
Reimagining Preventive Care and Digital Health:
A Paradigm Shift in a Health Insurance’s Role
Wasu Mekniran
1,2 a
, Jan-Niklas Kramer
1,5 b
and Tobias Kowatsch
2,3,4 c
1
Centre for Digital Health Interventions (CDHI), Institute of Technology Management,
University of St. Gallen, Switzerland
2
CDHI Department of Management, Technology, and Economics, ETH Zurich, Switzerland
3
Institute for Implementation Science in Health Care, University of Zurich, Switzerland
4
School of Medicine, University of St. Gallen, Switzerland
5
CSS Kranken-Versicherung AG, Switzerland
Keywords: Preventive Care, Business Model, Healthy Longevity, Health Insurance, Digital Health Technologies.
Abstract: Amidst non-communicable diseases' substantial health and economic burdens, health insurance companies
and digital health technologies (DHTs) are increasingly crucial in enabling preventive care and minimizing
global health expenditure. This position paper explores the perspective of an innovation manager of a Swiss
health insurer. The interview transcript was analyzed using thematic analysis. The results highlight the
importance of current regulations, the future role of health insurance companies, and the potential of DHTs
to promote preventive care and business model innovation.
1 INTRODUCTION
Healthcare expenditure per capita rose 6% across 50
countries in 2020 alone (World Health Organization,
2022). Several countries are under pressure to reform
healthcare systems. On the one hand, preventive care
delivered by digital health technologies (DHTs)
seems promising (Castro et al., 2023; Jaconson et al.,
2022; Kowatsch & Fleisch, 2021; Kramer et al.,
2020), as they can be a more accessible alternative to
traditional interventions. On the other hand, prevention
should be considered, as it accounts for less than 3% of
overall health expenditure, although focussing on
prevention can change the healthcare system from a
reactive to a proactive approach that promotes overall
health and well-being (Gmeinder et al., 2017).
To successfully implement preventive care,
several stakeholders, such as governmental and
regulatory bodies, should come together to shape a
health insurance plan, for example, through a
partnership between health insurer, hospitals, and
universities (Harrison, 2021). This indicates that
health insurers with a proper environment can
influence the healthcare system and play a key role in
a
https://orcid.org/0000-0001-5184-0438
b
https://orcid.org/0000-0002-8912-1209
c
https://orcid.org/0000-0001-5939-4145
achieving successful preventive care (Brook et al.,
2006); Herzlinger & Parsa-Parsi, 2004). Therefore,
our work aims to contribute to the existing scientific
literature by going deeper and studying a health
insurance perspective of preventive care and digital
health technologies.
This position paper explores the perspective of an
innovation manager at one of the largest Swiss health
insurance companies, CSS Group, which insures over
1.75 million customers with 98 agencies. The results
can inform external and internal drivers of business
model innovation (BMI), where redesigning business
processes in healthcare enables or improves the
implementation of preventive care. To this end, an
interview with the innovation manager was conducted
to answer the following research questions: (1) What
regulatory change is required to make preventive care
successful? (2) For what do we need DHTs most? (3)
What is the future role of a health insurer? and (4) Why
would a health insurer offer DHTs?
Next, related work on preventive care and BMI is
presented. The qualitative research methods are then
described. Finally, the results of the interview are
followed by a discussion and conclusion.
852
Mekniran, W., Kramer, J. and Kowatsch, T.
Reimagining Preventive Care and Digital Health: A Paradigm Shift in a Health Insurance’s Role.
DOI: 10.5220/0012400300003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 852-858
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
2 RELATED WORK
2.1 Focus on Preventive Care
Preventing non-communicable diseases (NCDs),
including common mental disorders, is essential to
reduce the substantial burden on healthcare systems.
Particularly in low-middle-income countries,
healthcare costs for NCD are worsening (Hajat &
Stein, 2018) (Murphy et al., 2020). Recognizing these
health and economic challenges, WHO declared 2021
to 2030 a decade of healthy aging (WHO, 2020). This
initiative aims to reform the current sick-care system,
where ambiguous actions hinder various stakeholders
from collectively promoting preventive care.
To achieve sustainable prevention and healthy
aging goals, the WHO outlined priority action areas
such as ensuring that communities foster and provide
access to long-term care for those in need. As aging
leads to NCDs, the obvious solution is to proactively
minimize those risks by living a healthier lifestyle.
This movement to extend the health span rather than
merely living longer refers to healthy longevity (Fried
et al., 2022).
2.2 Business Model Innovation
Business Model Innovation (BMI) is a
reconfiguration of the business model to generate
more value (Foss & Saebi, 2017). For instance,
transitioning from a product-based to a service-based
model, incorporating digital platforms for customer
engagement, or adopting a subscription model for
recurring revenue. Given this context, the way
healthcare providers administer health interventions
and how governments structure reimbursement
strategies can be examined through the lens of BMI.
This approach is vital for the successful
implementation of preventive care (Kaplan &
Milstein, 2019). For instance, if a digital channel is
used to deliver health interventions, trust plays a
pivotal role; therefore, the choice of the delivery
channel must be carefully considered (De Santis et
al., 2021). In a time of rapid demographic and
technological changes, preventive care needs suitable
business models and ecosystems to be truly efficient.
Therefore, current stakeholders in healthcare
systems, such as health insurance firms, need to
evaluate new business models to match their
capabilities with the desired value propositions. This
study explores possible approaches that could make
preventive care more effective and examines how
DHTs can offer valuable contributions.
3 METHODS
To address the research questions previously
mentioned, an interview was conducted with an
innovation manager. The interview framework was
developed based on topics highlighted during the
Scale-IT-up 2024 workshop, which focuses on
emerging business models in the field of digital
health. This workshop is held in collaboration with
the 17th International Joint Conference on
Biomedical Engineering Systems and Technologies
(BIOSTEC, 2024). The methodological details are
outlined below.
3.1 Data Collection
The interview was conducted with Dr. Jan-Niklas
Kramer in October 2023. The authors developed a
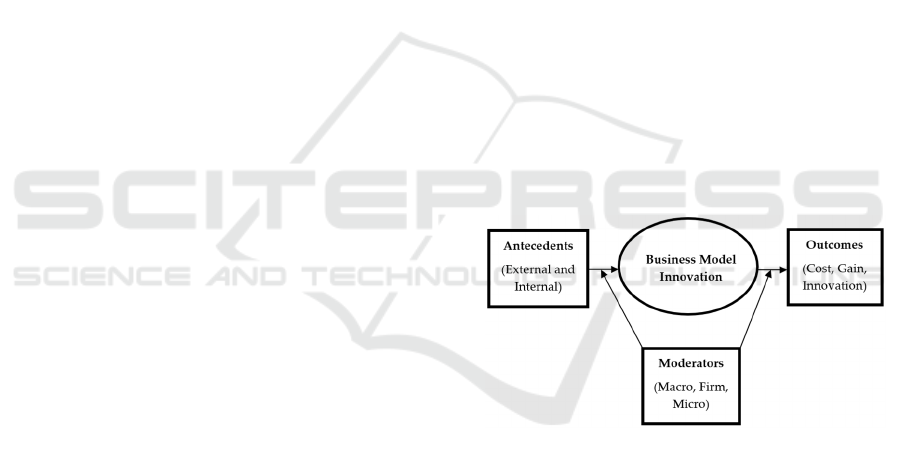
structured interview guide following a BMI research
framework in Figure 1 (Foss & Saebi, 2017). The
dimensions in this Business Model Innovation (BMI)
research framework offer insights into why
organizations are motivated to adopt BMI
(antecedents), how BMI is influenced at various
organizational tiers (moderators), what the
anticipated results of BMI are (outcomes), and the
process through which BMI evolves.
Figure 1: BMI research framework. Note: own illustration
adapted from Foss & Saebi (2017).
3.2 Data Analysis
The interview was conducted and transcribed with
Microsoft Teams Classic (version 1.6). This study
used the qualitative data analysis tool ATLAS.ti
(version 23) to analyze interview transcripts. The
preliminary coding frame is based on the interview
outline. Data were analyzed using a thematic analysis
process (Clarke et al., 2015).
The coding focused on areas of BMI to derive
insights from interview questions. This study
followed the thematic analysis approach of Clarke et
al. (2015): (1) becoming familiar with the data,
(2) generating codes, (3) generating themes,
Reimagining Preventive Care and Digital Health: A Paradigm Shift in a Health Insurance’s Role
853
(4) reviewing themes, (5) defining and naming
themes, and (6) finding examples.
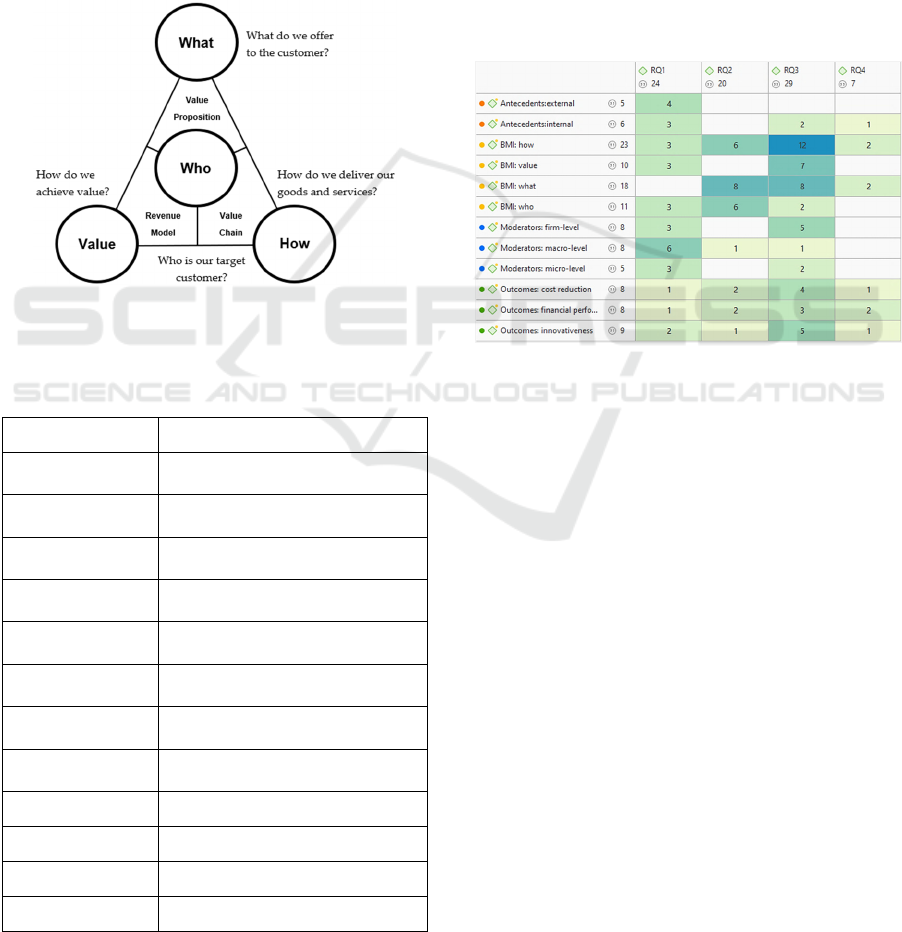
Table 1 lists themes and definitions used to derive
insight from answers to the research questions. This
study adopted a Business Model Navigator (BMN) to
help guide the data analysis process in Figure 2
(Gassmann et al., 2020). In addition, the BMI process
in the BMI research framework has been replaced
with the four dimensions of BMN: What, Who, How,
and Value. Eventually, the BMN dimensions provide
us with logic to investigate specific relationships in
business models, specifically what is offered, how it
is delivered, how the value is captured, and to whom.
Figure 2: Business Model Navigator’s dimensions. Note:
own illustration adapted from (Gassmann et al., 2020).
Table 1: Theme and its definition. Note: BMI stands for
business model innovation.
Theme Definition
Antecedents:
external
Change in competition,
stakeholder, etc.
Antecedents:
internal
Dynamic capabilities, change in
strateg
y
Moderators:
macro-level
Competition law, regulations
Moderators:
firm-level
Organizational values, design,
culture
Moderators:
micro-level
Managerial cognition, loss
aversion, etc.
Outcomes:
finance
Financial performance, revenue,
etc.
Outcomes:
innovativeness
New value creation
Outcomes:
cost reduction
Lower cost in operation
BMI: what Offering
BMI: who Target customer
BMI: how Delivery of an offer
BMI: value Revenue model and cost structure
4 RESULTS
This section describes emerging themes, the
identified corresponding BMI elements, and their
classifications according to our research questions,
for instance, What and Who dimensions of the
business model that capture the value proposition
aspect of the results are analyzed (Gassmann et al.,
2020). Figure 3 presents a heat map that displays the
overall distribution of themes derived from the
interview. The numerical values on the heat map
represent the frequency of each theme in relation to
each research question (RQ). In this way, the heat
map illustrates both the quote density and the
structure of this particular interview.
Figure 3: Heat map of theme distribution based on business
model innovation dimensions (vertical) according to the
research question 1-4 (horizontal).
4.1 What Regulatory Change Is
Required to Make Preventive Care
Successful?
Table 2 lists the external and internal motivators
(antecedents) and moderators at the macro-level that
set the landscape of preventive care in the current
state. An underlying message is that Swiss
regulations must enable preventive care offerings in
general
.
Although there are examples of alternative
reimbursement systems for secondary and tertiary
prevention, such as Prescription Digital Therapeutics
in Germany (FIDMD, 2020); (Fürstenau et al., 2023),
regulatory bodies still need to successfully combine
efforts to lower the hurdle of preventive care
implementation in Switzerland.
Scale-IT-up 2024 - Workshop on Emerging Business Models in Digital Health
854
Table 2: Quote on regulations for preventive care in the
current state.
Theme Quote
antecedents:
external
the regulatory landscape is a big hurdle
for prevention... The law limits
healthcare providers from offering
preventive services...
antecedents:
external
prevention is the responsibility of each
and everyone... himself or herself.
antecedents:
internal
Historically...the philosophy of the
Swiss healthcare system is... a sick care
system
antecedents:
internal
Ideally, the first step comes from the
policymakers themselves…and acting
together, this is something that does not
yet seem to be the case in Switzerland.
antecedents:
internal
...for example, the farmer and
MedTech and lobby, who could oppose
these regulations as they might threaten
their current business model.
moderators:
macro-level
...in Germany, for example, with the
DiGA list, it is not prevention, but it is
an example where the system has put a
legal process for the reimbursement.
moderators:
macro-level
We as a society need to (be) regulated,
(and) it is also an enabler.
4.2 For What Do We Need DHTs
Most?
Table 3 lists the value propositions of DHTs from the
What and Who dimensions of the business model,
along with the expected outcomes that could be
derived from DHTs. The results of the interview
suggest that DHTs are particularly beneficial for
improving access to care for stigmatized and chronic
diseases, such as HIV/AIDS and mental health issues,
especially among vulnerable populations such as the
elderly and low-income communities. Contrary to
popular belief, the primary users of DHTs tend to be
middle-aged rather than younger individuals,
according to CSS experience. There is a selection bias
among the user group, as healthier individuals
frequently adopt DHTs (Lupton, 2020).
Table 3: Quote on value propositions of DHTs.
Theme Quote
BMI:
what
...high value (for) the classic non-
communicable diseases, heart disease,
diabetes, and obesity.
BMI:
what
where there is a shortage in care such as
dermatology...similar(ly) mental
health...access to care is a great
opportunity for digital health.
BMI:
who
diseases that are stigmatized; mental
health, but also sexually transmitted
diseases.
BMI:
who
convenience factor (as) in our telemedicine
models we have a very broad spectrum of
people, but mostly they are drawn in by the
price.
BMI:
who
We often have a mean age of around
45…contradicts the assumption that digital
products are primarily for the younger
population.
BMI:
who
... The people who use digital products are
more health conscious, more healthy...
selection bias.
outcomes:
cost
reduction
...low burden way to access care, and...we
are seeing that digital health technologies
in mental health (are) among the most
successful examples.
4.3 What Is the Future Role of a
Health Insurer?
Table 4 reports on quotes around the future role of
health insurance companies from the How dimension
of the business model and the expected outcomes of
BMI. Three strategies that insurers could shift their
role based on the results of the interview: (1) staying
out of the healthcare market and pursuing a cost-
leadership strategy; (2) supporting healthcare
providers as contract innovators in implementing
preventive care (Gilson et al., 2009); and (3)
extending the range of offerings as a healthcare
provider themselves.
Reimagining Preventive Care and Digital Health: A Paradigm Shift in a Health Insurance’s Role
855

Table 4: Quote on the shift in the role of health insurance.
Theme Quote
BMI:
how
offering a capitation model where
physicians are also accountable and
responsible for prevention.
BMI:
how
...health content, with counselling
trying to help people navigate the
healthcare s
y
stem.
BMI:
how
...so-called managed care
contracts...typically between the
insurer and a
p
rimar
y
care network.
outcomes: cost
reduction
a cost leadership strategy, focusing
and reducing all other expenses and
focusing on paying the healthcare
b
ills.
outcomes:
financial
p
erformance
...to negotiate integrated care
contracts with hospitals and primary
p
h
y
sicians
(
Contract innovator
)
.
outcomes:
innovativeness
...move toward being a health care
partner and a health
organization...extending the business
model more towards healthcare
services.
4.4 Why Would a Health Insurer Offer
DHTs?
Table 5 highlights quotes about why health insurance
companies would offer DHTs. The findings suggest
that insurers can differentiate themselves by
improving the user experience, serving as both a
primary advisor and a comprehensive information
platform that links to additional healthcare services.
For example, the WELL app from the CSS allows
users to assess their symptoms and schedule doctor's
appointments, all within one platform. Furthermore,
DHTs promise to lower expenses related to the
management of chronic diseases. This can be
achieved through features such as medication
reminders and automated health summary, among
others.
Table 5: Quote on why insurance would offer DHTs.
Theme Quote
BMI:
how
...to facilitate information exchange
b
etween healthcare
p
roviders and.
BMI:
what
...project with the highest value
created...in the customer
ex
p
erience.
outcomes: cost
reduction
mainly for this purpose (as for)
chronic disease programs and the
main benefit would be cost savin
g
s.
outcomes:
innovativeness
...customer experience and
differentiation in the market.
5 DISCUSSION
The interview results show that the Swiss healthcare
system's focus is on sick care and not on preventive
care. To this end, the results are consistent with
previous work, which shows that prevention is mostly
neglected (Gmeinder et al., 2017). At the same time,
the capitation model is gaining momentum in health
insurance, confirming the trend of shifting values and
roles between insurers and healthcare providers
(Miller, 2009).
An explanation for the care-providing limit and
the absence of reimbursement models is described as
necessary changes in Section 4.1. Regulation is seen
as motivators and moderators of BMI that,
unfortunately, hinder the move away from sick care
to health care. Another structural challenge is the
annual option for customers to cancel their insurance
contracts. This arrangement discourages insurers
from investing in long-term preventive measures. The
reason is that the benefits of such investments, such
as cost savings, manifest over an extended period. If
a customer switches to a different health insurance
provider within that time, the financial advantages go
to the competitor. However, as described in Sections
4.2 and 4.3, insurers look forward to collaborating
with healthcare providers using DHTs and to
incentivizing healthcare providers to make
provisions, as the remuneration system, like the
capitation model, can have an impact on overall
health outcomes (Kaplan & Milstein, 2019). It was
also revealed that DHTs are primarily employed by
health insurance companies to improve the customer
healthcare experience, rather than focusing on illness
prevention (see Section 4.4).
The discovery was made that DHTs can provide
benefits, such as expanding care access for vulnerable
populations with stigmatized and chronic diseases.
Additionally, DHTs will further reduce the operating
costs of current healthcare providers. This could
include hospitals and other medical facilities by
automating primary care functions such as routine
checks, medication management, and basic
diagnostic tests.
As limitations and future scope of this work,
current findings should be deepened by additional
interviews to continually reduce opinion biases.
Second, the discussed region could be extended
beyond Switzerland to neighboring countries. Lastly,
employing a second or third investigator to
triangulate the coding process could reduce human
error. Future research will extend the current work to
include various stakeholders in the health insurance
Scale-IT-up 2024 - Workshop on Emerging Business Models in Digital Health
856

industry, such as policyholders, healthcare providers,
regulatory agencies, and insurers.
6 CONCLUSIONS
Qualitative data was collected and analyzed from an
interview with Dr. Kramer, an innovation manager at
one of Switzerland's largest health insurers.
According to our findings, regulatory frameworks for
preventive measures enable providers to offer to
individuals in need.
From a BMI perspective, our findings highlight
the trend of collaboration between insurers and
healthcare providers. This makes health insurers
important in setting the right incentives for primary
care providers, such as the capitation model that
controls the volume of care given and rewards a cost-
saving strategy (Miller, 2009).
Although there are approaches to achieving cost
leadership and innovating business models for health
insurance companies, DHTs present a great potential
to realistically enable future health insurance roles.
Lastly, future research can compare different
geographic regions and the paradigm-shifting
dynamic of preventive care.
CONFLICTS OF INTEREST
WM, JK, and TK are affiliated with the Centre for
Digital Health Interventions (CDHI), a joint initiative
of the Institute for Implementation Science in Health
Care, University of Zurich; the Department of
Management, Technology, and Economics at the
Swiss Federal Institute of Technology in Zürich; and
the Institute of Technology Management and School
of Medicine at the University of St Gallen. CDHI is
funded in part by CSS, a Swiss health insurer and
MavieNext, an Austrian healthcare provider. TK is
also a co-founder of Pathmate Technologies, a
university spin-off company that creates and delivers
digital clinical pathways. However, neither Pathmate
Technologies nor MavieNext were involved in this
research.
REFERENCES
BIOSTEC. (2024). Workshop on Emerging Business
Models in Digital Health—Scale-IT-up 2024. Scale-IT-
up 2024. https://biostec.scitevents.org/Scale-IT-up!.aspx
Brook, R. H., Keeler, E. B., Lohr, K. N., Newhouse, J. P.,
Ware, J. E., Rogers, W. H., Davies, A. R., Sherbourne,
C. D., Goldberg, G. A., Camp, P., Kamberg, C.,
Leibowitz, A., Keesey, J., & Reboussin, D. (2006). The
Health Insurance Experiment: A Classic RAND Study
Speaks to the Current Health Care Reform Debate.
RAND Corporation. https://www.rand.org/pubs/resear
ch_briefs/RB9174.html
Castro, O., Mair, J. L., Salamanca-Sanabria, A., Alattas, A.,
Keller, R., Zheng, S., Jabir, A., Lin, X., Frese, B. F.,
Lim, C. S., Santhanam, P., van Dam, R. M., Car, J., Lee,
J., Tai, E. S., Fleisch, E., von Wangenheim, F., Tudor
Car, L., Müller-Riemenschneider, F., & Kowatsch, T.
(2023). Development of “LvL UP 1.0”: A smartphone-
based, conversational agent-delivered holistic lifestyle
intervention for the prevention of non-communicable
diseases and common mental disorders. Frontiers in
Digital Health, 5. https://www.frontiersin.org/
articles/10.3389/fdgth.2023.1039171
Clarke, V., Braun, V., & Hayfield, N. (2015). Thematic
analysis. Qualitative psychology: A practical guide to
research methods, 3, 222–248.
De Santis, K. K., Jahnel, T., Sina, E., Wienert, J., & Zeeb,
H. (2021). Digitization and Health in Germany: Cross-
sectional Nationwide Survey. JMIR Public Health and
Surveillance, 7(11), e32951. https://doi.org/10.2196/
32951
FIDMD. (2020). The Fast-Track Process for Digital Health
Applications (Diga) According to Section 139e Sgb V:
A Guide for Manufacturers, Service Providers and
Users. https://www.bfarm.de/SharedDocs/Downloads/
EN/MedicalDevices/DiGA_Guide.pdf?__blob=public
ationFile
Foss, N. J., & Saebi, T. (2017). Fifteen Years of Research
on Business Model Innovation: How Far Have We
Come, and Where Should We Go? Journal of
Management, 43(1), 200–227. https://doi.org/10.1177/
0149206316675927
Fried, L. P., Wong, J. E.-L., & Dzau, V. (2022). A global
roadmap to seize the opportunities of healthy longevity.
Nature Aging, 1–4. https://doi.org/10.1038/s43587-
022-00332-7
Fürstenau, D., Gersch, M., & Schreiter, S. (2023). Digital
Therapeutics (DTx). Business & Information Systems
Engineering, 65(3), 349–360. https://doi.org/10.1007/
s12599-023-00804-z
Gassmann, O., Frankenberger, K., & Choudury, M. (2020).
The Business Model Navigator: 55+ models that will
revolutionise your business (Second Edition). Pearson.
Gilson, R. J., Sabel, C. F., & Scott, R. E. (2009).
Contracting for Innovation: Vertical Disintegration and
Interfirm Collaboration. Columbia Law Review, 109(3),
431–502.
Gmeinder, M., Morgan, D., & Mueller, M. (2017). How
much do OECD countries spend on prevention? OECD.
https://doi.org/10.1787/f19e803c-en
Hajat, C., & Stein, E. (2018). The global burden of multiple
chronic conditions: A narrative review. Preventive
Medicine Reports, 12, 284–293. https://doi.org/10.10
16/j.pmedr.2018.10.008
Reimagining Preventive Care and Digital Health: A Paradigm Shift in a Health Insurance’s Role
857

Harrison, M. (2021, Dezember 15). 5 Critical Priorities for
the U.S. Health Care System. Harvard Business
Review. https://hbr.org/2021/12/5-critical-priorities-
for-the-u-s-health-care-system
Herzlinger, R. E., & Parsa-Parsi, R. (2004). Consumer-
Driven Health Care: Lessons From Switzerland. JAMA,
292(10), 1213. https://doi.org/10.1001/jama.292.10.12
13
Jaconson, N. C., Kowatsch, T., & Marsch, L. A. (2022).
Digital therapeutics for mental health and addiction:
The state of the science and vision for the future.
Academic Press.
Kaplan, R. M., & Milstein, A. (2019). Contributions of
Health Care to Longevity: A Review of 4 Estimation
Methods. Annals of Family Medicine, 17(3), 267–272.
https://doi.org/10.1370/afm.2362
Kowatsch, T., & Fleisch, E. (2021). Digital Health
Interventions. In O. Gassmann & F. Ferrandina (Hrsg.),
Connected Business (S. 71–95). Springer International
Publishing. https://doi.org/10.1007/978-3-030-76897-
3_4
Kramer, J.-N., Künzler, F., Mishra, V., Smith, S. N., Kotz,
D., Scholz, U., Fleisch, E., & Kowatsch, T. (2020).
Which Components of a Smartphone Walking App
Help Users to Reach Personalized Step Goals? Results
From an Optimization Trial. Annals of Behavioral
Medicine, 54(7), 518–528. https://doi.org/10.1093/
abm/kaaa002
Lupton, D. (2020). ‘Better understanding about what’s
going on’: Young Australians’ use of digital
technologies for health and fitness. Sport, Education
and Society, 25(1), 1–13. https://doi.org/10.1080/1357
3322.2018.1555661
Miller, H. D. (2009). From volume to value: Better ways to
pay for health care. Health Affairs (Project Hope),
28(5), 1418–1428. https://doi.org/10.1377/hlthaff.28.
5.1418
Murphy, A., Palafox, B., Walli-Attaei, M., Powell-Jackson,
T., Rangarajan, S., Alhabib, K. F., Avezum, A. J.,
Calik, K. B. T., Chifamba, J., Choudhury, T., Dagenais,
G., Dans, A. L., Gupta, R., Iqbal, R., Kaur, M.,
Kelishadi, R., Khatib, R., Kruger, I. M., Kutty, V. R.,
… McKee, M. (2020). The household economic burden
of non-communicable diseases in 18 countries. BMJ
Global Health, 5(2), e002040. https://doi.org/10.1136/
bmjgh-2019-002040
WHO. (2020). Decade of healthy ageing: Baseline report.
World Health Organization. https://apps.who.int/iris/
handle/10665/338677
World Health Organization. (2022). Global spending on
health: Rising to the pandemic’s challenges. World
Health Organization.
APPENDIX
Topics of interest at the 17th International Joint
Conference on Biomedical Engineering Systems and
Technologies (BIOSTEC, 2024) include, but are not
limited to:
How to make prevention successful?
How to make healthy longevity successful?
How to make healthy aging successful?
How to make elderly care successful?
How to cope with the economic burden of
non-communicable diseases?
Which emerging business models in digital
health are promising?
What needs to change in terms of regulations
to make digital health successful?
What is the future role of a health insurance
company?
Which digital health technologies (DHTs)
are already used and reimbursed? In which
fields? What are those offerings? How are
these paid for? (self-paid, basic insurance,
additional insurance, etc.)
Are you offering DHTs? Did you develop
these DHTs yourself or are you partnering
with startups or other companies?
Do you offer DHTs rather in the prevention
or in the management of diseases?
For which diseases do you think we need
DHTs most? Why? Where do you think
DHTs will work best? (what kind of disease
and persona)
What is your main goal of offering these
DHTs? (new revenue streams, cost-
efficiency, customer loyalty)
What is the importance of business
ecosystems for these DHTs?
What kind of learnings did you generate so
far? Are there DHTs that worked better than
others? Why?
Could you already assess the effectiveness
and/or efficiency of DHTs?
What kind of DHTs failed? What were the
reasons?
How would you improve DHTs you are
offering?
Scale-IT-up 2024 - Workshop on Emerging Business Models in Digital Health
858
