
Transforming NCD Business Models in Switzerland: CSS Insurance
Perspective
Odile-Florence Giger
1a
, Christopher Bensch
2b
and Tobias Kowatsch
3,4 c
1
Institute of Technology Management, University of St. Gallen, St. Gallen, Switzerland
2
CSS Insurance, Lucerne, Switzerland
3
Institute for Implementation Science in Health Care, University of Zurich, Zurich, Switzerland
4
School of Medicine, University of St. Gallen, St. Gallen, Switzerland, Centre for Digital Health Interventions,
Department of Management, Technology, and Economics, ETH Zurich, Zurich, Switzerland
Keywords: NCD Management, Business Model, Health Insurance, Telemonitoring.
Abstract: The worldwide incidence of non-communicable diseases (NCDs) is increasing, prompting exploration into
technological advancements that present fresh prospects for treating and managing NCDs. Numerous well-
established companies have been working in the field of NCD management, providing digital tools for the
efficient management. Although there are many digital health companies nowadays, building them up at scale
is difficult due to a heterogeneous, inefficient, and fragmented healthcare system. Therefore, we engaged in
a conversation with Christopher Bensch, healthcare expert at CSS – one of Swiss’ largest health insurers – to
understand better which business models may improve the management of NCDs. The insights are structured
along the business model framework of the “Magic Triangle”. We found that the integration of healthcare
providers is crucial when implementing the business model. Furthermore, new business models should be
launched lean, pragmatic, and improved along the innovation process within the given regulatory rules rather
than waiting for the regulatory environment to change.
1 INTRODUCTION
Approximately 2.2 million people in Switzerland
suffer from noncommunicable diseases (NCDs) such
as heart disease, chronic obstructive pulmonary
diseases and diabetes (BAG, 2023). Total direct costs
of NCDs in Switzerland are estimated at 52 billion
Swiss francs per year, comprising about 80% of the
total healthcare costs (BAG, 2021). Hence, NCDs
stand as a widespread, detrimental, and expensive
condition.
Numerous companies offer their services for
managing NCDs (here referred as “NCD companies”)
leveraging digital health technologies (DHTs), i.e.
“computing platforms, connectivity, software, and
sensors [used] for health care and related uses.”
(Digital Therapeutics Alliance, 2023). These
technologies can improve access to health
information for both patients and providers, enable
a
https://orcid.org/0009-0005-7660-864X
b
https://orcid.org/0009-0000-5666-1914
c
https://orcid.org/0000-0001-5939-4145
remote patient monitoring, and deliver timely
healthcare recommendations and reminders to
patients (Klonoff, 2013). Therefore, DHTs can
positively affect patients (Hood et al., 2016; Keller et
al., 2022) and care providers (Doyle-Delgado &
Chamberlain, 2020). Nevertheless, new DHTs at the
nexus of the healthcare and tech industry require a
successful business model (Steinberg et al., 2015).
But even if digital health business models are
successfully built, scaling them up is often
challenging due to heterogeneous, inefficient, and
fragmented healthcare systems (Garber & Skinner,
2008). This fragmentation can be seen also in
Switzerland, where each of the 26 cantons has a
distinct health legislation. Still, each canton is vital
in delivering healthcare services (Maurer et al.,
2022). It is said that one of the biggest barriers to new
digital business models in Switzerland is the lack of
regulatory transparency and reimbursement
846
Giger, O., Bensch, C. and Kowatsch, T.
Transforming NCD Business Models in Switzerland: CSS Insurance Perspective.
DOI: 10.5220/0012400100003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 846-851
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
possibilities (Sojer et al., 2018). Facing many
challenges, the question arises of how new Swiss
business models for managing NCDs should look to
improve the treatment of patients and save costs
substantially.
Health insurance companies are interested in
finding innovative solutions to keep their plan
members healthy, improve the health outcomes for
those that need care at reasonable costs and thus
improving their competitive position in the market.
Therefore, we aimed to understand better how CSS,
one of Swiss’s largest health insurance companies,
thinks about offering services to individuals affected
by one or several NCDs. The CSS health insurance is
serving more than 1.75 Mio. customers, which make
up 20% of the total population (CSS, 2023). To tackle
healthcare challenges, CSS has implemented
different innovation strategies. First, they set an
example by founding the SwissHealth Ventures AG,
a fund of 50 million Swiss francs to invest in digital
healthcare startups (Enz, 2020). Together with
partners, CSS also launched the digital health
platform Well with the goal of improving integrated
care. They also initiated the CSS Health Lab, a
research collaboration with ETH Zurich and the
University of St. Gallen, with the overall goal of
researching digital business models, digital
biomarkers, and health interventions (CSS, 2023).
Against this background, we engaged in a
conversation with Christopher Bensch, who works in
strategy and corporate services as a healthcare expert
at CSS, to learn how he thinks about building up a
successful, sustainable, and scalable service for
individuals affected by NCDs. To this end, we asked
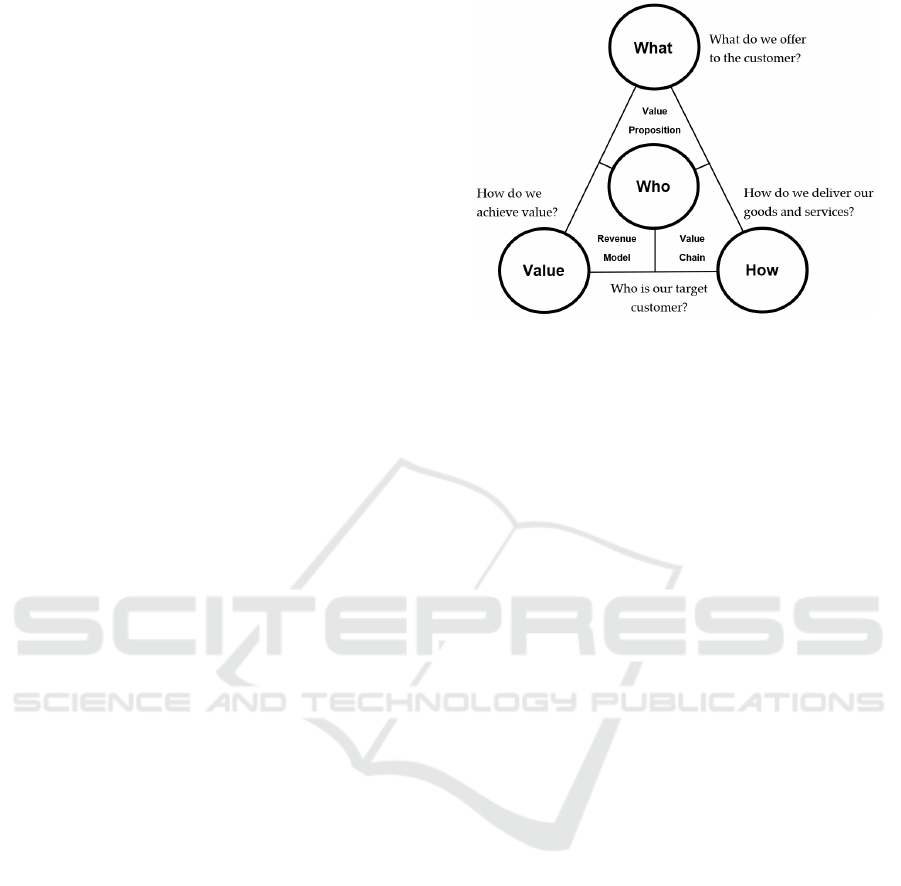
the following questions based on Gassmann et al.
(2017):
- WHAT should NCD companies offer (the
value proposition)?
- WHO should their target customers be (e.g.
companies, healthcare professionals,
patients)?
- HOW should their services be delivered (the
value chain)?
- How should these companies create VALUE
(the revenue model)?
In chapter 2, the insights of the interview with Mr.
Bensch will be structured along the business model
framework “Magic Triangle” as depicted in figure 1
(Gassmann et al., 2017). Furthermore, insights from
grey and academic literature will be used to discuss
the statements of Mr. Bensch. In chapter 3, we draw
a conclusion and show the limitations of this study.
Figure 1: Magic Triangle (Gassmann et al., 2017).
2 DISCUSSION
2.1 WHAT: Telemonitoring and
Integrated Software Solutions
According to Bensch (CB), telemonitoring solutions
are promising technologies to improve care
management for NCDs. Telemonitoring involves the
gathering, transmission, assessment, and
communication of a patient's personal health
information to their healthcare provider or extended
care team, all while being conducted beyond the
confines of a hospital or clinical setting, typically in
the patient's home. This is made possible through the
utilization of personal health technologies such as
wireless devices, wearable sensors, implanted health
monitors, smartphones, tablets, and mobile
applications (Gijsbers et al., 2022). There are many
conditions, such as diabetes, where regular
consultations are important but do not necessarily
require on-site and synchronous consultations (CB).
In Bensch’s opinion, the problem in NCD
management is that the time is not spent effectively
on those patients that need care most. This is due to
lacking means and time to identify the patients that
truly need care (CB). Generally, time is spread evenly
across all patients, so patients that manage their
disease well get more attention than needed, while
those that need more support are lacking the right
support (CB). Bensch sees here the true benefit of
telemonitoring (CB).
Telemonitoring has the potential to offer more
frequent and continuous patient monitoring. This
could enhance the quality of care, reduce the time
clinicians invest in patient management, and increase
monitoring frequency without overburdening
Transforming NCD Business Models in Switzerland: CSS Insurance Perspective
847

healthcare resources (Fazal et al., 2020; Ong et al.,
2016; Shah et al., 2021). This permits early
intervention and, ideally, the prevention of a
condition from worsening further which will then
lead to better health outcomes and ultimately save
costs (Malasinghe et al., 2019).
Furthermore, Bensch mentioned that there are
already digitized medical devices for patients (e.g.,
Continuous Glucose Monitoring) in NCD
management (CB). Those tools should be integrated
tightly in the health care pathways of providers to
enable telemonitoring and to improve the outcomes
of the treatment of the patient (CB). A recent study
supports these statements of Mr. Bensch, stating that
Switzerland could save up to 1.1 billion in costs only
by telemonitoring solutions for NCDs (McKinsey,
2021).
Furthermore, according to Bensch integrating
different software solutions in hospitals and general
practices could help improve the efficiency of current
care processes (CB). In Switzerland, many healthcare
providers are running on different IT systems, even in
the same clinic, different systems are not connected
leading to substantial process inefficiencies and
reduced operational agility (Blijleven et al., 2017).
Bensch names the example of Diabeter in the
Netherlands that has integrated a full technology
stack into their care pathways and into its daily
routine of care delivery. Diabeter, unlike traditional
hospital care, employs a specialized team for diabetes
patients. Each patient has a dedicated care manager
for continuous support, with regular check-ins and
annual assessments. The team provides ongoing care
adjustments through email, video calls, and phone
consultations. Patients also have access to a 24/7
emergency hotline for immediate specialist
assistance. Another example that Bensch mentioned,
is the US-based company Glooko that offers a tech
solution in diabetes management combining
telemonitoring and integration of different software
(CB). Glooko integrates several stakeholders
(patients, healthcare providers, medical device
companies, etc.) and different types of data (e.g.
blood glucose, diet, fitness, biometrics, insulin and
medication data) on one platform. It was shown that
their telemonitoring solution could significantly
improve an important health outcome (A1C, i.e., the
average blood sugar levels over the last three months)
of patients diagnosed with type 2 diabetes (Ranes,
2020).
2.2 WHO: Patients with Complex
Disease Management and
Healthcare Providers
According to Bensch, telemonitoring is especially
useful for patients with complex disease management
requirements and where connected medical devices
already exist (CB). Therefore, NCD business models
should target patients who suffer from severe health
conditions like diabetes, cardiovascular diseases, or
respiratory diseases (CB). In the case of diabetes,
healthcare provider will then be able to monitor,
coach, diagnose and treat the patient based on current
and historical data (CB). This can lead to more
personalized and effective care and better decision-
making (Malasinghe et al., 2019; Stone et al., 2010;
Zhai et al., 2014).
Regarding software solutions, Bensch assumes
that it will be mainly the healthcare providers that will
be the paying target group (CB). Studies show, that
for them, it will be easier to streamline clinical and
administrative processes, collect needed outcome
data reducing the need for manual data entry and
paperwork, which will lead to reduced errors and
improve patient safety (Kaushal, 2002; Ruland, 2002;
Ventola, 2014). The lack of open APIs has made it
hard so far to seamlessly integrate the different
solutions and make those compatible with each other
(Faruk et al., 2022).
2.3 HOW: Importance of Healthcare
Providers
For telemonitoring and integrated software solutions,
healthcare providers should be involved early on, as
their IT systems need to be connected to other
solutions (CB). Studies show that almost half of the
Swiss healthcare providers mention that a major
barrier to not implementing DTHs is a lack of
interoperability with their patient information
systems (Sojer et al., 2018). Also, ineffective
stakeholder collaboration hinders DHTs to thrive.
Many core stakeholders lack incentives to pursue new
DHTs together (Landers et al., 2023). Furthermore,
according to Bensch, when developing a new
business model, businesses should not wait for the
regulations to change, as this is estimated to take
several years. Although a Swiss regulatory sandbox
exists (Experimentierartikel, KVG Art. 59b) where
cantons and tariff partners are allowed to implement
innovative pilot projects to curb cost growth and
promote digitization in healthcare, Bensch’s opinion
is clear: Even with this new article, the process of
building up new DHTs will take longer than five
Scale-IT-up 2024 - Workshop on Emerging Business Models in Digital Health
848

years, as pilot projects have many requirements to
fulfill. Therefore, he recommends starting in a
pragmatic way within the given regulatory
framework and iterating the business model
continuously (CB).
2.4 VALUE: Patient Will Only Pay for
Integrated Solutions
Generating revenue is one of the most challenging
parts of NCD business models as many stakeholders
have different incentives (CB). In Bensch’s opinion,
patients will most likely only pay for DHTs (either
out of pocket or through additional insurance) if these
solutions are integrated in the care pathway of their
care provider (CB).
In other countries, DHTs are sometimes paid (or
provided by the state or health insurance. For
example, Germany established the Digitale
Versorgung Gesetz (DVG law) which makes DTx
solutions eligible for reimbursement (Mantovani et
al., 2023). Switzerland restricts what services a health
insurer reimburses, making it difficult for companies
to monetize their DHT offerings (CB). In some cases,
healthcare providers will pay for the DHT (e.g.
Glooko, eedoctors). Furthermore, as telemonitoring is
closely related to telemedicine, health insurance
companies may take over the reimbursement within
coverage of additional health insurance products
(CB). According to the doctor’s tariff “Tarmed”,
telemedicine can be reimbursed as well as the review
of patient records (CB).
3 CONCLUSIONS AND
LIMITATIONS
Implementing new business models in the NCD
management in Switzerland is still challenging.
Business models that might work in Switzerland
focus on diseases that are complex to manage and that
have digitized medical devices for the patients
(WHAT). Providing real value for both patients and
healthcare providers is crucial. As Switzerland is still
highly regulated and change can take several years, it
is advised to start lean, build up pragmatic solutions
within the current regulative setup, and improve the
business model iteratively (HOW). Lastly,
monetization still poses a major challenge. Potential
paying customers might be healthcare providers,
patients or insurances through additional coverage
(VALUE & WHO). Specifically, these findings
underline the importance of the integration of
healthcare providers when innovating in the field of
healthcare (HOW). Key success factors will be the
tight integration of technology components in
providers’ regular care pathways, overcoming the
interoperability issues between different IT systems
and handling the reluctance of healthcare providers
towards innovation, as many do not want to take an
active role in innovation (Landers et al., 2023).
Limitations
Although this work has emphasized the efficiency
benefits of telemonitoring, these benefits also need to
be harvested effectively. Telemonitoring solutions
generate a lot of data. Nevertheless, data without
interpretation will not necessarily lead to better
efficiency gains and improved outcomes. New
companies gathering many different data points
across thousands of individuals and making sense of
it generate powerful new business opportunities in the
future (Steinberg et al., 2015). One example is the
partnership between Glooko and Hedia, where
Hedia’s algorithm is integrated into the
telemonitoring solution of Glooko, making it easier
and faster for healthcare providers to interpret the
telemonitoring data of their patients (Glooko, 2023).
Therefore, in future work, a detailed analysis of how
telemonitoring solutions can provide substantial
value for healthcare providers is needed to guarantee
their willingness to pay.
Furthermore, this work is limited by its exclusive
dependence on a singular perspective of one expert
interview. Future research should integrate a more
diverse array of data sources, encompassing inputs
from various experts, studies, and industry reports.
This approach would offer a more thorough analysis,
ensuring the resilience and reliability of the findings.
CONFLICT OF INTEREST
OFG and TK are affiliated with the Centre for Digital
Health Interventions, a joint initiative of the Institute
for Implementation Science in Health Care,
University of Zurich, the Department of
Management, Technology, and Economics at ETH
Zurich, and the Institute of Technology Management
and School of Medicine at the University of
St.Gallen. CDHI is funded in part by CSS, a Swiss
health insurer and MavieNext, an Austrian healthcare
provider, and MTIP, a Swiss investor company. TK
is also a co-founder of Pathmate Technologies, a
university spin-off company that creates and delivers
digital clinical pathways. However, neither Pathmate
Transforming NCD Business Models in Switzerland: CSS Insurance Perspective
849

Technologies, MTIP nor MavieNext was involved in
this research.
REFERENCES
Angerer, A., Hollenstein, E., & Russ, C. (2021). Der Digital
Health Report 21/22: Die Zukunft des Schweizer
Gesundheitswesens [96,application/pdf].
https://doi.org/10.21256/ZHAW-2408
BAG. (2021). National Strategy for the Prevention of Non-
communicable Diseases (NCD) strategy.
https://www.bag.admin.ch/bag/en/home/strategie-und-
politik/nationale-gesundheitsstrategien/strategie-nicht-
uebertragbare-krankheiten.html
BAG. (2023). Zahlen und Fakten zu nichtübertragbaren
Krankheiten. https://www.bag.admin.ch/bag/de/home/
zahlen-und-statistiken/zahlen-fakten-nichtuebertragbar
e-krankheiten.html
Blijleven, V., Koelemeijer, K., & Jaspers, M. (2017).
Identifying and eliminating inefficiencies in
information system usage: A lean perspective.
International Journal of Medical Informatics, 107, 40–
47. https://doi.org/10.1016/j.ijmedinf.2017.08.005
CSS. (2023). https://www.css.ch/de/ueber-css/story/unter
nehmen.html#:~:text=Die%20CSS%20Gruppe%20ver
sichert%20%C3%BCber,bei%20ihren%20Kundinnen
%20und%20Kunden.
Davis, J. W., Chung, R., & Juarez, D. T. (2011). Prevalence
of comorbid conditions with aging among patients with
diabetes and cardiovascular disease. Hawaii Medical
Journal, 70(10), 209–213.
Digital Therapeutics Alliance. (2023). What is a DTx?
https://dtxalliance.org/understanding-dtx/what-is-a-
dtx/
Doyle-Delgado, K., & Chamberlain, J. J. (2020). Use of
Diabetes-Related Applications and Digital Health
Tools by People With Diabetes and Their Health Care
Providers. Clinical Diabetes, 38(5), 449–461.
https://doi.org/10.2337/cd20-0046
Enz, W. (2020, September 29). Der Krankenversicherer
CSS setzt viel Geld auf Startups. NZZ.
https://www.nzz.ch/wirtschaft/der-krankenversicherer-
css-setzt-viel-geld-auf-startups-ld.1578925
Faruk, M. J. H., Patinga, A. J., Migiro, L., Shahriar, H., &
Sneha, S. (2022). Leveraging Healthcare API to
transform Interoperability: API Security and Privacy.
2022 IEEE 46th Annual Computers, Software, and
Applications Conference (COMPSAC), 444–445.
https://doi.org/10.1109/COMPSAC54236.2022.00082
Fazal, N., Webb, A., Bangoura, J., & El Nasharty, M.
(2020). Telehealth: Improving maternity services by
modern technology. BMJ Open Quality, 9(4), e000895.
https://doi.org/10.1136/bmjoq-2019-000895
Garber, A. M., & Skinner, J. (2008). Is American Health
Care Uniquely Inefficient? Journal of Economic
Perspectives, 22(4), 27–50. https://doi.org/10.1257/
jep.22.4.27
Gassmann, O., Frankenberger, K., & Csik, M. (2017).
Geschäftsmodelle entwickeln: 55 innovative Konzepte
mit dem St. Galler Business Model Navigator (2. Aufl.).
Carl Hanser Verlag GmbH & Co. KG.
https://doi.org/10.3139/9783446452848
Gijsbers, H., Feenstra, T. M., Eminovic, N., Van Dam, D.,
Nurmohamed, S. A., Van De Belt, T., & Schijven, M.
P. (2022). Enablers and barriers in upscaling
telemonitoring across geographic boundaries: A
scoping review. BMJ Open, 12(4), e057494.
https://doi.org/10.1136/bmjopen-2021-057494
Glooko. (2023, April 11). Glooko Announces Partnership
with Insulin Dosing Algorithm Company Hedia. https://
glooko.com/news_reg/glooko-announces-partnership-
with-insulin-dosing-algorithm-company-hedia/
Hood, M., Wilson, R., Corsica, J., Bradley, L., Chirinos, D.,
& Vivo, A. (2016). What do we know about mobile
applications for diabetes self-management? A review of
reviews. Journal of Behavioral Medicine, 39(6), 981–
994. https://doi.org/10.1007/s10865-016-9765-3
Kaushal, R. (2002). Information technology and medication
safety: What is the benefit? Quality and Safety in
Health Care, 11(3), 261–265. https://doi.org/10.1136/
qhc.11.3.261
Keller, R., Hartmann, S., Teepe, G. W., Lohse, K.-M.,
Alattas, A., Tudor Car, L., Müller-Riemenschneider, F.,
Von Wangenheim, F., Mair, J. L., & Kowatsch, T.
(2022). Digital Behavior Change Interventions for the
Prevention and Management of Type 2 Diabetes:
Systematic Market Analysis. Journal of Medical
Internet Research, 24(1), e33348. https://doi.org/10.21
96/33348
Klonoff, D. C. (2013). The Current Status of mHealth for
Diabetes: Will it Be the Next Big Thing? Journal of
Diabetes Science and Technology, 7(3), 749–758.
https://doi.org/10.1177/193229681300700321
Landers, C., Vayena, E., Amann, J., & Blasimme, A.
(2023). Stuck in translation: Stakeholder perspectives
on impediments to responsible digital health. Frontiers
in Digital Health, 5, 1069410. https://doi.org/10.3389/
fdgth.2023.1069410
Malasinghe, L. P., Ramzan, N., & Dahal, K. (2019).
Remote patient monitoring: A comprehensive study.
Journal of Ambient Intelligence and Humanized
Computing, 10(1), 57–76. https://doi.org/10.1007/s126
52-017-0598-x
Mantovani, A., Leopaldi, C., Nighswander, C. M., & Di
Bidino, R. (2023). Access and reimbursement pathways
for digital health solutions and in vitro diagnostic
devices: Current scenario and challenges. Frontiers in
Medical Technology, 5, 1101476. https://doi.org/
10.3389/fmedt.2023.1101476
Maurer, M., Wieser, S., Kohler, A., & Thommen, C.
(2022). Sustainability and Resilience in the Swiss
Health System. https://www3.weforum.org/docs/
WEF_PHSSR_Switzerland_EN.pdf
McKinsey. (2021, September). Digitalisierung im
Gesundheitswesen: Die 8,2-Mrd.-CHF-Chance für die
Schweiz. https://www.mckinsey.com/ch/~/media/mck
insey/locations/europe%20and%20middle%20east/swi
Scale-IT-up 2024 - Workshop on Emerging Business Models in Digital Health
850

tzerland/our%20insights/digitization%20in%20healthc
are/digitalisierung%20im%20gesundheitswesen%20%
20die%2082mrdchance%20fr%20die%20schweiz%20
de.pdf
Ong, M. K., Romano, P. S., Edgington, S., Aronow, H. U.,
Auerbach, A. D., Black, J. T., De Marco, T., Escarce, J.
J., Evangelista, L. S., Hanna, B., Ganiats, T. G.,
Greenberg, B. H., Greenfield, S., Kaplan, S. H.,
Kimchi, A., Liu, H., Lombardo, D., Mangione, C. M.,
Sadeghi, B., … Better Effectiveness After Transition–
Heart Failure (BEAT-HF) Research Group. (2016).
Effectiveness of Remote Patient Monitoring After
Discharge of Hospitalized Patients With Heart Failure:
The Better Effectiveness After Transition -- Heart
Failure (BEAT-HF) Randomized Clinical Trial. JAMA
Internal Medicine, 176(3), 310–318. https://doi.org/
10.1001/jamainternmed.2015.7712
Ranes, L. (2020). Remote patient monitoring for adults with
type 2 diabetes. ADCES 2020 Research Abstracts. The
Diabetes Educator, 46(4), 398–406. https://doi.org/
10.1177/0145721720932682
Ruland, C. M. (2002). Handheld Technology to Improve
Patient Care: Evaluating a Support System for
Preference-based Care Planning at the Bedside. Journal
of the American Medical Informatics Association, 9(2),
192–201. https://doi.org/10.1197/jamia.M0891
Shah, S. S., Gvozdanovic, A., Knight, M., & Gagnon, J.
(2021). Mobile App–Based Remote Patient Monitoring
in Acute Medical Conditions: Prospective Feasibility
Study Exploring Digital Health Solutions on Clinical
Workload During the COVID Crisis. JMIR Formative
Research, 5(1), e23190. https://doi.org/10.2196/23190
Sojer, R., Röthlisberger, F., & Rayki, O. (2018). Angebot
und Nachfrage von digitalen Gesundheitsangeboten
(Teil I). Schweizerische Ärztezeitung. https://doi.org/
10.4414/saez.2018.17247
Steinberg, D., Horwitz, G., & Zohar, D. (2015). Building a
business model in digital medicine. Nature
Biotechnology, 33(9), Article 9. https://doi.org/10.103
8/nbt.3339
Stone, R. A., Rao, R. H., Sevick, M. A., Cheng, C., Hough,
L. J., Macpherson, D. S., Franko, C. M., Anglin, R. A.,
Obrosky, D. S., & DeRubertis, F. R. (2010). Active
Care Management Supported by Home Telemonitoring
in Veterans With Type 2 Diabetes. Diabetes Care,
33(3), 478–484. https://doi.org/10.2337/dc09-1012
Ventola, C. L. (2014). Mobile devices and apps for health
care professionals: Uses and benefits. P & T: A Peer-
Reviewed Journal for Formulary Management, 39(5),
356–364.
Zhai, Y., Zhu, W., Cai, Y., Sun, D., & Zhao, J. (2014).
Clinical- and Cost-effectiveness of Telemedicine in
Type 2 Diabetes Mellitus: A Systematic Review and
Meta-analysis. Medicine, 93(28), e312. https://doi.org/
10.1097/MD.0000000000000312
Transforming NCD Business Models in Switzerland: CSS Insurance Perspective
851
