
i-SART: An Intelligent Assistant for Safety Analysis
in Radiation Therapy
Natalia Silvis-Cividjian
1a
, Yijing Zhou
1b
, Anastasia Sarchosoglou
2c
and Evangelos Pappas
2d
1
Vrije Universiteit Amsterdam, Department of Computer Science, Amsterdam, The Netherlands
2
University of West Attica, Department of Biomedical Sciences, Athens, Greece
Keywords: Radiation Therapy, Safety and Risk Management, Digital Assistive Technology, Failure Modes and Effect
Analysis (FMEA), Natural Language Processing (NLP), Generative AI, Synthetic Data.
Abstract: Along with surgery and chemotherapy, radiation therapy (RT) is a very effective method to treat cancer. The
process is safety-critical, involving complex machines, human operators and software. A proactive hazard
analysis to predict what can go wrong in the process is therefore crucial. Failure Modes and Effect Analysis
(FMEA) is one of the methods widely used for risk assessment in healthcare. Unfortunately, the available
resources and FMEA expertise strongly vary across different RT organizations worldwide. This paper
describes i-SART, an interactive web-application that aims to close the gap by bringing together best practices
in conducting a sound RT-FMEA. Central is a database that at present contains approximately 420 FMs
collected from existing risk assessments and cleaned from ambiguities and duplicates using NLP techniques.
Innovative is that the database is designed to grow, due to both user input and generative AI algorithms. This
is work in progress. First experiments demonstrated that using machine learning in building i-START is
beneficial. However, further efforts will be needed to search for better solutions that do not require human
judgment for validation. We expect to release soon a prototype of i-SART that hopefully will contribute to
the global implementation and promotion of safe RT practices.
1 INTRODUCTION
Cancer is the second leading cause of death
worldwide. About 40% of world’s population will be
diagnosed with cancer at some point during their
lifetimes (NCI, 2017). Radiation therapy (RT) is a
highly effective cancer management approach
received by approximately 50% of all patients. One
can say that RT is a field where healthcare meets
informatics. The process takes place in complex,
computer-controlled linear accelerators (linacs),
where high-energy ionizing radiation is used to
reduce or eliminate the tumor(s) and at the same time
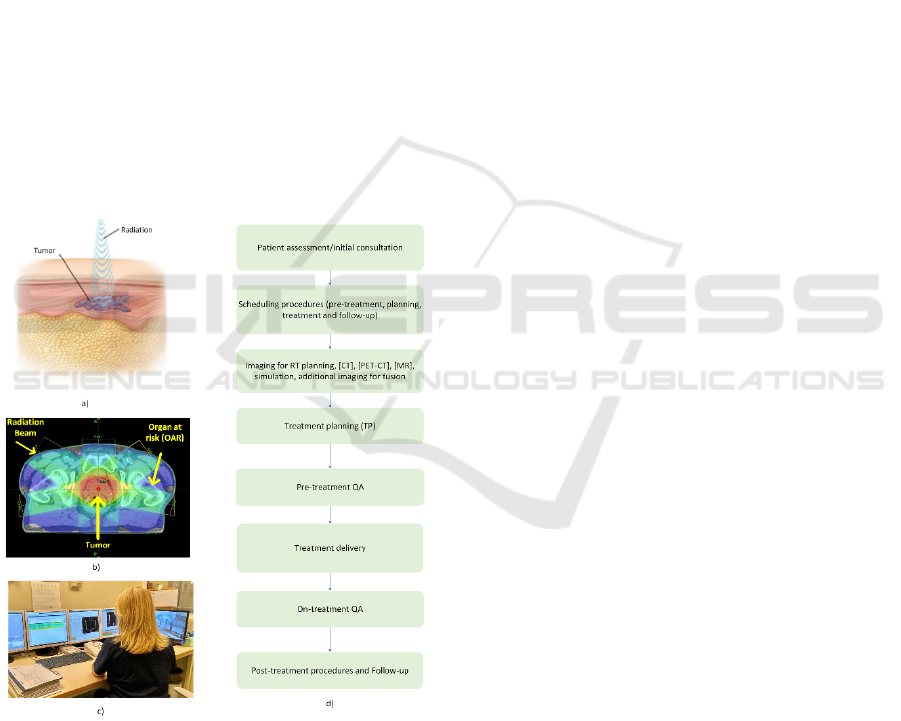
sparing the healthy tissue (Fig. 1). The core RT team
consists of different healthcare professionals,
including radiation oncologists, medical physicists,
radiation therapists, dosimetrists and nurses. A
generic process RT process is illustrated in Fig. 1.
a
https://orcid.org/0009-0004-4668-5946
b
https://orcid.org/0009-0007-6487-0004
c
https://orcid.org/0009-0007-6487-0046
d
https://orcid.org/0000-0001-8052-6392
After a patient is referred for radiotherapy and
assessed by a radiation oncologist, the next step
involves an imaging exam, usually a CT localization
scan. On these images, the radiation oncologist
delineates the specific regions that have to be
irradiated and prescribes the dose in each of these
regions. After that, the treatment planning and
treatment delivery teams accurately follow this
prescription and deliver the needed radiation, by
using the linac and various types of software
products. During the whole process, Quality
Assurance (QA) and patient monitoring activities are
mandatory.
A few devastating accidents that occurred in the
last decades demonstrate that the RT process is
safety-critical - any mistake, be it caused by
hardware, software or humans, can have fatal
consequences (Leveson and Turner, 1993), (Borras et
420
Silvis-Cividjian, N., Zhou, Y., Sarchosoglou, A. and Pappas, E.
i-SART: An Intelligent Assistant for Safety Analysis in Radiation Therapy.
DOI: 10.5220/0012364400003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 420-427
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
al., 2006). Therefore, RT is nowadays a strongly
regulated process, with safety standards in place
(Council of European Union, 2014), (IAEA, 2018).
According to these standards, an RT process needs to
be thoroughly assessed for all the risks it poses,
before obtaining permission to proceed (Huq et al.,
2016). This can be addressed with a proactive risk
analysis, which aims to anticipate failure modes (FM)
or hazards, defined as conditions that can lead to
incidents, or in other words, the various ways a
system can fail.
To conduct a safety assessment, the analysts can
choose from a range of systematic methods, such as
the traditional Failure Mode and Effects Analysis
(FMEA), Fault Tree Analysis (FTA) and Hazard and
Operability Analysis (HAZOP) (Pawlicki et al.,
2011), or the more modern Systems Theoretic
Accident Model and Process (STAMP) (Pawlicki et
al., 2016), (Silvis-Cividjian et al., 2020). All these
methods work in the same way: first, a team identifies
the potential hazards in a process, addresses their
causes and evaluates their effects, and finally
formulates appropriate mitigation measures.
Figure 1: a) The principle of RT; b) The geometry of RT,
where one can see that the tumor receives the highest
radiation dose (in red) and the healthy tissue the lowest (in
blue). From (Kane, 2014); c) A view from a typical
treatment facility room, where a radiation therapist needs to
distribute their attention over many computer screens.
Credits to A. Sarchosoglou; d) The workflow of a generic
RT process.
A general problem is that many RT departments
lack the time, training, or manpower required to
perform an in-depth risk assessment. Another problem
is that knowledge tends to remain compartmentalized
within departments, with safety analysis results often
not being shared widely. For example, currently there
is no centralized database with potential RT-specific
FMs that could be used as a reference by practitioners
who intend to conduct a proactive risk analysis. This
is a missed opportunity in our opinion, because
despite their diversity, all RT process workflows
feature in fact sufficient common FMs.
On the other hand, assistive and data mining
software applications, often powered by artificial
intelligence (AI), are rapidly emerging in all domains
of our daily life, including healthcare and RT.
Examples are software systems for electronic patient
dossiers, prediction of the response to a treatment,
disease risk assessment, or, specific for the RT
domain, radiation dose calculation, automatic
delineation of tumors and organs at risk on CT scan
images, or defacing of CT images of head-and-neck
cancer patients for privacy reasons, etc.
In this paper, we will present an attempt to close
the gap and improve RT safety worldwide with i-
SART, an online platform that assists practitioners in
performing an effective proactive FMEA-based
safety analysis. Central is a novel database that brings
together a large number of possible RT-specific FMs,
formulated in English and free of ambiguities or
duplicates. Innovative is that the database is designed
in such a way that new FM data can be fed not only
by safety-aware RT practitioners around the globe,
but also by state-of-the-art generative AI (GenAI)
algorithms. To the best of our knowledge, this is the
first attempt to use GenAI for synthetic FMs. As this
is work in progress, synthetic FMs were not included
yet in the i-SART database. Nevertheless, a prototype
of i-SART will be soon released for all interested RT-
practitioners.
The remainder of the paper is organized as
follows. In Section 2 we formulate the problem we try
to solve with i-SART, in Section 3 we will present the
design of i-SART, its database and user interface.
Section 4 will present some preliminary results and
Section 5 will outline our conclusions and future
work plans.
2 PROBLEM STATEMENT
First used by the US Military at the end of 40’s,
FMEA is a safety assessment method widely adopted
in systems engineering in 60’s (Arnzen, 1966).
i-SART: An Intelligent Assistant for Safety Analysis in Radiation Therapy
421
FMEA has been also widely used and recommended
for healthcare in general and RT in particular, in order
to prevent medical errors propagating and reaching
the patient (Ibanez, 2018), (Olch, 2014), (deRosier,
2002).
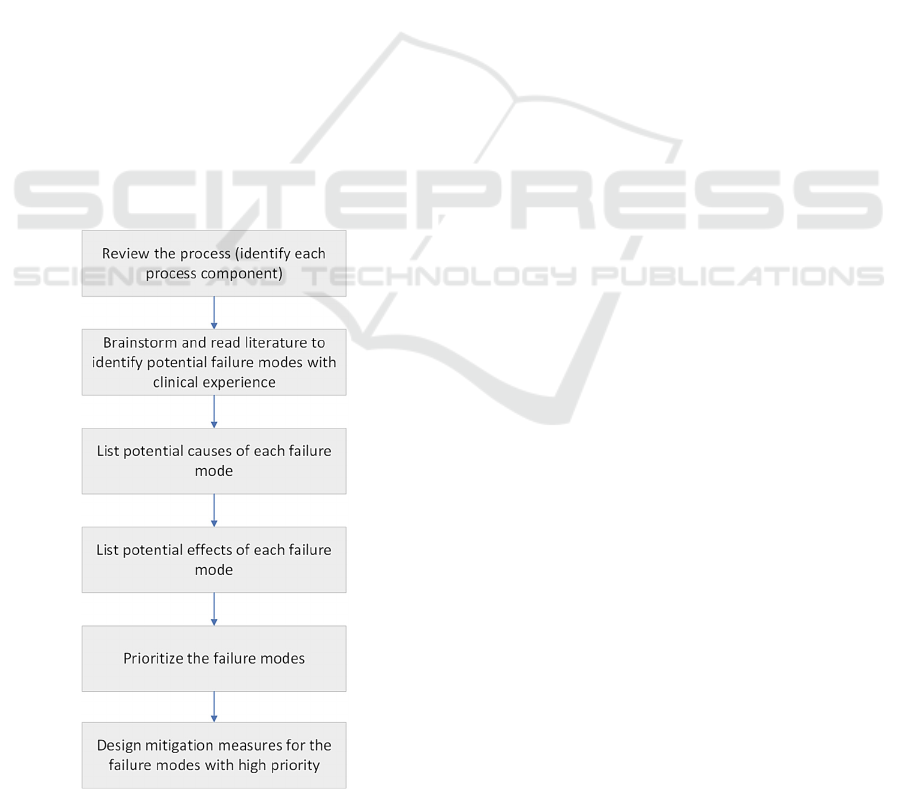
The general process flow of an FMEA is
illustrated in Fig. 2. The method is bottom-up,
meaning that for each component in the process, one
have to ask the question “How often would this
component fail, and what will happen if it fails?”. The
risk of each FM is evaluated using a Risk Priority
Number (RPN), calculated as the product of severity,
probability of occurrence, and detectability.
The result of an FMEA analysis is a list with all
possible FMs, ranked by their RPNs, their causes and
their effects, followed by measures to mitigate the
most critical ones. In an RT process, some FMs that
can occur are readily conceivable, such as “A wrong
patient is invited to the treatment room” or “The linac
gantry in rotation collides with the treatment couch”.
However, to conduct an analysis that will predict all
ways a process can fail is challenging. This task
demands considerable time, domain knowledge and
clinical experience. Unfortunately, these resources
may not always be readily available as the main task
of RT practitioners is to treat as many patients as
possible in a race against the clock with fast-evolving
cancer.
Figure 2: The workflow of an FMEA analysis.
To gain more insights into the current FMEA
practices within the RT, we recently conducted a
literature review that highlighted the diversity
between departments in the way they conduct their
FMEA (Sarchosoglou et al., 2022). A challenge we
encountered was for example the heterogeneity of the
terminology used to formulate FMs. Nonetheless, on
a more optimistic note, our findings also revealed
noteworthy similarities and common FMs that
support the need for a digital tool to aid departments
with their proactive risk assessment. Furthermore, the
level of safety awareness maturity strongly varies
among different RT organizations. In addition, the
knowledge about FMs is compartmentalized; if a
safety analysis was conducted somewhere, its results
usually stay in the department and are not widely
disseminated. Moreover, as technology in RT rapidly
advances, new, previously unidentified risks are
continuously emerging, presenting challenges to
professionals tasked with their implementation
(Ortiz-Lopez, 2009). Finally, education material and
non-proprietary digital tools to assist safety analysts
are practically non-existent.
The cumulative effect of all these challenges is that
incidents and errors of suboptimal RT treatment still
occur on daily basis (Ford and Evans, 2019). Hence,
there is an urgent need for assistance in conducting
hazard analyses, with the ultimate goal of enhancing
the safety of RT patients worldwide. This imperative
served as the driving force behind the initiation of the
i-SART project, a collaborative effort between the
computer science department at the Vrije Universiteit
in The Netherlands and the biomedical sciences
department at the University of West Attica in
Greece. The project addressed the following research
questions:
RQ1. Can we build an open-source software tool to
assist RT practitioners in conducting an effective
FMEA?
RQ2. Can we use machine learning to augment the
data obtained by the FMEA studies ?
3 i-SART, AN INTELLIGENT
FMEA ASSISTANT
The main goal of i-SART was to engage RT
practitioners in a dynamic FMEA learning
experience. Given the fact that RT professionals may
or may not have experience in FMEA, we expected
the usage of this tool to vary accordingly. On the one
HEALTHINF 2024 - 17th International Conference on Health Informatics
422
hand, FMEA beginners can use it as an expert system
to guide their analysis. On the other hand, RT experts
who are proficient in FMEA will be able to learn
about new FMs reported by other departments, or
share interesting FMs they have identified in their
institutions.
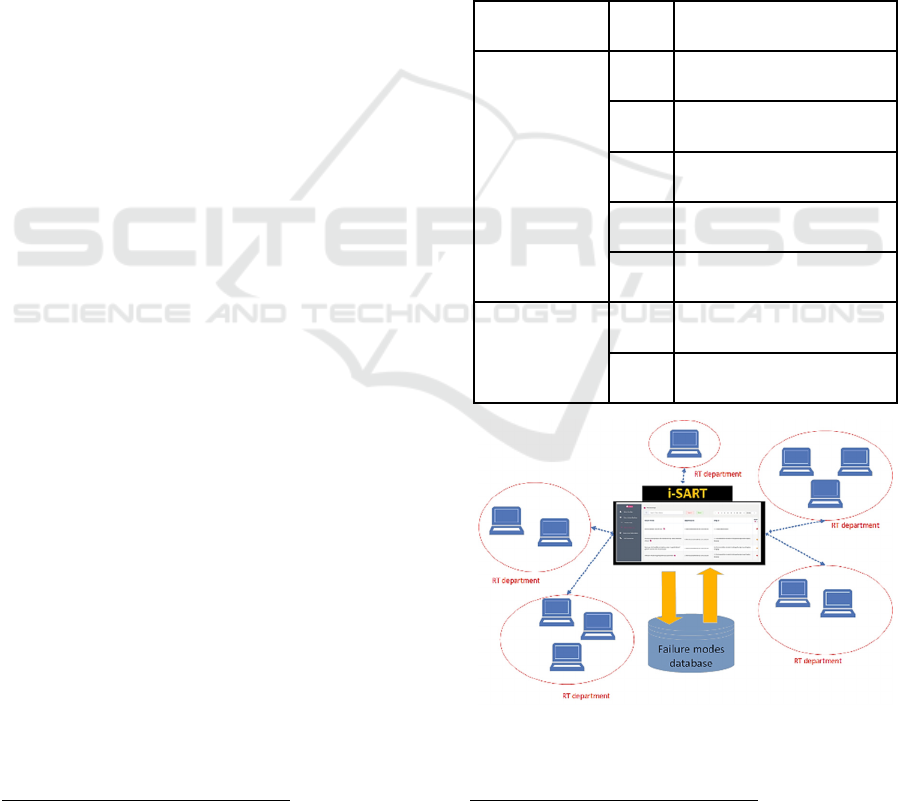
Technically, i-SART is designed as a cloud-
hosted web-application with two kinds of users:
administrators and RT practitioners (users), each with
their permissions and rights. The high-level
architecture of i-SART is illustrated in Fig. 3. Central
to i-SART is a novel database that aims to contain as
many as possible FMs that can occur in various RT
techniques, such as Intensity Modulated
Radiotherapy (IMRT), Stereotactic Body Radiation
Therapy (SBRT), etc. In the database, the FMs are
also grouped per sub-process and step in the RT sub-
process, such as Treatment planning, Treatment
delivery, etc. as illustrated in Fig. 1.
The web-application’s back-end was programmed
using Python 3.9 and the Django REST
1
framework.
Care was taken to ensure a secure transfer of
information between client and server, using the
JSON Web Token authentication
2
. A relational
database MySQL technology was used to achieve
persistent storage of both users’ and FM information.
The front-end user interface of i-SART was
developed using a Java-script-based framework
called Vue.js
3
. Its main function is to allow an RT
user to search in i-SART for FMs that might happen
in their particular RT process. There are also
searching, filtering and ordering functions available.
For example, if a user discovers a new FM in their
daily practice, they can add it to the i-SART database,
after a preliminary validation by the system
administrator, who is an RT expert. The administrator
can also visualize on a dashboard all the FMs in
different pie-charts, categorized based on their
severity or risk (see Fig. 4). A Vue chart component
library called Vue-ECharts
4
was used to plot these
charts. Finally, all users have the possibility to
evaluate the tool and send feedback and suggestions
to improve it.
1
https://www.djangoproject.com/
2
https://django-rest-framework-simplejwt.readthedocs.io/
en/latest/
4 FIRST RESULTS
4.1 First FM Data
The first step after the skeleton of the i-SART
prototype was ready, was to populate the FM
database. First 584 FMs were extracted from
scientific papers and un-published safety reports, all
written in English (see Table 1). All FMs were
classified into subprocesses and their corresponding
steps. Interesting is that we found that 32.5% of the
collected FMs fall into the subprocess Treatment
planning, 25.5% into the subprocess Treatment
delivery, and 20.7% into subprocess Imaging.
Table 1: Sources for the first collection of FMs .
Reference type #FMs Author/Year/Country
Research paper
16 Gilmore et al. (2021), UK
284 Pobbiati et al. (2019), Italy
220 Huq et al. (2016), USA
7 Bright et al. (2022), USA
26 Gehad et al. (2021), Egypt
Report from
individual RT
department
10 Not published, UK, 2022
21 Not-published, UK, 2021
Figure 3: The high-level architecture of i-SART.
3
https://vuejs.org/
4
https://github.com/ecomfe/vue-echarts
i-SART: An Intelligent Assistant for Safety Analysis in Radiation Therapy
423

Figure 4: A screenshot of the administrator’s dashboard
screen in i-SART.
4.2 Cleaning Data to Eliminate
Duplicates
Very soon however, we discovered that these “raw”
FMs contained many duplicates and ambiguities,
inherent to any text formulated in natural language.
We distinguished two types of duplicates: explicit,
defined as two exactly same FMs, which were easy to
detect, and implicit duplicates, where the semantics
was the same, but the syntax was different, which
were more difficult to detect. For example, we
considered the following two FMs as implicit
duplicates.
Collision risk due to gantry rotation
Gantry collision with visual aid device
We detected implicit duplicates using both manual
review by our RT expert team, and automated Natural
Language Processing (NLP) algorithms. For
example, first, the RT experts extracted a group of
keywords such as wrong, poor, imperfect, to help to
identify potential duplicates. Next, for each keyword,
all kinds of forms (i.e., verb, adjective, noun, adverb,
singular, plural) were generated using two NLP
libraries called inflect
5
and word-forms
6
and finally
were added to the keyword list. While we were aware
that words like "poor" and "wrong" may have
different causes and effects, we considered two FMs
containing these words as candidates for duplicates.
We eventually classified them as real duplicates only
after a thorough validation by our RT experts.
Next, we inspected FMs that exhibited a tree-like
structure. For instance, let us take a look at the
5
https://pypi.org/project/inflect/
following FMs, belonging to the subprocess Imaging
and its step “CT image acquisition”:
Wrong CT scan for treatment planning: wrong choice
of anatomical volumes
Wrong CT scan for treatment planning: fiducial
markers not implanted
Wrong CT scan for treatment planning (Vero®):
Optoelectronic markers not completely included into
the scan
Wrong CT scan for treatment planning
(CyberKnife®): scan volume not compliant to the
specifics requirements of the TPS
In all these four FMs, the text to the left of the colon
(:) describes the same unsafe situation (Wrong CT
scan), whereas the text to the right of the colon is an
elaboration on the specific causality. We suspected
that these FMs might be treated as implicit duplicates,
or at least be clustered in the same FM group. Again,
this happened in reality only after a validation by the
RT experts.
As a result of all these data-cleaning procedures,
we were able to eliminate 57 explicit duplicates, 37
implicit duplicates based on keywords and 130
implicit duplicates based on the tree-like structure.
Given the fact that an FM can be flagged as duplicate
multiple times by different filtering methods, we took
action to ensure each FM only appears once. As a
result, the total amount of uniquely duplicated FMs
was reduced to 166. Eventually, we ended up with
584-166 = 418 unique FMs, which we entered into the
database. We have to note that this is an indication of
the number of FMs available so far. This work is in
progress. Our team is working on fine-tuning the
application and improving the database. A prototype
of i-SART with approximately this number of FMs
will be soon available to be used and tested by
interested RT practitioners. To conclude, we would
like to emphasize that during the process of
eliminating the duplicates, the final decisions need to
be taken by our RT experts’ team, who will ensure
that no critical FM will get excluded by mistake.
4.3 Augmenting the Database with
Synthetic FMs
Although we were initially satisfied with the way we
populated the i-SART database, we also investigated
the possibility of augmenting the database with new,
synthetic AI-generated FMs. The reason for this was
the consideration that if the database will be used in
6
https://pypi.org/project/word-forms/
HEALTHINF 2024 - 17th International Conference on Health Informatics
424

the future for training machine learning algorithms, a
few hundred FMs will be definitely not sufficient to
achieve a high prediction accuracy. For example,
deep learning models used in NLP use typically
training datasets containing millions of items (Bailly,
2022). In this section, we will present a few
interesting results. We have to note here that these
were separate experiments and none of these results
have been yet implemented in i-SART.
Generative AI (GenAI) is a modern, powerful
technology that can produce new plausible media
content from existing content, including text, images,
audio, etc trying to mimic human creativity. It
originates in the research done at Google in 2017
(Vaswani, 2017) that first analyzed a language trying
to discover patterns in it, and then transformed this
analysis into a prediction on which word or phrase
should come next. Many GenAI algorithms exist,
varying from the probabilistic Naïve Bayes Networks
and Markov Models, to all kinds of feature-based
neural-networks variations, such as recursive neural
networks (RNN), convolutional neural networks
(CNN), and the GPT-2, -3 and -4 series, where GPT
stands for “Generative Pre-trained Transformer”.
Regardless the algorithm, automated text generation
works basically in the same way. In the beginning, all
probabilities or adjustable weights in the neural
network are unknown; we say that the model is not
trained. However, the model can learn these
parameters if provided with a huge number of training
examples. Eventually, when the training is finished,
and one starts with one word (also called prompt), the
model will be able to accurately predict the most
likely next word in a phrase.
Therefore, GenAI seemed a perfect approach
suitable for our purpose. We had a rather small
collection of training text data (the FMs) and we
wanted an AI algorithm to learn how to create more,
synthetic FMs. In line with these thoughts, we
conducted two preliminary experiments that explored
the performance of different GenAI algorithms.
The first experiment, in the context of a MSc CS
graduation project (Haddou, 2022), used two
different algorithms, Markov Chains and ChatGPT-3
to learn how to create new FMs based on an existing
collection. The training database was slightly
different, containing around 600 FMs collected from
literature and a few RT departments in Europe. From
these, eleven FMs that were generated with the
Markov Chains algorithm were presented for
validation to an RT expert. Out of these six were
found useful. There was at least one artificial FM
with a high RPN, namely “Incorrect image data set
associated with patient shifts determined” that was
interpreted by the RT expert as “patient shifts
determined by incorrect image data set”. Another FM
was very interesting because the RT expert had seen
it a lot of times before, namely ‘Patient head’s
position is not ideal’. The RT expert noted that this
FM would never come spontaneously to her mind.
This FM was clearly and correctly generated by the
Markov Chain algorithm.
The GPT-3 algorithm generated eleven FMs that
were also presented to the same RT expert. Out of these,
four of them were found useful. Especially the FM:
“Patient or nurse falls” and “Patient falls down due
to mobile phone dropping on the floor” were very
interesting. We could conclude from here that
synthetic FMs have the potential to raise awareness
or reveal unpredicted hazards that might occur during
any process, not necessarily RT specific.
The second experiment used a Generative
Adversarial Network (GAN) algorithm to generate
artificial FMs (Brophy, 2023). As a training dataset
we used our most recent FM database. GANs are a
branch of GenAI algorithms that consist of two
artificial neural networks, called Generator and
Discriminator (Goodfellow, 2020). The Generator
tries to generate new data as similar to original data
as possible, while the Discriminator’s role is to
determine if the input belongs to the real dataset or
not. The optimization process is characterized as a
game where the generator successfully learns to
“fool” the discriminator in such a way that the
discriminator cannot distinguish between the real one
and the synthetic one. In particular, our experiment
used the seqGAN model (Yu, 2017).
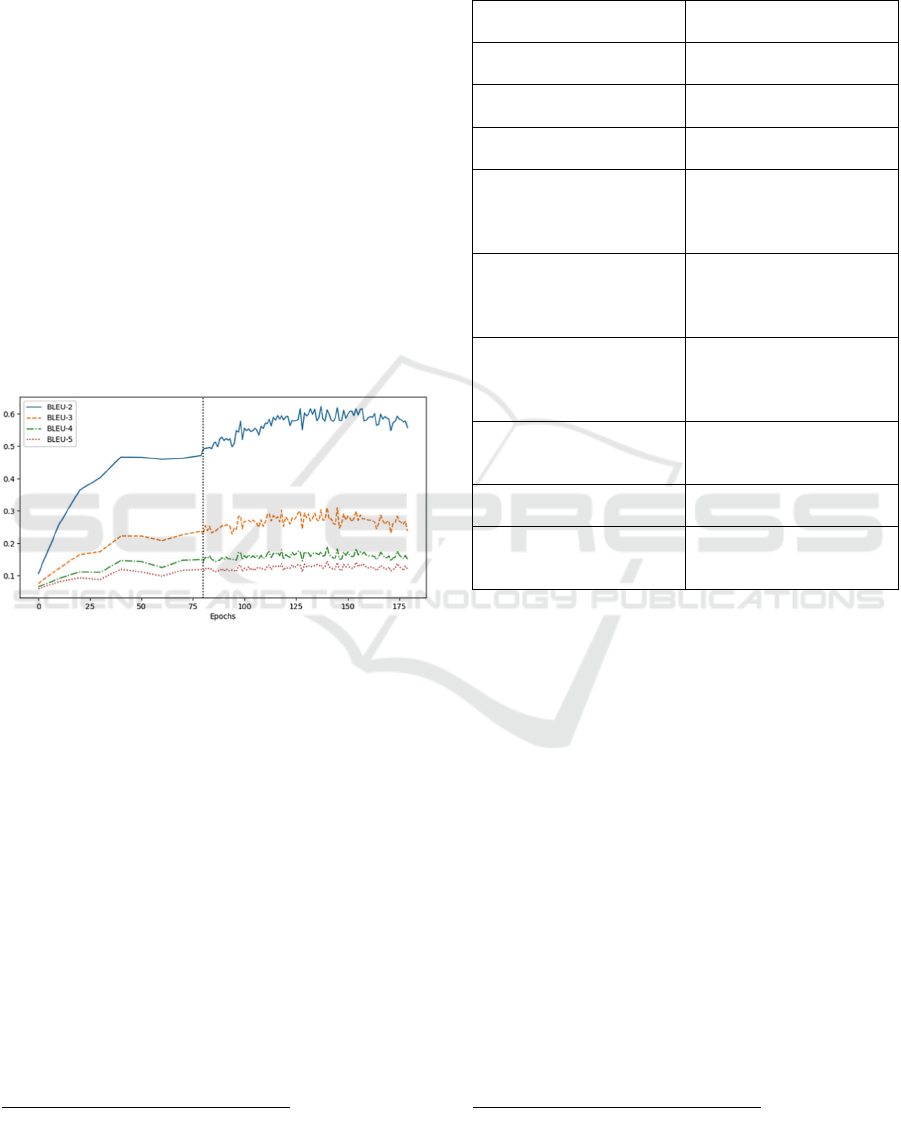
The Bilingual Evaluation Understudy (BLEU)
score was one of the metrics used to measure the
quality of the FMs produced by the generative
algorithm. The basic idea of the BLEU score is
straightforward: the closer the synthetic FM is to the
human-generated target sentence, the better it is; a
score of 1 means a perfect match, and 0 means no
match. A BLEU-score has different levels (n),
depending on how many n-grams are being
compared. For example, if n=1, each word from the
original and synthetic text will be compared, and if
n=2, each word pair will be matched. As training
data we used all the 584 raw FMs initially collected
as described in section 4.1, plus 1721 FM taken from
the headlines of incidents reported in IAEA
SAFRON, (SAFety in Radiation ONcology), an
i-SART: An Intelligent Assistant for Safety Analysis in Radiation Therapy
425
international platform that collects RT incidents and
promotes patient safety
7
.
The seqGAN model implemented in Pytorch
8
was
able to create additional 640 artificial FMs. From
these, 230 were identified as useful by an RT expert,
with 53 duplicates. A handful of them (only 9) were
considered as really novel with respect to the existing
FMs in the database (see Table 2). However, so far
we found that the synthetic FMs lacked syntactic
accuracy and clarity. Fig. 5 shows the performance of
the seqGAN algorithm measured using the BLEU
scores with levels n = 2, 3, 4, 5. The black dot line
splits the training into two phases: 1) Before the
divider is the pre-training process where the initial
generator was trained, and 2) after the divider is the
adversarial training process where the generator
continues to update based on the reward from the
discriminator. We can see that the more grams the
calculation of a BLEU score is based on, the lower
the score. In our experiment, the BLEU-2 values were
the highest and reached the maximum
value of 0.6.
Figure 5: The BLEU-[2, 3, 4, 5] scores of the synthetic FM
generation using the seqGAN model.
These first results show that using GenAI algorithms
is an interesting idea to generate synthetic FM.
However, more efforts will be needed in future to
increase their accuracy and eliminate the need of
human judgement.
Finally, we also identified a few limitations to this
approach. For example, when deciding if the newly
generated FM is a valid one, we consulted only one
RT practitioner, while the assessment of any FM in a
process needs an RT team. Moreover, we didn’t
include the steps in which an FM could occur. This
would bring more clarity to the results. We also
expect that a larger FM dataset will also improve the
accuracy. This will happen in time, when i-SART will
be used by a large community of RT practitioners.
Moreover, while AI integration is innovative, there’ s
7
https://www.iaea.org/resources/rpop/resources/databases-
and-learning-systems/safron
a risk of overconfidence in AI-generated FMs without
adequate human oversight.
Table 2: Novel, synthetic FMs created using GANs.
Synthetic Failure mode Correction/Comments
b
y
RT ex
p
ert
incorrect isocentre not
use
d
incorrect isocentre used
patient positioning with
wrong tattoo
(Nice! I haven’t seen this
in the 584 FMs!)
patient was treated with
wron
g
side of tattoo
(sounds similar to
p
revious one
)
incorrect selection of
appointments delivery
recorded on verification
s
y
stem
incorrect selection of
appointments on record
and verify system
PTV received higher and
treated on the patient
A higher dose was
prescribed for the PTV*
and was delivered to the
patient
incorrect collimator
angles not imported
collimator angles not
imported (Yes, although
I’m not sure if this is
technicall
y
p
ossible.
)
old treatment protocol use of the old treatment
protocol instead of the
new one
wrong field size on portal
ima
g
e
this is fully correct
planned for the wrong
beam angles for one of
treatment fields
wrong beam angles for
one of treatment fields
*PTV means Planning Target Volume and is the region
around the tumor that needs to be irradiated
5 CONCLUSION AND FUTURE
WORK
We presented i-SART, a novel web-application that
aims to assist RT practitioners in conducting a sound
proactive safety assessment using FMEA. i-SART is
the result of a successful cooperation between RT and
computer science researchers. Central is an FM
database that can grow due to contributions from
participating users. We also experimented with
machine learning techniques, such as NLP for
duplicates elimination and generative AI to create
synthetic FMs. We conclude that although machine
learning can be useful in assisting a safety assessment
process, the results need to be always validated by RT
experts. Future work includes optimizing the machine
learning algorithms, including a variety of other
8
https://github.com/williamSYSU/TextGAN-PyTorch
HEALTHINF 2024 - 17th International Conference on Health Informatics
426

safety analysis methods besides FMEA and
investigating the possibilities to offer i-SART as an
open-source collaborative tool for the international
RT community with the common goal of contributing
to a safe and fair global healthcare.
ACKOWLEDGEMENTS
We would like to thank prof. Annette ten Teije for her
support in pursuing our research. A prototype of i-
SART is currently hosted in the SciCloud, a virtual
server service for research offered by the Vrije
Universiteit in Amsterdam.
REFERENCES
Arnzen, H.E. (1966). Failure Modes and Effect Analysis:
Powerful Engineering Tool for Component and System
Optimization. Reliability and Maintainability
Conference, 355-71.
Bailly, A. et al. (2022). Effects of dataset size and
interactions on the prediction performance of logistic
regression and deep learning models. Computer
Methods and Programs in Biomedicine, Volume 213,
106504.
Bright, M. et al. (2022). Failure modes and effects analysis
for surface-guided DIBH breast radiotherapy. Journal
of applied clinical medical physics, 23(4), e13541
Borrás, C. et al. (2006). Overexposure of radiation therapy
patients in Panama: problem recognition and follow-up
measures. Revista Panamericana de Salud Pública,
20(2-3), 173-187.
Brophy, E. et al. (2023). Generative Adversarial Networks
in Time Series: A Systematic Literature Review. ACM
Comput. Surv. 55, 10, Article 199.
Council of the European Union. (2014). Directive
2013/59/Euratom on basic safety standards for
protection against the dangers arising from exposure to
ionising radiation and repealing Directives
89/618/Euratom, 90/641/Euratom, 96/29/Euratom,
97/43/Euratom and 2003/122/Euratom, Official
Journal of EU. L13; 57:1-73.
deRosier, J. et al. (2002). Using health care failure mode
and effect analysis. Joint Commission J. Qual.
Improvement 27, 248–267.
Ford, E. and Evans, S.B. (2018). Incident learning in
radiation oncology: A review, Medical Physics, 45:
e100-e19.
Gehad, S.M. et al. (2021). Failure Mode and Effect
Analysis for Three Dimensional Radiotherapy at Ain
Shams University Hospital, Int. J. of Adv. Res. 9 (Dec).
971-983.
Gilmore, M. D. and Rowbottom, C. G. (2021). Evaluation
of failure modes and effect analysis for routine risk
assessment of lung radiotherapy at a UK center. Journal
of applied clinical medical physics, 22(5), 36-47.
Goodfellow, I. et al. (2020). Generative adversarial
networks. Communications of the ACM, 63(11), 139-
144.
Haddou, S. 2022. iSART: Digital safety assistant for the
radiotherapy process. Msc CS thesis, Vrije Universiteit
Amsterdam.
Huq, M. S. et al. (2016). The report of Task Group 100 of
the AAPM: Application of risk analysis methods to
radiation therapy quality management, Medical
Physics, 43: 4209-62.
Ibanez-Rosello, B. et al. (2018). Failure modes and effects
analysis of total skin electron irradiation technique.
Clinical and Translational Oncology, 20(3), 330-365.
International Atomic Energy Agency (IAEA). (2018).
Radiation protection and safety in medical uses of
ionizing radiation. Safety Standards Series No. SSG-
46;
Kane, P., The impact of the VERT virtual reality system on
teaching and learning associated with radiation therapy
planning skills in the second year of the Bachelor of
Radiation Therapy. 2014
Leveson, N.G. and Turner, C.S. (1993). An investigation of
the Therac-25 accidents, in Computer, vol. 26, no. 7,
18-41.
National Cancer Institute (NCI). (2017). Cancer Statistics,
https://www.cancer.gov/, Accessed online 7-10-2023.
Olch, A. (2014). Quality and Safety in Radiation therapy
Learning the New Approaches in Task Group 100 and
Beyond, Medical Physics, 41: 067301.
Ortiz-Lopez, P. et al. (2009). Preventing accidental
exposures from new external beam radiation therapy
technologies. Ann ICRP, 39(4):1e86.
Pawlicki, T. et al. (2011). Quality and Safety in Radiation
therapy (CRC Press).
Pawlicki, T. et al. (2016). Application of systems and
control theory-based hazard analysis to radiation
oncology. Medical Physics, 43(3):1514-30.
Pobbiati, C. et al. (2019). Clinical risk analysis of the
patient’s path in an Advanced Radiotherapy Center
through FMEA method. Journal of Biomedical
Practitioners, 3(1).
Sarchosoglou, A. et al. (2022). Failure modes in stereotactic
radiosurgery. A narrative review, Radiography,
Volume 28, Issue 4, Pages 999-1009.
Silvis-Cividjian, N. et al. (2020). Using a systems-theoretic
approach to analyze safety in radiation therapy-first
steps and lessons learned. Safety Science, 122, 1-10.
Vaswani, A. et al. (2017). Attention is all you need. In
Proceedings of the 31st International Conference on
Neural Information Processing Systems (NIPS'17).
6000–6010.
Yu, L. et al. (2017). SeqGAN: Sequence generative
adversarial nets with policy gradient. In Proceedings of
the AAAI conference on artificial intelligence (31,1).
i-SART: An Intelligent Assistant for Safety Analysis in Radiation Therapy
427
