
Bridging Gaps in Fracture Rehabilitation: A Mobile Solution Proposal
for Comprehensive Recovery
Matthias Maszuhn
1
, Frerk M
¨
uller-Von Aschwege
1
, Felix Jansen
1
, Andreas Hein
1
, Hester Knol
2
,
David Snowdon
3
, Michael Buscherm
¨
ohle
4
, Dominik Barth
5
, Luisa Haag
5
, Nadine Wohlers
6
,
Linda R
¨
ude
6
and Oliver Pieske
6
1
OFFIS e. V., Escherweg 2, Oldenburg, Germany
2
Herodikos GmbH, August-Hanken-Str. 24, Oldenburg, Germany
3
Hochschule Osnabr
¨
uck, Albrechtstr. 30, Osnabr
¨
uck, Germany
4
KIZMO, Clinical Innovation Center for Medical Technology Oldenburg, Marie-Curie-Str. 1, Oldenburg, Germany
5
Dieter Marquardt Medizintechnik GmbH, Robert-Bosch-Str.1, Spaichingen, Germany
5
Evangelisches Krankenhaus Oldenburg - Klinik f
¨
ur Unfallchirurgie und Orthop
¨
adie, Sporttraumatologie, Steinweg 13-17,
Oldenburg, Germany
Keywords:
Aftercare, Fracture, Injury, Physiotherapy, Mobile Application, Pose Estimation, Neural Network, Load
Measurement.
Abstract:
This paper explores the prevalent challenges associated with musculoskeletal injuries across various demo-
graphics. It proposes the idea for a comprehensive mobile application designed to improve post-fracture
aftercare by addressing existing gaps in information sharing, personalization, and remote care. Comprising
three core components – recording and assessment of physiotherapy exercises, physical load measurement at
the fracture, and a shared documentation tool for all participants involved in the aftercare process – the system
aims to enhance patient compliance and improve recovery outcomes. The system will then be evaluated tech-
nically with healthy subjects to validate the system components. Subsequent usability evaluations will involve
feedback from both healthy subjects and potential end-users, paving the way for planned clinical investigations
with patients undergoing ankle fracture treatments to assess system efficacy, patient-reported outcomes, and
compliance.
1 INTRODUCTION
Musculoskeletal injuries are prevalent among in-
dividuals in Germany aged 65 and above (Fuchs
et al., 2013), often necessitating surgical interven-
tions. These injuries frequently result from falls
among elderly individuals (Kannus et al., 2002) and
require extended recovery periods. Respecting the de-
mographic shift, the frequency of such injuries is ex-
pected to further increase. Not only elderly people
suffer from musculoskeletal injuries, also younger in-
dividuals experience such injuries with an increasing
frequency (Rupp et al., 2021), particularly after acci-
dents, constituting a significant cause of work-related
absences (Bundesanstalt f
¨
ur Arbeitsschutz und Ar-
beitsmedizin, 2022). Beyond the impact on the qual-
ity of life, these injuries result in substantial health-
care and socioeconomic costs, including expenses
for surgical procedures, compensation for disability
leave, early retirement, rehabilitation measures, and
reduced productivity.
The quality of post-injury care is an essential fac-
tor for the success of the healing process. A good
quality can encourage a quick relief, full recovery of
the disease and is able to prevent further complica-
tions. The predominant factor influencing the over-
all expenses in patients with fractures and non-unions
is indirect costs, such as productivity-related losses
(Hak et al., 2014). Post-injury care encounters sev-
eral challenges in the current healthcare system. This
includes for example the insufficiently addressing of
prescriptions. Elderly individuals frequently receive
equivalent exercises and repetitions in physical ther-
apy following injuries, similar to younger patients.
(Teng et al., 2012). For a successful and fast recov-
ery of patients after musculoskeletal trauma surgery,
the patient requires individual treatment and therapy
by multiple healthcare professionals including sur-
geons, general physicians and physiotherapists (Fig-
ure 1). For an optimal multi modal, holistic and in-
646
Maszuhn, M., Aschwege, F., Jansen, F., Hein, A., Knol, H., Snowdon, D., Buschermöhle, M., Barth, D., Haag, L., Wohlers, N., Rüde, L. and Pieske, O.
Bridging Gaps in Fracture Rehabilitation: A Mobile Solution Proposal for Comprehensive Recovery.
DOI: 10.5220/0012434000003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 646-653
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.

dividual treatment, information about patients’ recov-
ery should be shared and discussed by the involved
healthcare professionals. However, studies indicate
that there still seems to be a lack of connectivity be-
tween healthcare professionals (Reeves and Zwaren-
stein, 2017). These shortcomings in patient centred
care lead to partially contradictory advice, which can-
not be comprehensively processed by the patients due
to insufficient expertise.
After being discharged from the hospital, surgeons
generally receive limited information about the pa-
tient’s recovery progress unless a subsequent oper-
ation is necessary. Physiotherapists customise ex-
ercise regimes to suit individual patients, however,
they only receive subjective feedback once or twice
a week. To date, there has been no exchange of in-
formation between physiotherapists and other health-
care professionals in Germany to adjust treatment.
If a re-injury takes place or if the process of recov-
ery diverges from expectations, it can prove to be
exceptionally disappointing for all those involved in
the post-injury care process. Insufficient communica-
tion often leads to a failure in documenting the fun-
damental reasons behind such setbacks. Noncompli-
ance with the healthcare professionals’ instructions,
incorrect instructions for specific patients, or errors
in the initial surgery may all contribute to this uncer-
tainty. Therefore, achieving full recovery from such
injuries hinges on patient compliance with daily exer-
cises, requiring motivation, education, and dedication
of patients and supervision, monitoring and coaching
by health care professionals. Due to the short and
limited therapy sessions, this supervision, coaching
and monitoring is often lacking, fostering insecurity
among both doctors and patients regarding the dura-
bility of the fracture.
An example demonstrating the importance of tai-
lored exercises and supervision during post surgery
treatment of musculoskeletal fractures is the weight-
bearing during recovery. The weight-bearing aspect
within post-care after getting a fracture injury re-
mains a contentious issue, as patients often have only
a rough estimate of the compression they can safely
apply to the affected body region. This is especially
valid for geriatric patients that often struggle to main-
tain the set weight-bearing restrictions (Kammerlan-
der et al., 2018). Commonly used training meth-
ods for weight bearing, for example using house-
hold weight-scales to define the load, neither show
good short-term nor long-term learning effects of the
prescribed limits (Dabke et al., 2004) (Braun et al.,
2017). Poorly managed weight-bearing during differ-
ent phases of post-injury care can have adverse conse-
quences on the long-term healing process, underscor-
ing the importance of effective communication and
measurement of these parameters.
Another aspect of individual care after muscu-
loskeletal injury is the need for more adaptable op-
tions for participating in physiotherapy. This require-
ment has become less pressing since the outbreak of
the COVID-19 pandemic, as scheduling appointments
proved challenging during times of restricted human
contact. For instance, attending physiotherapy ses-
sions in person often necessitates the assistance of
family members due to the patient’s limited mobility.
In addition, elderly people and patients with jobs re-
quiring traveling or or having an irregular daily work-
ing life benefit from a solution that makes remote
training sessions and exercises possible in an indepen-
dent setting full of flexibility. The reduced availability
of healthcare facilities in rural areas (Kassen
¨
arztliche
Bundesvereinigung Kd
¨
oR, 2022), combined with on-
going shortage of skilled workers (Bundesagentur f
¨
ur
Arbeit, 2023), further fuels the demand for meth-
ods that enable home-based physiotherapy. Nonethe-
less, existing online physiotherapy methods can be
challenging due to the need of therapists to demon-
strate exercises in front of a camera while looking
at the screen at the same time. Moreover, ambula-
tory physiotherapy approaches must be thoughtfully
considered to ensure patient compliance and maintain
the same level of efficacy as in on-site physiother-
apy. ”Its worth noting that correctly executed digital
physiotherapy has the potential to be just as effective
or even more effective than on-site physiotherapy.”
(Lara-Palomo et al., 2022) (Weise et al., 2022).
In summary, we have identified three primary
challenges within the current post-fracture aftercare
process we aim to address in this research:
1. How can we enhance the effectiveness and adher-
ence of digital physiotherapy as compared to cur-
rent literature?
2. How can we facilitate patient awareness of the
weight-bearing restrictions associated with their
fracture?
3. How can we enhance the documentation process
to facilitate the sharing of pertinent aftercare in-
formation among all stakeholders involved?
The following chapters are structured as follows:
Firstly, we outline our contribution and discuss cur-
rent related literature in section 2. Then we present
our method for addressing the research questions
mentioned above in section 3. Finally, we present
our findings. This is followed by a description of the
methodology in section 4. Our goal is to conduct ex-
tensive research to determine the effect of our appli-
cation on post-injury recovery. We compare the af-
Bridging Gaps in Fracture Rehabilitation: A Mobile Solution Proposal for Comprehensive Recovery
647
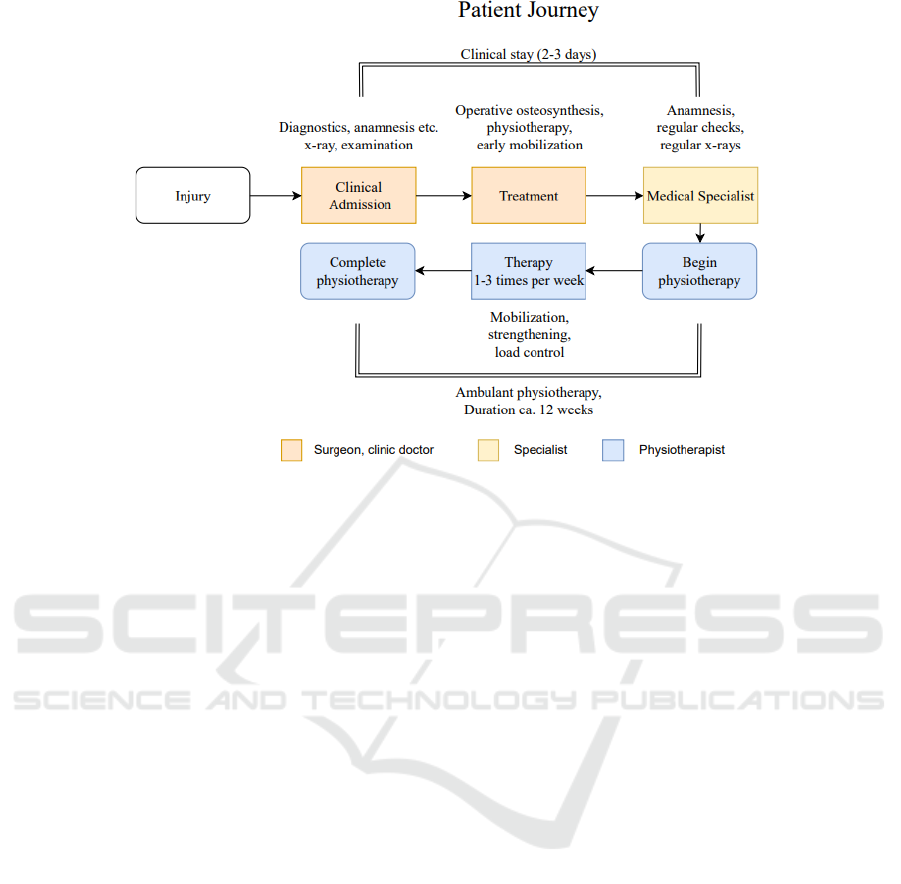
Figure 1: The diagram depicts a common pathway for patients following an ankle fracture and the stakeholders associated
with each stage. Following a hospital stay for up to three days, the patient is referred to a specialist who conducts periodic
examinations and x-rays on the injured area. The patient then undergoes physiotherapy for roughly twelve weeks with varying
phases of load management.
tercare process to conventional practices in section 5,
providing an objective evaluation. In addition, sec-
tion 6 presents a conclusion and outlines potential fu-
ture work.
2 RELATED WORK
Research into the usability of mobile applications
to assist physiotherapy has gained significant impor-
tance, particularly in light of the COVID-19 pan-
demic. Kasnakova et al. conducted a pivotal study
demonstrating that the utilization of mobile health ap-
plications can substantially enhance the rehabilitation
process (Kasnakova et al., 2022). Moreover, there
are already various systems available to assist patients
with at-home exercise programs. For instance, Ko-
maris et al. assessed an IMU-based system designed
to ensure the correct execution of physiotherapy exer-
cises during unsupervised treatments (Komaris et al.,
2022). Others have explored intricate 3D motion
capture systems (Mousavi et al., 2020) or offered
disease-specific information and structured training
schedules to enhance exercise accuracy (Thiengwit-
tayaporn et al., 2023). Weber et al. introduced a
smartphone-assisted training system that fosters the
repetition and consolidation of learned exercises by
facilitating audio-visual communication between pa-
tients and physiotherapists (Weber et al., 2023). A re-
view of current literature reveals a variety of exercise
evaluation tools based on motion tracking or inertial
measurement units (IMU) to assist patients. However,
we propose an experimental approach by employing
a neural network for the evaluation of exercise cor-
rectness and repetitions. Importantly, this approach
would not require a complex setup and is therefore
more suitable for at-home assessments. Our approach
leverages marker-less motion capture technology us-
ing standard 2D cameras, readily available in patients’
smartphones, tablets, and laptops.
In the domain of load measurement systems in
physiotherapy, Braun et al. conducted a survey in
2018 to explore the usage of measurement instru-
ments by physiotherapists in Germany (Braun et al.,
2018). Their findings indicated that physiotherapists
generally have a favorable view of using measurement
instruments, provided that there is financial compen-
sation for acquiring them. Notably, the prevalent ap-
proach in research involves insole measurement sys-
tems, which are already applied for gait, load, and
activity analysis (Braun et al., 2016). By integrating
the measurement system into the patient’s implant, we
aim to eliminate the need for additional tool purchases
and ensure the continuous availability of load data.
Regarding documentation tools for aftercare,
Griefahn et al. conducted a Delphi study to assess
the potential benefits of digitization in the documen-
tation processes of physiotherapists, outlining specific
HEALTHINF 2024 - 17th International Conference on Health Informatics
648

requirements for such an application (Griefahn et al.,
2020). Building upon this study, our objective is
to create a more standardized documentation process
that actively involves all stakeholders while maintain-
ing a degree of flexibility.
Finally, we would like to emphasize that the in-
tegration of these three components – mobile appli-
cations to support physiotherapy, load measurement
systems, and documentation tools for aftercare – rep-
resents a promising innovation. To the best of our
knowledge, such a combination has not been exten-
sively explored to date. We believe that this holistic
approach has the potential to significantly enhance the
efficiency and effectiveness of physiotherapeutic care.
3 CONTRIBUTION
In this work, we propose a comprehensive mobile ap-
plication that tackles the aforementioned problems.
Our primary objective is to enable individualized,
self performed and (at least partly) automatically su-
pervised training and rehabilitation exercises. Our
secondary objective is to equip patients with a tool
to monitor their weight-bearing and warn them if
they exceed the set limits. The third objective of
this project is to facilitate seamless data exchange
between physicians, physiotherapists, and patients,
streamlining and individualizing the aftercare jour-
ney. By addressing the existing gaps in information
sharing, personalization, and remote care, our system
aims to not only enhance the quality of post-injury
care but also foster patient compliance, ultimately re-
sulting in improved recovery outcomes.
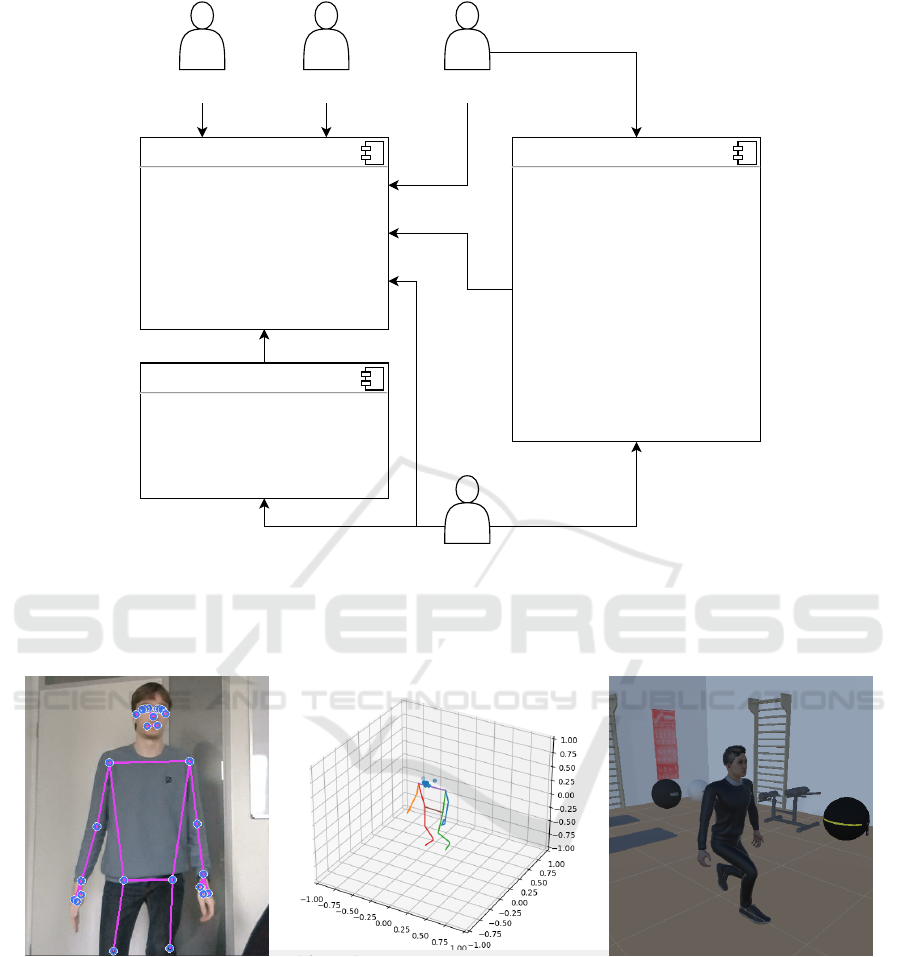
Our system is structured into three core compo-
nents shown in Figure 2, each offering a dedicated
interface for different users:
1. Recording and Assessment System for Physio-
therapy Exercises: This component serves as a com-
prehensive solution for exercise recording and eval-
uation. Physiotherapists can easily record exercises
using a standard camera, whether a smartphone or
webcam, or select from a pre-defined library of exer-
cises and customise them with individual patient an-
notations. These video recordings are employed to
train a neural network, which then assesses exercise
execution for correctness. Using marker-less motion
tracking technology, the system generates a 3D avatar
demonstrating the exercise on the patient’s tablet or
smartphone. AI algorithms dynamically adjust the
camera angle to provide the most optimal view based
on the specific exercise. The effectiveness and adher-
ence of the system is then being evaluated.
2. Load Measurement System: This system is
used for real-time monitoring and assessment of the
physical stress on the affected area, and alerts the pa-
tient in the event of overexertion. Healthcare profes-
sionals can access a graphical representation which
illustrates the linkage between physical strain, exer-
cise regimes, and the pain reported by patients. This
integrated view promotes more informed decision-
making concerning the suitability of exercises for
each patient’s distinctive situation.
3. Shared Documentation Tool: A collabora-
tive platform facilitates all stakeholders involved in
the aftercare process to access and update relevant
treatment-related data. Such information encom-
passes data obtained through exercise evaluations and
load measurements. Moreover, the tool functions as
an appointment prompt for patients, providing them
with an overview of their present condition and out-
lining the subsequent steps in their recovery process,
thereby serving a motivational purpose.
4 METHODOLOGY
4.1 Exercise Recording and Assessment
In our primary stage, we will concentrate on set-
ting up the tool for exercising and assessment. Al-
though our application has the potential to cover var-
ious fractures with similar post-injury care regimens,
we have chosen to use an ankle fracture as a repre-
sentative example for exercises and studies. Ankle
fractures are of special interest in this context as the
recommended exercises often involve delicate move-
ments of the leg and foot, which can prove difficult
to identify using motion capture tools. Consequently,
any approach capable of assessing these exercises
must also have the capacity to identify more complex
movements. The aftercare for ankle fractures typi-
cally comprises three phases, each varying in dura-
tion depending on the patient’s progress: the initial
stage involves no weight-bearing, the second stage
introduces partial weight-bearing, and the third stage
permits full weight-bearing adapted to pain levels. In
collaboration with physiotherapists in the team, we
have selected two exercises for each stage, resulting
in a total of six exercises that patients with ankle frac-
tures typically perform during their post-injury recov-
ery program.
Our primary objective in this stage is to display an
avatar demonstrating these exercises on the patient’s
mobile device as seen in Figure 3. Physiotherapists
should have the ability to record their exercises or
select from a library of pre-recorded exercises. To
facilitate exercise recording, we require a motion-
Bridging Gaps in Fracture Rehabilitation: A Mobile Solution Proposal for Comprehensive Recovery
649
Exercise Recording and Assessment
For physiotherapists:
+ Recording videos of exercises
with custom annotations
+ Choosing from pool of
predefined exercises
For patients:
+ Demonstrates exercises by
displaying an avatar on tablet or
smartphone
+ Estimates the patient's pose in
real-time from a video-stream
+ Evaluates repititions and
accuracy of exercises using a
recurrent neural network (RNN)
Physiotherapist
Patient
Surgeon
Clinic doctor /
Medical specialist
Documentation
+ Display of graphs for exercise
assessments and measured physical
load
+ Overview of injury and rehabilitation
process
+ Collection of documents (e.g. privacy
statement, therapy reports)
+ Schedular and appointment reminder
Load Measurement
+ Integrates different sensors to
measure relevant parameters
+ Includes strain gauge monitoring
physical load
+ Transfers data to application via NFC
Figure 2: The graphic gives an overview of the components planned in our application. The physiotherapists get access to an
exercise recording tool which is then used as the basis for the exercise assessments done by the patients. The documentation
tool gathers the data collected by the exercise assessments and the load measurements and offers further functionality such as
a collection of documents and a scheduler and appointment reminder.
Figure 3: The graphic displays the estimated joint coordinates in a 3D space on a scale from -1 to 1 as estimated by MediaPipe.
We used a standard webcam to record a squat here (left side). On the right side, there is an example of the animation for another
recorded exercise that could be enriched with additional information by the physiotherapist and displayed to a patient.
capture tool. We consider two established open-
source libraries, MediaPipe developed by Google and
OpenPose, which is a library developed by a group
of researchers and is free for commercial and non-
commercial use (Cao et al., 2017). Both libraries are
capable of identifying and tracking key body land-
marks in real-time video, such as those obtained from
a 2D camera stream. This technology allows to con-
vert a video stream into a sequence of joint positions
for each frame, with a target frame rate of approxi-
mately 20 images per second to ensure precision in
capturing even subtle movements. First experiments
with MediaPipe have shown that utilizing MediaPipe
for ankle joint detection poses a considerable chal-
lenge as subjects need to be fully captured within the
camera image, introducing potential deviations. This
difficulty arises from MediaPipe’s reliance on only
three coordinates in the ankle and feet area, impact-
HEALTHINF 2024 - 17th International Conference on Health Informatics
650

ing the precision of joint detection. Therefore, our
proposed solution involves integrating the pose esti-
mation capabilities of MediaPipe with a straightfor-
ward 2D camera detection of joint angles. This hybrid
approach aims to enhance the reliability of ankle joint
detection and address the limitations associated with
using MediaPipe alone.
By applying inverse kinematics, we can determine
the joint angles required to achieve the desired posi-
tion, creating a fluid animation of the recorded ex-
ercises that can be applied to any character model
with a humanoid skeletal rig. Adobe’s Mixamo pro-
vides a robust platform for character animation and
rigging, offering pre-rigged characters that are free to
use. Our goal is implementing animations for various
3D characters of Mixamo, enabling patients to select
their preferred avatar.
Another important objective is the detection and
assessment of patients’ exercises, primarily focusing
on two metrics: First the number of exercise repe-
titions and second the alignment with the therapist’s
example. To achieve this, we intend to train a neural
network with the joint angles obtained from record-
ings of exercises demonstrated by physiotherapists.
Specifically, we intend to apply a recurrent neural net-
work (RNN) to identify patterns and repetitions in ex-
ercises. Recognizing that patients and physiothera-
pists may perform exercises with variations or differ-
ent orientations to the camera system, we intend to es-
tablish joint angle limits for each exercise, which will
be included in the training dataset. Rather than seek-
ing exact replication of exercises, we will prioritize
determining whether a movement exceeds joint angle
limits (indicating potential harm) or falls below the
threshold of necessary motion (indicating ineffective-
ness). To gather a substantial amount of data, phys-
iotherapists shall document and classify ten iterations
of each movement.
4.2 Load Measurement
In the subsequent stage, we will introduce a measure-
ment system to assess the physical load on the frac-
ture. Initially, we equip a stabilizing sleeve with dif-
ferent sensors to measure relevant parameters at the
fracture like the physical load or the range of motion.
An integrated sensor will be utilized to closely mon-
itor load levels at frequent intervals. The recorded
data will be seamlessly transferred to a documenta-
tion system and displayed on the patient’s smartphone
or tablet. Our ultimate objective is to integrate a
strain gauge technology into an implant and to com-
bine the measurements of multiple sensors into an
holistic measurement of the load affecting the frac-
ture. However, due to regulatory constraints that ne-
cessitate medical approval for implants, we will also
measure the ground reaction forces using insoles in
our initial studies. We will subsequently compare the
recorded forces obtained from the insoles with those
obtained from our experimental system, allowing us
to assess the performance and accuracy of both mea-
surement methods.
4.3 Documentation
The final component of our application will combine
stress measurement data and exercise assessments
into a comprehensive documentation system with sep-
arate views and permissions for doctors, physiothera-
pists and patients. Additionally, the system will in-
corporate essential documents, such as therapy re-
ports and the patient’s privacy statement, ensuring
that these documents only need to be completed once.
Patients will be granted access to a graphical repre-
sentation of exercise history, weight-bearing capabili-
ties of their fracture, and the range of motion in the
affected joint. The app will function as a motiva-
tional tool for patients, inspiring them to adhere to
their workout plans and allowing them to document
personal impressions, including pain levels. This data
will provide physiotherapists with valuable insights
into the patients’ at-home exercise regimens. Fur-
thermore, the tool will help sharing important infor-
mation between healthcare professionals and improve
communication between them. Finally, the docu-
mentation system will feature a scheduler for physio-
therapy sessions, future surgeries, and other appoint-
ments, empowering patients to directly arrange ap-
pointments with doctors and physiotherapists while
receiving timely reminders.
5 STUDY DESIGN
The evaluation of our application will include various
studies to be explained later in this section. The aim
is to analyse the systems prototype and carry out ini-
tial trials in a clinical environment. To examine the
subsystems, a technical evaluation will be conducted
in a descriptive research design with healthy subjects.
For the load measurement system, we need to en-
sure the validity and reliability of the data. There-
fore, we will compare the recordings with a measure-
ment system in the laboratory which we consider to
be the gold standard. The same applies to the motion
tracking system, where we will compare the results of
our single camera approach with MediaPipe or Open-
Pose with a more complex multi-camera system in the
Bridging Gaps in Fracture Rehabilitation: A Mobile Solution Proposal for Comprehensive Recovery
651

laboratory. Following the technical evaluation, we
will continue with a system evaluation including all
the single components in a usability research design.
Healthy subjects representing patients and healthcare
professionals will evaluate the system regarding user-
friendliness and patient safety criteria. Once these
results have been implemented, initial investigations
in a clinical setting are planned. Patients undergoing
open reduction and internal fixation of ankle fractures
(Weber B type; no syndesmotic rupture) will be re-
cruited. Exclusion criteria would be impaired mobil-
ity or gait abnormalities prior to the fracture event,
patients with multiple injuries and patients under 18
years of age. Patient reported outcome measures, gait
parameters, frequency of use and compliance will be
evaluated.
6 CONCLUSION
In conclusion, this paper addresses the pressing chal-
lenges within the realm of post-fracture aftercare, rec-
ognizing the substantial impact of musculoskeletal in-
juries on individuals of all age groups and their asso-
ciated healthcare and socioeconomic costs. The qual-
ity of post-injury care is essential in determining re-
covery outcomes and preventing complications.
Our proposed mobile application, consisting of
three core components, presents a promising solu-
tion to these challenges. By enabling individual-
ized, self-performed exercise routines, facilitating
real-time load measurement, and streamlining data
exchange among patients, physicians, and physiother-
apists, we aim to enhance the overall quality of post-
injury care. The comprehensive methodology out-
lined in this paper provides a clear path for the imple-
mentation of these components, including the inno-
vative use of neural networks for exercise evaluation
and the integration of a strain gauge in an implant for
load measurement.
In future work, special emphasis should be placed
on the continuous refinement of the user interface
and user experience. Ensuring an intuitive and user-
friendly design will be key to maximising patient and
healthcare professional engagement with the mobile
application. Additionally we will investigate an ap-
proach combining load measurement data with coor-
dinates obtained from pose estimation as inputs for
our neural network. This integration has potential to
substantially improve the accuracy of exercise assess-
ments, offering a more comprehensive insight into the
physical capabilities of patients throughout their reha-
bilitation process.
ACKNOWLEDGMENT
This research paper is a part of the THEBEA
project, which has been generously funded by the
”Bundesministerium f
¨
ur Bildung und Forschung”
(BMBF), the German Federal Ministry of Education
and Research. We extend our gratitude to BMBF for
their support in advancing innovative solutions for im-
proving post-fracture aftercare.
REFERENCES
Braun, B. J., Bushuven, E., Hell, R., Veith, N. T.,
Buschbaum, J., Holstein, J. H., and Pohlemann, T.
(2016). A novel tool for continuous fracture aftercare -
clinical feasibility and first results of a new telemetric
gait analysis insole. Injury, 47(2):490–494.
Braun, B. J., Veith, N. T., Rollmann, M., Orth, M., Fritz,
T., Herath, S. C., Holstein, J. H., and Pohlemann, T.
(2017). Weight-bearing recommendations after oper-
ative fracture treatment—fact or fiction? gait results
with and feasibility of a dynamic, continuous pedo-
barography insole. Int. Orthop., 41(8):1507–1512.
Braun, T., Rieckmann, A., Weber, F., and Gr
¨
uneberg, C.
(2018). Current use of measurement instruments
by physiotherapists working in germany: a cross-
sectional online survey. BMC health services re-
search, 18(1):810.
Bundesagentur f
¨
ur Arbeit (2023). Blickpunkt arbeitsmarkt
– fachkr
¨
afteengpassanalyse 2022. Technical report,
Statistik/Arbeitsmarktberichterstattung, N
¨
urnberg.
Bundesanstalt f
¨
ur Arbeitsschutz und Arbeitsmedizin
(2022). Volkswirtschaftliche kosten durch arbeit-
sunf
¨
ahigkeit 2021. https://www.baua.de/DE/Themen/
Monitoring-Evaluation/Zahlen-Daten-Fakten/pdf/Ko
sten-2021.pdf.
Cao, Z., Simon, T., Wei, S.-E., and Sheikh, Y. (2017). Real-
time multi-person 2d pose estimation using part affin-
ity fields.
Dabke, H. V., Gupta, S. K., Holt, C. A., O’Callaghan,
P., and Dent, C. M. (2004). How accurate is partial
weightbearing? Clin. Orthop. Relat. Res., 421:282–
286.
Fuchs, J., Rabenberg, M., and Scheidt-Nave, C.
(2013). Pr
¨
avalenz ausgew
¨
ahlter muskuloskelettaler
erkrankungen. Bundesgesundheitsblatt - Gesundheits-
forschung - Gesundheitsschutz, 56(5):678–686.
Griefahn, A., Wolf, E., and Zalpour, C. (2020). Wie kann
die dokumentation in der physiotherapie durch die
digitalisierung effektiver und effizienter werden? –
eine delphi-studie. physioscience, 16(03):101–110.
Hak, D. J., Fitzpatrick, D., Bishop, J. A., Marsh, J. L., Tilp,
S., Schnettler, R., Simpson, H., and Alt, V. (2014).
Delayed union and nonunions: Epidemiology, clinical
issues, and financial aspects. Injury, 45:S3–S7.
Kammerlander, C., Pfeufer, D., Lisitano, L. A., Mehaffey,
S., B
¨
ocker, W., and Neuerburg, C. (2018). Inability of
HEALTHINF 2024 - 17th International Conference on Health Informatics
652

older adult patients with hip fracture to maintain post-
operative weight-bearing restrictions. J. Bone Joint
Surg. Am., 100(11):936–941.
Kannus, P., Palvanen, M., Niemi, S., Parkkari, J., and
J
¨
arvinen, M. (2002). Increasing number and inci-
dence of low-trauma ankle fractures in elderly peo-
ple: Finnish statistics during 1970-2000 and projec-
tions for the future. Bone, 31(3):430–433.
Kasnakova, P., Mihaylova, A., Djurdjev, B., and Tornyova,
B. (2022). Randomized controlled trial of multidis-
ciplinary rehabilitation therapy using mobile applica-
tions in cases of ankle fractures. European journal of
translational myology, 32(2).
Kassen
¨
arztliche Bundesvereinigung Kd
¨
oR (2022).
Regionale verteilung der
¨
Arztinnen und
¨
Arzte in der vertrags
¨
arztlichen versorgung.
https://gesundheitsdaten.kbv.de/cms/html/16402.php.
Komaris, D.-S., Tarfali, G., O’Flynn, B., and Tedesco, S.
(2022). Unsupervised imu-based evaluation of at-
home exercise programmes: a feasibility study. BMC
sports science, medicine & rehabilitation, 14(1):28.
Lara-Palomo, I. C., Gil-Mart
´
ınez, E., Ram
´
ırez-Garc
´
ıa, J. D.,
Capel-Alcaraz, A. M., Garc
´
ıa-L
´
opez, H., Castro-
S
´
anchez, A. M., and Antequera-Soler, E. (2022).
Efficacy of e-health interventions in patients with
chronic low-back pain: A systematic review with
meta-analysis. Telemed. J. E. Health., 28(12):1734–
1752.
Mousavi, S. H., Hijmans, J. M., Moeini, F., Rajabi, R., Fer-
ber, R., van der Worp, H., and Zwerver, J. (2020). Va-
lidity and reliability of a smartphone motion analysis
app for lower limb kinematics during treadmill run-
ning. Physical therapy in sport : official journal of the
Association of Chartered Physiotherapists in Sports
Medicine, 43:27–35.
Reeves, S, P. F. H. R. G. J. and Zwarenstein, M. (2017).
Interprofessional collaboration to improve profes-
sional practice and healthcare outcomes. Cochrane
Database of Systematic Reviews, (6).
Rupp, M., Walter, N., Pfeifer, C., Lang, S., Kerschbaum,
M., Krutsch, W., Baumann, F., and Alt, V. (2021). The
incidence of fractures among the adult population of
germany–an analysis from 2009 through 2019. Dtsch.
Arztebl. Int., 118(40):665–669.
Teng, K., Eng, C., Hess, C. A., Holt, M. A., Moran, R. T.,
Sharp, R. R., and Traboulsi, E. I. (2012). Building an
innovative model for personalized healthcare. Cleve
Clin J Med, 79(Suppl 1):S1–9.
Thiengwittayaporn, S., Wattanapreechanon, P., Sakon, P.,
Peethong, A., Ratisoontorn, N., Charoenphandhu, N.,
and Charoensiriwath, S. (2023). Development of a
mobile application to improve exercise accuracy and
quality of life in knee osteoarthritis patients: a ran-
domized controlled trial. Archives of Orthopaedic and
Trauma Surgery, 143(2):729–738.
Weber, F., M
¨
uller, C., Bahns, C., Kopkow, C., F
¨
arber, F.,
Gellert, P., Otte, I., Vollmar, H. C., Brannath, W.,
Diederich, F., Kloep, S., Rothgang, H., Dieter, V.,
Krauß, I., Kloek, C., Veenhof, C., Collisi, S., Rep-
schl
¨
ager, U., B
¨
obinger, H., Gr
¨
uneberg, C., Thiel, C.,
and Peschke, D. (2023). Smartphone-assisted training
with education for patients with hip and/or knee os-
teoarthritis (smart-e): study protocol for a multicentre
pragmatic randomized controlled trial. BMC Muscu-
loskeletal Disorders, 24(1):221.
Weise, H., Zenner, B., Schmiedchen, B., Benning, L., Bu-
litta, M., Schmitz, D., and Weise, K. (2022). The ef-
fect of an app-based home exercise program on self-
reported pain intensity in unspecific and degenera-
tive back pain: Pragmatic open-label randomized con-
trolled trial. J. Med. Internet Res., 24(10):e41899.
Bridging Gaps in Fracture Rehabilitation: A Mobile Solution Proposal for Comprehensive Recovery
653
