
Self-Medication of Antibiotic Use: Investigating Knowledge and
Attitude Among Rural Population in Umbul Natar Village, South of
Lampung
Dwi Aulia Ramdini
1
a
, Muhammad Fitra Wardhana Sayoeti
1
b
, Suharmanto
2
c
,
Ramadhan Triyandi
1
d
, Muhammad Iqbal
1
e
and Rano K Sinuraya
3,4
f
1
Departement of Pharmacy, Faculty Medicine, University of Lampung, Bandar Lampung, Indonesia
2
Departement of Public Health, Faculty of Medicine, Lampung University, Bandar Lampung, Indonesia
3
Departement of Pharmacology and Clinical Pharmacy, Faculty of Pharmacy, Universitas Padjadjaran, Indonesia
4
Unit of Global Health, Department of Health Sciences, University of Groningen/University Medical Center Groningen,
Groningen, The Netherlands
dwi.aulia@fk.unila.ac.id
Keywords: Knowledge, Attitude, Rural Population, Self-Medication with Antibiotic.
Abstract: Self-medication with antibiotics is a common phenomenon among the general population, including in rural
areas. This practice has been the subject of particular attention because the consequences are very dangerous
in terms of the development of antibiotic resistance. There are several factors underlying this practice in rural
communities. Therefore, it is necessary to study the knowledge, attitudes and practices of rural communities.
This study is an observational study with a cross-sectional approach. Data were collected using a validated
questionnaire. A total of 257 respondents dominated by low education level (53,53%) and low-income status
(98,44%). A numerous 59.92% had poor knowledge and 59.53% had a negative attitude. Factors such as
educational level (p=0.035), income status (p=0.010), knowledge (p=0.004) and attitude (p=0.000) were
significantly associated with the practice of self-medication with antibiotics. In general, socio-demographic
factors influence people's decision to self-medicate with antibiotics. The health care providers such as doctors
and physicians should be concerned to improve knowledge and awareness towards antibiotic use in properly.
1 INTRODUCTION
Self-medication of antibiotic is frequently
encountered in the general population. This act
closest to inappropriate antibiotic use and leads to
antibiotic resistance. Ninety percent of antibiotics are
purchased without a prescription (Puspitasari et al.,
2011). The Indonesian Minister of Health has issued
a regulation on general guidelines for the use of
antibiotics in Minister of Health Regulation No. 28 in
2021. Under these rules, antibiotics can only be given
or purchased with a medical prescription (Regulation
of The Minister of Health of The Republic of
Indonesia Number 28 of 2021, 2021).
a
https://orcid.org/0000-0003-0199-8717
b
https://orcid.org/0009-0009-2203-5312
c
https://orcid.org/0000-0002-2075-8308
d
https://orcid.org/0009-0009-9909-1232
e
https://orcid.org/0009-0009-7380-189X
f
https://orcid.org/0000-0001-6109-0482
The practice of self-medication involves the
unsupervised administration of medication, including
antibiotics, by an individual without seeking expert
medical advice for diagnosis or prescription (Nepal &
Bhatta, 2018). It is considered as unhealthy behaviour
and inappropriate as a treatment method.
Previous studies have shown that even when
people have access to knowledge about dosage,
appropriate duration of use and risk of drug
interactions, many still misuse antibiotics (Nepal &
Bhatta, 2018). This leads to antibiotic resistance,
where the infection is difficult to treat with standard
antibiotic therapy (Sachdev et al., 2022; Ventola,
2015).
Antibiotic resistance is a global health problem
and continues to be a major target framework. As
Ramdini, D. A., Sayoeti, M. F. W., Suharmanto, , Triyandi, R., Iqbal, M. and Sinuraya, R. K.
Self-Medication of Antibiotic Use: Investigating Knowledge and Attitude Among Rural Population in Umbul Natar Village, South of Lampung.
DOI: 10.5220/0013672400003873
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Medical Science and Health (ICOMESH 2023), pages 359-370
ISBN: 978-989-758-740-5
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
359

many as 700,000 people will die from antimicrobial
resistance in 2013, and by 2025, about 10 million
people will die each year from antimicrobial
resistance (WHO, 2014). Case fatality rates of
resistance in hospital-acquired infections in newborn
babies have been reported to range from 44.3% to
31%. Antimicrobial resistance is a condition where
the infection becomes resistant to standard antibiotic
therapy. This condition can affect the effectiveness of
therapy and the cost of treatment. Several factors are
the cause of antibiotic resistance, including overuse
and misuse (Aris et al., 2012; Voidăzan et al., 2019;
WHO, 2014).
Basic Health Research data from the Indonesian
Ministry of Health in 2013 reported that 10% of the
population kept antibiotics at home. Of these, 86.10%
received antibiotics without a prescription (The
Indonesian Ministry of Health, 2013). Antibiotic self-
medication is common in developed and developing
countries with a prevalence range of 35%-75% (F.A.
et al., 2009; Skliros et al., 2010). In Indonesia,
antibiotics are often given without prescription, such
as in pharmacies, drug stores, and even roadside
stalls. A survey on the population in the province of
Yogyakarta reported that 64% of purchases of
antibiotics were without prescription. Generally, the
use of antibiotics is in cases of respiratory disorders,
which is 80% (Hadi et al., 2008), including the
common cold, cough, sore throat, dizziness, and other
symptoms of respiratory disorders. Types of
antibiotics that are often used are amoxicillin,
fradiomycin-gramicidin, tetracycline, and
ciprofloxacin.
There are several factors that contribute to self-
medication with antibiotics. These include a lack of
knowledge about the use of antibiotics, a perception
of the high cost of visiting a doctor, and a belief that
antibiotics must always be used to treat a specific
illness. In fact, self-medication is an important factor
driving the overuse of antibiotics, especially in low
and middle-income countries, where antibiotics are
readily accessible without a prescription
(Ayukekbong et al., 2017). Low-income and middle-
income countries (LMICs) play an important role in
the global response to antimicrobial resistance
(AMR) (Chandler et al., 2016). The population in
these countries considers self-medication with
antibiotics to be cheaper and more affordable than
seeing a doctor. They were often associated with lack
knowledge and negative attitudes towards the
appropriate use of antibiotics (Dyar et al., 2020).
Various factors play a role in the behaviour of self-
medication antibiotics, such as purchasing antibiotics
freely without supervision, economic conditions and
urgency of time, the influence of family or friends,
and the level of community knowledge. Antibiotic
self-medication is affected by ease of access to
getting antibiotics without a prescription (Insany et
al., 2015). Good knowledge and positive attitude
considerably affect the practice of antibiotic self-
medication, although in some situations it does not
result in good practice regarding the use of antibiotics
(Pham-Duc et al., 2019). The study of Al Qarni et al.
stated that individuals with good knowledge about
antibiotics also have a good attitude towards the use
of antibiotics (Alqarni & Abdulbari, 2019).
One of the rural areas not far from the capital city
of Lampung is the village of Umbul Natar South
Lampung. The majority of the population in this
village work as farmers and traders, with a medium to
low level of education, which can provide an
overview of the pattern of antibiotic use in self-
medication. One of the strategies to tackle
antimicrobial resistance is to improve knowledge and
attitudes about antibiotic use. One of the efforts to
support the World Health Organization (WHO)
Emergency Programme on Antimicrobial Resistance
(AMR) is community education. Therefore, it is
necessary to investigate the relationship between
knowledge, attitudes and practices regarding
antibiotic self-medication in rural communities in
South Lampung, Indonesia. This study aims to
identify the factors that influence the implementation
of the antibiotic resistance control programme.
2 METHOD
2.1 Research Design
This is an analytical observational study with a cross-
sectional approach. The instrument used is a
questionnaire consisting of questions about
knowledge, attitudes, and practice in antibiotic self-
medication. The target population is community in
Umbul Natar Village South of Lampung, Indonesia.
Technic sampling by purposive sampling. The
inclusion criteria in this study were people from
adolescence to adulthood who were willing to be
respondents. The exclusion criteria were that the
respondents did not fill out the questionnaire. The
data obtained will be presented descriptively in tables
and figures. To determine the correlation between
demographic factors towards knowledge, attitudes,
and practice, we used the chi-square test was carried
out with a 95% confidence level (p <0.05). This
research has received ethical approval from the
Research Ethics Committee of the Faculty of
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
360

Medicine, the University of Lampung with Number
1378/ UN26.18/ PP.05.02.00/ 2020.
2.2 Collected Data Knowledge,
Attitude
Knowledge and attitude measurements were
conducted using a questionnaire adapted from similar
research questionnaires with modifications and
tailored to the expected information (10,20–22). The
questionnaire was narrated in Bahasa Indonesia and
consisted of 4 knowledge questions (K1-K4) on a
Guttman Scale, 7 attitude statements (A1-A7) on a
Likert scale and 4 practice questions on a Guttman
Scale. The questionnaire has been validated with the
Cronchbach score of knowledge, attitude and practice
questions being 0.684; 0.799; 0.604 respectively.
2.2.1 Knowledge
There are 4 question items (K1-K4) in the knowledge
section with true and false statements. K1, K2 and K4
are questions with false statements or unfavourable
question and K3 true statements or favourable
question. The determination of the knowledge level
referred to the cut of mean value of the respondent's
answer. The cut of median score is 3 which means
that less than 3 is considered as poor and more than
equal to 3 was as a good level.
2.2.2 Attitude
This section consists of 7 statement items with the
answers strongly agree, agree, disagree, and strongly
disagree. Statements A1, A2, A3, and A4 are
negative statements so that the highest score starts
from the answers strongly disagree = 4, disagree = 3,
agree = 2, and strongly agree = 1. Statements A5, A6,
and A7 are positive statements so that the highest
score starts from the answers strongly agree = 4, agree
= 3, disagree = 2, and strongly disagree = 1. The
criteria for the positive attitude category refer to the
median cut off score of the respondent's answer value,
where positive attitude ≥ 15, and negative attitude if
the value is < 15.
2.2.3 Practice
This section consists of 3 questions that aim to
determine antibiotic use or the experience of using
antibiotics. Description of the questions P1:
Did you
take the antibiotics as recommended by your doctor
or health care professional, P2:
Have you finished the
full course of antibiotics prescribed by your doctor,
P3:
Did you consult a healthcare professional before
antibiotic use? P4: Would you share the antibiotics
you are currently using if your family were ill.
Question P1-P3 are favourable and P4 unfavourable.
The questions using “Yes” or “No” answer, and if
they had a value of ≥2 then it was considered a good
practice. This statement illustrated respondents doing
antibiotic self-medication and practicing doing
antibiotics self-medication.
3 RESULTS
3.1 Demographic Data
A total of 257 respondents completed the
questionnaire. The socio-demographic data of the
respondents are presented in Table 1. Overall, most
of the respondents were male (50.97%) and
dominated by the age group of 36-55 years
(41.78%). Most of them had primary and basic
education (53.31%). In terms of income status, the
majority of the respondents were below the
regional minimum wage (90.44 %). Many
respondents worked as housewives (26.46%) and
farmers (19.07). Information about antibiotics was
received from the family by 75.49% of
respondents.
3.2 Knowledge’s and Attitude Data
Based on the respondents' answers to several
knowledge questions, the majority of respondents had
poor knowledge (59.92%) and as many as 40.08%
had good knowledge. Table 2 shows respondents'
responses to questions about antibiotics. Many
respondents thought that antibiotics did not need to be
finished (60.31%) and thought that antibiotics could
treat cold and cough (97.28%). In addition, most
respondents understood that antibiotics can boost the
immune system (98.44%), but many of them also
knew that antibiotics have side effects.
Self-Medication of Antibiotic Use: Investigating Knowledge and Attitude Among Rural Population in Umbul Natar Village, South of
Lampung
361

Table 1: Characteristic of Respondents
Characteristics n %
Sex
Male 131 50,97
Female 126 49,03
Age (cut off in years)
<35 135 52,53
≥ 35 122 47,47
Education level
Elementary and basic school 137 53,31
Middle education level 113 43,97
At University level 3 1,17
Income (Regional Minimum Rate)
Under Regional Minimum Rate 253 98,44
Regional Minimum Rate or more 22 8,56
Occupation
Businessman 19 7,39
Employee 17 6,61
Farmer 49 19,07
Freelancer 25 9,73
Housewife 68 26,46
Labor 35 13,62
Student 41 15,95
Unemployement 3 1,17
Source of information Antibiotic Use
Health Providers 29 11,28
Family 194 75,49
Friend/Colleague 32 12,45
Internet 2 0,78
Table 2: Knowledge Respondents on Antibiotic Use
Code Knowledge on antibiotic use Correct response % Incorrect response %
K1 Antibiotics don't require the full
course to be completed
155 60,31 102 39,69
K2 Antibiotic work for the flu and cough 250 97,28 7 2,72
K3 Antibiotic have side effect 251 97,67 6 2,33
K4 Antibiotics boosted your immune
system
253 98,44 4 1,56
Table 3 demonstrates the attitudes of the participants.
Statements A1-A4 are negative statements, whereas
disagree or strongly disagree indicates a positive
attitude. Regarding the results of participants'
responses to several attitude questions, the majority
had negative (59.53%) and some positive (40.47%)
attitudes. A total of 64.59% of respondents agreed
with the statement "Buying antibiotics without a
prescription". A total of 93.39% of respondents
agreed that they give antibiotics to their family as
long as they have the same illness, and 90.66% of
respondents agreed with the statement that they keep
a stock of antibiotics at home for use when they are
ill. In statement A4, 94.55% of respondents agreed
that they use antibiotics for farm animals (chickens).
Overall, negative attitudinal statements (A1-A4)
generally indicate that respondents self-medicate
with antibiotics. Statements A5-A7 are positive, i.e.
respondents agree or strongly agree, indicating a
positive attitude. A total of 89.11% of respondents
disagreed with the statement that a course of
antibiotics must be completed, more than 89.49% of
respondents agreed that not taking antibiotics
properly can be harmful to health (A6) and 94.55%
agreed with the statement that consultation with
health provider before taking antibiotics (A7). Most
respondents also have negative attitudes based on
favorable questions.
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
362
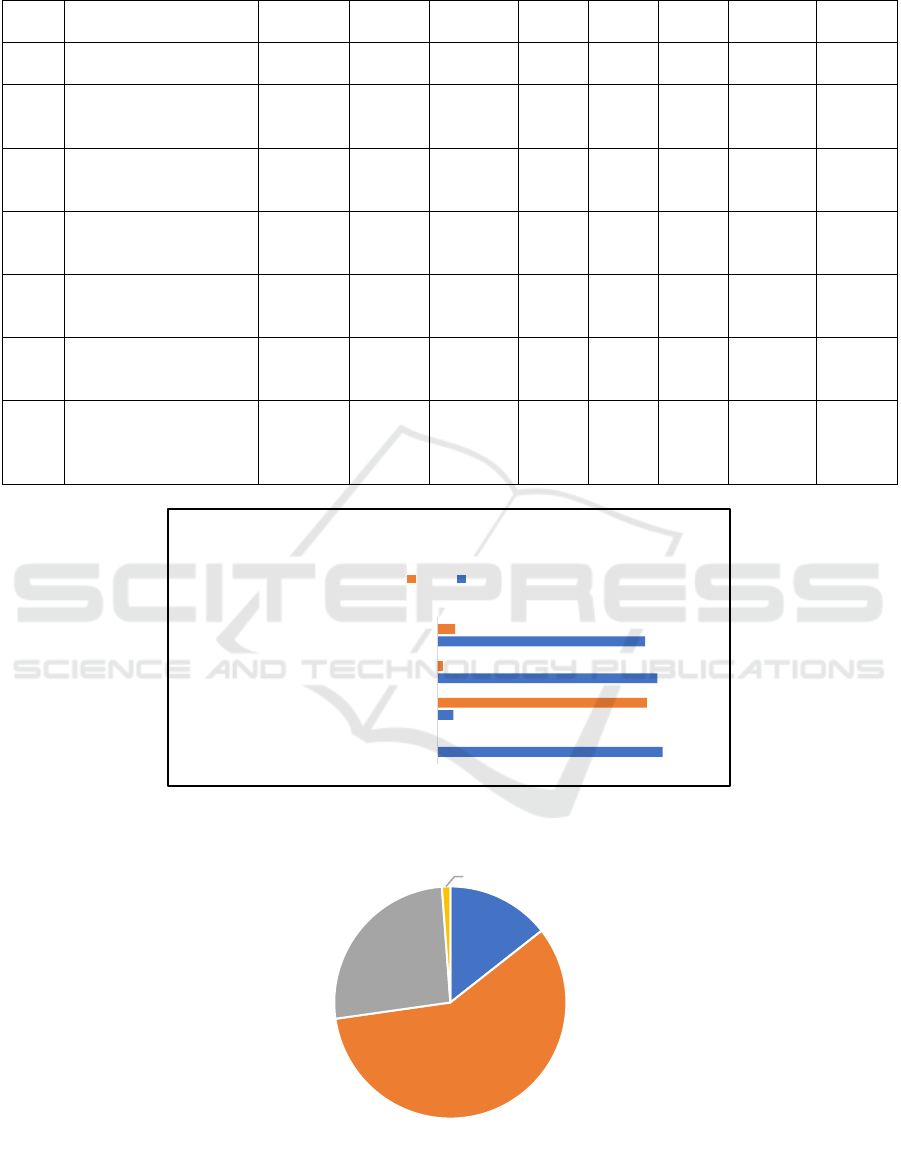
Table 3: Attitude Respondents on Antibiotic Use
Code Statements
Strongly
Disagree
% Disagree % Agree %
Strongly
agree
%
A1
Buy antibiotics without
a
p
rescri
p
tion
0 0,00 88 34,24 166 64,59 0 0,00
A2
Give antibiotics to the
family as long as
havin
g
the same illness
3 1,16 9 3,50 240 93,39 5 1,95
A3
Keep stock of
antibiotics at home for
usage when sic
k
2 0,77 8 3,11 233 90,66 14 5,45
A4
Antibiotics are given to
farm animals
(chickens)
0 0,00 5 1,95 243 94,55 9 3,50
A5
Full course of
antibiotics must be
finishe
d
0 0,00 229 89,11 13 5,06 15 5,84
A6
Not taking antibiotics
properly can be
harmful to health
2 0,77 230 89,49 21 8,17 4 1,56
A7
A health provider
should be consulted
before taking
antibiotics
0 0,00 5 1,95 243 94,55 9 3,50
Figure 4: Respondent’s Practice of Antibiotic used
Figure 3. Reasons for The Use of Antibiotic Self-Medication
100
7.0
97.67
92.22
0
93.00
2.33
7.78
P1 (Using Antibiotic recommended by Doctor)
P2 (finished the full course of antibiotics use )
P3 (Consult a healthcare professional before taking
antibiotics)
P4 (Shared antibiotic to Family)
Percentage of Respondent's Answer
No Yes
Low cost
15%
Easy accessible
58%
Low cost and easy
accessible
26%
Medication from
doctor doesn’t work
1%
Self-Medication of Antibiotic Use: Investigating Knowledge and Attitude Among Rural Population in Umbul Natar Village, South of
Lampung
363

Figure 3. Reasons to Use Antibiotics without Prescription Among Respondents.
We collected data reason for the use of antibiotic self-
medication from the respondents. Overall,
respondents were considered self-medication with
antibiotic is easy-accessible and low cost. Respondent
also consumed it for some medical problem such as
flu (33%), fever (32%), cough (21%) and others.
3.3 Correlation Characteristic
Respondents Toward Knowledge
and Attitude
We also analyzed a number of characteristics in
relation to knowledge and attitudes on a bivariate
basis (Table 4). Gender (p=0.308), level of education
(p=0.075), income (p=0.756) was not significantly
related to knowledge, but age was significantly
related to knowledge (p=0.032) with a p-value > 0.05.
Meanwhile, the factors age (p=0.045) and education
(p=0.018) were significantly related to the
respondents’ attitude with a p-value <0.05, but the
factors age (p=0.161) and income (p=0.102) were not
significantly related to this attitude.
Table 4: Characteristic’s Respondents toward Knowledge and Attitude
Characteristics
Knowledge
p-value
Attitude
p-value
Poor
n=154
%
Good
n=103
%
Negative
n=153
%
Positive
n=104
%
Gender
0,308
0,161 Male 83 32,3 48 18,7 84 32,7 47 18,3
Female 71 27,6 55 21,45 69 26,8 57 22,2
Age
0,032*
0,045* <35 years 72 28,0 63 24,5 72 28,0 63 24,5
≥ 35 years 82 31,9 40 15,6 81 31,5 41 16,0
Level of Education
0,075
0,018*
Elementary and
basic school
88 34,2 49 19,1 90 35,0 47 18,3
Middle education
level
60 23,3 53 20,6 57 22,2 56 21,8
At University level 6 2,3 1 0,4 6 6 1 0,4
Income (Regional
Minimum Rate)
0,756
0,102
Under Regional
Minimum Rate
142 55,3 93 36,2 144 56 91 35,4
Regional Minimum
Rate and more
12 4,7 10 3,9 9 3,5 13 5,1
Chi square with p value <0,05
Pain
4%
Allergy
4%
Sore throat
6%
Cough
21%
Fever
32%
Flu
33%
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
364
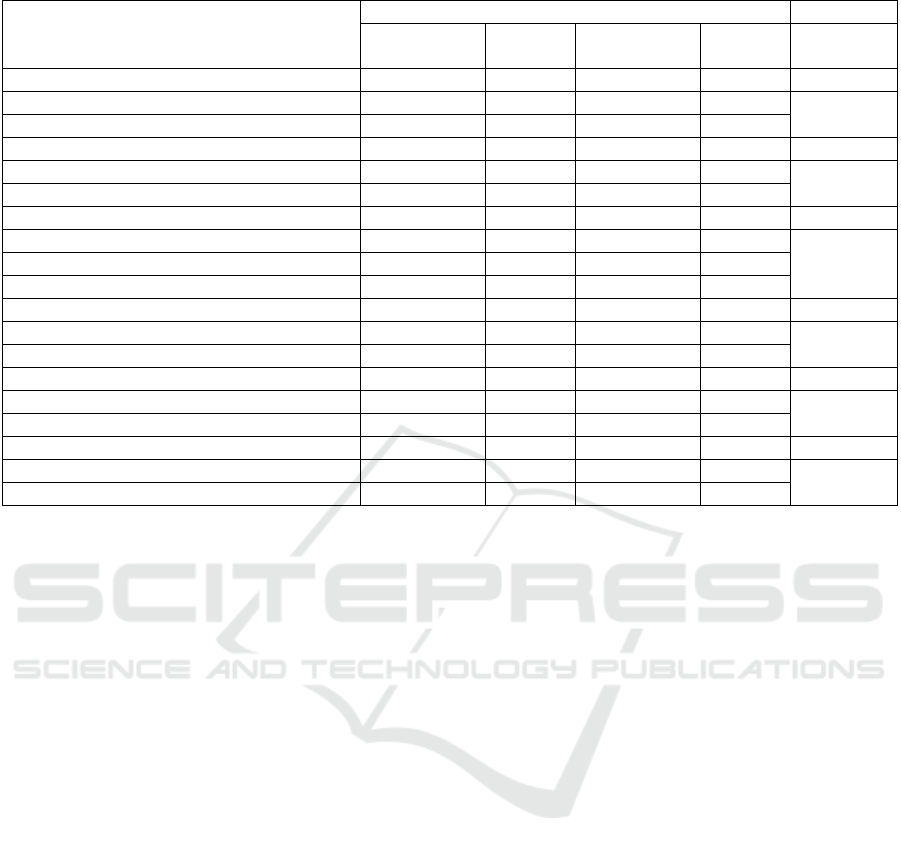
Table 5. Correlation Characteristics toward Self-Medication with Antibiotic
Characteristics
Self Medication Antibiotic
No
n=11
% Yes
n=246
% p value
Gender
Male 5 1,9 126 49,0 0,947
Female 6 2,3 120 46,7
Age
<35 years 9 3,5 126 49,0 0,093
≥ 35 years 2 0,8 120 46,7
Level of Education
Elementary and basic school 2 0,8 135 52,5 0,035*
Middle education level 9 3,5 104 40,5
At University level 0 0,0 7 2,7
Income (Regional Minimum Rate)
Under Regional Minimum Rate 22 7,53 245 83,90 0,010
Regional Minimum Rate and more 6 2,05 19 6,51
Knowledge
Poor 2 0,8 152 59,1 0,004*
Good 9 3,5 94 36,6
Attitude
Positive 10 3,9 94 36,6 0,000*
Negative 1 0,4 152 59,1
Chi square with p value <0,05
3.4 Characteristic’s Respondents
Toward Self-Medication with
Antibiotic Practice
We also assessed the relationship between socio-
demographic factors, level of knowledge and attitude
towards the practice of antibiotic self-medication
(Table 5). This analysis showed the respondents who
performed or had experience of antibiotic self-
medication based on the factors suspected to be
related. Based on the bivariate analysis, the factors of
education (p=0,035), income (p=0,010), knowledge
(p=0,004) and attitude (p=0,000) were significantly
associated with the practice of antibiotic self-
medication at p<0,05. On the other hand, other socio-
demographic factors such as gender (p=0,947) and
age (p=0,093) were not significantly associated with
the practice of self-medication with antibiotics
4 DISCUSSIONS
This is an observational study of antibiotic self-
medication in a village community in Lampung
Province. Of the 257 participants, 95.71% of
respondents were engaged in the practice of antibiotic
self-medication. The high prevalence of antibiotic
self-medication in the rural population is also found
in several countries, including Greece 77.9% (Skliros
et al., 2010), Sindh Pakistan 81.25% (Bilal et al.,
2016), and India 74% (Pentareddy et al., 2017), and
also in regions with different population
characteristics (non-rural), such as Yogyakarta
Indonesia (58%) (Kristina et al., 2020a), Saudi Arabia
(78.1%) (Al Rasheed et al., 2016), Eritrea (Africa)
(45.1%) (Ateshim et al., 2019), Tanzania (58%)
(Horumpende et al., 2018), and Ethiopia (67%)
(Bogale et al., 2019). These data indicate that self-
medication with antibiotics is common in rural
communities, especially among lower-middle-
income people. Some of the findings among the
respondents included the belief that antibiotics can
enhance the immune system and treat colds and
coughs. A study in Yogyakarta revealed that the
majority of respondents (58%) had a low level of
knowledge about antibiotic use and awareness, and
mistakenly thought that colds and coughs can be
treated with antibiotics (75%) (Kristina et al., 2020b).
Misperceptions about the indications for antibiotics
may influence people's attitudes and practices
regarding antibiotic use. No study has been done to
investigate the perception that antibiotics improve the
immune system, and it demonstrates a lack of
understanding of the immune system and the role of
antibiotics in the rural population. Another study
found that individuals engage in self-medication with
antibiotics for various reasons such as flu, cough,
Self-Medication of Antibiotic Use: Investigating Knowledge and Attitude Among Rural Population in Umbul Natar Village, South of
Lampung
365

common cold, sore throat, diarrhea, toothache, pain
relief, and fever (Aslam et al., 2020; Hawking et al.,
2017). Most people do not understand the difference
between antibacterial and antiviral, they consider they
are the same (Hawking et al., 2017). A similar
misunderstanding is also found in several countries
such as in South Africa (66%) (Farley et al., 2019),
Yogyakarta-Indonesia (70%) (Aris et al., 2012), and
Kosovo (42,1%) (Zajmi et al., 2017). Misconceptions
about antibiotics as having antiviral or antibacterial
properties are also found in some countries such as
Malaysia, 75% of respondents have an understanding
that antibiotics can cure colds and coughs (Ka Keat &
Chew Charn, 2012).
We found age and level of education associated to
attitude of self-medication with antibiotic. Bhardwaj
et al, reported that respondents with a high school
education level had less knowledge of antibiotics than
respondents with higher education (Bhardwaj et al.,
2021). Generally, our discovered shows respondents
in basic school to secondary school level (senior high
school, junior high school, and elementary school)
had insufficient knowledge level. Knowledge is an
essential component to determine attitudes and
practice. Good knowledge supports a person to be
more aware of how to use antibiotics properly
(Voidăzan et al., 2019). And it correlated positively
with attitudes towards antibiotic use (p<0.001) (Ka
Keat & Chew Charn, 2012).
Another fact from this study shows that majority
of the respondents agreed that antibiotics should be
given to farm animals. As reported in several studies,
antimicrobial use in farm animals is also quite
widespread (Founou et al., 2016; Van Boeckel et al.,
2015). One of the reasons for this is a lack of
understanding and public awareness of the correct use
of antibiotics. While antimicrobials have been used to
maintain animal health and improve productivity,
their overuse in feed has led to increased
antimicrobial resistance (Ma et al., 2021). The
attitude assessment showed that 90.75% of
respondents had a negative attitude towards the use of
antibiotics. Based on gender characteristics, men and
women have the same proportion of negative attitudes
towards the use of antibiotics. Mostly, respondents
who have a negative attitude are those with high
school education and below. Only the level of
education and knowledge correlate significantly to
the respondent's attitude (p<0.05). Another study
reported that higher levels of education relate to more
favourable attitudes towards antibiotic use (Alqarni &
Abdulbari, 2019; Waaseth et al., 2019). This indicate
that knowledge does not reflect a positive attitude, it
can be seen in the inconsistency of respondents'
answers. All respondents (100%) gave the correct
answer for the statement that antibiotics require a
prescription. However, 60.96% answered that they do
buy antibiotics without a prescription. People who
have negative attitudes toward antibiotic use tend to
keep antibiotics at home as stock when sick. Most of
the respondents agree with this statement (86,99%).
A study in the Philippines reported about 52.4% of
respondents agree with the statement of the need to
keep antibiotics in stock (Barber et al., 2017). Keep
antibiotic in stock leads improper and overuse
antibiotic, beside antibiotic use needs indication and
dosage appropriate. Numerous people use it refer to
the past history prescription from doctor.
Socioeconomics is one factor that influences self-
medication, such as income factor. Rural
communities tend to have low incomes or earn below
the regional minimum wage. This condition
encourages people to try solutions to overcome their
health problems by using antibiotics freely/without a
prescription (Haenssgen et al., 2019). The
characteristics of population studies affecting
towards antibiotics self-medication behaviour at
varied levels of significance. The rural population is
identical to the low-income and middle-income. We
found the majority of respondents have income below
the Regional Minimum Wage. Income level as factor
affecting to practice antibiotic self-medication
showed correlated significantly. Based on several
observational studies, it has been reported that
antibiotic self-medication antibiotics is more
frequently found in people with lower middle income
(Aslam et al., 2020). Self-medication was considered
to be less time-consuming, cheaper, and overall, more
convenient than accessing them through healthcare
facilities (Do et al., 2021). In this study, respondents
stated that the reason was that they thought the drugs
prescribed by doctors were less effective, as in the
Haque et al (2019) study which reported that one of
the driving factors is a lack of confidence in the drug
prescribed by physicians (Haque et al., 2019). In
contrast to the study in Croatia, where the number of
respondents with a high level of confidence in
doctor's treatment is greater and who tend to more and
they are those who have good knowledge (Farkaš et
al., 2019).
In general, behaviour is affected by knowledge
and attitudes. This study showed a significant
correlation between knowledge and attitudes towards
antibiotics self-medication (p<0.001). Poor
knowledge and negative attitudes correlate with
respondent's practice in using antibiotics without a
prescription. The results of surveys on the use of
antibiotics in various countries are quite diverse.
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
366

However, there have the same misconceptions
regarding knowledge and awareness, self-medication,
left-over antibiotics, and reasons for using antibiotics
(Antwi et al., 2020). Healthcare professionals,
including physicians, pharmacists, nurses, and other
healthcare professionals, have a responsibility for
clinical practice to keep antibiotics effective
(Napolitano et al., 2019; Pearson & Chandler, 2019;
Rábano-Blanco et al., 2019). The extent of
misconception and inappropriate practice in the
community and has been going on for a long time,
which makes this misunderstanding a serious matter
to be corrected. Attempt to increase knowledge and
awareness of the use of antibiotics can be done in
various ways, one of which is by pharmacist playing
an active role in educating the public (Shehadeh et al.,
2016). In addition, providing direct counselling on
antibiotic information has proven to be effective in
increasing knowledge and awareness of antibiotic use
(Mason et al., 2018). A systematic review study states
that the provision of information through leaflets
delivered during an infectious disease consultation is
more effective in increasing understanding and
attitudes towards drug use (De Bont et al., 2015).
Education on the risks of potential side effects of
antibiotics and their benefits is more likely to have a
major impact on antibiotic self-medication decisions
than education about antibiotic resistance (Spicer et
al., 2020). This study was an observational and did
not specific age population which would give the
certain information about self-medication antibiotic
use in rural areas. Our finding provides the general
information antibiotic self-medication in village
where majority had lower education level. Proper and
wise use of antibiotics is an effort to prevent antibiotic
resistance which is currently considered an
emergency global problem. Based on the results of
this study, factors associated with antibiotic self-
medication behaviour can help determine appropriate
strategies to prevent and overcome this problem.
Such as the outreach of information about antibiotic
use to people living in rural areas, taking into account
the characteristics of the population from the level of
education and socio-economic aspects. Furthermore,
the strategy of providing education for health workers
needs to be improved, especially for rural
populations.
5 CONCLUSIONS
Population living in rural area dominated lower level
of education, income status. These may have impact
or correlate to level of knowledge, attitude and
practice self-medication antibiotic. We found that
knowledge, attitude associated to self-medication
with antibiotic practice. The management risk that
would be implemented is improve the understanding
and awareness toward antibiotic use. Furthermore, it
needs contribution of health professional such
physician, pharmacist and nurse to encourage rural
communities to improving knowledge and positive
attitudes toward behaviour of antibiotic self-
medication.
ACKNOWLEDGEMENTS
We thank participants for their willingness to
complete the questionnaire. Authors would like to
thank pharmacies used as study sites as well as the
surveying pharmacy students at Universitas
Lampung, Indonesia.
CONFLICT OF INTEREST
The authors declared no conflict of interest in this
study
REFERENCES
Al Rasheed, A., Yagoub, U., Alkhashan, H., Abdelhay, O.,
Alawwad, A., Al Aboud, A., & Al Battal, S. (2016).
Prevalence and Predictors of Self-Medication with
Antibiotics in Al Wazarat Health Center, Riyadh City,
KSA. BioMed Research International, 2016.
https://doi.org/10.1155/2016/3916874
Alqarni, S. A., & Abdulbari, M. (2019). Knowledge and
attitude towards antibiotic use within consumers in
Alkharj, Saudi Arabia. Saudi Pharmaceutical Journal,
27(1). https://doi.org/10.1016/j.jsps.2018.09.003
Antwi, A. N., Stewart, A., & Crosbie, M. (2020). Fighting
antibiotic resistance: a narrative review of public
knowledge, attitudes, and perceptions of antibiotics use.
Perspectives in Public Health, XX(X).
https://doi.org/10.1177/1757913920921209
Aris, W., Sri, S., Charlotte, de C., & E, H. J. (2012).
Knowledge and beliefs about antibiotics among people
in Yogyakarta City Indonesia: a cross-sectional
population-based survey. Antimicrobial Resistance and
Infection Control, 1(38), 491.
Aslam, A., Gajdács, M., Zin, C. S., Rahman, N. S. A.,
Ahmed, S. I., Zafar, M. Z., & Jamshed, S. (2020).
Evidence of the practice of self-medication with
antibiotics among the lay public in low-and middle-
income countries: A scoping review. Antibiotics, 9(9),
1–17. https://doi.org/10.3390/antibiotics9090597
Self-Medication of Antibiotic Use: Investigating Knowledge and Attitude Among Rural Population in Umbul Natar Village, South of
Lampung
367

Ateshim, Y., Bereket, B., Major, F., Emun, Y., Woldai, B.,
Pasha, I., Habte, E., & Russom, M. (2019). Prevalence
of self-medication with antibiotics and associated
factors in the community of Asmara, Eritrea: A
descriptive cross-sectional survey. BMC Public Health,
19(1), 1–7. https://doi.org/10.1186/s12889-019-7020-x
Ayukekbong, J. A., Ntemgwa, M., & Atabe, A. N. (2017).
The threat of antimicrobial resistance in developing
countries: Causes and control strategies. In
Antimicrobial Resistance and Infection Control (Vol. 6,
Issue 1). https://doi.org/10.1186/s13756-017-0208-x
Barber, D. A., Casquejo, E., Ybañez, P. L., Pinote, M. T.,
Casquejo, L., Pinote, L. S., Estorgio, M., & Young, A.
M. (2017). Prevalence and correlates of antibiotic
sharing in the Philippines: antibiotic misconceptions
and community-level access to non-medical sources of
antibiotics. Tropical Medicine and International
Health, 22(5), 567–575.
https://doi.org/10.1111/tmi.12854
Bhardwaj, K., Shenoy M, S., Baliga, S., Unnikrishnan, B.,
& Baliga, B. S. (2021). Knowledge, attitude, and
practices related to antibiotic use and resistance among
the general public of coastal south Karnataka, India – A
cross-sectional survey. Clinical Epidemiology and
Global Health, 11.
https://doi.org/10.1016/j.cegh.2021.100717
Bilal, M., Haseeb, A., Khan, M. H., Arshad, M. H., Ladak,
A. A., Niazi, S. K., Musharraf, M. D., & Manji, A. A.
K. (2016). Self-medication with antibiotics among
people dwelling in rural areas of Sindh. Journal of
Clinical and Diagnostic Research, 10(5).
https://doi.org/10.7860/JCDR/2016/18294.7730
Bogale, A. A., Amhare, A. F., Chang, J., Bogale, H. A.,
Betaw, S. T., Gebrehiwot, N. T., & Fang, Y. (2019).
Knowledge, attitude, and practice of self-medication
with antibiotics among community residents in Addis
Ababa, Ethiopia. Expert Review of Anti-Infective
Therapy, 17(6), 459–466.
https://doi.org/10.1080/14787210.2019.1620105
Chandler, C. I. R., Hutchinson, E., & Hutchinson, C.
(2016). Addressing Antimicrobial Resistance through
Social Theory: An Anthropologically Oriented Report.
London School of Hygiene & Tropical Medicine,
November.
De Bont, E. G. P. M., Alink, M., Falkenberg, F. C. J.,
Dinant, G. J., & Cals, J. W. L. (2015). Patient
information leaflets to reduce antibiotic use and
reconsultation rates in general practice: A systematic
review. BMJ Open, 5(6).
https://doi.org/10.1136/bmjopen-2015-007612
Do, N. T. T., Vu, H. T. L., Nguyen, C. T. K., Punpuing, S.,
Khan, W. A., Gyapong, M., Asante, K. P., Munguambe,
K., Gómez-Olivé, F. X., John-Langba, J., Tran, T. K.,
Sunpuwan, M., Sevene, E., Nguyen, H. H., Ho, P. D.,
Matin, M. A., Ahmed, S., Karim, M. M., Cambaco, O.,
… Wertheim, H. F. L. (2021). Community-based
antibiotic access and use in six low-income and middle-
income countries: a mixed-method approach. The
Lancet Global Health, 9(5).
https://doi.org/10.1016/S2214-109X(21)00024-3
Dyar, O. J., Zhang, T., Peng, Y., Sun, M., Sun, C., Yin, J.,
Ding, L., Sun, C., Wang, Y., Sun, Q., Greko, C., &
Stålsby Lundborg, C. (2020). Knowledge, attitudes and
practices relating to antibiotic use and antibiotic
resistance among backyard pig farmers in rural
Shandong province, China.
Preventive Veterinary
Medicine, 175(June 2019), 104858.
https://doi.org/10.1016/j.prevetmed.2019.104858
F.A., S., Z.H., B., A., A. K., & R., A. E. (2009). Assessment
of self-medication of antibiotics in a Jordanian
population. In Medical Principles and Practice.
Farkaš, M., Glažar Ivče, D., Stojanović, S., Mavrinac, M.,
Mićović, V., & Tambić Andrašević, A. (2019). Parental
knowledge and awareness linked to antibiotic use and
resistance: Comparison of urban and rural population in
Croatia. Microbial Drug Resistance, 25(10).
https://doi.org/10.1089/mdr.2018.0424
Farley, E., Van den Bergh, D., Coetzee, R., Stewart, A., &
Boyles, T. (2019). Knowledge, attitudes and
perceptions of antibiotic use and resistance among
patients in South Africa: A cross-sectional study.
Southern African Journal of Infectious Diseases, 34(1).
https://doi.org/10.4102/sajid.v34i1.118
Founou, L. L., Founou, R. C., & Essack, S. Y. (2016).
Antibiotic resistance in the food chain: A developing
country-perspective. In Frontiers in Microbiology (Vol.
7, Issue NOV).
https://doi.org/10.3389/fmicb.2016.01881
Hadi, U., Duerink, D. O., Lestari, E. S., Nagelkerke, N. J.,
Werter, S., Keuter, M., Suwandojo, E., Rahardjo, E.,
van den Broek, P., & Gyssens, I. C. (2008). Survey of
antibiotic use of individuals visiting public healthcare
facilities in Indonesia. International Journal of
Infectious Diseases, 12(6), 622–629.
https://doi.org/10.1016/j.ijid.2008.01.002
Haenssgen, M. J., Charoenboon, N., Zanello, G., Mayxay,
M., Reed-Tsochas, F., Lubell, Y., Wertheim, H.,
Lienert, J., Xayavong, T., Khine Zaw, Y.,
Thepkhamkong, A., Sithongdeng, N.,
Khamsoukthavong, N., Phanthavong, C., Boualaiseng,
S., Vongsavang, S., Wibunjak, K., Chai-In, P.,
Thavethanutthanawin, P., … Ariana, P. (2019).
Antibiotic knowledge, attitudes and practices: New
insights from cross-sectional rural health behaviour
surveys in low-income and middle-income South-East
Asia. BMJ Open, 9(8).
https://doi.org/10.1136/bmjopen-2018-028224
Haque, M., Rahman, N. A. A., McKimm, J., Kibria, G. M.,
Majumder, M. A. A., Haque, S. Z., Islam, M. Z.,
Abdullah, S. L. B., Daher, A. M., Zulkifli, Z., Rahman,
S., Kabir, R., Lutfi, S. N. N. B., & Othman, N. S. A. B.
(2019). Self-medication of antibiotics: Investigating
practice among university students at the Malaysian
national defence university. Infection and Drug
Resistance, 12, 1333–1351.
https://doi.org/10.2147/IDR.S203364
Hawking, M. K. D., Lecky, D. M., Touboul Lundgren, P.,
Aldigs, E., Abdulmajed, H., Ioannidou, E., Paraskeva-
Hadjichambi, D., Khouri, P., Gal, M., Hadjichambis, A.
C., Mappouras, D., & McNulty, C. A. M. (2017).
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
368

Attitudes and behaviours of adolescents towards
antibiotics and self-care for respiratory tract infections:
A qualitative study. BMJ Open, 7(5).
https://doi.org/10.1136/bmjopen-2016-015308
Horumpende, P. G., Said, S. H., Mazuguni, F. S., Antony,
M. L., Kumburu, H. H., Sonda, T. B., Mwanziva, C. E.,
Mshana, S. E., Mmbaga, B. T., Kajeguka, D. C., &
Chilongola, J. O. (2018). Prevalence, determinants and
knowledge of antibacterial self-medication: A cross-
sectional study in North-eastern Tanzania. PLoS ONE,
13(10), 1–13.
https://doi.org/10.1371/journal.pone.0206623
Insany, A. N., Destiani, D. P., Sani, A., Sabdaningtyas, L.,
& Pradipta, I. S. (2015). Hubungan Persepsi terhadap
Perilaku Swamedikasi Antibiotik: Studi Observasional
melalui Pendekatan Teori Health Belief Model.
Indonesian Journal of Clinical Pharmacy.
Ka Keat, L., & Chew Charn, T. (2012). A cross-sectional
study of public knowledge and attitude towards
antibiotics in Putrajaya, Malaysia. Southern Med
Review, 5(2), 26–33.
http://www.fmhs.auckland.ac.nz/sop/smr/issues.aspx%
5Cnhttp://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE
=reference&D=emed11&NEWS=N&AN=201312528
6
Kristina, S. A., Wati, M. R., Prasetyo, S. D., & Fortwengel,
G. (2020a). Public knowledge and awareness towards
antibiotics use in Yogyakarta: A cross-sectional survey.
Pharmaceutical Sciences Asia, 47(2), 173–180.
https://doi.org/10.29090/PSA.2020.02.019.0008
Kristina, S. A., Wati, M. R., Prasetyo, S. D., & Fortwengel,
G. (2020b). Public knowledge and awareness towards
antibiotics use in Yogyakarta: A cross-sectional survey.
Pharmaceutical Sciences Asia, 47(2).
https://doi.org/10.29090/psa.2020.02.019.0008
Ma, F., Xu, S., Tang, Z., Li, Z., & Zhang, L. (2021). Use of
antimicrobials in food animals and impact of
transmission of antimicrobial resistance on humans. In
Biosafety and Health (Vol. 3, Issue 1).
https://doi.org/10.1016/j.bsheal.2020.09.004
Mason, T., Trochez, C., Thomas, R., Babar, M., Hesso, I.,
& Kayyali, R. (2018). Knowledge and awareness of the
general public and perception of pharmacists about
antibiotic resistance. BMC Public Health, 18(1), 1–10.
https://doi.org/10.1186/s12889-018-5614-3
Napolitano, F., Della Polla, G., De Simone, C., Lambiase,
C., Pelullo, C. P., & Angelillo, I. F. (2019). The
knowledge, attitudes, and practices of community
pharmacists in their approach to antibiotic use: A
nationwide survey in Italy. Antibiotics.
https://doi.org/10.3390/antibiotics8040177
Nepal, G., & Bhatta, S. (2018). Self-medication with
Antibiotics in WHO Southeast Asian Region: A
Systematic Review. Cureus.
https://doi.org/10.7759/cureus.2428
Pearson, M., & Chandler, C. (2019). Knowing antmicrobial
resistance in practice: a multi-country qualitative study
with human and animal healthcare professionals.
Global Health Action.
https://doi.org/10.1080/16549716.2019.1599560
Pentareddy, M. R., Vedula, P., B., R., L., J. C., &
Amarendar, S. (2017). Comparison of pattern of self-
medication among urban and rural population of
Telangana state, India. International Journal of Basic
& Clinical Pharmacology, 6(11).
https://doi.org/10.18203/2319-2003.ijbcp20174795
Pham-Duc, P., Cook, M. A., Cong-Hong, H., Nguyen-
Thuy, H., Padungtod, P., Nguyen-Thi, H., & Dang-
Xuan, S. (2019). Knowledge, attitudes and practices of
livestock and aquaculture producers regarding
antimicrobial use and resistance in Vietnam. PLoS
ONE. https://doi.org/10.1371/journal.pone.0223115
Puspitasari, H. P., Faturrohmah, A., & Hermansyah, A.
(2011). Do Indonesian community pharmacy workers
respond to antibiotics requests appropriately? Tropical
Medicine and International Health, 16(7), 840–846.
https://doi.org/10.1111/j.1365-3156.2011.02782.x
Rábano-Blanco, A., Domínguez-Martís, E. M., Mosteiro-
Miguéns, D. G., Freire-Garabal, M., & Novío, S.
(2019). Nursing students’ knowledge and awareness of
antibiotic use, resistance and stewardship: A descriptive
cross-sectional study. Antibiotics.
https://doi.org/10.3390/antibiotics8040203
Regulation of The Minister of Health of The Republic of
Indonesia Number 28 of 2021 (2021).
Sachdev, C., Anjankar, A., & Agrawal, J. (2022). Self-
Medication With Antibiotics: An Element Increasing
Resistance. Cureus, 14(10).
https://doi.org/10.7759/CUREUS.30844
Shehadeh, M. B., Suaifan, G. A. R. Y., & Hammad, E. A.
(2016). Active educational intervention as a tool to
improve safe and appropriate use of antibiotics. Saudi
Pharmaceutical Journal, 24(5).
https://doi.org/10.1016/j.jsps.2015.03.025
Skliros, E., Merkouris, P., Papazafiropoulou, A., Gikas, A.,
Matzouranis, G., Papafragos, C., Tsakanikas, I.,
Zarbala, I., Vasibosis, A., Stamataki, P., &
Sotiropoulos, A. (2010). Self-medication with
antibiotics in rural population in Greece: A cross-
sectional multicenter study. BMC Family Practice.
https://doi.org/10.1186/1471-2296-11-58
Spicer, J. O., Roberts, R. M., & Hicks, L. A. (2020).
Perceptions of the Benefits and Risks of Antibiotics
among Adult Patients and Parents with High Antibiotic
Utilization. Open Forum Infectious Diseases, 7(12), 1–
8. https://doi.org/10.1093/ofid/ofaa544
The Indonesian Ministry of Health. (2013). Basic Research
of Health 2013. Basic Health Research (Riskesdas) .
Van Boeckel, T. P., Brower, C., Gilbert, M., Grenfell, B. T.,
Levin, S. A., Robinson, T. P., Teillant, A., &
Laxminarayan, R. (2015). Global trends in
antimicrobial use in food animals. Proceedings of the
National Academy of Sciences of the United States of
America, 112(18).
https://doi.org/10.1073/pnas.1503141112
Ventola, C. L. (2015). The Antibiotic Resistance Crisi. P &
T, 40(4), 277–283.
https://doi.org/10.5796/electrochemistry.82.749
Voidăzan, S., Moldovan, G., Voidăzan, L., Zazgyva, A., &
Moldovan, H. (2019). Knowledge, attitudes and
Self-Medication of Antibiotic Use: Investigating Knowledge and Attitude Among Rural Population in Umbul Natar Village, South of
Lampung
369

practices regarding the use of antibiotics. Study on the
general population of Mureş County, Romania.
Infection and Drug Resistance, 12.
https://doi.org/10.2147/IDR.S214574
Waaseth, M., Adan, A., Røen, I. L., Eriksen, K., Stanojevic,
T., Halvorsen, K. H., Garcia, B. H., Holst, L., Ulshagen,
K. M., Blix, H. S., Ariansen, H., & Nordeng, H. M. E.
(2019). Knowledge of antibiotics and antibiotic
resistance among Norwegian pharmacy customers - A
cross-sectional study. BMC Public Health, 19(1).
https://doi.org/10.1186/s12889-019-6409-x
WHO. (2014). Antimicrobial Resistance Fact sheet. WHO,
Antimicrobial Resistance.
Zajmi, D., Berisha, M., Begolli, I., Hoxha, R., Mehmeti, R.,
Mulliqi-Osmani, G., Kurti, A., Loku, A., & Raka, L.
(2017). Public knowledge, attitudes and practices
regarding antibiotic use in Kosovo. Pharmacy Practice,
15(1), 1–7.
https://doi.org/10.18549/PharmPract.2017.01.827
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
370
