
Stroke Prehospital Decision Support Systems Based on Artificial
Intelligence: Grey Literature Scoping Review
Hoor Jalo
1a
, Eunji Lee
1
, Mattias Seth
1b
, Anna Bakidou
1,2 c
, Minna Pikkarainen
1,3
,
Katarina Jood
4,5 d
, Bengt Arne Sjöqvist
1e
and Stefan Candefjord
1f
1
Department of Electrical Engineering, Chalmers University of Technology, Gothenburg, Sweden
2
PreHospen – Centre for Prehospital Research, University of Borås, Borås, Sweden
3
Department of Occupational Therapy, Oslo Metropolitan University, Oslo, Norway
4
Department of Clinical Neuroscience, Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
5
Department of Neurology, Sahlgrenska University Hospital, Gothenburg, Sweden
katarina.jood@neuro.gu.se
Keywords: Artificial Intelligence (AI), Clinical Decision Support Systems (CDSSs), Grey Literature, Machine Learning
(ML), Prehospital Care, Stroke.
Abstract: Stroke is a leading cause of mortality and disability worldwide. Therefore, there is a growing interest in
prehospital point-of-care stroke clinical decision support systems (CDSSs), which with improved precision
can identify stroke and decrease the time to optimal treatment, thereby improving clinical outcomes. Artificial
intelligence (AI) may be a route to improve CDSSs for clinical benefit. Deploying AI in the area of prehospital
stroke care is still in its infancy. There are several existing systematic and scoping reviews summarizing the
progress of AI methods for stroke assessment. None of these reviews include grey literature, which could be
a valuable source of information, especially when analysing future research and development directions. This
paper aims to use grey literature to investigate stroke assessment CDSSs based on AI. The study adheres to
PRISMA guidelines and presents seven records showcasing promising technologies. These records included
three clinical trials, two smartphone applications, one master thesis and one PhD dissertation, which identify
electroencephalogram (EEG), video analysis and voice and facial recognition as potential data sources for
early stroke identification. The integration of these technologies may offer the prospect of faster and more
accurate CDSSs in the future.
1 INTRODUCTION
Stroke is a leading cause of death and disability
worldwide (Chennareddy et al., 2022). It is caused by
either a bleeding, called haemorrhagic stroke, or a
clot in one or more of the brain’s blood vessels, called
ischemic stroke which accounts for approximately
85% of cases (Meyran et al., 2020). For ischemic
stroke, two types of treatment are deployed:
thrombolysis (clot-dissolving drugs) or
thrombectomy (mechanically removing the clot)
a
http://orcid.org/0000-0001-6975-8520
b
http://orcid.org/0000-0002-3737-3316
c
http://orcid.org/0000-0002-4288-8146
d
http://orcid.org/0000-0001-8746-1771
e
http://orcid.org/0000-0002-6564-737X
f
http://orcid.org/0000-0001-7942-2190
(Lumley et al., 2020; Shlobin et al., 2022). The latter
is an advanced treatment that requires a specialist at a
comprehensive stroke centre (CSC) and is suited for
thrombectomy candidates, i.e., patients with large
vessel occlusion (LVO) with still viable brain tissue
that can be restored (Chennareddy et al., 2022;
Nicholls et al., 2022). Brain cells die as time passes
without treatment; hence, quick treatment is a critical
factor (Shlobin et al., 2022).
Most stroke patients are initially handled by a
prehospital team in an ambulance according to
458
Jalo, H., Lee, E., Seth, M., Bakidou, A., Pikkarainen, M., Jood, K., Sjöqvist, B. and Candefjord, S.
Stroke Prehospital Decision Support Systems Based on Artificial Intelligence: Grey Literature Scoping Review.
DOI: 10.5220/0012380400003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 458-465
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
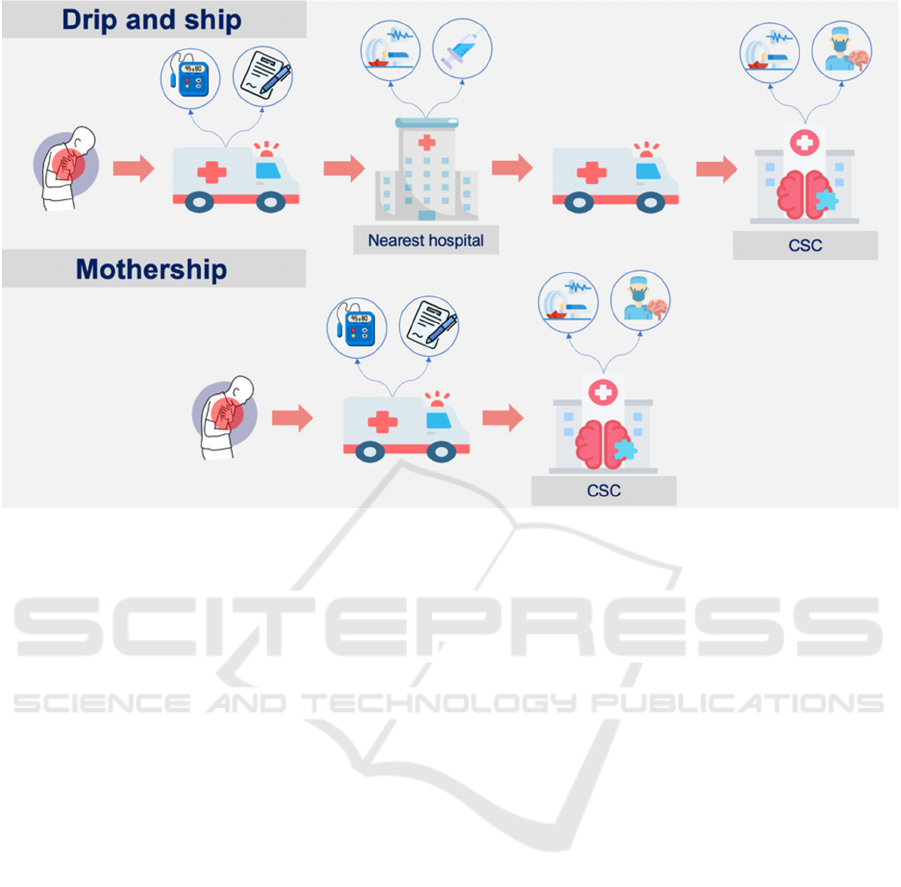
Figure 1: Drip-and-ship and mothership strategies.
predefined procedures including medical history,
patient assessment, glucose and vital signs
monitoring. In addition, various clinical stroke scales
are used to predict the likelihood of stroke and its
severity. These scales are symptom-based tests that
assess the patient’s stroke symptoms such as speech,
facial expression and arm and leg movements
(Nicholls et al., 2022). In hospital settings, the most
commonly used scale is called the National Institutes
of Health Stroke Scale (NIHSS); it is a validated scale
with a sensitivity of 86% and a specificity of 60% for
LVO (Nicholls et al., 2022). In prehospital settings,
the observation for NIHSS is too complicated to carry
out for the ambulance teams, therefore simpler,
mostly unvalidated scales, e.g., Los Angeles Motor
Scale, are frequently used. The accuracy of
prehospital stroke diagnosis, when relying solely on
stroke scales, remains low, with a 64% sensitivity
(Chennareddy et al., 2022), suggesting the need for
considering additional diagnostic methods or factors
in enhancing diagnostic accuracy.
It is crucial to streamline prehospital stroke
management (Fassbender et al., 2020). Currently,
stroke is typically confirmed at hospitals after brain
imaging is performed, such as computed tomography
(CT) and magnetic resonance imaging (MRI)
(Magnusson et al., 2022). According to international
stroke management guidelines, such as those
recommended by the American Stroke Association,
patients with suspected stroke are typically
transported to the nearest hospital. If the nearest
hospital is not a CSC and LVO is confirmed, the
patient should be transferred to a CSC where
thrombectomy can be performed (Nicholls et al.,
2022). This strategy is called drip-and-ship (Figure
1). Patients with a high probability of LVO may be
transported directly to the CSC, which is called the
mothership strategy (Fassbender et al., 2020; Nicholls
et al., 2022). Identification of more LVO patients in
the prehospital setting is crucial to reducing
prehospital delays and improving patient outcomes
(Nicholls et al., 2022).
The research group Care@Distance–Remote and
Prehospital Digital Health at Chalmers University of
Technology is focused on developing AI-based
prehospital clinical decision support systems
(CDSSs) for acute diseases, such as stroke. Our aim
is to enhance the performance in the identification of
LVO and provide support to reduce treatment delays.
This is in line with the American Heart Association
Guidelines (2019), which called for further research
to identify effective prehospital procedures for
triaging patients to the appropriate centers, including
hospital bypass algorithms (Nicholls et al., 2022).
Artificial intelligence (AI) and machine learning
(ML) deployed in CDSS can play an important role
in improving stroke assessment (Murray et al., 2020;
Shlobin et al., 2022). AI encompasses computer tasks
challenging for humans, including CDSSs, which
could be defined to fall within the AI realm although
Stroke Prehospital Decision Support Systems Based on Artificial Intelligence: Grey Literature Scoping Review
459
employing basic algorithms influenced by clinical
experience. The focus of this study is however
specifically on advanced ML algorithms,
characterized by their complex model architectures
and data-driven techniques, as we investigate their
potential for enhancing early stroke characterization.
Several recent scoping and systematic reviews
have summarized the progress of AI methods for
stroke assessment; however, none included grey
records (Chennareddy et al., 2022; Lumley et al.,
2020; Murray et al., 2020; Nicholls et al., 2022;
Ruksakulpiwat et al., 2021; Shlobin et al., 2022).
Grey literature can be a rich source of information
about solutions in premature stages, and the Institute
of Medicine Standards for Systematic Review (Berg
et al., 2011) and the Cochrane Handbook for
Systematic Reviews of Interventions (Higgins et al.,
2023) recommend incorporating grey literature in
systematic reviews. Our group is currently working
on a scoping review that is centered on the peer-
reviewed literature (Jalo et al., 2023). This study
therefore aims to complement our review and existing
reviews by specifically focusing on publicly available
grey literature that includes, among others, academic
papers (theses and dissertations), non-peer-reviewed
conference proceedings, research and committee
reports, government reports, clinical trials and
ongoing studies to identify promising AI-based
CDSSs for prehospital stroke assessment.
2 METHODS
Arksey and O'Malley (Arksey et al., 2005) describe a
scoping review as a form of literature review
designed to map the relevant literature within a
specific research domain. This scoping review was
carried out in accordance with Arksey and O’Malley
(Arksey et al., 2005), a five-stage methodology
including (1) identifying the research question(s), (2)
identifying relevant studies, (3) selecting studies, (4)
charting the data and (5) collating, summarizing and
reporting the results. The optional consultation stage
was not conducted in this scoping review because it
is challenging to evaluate new AI-based CDSSs due
to the intricate algorithms and methods involved.
The methodology started with identifying the
research question, and this review aims to answer the
following question: what are the promising AI-based
CDSSs for stroke assessment in prehospital settings?
To answer the identified research question, relevant
studies were identified by searching 12 databases,
focusing only on recent grey literature such as non-
peer-reviewed conference proceedings, theses,
dissertations and reports during the past 10 years. The
searched databases (ClinicalTrial, ProQuest, Arxiv,
EBSCOhost, Networked Digital Library of Theses
and Dissertations (NDLTD), University of
Wollongong (UOW) library, Bielefeld Academic
Search Engine (BASE), World Health Organization
(WHO), Canada’s drug and health technology agency
(CADTH), FiNDit, Open Access Theses and
Dissertations (OATD), University of South
California (USC) Library and Science daily) were
selected based on grey literature recommendations
published by James Cook University’s library (James
Cook University). Google Scholar was not included
in this study because a study found that most of the
not retrieved records in Google Scholar were grey
literature (Yasin et al., 2020).
Search terms included stroke, haemorrhagic
stroke, ischemic stroke, artificial intelligence,
machine learning and decision support systems,
which were systematically combined using Boolean
operators (AND, OR) to capture relevant studies.
Search strings were defined and adopted for each
database.
The third stage was to select studies based on
identified eligibility criteria (Table 1). Article
screening was done in two steps: (1) title and abstract
screening, and (2) full text screening.
Table 1: Eligibility criteria.
Inclusion criteria Exclusion criteria
Non-peer reviewed
records
Peer-reviewed journal and
peer-reviewed conference
articles
The record reports a
method for stroke
assessment
No focus on stroke
Stroke related to animal
studies
The record presents an
AI-based tool for stroke
assessment in the
prehospital setting
No AI-based method is
reported, or the method
cannot be used in the
prehospital setting, e.g.,
the use of brain imaging
is required
Written in English Not written in English
Published between 2012
and 2022
Older records or non-
retrievable
The included records were then summarized,
charted and reported. An Excel sheet was used to
extract the following data from each included study:
key information, aims, population and study subject
characteristics, methodology, main findings and
limitations of the study. By applying a consistent
approach to each included study, common
characteristics and descriptive summary were
provided.
HEALTHINF 2024 - 17th International Conference on Health Informatics
460
3 RESULTS
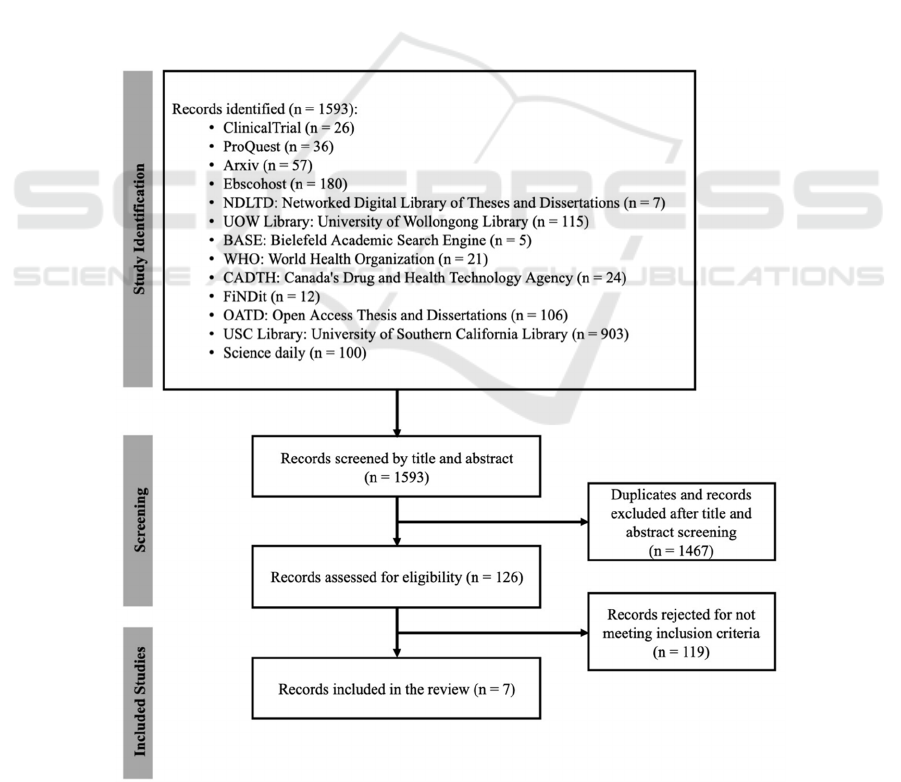
A total of 1593 grey literature records were identified
during Stage 2 (Figure 2). Initial title and abstract
screening and duplicate removal resulted in 126
records passed for full-text screening. Among these,
119 did not meet the inclusion criteria, including
studies published in peer-reviewed journals, not
retrieved data and records irrelevant to the research
questions. Seven relevant records were included and
are summarized in Table 2. No records were found
between 2012 and 2018.
An ongoing clinical trial in the Netherlands tests
the accuracy of AI-STROKE algorithms: one or more
novel AI-based electroencephalography (EEG)
algorithms to detect LVO in ambulances (Coutinho,
2022). EEG is performed using dry electrode EEG
caps, and investigators expect it to be done in less
than five minutes in ambulances (Coutinho, 2022).
The presence or absence of a clot will be confirmed
using CT scans at the emergency department (ED)
(Coutinho, 2022). The accuracy of the new
algorithms will be tested by comparing the area under
the receiver operating characteristic curve (AUC),
sensitivity, specificity, positive predictive value
(PPV) and negative predictive value (NPV) to
existing EEG algorithms (Coutinho, 2022).
Another ongoing clinical trial is a prospective
observational study in Sweden, which evaluates
measurements from EEG, heart rate variability
(HRV) and near-infrared spectroscopy (NIRS)
separately and combined to provide a specific
detection of cerebral ischemia (Block et al., 2020;
Block, 2022). The investigators hypothesize that
changes in those measurements can indicate cerebral
ischemia and reperfusion after being processed by
ML classification models. The study aims to find
specific patterns in EEG, HRV and NIRS to signify
cerebral ischemia and build a monitoring warning
system for the diagnosis of upcoming cerebral
ischemia (Block et al., 2020; Block, 2022).
Figure 2: Modified PRISMA flowchart to summarize retrieved records (Page et al., 2021).
Stroke Prehospital Decision Support Systems Based on Artificial Intelligence: Grey Literature Scoping Review
461
An ongoing clinical trial in Norway (Haukeland
University Hospital, 2022) works on an AI-based
prototype for acute stroke detection in emergency
medical calls. The study aims to use audio from
emergency calls and available data in hospital records
to implement an AI-based detection system and test
its performance against the current system by
comparing sensitivity and specificity.
Facial palsy is a common symptom in stroke
patients; facial recognition is thus an important
technique to be used in the detection of stroke. A
master thesis from TU Delft presented a system that
automatically detects facial paralysis based on deep
learning algorithms (Sourlos, 2020). The algorithm
first detects a patient’s face from an image, then
metrics are defined based on landmarks localized on
the face, to classify the input image (Sourlos, 2020).
In total, 203 images were analysed (60 of healthy
subjects, 40 of central palsy patients and 103 of
peripheral palsy patients), and an accuracy of 99.5%
was achieved for the healthy group and 90.9% for
patients with facial palsy (Sourlos, 2020).
Another promising technology is a mobile
application called Fatal Recognition that uses facial
recognition to detect early signs of stroke (Chan,
2019). Every time patients unlock their screen, an
algorithm detects signs of face-drooping, sends alerts
to contact emergency services and shows emergency
services contact details (Chan, 2019).
Table 2: Summary of the data extracted for novel CDSSs included in the scoping review.
Record
Study
design
Year Location Goal Methodology
Algorithm Development
Through AI for the Triage
of Stroke Patients in the
Ambulance with EEG
(AI-STROKE)
(Coutinho, 2022).
Clinical
trial
2022 Netherlands LVO detection in
ambulances
AI-based EEG
algorithms with the
use of dry electrode
caps
Detection of Cerebral
Ischemia with Artificial
Intelligence
(Block, 2022)
Clinical
trial
2022 Sweden Detection of cerebral
ischemia
ML models based on
EEG, HRV and NIRS
Artificial Intelligence
Support in Stroke Calls
(AISIS)
(Haukeland University
Hospital, 2022)
Clinical
trial
2022 Norway Acute stroke detection in
emergency medical calls
AI-based detection
system using audio
calls and health
records
Facial Imaging and
Diagnosis System for
Neurological Disorders
(Sourlos, 2020)
Master
thesis
2020 Netherlands Automatic detection of
facial paralysis
Deep learning-based
system
Fatal Recognition
(Chan, 2019)
Mobile
application
2019 Hong Kong Detection of early signs of
facial drooping in stroke
AI-based facial
drooping detection
AI-Stroke
(AI-Stroke, 2022)
Mobile
application
2022 France Indication of stroke and
characterization the stroke
type
Video analysis and
ML to perform NIHSS
scale
Human-Centred Machine
Learning for Healthcare:
Examples in Neurology
and Pulmonology
(Ramesh, 2020)
PhD
dissertation
2020 USA Hemiparesis detection in
stroke patients
Video analysis and
ML
HEALTHINF 2024 - 17th International Conference on Health Informatics
462

A company called AI-Stroke developed a
smartphone application to perform the NIHSS test,
and it guides the person close to the patient on how to
perform the test while recording a video of the patient
(AI-Stroke, 2022). The AI algorithm calculates the
NIHSS score, indicates the probability of having a
stroke and characterizes the stroke type. They aim to
create a dataset with videos from stroke patients and
healthy volunteers to be used in training the AI
model. An ethical application has been approved in
France, and the first patient was recently added to the
dataset Franc (AI-Stroke, 2022).
Video analysis based on ML was used to detect
hemiparesis in stroke patients in a sitting position as
a part of a PhD dissertation at the University of
California San Diego (Ramesh, 2020). Hemiparesis is
usually identified by the NIHSS test by asking the
patient to move the arm or leg (Ramesh, 2020). The
system was tested by eight stroke specialists, and a
video-based assessment was done as part of the
NIHSS test at rest in the sitting position. The accuracy
of the system was 68% and 61% when moving and at
rest, respectively (Ramesh, 2020).
4 DISCUSSIONS
Integration of innovative technology in prehospital
clinical assessment may lead to early stroke detection,
classification of stroke subtypes and fewer false-
positive stroke diagnosis. AI-based prehospital
CDSSs for stroke play a crucial role in the context of
embedded decision support systems. These
innovative technologies leverage the power of AI to
assist ambulance teams in making quick and accurate
decisions during the critical prehospital phase of
stroke care. By analysing various patient data, these
systems can quickly identify potential stroke cases,
prioritize them based on severity and provide real-
time recommendations for appropriate interventions
and transportation protocols, thereby allowing for
faster treatment and improved clinical outcomes.
The seven included records have highlighted
several methods for early stroke detection in the
prehospital environment, including EEG brain
imaging techniques and automated symptom-based
tools. Two clinical studies have used EEG, which has
a long-established sensitivity for early stroke
detection and has the potential to be used in
prehospital settings (Block et al., 2020; Erani et al.,
2020). EEG is a physiological monitoring technique
that is used to record the brain’s electrical activity and
can immediately detect changes in brain function
(Block et al., 2020; Erani et al., 2020). One of its
limitations is the long time spent in applying gel, but
this could be overcome by using rapidly applied dry
electrodes (Erani et al., 2020). A recent study
indicated that EEG signals contain further diagnostic
information compared to the current clinical
assessment (Erani et al., 2020). The AUC for acute
stroke diagnosis was 87.8 and 86.4 for LVO patients
when EEG was incorporated into the clinical routine
of stroke diagnosis (Erani et al., 2020).
Speech, facial palsy and impaired movement are
early stroke symptoms and are currently evaluated by
symptom-based clinical stroke scales. Many of the
stroke cases remain undetected in the prehospital
settings (Fassbender et al., 2020). For example, a
study compared the accuracy of 13 clinical stroke
scales for detecting thrombectomy candidates and
showed that 20% of thrombectomy candidates
remained undetected by the use of clinical stroke
scales (Fassbender et al., 2020). The recent
technologies focusing on early detection of these
symptoms thus have the potential to provide more
informative CDSS to improve prehospital stroke
detection, allowing for faster treatment and improved
clinical outcomes.
After applying the eligibility criteria, seven papers
were included in this study due to its narrow focus,
highlighting the need for further research in the
critical field of prehospital stroke assessment. This
aligns with a recent scoping review (Nicholls et al.,
2022) that aimed to identify LVO detection
techniques across various settings and included just
nine studies on AI-based methods. Out of these
studies, only three focused on AI-based prehospital
triaging tools. These tools included a smartphone
application designed to aid emergency medical
services professionals in patient assessment and
destination triage (Nogueira et al., 2017), a prediction
model that incorporated various predictors (Chen et
al., 2018) and a three-step triage tool aimed at
reducing prehospital assessment time (Zhao et al.,
2018). Notably, none of the studies presented AI-
based solutions involving EEG, video analysis, or
voice recognition for early stroke identification. This
study has thus presented early-stage research and
innovative concepts.
The main strength of this review is that it provides
information about the innovative technologies
usually not covered in reviews, with the potential to
improve stroke detection in prehospital settings.
Notably, this study pioneers the examination of a
research area that has not been well-explored, as
evidenced by the absence of records from 2012 to
2018. The results may thus serve as a basis for
developing an AI-based CDSS for early assessment
Stroke Prehospital Decision Support Systems Based on Artificial Intelligence: Grey Literature Scoping Review
463

of stroke. Limitations include that this study has been
conducted by only one reviewer, and many of the
presented results are ongoing clinical trials or yet-to-
be-performed studies. Those studies have different
study design, population and diagnostic accuracy
metrics which makes it difficult to perform
technology comparisons. Grey literature also captures
information related to emerging research areas that
are not yet published in peer-reviewed literature,
which makes a direct comparison with published
literature not feasible. However, it serves as a
valuable source of information by providing
preliminary research findings and insights into
emerging technologies. Future work may include
searching Google Scholar to see if more promising
techniques would be captured and widen the scope of
the review to include promising detection
technologies in hospitals. Future work also includes
searching the peer-reviewed literature to identify AI-
based CDSSs designed for assessing stroke in the
prehospital environment (Jalo et al., 2023).
5 CONCLUSIONS
This review has explored grey literature and
advancements in AI-based stroke assessment
methods in prehospital settings. It was found that in
future stroke assessments CDSS, EEG, audio
recognition, facial recognition and video records may
be used as data sources for decision-making. We
conclude that the reviewed technologies are
promising prehospital tools that have the potential to
aid in the early assessment of stroke, but they are yet
to be tested and validated. There are, however, not
many studies in this research area. More studies are
warranted due to the large clinical need.
Improvements in CDSSs would impact stroke
detection and patient triage, increasing the chance for
earlier initial treatment and the potential for fewer
secondary transfers of patients.
REFERENCES
AI-Stroke | Stroke Detection | Our Solution. (2022). AI-
Stroke. Retrieved from https://www.ai-stroke.com/our-
solution
Arksey, H., & O’Malley, L. (2005). Scoping studies:
towards a methodological framework. International
Journal of Social Research Methodology, 8(1), 19–32.
doi: 10.1080/1364557032000119616
Berg, A., Eden, J., Research, I. of M. (US) C. on S. for S.
R. of C. E., Levit, L., & Morton, S. (2011). Committee
On Standards For Systematic Reviews of Comparative
Effectiveness Research. In Finding What Works in
Health Care: Standards for Systematic Reviews.
National Academies Press (US). Retrieved from
https://www.ncbi.nlm.nih.gov/books/NBK209524/
Block, L. (2022). Detection of Cerebral Ischemia With
Artificial Intelligence- Biomarkers as Indicators in
Controlled Cerebral Ischemia and Reperfusion.
(Clinical Trial Registration No. NCT03919370).
clinicaltrials.gov. Retrieved from
https://clinicaltrials.gov/study/NCT03919370
Block, L., El-Merhi, A., Liljencrantz, J., Naredi, S., Staron,
M., & Odenstedt Hergès, H. (2020). Cerebral ischemia
detection using artificial intelligence (CIDAI)—A
study protocol. Acta Anaesthesiologica Scandinavica,
64(9), 1335–1342. doi: 10.1111/aas.13657
Chen, Z., Zhang, R., Xu, F., Gong, X., Shi, F., Zhang, M.,
& Lou, M. (2018). Novel Prehospital Prediction Model
of Large Vessel Occlusion Using Artificial Neural
Network. Frontiers in Aging Neuroscience, 10, 181.
doi: 10.3389/fnagi.2018.00181
Chennareddy, S., Kalagara, R., Smith, C., Matsoukas, S.,
Bhimani, A., Liang, J., Shapiro, S., De Leacy, R.,
Mokin, M., Fifi, J. T., Mocco, J., & Kellner, C. P.
(2022). Portable stroke detection devices: a systematic
scoping review of prehospital applications. BMC
Emergency Medicine, 22(1), 111. doi: 10.1186/s12873-
022-00663-z
Coutinho, J. (2022). Algorithm Development Through
Artificial Intelligence for the Triage of Stroke Patients
in the Ambulance With Electroencephalography
(Clinical Trial Registration No. NCT05437237).
clinicaltrials.gov. Retrieved from https://clinicaltrials.
gov/study/NCT05437237
Erani, F., Zolotova, N., Vanderschelden, B., Khoshab, N.,
Sarian, H., Nazarzai, L., Wu, J., Chakravarthy, B.,
Hoonpongsimanont, W., Yu, W., Shahbaba, B.,
Srinivasan, R., & Cramer, S. C. (2020). EEG Might
Improve Diagnosis of Acute Stroke and Large Vessel
Occlusion. Stroke, 51(11), 3361–3365. doi:
10.1161/STROKEAHA.120.030150
Fassbender, K., Walter, S., Grunwald, I. Q., Merzou, F.,
Mathur, S., Lesmeister, M., Liu, Y., Bertsch, T., &
Grotta, J. C. (2020). Prehospital stroke management in
the thrombectomy era. The Lancet. Neurology, 19(7),
601–610. doi: 10.1016/S1474-4422(20)30102-2
FATAL RECOGNITION. (2019). Mywebsite (New).
Retrieved from https://www.paulchancreative.com/
fatal-recognition
Haukeland University Hospital. (2022). Artificial
Intelligence (AI) Support in Stroke Calls - “The AISIS-
study” -Can Artificial Intelligence Improve the
Precision in Identifying Acute Stroke in Emergency
Medical Calls? (Clinical Trial Registration No.
NCT04648449). clinicaltrials.gov. Retrieved from
https://clinicaltrials.gov/study/NCT04648449
Higgins, J., J, T., & J, Chandler. (2023). Cochrane
Handbook for Systematic Reviews of Interventions.
Retrieved from https://training.cochrane.org/handbook
HEALTHINF 2024 - 17th International Conference on Health Informatics
464

Jalo, H., Seth, M., Pikkarainen, M., Häggström, I., Jood, K.,
Bakidou, A., Sjöqvist, B., & Candefjord, S. (2023).
Early identification and characterisation of stroke to
support prehospital decision-making using artificial
intelligence: a scoping review protocol. BMJ Open
13(5). doi: 10.1136/bmjopen-2022-069660
Lumley, H. A., Flynn, D., Shaw, L., McClelland, G., Ford,
G. A., White, P. M., & Price, C. I. (2020). A scoping
review of pre-hospital technology to assist ambulance
personnel with patient diagnosis or stratification during
the emergency assessment of suspected stroke. BMC
Emergency Medicine, 20(1), 30. doi: 10.1186/s12873-
020-00323-0
Magnusson, C., Herlitz, J., Sunnerhagen, K. S., Hansson,
P.-O., Andersson, J.-O., & Jood, K. (2022). Prehospital
recognition of stroke is associated with a lower risk of
death. Acta Neurologica Scandinavica, 146(2), 126–
136. doi: 10.1111/ane.13618
Meyran, D., Cassan, P., Avau, B., Singletary, E., &
Zideman, D. A. (2020). Stroke Recognition for First
Aid Providers: A Systematic Review and Meta-
Analysis. Cureus, 12(11), e11386. doi: 10.7759/
cureus.11386
Murray, N. M., Unberath, M., Hager, G. D., & Hui, F. K.
(2020). Artificial intelligence to diagnose ischemic
stroke and identify large vessel occlusions: a systematic
review. Journal of NeuroInterventional Surgery, 12(2),
156–164. doi: 10.1136/neurintsurg-2019-015135
Nicholls, J. K., Ince, J., Minhas, J. S., & Chung, E. M. L.
(2022). Emerging Detection Techniques for Large
Vessel Occlusion Stroke: A Scoping Review. Frontiers
in Neurology, 12, 780324. doi: 10.3389/fneur.2021.780
324
Nogueira, R. G., Silva, G. S., Lima, F. O., Yeh, Y.-C.,
Fleming, C., Branco, D., Yancey, A. H., Ratcliff, J. J.,
Wages, R. K., Doss, E., Bouslama, M., Grossberg, J.
A., Haussen, D. C., Sakano, T., & Frankel, M. R.
(2017). The FAST-ED App: A Smartphone Platform
for the Field Triage of Patients With Stroke. Stroke,
48(5), 1278–1284. doi: 10.1161/STROKEAHA.116.01
6026
Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I.,
Hoffmann, T. C., Mulrow, C. D., Shamseer, L.,
Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R.,
Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu,
M. M., Li, T., Loder, E. W., Mayo-Wilson, E.,
McDonald, S., … Moher, D. (2021). The PRISMA
2020 statement: an updated guideline for reporting
systematic reviews. BMJ, 372, n71. doi:
10.1136/bmj.n71
Ramesh, V. (2020). Human-Centered Machine Learning
for Healthcare: Examples in Neurology and
Pulmonology [ProQuest Dissertations Publishing].
Retrieved from https://search.proquest.com/docview/
2456394283?pq-origsite=primo
Ruksakulpiwat, S., Thongking, W., Zhou, W., Benjasirisan,
C., Phianhasin, L., Schiltz, N. K., & Brahmbhatt, S.
(2021). Machine learning-based patient classification
system for adults with stroke: A systematic review.
Chronic Illness, 17423953211067435. doi:
10.1177/17423953211067435
Shlobin, N. A., Baig, A. A., Waqas, M., Patel, T. R.,
Dossani, R. H., Wilson, M., Cappuzzo, J. M., Siddiqui,
A. H., Tutino, V. M., & Levy, E. I. (2022). Artificial
Intelligence for Large-Vessel Occlusion Stroke: A
Systematic Review. World Neurosurgery, 159, 207-
220.e1. doi: 10.1016/j.wneu.2021.12.004
Sources of Grey Literature - Finding Grey Literature -
Library Guides at James Cook University. Retrieved
from https://libguides.jcu.edu.au/grey-lit/sources
Sourlos, N. (2020). Facial Imaging and Diagnosis System
for Neurological Disorders. Retrieved from
https://repository.tudelft.nl/islandora/object/uuid%3Ae
60a60fc-073c-48b4-83af-d5823f309539
Yasin, A., Fatima, R., Wen, L., Afzal, W., Azhar, M., &
Torkar, R. (2020). On Using Grey Literature and
Google Scholar in Systematic Literature Reviews in
Software Engineering. IEEE Access, 8, 36226–36243.
doi: 10.1109/ACCESS.2020.2971712
Zhao, H., Pesavento, L., Coote, S., Rodrigues, E., Salvaris,
P., Smith, K., Bernard, S., Stephenson, M., Churilov,
L., Yassi, N., Davis, S. M., & Campbell, B. C. V.
(2018). Ambulance Clinical Triage for Acute Stroke
Treatment: Paramedic Triage Algorithm for Large
Vessel Occlusion. Stroke, 49(4), 945–951. doi:
10.1161/STROKEAHA.117.019307
Stroke Prehospital Decision Support Systems Based on Artificial Intelligence: Grey Literature Scoping Review
465
