
Quantified Health: A Feasibility Study on a Sensor-Based Feedback
and Assistance System in Cardiology, Oncology and Orthopaedics
Anne Grohnert
1
, Michael John
1
, Benny Häusler
1
, Christian Giertz
1
, Mirko Wolschke
2
, Jana Liebach
2
,
Rona Reibis
3
, Anne Klemmer
3
, Lisa Konrad
4
, Silke Kollath
4
and Jan C. Zoellick
5
1
Fraunhofer FOKUS, Kaiserin-Augusta-Allee 31, 10589 Berlin, Germany
2
Orthopaedics and Oncology clinic, Reha-Zentrum Lübben, Postbautenstraße 50, 15907 Lübben, Germany
3
Kardiologische Gemeinschaftspraxis am Park Sanssouci Potsdam, Zimmerstrasse 7A, 14471 Potsdam, Germany
4
Theraphysia GmbH, Hellersdorfer Straße 77, 12619 Berlin, Germany
5
Charité - Universitätsmedizin Berlin, corporate member of Freie Universität Berlin and Humboldt-Universität zu Berlin,
Charitéplatz 1, 10117 Berlin, Germany
Keywords: Mobile Assistance Systems, Sensor-Based Feedback, Telemedicine, Digital Care, Everyday Care.
Abstract: This paper reports the results of the Quantified Health project that developed a complex, digitally supported
intervention. The project provides insights into how a sensor-based system can be organizationally integrated
into the existing workflows of everyday treatment. The concluding pilot study took place in three medical
facilities and addressed patients of orthopaedic, oncologic and cardiologic diseases in an in- or outpatient
therapeutic setting. As a study result from the user's perspective, it is very appreciated to objectify the patient’s
health related behavior. Care providers considered it positive that they received more data from patients'
everyday lives and that the improved data situation can lead to more sustainable care. On the other side, the
time required to integrate a new digital application into the tightly scheduled daily treatment routine was
perceived as a hindering factor. Nevertheless, the results of the study show that a more generic sensor-based
assistance system could be used for different diseases and cross sectoral. Furthermore, the constant contact
with therapists increases patients' motivation to engage in health-preserving activities (self-regulation).
1 INTRODUCTION
In order to maintain or optimize the success of
temporary rehabilitation measures, longer-term
sustainable therapy is required. Particularly after an
inpatient stay, patients necessarily do not economize
movement sequences and control exercise limits
under everyday conditions (Thimmel et al., 2018).
During rehabilitation, the patient is subject to
constant supervision by doctors and therapists. In
contrast, after rehabilitation, the patient may
increasingly fall back into habitual behavioural
patterns. In the case of heart and pulmonary diseases,
but also in the field of oncology and orthopaedics,
most patients often have fears and inhibitions when
they return to work or everyday life. This leads to the
patient avoiding regular physical activities such as
walking or cycling. However, excessive intensity of
exercises can also have serious consequences for the
patient: Patients who were previously very active in
sports often exert themselves too much despite their
limited physical functionality.
Individualized therapy can help to strengthen the
general health condition and body awareness and to
consolidate the therapeutic progress already achieved
during rehabilitation. The possibility of objectifying
the own behavior with support by sensory feedback
and assistance systems offers a great opportunity for
patients to permanently change their own behavior
(Plaete et al., 2015). This helps patients to manage
better with everyday life and to exert themselves
more economically in their regular routines. By
improving their mobility in daily routines, patients
experience an increase in their quality of life, which
motivates them to live healthier and more sustainable
(self-motivation and self-control).
Especially in times like Covid 19, telemedical
feedback and assistance systems help to reduce
physical contact between patients and doctors while
maintaining therapeutic measures and treatment
quality (Omboni et al., 2022). Patients are supported
in their daily routines and healthcare professionals
retain control of the treatment process through
628
Grohnert, A., John, M., Häusler, B., Giertz, C., Wolschke, M., Liebach, J., Reibis, R., Klemmer, A., Konrad, L., Kollath, S. and Zoellick, J.
Quantified Health: A Feasibility Study on a Sensor-Based Feedback and Assistance System in Cardiology, Oncology and Orthopaedics.
DOI: 10.5220/0012431100003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 628-637
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
integrated feedback functionalities without the need
for physical presence.
Thus, the "Quantified Health" project focused on
investigating the factors and structures of telemedical
assistance systems that are both beneficial and
detrimental to the acceptance, use and satisfaction of
users, i.e. care providers and patients. The system was
testet with a variety of indications from different
medical disciplines in order to figure out how a
telemedical assistance system can contribute to cross-
indication, cross-specialty and cross-sector treatment
processes.
To assess the feasibility and usability of the
Quantified Health system an accompanying pilot
study was carried out at the rehabilitation-center in
Lübben (oncology, orthopaedics), the cardiology
practice at Sanssouci Park and at the orthopaedic
practice Theraphysia. For this purpose, 56 patients
were recruited during their stay in the participating
clinics or by the outpatient facilities and were
supervised by medical staff who were consulted about
this care approach in form of interviews.
2 RECENT WORK
Due to our knowledge, the approach of using a
telemedical assistance system across all indications
and sectors has not yet been adequately considered.
Research has already been conducted on sensor-based
feedback and assistance systems for individual
indications. Naeemabadi et al., 2020 provide an
overview of studies of sensor-based feedback systems
that were used for specific indications in the field of
orthopaedics (e.g. knee and hip endoprosthetics).
Eichler et al., 2019 investigated the use of a system
for movement therapy with real-time feedback based
on optical sensor technology in an evidence study, but
also for specific indications in the field of
orthopaedics. For cardiological diseases, Kumazawa
et al., 2022 examined the use of a training system with
computer-generated animations and Zhong et al.,
2023 provide an overview of the long-term effects of
cardiac remote rehabilitation for patients with
coronary heart disease. In a systematic review, Brick
et al., 2023 state that further research with more
diversified samples, common measures of disability
and pragmatic study designs are needed in the field of
oncology to advance telemedicine in cancer
rehabilitation due to the heterogeneity of the diseases.
Algarni et al., 2022 found in a survey of patient
perceptions of tele-rehabilitation across indications
that most patients are very or moderately confident
that therapists can successfully assess and treat their
problems using tele-rehabilitation. Wang et al, 2023
also used a survey to investigate the intention to use
and factors influencing the use of telerehabilitation to
treat patients with cross-indication rehabilitation
needs. Both studies did not consider the provider's
perspective.
In addition to the studies mentioned above, the
“Quantified Health” project investigated whether and
how a telemedicine system with specific functions
can be used across indications and sectors. The
evaluation of the technical feasibility and the
acceptance of the system from the perspective of
providers and patients were central to this research.
3 QUANTIFIED HEALTH
SYSTEM
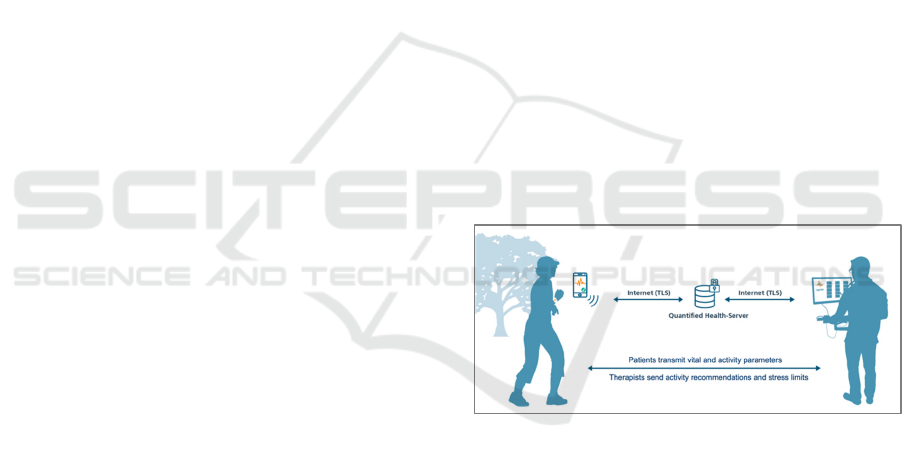
The Quantified Health system consists of several
components (see Figure 1). On the one hand, there is
the mobile patient app, which can use different
commercially available wearables as a data source
and, on the other, the therapy application for medical
staff to view the patient's individual data. The
Quantified Health Server serves as a central data
collection point and makes the data available to the
applications via secure transport.
Figure 1: System components of the Quantified Health
system.
3.1 Quantified Health App
The mobile component for patients consists of an app
and body-closed sensors in form of a smartwatch.
There are also input options for weight, blood
pressure and general well-being. The current vital and
activity parameters are displayed on the smartphone
app in the form of color-coded value fields. Similar to
a traffic light system, the colors of the fields provide
real-time feedback on the preset range of the vital
parameters, which are determined by the physician or
therapist. For example, the value field for heart rate
turns red if the heart rate rises above an individually
defined limit.
Quantified Health: A Feasibility Study on a Sensor-Based Feedback and Assistance System in Cardiology, Oncology and Orthopaedics
629

The training plan that the patient has agreed with
their doctor provides an overview of the goals that
have been set. The patient can switch between
everyday and training mode. There are 4 different
training categories available in the training mode:
Running, cycling, ergometer and an individual
training plan with various gymnastics exercises.
Training explanations also show statistics and
progress in relation to the current training plan.
Various vital and movement parameters are also
recorded in training mode, such as the number of
steps, distance covered and heart rate. The users can
describe their current condition in the diary. There is
also the option of rating the current mood on a scale
of 1 to 10 in the event of sudden indisposition. If
required, the current location (e.g., at home or at
work), the feeling of stress and specific symptoms are
also queried.
For simple and direct communication, e.g., if
doctors and therapists have noticed a health risk or
persistent stress, the app provides a bilateral
communication option in form of video conferencing.
3.2 Therapy-Application
The therapy application for doctors and therapists is a
tool with a graphical interface that medicals can use
to create and edit health data records for patients
(Patient Management System - PMS). These data
records contain information about patients (socio-
demographic data, medical history) and training plans
(e.g., recommendations for the number of steps). The
healthcare professional can set individual load limits
for everyday and training modes (e.g., individual
heart rate limit). In addition, training results and
relevant vital and activity data are graphically
processed and aggregated in the therapy application
so that the attending physician/therapist can identify
any trends in the patient's state of health. For example,
the average stride length and speed when running and
cycling are determined from the movement data of
the training mode. The training results and therapy-
relevant data stored in the system can also be used to
adapt individual therapy plans as part of a suggestion
system.
3.3 Quantified Health-Backend
The Quantified Health-Server stores all data of the
telemedical therapy and training system, i.e.,
participating patients, therapists, therapy plans and
training results. It is also responsible for the
synchronization and persistent storage of data from
all subsystems involved (mobile systems, therapy
application). The data collected and stored in the
project context are master data, health data and
identification data. These data are subject to special
protection requirements and are safeguarded by state-
of-the-art technical and organizational measures in
accordance with the GDPR.
4 MATERIALS & METHODS
The aim of the "Quantified Health" project was to
pilot and evaluate a complex, digitally supported
intervention from a user perspective in three medical
facilities across different diseases and sectors of the
german health care system. The use of a mobile
sensor-based assistance system was tested, which
accompanies patients with cardiological, orthopaedic
and oncological diseases in their everyday life as part
of follow-up treatment or aftercare.
Physiological deficits were determined and based
on sensory data, everyday stress situations were
analysed in real-time under medically and
therapeutically defined aspects and the patients
obtained immediate feedback on their state of health.
The medical staff was involved by receiving vital and
movement data from patients and by providing
feedback (e.g., manual modifications of activity
recommendations by the doctor and therapist
providing care) to the patients. This should help the
patient to manage better their health condition and
experience greater economy under physiological
load.
The 56 patients were recruited in the 3 facilities in
different ways (e.g. by direct communication, by a
displayed presentation explaining the study objective
and procedure installed on the practice TV screen in
waiting room), but based on similar inclusion and
exclusion criteria:
• Resilience according to the health status (e.g.
oncology: no metastases, orthopaedics: no
acute ischialgia, cardiology: no unstable
cardiac arrhythmia)
• Compliance required for physical activity (e.g.
extracardiac comorbidities or orthopaedic
limitations)
• Necessary affinity for technology (suitable
mobile device, available e-mail address,
digital questionnaires)
In all three facilities, separate appointments were
made with the patients for patient information and
education, data protection information, declaration of
consent, technical training and the creation of patient
data.
HEALTHINF 2024 - 17th International Conference on Health Informatics
630
For the data collection, patients were provided
with a smartwatch with sensors for measuring vital
and movement parameters for a period of 3-5 months.
As the data is particularly sensitive data under the
GDPR, appropriate technical and organizational
measures were implemented to protect the data. The
basis for data processing on the side of the patients
was based on a consent. In accordance with the
principle of data minimization, data was only
collected for the purpose of treatment within the study
and evaluated pseudonymously. Data transmission
was encrypted in accordance with current security
standards. All ethical and regulatory requirements
were safeguarded by obtaining an ethics vote. The
study was also published in the German Clinical
Trials Register.
The vital and movement parameters were
evaluated at a total of four measurement points (upon
enrolment (implementation and baseline), on
transition from supervision by the medical institution
to sole responsibility (approximately 4 weeks after
enrolment), 13 weeks after enrolment (end of the
intervention period), optional follow-up 21 weeks
after enrolment) and the subjective evaluation of the
tool was recorded in questionnaires.
The analyses included data from training sessions
that took at least 600 seconds (Bull et al., 2020) and
were within the time frame of enrolment (t0) to 13
weeks after enrolment (t2). Training sessions between
t2 and t3, as well as training sessions lasting 300-600
seconds, were considered separately. Trainings after
t3 and with a duration of less than 300 seconds were
not considered.
In addition to standardized socio-demographic
questions, validated scales were used as
questionnaires (Van der Laan et al., 1997),
(Venkatesh et al., 2003), (Davis et al., 1989), (Borg,
1998), (Bullinger, 1995), (Neyer et al., 2012),
(Stoyanov et al., 2016), (Parmanto et al., 2016). In
parallel, guided, semi-structured interviews were
conducted with two practitioners from each of the
three different medical facilities to obtain an
assessment of the system's everyday viability on the
side of the care providers.
The evaluation concept therefore used elements
from process-oriented formative evaluation research
(qualitative interviews) and effectiveness-oriented
summative evaluation research (quantitative app and
questionnaire data), which together assessed the
progress and feasibility of the Quantified Health
application.
5 RESULTS
The results presented below are based on data
recorded by the system. This necessarily represents a
reduced section of reality. It does not include, for
example, training units and steps that were completed
without using the system or training units that were
carried out with the system but were insufficiently
synchronized and transmitted.
A total of 56 people took part in the feasibility
study. They were on average 46 years old (SD = 16.58
years); 55% were female. Table 1 shows the socio-
demographic characteristics of the participants at the
three facilities.
Table 1: Socio-demographic characteristics of the study
sample by institution.
Total Onco. Cardio. Ortho.
N 56 21 18 17
Age (M, SD)
46.45
(16.58)
38.29
(10.39)
58.56
(14.22)
43.35
(18.23)
Gender (fem.)
55%
76%
33% 53%
BMI (M, SD)
26.40
(4.64)
26.05
(4.44)
26.03
(4.19)
27.28
(5.49)
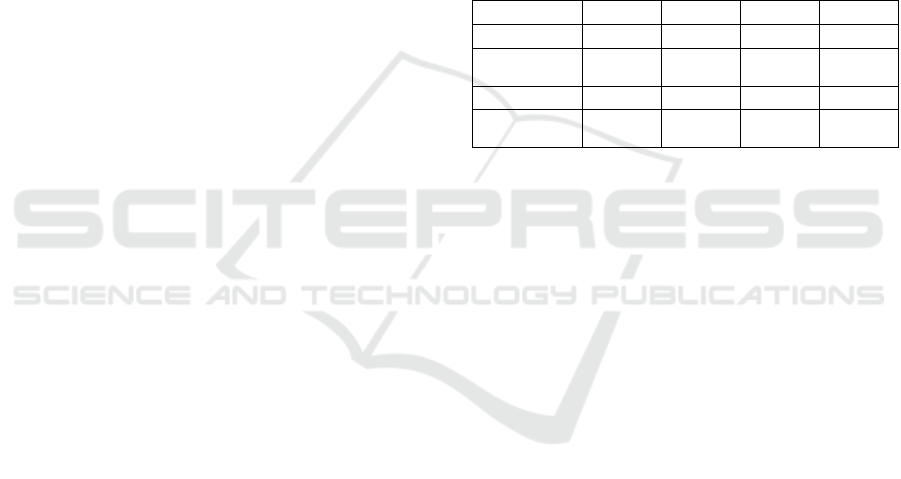
5.1 Training Frequency
A total of 1053 training sessions with a duration of
≥600 seconds were recorded for the 56 participants
over a period of 13 weeks. This corresponds to an
average training frequency of M = 1.45 training
sessions (SD = 2.33) per week. There were two
outliers with 8.23 and 13.38 training sessions per
week. No training was documented for eight
participants. Excluding these ten patients resulted in
an average weekly documented number of training
sessions of M = 1.29 (SD = 1.43). The average
training frequency of all participants varied
depending on the time point and showed a decreasing
trend with increasing duration of participation. The
training frequency in the first weeks of participation
was thus significantly higher than the training
frequency at the end of the intervention period. Figure
2 shows the progression of the training sessions over
time.
5.2 Feasibility - Dropout
For eight of the 56 participants, no training was
documented (14%). Beyond that, for 17 people
(30%), no training was recorded from week 5 no
onwards; after two thirds of the time (8 weeks),
Quantified Health: A Feasibility Study on a Sensor-Based Feedback and Assistance System in Cardiology, Oncology and Orthopaedics
631
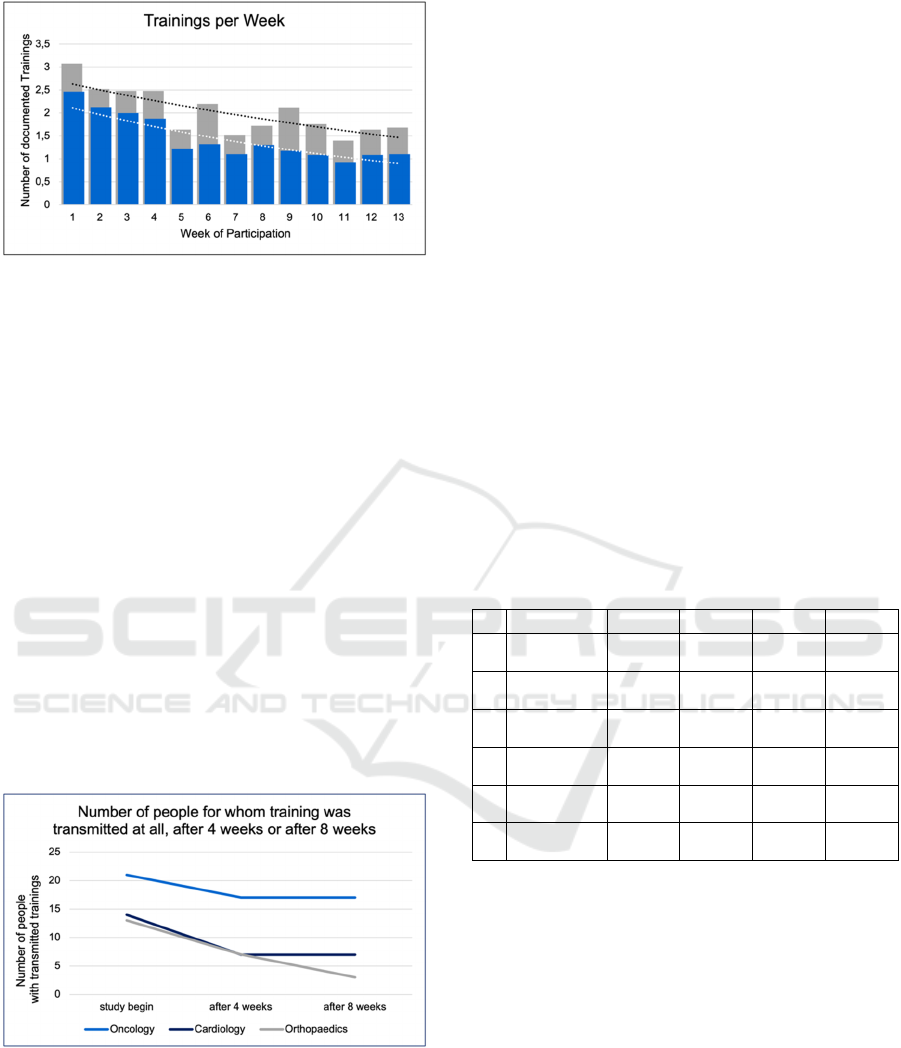
Figure 2: Number of documented weekly training sessions
over the 13-week intervention period. The blue bars show
the unadjusted data of all participants (n=56) incl. dropouts
and outliers. The gray bars show adjusted data of
participants who trained continuously (n=25) excluding
dropouts and outliers. The training target of two training
sessions per week was mainly achieved in the first weeks of
participation.
training was recorded for a further four people (7%).
This left 27 people (48%) whose training sessions
were recorded by the system after 8 weeks. Looking
only at those participants for whom training sessions
were recorded up to the end of the 13-week period (n
= 25), the training frequency was at the targeted level
(M = 2.01; SD = 1.59).; meaning just under half of
the participants completed training sessions over the
longest period of the project. Dropout rates of up to
30-50% are not uncommon in feasibility studies
(Fjeldsoe et al., 2010 & Pfaudler et al., 2015). Figure
3 shows the remaining patients since the beginning,
after 4 weeks and after 8 weeks, broken down by
indications.
Figure 3: Number of people for whom training sessions
were documented up to 4 weeks, for whom training sessions
were documented after 4 weeks of participation and for
whom training sessions were still documented after 8 weeks
of participation.
5.3 Therapy Success
Health-related well-being was measured using the
SF-36 with the subscales physical health and mental
health (Bullinger, 1995). A total of 49 participants
submitted at least one questionnaire; 12 participants
responded at one measurement time point, 23
participants responded at two measurement time
points and 14 participants responded at each of the
three measurement time points. Table 2 shows the
mean values of the two subscales physical and mental
health for the three institutions at the three
measurement points. The corresponding mixed
models show a good model fit for physical health
(ICC1 = .76) and mental health (ICC1 = .53). In both
cases, the initial values of the participants vary
significantly (physical: t(67) = 26.37, p < .001;
mental: t(82) = 27.22, p < .001). Both physical health
(t(55) = 2.58, p = .013) and mental health (t(60) =
2.01, p = .049) increased over time, similar to the
individual findings of other studies on the use of
telerehabilitation for specific indications (Jaswal et
al., 2023; Eichler et al., 2019).
Table 2: Mean value of physical and psychological well-
being by measurement time and therapeutic facilities.
Total Onco. Cardio. Ortho.
t
0
Physical
(N)
41.27
(34)
42.90
(15)
37.18
(11)
43.83
(8)
t
1
Physical
(N)
45.21
(34)
49.72
(13)
42.50
(12)
42.28
(9)
t
2
Physical
(N)
45.96
(32)
46.99
(15)
45.35
(11)
44.49
(6)
t
0
Psychological
(N)
44.80
(34)
43.38
(15)
47.35
(11)
43.98
(8)
t
1
Psychological
(N)
47.49
(34)
43.35
(13)
51.79
(12)
47.74
(9)
t
2
Psychological
(N)
48.68
(32)
49.58
(15)
48.58
(11)
46.64
(6)
5.4 Subjective Assessment of the
Patients
After Van der Laan et al., 1997 usefulness and
satisfaction can describe tendencies of acceptance
and rejection on a cognitive and emotional level.
Figure 4 provides information on the ratings
according to medical indication in the value spectrum
-2 (low acceptance) to +2 (high acceptance). Both
dimensions are in the positive range of the scale. The
system was therefore rated as useful and satisfactory
and confirms the findings of Algarni et al., 2022
regarding the positive perception of telemedicine
treatments by patients. Usefulness was more
pronounced than satisfaction across all indications.
Between t1 and t2, the cardiology participants rated
HEALTHINF 2024 - 17th International Conference on Health Informatics
632
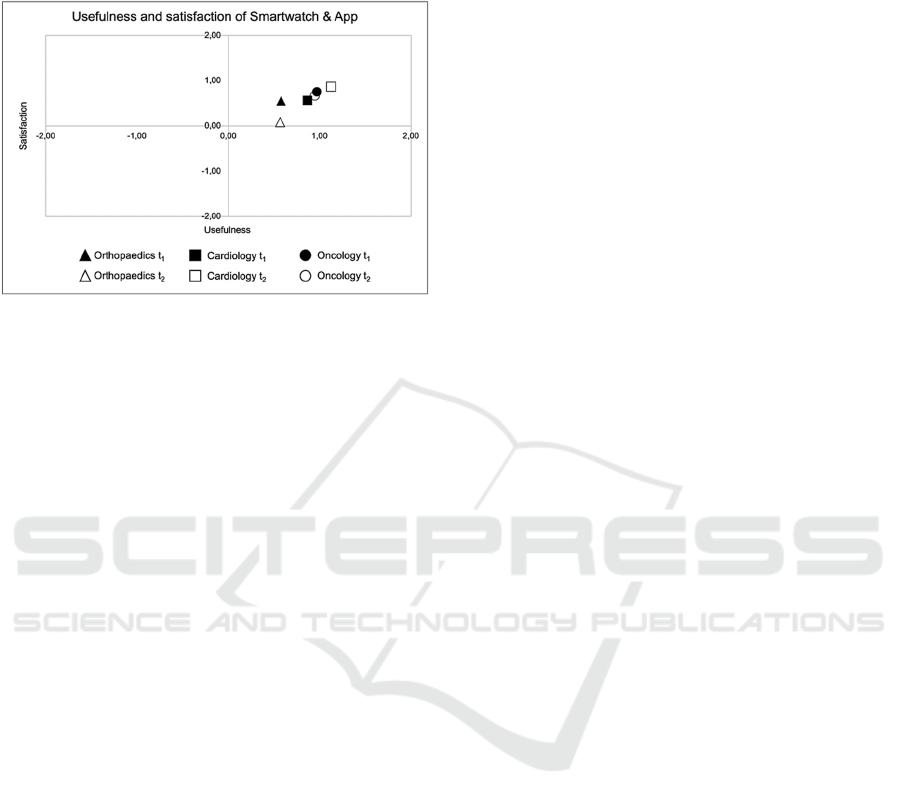
the system as more useful. Satisfaction increased in
cardiology but decreased in oncology and
orthopaedics.
Figure 4: Evaluation of usefulness and satisfaction at t1
(N=34) and t2 (N=32) by medical institution. The scale
ranges from -2 (low usefulness/satisfaction) to +2 (high
usefulness/satisfaction).
Another measure of usefulness in the value range 1
(low usefulness) to 5 (high usefulness) coupled with
usability (Venkatesh et al., 2003 & Davis et al., 1989)
produced a similar picture with positively assessed
usefulness. Usability was rated higher than usefulness
across all medical institutions. Effects between t1 and
t2 were negligible.
Of all questionnaire participants at t1 (N=34),
those who also completed the questionnaire at t2
(N=22) evaluated the system as more useful than
those who did not complete the t2 questionnaire
(N=12) (M = 1.02 vs. M = 0.48; t(32) = 2.08, p = .046
and M = 3.59 vs. M = 2.93; t(32) = 2.60, p = .014).
There were no significant differences between the
two groups in terms of satisfaction and usability.
5.5 Perspective of the Care Providers
The six interviews with the supervising therapists
(two in each medical institution), were used to discuss
(1) the care context (2) the expectations of and
towards patients and conflicts, (3) technologies in
everyday working life, (4) the introduction, everyday
use and evaluation of the quantified health system and
(5) the potential of digital care in the respective
rehabilitation setting. These results were described in
the evaluation report (Zöllick, 2023) and are
summarized below.
In an initial step, the patients' expectations were
compared with the services provided by the facility.
The summary of statements of medical care providers
involved in the project reflects the complex treatment
situation of lifestyle-changing therapy measures.
All participating therapeutic facilities use a
variety of technical devices in their daily work for
therapy and administration. Examples include digital
patient files, video calls as a method for consulting,
tablets and VR glasses. At the same time, therapists
emphasized the importance of the therapeutic hand as
an important tool. In addition to the benefits for
patients, the most important criterion for the use of
technology was emphasized as making work easier
for medical staff (Zöllick, 2023, p.17).
Therapists generally consider the easy usage and
operability as well as the reliability of the collected
data to be central to the acceptance of additional IT
systems in everyday treatment. These are the basic
prerequisites for therapists to provide patients with
valid feedback (Zöllick, 2023, p. 17f.), similar to the
findings of Wang et al., 2023 that the reliability of
data also plays a significant role in the acceptance of
telemedicine on the part of patients. Particularly
regarding the reliability of the data in the Quantified
Health system further potential for improvement has
been noted. Due to data protection requirements, the
project also involved duplication with other existing
IT systems, which required additional time. For
instance, the facility's own documentation system had
to be maintained in addition to the Quantified Health
PMS. Nevertheless, the advantages of the Quantified
Health PMS were emphasized as an additional source
of information and the possibility of monitoring and
closer interaction with patients (Zöllick, 2023, p.18).
The different expectations and approaches of
patients were identified as a potential source of
conflict with regard to their therapy and recovery
process. On the one side they range from the idea that
a massage works miracles, relieves pain and that a
certain amount of healing will occur over time with
the help of medication, up to those patients who want
to be informed precisely about their status and their
healing prognosis on the other side. The treatment
approach to patients must therefore be individualized
and sometimes insistent. From the perspective of care
givers patients are expected to be motivated to
participate and to reflect on how their own lifestyle
contributes to health problems (Zöllick, 2023, p.16).
Conflicts therefore arise on the one hand at the level
of patients' false expectations, which often result in a
lack of adherence. For some patients, retirement
requests can also prevent an active attitude towards
the rehabilitative measures (Zöllick, 2023, p.17).
These different expectations of the patient's
individual recovery process have an impact on
adherence: while adherence to treatment can still be
effectively ensured in an inpatient facility due to the
strict treatment plan, this appears to be much more
Quantified Health: A Feasibility Study on a Sensor-Based Feedback and Assistance System in Cardiology, Oncology and Orthopaedics
633

difficult for less adherent patients in an outpatient
setting. The therapists' limited personnel resources
also complicate the scheduling of appointments and
thus the flexible and intensive continuation of
therapeutic measures (Zöllick, 2023, p.17).
Nevertheless, checking the effectiveness of
training and therapy appears to be a motivator for
therapists when using additional, data-based therapy
systems, as the data can also be used to better explain
their effective training areas to patients (Zöllick,
2023, p.19). The future of digitalization in therapeutic
care is seen in the integration of different digital
documentation systems. From the therapists'
perspective, it would be desirable for all data, from
patient administration and service provision
documentation to the patients' medical parameters, to
be integrated into one system. Such a reliable,
integrated database would potentially reduce visits to
the doctor and facilitate therapeutic work. It would
also enable the transition between the inpatient and
outpatient sectors and between medical and
therapeutic therapy measures. Such a system also
offers potential for new healthcare professions, e.g.,
digitally supported prevention and rehabilitation
(Zöllick, 2023, p. 20).
6 DISCUSSIONS
Based on the results of the previous chapter, the
research questions initially posed in the project are
discussed below and lessons learned and
recommendations for action are derived from them.
The piloting of the Quantified Health system
corresponds to a feasibility study and was intended to
answer the question to which extent a telemedical
assistance systems can be used across indications and
sectors. Therefore, the added value and barriers,
particularly for patients but also for the care providers
involved, were examined. As mentioned above the
lessons learned described below are based on the
preparation for and discussions during the final event
at Fraunhofer FOKUS as well as the feasibility
evaluation by Charité Universitätsmedizin Berlin.
6.1 Different System Usage According
to Health Care Sector and
Professional Groups
Based on the feedback from the care providers
involved and the accompanying evaluation study, one
generic telemedical assistance and care systems can
generally be used across different indications.
For instance, in the outpatient sector, telemedical
assistance and care systems can be used primarily for
preventive purposes and to support therapy. Medical
professionals gain a deeper insight into the patient's
state of health and activities based on everyday and
training data. Based on these data they can adapt
therapy measures accordingly. Patients are more
strongly motivated (positive pressure) to exercise
adequately, i.e., sufficiently and in a controlled
manner. They gain additional therapy opportunities
alongside their conventional therapy.
In inpatient and rehabilitative area, telemedical
assistance and support systems can be especially used
in aftercare. This ensures regular contact between
therapists and patients, which contributes to the
sustainability of inpatient therapy measures. Since
aftercare does not necessarily have to be provided
following an inpatient stay, such systems can help to
close this gap.
The application of the system across different
sectors also showed that inpatient care represents a
good entry point for the use of such systems, as there
is longer-term contact with patients on site and
therefore more time for recruitment and referral to the
system. When care providers use the system, it should
be noted that different professional groups (sports
therapist, physiotherapist, doctor, study nurse) may
use the underlying system differently: Sports
physicians and sports scientists focus more on
training planning and training control,
physiotherapists pay close attention to the quality of
exercise execution, cardiologists primarily focus on
monitoring of vital signs.
6.2 Configurability for the Indications
Is Required
Nevertheless, the various application contexts in the
Quantified Health project, different needs of the
addressed indications (orthopedics, oncology,
cardiology) or sections (outpatient practices, inpatient
facilities) result in the need of different configuration
of data types and system functionalities. For example,
activity data (e.g., steps) and certain vital signs such
as pulse are required for all indications. However,
special values such as weight or the Borgscale
(current feeling of exertion) are used to varying
degrees in the individual indications. The same
applies to special system functionalities. For
example, everyday values are decisive in the
cardiology field, whereas the focus in the oncology
and orthopedic fields is on the training mode. In order
to keep telemedical assistance systems simple and
reduce complexity as much as possible, they should
HEALTHINF 2024 - 17th International Conference on Health Informatics
634

be configurable by the medical staff providing care
for the indication-specific use, so that certain
functions and the recording of special values can be
modularly adapted to the specific application. The
easy-to-understand aggregation of measurement and
therapy data in the form of a traffic light system, for
example, is essential for therapists and doctors.
6.3 Data Insight and Data Processing
Motivate both Patients and Care
Providers
Safety in everyday life can be restored and increased
using telemedical assistance and care systems. For a
particular group of patients, the use of telemedical
assistance and support systems increases motivation
to resume adequate physical activity. A certain self-
efficacy for the participants can be derived from this.
The patients' desire for a fine-grained insight into
their own health data and its progression (on a per-
day basis and statistically as an overview) was
established. However, it needs carefully to be
considered to which extent big volumes of available
personal health data can be meaningfully presented
on the sometimes very small displays of consumer
devices needs to be examined further. On the medical
side, optimizations of visualization (e.g., as a traffic
light system) and data aggregation can also increase
efficiency and thus make work easier for doctors and
therapists. Not every recorded health date is relevant
for the further course of treatment.
6.4 Integration or Connection to
Existing Systems Increases
Acceptance in Everyday Life
Naeemabadi et al., 2020 concluded that telemedical
assistance systems must be easy to use for patients. It
also turned out that, in addition to the desire for ease
of use and operability, there is also a need to combine
telemedical services with existing systems.
Fitness wristbands and smartwatches are often
already available in the consumer sector. Any further
additional component as a data source is less
desirable. This means that telemedical systems should
be developed in such a way that they can also
communicate with common components from the
consumer sector as a data source. On the medical side,
the various facilities already have a patient
management system (PMS). A redundant software
component for pure patient management is not
welcome, as it increases the documentation effort.
Instead, it should be possible to integrate the results
and recorded data of the additional digital health
application into the existing PMS. This means that
additional telemedical modules should be integrated
into the existing PMS via open easy-to-use interfaces.
6.5 Creation of New Jobs and
Professional Fields
The deployment and use of telemedical assistance and
feedback systems requires more attention from
physicians and therapists. This means that they
cannot be integrated into the daily workflow without
additional resources (time/staff). Telemedical
assistance and care systems contribute less to
increasing efficiency and resource optimization.
Rather, they improve the quality of therapy and
aftercare by creating added value for both patients
and healthcare professionals. Thus the use of such
systems results in additional costs for medical care. In
order to integrate telemedical therapy measures into
daily treatment routines an additional job or job
profile must be created, the so-called tele-therapist or
tele-physician. This professional position is
characterized by the fact that both technical skills and
medical expertise are required. Depending on the
indication and functionalities used in such systems
(e.g., video conferencing), psychological support
may also be required, as certain patient groups (e.g.,
oncology) not only require movement during
aftercare, but also make use of face-to-face
discussions with therapists.
During the project, it became obvious that a
private practice cannot offer digital care around the
clock. Due to the low volume of patients, it may not
be efficient in the outpatient sector to have one tele-
therapist per each care facility. In order to close this
gap in the health care system a flexible service
structure should be created, which can be provided by
a central service provider to be set up. Connected tele-
therapists or tele-physicians could support several
established medical practices via telemedicine
centers. The services offered via a center should
differentiate between a kind of on-call service (e.g.,
for the psychological care of oncological patients)
and selective support in everyday life (e.g., when
discussing therapy goals for cardiological or
orthopaedic patients).
7 CONCLUSIONS
In summary, the functions provided by the Quantified
Health system were sufficient for all indications.
Although commercially available systems (fitness
wristbands, smartwatches, PMS) also provide
Quantified Health: A Feasibility Study on a Sensor-Based Feedback and Assistance System in Cardiology, Oncology and Orthopaedics
635

separate functions, they do not yet act as an integrated
medical approved system from a technical
perspective. Regarding the target groups, however,
these functions must be weighted differently. For
example, an explicit training mode may not be
necessary in cardiology, as everyday values are
increasingly monitored during the process of
treatment. Configuration options should therefore be
integrated into the Quantified Health App or PMS in
order to adapt the system to the respective indication
and the media skills of the end user.
In principle, the acceptance of the Quantified
Health system was given among end users. Future
applications of the system are possible in the area of
prevention (e.g., to control high blood pressure), after
an acute event (e.g., in inpatient rehabilitation or
aftercare) but also for treatment of chronic diseases in
order to modulate lifestyle in everyday life. However,
a certain degree of affinity with technology was a
prerequisite for the use of the Quantified Health
system. It became clear that the large number of
functions provided can lead to users being
overwhelmed by the possible system operations.
Especially in inpatient aftercare, the additional
support in everyday life is perceived as a benefit for
patients and fills a gap in the healthcare system. The
acute event is often a starting point for lifestyle-
changing activities following inpatient treatment.
Constant contact with the doctor or therapist increases
the patient's motivation. In the outpatient setting,
especially for chronic patients, this process is much
more protracted and sometimes problematic, because
behavior patterns that have been practiced over long
term have to be changed.
The project also revealed that an additional digital
system would be difficult to integrate into existing
workflows under the current working conditions.
New tele-workstations for tele-doctors and tele-
therapists should be created here. The care providers
were consistently positive about the fact that they
would receive more data from patients' everyday lives
and that the improved data situation could also
provide motivation for the sustainable care of
patients.
Integrated solutions with well-bridged interfaces
in particular allow medical care providers and
patients to supplement prevention and rehabilitation
measures and therefore have considerable social and
economic potential. The project results of Quantified
Health can be used to develop a reference architecture
(description of the technical components and process
recommendations) for digital aftercare in everyday
life for the indications of cardiology, oncology and
orthopedics. Initial concepts for a standardized, cross-
indication open telehealth platform already exist.
In order to be able to define business models, the
next step would be to determine not only the targeted,
medical examination of effectiveness but also the
economic efficiency. Business models can then be
derived from these results. Future work on cross-
indication teleassistance systems should therefore
focus on
• Technical adaptation and optimization in
accordance with the lessons learned and
recommendations for action,
• the audit of effectiveness and efficiency and
• the requirements for inclusion in standard care
by providing an accounting code.
ACKNOWLEDGEMENTS
This work was supported by the project DiBeA
funded by the German Federal Ministry of Health
based on a decision of the German Federal Parliament
(Bundestag) under funding ID ZMI1-2521TEL20A.
REFERENCES
Algarni, F. S., Alshammari, M. O., Sidimohammad, U.,
Khayat, S. A., Aljabbary, A., & Altowaijri, A. M.
(2022). Tele-Rehabilitation Service from the Patient's
Perspective: A Cross-Sectional Study. Journal of
Patient Experience, 9, 23743735221130820.
Borg, G. (1998). Borg's perceived exertion and pain scales.
Human kinetics.
Brick, R., Padgett, L., Jones, J., Wood, K. C., Pergolotti,
M., Marshall, T. F., ... & Lyons, K. D. (2023). The
influence of telehealth-based cancer rehabilitation
interventions on disability: a systematic review. Journal
of Cancer Survivorship, 17(6), 1725-1750.
Bull, F. C., Al-Ansari, S. S., Biddle, S., Borodulin, K.,
Buman, M. P., Cardon, G., ... & Willumsen, J. F.
(2020). World Health Organization 2020 guidelines on
physical activity and sedentary behaviour. British
journal of sports medicine, 54(24), 1451-1462.
Bullinger, M. (1995). Der deutsche SF-36 Health Survey.
Ubersetzung und psychometrische Testung eines
krankheitsubergreifenden Instruments zur Erfassung
der gesundheitsbezogenen Lebensqualitat [Translation
and psychometric testing of a questionnaire on
subjectively perceived quality of life]. Zeitschrift fur
Gesundheitswissenschaften, 3, 21-36.
Davis, F. D., Bagozzi, R. P., & Warshaw, P. R. (1989). User
acceptance of computer technology: A comparison of
two theoretical models. Management science, 35(8),
982-1003.
HEALTHINF 2024 - 17th International Conference on Health Informatics
636

Eichler, S., Salzwedel, A., Rabe, S., Mueller, S., Mayer, F.,
Wochatz, M., ... & Völler, H. (2019). The effectiveness
of telerehabilitation as a supplement to rehabilitation in
patients after total knee or hip replacement: randomized
controlled trial. JMIR rehabilitation and assistive
technologies, 6(2), e14236.
Fjeldsoe, B. S., Miller, Y. D., & Marshall, A. L. (2010).
MobileMums: a randomized controlled trial of an SMS-
based physical activity intervention. Annals of
behavioral medicine, 39(2), 101-111.
Jaswal, S., Lo, J., Sithamparanathan, G., & Nowrouzi-Kia,
B. (2023). The era of technology in healthcare: an
evaluation of telerehabilitation on patient outcomes—a
systematic review and meta-analysis protocol.
Systematic Reviews, 12(1), 1-7.
Kumazawa, N., Koyama, S., Mukaino, M., Tsuchiyama, K.,
Tatemoto, T., Tanikawa, H., ... & Tanabe, S. (2022).
Development and preliminary evaluation of a tele-
rehabilitation exercise system using computer-
generated animation. Fujita medical journal, 8(4), 114-
120.
Naeemabadi, M., Fazlali, H., Najafi, S., Dinesen, B., &
Hansen, J. (2020). Telerehabilitation for patients with
knee osteoarthritis: a focused review of technologies
and teleservices. JMIR Biomedical Engineering, 5(1),
e16991.
Neyer, F. J., Felber, J., & Gebhardt, C. (2012). Entwicklung
und validierung einer kurzskala zur erfassung von
technikbereitschaft. Diagnostica.
Omboni, S., Padwal, R. S., Alessa, T., Benczúr, B., Green,
B. B., Hubbard, I., ... & Wang, J. (2022). The
worldwide impact of telemedicine during COVID-19:
current evidence and recommendations for the future.
Connected health, 1, 7.
Parmanto, B., Lewis Jr, A. N., Graham, K. M., & Bertolet,
M. H. (2016). Development of the telehealth usability
questionnaire (TUQ). International journal of
telerehabilitation, 8(1), 3.
Pfaudler, S., Hoberg, E., & Benninghoven, D. (2015).
Internetbasierte Nachsorge für Patienten nach
multimodaler orthopädischer Rehabilitation–
Machbarkeit und Akzeptanz. Physikalische Medizin,
Rehabilitationsmedizin, Kurortmedizin, 25(02), 81-89.
Plaete, J., Crombez, G., DeSmet, A., Deveugele, M.,
Verloigne, M., & De Bourdeaudhuij, I. (2015). What do
general practitioners think about an online self-
regulation programme for health promotion? Focus
group interviews. BMC family practice, 16, 1-11.
Stoyanov, S. R., Hides, L., Kavanagh, D. J., & Wilson, H.
(2016). Development and validation of the user version
of the Mobile Application Rating Scale (uMARS).
JMIR mHealth and uHealth, 4(2), e5849.
Thimmel, R., Schubert, M., & Viehmeier, S. (2018).
Übergreifende Aspekte zum Reha-Prozess. Rehabilita-
tion: Vom Antrag bis zur Nachsorge–für Ärzte,
Psychotherapeuten und andere Gesundheitsberufe, 217-
228.
Van Der Laan, J. D., Heino, A., & De Waard, D. (1997). A
simple procedure for the assessment of acceptance of
advanced transport telematics. Transportation Research
Part C: Emerging Technologies, 5(1), 1-10.
Venkatesh, V., Morris, M. G., Davis, G. B., & Davis, F. D.
(2003). User acceptance of information technology:
Toward a unified view. MIS quarterly, 425-478.
Wang, M. Y., Chen, H., Gong, C., Peng, X. M., Zhong, Y.
B., Wu, C. M., ... & Wu, Y. Q. (2023). Understanding
the use intention and influencing factors of
telerehabilitation in people with rehabilitation needs: a
cross-sectional survey. Frontiers in Public Health, 11.
Zhong, W., Liu, R., Cheng, H., Xu, L., Wang, L., He, C., &
Wei, Q. (2023). Longer-Term Effects of Cardiac
Telerehabilitation on Patients With Coronary Artery
Disease: Systematic Review and Meta-Analysis. JMIR
mHealth and uHealth, 11, e46359.
Zöllick, J. (2023). Evaluationsbericht „Quantified Health -
Bericht über eine dreimonatige Machbarkeitsstudie zu
einem sensorbasierten Feedback- und Assistenzsystem
in drei Reha-Settings“, projektinternes Dokument, 30 S.
Quantified Health: A Feasibility Study on a Sensor-Based Feedback and Assistance System in Cardiology, Oncology and Orthopaedics
637
