
Exploring the Power of Triple Crown Process Modeling in Healthcare:
Sepsis Case
Camelia Maleki
a
and Frederik Gailly
b
Faculty of Economics and Business Administration, Ghent University, Tweekerkenstraat 2, Gent, Belgium
Keywords:
Patient Care Process, Triple Crown Modeling Approach, Process Improvement.
Abstract:
Effective process modeling plays a pivotal role in optimizing patient care processes within the continually
evolving healthcare landscape. This paper focuses on the application of the Triple Crown standard, which
encompasses the Business Process Model and Notation (BPMN), Case Management Model and Notation
(CMMN), and Decision Model and Notation (DMN), within the context of the sepsis diagnosis process.
Through an in-depth exploration of this case study, the paper uncovers the immense potential of these stan-
dards in empowering healthcare practitioners to streamline workflows, enhance decision-making at critical
junctures, and ensure the delivery of the highest quality care despite the diverse challenges inherent in patient
care processes. By dissecting key dimensions such as flexibility, data and information flow, complexity man-
agement, and decision points, this study provides valuable insights into how the Triple Crown approach can
significantly enhance patient care process models.
1 INTRODUCTION
In today’s intricate healthcare landscape, healthcare
process modeling plays a pivotal role in efficiently
managing the flexibility and complexity inherent in
these processes. It not only aids in identifying
and eliminating inefficiencies, and addressing bottle-
necks but also allows for dynamic adaptation to the
ever-evolving nature of healthcare procedures. Pro-
cess models empower healthcare providers and pol-
icymakers with the ability to make well-informed
decisions, thereby providing a framework for un-
derstanding and responding to fluctuations caused
by emerging medical technologies, shifting patient
needs, evolving regulatory requirements, and other
factors. This enables healthcare professionals to
stay agile, predict potential challenges and opportuni-
ties, and make adjustments to ensure optimal patient
care(Pufahl et al., 2022).
Healthcare organizations are responsible for car-
rying out a variety of processes that vary in their
characteristics and needs, ranging from clinical pro-
cedures like diagnosis and treatment to organizational
and administrative tasks such as scheduling appoint-
ments and registering patients. These processes are
a
https://orcid.org/0000-0002-7818-2559
b
https://orcid.org/0000-0003-0481-9745
not isolated from one another, but rather intercon-
nected and dependent. Patient care processes have
become particularly important in recent years as they
consider both organizational requirements and clini-
cal tasks(Mans et al., 2015). In the patient care pro-
cesses, many sections require healthcare providers to
make decisions based on their knowledge and exper-
tise (Di Ciccio et al., 2015). These parts are dy-
namic, flexible, and often referred to as ”knowledge-
intensive”. However, some tasks follow a specific
workflow or set of instructions, such as regular assess-
ments or performing a specific protocol(Rojo et al.,
2008).
To effectively model a process, it is imperative to
first grasp its priorities and challenges. Lenz et al
(Lenz and Reichert, 2007) conducted an investigation
into the primary challenges associated with support-
ing and representing care processes, taking into ac-
count their unique characteristics. One major issue
arises from the restricted process flexibility inherent
in existing traditional languages. This limitation en-
tails the ability of the implemented process to exe-
cute based on a loosely or partially specified model
that is completed at runtime. (Lenz et al., 2012).
Another concern relates to complexity management.
Since the primary goal of business process diagrams
is to enhance communication among process-related
stakeholders, overly complex diagrams can hinder
516
Maleki, C. and Gailly, F.
Exploring the Power of Triple Crown Process Modeling in Healthcare: Sepsis Case.
DOI: 10.5220/0012394000003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 516-528
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.

their correctness and comprehension. Improper use
of a modeling language regardless of the character-
istics and requirements of a process can result in re-
duced clarity and increased complexity in model.(Jo
ˇ
st
et al., 2019). Moreover, patient care processes de-
pend on medical knowledge and case-specific deci-
sions. This entails that healthcare professionals de-
pend on the amalgamation of the finest accessible ev-
idence, clinical expertise, and patient preferences to
arrive at well-informed decisions. To proficiently ma-
neuver through these processes, it becomes crucial
to establish streamlined information exchange and a
comprehensive depiction of the decision-making as-
pect within process models (Pufahl et al., 2022). In
light of these challenges and requirements, it becomes
evident that relying exclusively on a single model-
ing language may fall short of creating a compre-
hensive model, as different aspects of patient care
processes possess distinct characteristics and prior-
ities. Therefore, it may be essential to employ a
combination of modeling languages to comprehen-
sively capture the patient care process and represent
all its dimensions.(Pufahl et al., 2022; Mulyar et al.,
2008a). One choice for this is the Triple Crown of
OMG, which combines the BPMN (Activity-centric
language), CMMN (Artifact-centric language), and
DMN (Decision-centric language). The Triple Crown
approach is a popular choice due to its comprehensive
nature, adaptability, and standardization. It allows
healthcare providers to model both the workflow-
oriented and knowledge-intensive aspects of a pro-
cess and offers flexibility by allowing organizations
to choose one or more of the standards based on their
specific needs(OMG Healthcare Domain Taskforce,
2020).
This paper aims to shed light on the substantial po-
tential inherent in the Triple Crown standard. By eval-
uating the synergistic capabilities of BPMN, CMMN,
and DMN in enhancing critical aspects of patient care
process models. In our pursuit of evaluating the mod-
eling languages within the healthcare landscape, we
deliberately chose to examine four critical dimen-
sions: flexibility, complexity management, informa-
tion flow, and decision-making due to their fundamen-
tal significance in providing a comprehensive repre-
sentation of patient care processes. These four dimen-
sions are intricately interconnected and collectively
underpin the success of healthcare process modeling.
By focusing our research on these dimensions, we aim
to provide a comprehensive assessment of the Triple
Crown standard’s applicability and effectiveness in
the patient care processes. Ultimately, our goal is to
empower healthcare practitioners with the tools they
need to navigate the complex and ever-changing land-
scape of patient care, thereby enhancing the quality of
care delivered to patients.
2 BACKGROUND
The ”OMG Triple Crown” refers to the three ma-
jor standards developed by the Object Management
Group (OMG) for business process management
(BPM), decision management (DM), and case man-
agement (CM). These three standards are the Busi-
ness Process Model and Notation (BPMN)(OMG,
2011), the Decision Model and Notation (DMN), and
the Case Management Model and Notation (CMMN)
(OMG, 2016). Together, they provide a comprehen-
sive framework for modeling, analyzing, and manag-
ing complex business processes, decisions, and cases
(OMG Healthcare Domain Taskforce, 2020)
2.0.1 BPMN in Healthcare
Several studies have concentrated on the analysis of
BPMN’s benefits within the healthcare sector, with
a focus on its application in specific medical scenar-
ios, as discussed below. Rolon et al. (Rol
´
on et al.,
2008) employed BPMN to visualize and enhance pro-
grammed surgical patient processes. Rojo et al. (Rojo
et al., 2008) conducted an examination of the utility
of BPMN in modeling anatomic pathology processes.
In a separate study (Barbagallo et al., 2015), BPMN
is used to model standard operating pathways, to ana-
lyze the challenges related to operating room planning
and scheduling.
2.0.2 CMMN in Healthcare
In the work of (Herzberg et al., 2015), they present
an approach aimed at addressing the requirements of
a flexible healthcare process through the utilization of
CMMN. Additionally, they explore the establishment
of case monitoring and analysis by combining event
processing and case management. Another relevant
study, as proposed in (Mei et al., 2014), introduces a
CMMN-based model for care pathways in CHF (con-
gestive heart failure) processes.
2.0.3 Combination of BPMN, CMMN, and
DMN in Healthcare
In this section, we highlight studies that have lever-
aged a combination of OMG standards to model
healthcare processes. It’s important to note that
DMN cannot function independently and is typically
employed in conjunction with other modeling lan-
guages. For example, Wiemuth et al. (Wiemuth
Exploring the Power of Triple Crown Process Modeling in Healthcare: Sepsis Case
517
et al., 2017) demonstrated the utilization of a com-
bination of BPMN, CMMN, and DMN to model non-
deterministic medical processes. Likewise, Junger et
al. [2] conducted a comparative analysis of the ca-
pabilities of BPMN, CMMN, and a combination of
both notations in representing adaptable surgical pro-
cedures. The evidence-based decision-making is ex-
plored in (Combi et al., 2016). This study serves
as the foundation for the methodology discussed in
(Combi et al., 2017), which recommends the com-
bination of BPMN and DMN to depict decision-
intensive healthcare processes( particularly chronic
care processes).
Despite prior research on the utilization of BPMN,
CMMN, and DMN in the healthcare domain, a void
persists in the literature when it comes to applying all
three notations (the Triple Crown approach) within
healthcare processes and assessing its efficacy. This
paper endeavors to bridge this gap by investigating
the Triple Crown approach within the realm of health-
care process modeling. Through a detailed analysis
of critical facets and an assessment of its capacity to
optimize workflows and elevate decision-making, this
study contributes to the growing body of literature on
healthcare process modeling.
3 METHODOLOGY
In this section, we have outlined a methodology that
facilitates the creation of a healthcare process model
utilizing the triple crown standard.
1. Define the scope of the process
(a) What is the goal of the process?
(b) What is the start and end point?
2. Define the key performance indicators. they
should reflect the critical success factors and the
value proposition of your process.
3. Define the process
(a) List of Activity groups, Artifacts, Events, and
Goals that are used in the Model
(b) Identify the relationship between elements
4. Choose the appropriate modeling language for
each part of the process, taking into consideration
the content captured and the key performance in-
dicators (KPIs)
5. Create the first draft of the models
6. Continuously refine and validate the model until
it is functional. Some techniques are listed below:
(a) Expert Review: Engage healthcare profession-
als and experts
(b) Comparative Analysis: Compare the model
with existing documentation and guidelines.
(c) Regulatory Compliance: Ensure that the model
complies with relevant healthcare regulations
and standards
(d) Audit Trails and Documentation: Maintain
thorough documentation of the model’s devel-
opment and validation process
(e) Simulation: If possible use simulation software
to execute the process model under different
scenarios
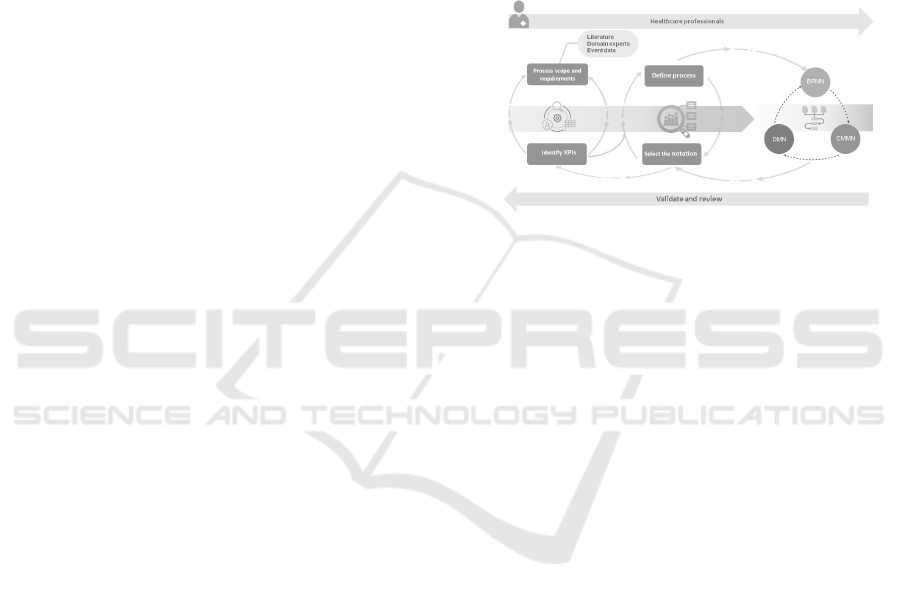
Figure 1: Main steps of the proposed design methodology.
4 SEPSIS CASE STUDY
In many situations, including the sepsis diagnosing
process, there are no documented procedures that dic-
tate the way in which the care process is undertaken.
Consequently, there is a need to discover the process
from first principles. During this phase of the method-
ology, the aim is to gain a thorough understanding of
the current healthcare process.
The study aimed to comprehensively understand
the sepsis diagnosing process in healthcare by gather-
ing data from various sources. Three primary meth-
ods were employed: event logs from a reputable
Dutch hospital, clinical guidelines, and interviews
with healthcare professionals. The event logs, con-
sisting of 15,214 recorded events related to 1,050 sep-
sis cases, were obtained from the hospital’s enterprise
resource planning (ERP) system. While valuable,
these event logs did not cover all aspects of the sepsis
process. To address this limitation and obtain a more
holistic perspective, interviews with healthcare pro-
fessionals and relevant clinical guidelines were uti-
lized. This combined approach provided nuanced de-
tails that enhanced the analysis, resulting in a rich
dataset for a thorough exploration of the sepsis pro-
cess. The diverse data sources enabled the researchers
to model and evaluate different aspects of the sepsis
process, highlighting the strengths and limitations of
various modeling languages.
HEALTHINF 2024 - 17th International Conference on Health Informatics
518
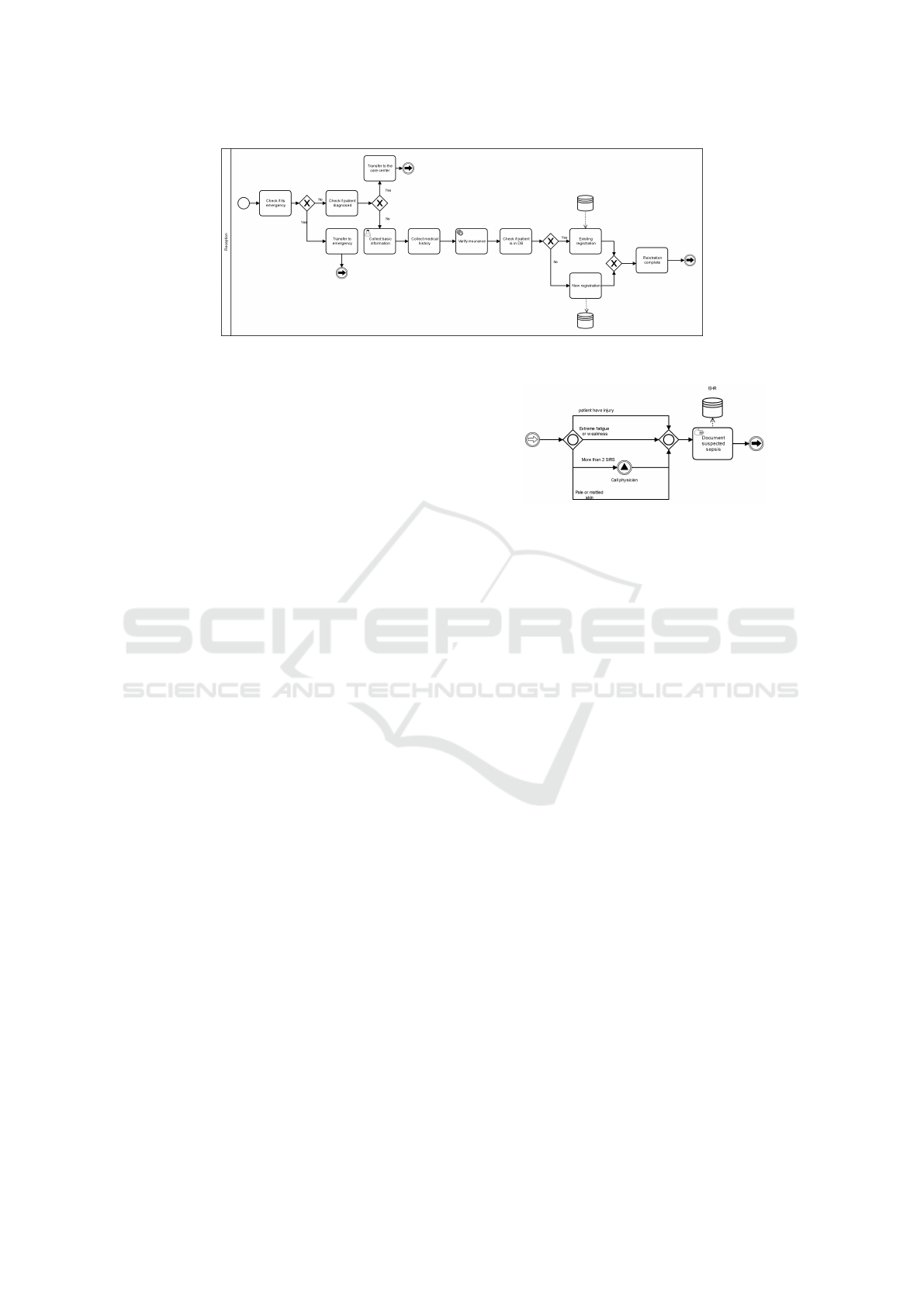
Figure 2: Patient administration process with BPMN.
4.1 Patient Administration
Patient administration is the functional, structural
consolidation of patient registration, admitting, and
other patient-generated activities in the hospital. It
is a simple and concise process (Table 2) requiring
no specific knowledge and low levels of flexibility.
This part of the process begins when a patient arrives
through the acceptance process in the Entrance Room
and ends with sending the patient for sepsis triage
(Figure 2).
The choice to implement BPMN for the patient
registration process was based on its ability to effec-
tively capture structured, sequential, and task-centric
processes. BPMN aligns well with the distinct activ-
ity groups in patient registration, offering a straight-
forward representation of tasks. In contrast, CMMN
introduces additional elements like cases, stages, and
milestones, leading to unnecessary complexity for a
simple patient registration process. BPMN’s flexi-
bility patterns, incorporating gateways and subpro-
cesses, make it more suitable for handling variations
in patient registration, whereas CMMN requires nav-
igating multiple paths and outcomes, making the pro-
cess more challenging to understand.
4.2 Patient Diagnostic Exams
Upon patient registration, the nurse prioritizes pa-
tients by severity, entering triage information into the
electronic health record (EHR). If sepsis is suspected,
the nurse initiates the formal sepsis pathway, docu-
menting the start in a clinical note in the EHR, and
promptly communicates with the first available physi-
cian. This process primarily involves documenting
patient situations, categorized as a structured and rou-
tine process with low flexibility and complexity. Con-
sequently, the decision was made to model this part
using BPMN.
In the second and main part of the diagnosis pro-
cess, the physician assesses the patient’s condition,
Figure 3: First part of diagnose process with BPMN.
drawing on clinical skills, patient information, and
diagnostic testing to ensure an accurate evaluation.
The diagnosis process involves gathering information
and employing clinical reasoning to identify the pa-
tient’s health problem. This process, as highlighted
by Rzepinski et al. (Rzepi
´
nski, 2007), is not entirely
predictable and demands flexible execution. It com-
mences with initial examinations and patient inter-
views, concluding with the documentation of the di-
agnostic report.
The issue here is that the specific sequence and
set of activities in the patient examination process do
not follow a particular script and order, but rather are
based on a diagnostic procedure (e.g., information
discovered in one step can drastically alter the next
set of steps). In BPMN, we can represent this pro-
cess as an ”ad hoc subprocess” which is a group of
tasks designed for handling a specific case and can be
executed in any order (Ye et al., 2008). While both
BPMN ad hoc sub-processes and CMMN tasks can
involve tasks without a predefined order, There are
some limitations of BPMN ad hoc sub-processes in
comparison with CMMN tasks. Here are some limi-
tations of BPMN ad hoc sub-processes:
• Unpredictable Flow: In an ad hoc sub-process,
the exact sequence of activities is not predefined.
This can make it challenging to grasp the overall
process flow, as the order of activities might vary
from instance to instance.
• Variability: With the possibility of repeated ac-
tivities and different ordering, the number of po-
tential paths through the process can grow signifi-
Exploring the Power of Triple Crown Process Modeling in Healthcare: Sepsis Case
519
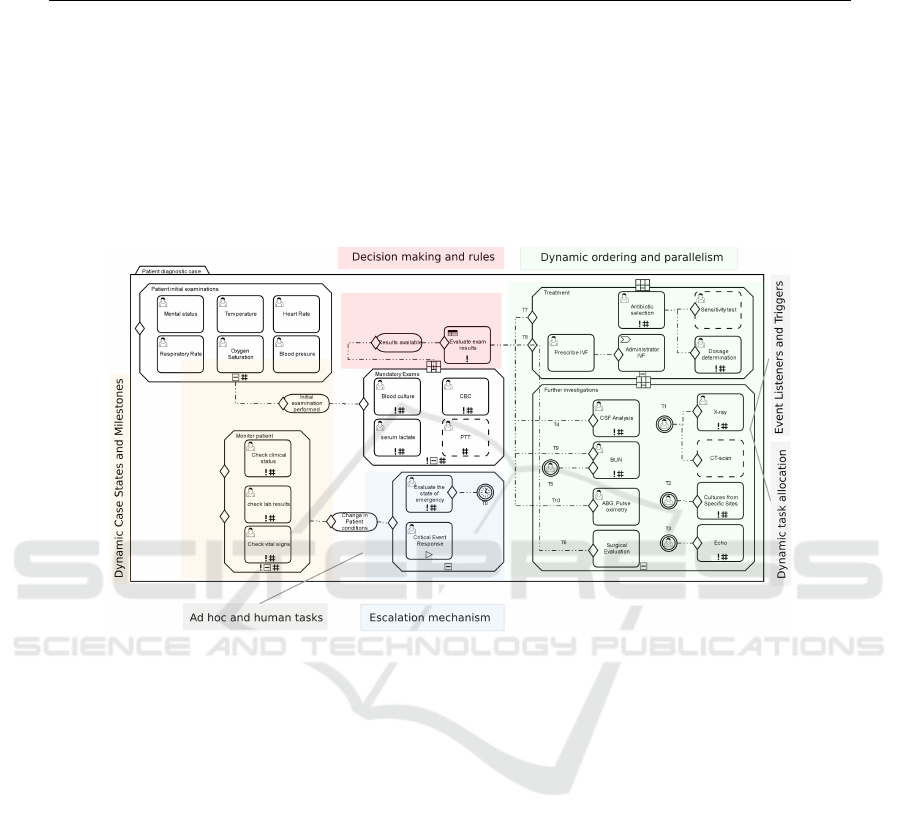
Table 1: Events and response activities after evaluating the results.
ID Event description Response
T0 10 minutes timer event notify the care staff to evaluate the patient’s status
T1 Alert for respiratory symptoms Doing Chest X-ray and/or CT scan
T2 Request culture Culture from a specific site
T3 Alert: Cardiovascular instability Echo exam
T4 High risk: Brain infection CFS analysis
T5 High risk: Request for Dialysis Dialysis
T6 surgical intervention is a consideration evaluation by a surgical team to assess the need for surgery
T7 Alert: presence of infection Prescribe Antibiotics
T8 Alert: have hypertension Administrator IVF
T9 Alert: renal failure BUN exam
T10 Alert: decreased oxygen saturation ABg, Pulse oximetry
Figure 4: Patient exam sub-process with CMMN.
cantly, making it more difficult to understand and
analyze the process as a whole.
• Diagram Clutter: When activities are not con-
strained to a predefined sequence, the diagram
can become cluttered with various arrows indicat-
ing conditional flows and potential transitions be-
tween activities, making the visual representation
more complex.
• Loss of Structure: Traditional BPMN diagrams
have a clear structure with defined start and end
points. Ad hoc sub-processes introduce a level of
non-linearity that might blur the structure, espe-
cially when used extensively.
• Cognitive Load: Readers of the diagram need
to mentally keep track of potential sequences and
conditional flows, which increases the cognitive
load required to understand the process.
• Limited Standardization: Ad hoc sub-
processes can be interpreted and modeled differ-
ently by different people, leading to inconsisten-
cies in understanding
We will investigate how CMMN can address
BPMN limitations. As depicted in Figure 4, we mod-
eled investigations that are performed for sepsis ex-
ams in CMMN. The model includes four main stages:
Mandatory exams, patient initial exams, treatment,
and further investigation. All stages are initiated ac-
cording to the triggering event that represents the in-
cident escalation. The first stage in the model is to
”perform an initial exam” which is depicted as 6 hu-
man tasks. The purpose of these tasks is to gather
real-time information about patient vital signs. Based
on the collected information from this stage and per-
forming the exams in the ”mandatory exams” stage,
the patient’s situation is evaluated through a Decision-
Task called ”evaluate exam results”. This task can
be modeled with a DMN decision table. This task
contains the events and their corresponding decisions
(response activity) based on the patient exam results
(T4, T5, T9, etc.) (Table 3). For example, the T7.
The presence of infection initiates the treatment stage,
which includes a Human Task called ”antibiotic se-
lection” and ”dosage determination”. The next stage
HEALTHINF 2024 - 17th International Conference on Health Informatics
520
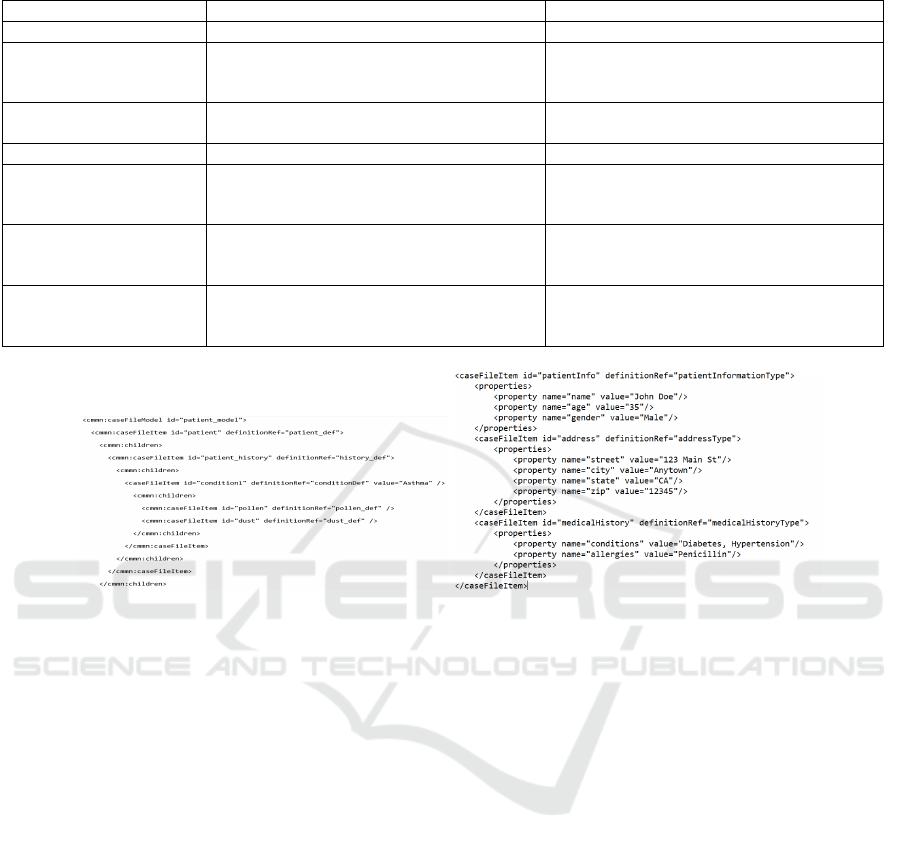
Table 2: Comparing the data modeling capabilities languages.
Measures BPMN
CMMN
collections
Data Object with a ”Collection” property CaseFileItem used to represent collections
Relationships By Data Associations
Elements like association, dependency, re-
quired rule, and onPart condition
Meta data
Can be represented by annotations
CaseFileItemDefinition can be used to rep-
resent metadata
Hierarchical data
BPMN can not represent hierarchical data By using Case File Items
Object oriented data
structure
BPMN is not designed to model object-
oriented data structures
using Case File object that is a container to
hold data and other objects related to a par-
ticular case instance
Complex data structures
BPMN is not well-suited for complex data
structures that involve multiple data types
using caseFileItem and PlanItem
lifecycle
BPMN does not have a specific notation to
represent lifecycles
CMMN can manage various states a case
file item goes through, like ”update”, ”re-
place”, ”add”
Figure 5: Simple example of hierarchical and nested data using casefileitem.
of our investigation involves addressing various sce-
narios where patients may require additional exami-
nations triggered by different event escalations. For
instance, in the case of T4 (high risk: Brain infec-
tion), a critical Human Task must be executed: CPS
analysis.
The inherent flexibility mechanisms of CMMN,
exemplified in Figure 4, serve as valuable tools for ac-
commodating diverse scenarios and variations within
a process model. The escalation mechanism allows
the process to adapt by escalating tasks or cases when
predefined conditions are met, ensuring timely res-
olution. Ordering and parallelism offer agility to
manage tasks sequentially or concurrently. Ad hoc
and human tasks permit the on-the-fly inclusion of
tasks as needed, while dynamic task allocation en-
sures dynamic assignment of the right resources based
on changing requirements. Conditional expressions
in ”ifparts” provide dynamic control over case ele-
ment activation and completion. Milestones facili-
tate progress tracking and action triggering, and dis-
cretionary tasks offer optional activities that adapt
to case-specific requirements.(Routis et al., 2020;
Zensen and Kuster, 2018). These mechanisms col-
lectively eliminate the need to create multiple process
models, streamline processes, and enhance the adapt-
ability of a process(Andree et al., 2022; Routis et al.,
2023; Kurz et al., 2015).
This example demonstrates how CMMN success-
fully addresses the mentioned issues. for example,
CMMN leverages a combination of case context man-
agement, case stages, milestones, event listeners, dy-
namic task allocation, and flexible dependencies, to
effectively manage maintenance challenges and ad-
dress the unpredictable flow within case management
scenarios.
One more challenge during the triage and diag-
nostic process is ensuring the quality of the data and
information during the process(Albahri et al., 2018).
Representing complex data structures, such as hierar-
chical or nested data structures like trees or graphs,
with BPMN data objects can be difficult. The patient
exam results, for example, contain essential details
about different exams, and other nested elements that
are critical for healthcare staff to access with the high-
est level of accuracy and completeness. We presented
a comparison of the data modeling capabilities of both
CMMN and BPMN This example demonstrates how
CMMN successfully addresses the mentioned issues.
for example, CMMN leverages a combination of case
Exploring the Power of Triple Crown Process Modeling in Healthcare: Sepsis Case
521

context management, case stages, milestones, event
listeners, dynamic task allocation, case plans, ad hoc
tasks, and flexible dependencies, to effectively man-
age maintenance challenges and address the unpre-
dictable flow within case management scenarios. or
for managing diagram clutter the notation includes
features like stages and plans that help organize and
structure tasks within a case.
An additional challenge during the triage and di-
agnostic process is ensuring the quality of data and
information (Albahri et al., 2018). Representing com-
plex data structures, such as hierarchical or nested
data structures like trees or graphs, with BPMN data
objects can be challenging. For instance, patient exam
results contain crucial details about various exams
and other nested elements critical for healthcare staff
to access with the highest level of accuracy and com-
pleteness. We provided a comparison of the data mod-
eling capabilities of both CMMN and BPMN.(Gagne,
2016; Von Rosing et al., 2014; Neskovic and Kirch-
ner, 2016). As shown in the table although both
BPMN and CMMN offer data modeling capabili-
ties, CMMN is particularly suited for handling intri-
cate data structures in case management procedures
and offers more sophisticated elements for model-
ing complex care process data. In addition, CMMN
comes with built-in access control capabilities and au-
dit trails including user roles and permissions, case
and task ownership, and user-defined access control
rules. Consequently, CMMN offers a range of fea-
tures that can aid in preserving the integrity, and ac-
cessibility of patient data.
4.3 Diagnose Process
The final diagnostic step involves determining sepsis
severity, a task heavily reliant on physician expertise
and intricate decision-making. While CMMN is ver-
satile for various processes, it may have limitations in
modeling complex decision scenarios. Though it sup-
ports simple decision-making with sentry and event
elements, CMMN might not be optimal for intricate
decision-making with multiple conditions and rules.
In this phase, models are created using standard
BPMN and DMN. Executable standard BPMN el-
ements are employed, with decision-making rules
translated into first-order logic (FO(·)). The challenge
encountered during this part is the difficulty in mod-
eling certain rules using standard BPMN constructs
due to their complex logical conditions which can-
not be easily represented through a sequence of tasks
and gateways. While it may be possible to model
these rules using more advanced BPMN constructs,
such as nested subprocesses or complex gateways, it
would likely result in a highly complex and difficult-
to-understand diagram that may not be practical for
a real-world scenario. As an example, consider the
following rule:
∀x[patient](Fever(x) ∧W BC(x) ∧Con f irmedin f ection(x)
∧(SBP(x) < 90 ∧ (HoT N(x) ∨ Lac > 4))∧ (∃y[labtest]
(ordered a f ter(y, x) ∧ ∆Lac(y, x) ≥ 0.5 ∧ ∆SBP(y, x) ≤ 20)∨
(∃z[medication](ordereda f ter(z, x) ∧Vasopressor(z)∧
∆Dose(z, x) ≥ 0.5 ∧ ∆SBP(z, x ) ≤ 20)))
→ Re f ractorysepticshock(x)
This rule states that if a patient has a fever, positive
blood cultures, and a confirmed infection, and their
systolic blood pressure is below 90 mmHg, and either
they have evidence of tissue hypoperfusion (HoTN)
or lactate levels above 4 mmol/L, and they have ei-
ther experienced a significant increase in lactate levels
or a decrease in systolic blood pressure by 20 mmHg
or more after receiving vasopressor medication, then
they should be diagnosed with refractory septic shock.
There are a few technical issues with modeling this
rule in BPMN:
• Expressing Temporal Relationships: BPMN
can express temporal relationships between activ-
ities using gateways and events, but it can be diffi-
cult to represent complex temporal relationships,
such as ”orderedafter” in the rule.
• Expressing Logical Conditions: BPMN can ex-
press simple logical conditions using gateways
and events, but more complex logical conditions
in the rule, can be difficult to represent (e.g., the
change in lactate levels (∆Lac) between ”y” and
”x” is greater than or equal to 0.5, and the change
in systolic blood pressure (∆SBP) between ”y”
and ”x” is less than or equal to 20).
• Expressing Quantitative Conditions: BPMN is
not designed to represent quantitative conditions,
such as ∆Lac(y, x) ≥ 0.5. While it may be pos-
sible to use data objects or variables to represent
these values, it can be less intuitive than express-
ing them in a decision table.
• Handling Nested Expressions: The rule contains
nested expressions, such as the combination of
”OR” and ”AND” operators within parentheses.
While it is possible to represent nested expres-
sions in BPMN, it can make the diagram more
complex and harder to read.
However, this rule can be represented clearly and
concisely in a DMN decision table by breaking it
down into smaller logical expressions and assigning
them to decision inputs and outputs (Figure 6).
To compare BPMN and DMN in decision model-
ing, we have decided to limit our scope to a set of
rules for the sepsis severity diagnostic process that
HEALTHINF 2024 - 17th International Conference on Health Informatics
522
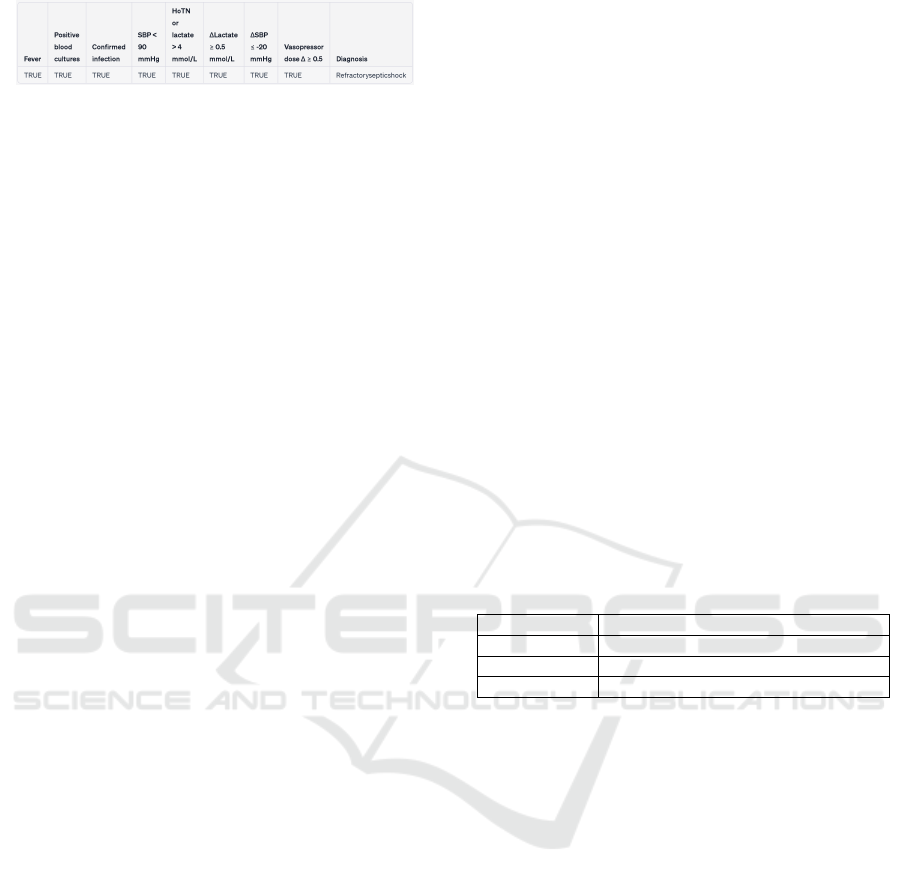
Figure 6: Decision table with the rule for refractory septic
shock.
can be modeled by both languages, excluding very
complex rules that BPMN may not be capable of
modeling. We have defined specific rules for diag-
nosing the severity of sepsis based on clinical guide-
lines, sepsis protocols, and insights gathered from in-
terviews with healthcare experts (Dugar et al., 2020;
Taj et al., 2022). These rules serve as a framework
to assess the severity of sepsis cases and guide the
decision-making process in our model. Below is a list
of some examples of these rules:
∀x[patient](Fever(x) ∧W BC(x) ∧ SBP(x) > 90 → SIRS(x))
∀x[patient](Fever(x) ∧W BC(x) ∧Con f irmedin f ection(x)
∧SBP(x) > 90 ∧ Lac < 2 → Sepsis(x))
∀x[patient](Fever(x) ∧W BC(x) ∧Con f irmedin f ection(x)
∧SBP(x) < 90 ∧ Lac > 4 → Septicshock(x))
∀x[patient](Fever(x) ∧W BC(x) ∧Con f irmedin f ection(x)
∧SBP(x) < 90 ∧ HoT N(x) ∧ Lac > 4 → Septicshock(x))
∀x[patient](Fever(x) ∧W BC(x) ∧Con f irmedin f ection(x)
∧SBP(x) < 90 ∧ 2 < Lac < 4 → Seversepsis(x))
∀x[patient](Fever(x) ∧W BC(x) ∧Con f irmedin f ection(x)
∧SBP(x) < 90 ∧ 2 < Lac < 4 ∧ OD(x) → Septicshock(x))
BPMN allows representing decisions and their im-
pact or consequence respectively. However, BPMN
is not meant to represent the detailed decision logic
since modeling the decision logic often results in an
Intricate mess of nodes and connections (see Figure
8). According to integrated BPMN and DMN mod-
eling, decisions are not mapped to control flow ele-
ments. Rather, decisions are externalized into a sepa-
rate DMN decision model that can be invoked by the
process.
To calculate decision table values, it is essen-
tial to outline the requirements for decision-making,
graphically represented in a Decision Requirements
Diagram (DRD). The DRD comprises four element
types: decision, input data, business knowledge
model, and knowledge source. Oval shapes like ”Pa-
tient history” represent input data, while ”evaluate pa-
tient result” and ”identify sepsis severeness” are de-
cision nodes. Process resources, such as physicians
and guidelines, are considered knowledge sources, di-
rectly influencing decision-making. Text annotations
can serve as knowledge sources or input data, depend-
ing on their information content.
Figure 7 provides an overview of decision model
execution. In the table’s upper left corner, ”unique”
signifies the defined hit policy for the decision table,
indicating that only one of the rows below can be true
when a decision is required.
5 DISCUSSION
In this section, we will explore our approaches in
terms of their capacity to handle complexity and flex-
ibility.
5.1 Complexity Management
Analyzing BPMN, CMMN, and DMN reveals the po-
tential for a more comprehensive model through their
integration. However, our focus here is to assess
whether the combined model is more complex than
the standalone BPMN model. Currently, no widely
accepted unified complexity metric exists due to the
distinct purposes, elements, and scenarios these nota-
tions involve in business process management and de-
cision modeling. Each notation has unique elements
and objectives, making a universally applicable com-
plexity metric challenging. One potential solution
is adapting existing complexity metrics like nesting
depth and control flow complexity (CFC) to consis-
tently assess the impact of using these languages to-
gether.(Kluza and Nalepa, 2012). Table 3 summarizes
metrics used for complexity measurement.
Table 3: Process model complexity metrics.
metrics Focus
NOA, NOAC Measure the activity complexity
CFC Measure the control-flow complexity
Depth Evaluate the nesting of the process
The NOA metric calculates activity complexity
and was inspired by lines of code (LOC) metric.
NOAC metric considers both activities and control-
flow elements for well-structured models. The for-
mula of CFC that captures the complexity of XOR-
split, OR-split, and AND-split constructs is as fol-
lows:
CFC
XOR−split
(a) = f an − out
a
(1)
XOR-split CFC is determined by the number of in-
duced states introduced with the split. For XOR splits,
the complexity corresponds to the fan-out of the split.
CFC
OR−split
(a) = 2
f an−out(a)
− 1 (2)
OR-split CFC is also determined by the number of
induced states introduced with the split.
CFC
AND−split
(a) = 1 (3)
For AND splits, the complexity is simply 1. Lastly,
Depth is defined as the nesting of the process model.
If there is a split gateway, the depth is increased with
one. If there is a join gateway, the depth is decreased
with one. The cumulative sum is taken and the max-
imum of the cumulative sum is calculated for each
Exploring the Power of Triple Crown Process Modeling in Healthcare: Sepsis Case
523
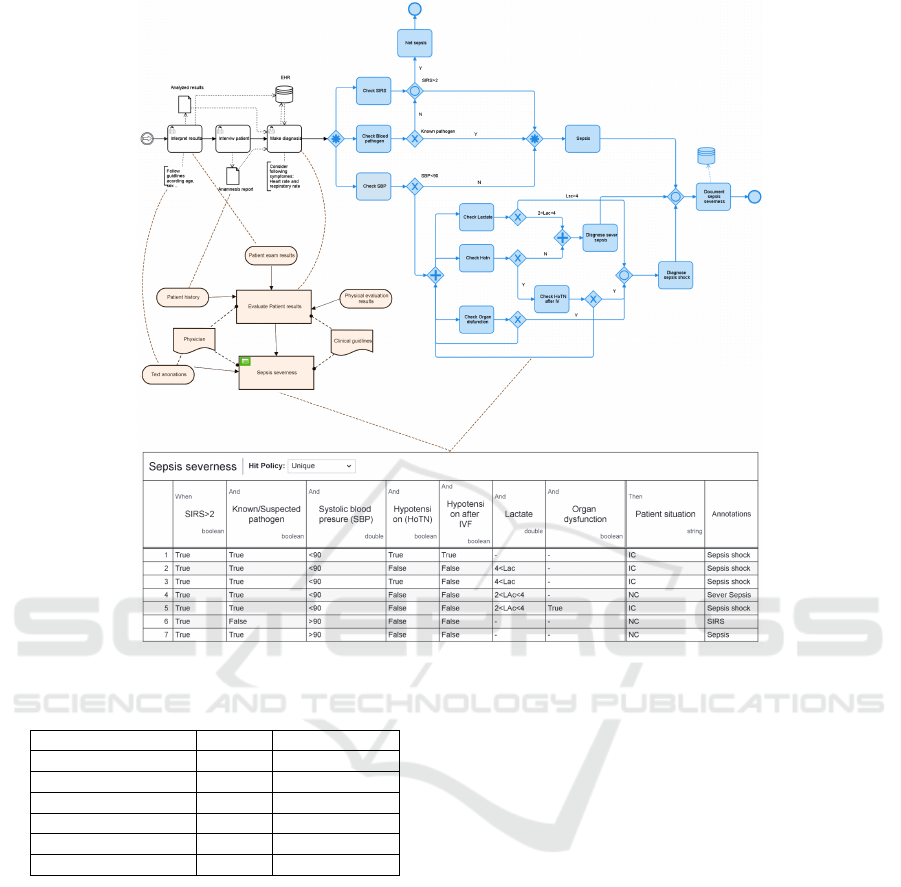
Figure 7: Transform a BPMN model into DMN.
Table 4: Complexity metrics comparison.
Complexity metrics BPMN BPMN+DMN
NOA, NOAC 27, 56 14, 30
CFC XOR-Split 19 7
CFC OR-split 15 9
CFC And gateway 2 0
Total CFC 36 16
Depth 5 3
path. The nesting depth is the maximum of each path
value.
Table 4 shows that combining BPMN and DMN
reduces process model complexity. According to
(S
´
anchez-Gonz
´
alez et al., 2011), a process model
with CFC OR-split decision nodes exceeding a value
of 14 can be incomprehensible; our BPMN process
had a value of 15. After integrating DMN, the value
decreased to 9, making it understandable. In sum-
mary, the BPMN-DMN combination streamlines pro-
cess model complexity by reducing gateways and
flows. However, it introduces new intricacies related
to additional decision models. Despite this, the added
complexity shifts from the process model to the deci-
sion model. DMN decision tables facilitate the identi-
fication of overlapping and missing rules, allowing for
rule reordering and consolidation, leading to a more
concise decision-making process in the workflow, un-
like situations with complex sequential structures.
To perform a meaningful comparison of complex-
ity between BPMN and CMMN, it’s crucial to ensure
that we have an identical process model represented
in both notations. While we already have the patient
registration process represented in both languages as a
structured process, to assess the complexity of a flex-
ible process model, we need to recreate what we’ve
modeled in CMMN using BPMN. However, model-
ing the entire CMMN model within BPMN poses a
formidable challenge, as certain elements are inher-
ently unsuitable for representation in BPMN. As a re-
sult, we have opted to narrow our focus to a specific
part of the CMMN model depicted in Figure 5, which
we will then represent using BPMN notation. (Figure
8).
Given these fundamental distinctions between
BPMN and CMMN, many established complexity
metrics may not be directly applicable to CMMN. For
example, one common metric is Activity Complex-
ity (AC), which quantifies the nodes within a process
HEALTHINF 2024 - 17th International Conference on Health Informatics
524
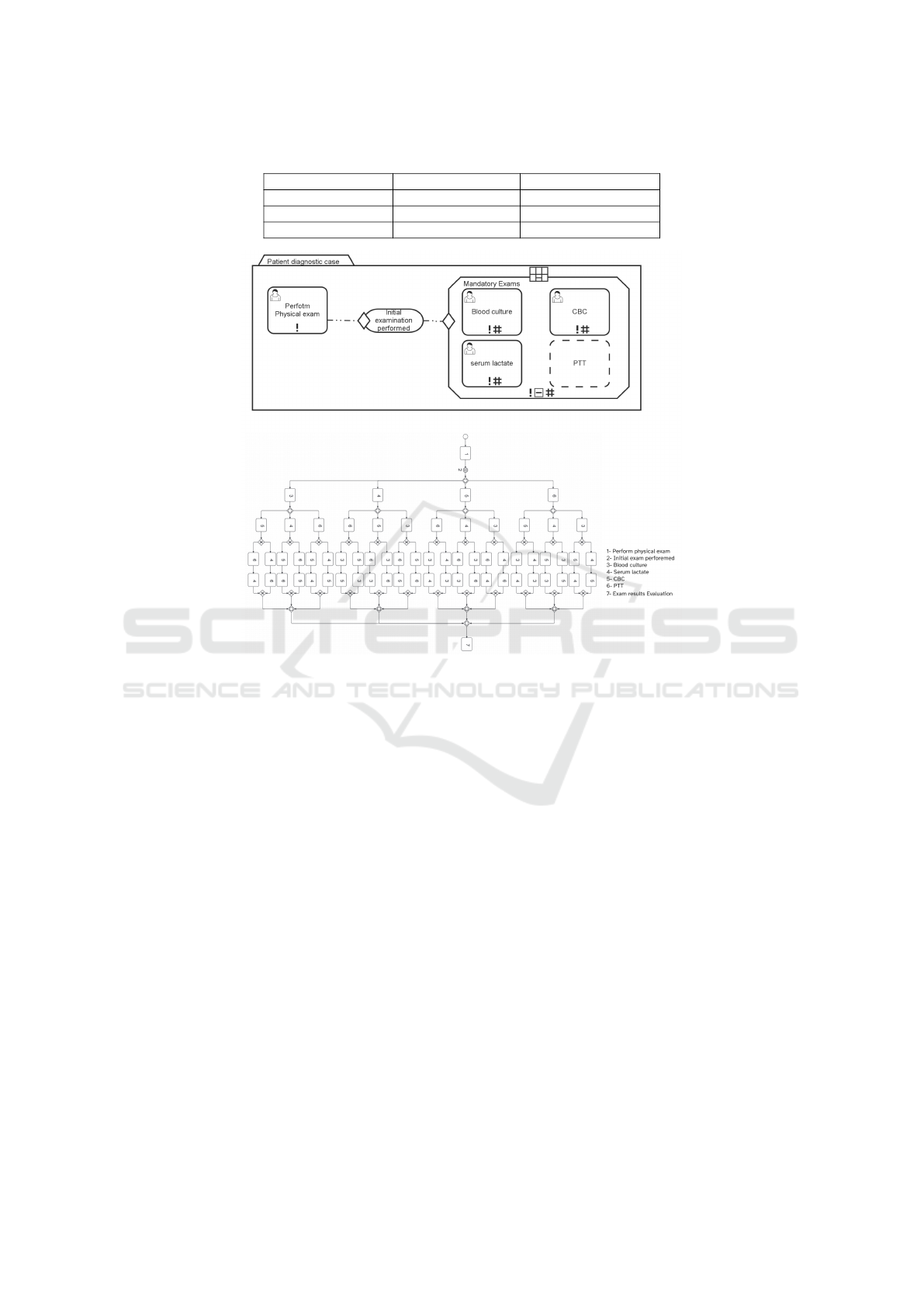
Table 5: Complexity metrics comparision.
Flexible Structured
Complexity metrics BPMN CMMN BPMN CMMN
AC 66 5 16 14
CNC 1.28 0.83 1 1.07
Figure 8: Comparison of BPMN and CMMN complexity in a flexible process.
graph. Assuming that all elements in a CMMN model
can be considered as nodes, AC can be calculated for
both BPMN and CMMN models (Marin, ). However,
certain complexity metrics, like Control Flow Com-
plexity (CFC), do not find relevance in CMMN. This
is because CMMN lacks equivalents to the AND, OR,
or XOR nodes present in BPMN. Therefore, for com-
plexity measurement, we utilize Activity Complexity
(AC) to count the activities. Additionally, we em-
ploy a complexity metric known as the Coefficient
of Network Connectivity (CNC) exploits the notion
of connectivity between elements to quantify struc-
tural complexity. Inspired by Graph theory, the given
metric explores the relation of the number of Arcs to
the number of Nodes. Higher values of it reveal a
dense model, which is more likely to contain errors
since the modeler has to perceive more connections
between nodes than in a model that is less dense. In
this metric, all activity elements are counted as nodes,
and all connectors are counted as arcs.
CNC = Arcs ÷ Nodes (4)
In CMMN, we assume elements that represent
various types of relationships in CMMN, including
Entry Criteria, Exit Criteria, On-Part Relationships,
and sentries, as connectors.
Figure 11 illustrates that even a small segment
of a CMMN model can become intricately complex
when translated into the context of BPMN, resulting
in 4! different execution sequences for each sequen-
tial ordering of activities. This unnecessary complex-
ity, combined with potential limitations in expressive-
ness, can hinder process model maintainability, re-
quiring multiple adjustments. While modeling flex-
ible processes in CMMN may reduce the number of
activities and overall process model density, a com-
parison of CMMN and BPMN complexity in a struc-
tured process reveals no notable difference in AC and
CNC metrics between the two models. Consequently,
CMMN not only fails to reduce complexity in struc-
tured processes but also introduces additional com-
plexities to the model.
It is undeniably true that CMMN and DMN in-
troduce additional layers of complexity to the overall
model. Nevertheless, when dealing with knowledge-
intensive or decision-centric processes, attempting to
replicate the quality of CMMN or DMN using BPMN
invariably results in heightened complexity, and a di-
Exploring the Power of Triple Crown Process Modeling in Healthcare: Sepsis Case
525
Table 6: Catalog of flexibility patterns.
Flexibility pattern CMMN BPMN Flexibility pattern CMMN BPMN
Flexible initiation Flexible reordering
Alternative entry-points + + Interleaving + +
Entrance skip + - Swap - -
Undefined entry + - Momentary reordering - -
Momentary entry change - - Permanent reordering + \ - -
Permanent entry change - - Flexible elimination
Flexible termination Task skip + \ - -
Alternative exit points + + Foreseen bypass + +
Termination skip + + \ - Momentary task elimination - -
Undefined exit + - Permanent task elimination - -
Momentary exit change - - Flexible extension
Permanent exit change - - Task invocation + -
Flexible selection Late creation + \ - -
Choice + + Momentary task insertion + \- -
Task substitution - - Permanent task insertion - -
Late selection + - Flexible Repetition
Permanent choice insertion + \ - - Redo + \ - -
Momentary choice insertion + \ - - Momentary loop insertion + \ - -
Flexible Concurrency Iteration + +
Parallelism + + Permanent loop insertion - -
Momentary Task Parallelization - -
Parmanent Task Parallelization - -
minished level of overall quality. In some cases, it
may even fall short of the comprehensiveness offered
by CMMN or DMN models. Therefore, it is impera-
tive that we exercise caution and judiciously employ
these modeling approaches only in situations where
they can yield optimal efficiency and performance.
5.2 Flexibility
Flexibility, particularly in the context of processes,
has undergone extensive exploration in academic re-
search, leading to the introduction of numerous tax-
onomies. One of the most comprehensive taxonomies
is presented by Mulyar et al. (Mulyar et al., 2008b).
This taxonomy delineates two types of process flexi-
bility: flexibility during design time, which addresses
foreseeable changes accommodated in modeled pro-
cess schemas, and flexibility during runtime, allowing
alterations to the process instance after initiation. Or-
ganized based on this taxonomy, patterns are grouped
into eight distinct categories (Table 6). These pat-
terns facilitate high-level structural changes in pro-
cess models, encompassing actions such as adding,
deleting, selecting, or relocating activities and process
fragments.
BPMN, in its traditional form, is a static model-
ing language that defines processes at design time. It
is not inherently designed to handle dynamic or run-
time changes to process structures. So it can just han-
dle patterns like ”choice” by using gateways to al-
low the selection of one of several alternative tasks
at design time. CMMN offers a robust framework
for modeling and adapting knowledge-intensive pro-
cesses, providing flexibility patterns for managing dy-
namic processes. It allows for adding, deleting, mov-
ing, and adapting activities and process fragments at
a high level of abstraction. However, there are sce-
narios where CMMN may not fully capture the dy-
namic and unpredictable nature of certain processes.
It is not designed to provide a high level of flexibility
in modifying the case model at runtime. CMMN in-
troduces discretionary elements, allowing tasks and
stages to be manually activated during case execu-
tion, enabling execution-time planning for handling
unpredictability. These mechanisms offer some run-
time adaptability like ”late selection”, ”late creation”
or ”momentary choice insertion”. However, their ap-
plication relies on predictions made during the de-
sign phase, making CMMN most suitable for scenar-
ios requiring flexibility within the originally designed
case structure. For extensive runtime changes or sit-
uations involving unpredictable events, extreme vari-
ability, emergent behaviors, and rapid changes, alter-
native workflow or process management systems may
be more appropriate
The sepsis diagnosis process, unlike emergency
room processes, is not entirely unstructured. Many
potential variations and changes in these processes
can be predicted during the design phase, based on
clinical guidelines and insights from domain experts.
Here are key flexibility patterns crucial to this pro-
cess:
• Late Selection: Essential when test results or pa-
HEALTHINF 2024 - 17th International Conference on Health Informatics
526

tient conditions evolve over time, late selection is
crucial for adapting the care plan accordingly.
• Late Creation: When there’s a need to create new
tasks in response to unexpected patient develop-
ments or additional requirements during the diag-
nosis.
• Parallelism: Sepsis exams often involve multiple
concurrent tasks, such as laboratory tests, patient
assessment, and treatment initiation. The paral-
lelism pattern allows for handling these tasks si-
multaneously.
• Iteration and Momentary Loop Insertion: Sepsis
exams might involve iterative processes, such as
repeated assessments or treatments at specific in-
tervals. Using these patterns allows modeling of
recurring activities.
As shown in Table 6 CMMN is a well-suited model-
ing approach to efficiently accommodate the flexibil-
ity patterns mentioned. Therefore, CMMN can be a
suitable choice for modeling and managing the flexi-
ble parts of these processes.
6 CONCLUSION
In conclusion, this paper has illuminated the poten-
tial of the Triple Crown standard, comprising BPMN,
CMMN, and DMN, in effectively representing patient
care processes. Our exploration has delved into crit-
ical dimensions, including flexibility, data and infor-
mation flow, complexity management, and decision
points, vividly demonstrating how the Triple Crown
approach can substantially enhance patient care pro-
cess models. We have shown that, based on selected
KPIs, we can harness the combination of these lan-
guages to unlock their potential for creating more
comprehensive models. In this paper, we tackled
three challenges in patient care process modeling:
• Patients exhibit a variety of conditions and unique
needs that must be taken into account when mod-
eling a care process: Utilized CMMN to establish
distinct abstraction levels for representing pro-
cess variants and diverse paths, effectively captur-
ing various aspects of flexibility while mitigating
complexity
• Complex decisions for diagnosing and treatment
of patients: DMN offers a modular decision re-
quirements hierarchy which allows for the decom-
position of complex decision logic into smaller,
more manageable components
• In patient care processes, achieving evidence-
based decision making requires a high-quality
flow of information : CMMN excels in its capac-
ity to model a wide range of data structures, mak-
ing it a versatile choice for representing the di-
verse and complex information inherent in patient
care processes
Nevertheless, it is imperative to acknowledge the
challenges associated with CMMN and DMN, includ-
ing complexity, limited tool support, and integration
issues. To ensure the successful implementation of
these modeling languages, stakeholders must invest
time and resources in learning and addressing these
challenges.
To enhance the applicability of our findings, future
research endeavors should encompass evaluations and
analyses in our work, with a dedicated focus on vali-
dating the conclusions drawn in this paper.
REFERENCES
Albahri, O. S., Albahri, A. S., Mohammed, K., Zaidan, A.,
Zaidan, B., Hashim, M., and Salman, O. H. (2018).
Systematic review of real-time remote health moni-
toring system in triage and priority-based sensor tech-
nology: Taxonomy, open challenges, motivation and
recommendations. Journal of medical systems, 42:1–
27.
Andree, K., Ihde, S., Weske, M., and Pufahl, L. (2022). An
exception handling framework for case management.
Software and Systems Modeling, 21(3):939–962.
Barbagallo, S., Corradi, L., De Ville de Goyet, J., Iannucci,
M., Porro, I., Rosso, N., Tanfani, E., and Testi, A.
(2015). Optimization and planning of operating the-
atre activities: an original definition of pathways and
process modeling. BMC medical informatics and de-
cision making, 15:1–16.
Combi, C., Oliboni, B., Zardini, A., and Zerbato, F. (2017).
A Methodological Framework for the Integrated De-
sign of Decision-Intensive Care Pathways—an Appli-
cation to the Management of COPD Patients. Journal
of Healthcare Informatics Research, 1(2):157–217.
Combi, C., Oliboni, B., Zardiniy, A., and Zerbato, F. (2016).
Seamless design of decision-intensive care pathways.
In 2016 IEEE International Conference on Healthcare
Informatics (ICHI), pages 35–45. IEEE.
Di Ciccio, C., Marrella, A., and Russo, A. (2015).
Knowledge-Intensive Processes: Characteristics, Re-
quirements and Analysis of Contemporary Ap-
proaches. Journal on Data Semantics, 4(1):29–57.
Dugar, S., Choudhary, C., and Duggal, A. (2020). Sepsis
and septic shock: Guideline-based management.
Gagne, D. (2016). Case Management Model and Notation
(CMMN): An Introduction. (December).
Herzberg, N., Kirchner, K., and Weske, M. (2015). Model-
ing and monitoring variability in hospital treatments:
a scenario using cmmn. In Business Process Man-
agement Workshops: BPM 2014 International Work-
Exploring the Power of Triple Crown Process Modeling in Healthcare: Sepsis Case
527

shops, Eindhoven, The Netherlands, September 7-8,
2014, Revised Papers 12, pages 3–15. Springer.
Jo
ˇ
st, G., Heri
ˇ
cko, M., and Polan
ˇ
ci
ˇ
c, G. (2019). Theo-
retical foundations and implementation of business
process diagrams’ complexity management technique
based on highlights. Software & Systems Modeling,
18:1079–1095.
Kluza, K. and Nalepa, G. J. (2012). Proposal of square met-
rics for measuring business process model complexity.
In 2012 Federated Conference on Computer Science
and Information Systems (FedCSIS), pages 919–922.
IEEE.
Kurz, M., Schmidt, W., Fleischmann, A., and Lederer, M.
(2015). Leveraging cmmn for acm: examining the
applicability of a new omg standard for adaptive case
management. In Proceedings of the 7th international
conference on subject-oriented business process man-
agement, pages 1–9.
Lenz, R., Peleg, M., and Reichert, M. (2012). Healthcare
process support: achievements, challenges, current re-
search. International Journal of Knowledge-Based
Organizations (IJKBO), 2(4).
Lenz, R. and Reichert, M. (2007). It support for healthcare
processes–premises, challenges, perspectives. Data &
Knowledge Engineering, 61(1):39–58.
Mans, R. S., Van der Aalst, W. M., and Vanwersch, R. J.
(2015). Process mining in healthcare: evaluating and
exploiting operational healthcare processes. Springer.
Marin, M. A. Complexity metrics for the case management
modeling notation (cmmn).
Mei, J., Li, J., Yu, Y., Li, X., Liu, H., and Xie, G. (2014).
Embracing case management for computerization of
care pathways. In MIE, pages 3–7.
Mulyar, N., Pesic, M., Van Der Aalst, W. M., and Peleg, M.
(2008a). Declarative and procedural approaches for
modelling clinical guidelines: addressing flexibility
issues. In Business Process Management Workshops:
BPM 2007 International Workshops, BPI, BPD, CBP,
ProHealth, RefMod, semantics4ws, Brisbane, Aus-
tralia, September 24, 2007, Revised Selected Papers
5, pages 335–346. Springer.
Mulyar, N., van der Aalst, W. M., and Russell, N. (2008b).
Process flexibility patterns.
Neskovic, S. and Kirchner, K. (2016). Using context infor-
mation and cmmn to model knowledge-. pages 17–21.
OMG (2011). Business Process Model and Notation . (Jan-
uary):538.
OMG (2016). Case Management Model and Notation 1.1
Beta. (March):124.
OMG Healthcare Domain Taskforce (2020). The BPM+
Field Guide to Shareable Clinical Pathways. page 125.
Pufahl, L., Zerbato, F., Weber, B., and Weber, I. (2022).
Bpmn in healthcare: Challenges and best practices.
Information Systems, 107:102013.
Rojo, M. G., Rol
´
on, E., Calahorra, L., Garc
´
ıa, F.
´
O.,
S
´
anchez, R. P., Ruiz, F., Ballester, N., Armenteros,
M., Rodr
´
ıguez, T., and Espartero, R. M. (2008). Im-
plementation of the business process modelling nota-
tion (bpmn) in the modelling of anatomic pathology
processes. In Diagnostic pathology, volume 3, pages
1–4. BioMed Central.
Rol
´
on, E., Aguilar, E., Garc
´
ıa, F., Ruiz, F., Piattini, M.,
Calahorra, L., et al. (2008). Process modeling of the
health sector using bpmn: a case study. In Proceed-
ings of First International Conference on Health In-
formatics, HEALTHINF 2008, volume 2, pages 173–
8.
Routis, I., Bardaki, C., Nikolaidou, M., Dede, G., and
Anagnostopoulos, D. (2023). Exploring cmmn ap-
plicability to knowledge-intensive process modeling:
An empirical evaluation by modelers. Knowledge and
Process Management, 30(1):33–54.
Routis, I., Nikolaidou, M., and Anagnostopoulos, D.
(2020). Empirical evaluation of CMMN models: a
collaborative process case study. Software and Sys-
tems Modeling, 19(6):1395–1413.
Rzepi
´
nski, T. M. (2007). The structure of diagnosis in
medicine: Introduction to interrogative characteris-
tics. Theoretical Medicine and Bioethics, 28:63–81.
S
´
anchez-Gonz
´
alez, L., Ruiz, F., Garc
´
ıa, F., and Cardoso, J.
(2011). Towards thresholds of control flow complex-
ity measures for bpmn models. In Proceedings of the
2011 ACM symposium on Applied computing, pages
1445–1450.
Taj, M., Brenner, M., Sulaiman, Z., and Pandian, V. (2022).
Sepsis protocols to reduce mortality in resource-
restricted settings: A systematic review. Intensive and
Critical Care Nursing, page 103255.
Von Rosing, M., White, S. A., Cummins, F., and De Man,
H. (2014). Business process model and notation-
BPMN. The Complete Business Process Handbook:
Body of Knowledge from Process Modeling to BPM,
1(January):429–453.
Wiemuth, M., Junger, D., Leitritz, M., Neumann, J., Neu-
muth, T., and Burgert, O. (2017). Application fields
for the new object management group (omg) standards
case management model and notation (cmmn) and de-
cision management notation (dmn) in the periopera-
tive field. International journal of computer assisted
radiology and surgery, 12:1439–1449.
Ye, J., Sun, S., Song, W., and Wen, L. (2008). Formal se-
mantics of bpmn process models using yawl. In 2008
Second International Symposium on Intelligent Infor-
mation Technology Application, volume 2, pages 70–
74. IEEE.
Zensen, A. and Kuster, J. (2018). A comparison of flex-
ible BPMN and CMMN in practice: A case study
on component release processes. Proceedings - 2018
IEEE 22nd International Enterprise Distributed Ob-
ject Computing Conference, EDOC 2018, pages 105–
114.
HEALTHINF 2024 - 17th International Conference on Health Informatics
528
