
Implications and Perceptions of Digital Health Technologies:
A Multiple Case Study on the Payers’ Viewpoint
Kai Gand
1a
, Hannes Schlieter
1b
, Elena Torrente Segarra
2
and Andreea Garaiacu
3
1
Research Group Digital Health, TUD Dresden University of Technology, Dresden, Germany
2
Digital Health Development, Digital Health Innolab, DKV, Barcelona, Spain
3
National Health Insurance House, Bucharest, Romania
Keywords: Digital Health Technologies, eHealth, Case Study, Survey.
Abstract: The study delves into the implications and perceptions of Digital Health Technologies (DHT) within the
healthcare system. Among the many relevant stakeholders, the present study’s objective is to explore the
perspective of health insurers particularly. On this, we have conducted a survey (1 face-to-face interview, 5
online questionnaires) for a multiple case study on lessons from European health insurance entities from 5
countries regarding usage scenarios of DHT. Recognized for their transformative potential, DHT promises to
address demographic shifts, streamline payment processes, and enhance patient management, especially for
chronic diseases. However, the survey participants still see challenges in terms of their long-term effectiveness,
demographic and regulatory constraints. Countries like Germany have pioneered regulatory frameworks, but
issues of trust and interoperability persist. The economic implications of DHT present both potential cost
savings and financial burdens. Health insurers emerge as pivotal players, acting as gatekeepers for DHT
quality and driving adoption. As the DHT landscape evolves, continuous evaluation, adaptation, and multi-
stakeholder collaboration are paramount for harnessing their full potential.
1 INTRODUCTION
1.1 Problem Statement
The demographical development in Western
healthcare systems increases the morbidity of
patients. Particularly, non-communicable diseases
(NCDs), such as diabetes, hypertension, asthma,
depression, and anxiety, impose a substantial health
and economic burden on society (Vandenberghe &
Albrecht, 2020). To address this challenge, healthcare
delivery must rapidly shift from traditional processes
to scalable digital health technologies (DHT; (Digital
Therapeutics Alliance, 2023)). DHT (such as
technology-supported blended care, patient
monitoring, digital diagnostics, digital therapeutics)
offer the potential to improve the quality, efficiency,
and accessibility of healthcare (Chaudhry et al., 2006;
Stroetmann et al., 2010).
However, there are still significant challenges to
the sustainable and scalable implementation and
a
https://orcid.org/0000-0003-2065-8523
b
https://orcid.org/0000-0002-6513-9017
diffusion of DHT. One key challenge is developing
and implementing effective business models that can
support the long-term adoption and use of DHT
(Gand, 2017; Veit et al., 2014). Another challenge is
ensuring that DHT are accessible and reasonably
priced or affordable for all stakeholders, including
those in underserved and low-income communities
(Suter et al., 2009). The fact that there are many
different stakeholders in the healthcare system
(various healthcare providers, health insurance
companies, patients, politicians) or the importance of
managing health-related data very carefully (cf.,
implications regarding privacy and security concerns)
are major challenges for the implementation as well.
To address these challenges, the present study’s
objective is to bring together the perspectives of
payers and academics to discuss emerging business
models of DHT. Thus, the research objective is to
explore this perspective of health insurers
particularly.
Gand, K., Schlieter, H., Segarra, E. and Garaiacu, A.
Implications and Perceptions of Digital Health Technologies: A Multiple Case Study on the Payers’ Viewpoint.
DOI: 10.5220/0012401800003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 871-878
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
871
1.2 Methods
To address these open points, we have conducted a
multiple case study (Yin, 2014) on lessons learned
and perspectives from health insurance companies
regarding usage scenarios of DHT. A survey (1 as
face-to-face interview, 5 as online questionnaires) has
been used to get the respective insights. Details on the
survey modes can be found in the appendix (see Table
4). The two survey modes are equally important
sources of evidence with qualitative data for the
overall case study. The participants and the
organizations they represent constitute the partial
cases in the sense of a replication design of the overall
case study (Yin, 2014). The problem areas outlined
above are operationalized in terms of the survey with
the individual questions listed in Table 1 (Q#) and
discussed in the corresponding sections in Chapter 2.
The questions correspond to the elements of the
questionnaire and the key questions of the interview.
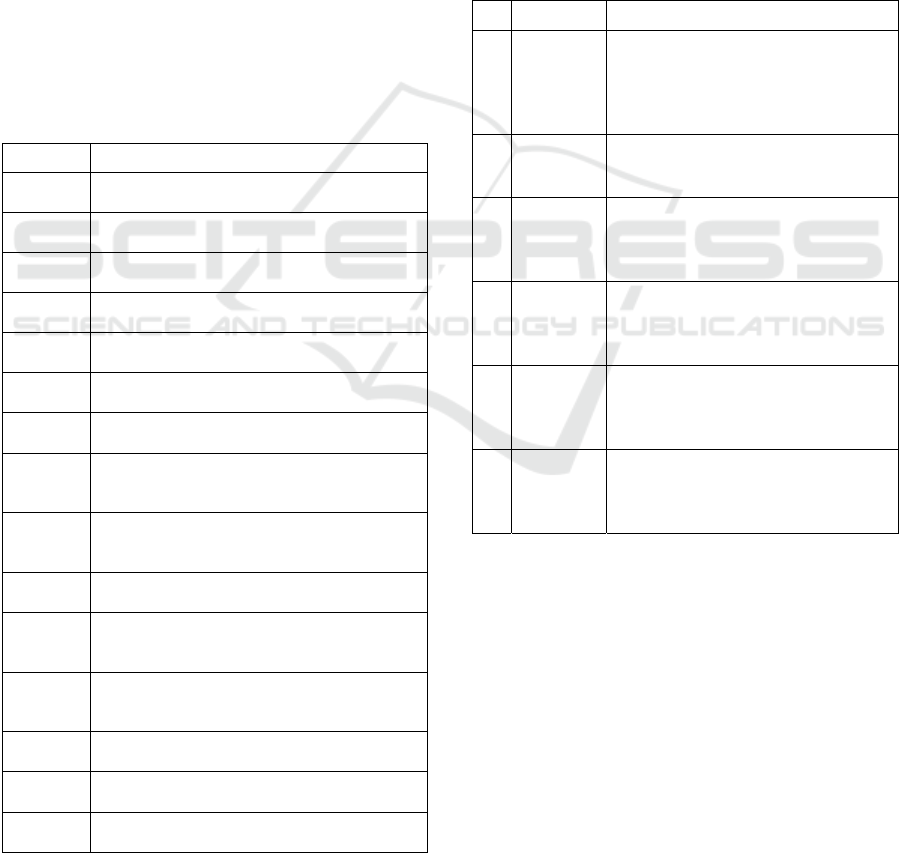
Table 1: Details on the survey elements.
No. Questions
Q1 – Sec.
2.1
How important are DHT for healthcare in
general?
Q2 – Sec.
2.1
How important are DHT from the payer's point
of view?
Q3 – Sec.
2.1
How can DHT help to make healthcare ready
for the future developments?
Q4 – Sec.
2.1
How can DHT be used for prevention, healthy
longevity, healthy aging, and elderly care?
Q5– Sec.
2.2
How to cope with the economic burden of
NCDs (with or without DHT)?
Q6 – Sec.
2.2
Which emerging business models of DHT are
p
romising?
Q7 – Sec.
2.4
What needs to change in terms of regulations to
make DHT successful?
Q8 – Sec.
2.3
Do you see a change in the role of health
insurances in the future (given the rise of DHT
or in general)?
Q9 – Sec.
2.5
Are you offering DHT? Did you develop these
DHT yourself or are you partnering with start-
ups or other companies?
Q10 – Sec.
2.5
Which DHT are already used and reimbursed?
In which fields? How are these paid for?
Q11 – Sec.
2.5
For which diseases do you think we need DHT
most? Where do you think DHT will work
b
est?
Q12 – Sec.
2.5
What is your main goal in offering these DHT?
(new revenue streams, cost-efficiency,
customer loyalty)
Q13 – Sec.
2.6
What learnings did you generate? Are there
DHT that worked better than others?
Q14 – Sec.
2.7
Could you already assess the effectiveness
and/or efficiency of DHT?
Q15 – Sec.
1.2
Details of the representatives / respondents
The Europe-wide professional network of the
authors (contacts via the membership lists of two
European associations accessible to the authors were
contacted; total number of contacted not known) was
used to look for suitable representatives of the payer
or insurer side in the healthcare system (note: given
the various healthcare systems, some with direct state
reimbursement, some with private or public health
insurers, the terms "payer" and "insurer" should be
understood interchangeably here). If the feedback
was positive, they were invited to participate in the
survey. Table 2 provides an overview of the survey
participants/analysis units of the case study.
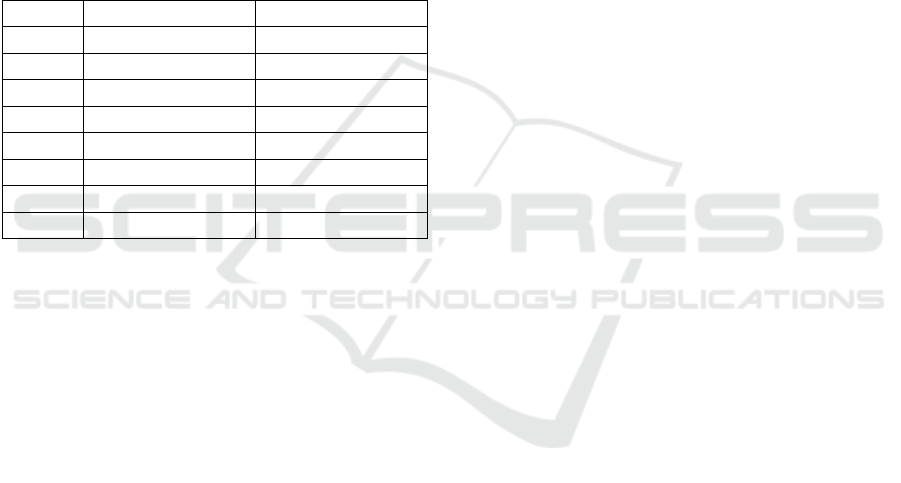
Table 2: Overview of the representatives (R#) included -
details on the analysis units of the case study.
No. Country Characteristics (pseudonymised)
R1 Hungary Central national agency for the
management of the National Health
Insurance, maintenance of records,
keeping financial accounts and
fulfilling reporting obligations
R2 The
Netherlands
Trade, interest, liaising organisation of
companies offering health insurance;
b
alances different interests in healthcare
R3 Romania Public, autonomous national
institution to ensure unitary and
coordinated functioning of the social
health insurance system
R4 Spain Private health insurance with more
than 50,000 customers that offers
access to the medicine and other
related insurance services
R5 Germany Statutory (=non-profit, for the
common good), nationally represented
health insurance with more than
500,000 insured
p
eo
p
le
R6 Germany Biggest statutory (=non-profit, for the
common good), nationally represented
health insurance with more than 11
million insured
p
eo
p
le
In principle, a larger number of participants
would have been possible by using the survey
instrument. In the context of the case study, however,
the resulting number was considered sufficient after
one follow-up reminder for the members of the
requested associations.
2 INSIGHTS ON THE USE OF
DHT
In general, we have chosen a summary perspective for
the study. In the case of special aspects of individual
Scale-IT-up 2024 - Workshop on Emerging Business Models in Digital Health
872
participants, these are reported specifically (see their
no. as displayed in Table 2). Partly, the given answers
did not fully fit the questions or if the participants
could not give an answer. When analysing the
answers, these have been partly clustered and
summarised to understand and address better the
primary study aim.
2.1 General Aspects
First, we asked the participants to rate the importance
of DHT from their point of view on a 5-point Likert
scale (Q1+Q2; see Table 3). For both, we got mostly
high ratings (meaning (very) high importance) -
putting digitisation as a cornerstone of healthcare.
Table 3: Responses for Q1 and Q2 (5-point Likert scale).
Q1 Q2
R1 4 4
R2 3 3
R3 5 5
R4 4 4
R5 4 4
Mean 4 4
Median 4 4
Mode 4 4
Further on, we requested the participants’ views
on DHT’s role in making healthcare ready for future
developments. In this regard, on the more
strategic/overarching level the participants mention a
possible reduction in the pressure on healthcare
providers, as remote access, for example, would make
it easier to implement more efficient processes and
overcome physical distance, thus reducing the overall
costs of healthcare delivery, and helping to prevent
illnesses (R1,4). Overall, DHT are associated with the
hope of being able to address larger demographic
changes, such as the lowering number of workers.
Operationally, payment processes and access (also to
medical) information could be facilitated, expensive
duplicate examinations could be avoided with
digitally available data (imaging procedures are
particularly expensive in this regard and could often
be easily reduced in number, which would also reduce
radiation exposure). DHT could also help patients
manage their chronic diseases by offering measures
to monitor relevant vital parameters, help establish
changes and offer support in everyday life (R1-6). It
is important to stress that these effects can only be
attained if the DHT offer a real benefit for patients
and medical staff and are used on a voluntary basis
(R5).
2.2 Economic Perspective
DHT help the payers to have very actual statistics
regarding the situation of all diseases and can make
optimised distributions of payments on that basis
(R3). On the other side, by creating consciousness of
how behaviour affects patients' disease, the economic
burden that comes with it could be alleviated. This is
achieved through earlier treatment or the avoidance
of the illness or deterioration due to a behaviour that
is better suited to one's own condition. DHT can, at
least in principle, offer the potential to provide more
constant support than is possible, for example,
through occasional visits to the doctor (R2,5,6).
The best way to cope with NCDs would be to
prevent them. With regards to the demographic
change, it would need a prompt major change in
individual behaviour of people and the circumstances
they live in, to nudge a healthier lifestyle. But with
regards to the ageing population, there also needs to
be an investment in secondary and tertiary
prevention, meaning that these diseases can be
detected at an early stage and empower patients with
NCDs to manage their disease. DHT could be
respective means and, in this sense, investments. If
these investments get reimbursed by a healthier
population is, however, uncertain (R5).
In addition to investments, business models
should also be considered as part of the advantages,
compensation, or benefits of these investments
(Mettler, 2016). However, scaling DHT also
generates additional costs. It may also not be clear
how or to what extent these additional costs can be
offset. Partly, the insurers' budgets are relatively
rigid. It is also questionable whether the healthcare
providers will be willing to pass on the efficiency
gains associated with digitalisation (cost shift away
from personnel towards infrastructure) or to accept a
corresponding change in budget structures. On the
other hand, to realise the benefits, it would also be
necessary to consider how patients or users of DHT
could be more effectively incentivised. Direct cash
benefits are sometimes difficult. If necessary,
agreements in the pharmaceutical sector would also
be conceivable. This would allow to control better
that less expensive but still effective drugs are used.
On a small scale, some existing prevention or bonus
programmes already have incentive mechanisms
(small payments or monetary-like benefits), which
might be expandable. Such mechanisms might then
also go hand in hand with a changed relationship
between the insured and the insurance in the direction
of a stronger companionship (R6).
Implications and Perceptions of Digital Health Technologies: A Multiple Case Study on the Payers’ Viewpoint
873

2.3 Potential Shift of the Role of Health
Insurers
There is a growing interest of health insurances in the
DHT market, and adoption models are being
considered to a greater extent. The participants see a
shift towards putting more pressure to adopt proven
DHT in healthcare through their purchasing power
(R1,2). Also, there is a shift towards more
preventative care and shared decision-making. It will
become more and more important that health
insurances guarantee the quality of the healthcare
system by only reimbursing DHT and other means
that have proven their positive effect. Health
insurances will be some kind of gatekeeper for high-
quality healthcare (R5). Also, they should act as a
gatekeeper and driver for using data. As particularly
highlighted in the case of Germany (R5,6; probably
true also for others), since a lot of valuable data is
stored on the statutory health insurance’s side, it
might or should be their future role to use this data to
improve healthcare. This data can be analysed on an
individual level (e.g., to find risk factors for serious
health threads) or on an aggregated level (allowing
population risk factor analyses). Data will also
be/need to be made available through the EHDS
(European Commission, 2023a), even increasing the
need for effective digitisation.
An interesting approach could also be that
patients or insured persons are more strongly guided
through the still complicated processes of the
healthcare system (where he/she must go, which steps
are pending) by DHT on the insurer side. Also, a kind
of pre-analysis of symptoms plus greater use of video
consultations could be possible to speed up processes
and enable control with increasingly limited
resources. As another example, it would be
interesting if the data of the healthcare service
providers were directly available to the health
insurance funds. A quick pre-check based on the
planned treatment would be conceivable in this way
(the concrete design for compatibility with the GDPR
remains to be seen). A second opinion could be
offered to be able to provide more information about
a cost-intensive and possibly risky treatment. The
autonomy of the individual would and should, thus,
be strengthened by the support of DHT. Digitalisation
could thus be seen as an opportunity to guide and
direct more, which hardly ever happens today. This
would result in an approach of hybrid treatment or
blended care (R6). Additional restrictions on the part
of the Medical Device Regulation (MDR; (European
Commission, 2023b)) could then also have to be
considered.
2.4 Regulations
First, broad access to DHT is important so that no user
(both on the patient and healthcare provider side) is
excluded (R1). This also touches on issues of
interoperability and usability of DHT (Katehakis &
Kouroubali, 2019). To achieve a uniform solution that
does not distort competition, pan-European
regulation is desirable. The direction currently being
taken by the legislator, including better use of (health)
data, is certainly conducive to a better basis and
ultimately also acceptance of DHT (R6; see, for
example, the recent European Data Governance Act
(European Commission, 2023c)).
For the case of Germany (R5,6), the situation is a
bit special as the country pioneered the field of DHT
(formally called “DiGA” - German abbreviation for
Digital Health Application) by making them
reimbursable by the statutory healthcare system back
in 2020 (Federal Institute for Drugs and Medical
Devices, 2023a). So, it is not the regulation that is
holding back the success of DHT, but rather a lack of
trust and fear of transparency of some stakeholders.
Interoperability challenges also remain. For example,
no data-side connection is currently possible between
DiGAs and the official electronic health record. Also,
specifications for data interfaces are not yet binding
or clear enough so that DHT solutions can always
function similarly. However, a basic framework
would be sufficient. Detailed regulations and the
concrete design could certainly be left to the
individual actors avoiding overregulation (R6).
2.5 Reasons and Modes to Offer DHT
There may be a general positive opinion about DHT.
But offering or even developing DHT is another
matter. R1 has no offer here now. For R2, at least
some healthcare insurers offer various DHT in
various fields. These are mostly offered through
third-party developers - not developed in-house.
Payment also ranges from self-pay to basic insurances
to private additional insurance. Also for R4, there are
DHT offered - both in-house developments and in
partnerships with external companies. In general,
telemedicine is a common offering nowadays.
Payment models vary without a common policy.
Overall, the participants have only limited
capacity to act as providers or developers of DHT
themselves. Therefore, they are also dependent on
what software providers offer and can only partially
control which areas and diseases DHT focus on (R1).
Selectability is partly seen as a non-existent luxury,
Scale-IT-up 2024 - Workshop on Emerging Business Models in Digital Health
874

as the transformation agendas towards digitalisation
are still in the conception phase (R2).
As primary goals for using DHT, the participants
name enabling patient access, cost efficiency (R1-5),
maintaining quality and affordability of care and the
healthcare system. In fact, the system can only be
maintained if innovative solutions such as DHT are
used (R2,5). Also, DHT can increase the loyalty of
customers/insured people, improve the system on the
technical part and add more services, cover more
diseases (R3,4). It should also be noted that even large
to very large insurers may not necessarily have a
target group that matches the demographic and
population characteristics of the overall population.
For example, if younger people and families are the
target group, the focus may be more on DHT for
pregnant women (R6).
In general, a particular need for DHT is seen
mostly in the field of management of chronic diseases
(R4,5). Monitoring the health status (with various
means) would also be a reasonable area DHT can
contribute easily (R2,4,5). On that basis, patients may
establish changes in everyday life to become healthier
(R5). Also for R3, the available DHT are offered
rather in the management of diseases. DHT can also
offer good added value, especially around
psychological support, or mental illness. Here it is
particularly important that help is found at an early
stage and at a very low threshold. Shame and social
acceptance are still problematic with mental issues.
The anonymity of DHT (compared to face-to-face
therapy) could be particularly advantageous in this
sense (given that mental health issues are still often
shameful). Simple but very effective analogue means
such as diaries and daily or nutritional advice are also
very easy to transfer and make available in DHT (R6).
DHT also make it easier to deal with cases that are
still difficult today in general, such as the coverage of
(rarer) foreign languages or also the connection of
remote (foreign-language or very specialised)
doctors. Precision and clarity (not only but also
linguistically) are essential (R6). Health insurances
need (and want) to ensure high-quality healthcare as
some kind of gatekeeper to ensure an efficient and
effective use of means (R5).
For Germany (R5,6), the situation is again a bit
special. The statutory health insurances must fully
reimburse the DiGAs, which are listed by the Federal
Institute for Drugs and Medical Devices (German
abbreviation: BfArM) and prescribed by a physician
to a patient (with no additional costs for them).
Furthermore, the health insurances can reimburse
DHT, which are not (yet) part of this list, via special
contracts and offer DHT of their own (choice). In this
case, the data flow can also be controlled much more
easily, user statistics are available. Due to the
complicated legal situation of the public health
insurance funds in Germany, only a few participate
directly in developers but rather buy or license the
DHT from external providers (R6).
Regarding focus, the DHT listed by BfArM are
mostly for the management of diseases, and only a
few are for prevention. The role of the gatekeeper for
quality results from the fact that offers from the health
insurance funds are either checked via the BfArM
procedure or come into reimbursement via selective
contracts and thus become attractive for patients
because they receive the offers on prescription.
Google and Co. are (so far) pushing into the second
healthcare market, where offers are paid for
themselves, and these are not officially checked (also
with a view to data protection). However, there is a
limit here (in the German market) with "lifestyle"
offers because these are generally not reimbursed by
the statutory health insurance (R5).
There was the further comment that electronic
patient records should also be counted as DHT and
very important ones at that. Especially from the
insurers' point of view, there is a great added value
here, as significantly better data availability goes
along with it. In Germany, in particular, the records
have a somewhat difficult public image, but their use
is increasing.
2.6 General Learnings
From the participants' experiences with the offer of
DHT, some generalisable experiences emerge. For
example, clinical validation or proof of benefit is
considered central. However, this is difficult to
achieve, especially for software development start-
ups (as service providers), partly because they lack
experience. So, also the buying/licensing side
somehow stays with this kind of uncertainty. It is
crucial that a good, clear use case/minimal viable
product is defined so that everyone knows what
benefit the DHT can provide or address (R4). Also,
there are already some insights on the distinct use of
DHT (R5): These are mostly used by women. As
already mentioned, DHT are usually developed for
one specific disease, which does not necessarily
reflect the full needs of the patients. That could be
problematic for those who suffer from further
diseases (co-morbidities). Patients often do not
complete the whole recommended treatment cycle.
This, in turn, reduces the overall added value of
implementing DHT.
Implications and Perceptions of Digital Health Technologies: A Multiple Case Study on the Payers’ Viewpoint
875

It is also interesting that the obvious group of
presumed digital affine people (<40 years) are partly
not so much in the focus on the use or offer of DHT
(apart from more specific target groups such as
pregnant women). This group is simply less affected
by diseases, so the benefit expectation in relation to
DHT is lower. Thus, it is rather the 40–60-year-olds
where the need for support through DHT is greater or
content for filling the electronic health record is
available because there is already a certain medical
history. In the meantime, a certain digital competence
is also available. Nevertheless, the digitally more
affine society is growing, so that user-side limitations
will certainly decrease in the future (R6; (United
Nations Economic Commission for Europe, 2021)).
If there is a failure of DHT (or their lack of
sustainable use or upscaling), this can have further
causes. A DHT may have been developed for a very,
probably too specific purpose. In such cases, the DHT
was not able to cope with the complexity of the
overall system in real-life use, or its overall added
value was too low, and it could not be cost-effective
(R2,5). The situation is similar if the use case is
poorly designed, i.e., not very appropriate to the
needs or the healthcare system (R4). Or, in some
cases, the provisionally assumed clinical/medical
benefit does not materialise in the form of greater
practical benefit, so further use was discontinued (this
was the case, for example, with some DiGAs that
were delisted by the BfArM again; R6; (Federal
Institute for Drugs and Medical Devices, 2023b)).
2.7 Learnings Regarding Effectiveness
and Efficiency of DHT
Another kind of experience is that, so far, hardly any
statements can be made on the effectiveness and
efficiency of the use of DHT; the positive effects of
several available DHT are not finally proven, which
could be problematic (R5). They are still a too new
technology (e.g., DiGAs have only been available in
Germany since 2020), and there is not enough (long-
term) data available on the effect on individual
patients or their clinical pictures, and this effect may
only occur over a longer period or is generally not
easy to specify. The effort required for such a survey
is also considerable (R2). Nevertheless, the size of an
insurer is sometimes positively related to the
evaluability of DHT offerings. A larger user base at
least potentially facilitates evaluation because there
are likely to be more actual users in absolute terms.
This, in turn, may also have a slight advantage in
terms of attractiveness towards DHT providers, as the
insurer could more easily accompany an evaluation
(R6).
In general, prevention is a meaningful concern
where DHT can provide good and low-threshold
support so that, ultimately, patients can take better
care of themselves or their health with this additional
support (R2,6). Nevertheless, a higher burden on the
healthcare system can also arise here if the attention
of patients is increased for possibly non-critical health
aspects. All in all, the financial effects of preventive
measures or the evidence for them, at least in the short
term, is not entirely clear. But from the point of view
of care and medical science, more prevention
certainly makes sense in principle (R2,6).
Only in the case of DiGAs, it is the case that at
least an initial proof of benefit must be provided for
them to be officially listed by BfArM. However, they
can also be delisted if no effect or an undesirable
effect should occur in the longer term (R5,6).
It is true that a prescribed DiGA must also be paid
for. The success in introducing the DiGAs (there are
currently over 40 officially listed) is, on the one hand,
gratifying. However, with costs per application and
user averaging over 200 EUR, this also leads to new
financial burdens, whereas the savings effects have
yet to become apparent (potentially through
avoidance of doctor's visits and improved health in
general).
Another observed effect was that even with high-
quality DHT, a certain saturation effect occurs at
some point. If so, these solutions would have to be
improved and extended by further functionalities. Of
course, this then jeopardises cost-effectiveness and
makes it more difficult to prove usefulness due to
changed circumstances (R4).
3 CONCLUSIONS
The integration and adoption of DHT within the
healthcare landscape, especially from the perspective
of health insurers, is both promising and challenging.
The unanimous recognition of DHT's importance
underscores the potential of digitization in
revolutionizing healthcare. DHT promise to address
the challenges of an aging population, streamline
payment processes, enhance patient management,
especially for chronic diseases, and potentially reduce
healthcare costs. However, several challenges and
considerations emerge as a summary from the above:
Effectiveness and Efficiency: Despite the
potential benefits, there's a notable lack of
long-term data on the effectiveness and
Scale-IT-up 2024 - Workshop on Emerging Business Models in Digital Health
876

efficiency of DHT. While some initial benefits
are observed, the long-term impact, especially
in terms of cost savings and clinical outcomes,
remains uncertain.
Adoption and Usage: The demographic target
group for DHT is not just the younger, tech-
savvy population. Middle-aged individuals
(40-60 years) present a significant user base,
given their health needs and growing digital
competence.
Regulation and Trust: While countries like
Germany have pioneered in creating a
regulatory framework for DHT, challenges like
trust, transparency, and interoperability persist.
Overregulation is a concern, but so is the need
for a framework that ensures the safety and
efficacy of these technologies.
Economic Implications: DHT present both an
opportunity for cost savings and a potential
financial burden. The balance between these
two outcomes is yet to be determined. The role
of health insurers in this equation, especially in
terms of reimbursement models and
partnerships with DHT providers, is pivotal. It
should also be noted, however, that hardly any
new business models have emerged so far. It is
rather the case that the topic of DHT arises
extrinsically, either to be able to meet the
supply situation better or to take regulations
into account (e.g., the introduction of DiGAs).
The non-mention of new business models is
thus also a recognition that, in case of doubt,
there is still potential for change here. In part,
there is still a rather restrained adoption, a very
gradual, partly small-scale engagement with
the topic.
Role of Health Insurers: Health insurers are
poised to play a significant role as gatekeepers,
ensuring the quality of DHT and potentially
driving their adoption. Their role in data
management, especially in leveraging patient
data for improved healthcare outcomes, is also
noteworthy.
Future Directions: As the DHT landscape
evolves, continuous evaluation and adaptation
are crucial. Technologies that fail to deliver
tangible benefits might need to be phased out
or improved. Furthermore, as the DHT
landscape becomes more saturated,
innovations will need to offer added
functionalities and address specific healthcare
challenges to remain relevant.
In summary, the present case study was able to
provide some relevant, exploratory insights into the
payer side’s perspective on DHT. Figure 1 provides a
summary of the given challenges.
Figure 1: Summary of the given challenges in the field of
DHT (This figure has been designed using images from
Flaticon.com).
Here, it should also be noted, however, that the
study cohort hardly showed any (national) differences
regarding the above-mentioned questions. There was
no major outlier in the responses, hardly any strongly
divergent opinion. On the one hand, this is due to the
relatively small size of the cohort, which, however, is
not critical in the sense of case study research. At the
same time, participation in the survey was not
controlled by the inviters (voluntary participation in
case of own interest). This resulted in a sample
distribution that was not known in advance and is
only of limited diversity. Accordingly, the potential
for future research results in a broader coverage of
more diverse aspects or healthcare systems or the
implementation of in-depth analyses for particularly
interesting aspects.
Overall, while DHT offer transformative potential
for the healthcare sector, their integration requires a
balanced approach, considering clinical outcomes,
economic implications, regulatory frameworks, and
the evolving needs of the patient population.
Collaboration among stakeholders, including health
insurers, DHT providers, regulators, and patients, will
be crucial in realizing the full potential of DHT.
Implications and Perceptions of Digital Health Technologies: A Multiple Case Study on the Payers’ Viewpoint
877
ACKNOWLEDGEMENTS
The authors would like to thank the participants of the
survey, including the ones who did not want to be
individually mentioned or included as co-author here.
REFERENCES
Chaudhry, B., Wang, J., Wu, S., Maglione, M., Mojica, W.,
Roth, E., Morton, S. C., & Shekelle, P. G. (2006).
Systematic Review: Impact of Health Information
Technology on Quality, Efficiency, and Costs of
Medical Care. Annals of Internal Medicine, 144(10),
742–752.
Digital Therapeutics Alliance. (2023). Digital Health
Technology Ecosystem Categorization. https://dtxalli
ance.org/wp-content/uploads/2023/06/DTA_FS_DHT-
Ecosystem-Categorization.pdf
European Commission. (2023a, September 27). European
Health Data Space. https://health.ec.europa.eu/ehealth-
digital-health-and-care/european-health-data-space_en
European Commission. (2023b, September 27). Medical
Devices—New regulations. https://health.ec.europa.eu/
medical-devices-new-regulations_en
European Commission. (2023c, October). Data
Governance Act explained—Shaping Europe’s digital
future. https://digital-strategy.ec.europa.eu/en/policies/
data-governance-act-explained
Federal Institute for Drugs and Medical Devices. (2023a).
BfArM - Digital Health Applications (DiGA).
https://www.bfarm.de/EN/Medical-devices/Tasks/DiG
A-and-DiPA/Digital-Health-Applications/_node.html
Federal Institute for Drugs and Medical Devices. (2023b).
DiGA Registry—List of retired applications.
https://diga.bfarm.de/de/verzeichnis?type=%5B%22ret
ired%22%5D
Gand, K. (2017). Investigating on Requirements for
Business Model Representations—The Case of
Information Technology in Healthcare. Proceedings
IEEE 19th Conference on Business Informatics, 471–
480.
Katehakis, D. G., & Kouroubali, A. (2019). A framework
for eHealth interoperability management. Journal of
Strategic Innovation and Sustainability, 14(5), 51–61.
Mettler, T. (2016). Anticipating mismatches of HIT
investments: Developing a viability-fit model for e-
health services. International Journal of Medical
Informatics, 85(1), 104–115.
Stroetmann, K. A., Kubitschke, L., Robinson, S.,
Stroetmann, V., Kullen, K., & McDaid, D. (2010). How
can telehealth help in the provision of integrated care?
(Health Systems and Policy Analysis - Policy Brief 13).
World Health Organization.
Suter, E., Oelke, N. D., Adair, C. E., & Armitage, G. D.
(2009). Ten Key Principles for Successful Health
Systems Integration. Healthcare Quarterly, 13(Spec
No), 16–23.
United Nations Economic Commission for Europe. (2021).
Ageing in the digital era – UNECE highlights key
actions to ensure digital inclusion of older persons.
https://unece.org/media/press/358156
Vandenberghe, D., & Albrecht, J. (2020). The financial
burden of non-communicable diseases in the European
Union: A systematic review. European Journal of
Public Health, 30(4), 833–839.
Veit, D., Clemons, E., Benlian, A., Buxmann, P., Hess, T.,
Kundisch, D., Leimeister, M., Loos, P., & Spann, M.
(2014). Business Models. Business & Information
Systems Engineering, 6(1), 45–53.
Yin, R. K. (2014). Case Study Research – Design and
Methods. Sage Publications.
APPENDIX
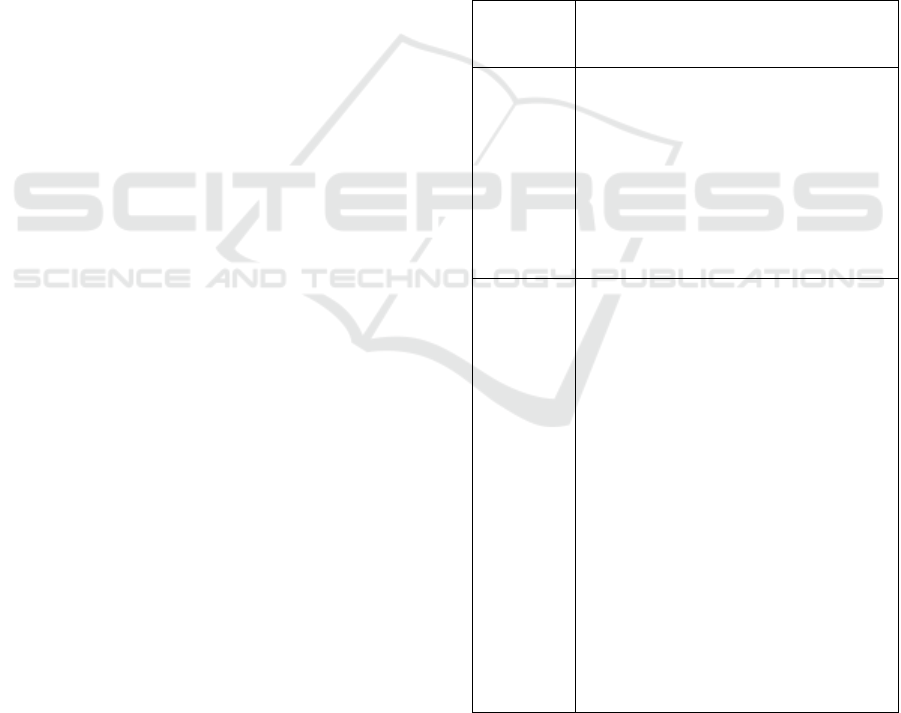
Table 4: Details on the mode of the survey.
Mode of
the survey
Details
Online
survey
(N=5;
for R1-R5)
A LimeSurvey instance by the main
authors’ institution has been used with
the elements as displayed in Table 1
The link to the survey has been sent
via the Europe-wide network of the
authors to contact representatives of
the payer or insurer side in the health
care system. A reminder was sent out
two weeks later.
Guideline-
based in-
person
interview
(N=1;
for R6)
The elements in Table 1 have served as
a guideline for the interview.
Not every single element was gone
through step by step. On the one hand,
the flow of the conversation should not
be interrupted unnecessarily. On the
other hand, partial aspects of some
questions were already addressed in a
previous answer, so that all relevant
aspects were nevertheless covered.
The conversation lasted about 1 hour.
Two people took part on both the
respondent and interviewer sides. This
ensured a good match with the survey
objectives.
A written summary of the interview
has been created based on the notes
taken during the interview.
Scale-IT-up 2024 - Workshop on Emerging Business Models in Digital Health
878
