
Bed Management System Implementation: Experimental Study
Flannag
´
an Noonan
a
, Michelle Hanlon, Juncal Nogales, Ciar
´
an Doyle, Eilish Broderick
and Joseph Walsh
b
IMaR, Munster Technological University, Kerry Campus, Clash, Tralee, Kerry, Ireland
flannagan.noonan@mtu.ie, michelle.j.hanlon@research.ittralee.ie, {juncal.nogales, ciaran.doyle, eilish.broderick,
Keywords:
Bed Management, Patient Throughput, Hospital Administration, Hospital Admission, Hospital System
Deployment.
Abstract:
Many hospitals today use bed management systems that are primarily manual and paper-based. This inhibits
efficiency and informed decision making, as communication is constrained. Hence these systems are essen-
tially memoryless as lessons learned reside with individuals but are lost to the organisation as a whole. Elec-
tronic systems that can capture and record checkpoints on the patient pathway allow that data to be analysed.
This can help with improving efficiency and prediction, allowing “what if” scenarios to be examined with data
to support it. This paper presents the outcome of developing a bed management system and deploying it in a
hospital for a live trial over a period of approximately three months. It also highlights improvements suggested
through system usage over the period of the deployment and presents a novel efficiency measure.
1 INTRODUCTION
The Global COVID-19 pandemic has caused a large
spike in patient numbers in hospitals due to the
high number of emergency patients suffering with the
virus. Another impact of the pandemic is a deferment
in elective patient treatments due to pressure from
treating pandemic patients. The need to reduce pa-
tient waiting lists will cause further pressure on hos-
pitals once pandemic patient numbers decline.
Globally, efficiencies in hospitals are being
sought, to improve the service and treatment of people
while controlling the cost of providing the service.
This paper discusses the implementation of a hos-
pital bed management system, developed in associa-
tion with a local hospital, part of the largest provider
of private healthcare in Ireland. The system tracks
the patient movement along the patient pathway, al-
lowing an examination of the system as a whole and
creates a novel measure of efficiency, occupied versus
unoccupied times with unoccupied time being further
divided into idle time and out of service (OOS) time.
a
https://orcid.org/0000-0001-9624-5181
b
https://orcid.org/0000-0002-6756-3700
2 HOSPITAL SYSTEMS
Hospitals use a system, commonly referred to as a
Hospital Information System (HIS), which is primar-
ily a billing system, as the basis for supporting paper
based manual systems for bed and patient manage-
ment. The level of information retained, on the patient
journey, by the HIS is generally minimal, such that
different individual patient journeys cannot be com-
pared accurately.
A patient arriving in a private hospital, having
been referred by a Consultant, for an elective proce-
dure or a General Practitioner (GP) as an emergency
patient, will first approach the Admissions personnel.
Once processed, they will be escorted to their bed, by
a Healthcare Assistant (HCA) in preparation for any
procedure or observation as part of their treatment.
They may also have had to attend for preadmission
tests.
Once their treatment is complete, the multidisci-
plinary team will coordinate discharge. The patient’s
Consultant will authorise it and the Nursing staff will
manage it. Once discharged, the preparation of the
bed for the next patient, bed renewal, will commence.
This will involve the HCA, stripping the bed and later
dressing the bed. Housekeeping will clean the bed
area and / or the room and bathroom. Sometime after
the bed renewal is complete, the Bed Manager will be
370
Noonan, F., Hanlon, M., Nogales, J., Doyle, C., Broderick, E. and Walsh, J.
Bed Management System Implementation: Experimental Study.
DOI: 10.5220/0012346700003657
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 17th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2024) - Volume 2, pages 370-377
ISBN: 978-989-758-688-0; ISSN: 2184-4305
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
advised of the bed being available and the cycle will
repeat.
The HIS generally does not record the checkpoints
above, but the deployed system, discussed in the pa-
per, does.
2.1 Communications and Data
Noonan et al. (2019), provides an overview of the lit-
erature on Bed Management. It highlights the issues
recorded and the solutions suggested in the domain
of Bed Management. The solutions broadly align un-
der addressing the areas of communications, process
change or modelling and prediction. Balaji & Brown-
lee (2018), suggests that critically the process needs to
be understood and the process is complex, spanning
multiple departments requiring departmental work-
flow and inter-departmental process optimisation. It
also stresses the need for measurement and commu-
nication, particularly given the interdisciplinary teams
managing the patient care. However, systems that are
predominantly manual and paper based are not con-
ducive to easy measurement and therefore communi-
cating these measurements can be burdensome in the
absence of a dedicated communication mechanism.
Discharge Before Noon (DBN) is another area in-
vestigated for its impact on Length of Stay (LOS), a
measure of how long a patient stays in the hospital.
The impact is around getting patients discharged early
in the day, to avoid impact on placing the next tranche
of patients in a bed. One early study Wertheimer et al.
(2014) implemented a system that recorded a reduced
mean LOS and a non-statistically significant reduc-
tion in 30-day readmission rates. However, Rachoin
et al. (2020), James et al. (2019) suggest that while
DBN does reduce patient LOS for surgical patients,
the reduction is not necessarily the same for medical
patients. In all cases, an easy mechanism for captur-
ing patient admission and discharge enables easy im-
plementation of studies such as this.
2.2 Modelling and Prediction
Modiuddin et al. (2017) reviews literature on simu-
lation of patient flow within Emergency Departments
(ED). The studies reported on, show that simulation
modelling can be used to pretest the impact of work-
flow / process changes in a safe way.
Novati et al. (2017) records the long term achieve-
ment of reduction in mean LOS through a previous
implementation of a bed management model.
Modelling techniques rely on data for both model
development and testing. Extracting this data from
paper based records or relying on the minimal data
checkpoints available for HIS type systems limits the
effectiveness of the model. Thus greater data capture
allows for better modelling to achieve better efficien-
cies.
3 SOLUTION ADOPTED
An electronic system was developed to manage the
bed / patient flow in the hospital. This system allowed
a real-time view of hospital occupancy and captured
data to allow subsequent analysis as a means to im-
prove bed management and patient throughput.The
following provides an overview of the system. For
a more comprehensive account see Noonan et al.
(2023).
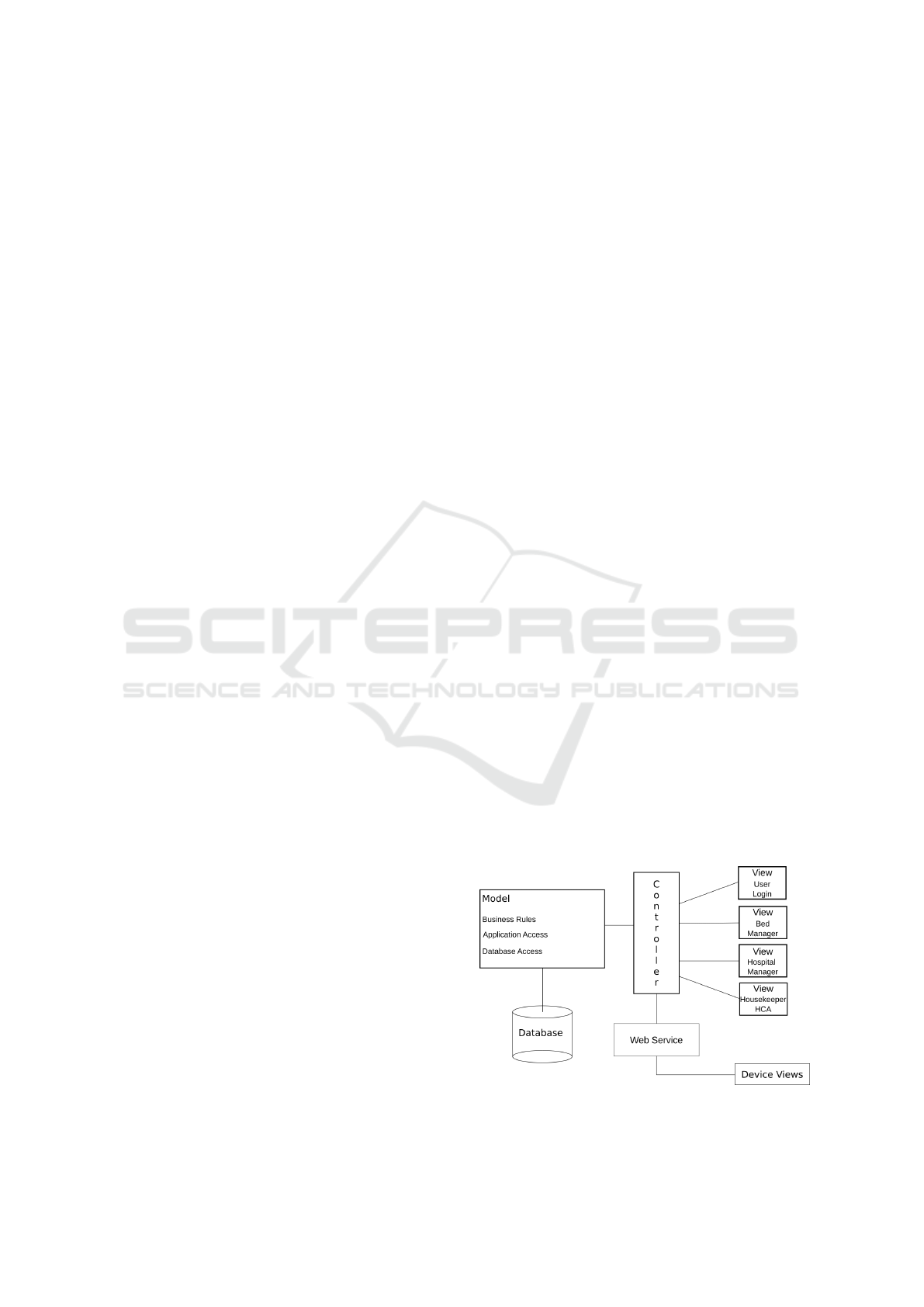
Fig. 1 is the model for the system using a
Model-View-Controller (MVC) pattern with an SQL
database for data capture, storage and interrogation.
The main system is a web based application for use
by the bed managers and hospital administrators. The
web element allows elective patients to be preas-
signed to beds, emergency patients details recorded
pending agreement to admit and bed availability to be
determined. Each ward has a graphical view that can
be used to determine the available beds. Additionally
there are views that provide a synopsis of the bed sta-
tus throughout the hospital.
There is a mobile device element to facilitate mo-
bile elements of data capture such as escorting a pa-
tient to the bed they are going to occupy. This duty is
generally performed by HCA staff. Both Housekeep-
ing and HCA staff are involved in bed renewal, ensur-
ing the bed is available for the next patient and they
are mobile when moving from room to room. They
record bed renewal job completion using a mobile de-
vice.
Fig. 2 illustrates the checkpoints for data capture.
For a given patient, a request is made to the hospital
Figure 1: Design Model for Bed Management Application.
Bed Management System Implementation: Experimental Study
371
Bed Manager, to accommodate a patient, from either
a Consultant for an elective patient or a General Prac-
titioner (GP) for an emergency patient. The Bed Man-
ager enters the patient data on the web application and
ultimately allocates the patient a bed.
Table 1 defines the status cycles for the patient-
bed relationship and their triggers corresponding to
Figure 2.
The Web Application, Graphical User interface
(GUI), displays the status of the bed and any of the
activities occurring above will update in real-time.
4 SOLUTION IMPLEMENTATION
In an initial trial, in which the developed system was
tested on 450 actual patient presentations, names and
dates of birth were anonymised. All data entry was
performed by a single person, mostly by the project
manager but also the Hospital Manager. This data
being entered after the fact, albeit on the same day,
did not reflect accurate timestamps for events such as
arrival at the bed but the concept of capturing times-
tamp was proven. The hospital manager also entered
test data, to better understand the system and was im-
pressed with the ease of use of the system. A very
basic system of a laptop computer containing the web
and database servers, and functioning as the data en-
try terminal for patient data was used along with a
WiFi virtual local area network to connect two An-
droid based mobile devices to carry out the mobile
elements of the checkpoints.
A number of issues were identified from this trial,
prior to the live trial:
• One issue raised was that the colour used for non-
gender beds (green) caused confusion with the
colour used in the ward dashboard pie chart to in-
Table 1: Bed Status Transitions.
Status Steps Status Change Notes
Patient Allocated to
Bed
Available → Allocated
Pending
Bed Manager;
ADON; Dayward
CNM
Patient scanned at
Admissions
Allocated Pending →
Allocated On Site
Patient Details
Captured
Patient Admitted via
Scan at Bedside
Allocated On Site →
Occupied
HCA Patient
Escort
Patient Treated Occupied No Data Collected
Patient Discharged
Occupied → OOS
Pending
Captured at Ward
or Reception
Bed Accepted for
Cleaning Or
Dressing
OOS Pending → OOS
In Progress
HCA &
Housekeeping
Accept via
Application
Bed Recorded
Cleaned & Dressed
OOS In Progress →
Available
HCA &
Housekeeping
Confirm via Scan
dicate “available”. The the colour to indicate gen-
der neutral beds was changed to orange.
• A second issue was the graphical refresh of the
ward views. The Scaleable Vector Graphics
(SVG) files representing the wards are embedded
pictures. Their state of not being current, or being
stale, is not reported via the normal server client
HTML process. This was resolved using dedi-
cated refresh methods and a refresh button.
4.1 Live Trial Pre-Deployment Checks
Based on the non-live trial, some checks were imple-
mented and changes were required
The application was run via two servers, IIS and
MS SQL allowing for deployment in the hospital IT
Centre. However due to time constraints to get that
enabled it was agreed with the Hospital Manager to
proceed using the server on the laptop in the hospital,
for the duration of the live trial.
An unknown from the previous in-hospital test-
ing was how data entry, using mobile devices from
dispersed locations, would perform. The connectiv-
ity via WiFi to the laptop was trialled from various
points in the hospital, including the ward, the Admis-
sions area and the reception area. This highlighted an
issue with reception not having a reliable wireless net-
work signal for bed release. This was raised with the
IT department in the hospital and arrangements were
made to deploy an access point there. However, this
took some weeks to get implemented.
As staff using the mobile applications needed to
be recorded as users on the system database, all staff
associated with the trial were identified and added as
users to the system.
An issue of connectivity from the phones to the
server presented itself spuriously while preparing for
going live. Frequently, the phones would not connect
to the server. This issue had not materialised in the
system development or in the earlier trial.
Significant effort was put into rectifying this, in-
cluding bringing in a third party to review the fault
localisation procedures and suggest actions to rem-
edy the issue. No definitive root cause was estab-
lished. The Public firewall on the laptop, was set to
“off” as firewall issues were suspected. The use of
the “Zoom” video conferencing application, popular
during the COVID-19 pandemic using the thin clients
connected to the Citrix farm, caused major issues on
the hospital TCP/IP network volumes. The IT Depart-
ment did comment that this issue caused degradation
and outage to other network services. Once use of
“Zoom” on this service was stopped, the issue did not
manifest again.
HEALTHINF 2024 - 17th International Conference on Health Informatics
372
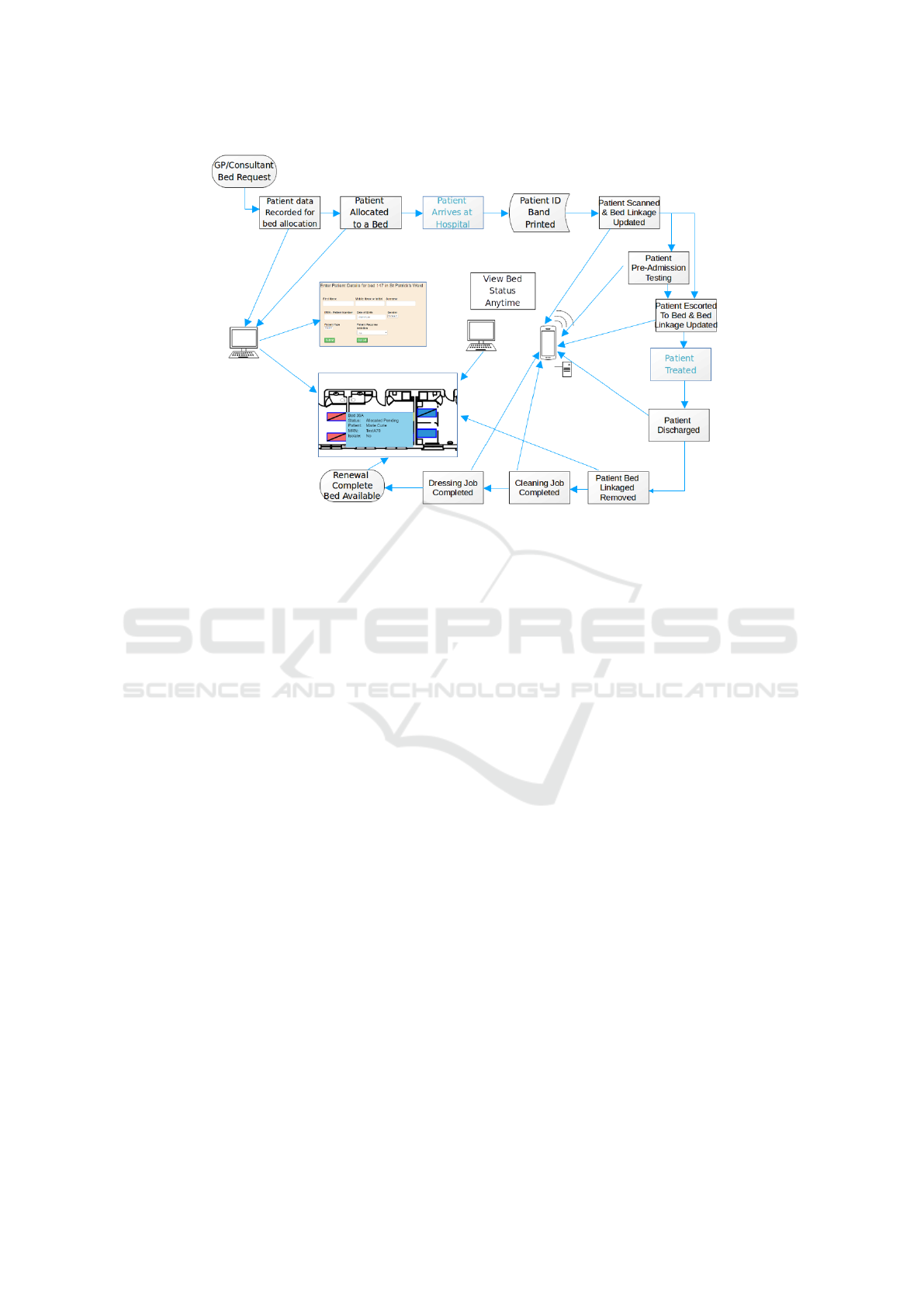
Figure 2: Data capture and flow for the bed management application.
A single ward was chosen as a pilot site for de-
ployment. This constraint was due to the number of
devices available for operation, the limited ability to
supply support over the whole hospital and the ability
to manage the operation and volume over the whole
hospital. This decision was on balance a positive one
as it allowed the objectives to be met but without ma-
jor impact on the hospital overall. It also allowed a
defined focus for determining the impact the system
produced.
4.2 Trial Objectives
The primary objective was to establish the data de-
tail that could be gathered using the application in a
live environment and determine the usefulness of the
data to improve the patient throughput in the hospital.
Success can be measured in terms of the core features
being available and functioning to capture and record
the required data and timestamps.
Establishing timestamp data at the points in Fig-
ure 2 and to record them as they occur, was thought
to be important to establish timing for patient move-
ment. Equally, generating feedback to Housekeeping
and HCA staff regarding beds requiring renewal was
key.
On the use envisaged for the application by the
hospital, the Hospital Manager indicated that bed oc-
cupancy figures were a major criteria in senior man-
ager review of hospital operation. Thus, a view of the
occupied time of the beds and provision of a break-
down of the occupied time versus idle time was re-
quired. It was also thought that a further breakdown
on unoccupied time could be achieved by separating
the idle time from the out of service time. Out of
service time was recorded as commencing once a pa-
tient had departed the hospital having been scanned
on exit. This additional time breakdown is a novel
element.
A further objective was to establish a basis for
a critical evaluation of the system as implemented
against the inherent paper-based system and HIS to
assess its potential and capabilities, shown in tables 2
and 3.
4.3 Personnel Training
A brief overview of the system was developed for
the hospital’s Heads of Department (HoDs), to pro-
vide them with an understanding of the input required
of their staff. Once their agreement was obtained
and they identified employees that should be trained,
the names were added as users on the system. A
training plan was established and a one-sheet training
overview was produced per role. As an example, the
one-sheet overview for the Admissions role is shown
in Figure 3.
The individuals to be trained, were then ap-
proached, to identify a suitable time for training and
given a QR code with their name and role. Due to
the teams working different shifts in the hospital, the
training was arranged for the evening or weekends as
appropriate.
The level of interest was very positive. Forty-
Bed Management System Implementation: Experimental Study
373

Figure 3: Training Document One-sheet Overview.
three members of staff were trained initially, consist-
ing of the Housekeeping and Health Care Assistant
team members, the Admissions team in its entirety
and a Receptionist team member. Additional training
was provided as required.
The bed manager initially declined to be trained
citing a lack of time and a period of a high level of
stress. This was due firstly, in managing the bed allo-
cations but also due to an additional task of assigning
patients to undertake COVID-19 Polymerase Chain
Reaction (PCR) tests and the follow up to ensure the
patients tested negative. Thus the author assumed the
bed manager data entry role, initially, with a goal of
passing the role over to the Bed Manager after the
trial was up and running and had achieved a level of
stabilisation.
Before trial start, training was carried out using
the trial system itself. At trial start a second sys-
tem was deployed on another laptop with a separate
dedicated private IP sub network provided by a mo-
bile phone hotspot. This system was also used to
test changes made to the software prior to applying
changes to the live server, as the trial progressed.
A series of QR codes based on cartoon character
names were created, as patients, for training. This
was done to highlight that the patients were not real
patients and to lighten the atmosphere. The mock pa-
tient status was set to that pertinent to the role be-
ing trained and the one-sheet procedure was walked
through. The personnel then retained the one-sheet
overview as a reference. The preferred option was to
train people on a one-to-one basis but given the time
constraints and personnel availability, sometimes up
to a three-to-one ratio was used.
5 TRIAL COMMENCEMENT
As mentioned earlier, the author assumed the role of
“bed manager” to input the data for the trial. This in-
troduced an element of latency into the system, due
to the logistics of meeting with the actual Bed Man-
ager for updates. Further complications arose when
the position of Bed Manager evolved to include a sec-
ond individual. The newcomer to the role would ide-
ally have had trial system training in addition to their
standard training. This was too onerous for the in-
cumbent Bed Manager, but as the trial progressed,
both individuals received system training from the au-
thor. Currently, to maintain an updated view of bed
status, the Bed Manager must walk the hospital. This
conflicted with the need for constant contact, by the
author to the Bed Manager to ensure optimal data en-
try. Thus bed moves were sometimes missed and GP
referrals entered after the fact. Consultation with the
Admissions personnel, particularly at the commence-
HEALTHINF 2024 - 17th International Conference on Health Informatics
374
ment of the day, proved a less onerous route for entry
of data for patients due to be admitted.
It emerged that accessing the application server
from computers on the existing hospital network had
been “blacklisted”. A request to get this issue rectified
triggered concern regarding exposure of patient data
to a potentially vulnerable web-server. An agreement
to proceed was reached by undertaking “hardening”
of the server and moving the infrastructure onto the
most secure WiFi VLAN network, with an associated
change in endpoint IP address, which “white-listed”
the server allowing access. The trial had to be stopped
for four days while this work was completed. The
plan to move the system to servers created in the op-
erations centre was not implemented due to the eight
weeks minimum lead time involved.
Another complication was that the Medical As-
sessment Unit (MAU), which functioned as the pri-
vate hospital equivalent of an Emergency Ward, was
provided with one or more beds on the trial ward on
a daily basis. This was to allow them admit patients
at their discretion. These patient details were difficult
to obtain, generally being entered on the trial system
after the fact. Additionally, the MAU used linear bar-
codes for their admissions process, which were not
readable by the scanning devices used for the system.
When the primary Admissions department changed
from linear to 2D barcodes, QR codes, the MAU re-
tained the linear codes, a fact discovered by the Re-
ceptionist scanning patients on exit. This was not re-
solved by the end of the trial, but a work around was
to produce a separate QR code for these patients to
allow their beds to be released.
The new Bed Manager highlighted her difficulty
with identifying which bed was which from the ward
graphic. Placing the cursor over a bed triggered a pop-
up with the bed details but lack of familiarity with the
ward layout meant that she struggled to find a specific
bed for patient placement. The graphic was updated
to include the bed number adjacent to the bed, to re-
solve this.
To address the issue of patients being allocated to
a bed that is not yet ready, a view of the trial ward was
created. This view, or web page, listed the available
and out of service beds. Thus, the Admissions role
could login to the application, to validate beds being
allocated to patients as available and in-service. Since
the view auto refreshed, it could be left open for quick
access.
Another change arose from the preparation of a
daily report to the Hospital Manager. It was found
challenging to review the status of the ward histori-
cally, either earlier in a same day or previous days.
To this end, a view was produced that allowed a his-
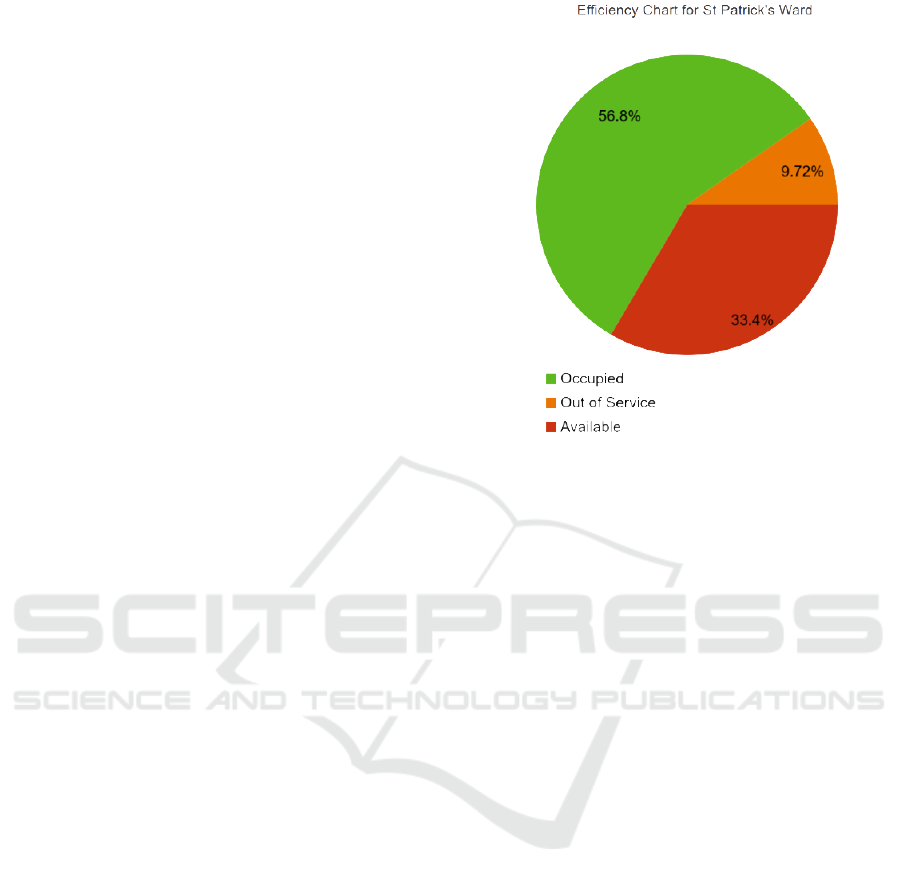
Figure 4: Bed Usage and Unoccupied Time (%).
toric view of the ward, on a given date and time for
comparison with the current status, both shown in the
same view.
This comparison page was very well received by
the Hospital Manager. The comparison page provided
a basis for a view, summarising the bed usage, bed
idle and bed out of service, from commencement of
the trial. This was seen, by the Hospital Manager, as
a key tool to examine the efficiency of the functioning
of the ward. The graphic in figure 4 is the actual data
over the period of the trial.
5.1 Trial Outcomes
The trial was implemented from 07:00 until 19:00
Monday to Friday as outside of these hours it was dif-
ficult to get buy-in from the staff. Ultimately very few
patients would be admitted outside these hours and at
weekends. Discharges are, however, common at the
weekend and the Receptionist was not available to re-
lease the bed. The process of bed renewal automati-
cally released the bed-patient linkage. The discharges
are captured but without a valid patient egress times-
tamp.
A total of five hundred and seventy four (574)
patients were recorded for the trial ward between
November 15th 2020 and February 26th 2021, when
the trial ended. A total of four thousand one hundred
and thirty one (4131) StatusLog records, linking a pa-
tient with a bed, were generated over the same time
period. Given that one patient visit accounts for six
StatusLog records, it would be expected that 6 times
574 = 3444 StatusLog records should exist. The addi-
Bed Management System Implementation: Experimental Study
375

tional records are associated with patient moves and
patients visiting the hospital more than once over the
period of the trial.
A total of forty seven (47) patient moves were
recorded, which underestimates the number of patient
moves that occurred by about 50%. This was chiefly
because patients allocated beds in the trial ward were
often admitted to a different ward initially and then
moved to the trial ward. This allocation of patients to
alternative wards, was often due to the trial ward op-
erating at capacity but also being the optimum ward
for the patient type, an orthopaedic patient. A patient
would be admitted pending surgery and a bed would
be available in the trial ward on surgery completion.
Patient moves were also missed due to the author
adopting the “bed manager” data entry role. On occa-
sion, the first indication of a move would be due to the
release of a bed through the bed renewal process, and
the released patient appearing in a different bed. This
necessitated the patient being readmitted. This sce-
nario would be negated by the bed manager operating
the system.
A total of sixty nine (69) patients were “Ear-
marked”, that is assigned to a bed that was either al-
ready occupied but pending an imminent discharge,
or the bed was “Out of Service” pending cleaning.
Subsequently releasing the bed for the existing patient
and/or completing the renewal of the bed, allowed the
“Earmarked” patient to automatically take on the sta-
tus of “Allocated Pending” and then followed the nor-
mal status cycles presenting at admission.
The trial was arranged on the understanding that
bed stripping and redressing were implemented by
the HCA role. In practice, both Nurses and Student
Nurses contributed significantly to bed stripping and
redressing. QR codes, for the HCA role to allow scan-
ning for completion of the bed dressing, were pro-
vided to the Nursing staff on the ward once this was
highlighted, but uptake was negligible.
One particular area of concern was the variable
approach to completing scanning. Housekeeping
compliance was very high initially but changed fol-
lowing the stopping and recommencing of the trial to
harden the server. This was addressed by retraining
sessions and highlighting the continuation of the trial.
This restored the high compliance by Housekeeping.
The HCA contribution was more difficult to cor-
rect due to Nursing staff and students making the
beds. Additionally, low staffing level on some days
hampered compliance. The Ward Clerk was trained
on the use of the system and tasked with engaging the
HCAs and Nursing staff, but this was not a notable
success. An effort to deploy a screen on the ward, that
would provide feedback to both HCAs and House-
keeping on their contribution, was implemented but
ultimately was not completed by the end of the trial
due to staffing issues in the IT Department.
In terms of the objectives, the detail that could
be gathered proved successful. Patient bed release
was seen to highlight beds requiring renewal, before
Housekeeping and HCAs were apprised of this ver-
bally by the Nursing staff. Additionally, the lack of
availability of beds prior to patient admission was
shown to reflect the true situation, providing Admis-
sions with an accurate view of the situation on the
Ward. Both these improvements in the flow of in-
formation contribute significantly to a positive patient
experience.
Accurate timing of patient movements was not
fully achieved in the trial, as it was hampered by lack
of Bed Manager engagement, issues with HCA scan-
ning, and the limitation of having a single ward as
the focus of the trial missing patient transfers. How-
ever, for patients being admitted to the ward, status
change from “Allocated On Site” to “Occupied” could
be used to provide a mechanism to trigger patient
preparation for their procedures by the Clinical staff
both on an “is present” and “known location” basis.
Both occupied and unoccupied times are useful
metrics, which provide a breakdown on bed effi-
ciency. The unoccupied time is broken down further
in terms of beds being unoccupied due to being “va-
cant” or “out of service”. This allows focus on the bed
usage and is a broker for discussion on how efficiency
can be improved.
6 RESULTS
In the existing system it is difficult to quantify the ac-
curacy of timestamps, for events. Events entered on
the HIS will be available to other users of the sys-
tem, once entered, but there may be a delay between
an event occurring and being entered. Information on
some events are held locally and timestamp informa-
tion is not necessarily recorded.
In comparison, the new systems automatically
records events and timestamps, once tasks have been
completed and scanned. The information is then
available to all system users. The new system cap-
tures additional events and their timestamps.
Table 2 lists the data capture comparison for the
existing system and the new system.
It is difficult to define times for events to be
recorded, for the existing system. Not all events
recorded by the existing system have recorded times-
tamps. Generally, the existing system can be regarded
as best effort and only events recorded on the HIS can
HEALTHINF 2024 - 17th International Conference on Health Informatics
376

be regarded as having a hospital-wide or global view.
A comparison of the timing of events is provided in
Table 3 below for the existing and new systems and is
discussed below.
7 CONCLUSIONS
This paper describes the deployment of an application
and devices to gather and record data for the purposes
of study and review of the patient pathway.
It highlights the difficulties and complexities of
data networks in remote data gathering.
The results section, Section 6, shows that the new
system coherently captures events and their times-
tamps for patients’ journeys through the patient path-
way. This not only provides a hospitalwide view of a
given patient status but also, over time, allows accu-
mulation and analysis of data for patterns and trends
as a basis for improving efficiency of patient through-
put.
The efficiency can be measured by:
• reviewing the occupation level
• the amount of idle beds, or
• measuring the time that beds are out of service
The checkpoint data captured with this efficiency
measure can drive change for increasing efficiency.
In terms of future work, the development of a
Higher Level 7 (HL7) interface would be key.
It would enable integration of the application with
an existing HIS, as a subsystem. Data transfer of
existing information would be facilitated, allowing a
single data repository and, at the same time, adding
all the functionality offered by this application.
Table 2: Event Capture Comparison.
Existing System New System
Desired Feature HIS
Local /
Individual
Global View
Pre-Allocate Bed to
Patient
No
Yes - Bed
Manager
Yes
Record Admission Yes No Yes
Record Arrival at bed No No Yes
Capture Patient
Egress From Hospital
No No Yes
Capture Bed Renewal
Requirement
No Yes - Nurse Yes
Bed Available
Notification After
Renewal
No
Yes -
Nursing /
H’keeping
Yes
Graphical View of
Patient Fill
No No Yes
Table 3: Event Capture Timing Comparison.
Features
Existing System
Timings
New System
Timings
Pre-Allocate Bed
to Patient
Local Communication
varying
Global Immediate
Record Admission Global Immediate Global Immediate
Record Arrival at
bed
Not Available Global Immediate
Capture Patient
Egress From
Hospital
Not Available Global Immediate
Capture Bed
Renewal
Requirement
Local - Verbal
Communication
Global Immediate
Bed Available
Notification After
Renewal
Local - Verbal
Communication
Global Immediate
Graphical View of
Patient Fill
Not Available Global Immediate
REFERENCES
Balaji, R. and Brownlee, M. (2018). Bed
management optimization. From Infosys:
https://www.infosys.com/industries/healthcare/
documents/hospital-bed-management.pdf.
James, H., Steiner, M., Holmes, G., and Stephens, J. (2019).
The association of discharge before noon and length
of stay in hospitalized pediatric patients. Journal of
Hospital Medicine, 14(1):28–32.
Mohiuddin, S., Busby, J., Savovi
´
c, J., Richards, A., North-
stone, K., Hollingworth, W., Donovan, J., and Vasi-
lakis, C. Patient flow within UK emergency de-
partments: a systematic review of the use of com-
puter simulation modelling methods. BMJ Open,
7(5):e015007.
Noonan, F., Nogales, J., Doyle, C., Broderick, E., and
Walsh, J. (2023). Bed management system develop-
ment. In HEALTHINF, pages 376–383.
Noonan, F., O’Brien, J., Broderick, E., Richardson, I., and
Walsh, J. (2019). Hospital bed management practices:
A review. In HEALTHINF, pages 326–331.
Novati, R., Papalia, R., Peano, L., Gorraz, A., Artuso, L.,
Canta, M. G., Vescovo, G. D., and Galotto, C. (2017).
Effectiveness of an hospital bed management model:
results of four years of follow-up. Ann Ig, 29(3):189–
196.
Rachoin, J., Aplin, K., Kupersmith, E., Gahdhi, S., Travis,
K., Stefaniak, M., and Cerceo, E. (2020). Discharge
before noon: is the sun half up or half down? Ameri-
can Journal of Managed Care, 26(8):e246–e251.
Wertheimer, B., Jacobs, R., Bailey, M., Holstein, S., Chat-
field, S., Ohta, B., Horrocks, A., and Hochman, K.
(2014). Discharge before noon: An achievable hospi-
tal goal. Journal of Hospital Medicine, 9(4):210–214.
Bed Management System Implementation: Experimental Study
377
