
Na
¨
ıve Bayes as a Probabilistic Tool for Monitoring the Health Status of
Chronic Patients
Laura Teresa Mart
´
ınez-Marquina
1 a
, Mar
´
ıa Teresa Jurado-Camino
1 b
,
Isabel Caballero-L
´
opez-Fando
2 c
and Inmaculada Mora-Jim
´
enez
1 d
1
Dept. Signal Theory and Communications, Telematics and Computing Systems, Rey Juan Carlos University, Madrid, Spain
2
University Hospital of Fuenlabrada, Madrid, Spain
Keywords:
Interpretability, Time-Dependent Patterns, Clinical Codes, Sex-Based Model, Clinical Decision Support.
Abstract:
Chronic diseases have emerged as a pervasive global health concern, standing as a leading cause of mortality.
Among these, prevalent conditions encompass diabetes, hypertension, congestive heart failure and chronic
obstructive pulmonary disease. The large amount of data in Electronic Health Records is being exploited by
machine learning schemes to design clinical decision support systems, usually of limited practical application
because of lack of transparency. To overcome this issue and given the dynamic nature of the health-status
over time, we propose here a patient health monitoring scheme based on a N
¨
aive Bayes approach because of
its interpretability, minimal computational cost, and efficient handling of high-dimensional and unbalanced
data. Our approach considers clinical codes (diagnosis and drugs) on real data collected by a Spanish hospital
and provides a probability score for different chronic health-statuses. A gender-based approach has also been
explored, exhibiting promising performance when there is a significant patient population for each sex. We
conclude that pharmacological codes are more informative, although the best performance was obtained by
using all the clinical codes and demographic features. Though a more exhaustive study on patient monitoring
is necessary, the proposed NB scheme can be considered a proof of concept which has demonstrated to be a
valuable tool and easily interpretable method.
1 INTRODUCTION
In recent years, there has been an alarming increase in
the number of chronic patients, mainly in developed
countries, due to the aging global population. Nearly
50% of the United States population (Raghupathi and
Raghupathi, 2018) and 35% in Europe (Nolte et al.,
2014), has some type of Chronic Condition (CC). CCs
are the main cause of morbidity, being largely re-
sponsible for activity limitations in older adults and
causing 60% of mortality (Atella et al., 2019). Fur-
thermore, CCs entail significant socioeconomic reper-
cussions that directly influence the healthcare sys-
tem, amounting to 25% of the healthcare budget (Van-
denberghe and Albrecht, 2020). This emphasizes
the need for a paradigm change, drawing the atten-
tion not solely towards treating the illness, but rather
a
https://orcid.org/0009-0007-4975-1162
b
https://orcid.org/0000-0002-5646-1290
c
https://orcid.org/0000-0003-0193-4406
d
https://orcid.org/0000-0003-0735-367X
towards its prevention (Vandenberghe and Albrecht,
2020) or slowing its progression. In this scenario, ar-
tificial intelligence and data-driven models can be of
great assistance in achieving the well-known “Triple
Aim” of healthcare systems, which is based on im-
proving patient care experience, enhancing popula-
tion health, and reducing medical care costs (Berwick
et al., 2008).
In the healthcare context, Machine Learning (ML)
is bringing about a true revolution, with increasing
investment in research over the last decade. Auto-
matically deriving insights from longitudinal Elec-
tronic Health Records (EHR) data offers new po-
tential for clinical research, as patient information
evolves through healthcare interactions (Zhao et al.,
2017) across time. One of the main challenges of ML
models on healthcare is their lack of interpretability.
Ignoring this issue could greatly hinder the real-world
utilization of data-driven models (Vellido, 2020).
Owing to the worsening effects of CCs, studying
the temporal progression of chronic patients is vital.
Given that their clinical journey is mirrored in diag-
Martínez-Marquina, L., Jurado-Camino, M., Caballero-López-Fando, I. and Mora-Jiménez, I.
Naïve Bayes as a Probabilistic Tool for Monitoring the Health Status of Chronic Patients.
DOI: 10.5220/0012353000003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 393-403
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
393

nosis and medication timelines, our paper suggests
utilizing this data for health status monitoring and
prediction. In the clinical setting, these predictions
could be used by healthcare experts to establish in-
tervention measures to slow down the progression of
the CC. Specifically, in this paper we have considered
demographic and clinical data of chronic patients as-
sociated with the University Hospital of Fuenlabrada
(UHF) in Madrid region (Spain), with the research
being previously approved by the Ethics Committee
of the UHF. Our research group has already pub-
lished some works in this topic, focusing on diabetic
and hypertensive population (Soguero et al., 2020;
Chushig-Muzo et al., 2022; Chushig-Muzo et al.,
2020; Chushig-Muzo et al., 2021). In contrast to our
previous articles, our focus in this paper expands the
variety of CC and delves into the temporal monitor-
ing of the chronic patient’s health status. Specifically,
we deal here with the following CC: diabetes, hyper-
tension, congestive heart failure, and chronic obstruc-
tive pulmonary disease. Another distinction from our
prior studies involves accounting for the sex variable.
Though both genders demonstrate an escalating CC
risk with age, this rise is often more dramatic among
women (Ellis et al., 2022).
Thus, examining risk factors independently for
men and women could substantially enhance the ef-
ficacy of tailored interventions for each gender.
As in our previous works, the identification of
the chronic patients is carried out using the annual
records of each patient and the Clinical Risk Group
population grouper, since it is internationally vali-
dated (Hughes et al., 2004).
To characterize the patient’s health status over
time, we propose in this paper to use the Na
¨
ıve Bayes
(NB) scheme (Mitchell, 1997) due to its simplicity,
efficiency in the handling of a large number of vari-
ables, complexity, transparency and interpretability,
all of these very important items in clinical decision
support systems. NB has been successfully applied
within the medical domain (Al et al., 2012; Bhu-
vaneswari and Kalaiselvi, 2012; Hickey, 2013), en-
compassing a wide range of scenarios from estimating
the risk of post-partum depression (Jim
´
enez-Serrano
et al., 2015) to, more recently, predicting the diagno-
sis of Alzheimer’s disease (Chang et al., 2021). In
this work, the NB approach has been used by con-
sidering both, continuous (age) and categorical vari-
ables (diagnosis and drug codes). As the NB classifier
relies on the Maximum A Posteriori (MAP) decision
rule (Demirbas, 1988), its probabilistic foundation en-
ables identification of the most likely CC for a patient
within a specific time frame, and also its associated
probability. Note that the MAP rule takes into consid-
eration the prior probability for every CC, so a care-
ful analysis when dealing with highly unbalanced CC
must be considered.
The rest of the paper is structured as follows.
Section 2 presents our dataset description and cor-
responding exploratory analysis, focusing on the sex
variable. The methods used for the temporal analysis
and prediction of the patient’s health status are in Sec-
tion 3. Section 4 explains the process followed for the
models’ designs. The results obtained when evalu-
ating different models, just considering demographic
features, their combination with clinical codes, sex-
based models, and the strategy for temporal monitor-
ing are presented in Section 5. Conclusions are drawn
in Section 6.
2 DATASET DESCRIPTION AND
EXPLORATORY ANALYSIS
Demographic and clinical data were extracted from
EHRs linked to the UHF, considering several types
of chronic patients older than 18 years, getting a to-
tal of 16,791 patients (also named samples according
to the ML terminology). Clinical data correspond to
diagnostic and pharmacological records of these pa-
tients, both encoded using internationally recognized
systems. Thus, diagnoses are coded according to the
9th revision of the International Classification of Dis-
eases (ICD-9) and pharmaceuticals coded according
to the Anatomical Therapeutic Chemical (ATC) clas-
sification system (Ronning, 2002).
The ICD-9 code consists of 5 Alpha-Numeric
Characters (ANCs) with a decimal point between
the third and fourth ANCs. Owing to the inclusion
of new codes, this system has been renamed with
the suffix CM (Clinical Modifications), ultimately re-
ferred to as ICD-9-CM (Association, 2004). The
ATC code consists of 7 ANCs hierarchically struc-
tured into several levels: anatomical (first ANC, first
letter of the anatomical group where the drug acts),
therapeutic subgroup (second and third ANCs), phar-
macological (fourth ANC), and chemical subgroup
(fifth ANC). Although a quite complete definition of
the pharmacological code is obtained with the first
five ANCs, the chemical substance (sixth and seventh
ANCs) provides additional information. To reduce
data dimensionality (number of clinical codes) and in
line with the methodology of previous studies in our
group (Chushig-Muzo et al., 2022), we only consider
here the first three digits of the ICD-9-CM and the five
digits of the ATC codes, resulting in 1,517 diagnosis
features and 746 drug features.
As in our previous works (Chushig-Muzo et al.,
HEALTHINF 2024 - 17th International Conference on Health Informatics
394

2022; Soguero et al., 2020; Chushig-Muzo et al.,
2020; Chushig-Muzo et al., 2021), chronic patients
were clinically identified according to a Population
Classification System named Clinical Risk Groups
(CRGs), internationally validated and oriented to-
wards chronic patients (Hughes et al., 2004).
This system considers demographic factors (age
and sex), clinical attributes (diagnoses, procedures,
and medications), and the corresponding dates of pa-
tient encounters over a specified time frame, typically
one year. Its purpose is to assign each patient to one
of the 1,080 health statuses. The identification of the
CRG health groups is denoted by a 5-digit code. The
first digit represents the overall patient’s health sta-
tus, with 9 potential core health statutes: 1 (healthy),
2 (significant acute disease), 3 (single minor CC), 4
(minor CC in multiple organ systems), 5 (single dom-
inant or moderate CC), 6 (significant CCs in multiple
organ systems), 7 (dominant CC in 3 or more organ
systems), 8 (dominant and metastatic malignancies)
and 9 (catastrophic condition). The next three digits
represent a more specific health condition and are re-
ferred to as base-CRG. The last digit is the severity
level (not considered here).
As CRGs provide a clinically accepted categoriza-
tion for identifying patients with significant CCs, they
can be employed as the ground truth to guide a super-
vised ML task and construct a predictive model of the
patient’s health status. For this purpose, this study
considers the more prevalent CCs: Congestive Heart
Failure (CHF), Hypertension (HT), Diabetes (DIA)
and Chronic Obstructive Pulmonary Disease (COPD).
Since we will consider these CC and the combina-
tion of them, finally we will select only a total of
10 health status groups, from the 1,080 status groups
available in the CRG system. Thus, patients with only
one CC are assigned to CRGs where the first digit is
5, i.e, CRG-5179 (CHF), CRG-5192 (HT),and CRG-
5424 (DIA). Note that COPD has not an specific CRG
group. Individuals with two simultaneous CCs are as-
signed to CRGs starting with the number 6, i.e., CRG-
6190 (CHF and COPD), CRG-6191 (CHF and DIA),
and CRG-6313 (HT and DIA). Groups linked to more
than two simultaneous CCs start with the number 7,
i.e, CRG-7060 (CHF, DIA and COPD), CRG-7080
(CHF, DIA and other CC), CRG-7081 (CHF, COPD
and other CC), and CRG-7140 (HT, DIA and other
CC).
Considering all the previous aspects, the database
comprised 16,791 patients with anonymous data
records from the UHF, each uniquely identified with
an ID and associated with just one of the aforemen-
tioned 10 CRG groups. For each patient, demo-
graphic data (age, sex) and clinical data (diagnoses,
procedures, drugs) recorded during one year are avail-
able, along with the corresponding registration dates.
All this information is used by the CRG system to
assign every patient to one CRG group. Table 1 sum-
marizes the demographic data per CRG.
Table 1: Statistics per CRG: number of patients, % of
women and age (average, and standard deviation in brack-
ets).
CRG
# Patients Women (in %) Age
5179 114 66.7 68.9(13.8)
5192 10,126 56.3 57.9(12.0)
5424 1,939 40.6 53.9(15.6)
6190 96 56.2 79.0(11.7)
6191 120 66.7 72.6(11.6)
6313 3,228 47.7 62.3(10.7)
7060 159 59.1 70.6(10.9)
7080 93 59.1 73.3(12.5)
7081 187 50.8 80.8(11.9)
7040 729 58.2 67.4(10.9)
Following our previous analysis (Chushig-Muzo
et al., 2022; Soguero et al., 2020; Chushig-Muzo
et al., 2020; Chushig-Muzo et al., 2021), every
patient is characterized by a binary feature vector
x = [x
1
, x
2
, ··· , x
d
, · ·· , x
D
] with x
d
∈ {0, 1}, com-
posed by 1,517 diagnoses codes and 746 drug ones
(D = 2,263 features). Each element of x is encoded
with a value of ‘1’ if the corresponding code was reg-
istered for the patient some time during the year, and
with ‘0’ otherwise. Thus, we can compute the pres-
ence rate for each code and CRG, creating the named
“profile” for each CRG when considering all codes in
a bar graph, as shown in other publications (Chushig-
Muzo et al., 2021; Jurado-Camino et al., 2023) and
not presented here for limitation space.
To gain knowledge of the most prevalent clini-
cal code per sex linked to each CRG, an exploration
of the profiles was carried out. The presence rate
of the most common diagnosis and pharmacological
codes on each CRG, separated by sex, is summa-
rized in Tables 2 and 3, respectively. Note that the
ICD-9-CM code with the highest presence rate in al-
most all the considered CRGs (excepting CRG-5424)
is ‘401’, representing Essential Hypertension (EHT).
This is a result of the tight relation between HT and
CHF (Pugliese et al., 2020), as well as of the asso-
ciation between insulin resistance and elevated blood
pressure (Sowers, James R and Frohlich, Edward D,
2003). Other diagnosis codes with high rate are ‘428’
(heart failure) and ‘250’ (diabetes mellitus), which are
commonly associated with all CRGs linked to cardio-
vascular and diabetic patients, respectively.
The highest presence rates in pharmacological
Naïve Bayes as a Probabilistic Tool for Monitoring the Health Status of Chronic Patients
395

codes are summarized in Table 3. The most preva-
lent medications start with the letters A, B, C, and
N. In line with the anatomical classification previ-
ously presented, these letters represent the Alimen-
tary, Blood, Cardiovascular, and Nervous systems, re-
spectively. Although drugs beginning with A tend
to be more associated with DIA and those beginning
with C with cardiac problems, there are drugs com-
monly used across all CRGs as paracetamol or ibupro-
fen which primarily affect the Nervous system. These
medications show some differences between women
and men, which could be linked with period pains.
Table 2: Presence rate in each CRG when considering six
of the most prevalent ICD-9-CM codes. Highest value for
each CRG and sex (Men M and Women W ) are in bold.
IDC-9-CM Codes
250 272 401 427 428 719
CRG M W M W M W M W M W M W
5179 0.03 0.05 0.29 0.16 0.40 0.42 0.50 0.39 0.67 0.43 0.14 0.14
5192 0.01 0.01 0.18 0.20 0.70 0.68 0.01 0.01 0.00 0.00 0.10 0.16
5424 0.78 0.77 0.17 0.17 0.06 0.07 0.00 0.00 0.00 0.00 0.10 0.12
6190 0.00 0.02 0.47 0.31 0.58 0.66 0.51 0.32 0.79 0.76 0.09 0.12
6191 0.66 0.79 0.24 0.32 0.32 0.63 0.31 0.44 0.48 0.52 0.15 0.17
6313 0.78 0.76 0.22 0.26 0.57 0.63 0.01 0.01 0.00 0.00 0.10 0.16
7060 0.85 0.77 0.42 0.42 0.54 0.58 0.51 0.45 0.66 0.82 0.13 0.12
7080 0.86 0.84 0.57 0.44 0.51 0.65 0.25 0.38 0.62 0.62 0.07 0.11
7081 0.16 0.26 0.23 0.44 0.42 0.59 0.58 0.56 0.85 0.83 0.03 0.10
7140 0.75 0.72 0.24 0.23 0.58 0.62 0.03 0.01 0.01 0.01 0.11 0.15
Table 3: Presence rate in each CRG when considering six of
the most prevalent ATC codes. Highest value for each CRG
and sex (Men M and Women W ) are in bold.
ATC Codes
A02BC A10BA B01AA C03CA C10AA N02BE
CRG M W M W M W M W M W M W
5179 0.69 0.67 0.00 0.00 0.64 0.67 0.76 0.82 0.60 0.46 0.52 0.72
5192 0.33 0.47 0.00 0.00 0.01 0.01 0.02 0.05 0.33 0.35 0.32 0.50
5424 0.27 0.41 0.57 0.49 0.00 0.01 0.01 0.02 0.49 0.44 0.29 0.44
6190 0.97 0.89 0.00 0.00 0.70 0.41 0.92 0.95 0.70 0.44 0.82 0.90
6191 0.74 0.88 0.65 0.38 0.61 0.61 0.95 0.94 0.66 0.72 0.62 0.76
6313 0.42 0.62 0.68 0.68 0.01 0.02 0.05 0.07 0.68 0.69 0.35 0.56
7060 0.91 0.91 0.39 0.37 0.43 0.62 0.97 0.98 0.64 0.62 0.80 0.91
7080 0.80 0.97 0.27 0.42 0.17 0.43 1.00 0.95 0.75 0.58 0.74 0.88
7081 0.96 0.97 0.08 0.10 0.40 0.50 0.99 0.98 0.38 0.47 0.94 0.96
7140 0.65 0.75 0.59 0.62 0.05 0.03 0.12 0.14 0.60 0.66 0.52 0.69
3 METHODS
We present here the fundamentals of the probabilis-
tic approach used for prediction purposes, as well as
the data preprocessing applied for subsequent tempo-
ral monitoring.
3.1 Na
¨
ıve Bayes for Heterogeneous Data
Based on the Bayes’ conditional probability theo-
rem, the NB approach has shown good results un-
der the na
¨
ıve assumption that features are class in-
dependent (Mitchell, 1997). NB belongs to the fam-
ily of MAP classifiers (Demirbas, 1988), which cal-
culate the probability of the class conditioned to an
specific feature vector. It stands out for its strong
computational efficiency and ability to handle high-
dimensional data effectively (Hickey, 2013; Al et al.,
2012; Jim
´
enez-Serrano et al., 2015; Bhuvaneswari
and Kalaiselvi, 2012; Chang et al., 2021). NB can
also use features of diverse nature (heterogeneous
data).
As shown in Equation (1), given a set of C classes
(C = 10 in this work) and vector x, the NB scheme
assigns to x the class maximizing the posterior prob-
ability P(c
i
|x).
argmax
c
i
P(c
i
|x) = argmax
c
i
P(x|c
i
)P(c
i
)
P(x)
,
i = 1, ..., C
(1)
where P(c
i
) is the prior probability of class c
i
, P(x|c
i
)
is the likelihood of class c
i
and P(x) is the marginal
probability.
For the application of this NB framework, the na-
ture of the considered variables must be taken into
account. In the context of this study, heterogeneous
data are used, considering both binary features (pres-
ence/absence of clinical and pharmacological codes,
represented by features named as x
d
and coded as
‘1’/‘0’, respectively) and the numerical feature “age”
(represented by the feature named x
r
). Thus, the
D-dimensional binary vector x is transformed into a
D+1-dimensional one named x’ when considering the
“age” attribute too. As a result, according to NB, the
likelihood of class c
i
is estimated as:
ˆ
P(x
′
|c
i
) =
"
D
∏
d=1
ˆ
P(x
d
= 1|c
i
)
b
(1 −
ˆ
P(x
d
= 1|c
i
))
1−b
#
ˆ
P(x
r
|c
i
), i = 1, ·· · , C, b ∈ {0, 1}
(2)
with the part within brackets representing the esti-
mation of the likelihood of vector x following the
Bernoulli distribution (Sinharay, 2010), and
ˆ
P(x
d
=
1 |c
i
) is estimated as the relative frequency of the d-th
feature when it is “on” (x
d
= 1). However, this may
lead to a probability of 0 for feature values that are
absent in the dataset, significantly affecting the esti-
mation provided by Equation (2). To ensure non-zero
likelihoods, a common practice is to apply Laplace
smoothing (Kibriya et al., 2005).
Regarding the “age” variable, since the number of
potential values is high (between 18 and 103 in this
work), to use a frequentist approach with every possi-
ble value can lead to very abrupt changes in the prob-
ability between consecutive age values, especially in
HEALTHINF 2024 - 17th International Conference on Health Informatics
396
CRGs with few patients. To address this issue, we
proceed as if it were a continuous variable, obtaining
the probability in intervals. In this work, the follow-
ing six intervals were established for x
r
on the basis
of the exploratory analysis: ≤ 29; 30-40; 41-49; 50-
59; 60-74; ≥75. Though the relative frequency could
be used for estimating probabilities in each interval,
we empirically found using synthetic data that more
acute estimates were provided when getting the prob-
ability density function (pdf ) in a non-parametric way
by using Gaussian kernels and the Parzen windows
method (Parzen, 1962; Silverman, 1986) and then in-
tegrating it to have the corresponding probability. Fig-
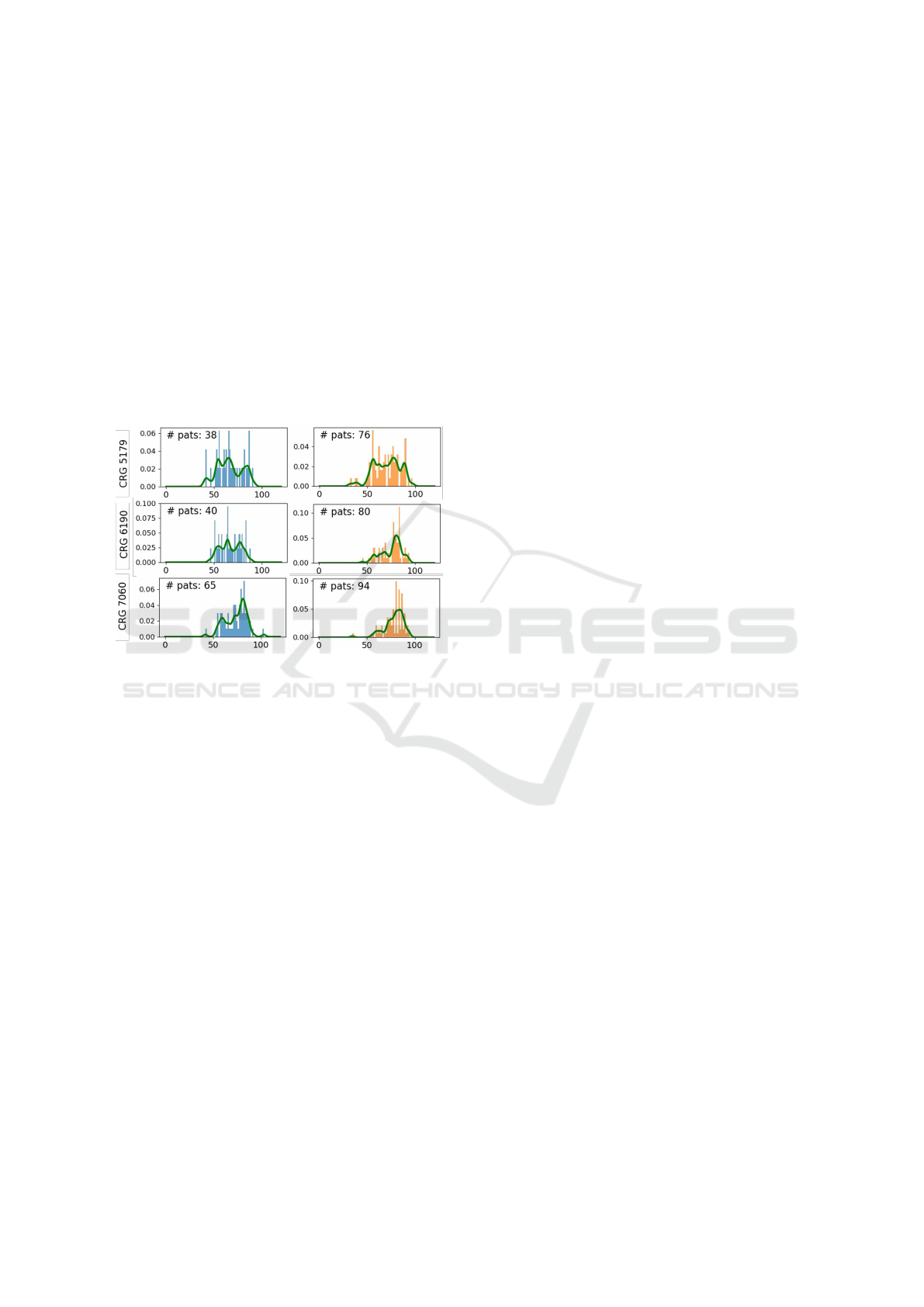
ure 1 shows both approaches for CRG-5179, CRG-
6190 and CRG-7060, both for women and men.
Figure 1: Normalized histograms for the age (left panels,
blue, for men; right panels, orange, for women) and corre-
sponding pdf estimation using Parzen windows (in green).
3.2 Data Preprocessing for Temporal
Monitoring
In healthcare, time series are usually irregularly sam-
pled, with irregular temporal intervals between two
consecutive clinical registers. To address this is-
sue,pharmacological data, reported on a monthly ba-
sis, are used in this work. However, the peculiarities
of the Spanish health system, with a different EHR in
each Spanish region (17 regions, with no interoper-
ability between EHRs), can lead to data gaps in one
of them over extended periods of time. These gaps
may arise from factors like lengthy vacation periods,
during which patients are away from their usual res-
idence, resulting in no registration of the medication
dispensation in their region. These gaps manifest as
missing data in the patient’s EHR accessible by the
UHF.
In order to overcome the difficulties in the analysis
produced by the lack of encounters with the regional
health system, we carry out a preprocessing stage us-
ing temporal data.
In particular, we propose to use a exponential
weighting function ensuring that the drug presence
is not deactivated abruptly in the next month if the
drug dispensation has not been registered. Instead,
for each feature, exponential weighting functions are
added and the result is used to create the new binary
temporal values for the corresponding feature x
d
af-
ter thresholding. Figure 2 shows an example of the
temporal vector with twelve months, with the phar-
macy symbol indicating that the drug has been col-
lected (see the binary feature, with ‘1’ value in Feb,
Apr, May, Jul, Oct, Nov and Dec). Since the exponen-
tial function is continuous and we just have one value
per month, the exponential weighting function of one
month length (blue line in Fig. 2) is sampled every
month. As displayed in Figure 2, when the sampled
value is above the threshold (0.5, dotted red line), for
each month the corresponding element is set to ‘1’
(‘0’, otherwise) in the preprocessed feature. The new
temporal sequence of values is shown in Fig. 2 as in-
terpolated monthly feature. Note that, even when the
drug is not dispensed on a monthly basis, the new val-
ues exhibit a scenario most similar to the ideal one
(regular drug dispensation, linked to permanent use
by chronic patients).
To deal with temporal data, it is common the use
of sliding windows (Chen et al., 2017). In this work,
the window length gather data over three months, en-
compassing also data from the preceding two months
before the target month in which we want to predict
the patient’s health status.
4 EXPERIMENTAL DESIGN
We detail here the procedure to create the design and
test sets, to overcome overfitting and achieve good
generalization capabilities. Next, the model construc-
tion is explained.
4.1 Experimental Setup
For this study the dataset was split into design and test
sets in a proportion of 70%-30%. The design set, used
to train the NB model using feature vectors summariz-
ing annual encounters, was further split into training
(80%) and validation set (20%). The test set was used
to evaluate the NB model considering two time scales:
annual and quarterly. To avoid a bias linked to the use
of a particular split, 10 different training-validation-
test splits X = {X
1
, ..., X
10
} were performed.
Since feature vectors summarize the encounters
over a relatively long period of time (annual or quar-
Naïve Bayes as a Probabilistic Tool for Monitoring the Health Status of Chronic Patients
397
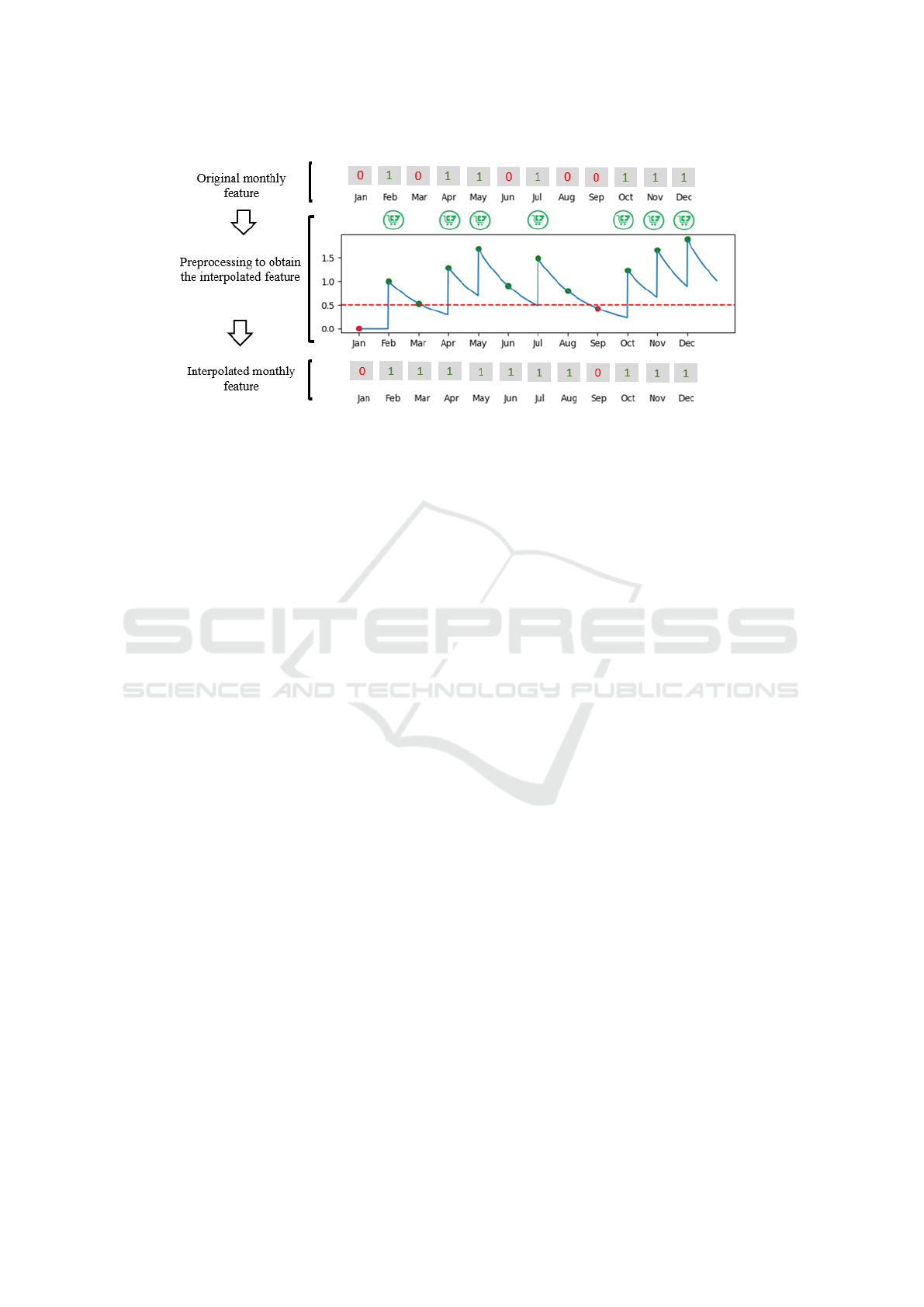
Figure 2: Top panel displays the original monthly feature vector for a specific drug, with ‘1’ representing the drug dispensation
with a pharmacy symbol in green. Middle panel shows the preprocessing applied to the original feature vector by using an
exponential weighting function (in this case, with 1 month decay, see blue line). Bottom panel represents the preprocessed
feature vector after thresholding the previous blue function with a 0.5 value (dashed red line).
terly), it is possible that different patients are repre-
sented by equal vectors.
Taking this into account, and with the intention of
ensuring an appropriate design, it was checked that
patients assigned to different CRGs were not rep-
resented by the same feature vector. Additionally,
identical vectors associated with the same CRG (448
vectors in total) were temporarily removed from the
dataset and grouped together in the set R . Note that
not all vectors in R are identical among themselves,
but each one has at least another identical feature vec-
tor in R . After the initial split of vectors not included
in R into training, validation and test subsets, similar
vectors in R were proportionally distributed in those
subsets, as shown in Figure 3.
Regarding the sex-based models (separating
women and men), a similar setup was carried out
in parallel, resulting in 10 partitions for women
X
F
= {X
F
1
, ..., X
F
10
} and another 10 for men X
M
=
{X
M
1
, ..., X
M
10
}.
4.2 Na
¨
ıve Bayes Model Construction
and Figures of Merit
Several NB models were explored by using the an-
nual summary of clinical variables. First, two models
using separately diagnoses codes and pharmacologi-
cal codes were considered. Second, a model using
both diagnosis and pharmacological (clinical) data,
together with demographic data, was tackled. Finally,
sex-based models were designed.
The NB performance was assessed using various
figures of merit. Besides the accuracy rate for each
CRG, we also considered the multiclass Confusion
Matrix (CM) and the multiclass Receiver Operating
Curves, with their corresponding Areas Under the
Curve (AUC) (Hanley and McNeil, 1982). Together
with the AUC per CRG, we also present the Macro-
Average AUC and the Micro-Average AUC (weighted
average based on the number of patients per CRG),
usually used in multiclass tasks (Fodeh et al., 2021).
For each scenario (different input feature vectors),
10 models were designed (one model per partition
in X ). In the case of sex-based models, partitions
X
M
and X
F
were considered. For the NB hyper-
parameter selection, we explored four values of the
Laplace smoothing parameter {0.01, 0.05, 0.1, 0.5},
being 0.05 or 0.1 the most selected values according
to the the Macro-Average AUC on the validation set
(see Figure 3).
5 RESULTS
This section presents the test results using a summary
of the annual data and also considering sex-based
models. The proof of concept with temporal moni-
toring throughout the year, conducted using pharma-
cological data, is finally presented.
5.1 Using Data Registered over a Year
Binary feature vectors summarizing the patient’s clin-
ical encounters during one year have been considered,
designing two different models: the Diagn-Model
uses only diagnoses features, while the Pharm-Model
just considers pharmacological features. We explored
both equiprobable schemes (yielding best outcomes)
HEALTHINF 2024 - 17th International Conference on Health Informatics
398
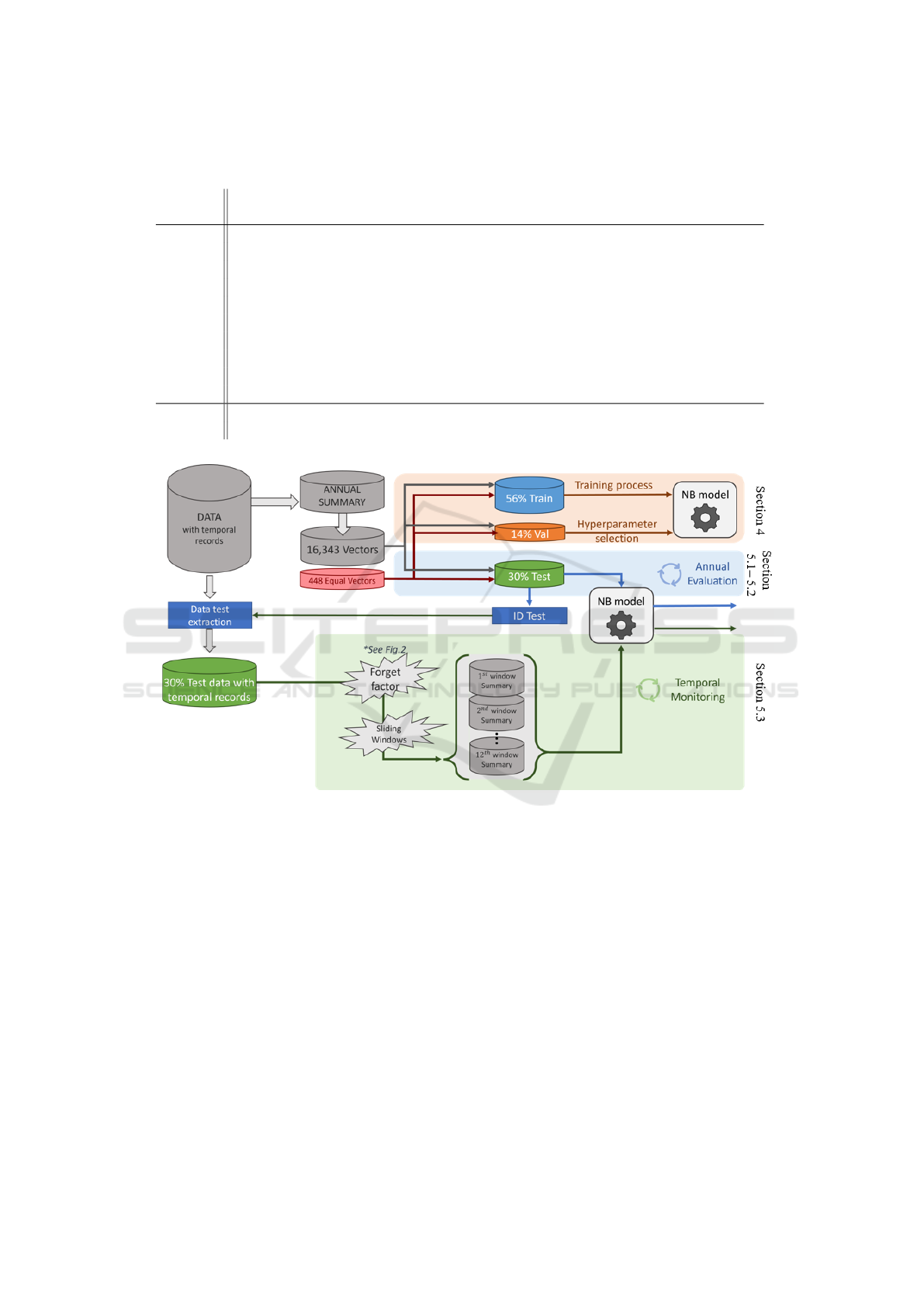
Table 4: Average AUC per CRG (10 test partitions) when using different models, including sex-based ones (rightmost
columns).
CRG
Diagn
Model
Pharm
Model
Clinical&Demog
Model
Clinical&Demog
Men-model
Clinical&Demog
Women-model
5179 0.712 0.801 0.821 0.780 0.840
5192 0.864 0.893 0.952 0.955 0.953
5424 0.793 0.877 0.899 0.903 0.889
6190 0.640 0.711 0.697 0.610 0.636
6191 0.606 0.810 0.775 0.706 0.740
6313 0.729 0.811 0.857 0.869 0.862
7060
0.723 0.734 0.747 0.742 0.752
7080 0.603 0.660 0.636 0.590 0.623
7081 0.800 0.791 0.835 0.829 0.832
7140 0.752 0.725 0.787 0.759 0.803
Macro 0.722 0.782 0.801 0.774 0.793
Micro 0.817 0.862 0.912 0.913 0.914
Figure 3: General framework for the NB model design, annual evaluation and temporal monitoring.
and a priori probability estimates based on the occur-
rence rate. The results presented in this paper corre-
spond to equiprobable schemes.
When analyzing the test CMs with the annual
summary data, we observed that the Diagn-Model
shows more confusion between CRGs linked to one
significant CD (CRGs starting with the number 5).
The Pharm-Model, even using a lower number of fea-
tures, improves the results linked to CRGs with dom-
inant CDs in triplets (CRGs starting with the num-
ber 7), which is of paramount interest due to the
worst health status of patients assigned to this kind of
CRGs. These results show that drug codes are more
informative than diagnosis ones.
Analizing the AUC values in Table 4, an improve-
ment in macro and micro AUC is shown when com-
paring the Pharm-Model with the Diagn-model. We
also observe best AUC values for the Pharm-Model
in most of each particular CRG excepting those in the
core health-status number 7 (more than two dominant
CC). This lack of improvement could potentially be
attributed to the lack of specificity in the third CC
encompassed in this core health-status. Additionally,
note that the annual summary may oversimplify the
patient’s characterization, making the task more diffi-
cult due to the complex patients’ health status within
these limited groups.
We also studied the performance when using all
the clinical (diagnosis and pharmacological) codes
and the demographic variable ‘age’. As expected,
the Clinical&Demog-Model provides the best values
of Macro-Average AUC (0.801) and Micro-Average
Naïve Bayes as a Probabilistic Tool for Monitoring the Health Status of Chronic Patients
399

AUC (0.912) and also the highest AUC for most of
the CRGs. Among those showing no improvement
(see Table 4), the CRG-6190 (CHF and COPD) is
often erroneously associated with CRG-7081 accord-
ing to the CMs in Figure 4. This confusion likely
arises due to the shared CCs (CHF and COPD) and
the lack of specificity in the third CC of CRG-7081
(CHF, COPD, and other CC). Additionally, observa-
tions suggest that when using the Clinical&Demog-
Model, patients within CRG-6191 (CHF and DIA)
display a higher level of confusion with those in CRG-
6313 (HT and DIA). This could be attributed to the
close relationship between CHF and HT, coupled with
the limited specificity of the diagnosis code linked to
EHT (401, one of the most prevalent codes across sev-
eral CRGs, as shown in Table 2).
5.2 Sex-Based Analysis
The differences found in Section 2 when considering
the “sex” variable suggested us to do a sex-based anal-
ysis when considering the best NB approach. There-
fore, two models using both clinical and demographic
features were created, designed and evaluated with
patients of each sex separately.
Results in Table 4 show that for those CRG
with a large or moderate number of patients (i.e.
CRG-5192, CRG-6313, CRG-5424, with more than
1,000 patients) it is advantageous to design sex-
based models. That is, the AUC provided by any of
the sex-based (women and men) models with more
than 1,000 patients is higher in comparison with the
Clinical&Demog-Model. Apart from that, for CRGs
with a low number of patients and also in compari-
son with the Clinical&Demog-Model, the best AUC is
usually obtained with the sex-based model for which
there is a higher prevalence in the CRG. Thus, this is
the case of CRG-5179 (CHF), CRG-7060 (CHF, DIA
and COPD) and CRG-7140 (HT, DIA and other) for
the women-based model.
5.3 Temporal Monitoring
As previously mentioned in Subsection 3.2, for tem-
poral monitoring it is desirable to work with a series
regularly sampled. Owing to this reason, and also to
the fact that our pharmacological data are automati-
cally registered (they refer to dispensation since are
also used for accounting purposes) and diagnoses are
provided after codification of the clinical narrative,
we decided to use the Pharma-Model.
Although chronic patients require a regular intake
of specific medications, the medication records are
not always consistently recorded on the EHR, and do
not always accurately reflect patients’ drug consump-
tion. This can pose a challenge in the application of
ML techniques, reason for introducing the “forget fac-
tor function” which gives exponentially less weight to
the registration of ATC codes as time evolves. Differ-
ent decay rates of the exponential weighting function
were explored, allowing a certain presence of a partic-
ular ATC code to be maintained for more or less time.
Decay values of zero, one, two, and three months
were investigated. In general, as shown in Table 5,
a slower decay of the exponential function led to bet-
ter results in the accuracy rate for each CRG.
The only exception was CRG-5424 (DIA), in
which the lower the decay value, the better the accu-
racy rate. In fact, the best result for this CRG was
achieved with no decay value. This might be due
to the different acute and occasional co-morbidities
associated with diabetic patients, whose occasional
treatment is more reflected in the patient’s annual
summary than in the quarterly one.
The accuracy rate obtained with the NB model
trained when considering the presence/absence of
ATC codes during one year are used as a baseline to
evaluate the outcomes of the temporal monitoring (see
first row in Table 5).
Regarding the quarterly results, the first value of
each cell represents the average accuracy with results
spanning from March to December, encompassing 10
values due to the exclusion of January and February
(as these windows lack three months’ worth of data).
The second value, enclosed in parentheses, indicates
the standard deviation of the accuracy rate. Note that
the average accuracy rate for specific CRGs (5179,
5424, and 6191) within the quarterly scenario sur-
passes that achieved using annual summary data, par-
ticularly when employing a 3-month decay weight-
ing function. Patients with a more severe health
status, characterized by dominant CCs across three
or more organ systems (indicated by gold-standard
CRGs starting with 7), exhibit a higher accuracy rate
with annual summary data compared to the quarterly
approach. The limited 3-month data collection pe-
riod might not adequately capture all the CC inher-
ent to CRG7, potentially underestimating the patient’s
health condition into other CRGs sharing two of the
CCs.
Continuing with the temporal monitoring, we fo-
cused on analyzing the posterior probabilities esti-
mated by the model within each time window. These
probabilities were examined from two distinct view-
points: (i) First, the posterior probability
ˆ
P(CRG
i
|x)
was evaluated in cases where patients were associated
with CRG
i
; (ii) secondly,
ˆ
P(CRG
i
|x) was assessed
for patients not linked to CRG
i
. In an optimal sce-
HEALTHINF 2024 - 17th International Conference on Health Informatics
400

Figure 4: Average CM across the 10 test partitions for both the Pharm-Model (left) and the Clinical&Demog-Model (right).
In each cell: the first value indicates the average count of test instances; the number within parentheses is the corresponding
percentage, relative to the CRG established as the gold standard.
Table 5: Accuracy rate for each CRG using the summary
over one year (Ann) and the average rate (and standard de-
viation, in brackets) when using the summary over quarterly
sliding windows (Qua) with different weight decay.
CRG Ann
Qua
0 m.
Qua
1 m.
Qua
2 m.
Qua
3 m.
5179 0.61
0.63
(0.02)
0.65
(0.02)
0.66
(0.01)
0.66
(0.01)
5192 0.87
0.76
(0.01)
0.77
(0.01)
0.78
(0.01)
0.77
(0.01)
5424 0.78
0.88
(0.01)
0.88
(0.01)
0.86
(0.01)
0.85
(0.01)
6190 0.43
0.27
(0.07)
0.33
(0.07)
0.39
(0.02)
0.42
(0.03)
6191 0.63
0.59
(0.02)
0.62
(0.02)
0.64
(0.03)
0.64
(0.03)
6313 0.67
0.60
(0.02)
0.60
(0.02)
0.60
(0.02)
0.60
(0.02)
7060 0.47
0.11
(0.04)
0.15
(0.04)
0.19
(0.04)
0.23
(0.03)
7080 0.34
0.21
(0.03)
0.24
(0.04)
0.28
(0.06)
0.28
(0.07)
7081 0.59
0.15
(0.03)
0.19
(0.03)
0.24
(0.03)
0.28
(0.04)
7040 0.53
0.34
(0.03)
0.38
(0.02)
0.42
(0.03)
0.44
(0.04)
nario, the probabilities in (i) should consistently be
the highest among all those computed for the same
vector x. However, this is not always the case, and
at times, they may not rank as the highest probabili-
ties. As illustrated in Figure 5 for CRG-5179, two box
plots (green and red) were generated for each evalu-
ation. The green boxes represent probabilities when
the NB model correctly assigns the patient to the gold-
standard CRG, while the red boxes depict instances
where
ˆ
P(CRG-5179|x) isn’t the highest (misclassi-
fied cases). This approach enables an evaluation of
the “confidence” exhibited by the NB model when as-
signing patients to CRG-5179 (in this representation),
while facilitating a comparison of outcomes obtained
from annual and quarterly summary data. Note that,
when considering cases assigned to CRG-5179, the
median of the posterior probabilities (green) consis-
tently remains above 0.8, particularly from the month
of March onward.
Concerning
ˆ
P(CRG
i
|x) for patients not associated
with CRG
i
, the focus is on identifying cases where
this probability holds the highest value, leading to
an incorrect assignment to CRG
i
. In Figure 6, the
gold standard CRG is presented in the vertical axis
(9 box plots among the 10 CRGs) and probabilities
of the misclassified samples are organized according
to the actual CRG they are linked to, both for the
annual summary data (left panel) and two represen-
tative situations of the quarterly summary data (two
panels on the right). In this context, a significant in-
crease is observed in the number of patients misclas-
sified as CRG-5179, particularly among those orig-
inally linked to CRG-5192, CRG-5424, and CRG-
7140, when quarterly summary data is employed.
However, the probability distribution corresponding
to these misclassifications remains similar to those es-
timated using annual data.
Naïve Bayes as a Probabilistic Tool for Monitoring the Health Status of Chronic Patients
401
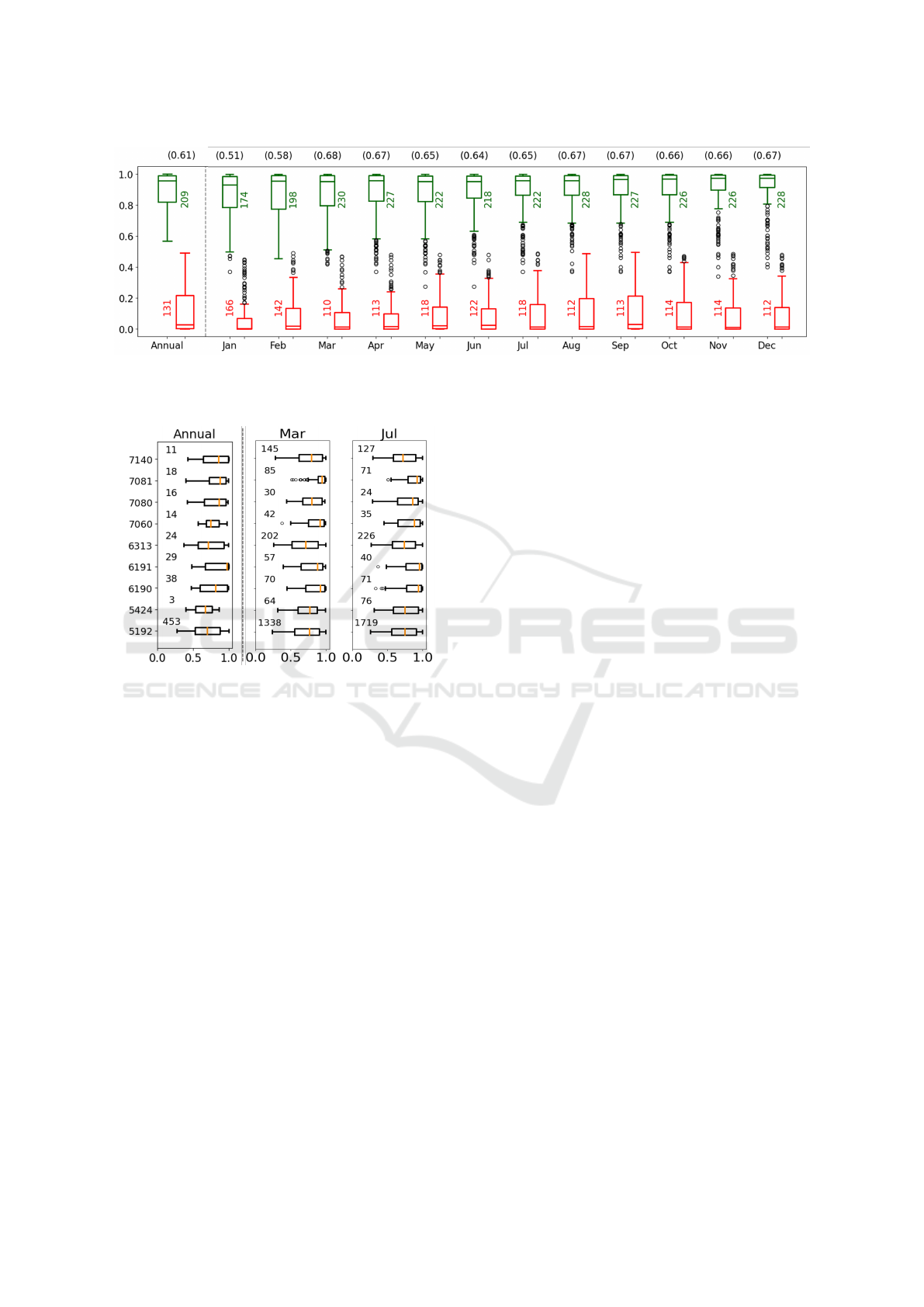
Figure 5: Count of test patients and statistics of
ˆ
P(CRG−5179|x) for the NB scheme when patients linked to CRG-5179: an-
nual data summary (leftmost panel) and quarterly data summary (3 months) for each month. Green/red, for correctly/wrongly
labelled patients. Accuracy rates are in brackets at the top.
Figure 6: Count of test patients and box plots of
ˆ
P(GRG−5179|x) when it emerges as the highest value, de-
spite the gold-standard CRG is in the vertical axis. Annual
data (left panel) and quarterly data summary linked to win-
dows centered on March and July (panels right of the dotted
line).
6 CONCLUSIONS AND FUTURE
WORK
Despite the straightforward nature of the Na
¨
ıve Bayes
approach, its application as a tool for identifying and
monitoring patient health statuses has yielded promis-
ing outcomes, particularly when incorporating clini-
cal codes and demographic attributes. Notably, in sce-
narios with a substantial sample size (such as CRG-
5192, 5424, and 6313), an approach based on gen-
der has exhibited advantages. This avenue opens the
opportunity to investigate how gender influences the
health conditions of chronic patients. Furthermore,
the adoption of a gender-based feature selection strat-
egy could potentially address the issue of high dimen-
sionality, thereby positively impacting the model’s
performance.
Healthcare monitoring involves real data exhibit-
ing a sequential structure, thereby implying that the
interpretation of a pattern can be influenced by con-
textual information. To take temporal dependencies
into account, we are currently exploring the use of re-
current neuronal models and its application to stream-
ing data, seeking to enhance our monitoring capabili-
ties.
In scenarios involving chronic patients, it would
be also interesting to consider the incorporation of
additional rules within the monitoring framework to
enhance performance. This may be particularly perti-
nent given that the intrinsic nature of CCs indicates
that the patient’s health status (in the context dis-
cussed in this study, denoting CRG assignment) can-
not experience improvement.
ACKNOWLEDGMENT
This work was partly funded by the Spanish Re-
search Agency, grant number PID2019-106623RB-
C41/AEI/10.13039/501100011033 (BigTheory),
PID2022-136887NB-I00 (POLIGRAPH) and by the
European Union NextGeneration-EU funds (Youth
Employment Plan of the Spanish Government) in the
INVESTIGO project with reference URJC-AI-11.
REFERENCES
Al, K. et al. (2012). Medical data classification with naive
bayes approach. Information Technology Journal,
11(9):1166–1174.
Association, A. M. (2004). ICD-9-CM 2005: International
Classification of Diseases, 9th Revision Clinical Mod-
ification (Physician Edition). American Medical As-
sociation Press.
Atella, V. et al. (2019). Trends in age-related disease burden
and healthcare utilization. Aging Cell, 18(1):e12861.
HEALTHINF 2024 - 17th International Conference on Health Informatics
402

Berwick, D. M., Nolan, T. W., and Whittington, J. (2008).
The triple aim: care, health, and cost. Health Affairs,
27(3):759–769.
Bhuvaneswari, R. and Kalaiselvi, K. (2012). Naive
bayesian classification approach in healthcare appli-
cations. International Journal of Computer Science
and Telecommunications, 3(1):106–112.
Chang, C.-H., Lin, C.-H., and Lane, H.-Y. (2021). Ma-
chine learning and novel biomarkers for the diagnosis
of alzheimer’s disease. Intl. J. Mol. Sci., 22(5):2761.
Chen, M. et al. (2017). Disease prediction by machine
learning over big data from healthcare communities.
IEEE Access, 5:8869–79.
Chushig-Muzo, D., Soguero-Ruiz, C., de Miguel, P., and
Mora-Jim
´
enez, I. (2021). Interpreting clinical latent
representations using autoencoders and probabilistic
models. Artif Intellig in Medicine, 122:102211.
Chushig-Muzo, D., Soguero-Ruiz, C., de Miguel, P., and
Mora-Jim
´
enez, I. (2022). Learning and visualizing
chronic latent representations using electronic health
records. BioData Mining, 15(1):1–27.
Chushig-Muzo, D., Soguero-Ruiz, C., Engelbrecht, A.,
de Miguel, P., and Mora-Jim
´
enez, I. (2020). Data-
driven visual characterization of patient health-status
using electronic health records and self-organizing
maps. IEEE Access, 8:137019–31.
Demirbas, K. (1988). Maximum a posteriori approach
to object recognition with distributed sensors. IEEE
Transactions on Aerospace and Electronic Systems,
24(3):309–313.
Ellis, R. et al. (2022). Development and assessment of a
new framework for disease surveillance, prediction,
and risk adjustment:the diagnostic items classification
system. In J Am Med Ass Health Forum, volume 3.
Fodeh, S. J. et al. (2021). Utilizing a multi-class classifi-
cation approach to detect therapeutic and recreational
misuse of opioids on twitter. Computers in Biology
and Medicine, 129:104132.
Hanley, J. A. and McNeil, B. J. (1982). The meaning and
use of the area under a Receiver Operating Character-
istic curve. Radiology, 143(1):29–36.
Hickey, S. J. (2013). Naive bayes classification of public
health data with greedy feature selection. Communi-
cations of the Institute of Mathematics and its Appli-
cations, 13(2):7.
Hughes, J. S., Averill, R. F., et al. (2004). Clinical risk
groups (crgs): a classification system for risk-adjusted
capitation-based payment and health care manage-
ment. Medical Care, pages 81–90.
Jim
´
enez-Serrano, S. et al. (2015). A mobile health
application to predict postpartum depression based
on machine learning. Telemedicine and e-Health,
21(7):567–574.
Jurado-Camino, M., Chushig, D., Soguero, C., de Miguel,
P., and Mora, I. (2023). On the use of generative
adversarial networks to predict health status among
chronic patients. In Health Informatics, pages 167–
178.
Kibriya, A. M. et al. (2005). Multinomial naive bayes for
text categorization revisited. In Austr J Conf on Arti-
ficial Intelligence, pages 488–99.
Mitchell, T. M. (1997). Machine Learning. McGraw Hill.
Nolte, E. et al. (2014). Assessing chronic disease man-
agement in european health systems. concepts and ap-
proaches. World Health Organiz.
Parzen, E. (1962). On estimation of a probability den-
sity function and model. The Annals of Mathematical
Statistics, 33(3):1065–76.
Pugliese, N. R. et al. (2020). The renin-angiotensin-
aldosterone system: a crossroad from arterial hyper-
tension to heart failure. Heart Failure Reviews, 25:31–
42.
Raghupathi, W. and Raghupathi, V. (2018). An empirical
study of chronic diseases in the united states: a visual
analytics approach to public health. Intl J. of Env. Re-
search and Public Health, 15(3):431.
Ronning, M. (2002). A historical overview of the atc/ddd
methodology. World Health Organization drug infor-
mation, 16(3):233.
Silverman, B. W. (1986). Density Estimation for Statistics
and Data Analysis. London: Chapman & Hall.
Sinharay, S. (2010). International Encyclopedia of Educa-
tion, chapter Discrete probability distributions. Else-
vier Science.
Soguero, C., Mora, I., Mohedano, M. A., Rubio, M.,
de Miguel, P., and Sanchez, A. (2020). Visually
guided classification trees for analyzing chronic pa-
tients. BioMed Central Bioinformatics, 21:1–19.
Sowers, James R and Frohlich, Edward D (2003). Insulin
and insulin resistance: impact on blood pressure and
cardiovascular disease. The Medical clinics of North
America, 87(5):s1005–s1027.
Vandenberghe, D. and Albrecht, J. (2020). The financial
burden of non-communicable diseases in the european
union: a systematic review. European Journal of Pub-
lic Health, 30(4):833–839.
Vellido, A. (2020). The importance of interpretability and
visualization in machine learning for applications in
medicine and health care. Neural Computing and Ap-
plications, 32(24):18069–18083.
Zhao, J. et al. (2017). Learning from heterogeneous tem-
poral data in electronic health records. J. Biomedical
Informatics, 65:105–119.
Naïve Bayes as a Probabilistic Tool for Monitoring the Health Status of Chronic Patients
403
