyze them to vali-
date the quality of the system designed. For this pur-
pose, we have conducted extensive tests to validate
the application.
There is no other system with a similar purpose.
Therefore, the design and functionality have been re-
fined in collaboration with three specialists with ex-
perience in bone fracture reduction, a physiothera-
pist and an orthopedic surgeon. Each of the 5 users
was tasked to replicating a fracture type from the
AO/OTA classification in the proximal and and dis-
tal area of three different bones: a femur, a humerus
and a fibula. The fibula can be considered the sim-
plest model, given that the deformity at the ends is
smaller. It has been presented as the initial case to
test the developed tool. The humerus and femur ex-
hibit more significant deformities, with the femur be-
ing the most irregularly shaped and representing the
most complex case presented to the specialists. Each
bone has a different shape in these sections. Before
starting the tests, they were instructed on the controls
necessary to select the bone, rotate it and how to draw
the fracture line on it using the HTC Vive controllers.
Technical testing focused on system performance, sta-
bility, immersion and user interface usability.
Figure 5 shows different fracture patterns drawn
by experts on the end segment of the epiphysis of a
human humerus. All the patterns are based on the
AO/OTA classification (Meinberg et al., 2018). The
image shows all the fracture lines that make up the
pattern in red. In addition, the lines drawn on the
back of the model, the non-visible part of the geom-
etry, are shown so that the user can take them into
account when closing the lines completely. Figure
5a represents an oblique fracture in the surgical neck
area. Figure 5b shows a wedge-shaped fracture with-
out fragmentation at the head of the humerus while
figure 5c shows a compound fracture with many frag-
ments in the same area. The visual improvement
is considerable when defining the patterns, since the
simulator allows the deformations of the bone surface
to be identified with a high level of detail. Figure 6b
shows the view of the fracture pattern from the lon-
gitudinal axis of the bone on which it is drawn (Fig
6a.).
A survey was used to evaluate the tool using a 5-
item Likert scale. Table 1 shows the median and av-
erage results obtained through the survey in the dif-
ferent aspects considered. In general, most aspects
were rated positively by the expert group. Among the
main evaluations, the scores for the interface and the
drawing of fracture lines on the bone model stand out,
where all experts agreed with the maximum score.
This reflects the fact that the developed tool has an
intuitive interface and sufficient functionality to draw
the patterns in the most complex areas in a simple
way.
We can see how the complexity increases when it
comes to completely closing the fracture lines in the
questions about painting the fracture lines. The high
precision of the controls makes it a complex task to
completely close the fracture line, as the start and end
points did not coincide. Achieving this task demands
Virtual Reality for Detailed Visualization and Generation of Proximal and Distal Bone Fracture Patterns
303

Figure 3: Editor interface for drawing fracture patterns. a) Bone selection menu, b) Drawing configuration menu, and c)
Fracture line deletion submenu.
Figure 4: Interaction system to draw the fracture bone pat-
tern using the controllers.
Table 1: Results of the user experience survey in the VR
environment.
Item Median Average
Interaction 5 4,6±0,49
Interface 5 5
Draw fracture lines 5 5
Join fracture lines 4 4±0,40
Close fracture lines 4 3,8±0,40
Delete fracture lines 5 4,6±0,49
Learning curve 3 3,4±0,49
Immersion and realism 3 3,2±0,40
Fluency 5 5
significant user dexterity. In the future, an automated
system will be incorporated to assist users in closing
the fracture line.
The degree of realism and immersion of the tool
and the learning curve stand out as the worst aspects
evaluated by the experts. The experts informed us
that the enhancement in bone visualization is signif-
icant, but they noted that the environment surround-
ing the bone fell short of resembling a real operating
room. This is due to the fact that the tool was de-
signed to improve the visualization of fracture lines
and deformities on bone surfaces, somewhat omitting
the environment in which the simulation was devel-
oped. Therefore, this is an aspect that needs improve-
ment in the future. On the other hand, although the
interaction mechanisms were rated as intuitive, repro-
ducing a clinical case without training the user is not
trivial. The initial training proved insufficient to facil-
itate rapid and accurate pattern drawing. However, as
participants advanced through the tests, the rendering
of fracture patterns became quicker and more precise,
resulting in a reduction of poorly drawn lines during
the process. In future versions, an initial scene will
be included to train users in the use of the tool and to
facilitate the drawing process.
Subsequently, the experts were asked to perform
the same tests with a keyboard and mouse without a
virtual reality environment. Table 2 presents feedback
obtained by the experts after assessing the system
without the virtual environment. While they noted
that the new system was more comfortable, the inter-
action to draw the fracture patterns and the visualiza-
tion was noticeably inferior. Achieving a specific per-
spective for model visualization proved to be a rather
tedious task with the mouse. Moreover, the accuracy
in drawing lines was not as precise as in the VR envi-
ronment. As depicted, the scores decrease in almost
all aspects evaluated. However, the learning curve is
lower than in the virtual reality-based system. This
may be attributed to users being more accustomed to
use this type of device for interaction with a 3D envi-
ronment.
GRAPP 2024 - 19th International Conference on Computer Graphics Theory and Applications
304
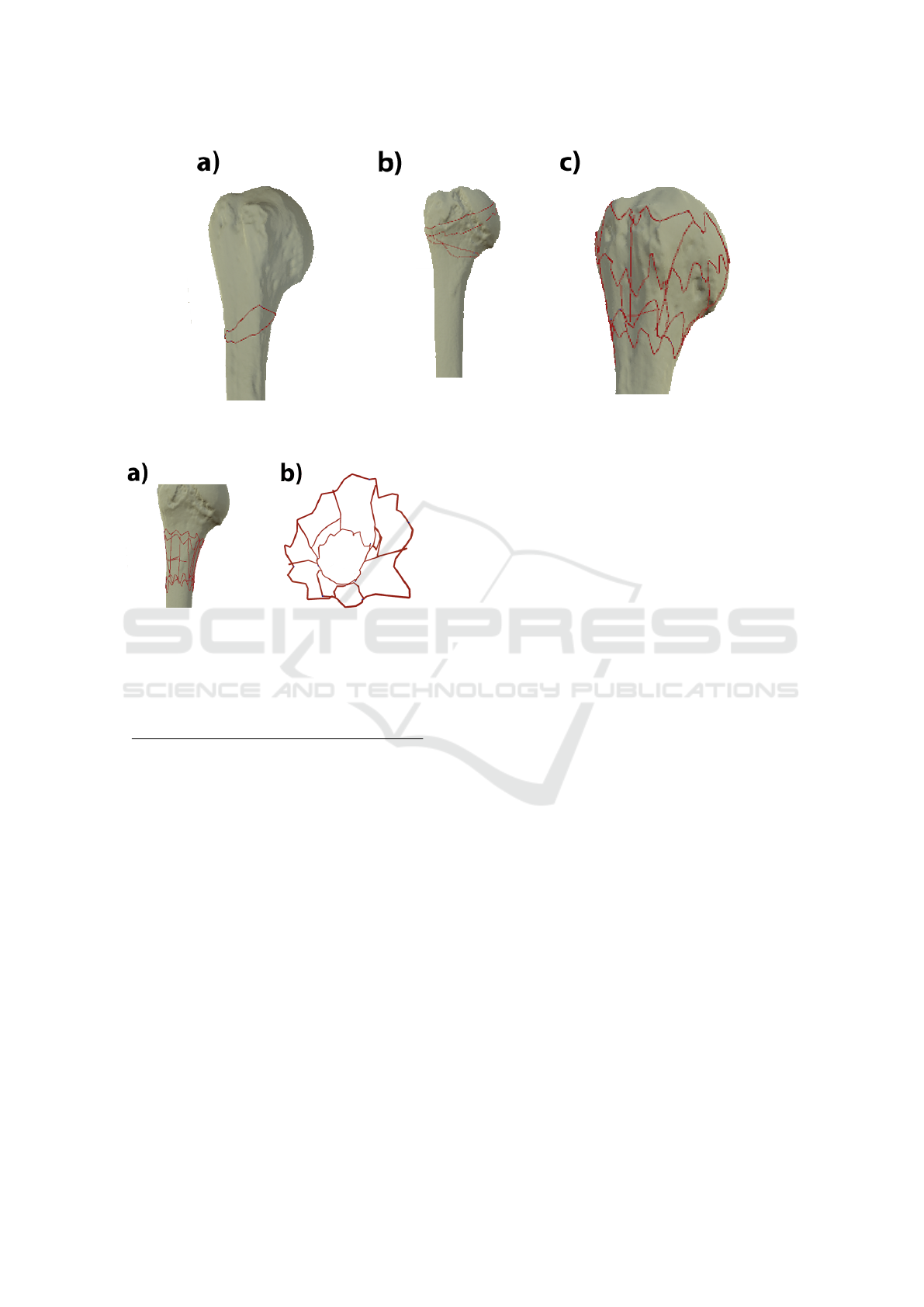
Figure 5: Different fracture patterns drawn in the end segment of the epiphysis of a human humerus. a) Represents an oblique
fracture, b) a intact wedge fracture and c) a fragmentary fracture.
Figure 6: a) Fracture pattern on a bone model. b) Frac-
ture pattern observed from the longitudinal axis of the bone
model.
Table 2: Results of the user experience survey without the
VR environment.
Item Median Average
Interaction 5 4,6±0,49
Interface 5 5
Draw fracture lines 3 3,4±0,49
Join fracture lines 3 3±0,63
Close fracture lines 3 2,6±0,8
Delete fracture lines 5 4,8±0,4
Learning curve 4 4,4±0,49
Immersion and realism 3 3 ±0
Fluency 5 5
5 DISCUSSION
VR allows users to interact with 3D models of frac-
tures in an immersive environment, providing a more
realistic and robust understanding of fracture charac-
teristics compared to traditional 2D imaging methods.
This includes understanding complex structures, ori-
entations of fracture lines, bone deformities, and de-
tails about bone fragment dispersion.
As the VR environment allows users to modify
viewing angles freely, this assists in creating precise
surgical plans as one can explore the fracture from
various perspectives that might not be possible with
traditional imaging. The capability to draw fracture
lines directly on the 3D bone models within the VR
environment also enhances the precision and person-
alization of surgical planning.
Haptic feedback is integrated into the VR tool,
providing the sensation of drawing on a real bone
surface via vibrations, improving the tactile realism.
This can be particularly useful for tactile learners and
enhances the overall understanding of the physical
characteristics of the bone and fractures. Further-
more, since the VR tool allows exporting of fracture
patterns, these can be integrated with other medical
tools or simulations, which can boost surgical plan-
ning or training processes.
The primary advantage, however, is that VR gives
the potential to rehearse, repeat, and correct pro-
cedures virtually before performing actual surgery,
which can improve the likelihood of positive patient
outcomes.
6 CONCLUSIONS AND FUTURE
WORK
This research has successfully demonstrated the ap-
plication of VR in the medical field, particularly in
the study of bone fractures. We have created a sys-
tem that allows medical professionals to visualize and
interact with 3D models of long bones to draw frac-
ture patterns. This technology has proven to be par-
ticularly effective in examining the complex areas of
bone fractures, such as the proximal and distal end
segments.
Virtual Reality for Detailed Visualization and Generation of Proximal and Distal Bone Fracture Patterns
305

The application developed significantly improves
the visualization of bone deformities as well as the in-
teraction to represent different clinical cases of frac-
ture on human bones. In addition, haptic feedback
is included when drawing, using the changes in the
geometry of the model. The ability to draw and ma-
nipulate fracture lines directly on the bone models
has been highly rated by experts, reflecting the rel-
evance in medical practice. Moreover, the ability to
export these fracture patterns enhances its application
in various medical scenarios, extending its utility be-
yond mere visualization. These patterns can be used
in other medical tools, facilitating a more comprehen-
sive use in diagnostics, treatment planning, and edu-
cational purposes.
The extension of the variety of patterns generated
with the tool enables a wider range of fractures to be
covered. This is a key element as the extension makes
it possible to work with a wider range of medical sce-
narios or generate databases with more accurate infor-
mation about the fracture area.
However, certain challenges such as the precision
in closing fracture lines and the degree of realism and
immersion need to be addressed. While the tool ex-
cels in visualizing fracture lines and bone deformities,
improvements in the simulation environment and user
training are required for a more comprehensive appli-
cation.
REFERENCES
A
¨
ım, F., Lonjon, G., Hannouche, D., and Nizard, R. (2016).
Effectiveness of virtual reality training in orthopaedic
surgery. Arthroscopy, 32(1):224–232.
Akhtar, K., Sugand, K., Sperrin, M., Cobb, J., Standfield,
N., and Gupte, C. (2015). Training safer orthopedic
surgeons. Acta Orthopaedica, 86(5):616–621.
Azar, F., Canale, S., and Beaty, J. (2020). Campbell’s Op-
erative Orthopaedics. Number v. 4. Elsevier Health
Sciences.
Citak, M., Gardner, M. J., Kendoff, D., Tarte, S., Krettek,
C., Nolte, L.-P., and H
¨
ufner, T. (2008). Virtual 3d
planning of acetabular fracture reduction. Journal of
Orthopaedic Research, 26(4):547–552.
Fu, Y., Hu, Y., and Sundstedt, V. (2022). A systematic liter-
ature review of virtual, augmented, and mixed reality
game applications in healthcare. ACM Transactions
on Computing for Healthcare, 3(2):1–27.
Gusai, E., Bassano, C., Solari, F., and Chessa, M. (2017).
Interaction in an immersive collaborative virtual real-
ity environment: A comparison between leap motion
and HTC controllers. In New Trends in Image Anal-
ysis and Processing – ICIAP 2017, pages 290–300.
Springer International Publishing.
Herne, R., Shiratuddin, M. F., Rai, S., Blacker, D., and
Laga, H. (2022). Improving engagement of stroke
survivors using desktop virtual reality-based serious
games for upper limb rehabilitation: A multiple case
study. IEEE Access, 10:46354–46371.
Homma, Y., Mogami, A., Baba, T., Naito, K., Watari,
T., Obayashi, O., and Kaneko, K. (2019). Is actual
surgical experience reflected in virtual reality simu-
lation surgery for a femoral neck fracture? Euro-
pean Journal of Orthopaedic Surgery & Traumatol-
ogy, 29(7):1429–1434.
Jones, D. (2010). Rockwood and green’s fractures in adults
(7th ed, 2 volume. The Journal of Bone & Joint
Surgery British Volume, 92-B(10):1480–1480.
Loetscher, T., Barrett, A. M., Billinghurst, M., and Lange,
B. (2023). Immersive medical virtual reality: still a
novelty or already a necessity? Journal of Neurology,
Neurosurgery & Psychiatry, 94(7):499–501.
Meinberg, E., Agel, J., Roberts, C., Karam, M., and Kel-
lam, J. (2018). Fracture and dislocation classification
compendium 2018. Journal of Orthopaedic Trauma,
32(1):S1–S10.
M
¨
oller, T. and Trumbore, B. (1997). Fast, minimum storage
ray-triangle intersection. Journal of Graphics Tools,
2(1):21–28.
Negrillo-C
´
ardenas, J., Jim
´
enez-P
´
erez, J.-R., Madeira, J.,
and Feito, F. R. (2021). A virtual reality simulator
for training the surgical reduction of patient-specific
supracondylar humerus fractures. International Jour-
nal of Computer Assisted Radiology and Surgery,
17(1):65–73.
Parra-Cabrera, G., P
´
erez-Cano, F. D., and Jim
´
enez-
Delgado, J. J. (2022). Fracture pattern projection
on 3d bone models as support for bone fracture
simulations. Computer Methods and Programs in
Biomedicine, 224:106980.
P
´
erez-Cano, F., Jim
´
enez-P
´
erez, J., Molina-Viedma, A.,
L
´
opez-Alba, E., Luque-Luque, A., Delgado-Mart
´
ınez,
A., D
´
ıaz-Garrido, F., and Jim
´
enez-Delgado, J. (2023).
Human femur fracture by mechanical compression:
Towards the repeatability of bone fracture acquisition.
Computers in Biology and Medicine, 164:107249.
Reer, F., Wehden, L.-O., Janzik, R., Tang, W. Y., and
Quandt, T. (2022). Virtual reality technology and
game enjoyment: The contributions of natural map-
ping and need satisfaction. Computers in Human Be-
havior, 132:107242.
Tsai, M.-D., Hsieh, M.-S., and Jou, S.-B. (2001). Virtual
reality orthopedic surgery simulator. Computers in Bi-
ology and Medicine, 31(5):333–351.
Vaughan, N., Dubey, V. N., Wainwright, T. W., and Middle-
ton, R. G. (2016). A review of virtual reality based
training simulators for orthopaedic surgery. Medical
Engineering & Physics, 38(2):59–71.
GRAPP 2024 - 19th International Conference on Computer Graphics Theory and Applications
306
