
Interprofessional Collaboration for Effective Communication in
Integrated Patient Development Records: A Systematic Review
Citra Suraya
1,2,* a
, Tukimin bin Sansuwito
1b
and Aris Citra Wisuda
2c
1
Faculty of Nursing, Lincoln University College, 47301 Petaling Jaya, Selangor Darul Ehsan, Malaysia
2
Program Studi Keperawatan, Sekolah Tinggi Ilmu Kesehatan Bina Husada Palembang, Indonesia
Keywords: Effective Communication, Interprofessional Collaboration, Integrated Patient Development Records.
Abstract: Interprofessional collaboration (IPC) involves integrating health professionals with diverse educational
backgrounds into a cohesive team, with the aim of enhancing the quality of healthcare services. This research
aims to identify the types of professions involved in interprofessional collaboration, delineate the components
of effective communication within interprofessional collaboration, understand the elements of collaboration
in its implementation, and identify inhibiting factors in interprofessional collaboration. The chosen
methodology is a Systematic Review design. The findings indicate that the components of collaboration in
implementing interprofessional collaboration encompass cooperation, partnership, coordination, and
decision-making. Inhibiting factors in interprofessional collaboration include attitudes and behaviors,
instances of laziness, forgetfulness, fatigue, differing opinions, and hastiness, leading to ineffective
documentation of integrated patient development records. Integrated patient development records rely on
collaboration among professionals, including doctors, nurses/midwives, support staff, nutritionists, and
others. It is suggested that leaders motivate their subordinates by providing incentives and sanctions.
1 INTRODUCTION
Integrated Patient Development Records form a
crucial component of the stages involved in assessing
the action process. These records are instrumental in
gathering data to determine the success of the service,
with evaluation being a key aspect of the nursing
process (Hickey & Giardino, 2019). During the
evaluation stage, a comprehensive review is
conducted to assess the patient's response to the
actions administered by the collaborative
interprofessional team. Integrating this stage with the
Development records of patients undergoing regular
treatment facilitates the determination of the
effectiveness of the action plan. This evaluation
enables decisions on whether to continue, revise, or
halt the current plan. When implemented effectively,
this approach enhances optimal communication
within interprofessional collaboration (Smith, 2021;
Houston, 2022).
Within the nursing evaluation process, a crucial
a
https://orcid.org/0000-0002-4445-6443
b
https://orcid.org/0000-0001-7323-4308
c
https://orcid.org/0000-0001-7420-1591
objective is to establish effective communication
between patients and service providers. The ability to
build this communication is a key element influencing
nurses' ease in optimally collecting patient data (Al-
Hussami, 2017). Furthermore, effective
communication in the nursing process serves as an
indicator of patient satisfaction with the provided
services (Harding & Hagler, 2022). Recognizing its
significance, effective communication emerges as a
cornerstone for nurses and other health workers in
ensuring patient safety. Communication that is both
effective and timely, complete, clear, and
comprehensible to the recipient is pivotal in reducing
errors and enhancing overall patient safety (Ministry
of Health Republic Indonesia, 2018).
Interprofessional collaboration (IPC) refers to the
cooperation among health professionals with diverse
educational backgrounds, forming a collaborative
team aimed at enhancing the quality of effective health
services (WHO, 2021). This collaborative framework
encompasses various professionals such as doctors,
286
Suraya, C., Sansuwito, T. B. and Wisuda, A. C.
Interprofessional Collaboration for Effective Communication in Integrated Patient Development Records: A Systematic Review.
DOI: 10.5220/0013671500003873
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Medical Science and Health (ICOMESH 2023), pages 286-298
ISBN: 978-989-758-740-5
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.

dentists, nurses, midwives, nutritionists, pharmacists,
and other health workers, all contributing to the
provision of healthcare services for patients (Ku,
2017).
According to Rao (2019), an unintegrated patient
Development evaluation recording system can lead to
inefficiencies between units and other departments
due to repetitive and separate data recording, starting
from registration, through polyclinics, and
culminating in medical records reporting. Conversely,
an integrated nursing evaluation system streamlines
the process, facilitating corrective clinical decisions
for nurses and interprofessional staff when analyzing
and treating patient conditions. In line with the
Hospital Accreditation Committee in Indonesia
(Ministry of Health the Republic of Indonesia, 2019),
integrated nursing evaluation, as part of the medical
record model, serves as a standard for assessing
hospital quality. In practice, hospitals are encouraged
to evolve patient health records into integrated
medical records, with one crucial component being
the implementation of an integrated patient
Development record form.
The completeness of documents in nursing
evaluation supports effective communication through
qualitative and quantitative analysis, an activity that
assesses both the content's completeness and the
quality's consistency in a medical record. The
thoroughness of medical record documents is crucial
as it directly impacts the treatment process and patient
health services (Einarsen & Giske, 2019). This
assertion aligns with Mayang Sari & Fitriyani (2022)
that implementing patient Development records
serves several objectives, including concluding the
nursing action plan, modifying it, and continuing it.
Evaluation, conducted through various stages and
methods, requires nurses to have a comprehensive
understanding and to execute it appropriately for the
optimal functioning of nursing care. Consequently,
the role of nurses is pivotal in coordinating health
services for patients and fostering positive
relationships among professions in hospitals.
2 METHODS
The methodology employed in this study is a
Systematic Review, involving critical and systematic
thinking through the examination and analysis of
various research articles using logical and
argumentative methods. The PRISMA (Preferred
Reporting Items for Systematic Reviews and Meta-
analyses) method serves as the guiding framework for
this study, assisting in the analysis of the literature
obtained. Articles were evaluated for inclusion using
the Critical Appraisal Skills Program (CASP),
specifically applying Duffy's Research Appraisal
Checklist Approach. The research employed the
PICO framework, defining the Problem (P) as
Effective Communication, Intervention (I) as
Interprofessional Collaboration, Comparison (C) as
not applicable, and Output (O) as the role of
integrated patient Development notes.
For the literature search, databases such as Google
Scholar, ScienceDirect, PubMed, Garuda, and
ProQuest were utilized. The search included
keywords like "Effective communication in
interprofessional collaboration" and "integrated
patient Development records." Inclusion criteria
covered articles related to the role of interprofessional
collaboration in the integrated evaluation of patient
Development records, methods used to complete
patient Development records in interprofessional
collaboration, factors influencing effective
communication, and articles in Indonesian and
English published from 2019 to 2023. Exclusion
criteria comprised reviews of direct verbal
communication between professions, reviews of
interprofessional readiness in collaboration, topics
related to community health centers, doctor-patient
communication, and journals displaying only
abstracts or incomplete text. Study selection and data
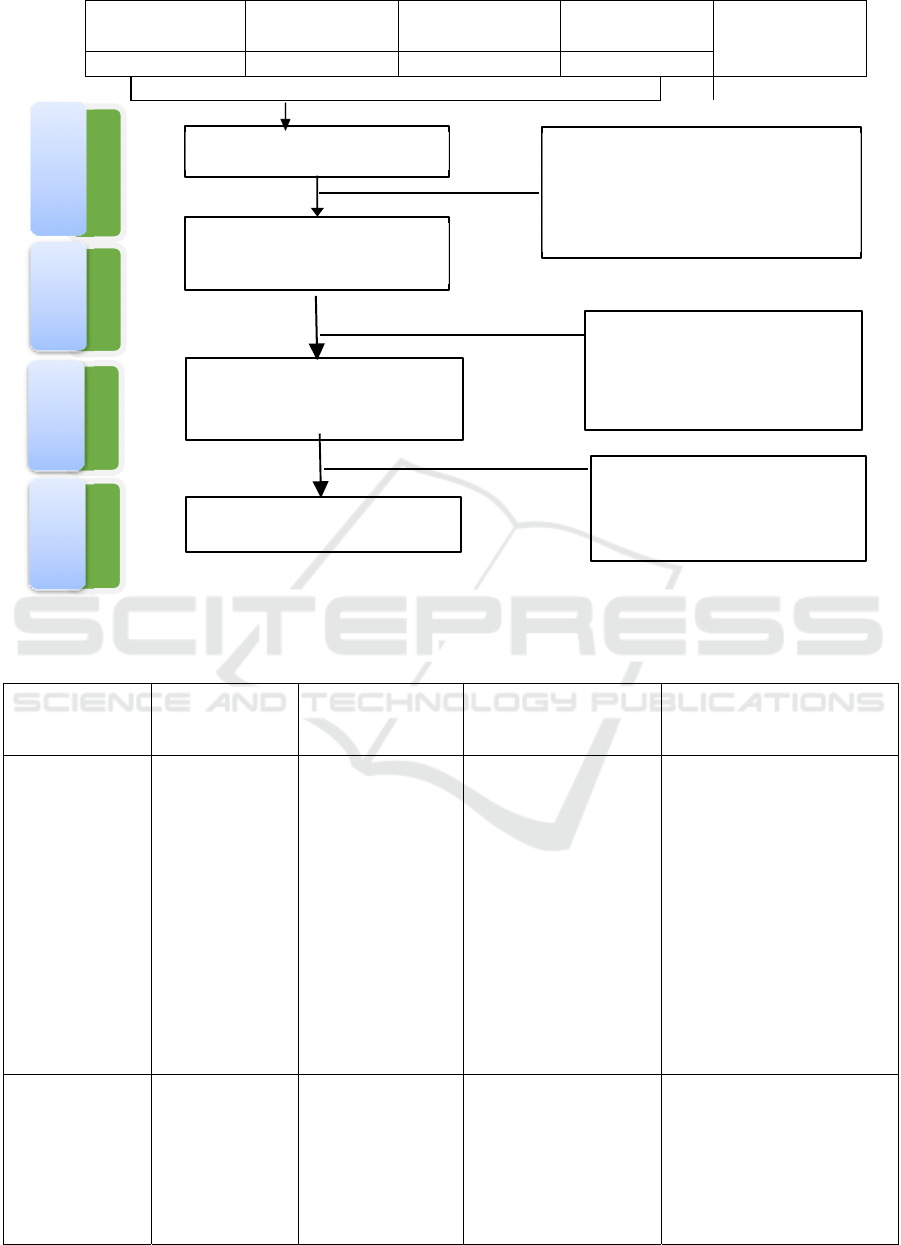
quality are illustrated in Figure 1.
3 RESULTS
Based on the search results from databases such as
Google Scholar, Garuda, Science Direct, and
ProQuest, 685 articles were initially identified.
Applying filtering criteria, including full text
availability and the publication period of 2019-2023,
refined the search and yielded a total of 183 articles
relevant to the research topic. Subsequently, a
duplication check was conducted on the 183
collected articles, resulting in the identification and
exclusion of 147 duplicates. Following an analysis
based on the specified inclusion and exclusion
criteria, 30 articles did not meet the requirements.
Consequently, the remaining six articles will be
presented in the research results and analyzed in the
discussion section, leading to the formulation of
conclusions and suggestions. The results of data
extraction are presented in Table 1.
Interprofessional Collaboration for Effective Communication in Integrated Patient Development Records: A Systematic Review
287
I
d
e
n
Google Scholar Pubmed
Garuda
Proquest
n = 685
297 176 79 133
Figure 1. Flowcharts for the results of data extraction are shown in Figure
Table 1: Data Extraction of Research Articles
Author Name
(Year)
Name Journal
(Vol, No)
Title
Method
(Population / Sample)
Research result
(Kusumaningrum
et al., 2019)
Indonesian
Journal of Nurses
and Midwifery.
The
Implementation of
Integrated Patient
Development Notes
in Interprofessional
Collaboration
Practice
A correlational
descriptive design was
employed for this study.
Samples were randomly
selected, resulting in a
total of 47 nurses.
1.
Types of
professions involved in IPC
include doctors, nurses,
midwives, nutritionists, and
physiotherapists.
2.
There is no
communication component in
IPC.
3.
Collaboration
components in implementing
IPC include cooperation,
partnership, coordination, and
joint decision-making.
4.
There are no
inhibitors in IPC.
(Bakhtiar &
Duma, 2020)
Husada
Mahakam: Jurnal
Kesehatan
Implementation of
Interprofessional
Collaboration in
Health Service
Facilities
A qualitative design
with a
phenomenological
approach was employed,
involving participants
such as medical
specialists, nurses,
pharmacists,
1.
Types of
professions involved in IPC
include specialist doctors,
nurses, pharmacists,
nutritionists, and
physiotherapists.
2.
There is no
communication com
p
onent in
Exclusion
> Last 5 years (n =164)
Not English & Indonesian (n =72)
The title and abstract do not match
the research questions (n =266)
Relating to Author’s topic
(n=183)
Articles identified,
2018
-
2023
screening
Exclusion
147 was exludeddue to
duplication
Eligibility
Identification of journal contents
and selected (n=36)
Exclusion
30 were exluded based on
inclusion and exclusion
criteria
Included
Articles reviewed, n=6
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
288
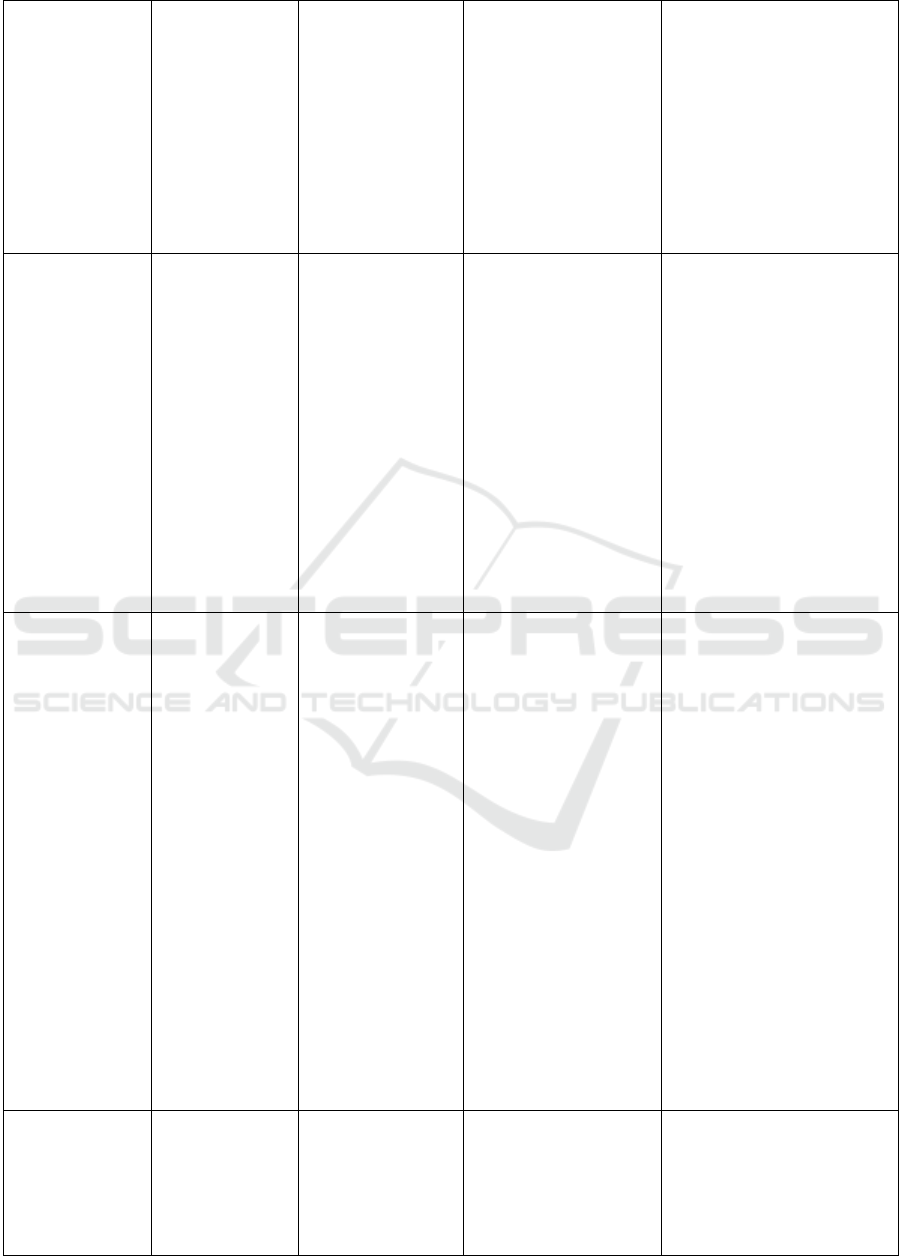
nutritionists, and
physiotherapists.
IPC.
3. Collaboration
components in implementing
IPC include cooperation,
discussion, coordination, and
decision-making.
4. Factors that
hinder health in IPC are
workload, attitude,
interprofessional
coordination, and
communication.
(Fathya et al.,
2021)
Jurnal
Pendidikan
Kedokteran
Indonesia: The
Indonesian
Journal of
Medical
Education
Implementation of
Interprofessional
Collaborative
Practice in Type B
Teaching General
Hospitals.
A mixed-methods
design was employed,
involving participants
such as medical
specialists, nurses,
pharmacists,
nutritionists, and
physiotherapists.
1. Types of professions
involved in IPC are nurses
and specialist doctors.
2. The communication
components in IPC are trust,
support, empathy, and an
open attitude.
3. Collaboration
components in implementing
IPC include control of power,
field of practice, common
interests, and common goals.
4. Factors inhibiting IPC
are doctors, and the nurse will
discuss if the instructions are
not in accordance with the
scope of nursing practice.
(Abd El Rahman
et al., 2021)
Journal of
Multidisciplinary
Healthcare.
Quality of
Interprofessional
Collaboration;
Development notes
in damage
evaluation and its
impact on
Continuity of
patient care
A correlational
descriptive design was
employed for this study.
Samples were randomly
selected, resulting in 47
respondents.
1. Types of professions
involved in IPC include
midwives, nurses,
physiotherapists, dietitians,
general practitioners, dentists,
specialist doctors, and
pharmacists.
2. There is no specific
communication component
mentioned in IPC.
3. Collaboration
components in implementing
IPC include partnerships,
aspects of cooperation and
coordination, and
interprofessional
communication.
4. Barriers to IPC are
inequality, overlapping
authority, the ratio of patients
to health workers, personal
character, communication
barriers, and lack of
institutional support.
Suéli Regina
Sulzbach, Carla
Argenta, Edlamar
Kátia Adamy,
William Campo
Meschial (2022)
Menoufia
Nursing Journal
Faculty of
Nursing
Menoufia
University
Evaluation of
nursing records
through Quality
Diagnosis,
Interventions, and
Outcomes inpatient
Develo
p
ment notes
This is a cross-sectional
study using document
analysis, which is part of
the research macro-
project 'Nursing Process
as Care Technology in
the Health Care
1. There is no specific type
of profession mentioned in
IPC.
2. Communication
components in IPC include
empathy, equality, openness,
Interprofessional Collaboration for Effective Communication in Integrated Patient Development Records: A Systematic Review
289
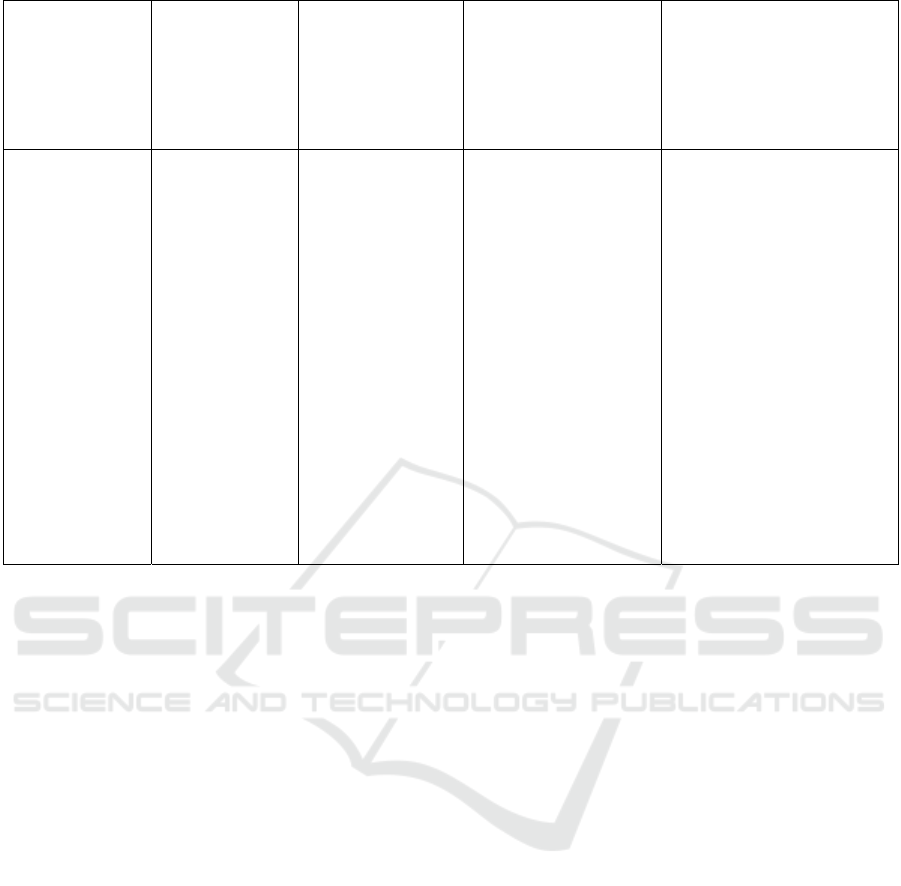
by Interprofessional
Collaboration
Network: Teaching
Interprofessional
Collaboration.' The
sample consisted of 54
respondents.
and support.
3. There is no specific
collaboration component
mentioned in implementing
IPC.
4. There are no specified
inhibitors mentioned in IPC.
(Noviyanti et al.,
2023)
Indonesian
Journal of Health
Information
Management
(IJHIM)
Effective
Communication In
The
Implementation Of
Interprofessional
Collaboration In
The Hospital
This study utilized a
mixed-methods design
involving medical
specialists, nurses,
pharmacists,
nutritionists, and
physiotherapists.
1. The types of
professions involved in IPC
include midwives, nurses,
physiotherapists, dietitians,
general practitioners, dentists,
specialist doctors, and
pharmacists.
2. There is no
specific communication
component mentioned in IPC.
3. The
collaboration component in
implementing IPC involves
partnership and cooperation
towards predetermined goals.
4. The obstacles
to IPC include the ratio of
patients to health workers and
the absence of established
standards.
3.1 Synthesis Results
Based on the results of data extraction, the following
synthesis findings were identified:
a. Understanding the types of professions involved in
interprofessional collaboration in hospitals.
b. Recognizing the components of effective
communication in interprofessional collaboration
in hospitals.
c. Identifying the components of collaboration in
implementing interprofessional collaboration in
hospitals.
d. Understanding the inhibiting factors in
interprofessional collaboration in hospitals.
4 DISCUSSION
4.1 Types of Professions Involved in
Interprofessional Collaboration in
Hospitals
The types of professions involved in IPC are detailed
in several studies, including those by
Kusumaningrum et al. (2019), Bakhtiar & Duma
(2020), Fathya et al. (2021), Suéli Regina Sulzbach,
Carla Argenta, Edlamar Kátia Adamy, William
Campo Meschial (2022), Noviyanti et al. (2023), and
Abd El Rahman et al. (2021). According to
Kusumaningrum et al. (2019), the professions
engaged in IPC include doctors, nurses, midwives,
nutritionists, and physiotherapists. This study
revealed that among the seven respondents, 8.6%
were doctors, 61.7% were nurses, 13.0% were
midwives, 7.4% were nutritionists, and 6.2% were
physiotherapists.
Research conducted by Bakhtiar & Duma (2020)
reveals that the professionals involved in IPC
encompass specialist doctors, nurses, pharmacists,
nutritionists, and physiotherapists. This study
elucidates that the treating doctor plays a crucial role
in determining a medical diagnosis, administering
therapy, making decisions about the patient's
treatment, and deciding when to discharge the patient
from the hospital. In addition, nurses serve as
communicators between health professionals and
facilitate communication between patients and health
professionals. The role of a nutritionist involves
providing nutritional care, offering dietary guidance,
and educating patients about nutrition. Lastly,
physiotherapists specialize in addressing movement
and body function problems.
Research conducted by Fathya et al. (2021)
indicates that the professions involved in IPC are
nurses and specialist doctors. The study reports that
out of 160 respondents, 130 were D3 nurses (81.2%),
19 were S1 nurses (11.9%), and 11 were specialist
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
290

doctors (6.9%). Similarly, in a study by Suéli Regina
Sulzbach, Carla Argenta, Edlamar Kátia Adamy,
William Campo Meschial (2022), the types of
professions engaged in IPC include nurses and
specialist doctors. This study highlights that 82% of
the respondents belonged to the nursing profession,
while 76% were specialist doctors.
Research by Abd El Rahman et al. (2021) reveals
that various professions are involved in IPC,
encompassing midwives, nurses, physiotherapists,
dietitians, general practitioners, dentists, specialist
doctors, and pharmacists. The distribution of
respondents across these professions is as follows: 72
midwives (22.5%), 166 nurses (51.9%), five
physiotherapists (1.6%), six dietitians (1.9%), 15
general practitioners (4.7%), three dentists (0.9%),
33 specialist doctors (10.3%), and 20 pharmacists
(6.3%). Contrastingly, Noviyanti et al. (2023) found
that various professions participate in
interprofessional collaboration, including general
practitioners, specialist doctors, dentists, nurses,
midwives, physiotherapists, dietitians, and
pharmacists.
According to Republic Government Regulation
No. 93 of 2015, a teaching hospital is defined as a
facility that serves as a hub for education, research,
and integrated health services within the realms of
medical and dental education, continuous education,
and various health education initiatives, all
conducted in a multi-professional manner. To
achieve this, the Hospital Accreditation Commission
in MKE (Communication and Education
Management) standard five outlines regulations
pertaining to communication and education
management among health professions. MKE
Standard 5 emphasizes that the communication of
patient care information and outcomes must occur
seamlessly among health professionals working in
shifts. Effective communication between health
professionals is deemed crucial for the smooth
operation of the care process (Ministry of Health the
Republic of Indonesia, 2019).
The World Health Organization (WHO), in both
unspecified past instances and in 2022, has launched
patient safety initiatives with an Interprofessional
Collaboration (IPC) strategy to reduce incidents
causing harm to patients. Both the Institute of
Medicine (IOM) and WHO advocate for health
professionals to collaborate in IPC to enhance health
services (Rørtveit et al., 2020). Ineffective IPC can
negatively impact hospitals, staff, and patients as
service recipients, leading to increased
dissatisfaction and heightened demands from
patients or their families. Adverse incidents arising at
the collaborative practice level are often attributed to
a failure to communicate crucial information among
health workers, particularly doctors and nurses
(Haugen, 2022). The implementation of
interprofessional collaboration in health services
describes a process wherein professionals from
various scientific fields collaborate to provide
holistic and integrated health services, aiming to
achieve healing and well-being for patients (Harding
& Hagler, 2022).
Interprofessionalism is currently a priority in
healthcare (Whelton et al., 2018). Numerous health
professionals endorse interprofessional
collaboration, firmly believing that such
collaboration enhances the quality of care. Over the
past decade, interprofessional health teams have
garnered significant attention, as healthcare delivery
increasingly relies on collaboration, healthcare
provider competency, and knowledge (van den
Heuvel et al., 2022).
In Greece, the importance of Interprofessional
Collaboration (IPC) is outlined in the "Code of
Nursing Deontology" Specifically, Article 12 of the
Code emphasizes that "A nurse must maintain
positive relationships with fellow nurses, doctors,
and other professionals while carrying out their
duties. This involves recognizing and respecting any
differences, always considering the operational
benefits of services." Correspondingly, Section 4 in
Article 21 of the Code of Medical Deontology
highlights that Physicians are expected to promote
respect, nurture positive relationships, and
collaborate with nurses and other personnel in their
practices. This involves acknowledging and
accommodating differences, while prioritizing the
interests of the patient and the efficient operation of
service benefits (Hardy, 2020).
According to the American Nurses Association
(ANA), collaboration is a reciprocal relationship in
which care providers hold the primary responsibility
for patient care within the framework of their
respective fields (Hickey & Giardino, 2019).
Collaborative practice emphasizes shared
responsibility in patient care management, featuring
a mutual decision-making process based on the
education and abilities of each practitioner.
From the perspective of the Department of
Veterans Affairs in the United States, as highlighted
by (Herdman & Heather, 2021), the components of
Interprofessional Collaboration (IPC) encompass
doctors, nurses, pharmacists, psychiatrists, and
technical personnel in health agencies. The
implementation of IPC has been successful in several
countries. The World Health Organization (WHO)
Interprofessional Collaboration for Effective Communication in Integrated Patient Development Records: A Systematic Review
291

noted that, in 2013, five countries excelled in
implementing the IPC concept, namely Canada, the
United States, India, Brazil, and South Africa.
In the 1
st
edition of the National Standards for
Accreditation of Hospitals (SNARS), specifically in
Part II, Patient Focused Service Standards, it is
outlined that one of the competencies of Care Service
Providers (PPA) is interprofessional collaboration.
This competency is divided into four domains:
values/ethics in interprofessional practice,
roles/responsibilities, interprofessional
communication, and teams and teamwork (Santosa &
Ariyani, 2020). The application of Interprofessional
Collaboration (IPC) in health services is considered
a strategic approach to achieve effective and efficient
quality outcomes. In developed countries, IPC has
become an integral part of health services in
hospitals. The Health Profession Accreditors
Collaborative (HPAC) has also published a guide on
implementing IPC (Ministry of Health the Republic
of Indonesia, 2019).
Therefore, based on the information presented in
the four articles mentioned above, it can be
concluded that the types of professions involved in
interprofessional collaboration include general
practitioners, specialist doctors, dentists, nurses,
midwives, nutritionists, physiotherapists, and
dietitians. Among the five articles, there is one that
does not specify any types of professions involved in
interprofessional collaboration.
4.2 Components of Effective
Communication in
Interprofessional Collaboration in
Hospitals
The effective communication component in IPC is
found in the research of Fathya et al. (2021) and Abd
El Rahman et al. (2021). The components of effective
communication in interprofessional collaboration
consist of several, namely:
a. Believe
The research by Fathya et al. (2021) elucidated
that 77.07% of respondents reported the
establishment of trust when engaging in effective
collaboration.
b. Support
The research by Fathya et al. (2021) revealed that
77.73% of respondents obtained support through
effective collaboration. Additionally, the research
conducted by Abd El Rahman et al. (2021)
explained that the majority of respondents,
specifically 39 individuals, rated their
collaboration as good, constituting 53.8% of the
total.
c. Empathy
Research by Fathya et al. (2021) explained that
the highest score was obtained, namely 80.37%,
with the statement, "Doctors and nurses
understand each other's need for humor in
establishing communication within reasonable
limits. Research by Abd El Rahman et al. (2021)
explains that the majority of 39 respondents rated
empathy as good (64.1%).
d. Open attitude
Research by Fathya et al. (2021) revealed that the
highest score, namely 80.37%, was obtained with
the statement, "Doctors and nurses understand
each other's need for humor in establishing
communication within reasonable limits."
Additionally, research conducted by Abd El
Rahman et al. (2021) explained that the majority
of 39 respondents rated empathy as good,
comprising 64.1% of the total.
e. Similarity
Research by Abd El Rahman et al. (2021)
explained that the majority of 39 respondents
rated similarity as good (66.7%).
Communication is a fundamental clinical skill
that must be consistently, competently, and
efficiently practiced to facilitate the establishment of
trust between medical staff and patients (Singh et al.,
2019). Effective collaboration requires proficient
communication not only within health teams but also
in developing doctor-patient relationships. This
fosters information sharing, delivery of treatment,
and overall patient satisfaction (Mohamadirizi et al.,
2021). Consequently, health services can be carried
out safely and effectively. This principle is also
enshrined in Minister of Health Regulation
1691/MENKES/PER/VIII/2011, where effective
communication is identified as one of the goals of
patient safety. Through strong collaboration among
health professionals in health services, patients can
receive holistic treatment, leading to improved
treatment outcomes and increased patient satisfaction
(Ministry of Health Republic Indonesia, 2018).
In the research conducted by Fathya et al. (2021),
the components of effective communication in
Interprofessional Collaboration (IPC) include trust,
support, empathy, and an open attitude. Specifically,
trust was reported by 77.07% of respondents who
collaborated effectively, support was reported by
77.73% of respondents in effective collaboration, and
empathy achieved the highest value at 80.37%,
particularly with the statement "Doctors and nurses
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
292

understand each other's need for humor in
establishing communication within reasonable
limits." However, an open attitude received the
lowest score at 75.54%, particularly with the
statement "Doctors and nurses are able to understand
the patient's psychosocial condition.
Research conducted by Abd El Rahman et al.
(2021) reveals that the components of effective
communication in Interprofessional Collaboration
(IPC) include empathy, equality, openness, and
support. The majority of the 39 respondents assessed
empathy as good (64.1%), equality as good (66.7%),
openness as good (64.1%), and support as good
(53.8%).
This finding aligns with research by
Kusumaningrum et al. (2019), Bakhtiar & Duma
(2020), and Noviyanti et al. (2023), emphasizing the
presence of IPC components in effective
communication. According to Suéli Regina
Sulzbach, Carla Argenta, Edlamar Kátia Adamy,
William Campo Meschial (2022), effective
communication is achieved when the understanding
of the message conveyed by the communicator
matches the understanding of the message by the
communicant. Five general qualities contribute to
effective communication: openness, supportiveness,
a positive attitude, understanding others' feelings,
and equality. Effective communication must also be
based on effective interprofessional relationships
which meet the following requirements:
1) Credibility, in a literal sense, refers to someone
possessing advantages, and it involves the
recipient recognizing the communicator's
competence in the discussed matter. It is
associated with the communicator's attitude or
firm stance, ensuring that the conveyed message
remains unchanged. The conveyed message
typically has a purpose, aiming for positive
change.
2) Context: The conveyed message aligns with the
current needs.
3) Content: The message should be interesting,
engaging, and adaptable to the audience.
4) Clarity: The conveyed message must be clear and
free from multiple interpretations.
5) Continuity and consistency are essential; the
conveyed message should remain consistent and
continuous, adhering to the established topic and
communication objectives.
6) Target capability (the audience's capability),
material, and message delivery techniques are
adjusted to the audience's reception ability to
ensure clarity and avoid confusion.
From the two articles above, it can be concluded
that there are components of effective
communication in interprofessional collaboration,
namely trust, support, empathy, open attitude, and
equality. However, out of the four articles, three
articles did not mention the components of effective
communication in interprofessional collaboration.
4.3 Collaboration Components in
Implementing Interprofessional
Collaboration in Hospitals
The collaboration component in implementing IPC
can be found in the research of Kusumaningrum et al.
(2019), Bakhtiar & Duma (2020), Fathya et al.
(2021), and the research of Abd El Rahman et al.
(2021). The collaboration components in
implementing interprofessional collaboration consist
of several, namely:
a. Cooperation
Collaboration is defined as work carried out
by two or more people working together
across professions to achieve previously
planned and mutually agreed-upon goals. In
hospitals, teamwork has become a necessity
for achieving success in reaching goals (Iula
et al., 2020) Research by Kusumaningrum et
al. (2019) demonstrates a strong correlation
strength with a positive correlation direction,
and research by Bakhtiar & Duma (2020)
indicates that the cooperation aspect has been
well-implemented. Furthermore, research by
Abd El Rahman et al. (2021) reveals that
82.2% of respondents have collaborated
effectively in the cooperation domain.
b. Partnership
A partnership involves collaboration among
various parties, including both government
and private entities, where each participant
serves as partners or colleagues working
together to achieve common goals, fulfill
obligations, and share risks, responsibilities,
resources, capabilities, and profits. Research
by Kusumaningrum et al. (2019) reveals
moderate correlation strength with a positive
correlation direction, while research by Abd
El Rahman et al. (2021) indicates that 67.8%
of respondents had a good correlation.
c. Coordination
Coordination is an activity carried out by
various equal parties to jointly organize or
agree on something and provide information
to each other, ensuring that the process of
carrying out tasks and the success of one party
do not interfere with the other party (Suéli
Interprofessional Collaboration for Effective Communication in Integrated Patient Development Records: A Systematic Review
293

Regina Sulzbach, Carla Argenta, Edlamar
Kátia Adamy, William Campo Meschial,
2022).
Research by Kusumaningrum et al. (2019)
reveals a strong correlation strength with a
positive correlation direction. Additionally,
research by Bakhtiar & Duma (2020) indicates
that the coordination aspect has been
implemented effectively. However, research
by Abd El Rahman et al. (2021) shows that the
coordination domain has the lowest
percentage of good collaboration (66.7%), and
the communication component can influence
this. Therefore, it would be better to improve
communication between health workers in the
team to enhance overall performance.
d. Decision-making
Shared decision-making is the process of
making decisions about patient care actions
based on mutual agreement (Murdiany, 2021).
According to Zamani et al. (2018), the
characteristics of shared decision-making
include: (a) involvement of two or more
participants; (b) collaboration among all parties
to reach an agreement on available treatments;
(c) sharing of information among all
individuals involved; and (d) reaching a
collaborative agreement for the care to be
carried out and implemented by the Care
Service Provider (PPA).
Research by Kusumaningrum et al. (2019)
reveals moderate correlation strength with a
positive correlation direction, and research by
Bakhtiar & Duma (2020) indicates that the
decision-making aspect has been implemented
effectively.
e. Discussion
Bakhtiar & Duma (2020) conducted research
that demonstrates the successful
implementation of the discussion aspect.
f. Power control
Fathya et al. (2021) research explained that the
control aspect of power received a rating of
76.37%.
g. Practice environment
In their research, Fathya et al. (2021) explained
that the lowest score in this aspect was 75.28%,
as indicated by the statement 'Doctors and
nurses discuss their respective areas of practice.
h. Common interest
In their research, Fathya et al. (2021) explained
that the aspect of shared interests received the
highest score, namely 80.59%. This was
indicated by the statement, 'The nurse asked the
doctor for advice on what might be needed to
strengthen the patient's support system.
i. Common goals
In their research, Fathya et al. (2021) explained
that the aspect of shared goals achieved a score
of 76.83%.
j. Interprofessional communication
Fathya et al. (2021) research on the AITCS II
questionnaire indicates that the communication
component is not analyzed separately but is
integrated into the coordination and partnership
components. According to Singh et al. (2019),
workers collaborate by consistently,
sensitively, and professionally communicating,
as well as demonstrating effective interpersonal
skills." Indicators include:
1) Communicate clearly, comprehensively,
and in a culturally appropriate manner both
orally and in writing.
2) Actively listen to and respect client needs
and concerns.
3) Actively listen to the knowledge and
opinions of all team members.
4) Describes effective working relationships
with clients and team members.
5) Use information and communication
systems effectively to improve client
services.
6) Respect the values, beliefs, and culture of
all parties concerned.
Based on the four articles above, it can be
concluded that the components of implementing
interprofessional collaboration include cooperation,
partnership, coordination, joint decision-making,
discussion, control of power, field of practice,
common interests, common goals, and
interprofessional communication.
4.4 Inhibiting Factors in
Interprofessional Collaboration in
Hospitals
Inhibiting factors in IPC are found in the research of
Bakhtiar & Duma (2020), Abd El Rahman et al.
(2021), and the research of Noviyanti et al. (2023).
The inhibiting factors in interprofessional
collaboration consist of several factors, namely:
a. Workload
Bakhtiar & Duma (2020) research indicates that
individuals bear varying workloads, leading to
suboptimal recording on the Integrated Patient
Development Notes due to excessive workload.
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
294

This is because care service providers (PPA) not
only document patient care but also record
additional responsibilities, such as attending to
patient conditions, conducting doctor visits,
performing surgeries, and so on.
b. Attitude and behavior
Bakhtiar & Duma (2020) research indicates that
the attitudes and behavior of care service
providers (PPA) include laziness, fatigue,
differences in perception, forgetfulness, and
haste, resulting in ineffective documentation of
integrated patient Development notes. The
leader or head of the medical records installation
should motivate subordinates by providing
rewards and sanctions to ensure disciplined
documentation of Integrated Patient
Development Notes. Additionally, the
competency and educational backgrounds of
team members vary; individuals with diplomas
have different competencies from those with
other educational backgrounds, posing an
obstacle if training is not conducted. Hospitals,
particularly the Human Resources Department
(HRD), should pay more attention to medical
record officers, ensuring education aligns with
the Regulation of the Minister of Health of the
Republic of Indonesia Number 55 of 2013
concerning the Implementation of Medical
Recorder Work, where the minimum educational
qualification is a Diploma in Medical Records
and Health Information. Hospital management
should conduct regular training or seminars
related to Integrated Patient Development Notes
documentation to enhance the knowledge and
skills of officers.
c. Inequality
Abd El Rahman et al. (2021) research indicates
that inequality is observed in the existence of
professions whose domains are perceived as
merely supportive to other professions.
d. Overlapping Authorities and the Ratio of
Patients to Health Workers
Research by Abd El Rahman et al. (2021) and
Noviyanti et al. (2023) states that overlapping
actions or authority between health professions
is common in the health sector. This
phenomenon is associated with the unbalanced
ratio of patients to health workers.
e. Personal Character.
Research by Abd El Rahman et al. (2021) and
Noviyanti et al. (2023) state that health workers'
lack of awareness regarding the roles of other
professions in the team creates an obstacle to
collaboration.
f. Common interest
Research by Abd El Rahman et al. (2021) and
Noviyanti et al. (2023) states that several
participants emphasized the significance of
hospital institutional support in promoting
interprofessional collaboration, whether
through policies or facility support. The
absence of hospital institutional support in
formulating policies related to interprofessional
collaboration poses a barrier to its
implementation. Institutional support,
manifested through clear governance,
structured protocols, defined authority
boundaries, administrative support, and shared
operational procedures, serves as a driving
force for fostering interprofessional
collaboration in hospitals. Facilities that support
closer access to team members, such as team
interaction rooms and accessible information
technology for all team members to access
medical records, are believed to enhance
interprofessional communication.
g. Doctors and nurses discuss if what is instructed
is not in accordance with the scope of care
practice.
The nurse communicates to the doctor all the
challenges the patient faces in navigating
treatment options and their consequences.
Additionally, the nurse provides the doctor with
insights into specific areas of care. Furthermore,
nurses emphasize the importance of medical care
when discussing treatment options with patients.
Meanwhile, no inhibiting factors in IPC were
identified in the research conducted by
Kusumaningrum et al. (2019) and Suéli Regina
Sulzbach, Carla Argenta, Edlamar Kátia Adamy,
William Campo Meschial (2022), According to the
Joint Commission on Accreditation of Healthcare
Organizations, medical errors rank fifth among the top
ten causes of death in the United States. The root of
this problem is poor collaboration between health
workers, leading to treatment delays and fatal errors in
operations (Kamil et al., 2020). Additionally,
according to the Australian National Prescribing
Service, 6% of hospital cases result from drug side
effects and treatment errors, both of which arise due
to poor collaboration among health professionals
(Hickey & Giardino, 2019).
Urquhart et al. (2018) explained that 70-80% of
errors in health services result from poor
communication and a lack of understanding among
team members. Effective team collaboration is crucial
Interprofessional Collaboration for Effective Communication in Integrated Patient Development Records: A Systematic Review
295

for reducing patient safety issues. In several large
hospitals in Indonesia, evidence of equal team
collaboration is lacking, and partnerships remain
largely a government discourse. Only 15% of
respondents consider the quality of patient safety,
based on service and communication among health
workers, to be good, as revealed in research conducted
in 40 hospitals across Indonesia. This is evident in the
high number of medication errors in places like
Yogyakarta and Bali, where 1563 cases were reported
in 20 weeks (Craven, 2016). The significant errors in
prescription writing (98.69%) in Indonesia contribute
to pharmacist errors in preparing and providing
information about the medication. From 2015 to 2016,
317 cases of suspected malpractice were reported to
the Indonesian Medical Council (KKI) (Fukada,
2018).
Collaboration between health professionals in
Indonesia is still far from ideal, with overlapping roles
between health professions persisting. One of the
causes of this issue could be a lack of understanding
among health professionals regarding each other's
competence or insufficient communication among
health workers in teamwork and collaboration (Rao,
2019). Improving interprofessional collaboration is
essential to enhance satisfaction among health service
users.
So, it can be concluded from the three articles
above that inhibiting factors in interprofessional
collaboration include workload, attitudes and
behavior, inequality, overlapping authority, the ratio
of patients to health workers, personal character,
communication barriers, and lack of institutional
support. It is noted that doctors and nurses discuss
only when instructed and not within the scope of
nursing practice. Among the five articles, two do not
mention inhibiting factors in interprofessional
collaboration.
5 CONCLUSIONS
1. The types of professions involved in
interprofessional collaboration in hospitals
include general practitioners, specialist doctors,
dentists, nurses, midwives, nutritionists,
physiotherapists, pharmacists, and dietitians.
2. The components of effective communication in
interprofessional collaboration in hospitals
encompass trust, support, empathy, an open
attitude, and equality.
3. Collaboration components in implementing
interprofessional collaboration in hospitals
comprise cooperation, partnership, coordination,
joint decision-making, discussion, control of
power, field of practice, common interests,
common goals, and interprofessional
communication.
4. Inhibiting factors in interprofessional
collaboration in hospitals are workload, attitudes,
and behavior; discussions between doctors and
nurses may occur if instructions are not within the
scope of nursing practice; inequality; overlapping
authority; the ratio of patients to health workers;
personal character; communication obstacles,
and lack of institutional support.
Based on the conclusions above, the suggestions
given are:
1. Communication between health workers in the
team should be improved to enhance overall
performance.
2. The hospital, particularly the Human Resources
Department (HRD), should pay more attention to
the education of medical records officers, with a
focus on achieving a minimum educational
qualification of a Diploma in Medical Records
and Health Information.
3. The leader/head of the medical records
installation should motivate subordinates by
providing rewards and sanctions to ensure
disciplined documentation of Integrated Patient
Development Notes.
4. Hospital management should organize regular
training seminars focused on Integrated Patient
Development Notes documentation to enhance
the knowledge and skills of officers.
ACKNOWLEDGMENTS
The researcher would like to express his gratitude to
the Honourable :
1. Dr. Tukimin bin Sansuwito, as a supervisor who
has provided guidance and advice to make this
research dissertation proposal perfect.
2. Dr. Duke, as a supervisor who has provided
guidance and advice to make this research
dissertation proposal perfect.
REFERENCES
Abd El Rahman, A., Ibrahim, M., & Diab, G. (2021).
Quality of Nursing Documentation; progress notes in
damage evaluation and its impact on Continuity of
patient care. Menoufia Nursing Journal, 6(2), 1–18.
https://doi.org/10.21608/menj.2021.206094
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
296

Al-Hussami, M. (2017). Patients’ perception of the quality
of nursing care and related hospital services. 1(2), 1–6.
https://doi.org/10.15761/HPC.1000110
Bakhtiar, R., & Duma, K. (2020). Implementation of
Interprofessional Collaboration in Health Service
Facilities. Husada Mahakam: Jurnal Kesehatan, 10(2),
41–53.
Craven, R. F. (2016). Fundamentals of Nursing: Human
Health and Function. LWW.
Einarsen, K. A., & Giske, T. (2019). Nursing Students’
Longitudinal Learning Outcomes After Participation in
a Research Project in a Hospital. International Practice
Development Journal, 9(1), 1–10.
https://doi.org/10.19043/ipdj.91.004
Fathya, N. A., Effendy, C., & Prabandari, Y. S. (2021).
Implementation of Interprofessional Collaborative
Practice in Type B Teaching General Hospitals: a
Mixed Methods Study. Jurnal Pendidikan Kedokteran
Indonesia: The Indonesian Journal of Medical
Education, 10(2), 162.
https://doi.org/10.22146/jpki.60093
Fukada, M. (2018). Nursing competency: Definition,
structure and development. Yonaga Acta Medica, 61, 1–
7. https://doi.org/10.33160/yam.2018.03.001
Harding, M., & Hagler, D. (2022). Conceptual Nursing
Care Planning (L. Newton (Ed.)). Book Aid
International.
Hardy, L. R. (Ed.). (2020). 045 EB - 2020 - Fast Facts in
Health Informatics for Nurses. New York: Springer
Publishing Company.
Haugen, N. (2022). Nursing Care Planning; Prioritization,
DElegation, and Clinical Reasoning. Revised Reprint
With 2021-2023 NANDA-I (S. J. Galura (Ed.); 8th ed.).
Herdman, & Heather, T. (2021). NANDA International
Nursing Diagnoses Definitions & Classification
(Kamitsuru (Ed.); Twelfth). Thieme Medical
Publishers, Inc. https://doi.org/10.1055/b000000515
Hickey, J. V., & Giardino, E. R. (2019). The Role of the
Nurse in Quality Improvement and Patient Safety. The
Journal of Neurological and Neurosurgical Nursing,
8(1), 30–36. https://doi.org/10.15225/pnn.2019.8.1.5
Houston, M. C. (2022). The Truth About Heart Disease
(Charless & S. Handerson (Eds.); First). CRD Press
(Taylor & Francis Group).
I, C. A., Zanatta, E. A., & Abido, S. C. (2022). Evaluation
of nursing records through Quality Diagnosis,
Interventions and Outcomes in patient progress notes.
1–19.
Iula, A., Ialungo, C., de Waure, C., Raponi, M., Burgazzoli,
M., Zega, M., Galletti, C., & Damiani, G. (2020).
Quality of care: Ecological study for the evaluation of
completeness and accuracy in nursing assessment.
International Journal of Environmental Research and
Public Health, 17(9), 1–9.
https://doi.org/10.3390/ijerph17093259
Kamil, H., Rachmah, R., Wardani, E., & Björvell, C.
(2020). How to optimize integrated patient progress
notes: A multidisciplinary focus group study in
Indonesia. Journal of Multidisciplinary Healthcare, 13,
1–8. https://doi.org/10.2147/JMDH.S229907
Ku, Y. (2017). Spiritual Care in Nursing Concept Analysis
of Interesting Patient. 1–4.
https://doi.org/10.21767/2574-2825.1000005
Kusumaningrum, P. R., Dharmana, E., & Sulisno, M.
(2019). The Implementation of Integrated Patient
Progress Notes in Interprofessional Collaborative
Practice. Jurnal Ners Dan Kebidanan Indonesia, 6(1),
32. https://doi.org/10.21927/jnki.2018.6(1).32-41
Mayang Sari, N., & Fitriyani, N. (2022). Nursing Care of
Type II Diabetes Mellitus Patients in Fulfilling
Nutritional Needs. Jurnal Kesehatan Universitas
Kusuma Husada Surakarta, 56, 1–9.
Ministry Of Health Republic Indonesia. (2018). Main
Results of Basic Health Research. Kementrian
Kesehatan RI.
Ministry of Health the Republic of Indonesia. (2019).
Regulation of The Minister of Health of The Republic of
Indonesia Number 26 Year 2019 About Implementing
Regulation of Law Number 38 Year 2014 Concerning
Nursing. Jakarta: Minister of Health of the Republic of
Indonesia.
Mohamadirizi, S., Yazdannik, A., Mohamadi, M., & Omid,
A. (2021). The Effectiveness of Two Evaluation
Techniques in The Clinical Education Field: A Step for
Promotion of Bachelor Nursing Student’s Satisfaction.
Journal of Education and Health Promotion, 10(108),
1–6. https://doi.org/10.4103/jehp.jehp_504_20
Murdiany, N. A. (2021). Interprofessional Communication
Relationships with Nurse-Doctor Collaboration at Irna
Rsud H. Damanhuri Barabai. Journal of Nursing
Invention E-ISSN 2828-481X, 2(1), 41–48.
https://doi.org/10.33859/jni.v2i1.117
Noviyanti, A., Lita Sari, N., Lestari, T., Mitra Husada
Karanganyar Brigjen Katamso Barat, Stik. J., Papahan
Indah, G., Tasikmadu, K., Karanganyar, K., & Tengah,
J. (2023). Literature Review: Effective Communication
in The Implementation of Interprofessional
Collaboration In The Hospital. Indonesian Journal of
Health Information Management (IJHIM), 3(1), 1.
Rao, B. J. (2019). Innovative Teaching Pedagogy in
Nursing Education. International Journal of Nursing
Education, 11(4), 176–180.
https://doi.org/10.5958/0974-9357.2019.00114.4
Rørtveit, K., Saetre Hansen, B., Joa, I., Lode, K., &
Severinsson, E. (2020). Qualitative evaluation in
nursing interventions—A review of the literature.
Nursing Open, 7(5), 1285–1298.
https://doi.org/10.1002/nop2.519
Santosa, & Ariyani, S. P. (2020). Descriptive Analysis of
the Application of Effective Communication Using the
SBAR (Situation Background Assessment
Recommendation) Technique for Patient Safety in
Hospital Practitioners in Pati District. Syntax Idea,
2(5),
132–141. https://doi.org/10.36418/syntax-
idea.v2i5.276
Singh, S., Gupta, A. K., & Chanana, L. (2019). Service
Quality Parameters for Social Media-Based
Goverment-to-Citizen Service. In S. C. Satapathy & A.
Joshi (Eds.), Information and Communication
Technology for Intelligent Systems (Vol. 1, pp. 193–
Interprofessional Collaboration for Effective Communication in Integrated Patient Development Records: A Systematic Review
297

206). Singapore: Springer Nature Singapore Pte Ltd.
https://doi.org/10.1007/978-981-13-1742-2_20
Smith, Y. (2021). Roles of a Nurse. News Medical Life
Sciences.
Urquhart, C., Currell, R., Grant, M. J., & Hardiker, N. R.
(2018). Nursing record systems: Effects on nursing
practice and healthcare outcomes. Cochrane Database
of Systematic Reviews, 2018(5).
https://doi.org/10.1002/14651858.CD002099.pub3
van den Heuvel, L. M., Sarina, T., Sweeting, J., Yeates, L.,
Bates, K., Spinks, C., O’Donnell, C., Sears, S. F.,
McGeechan, K., Semsarian, C., & Ingles, J. (2022). A
Prospective Longitudinal Study of Health-Related
Quality of Life and Psychological Wellbeing After an
Implantable Cardioverter in Patients with Genetic Heart
Diseases. Heart Rhythm O2, 3(2), 143–151.
https://doi.org/10.1016/j.hroo.2022.02.003
Whelton, P. K., Carey, R. M., Aronow, W. S., Casey, D. E.,
Collins, K. J., Himmelfarb, C. D., DePalma, S. M.,
Gidding, S., Jamerson, K. A., Jones, D. W.,
MacLaughlin, E. J., Muntner, P., Ovbiagele, B., Smith,
S. C., Spencer, C. C., Stafford, R. S., Taler, S. J.,
Thomas, R. J., Williams, K. A., … Hundley, J. (2018).
2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/
ASH/ASPC/NMA/PCNA Guideline for the Prevention,
Detection, Evaluation, and Management of High Blood
Pressure in Adults. Hypertension, 71(6), E13–E115.
https://doi.org/10.1161/HYP.0000000000000065
WHO. (2021). World Health Statistics; Monitoring Health
for The SDGs (Sustainable Development Goals).
https://apps.who.int/iris/bitstream/handle/10665/34270
3/9789240027053-eng.pdf
Zamani, S. N., Zarei, E., Haji Alizadeh, K., & Naami, A. Z.
(2018). Effectiveness of Combination of Cognitive-
Behavioral Therapy and Resilience Training Based on
Islamic Spirituality and Cognitive Flexibility on
Postpartum Depression, Fear of Labor Pain and Quality
of Life. Hormozgan Medical Journal, 22(4), e86489.
https://doi.org/10.5812/hmj.86489
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
298
