
Analysis of Sequential Organ Failure Assessment (SOFA) Score
Profile in Relation to Length of Stay and Patient Outcome in the ICU
of Abdul Moeloek Regional General Hospital
Ari Wahyuni
1,*
, Liana Sidharti
1
and Desy Kusumaningrum
2
1
Department of Anesthesiology and Intensive Care, Faculty of Medicine, University of Lampung,
Bandar Lampung, Indonesia
2
Faculty of Medicine,University of Lampung, Bandar Lampung, Indonesia
Keywords: ICU, Length of Stay, Mortality, Sepsis, SOFA Score.
Abstract: Sepsis is a severe dysfunction of the body's organs triggered by the immune system's imbalance in reaction to
an infection. The Sequential Organ Failure Assessment (SOFA) score is utilized to evaluate the organ failure
linked to sepsis. An increase in the SOFA score is associated with worse patient outcomes or higher mortality
rates. This study seeks to analyze the correlation between SOFA scores, length of stay, and mortality in sepsis
patients. The study subjects are sepsis patients treated in the Intensive Care Unit (ICU) of Dr. H. Abdul
Moeloek Regional General Hospital. The research was conducted from May to October 2023. This study is a
prospective cohort analytical observational research conducted at Dr. H. Abdul Moeloek Regional General
Hospital and the University of Lampung between May and October 2023. A total of 137 patients were
involved during a span of three months, with 89 patients chosen as subjects for this study, while 48 patients
were excluded because of incomplete data. The Spearman Correlation normality test displayed a correlation
between the SOFA score and Length of Stay with a significance value of 0.367. Since this value is >0.05, H0
is accepted, and H1 is rejected. The Spearman Correlation normality test indicated a correlation between the
SOFA score and the patients' final condition with a significance value of 0.000. As this value is <0.05, H0 is
rejected, and H1 is accepted. The correlation coefficient of 0.097 indicates a very weak level of association
between the SOFA score and Length of Stay, suggesting no significant correlation between the two variables.
However, a correlation coefficient of 0.592 denotes a moderately robust level of association between the
SOFA score and the Patients' Final Condition, highlighting a correlation between the two variables.
1 INTRODUCTION
Sepsis is a health issue prevalent in society
characterized by a severe clinical infection syndrome
marked by cardinal inflammatory signs such as
leukocyte accumulation, vasodilation, and increased
microvascular permeability occurring in tissues far
from the source of infection (Darwis & Probosuseno,
2019).
According to the WHO (2017), there were 48.9
million reported cases with 11 million deaths
associated with sepsis, contributing for 20% of all
deaths worldwide. Each year, sepsis causes 6 million
deaths and has been designated as a global health
priority by the WHO. Sepsis cases rank among the top
ten causes of death in the United States (Marik &
Taeb, 2011).
A study conducted in 2009 across 16 Asian
countries, including Indonesia, stated that the
incidence of severe sepsis and septic shock in ICU
wards was 10.9%, with a corresponding mortality rate
of 44 percent. Another study at RSCM Jakarta in
2012, spanning one month, it was found that among
84 intensive care cases, there were 23 instances of
severe sepsis and septic shock, resulting in a mortality
rate of 47.8 percent (Kemenkes, 2017).
Based on data retrieved from patient medical
records at RSUP Dr. Sardjito Yogyakarta in 2016, the
incidence of sepsis in internal disease inpatient wards
amounted to 704 cases (17.06%) out of the total
number of treated patients, with 431 (61.22%) deaths
among diagnosed sepsis patients. In 2017, there was
a decrease in sepsis incidence to 454 cases (9.71%)
out of the total number of treated patients, with 278
Wahyuni, A., Sidharti, L. and Kusumaningrum, D.
Analysis of Sequential Organ Failure Assessment (SOFA) Score Profile in Relation to Length of Stay and Patient Outcome in the ICU of Abdul Moeloek Regional General Hospital.
DOI: 10.5220/0013668100003873
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Medical Science and Health (ICOMESH 2023), pages 203-207
ISBN: 978-989-758-740-5
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
203

(61.23%) deaths among diagnosed sepsis patients
(Darwis & Probosuseno, 2019).
Assessment systems for organ damage and failure
can be monitored using ICU illness scores such as
APACHE II, SAPS II, and the SOFA score to assess
the severity of the disease (Dirgantoro, 2018). The
APACHE II scoring system itself has several
limitations due to selection bias, lead time bias, and
the difficulty in determining the primary diagnosis
leading patients into the ICU, requiring a higher cost
due to multiple laboratory variables tested and a
lengther time to obtain results. Whereas the SAPS II
system, although the first system to use statistical
modeling techniques, is difficult to establish
considering data must be collected within one hour
after the patient enters the ICU (Sugiman, 2011).
In sepsis, organ dysfunction can be recognized by
a sudden increase of at least 2 points in the overall
SOFA score because of an infection. Each organ has
a value ranging from 0 (normal function) to 4 (very
abnormal), resulting in a maximum total score of 24
(Seymour et al., 2016). The researchers chose the
SOFA score because it's not a one-time assessment; it
can be evaluated periodically, observing score
increases or decreases. The SOFA score isn't just
calculated upon patient admission but also every 24
hours. Parameters in the SOFA score are deemed
ideal for depicting organ dysfunction (Singer et al.,
2016). Moreover, the SOFA score attributes values to
individual organ systems depending on one or
multiple variables, fewer than other ICU severity
assessment systems like APACHE II and SAPS II
(Dirgantoro, 2018).
Identifying sepsis before significant organ failure
occurs poses a challenge to all medical professionals.
For primary care doctors, detecting potentially septic
patients among many individuals presenting with
uncomplicated infections, as well as those not
progressing to sepsis, requires specific skills (Tavare
& Oflyn, 2017). The lack of diagnostic tools is a
major obstacle in the early management of sepsis.
This is compounded by the fact that sepsis presents as
a heterogeneous set of symptoms without a gold
standard for diagnosis (Mclymont & Glover, 2016).
2 METHODS
2.1 Research Design
This research is an analytical observational research
using a prospective cohort study approach. It was
carried out at RSUD Dr. H. Abdul Moeloek and
University of Lampung from Mei to October 2023.
2.2 Sample Research
The subjects of this study were individuals admitted
to the ICU at Dr. H. Abdul Moeloek Regional General
Hospital who met the study criteria. Inclusion criteria
for this research were patients aged ≥18 years
diagnosed with either sepsis or septic shock.
Exclusion criteria included patients discharged
without the approval of the attending physician or
upon their own request, and patients with a SOFA
score <2 assessed based on serum creatinine
concentration, platelet count, and Glasgow Coma
Scale (GCS) within 24 hours following the diagnosis
of sepsis. A total of 137 patients were identified over
three months, with 89 patients included as subjects in
this study, while 48 patients were excluded due to
incomplete patient data.
2.3 Data Analysis Research
In this research, the data was performed on the data
using SPSS version 22.0. Spearman's test was utilized
for numerical data to evaluate the distribution of the
data. Descriptive data were reported as the mean and
standard deviation (SD) for normally distributed data
or as the median and interquartile range for data that
did not follow a normal distribution. Bivariate
analysis was conducted to compare variable
differences between subjects who experienced
improvement and those who deceased.
3 RESULTS
The SOFA score is one of the scoring systems
commonly used to depict organ failure or
dysfunction, typically measured in patients
undergoing treatment in the intensive care unit. The
influence distribution factor are presented in the table
1.
Table 1: Distribution Frequency of Patients Age.
Data Criteria Patients Age
N 89
Minimun 18
Maximu
m
94
Mean 56.49
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
204
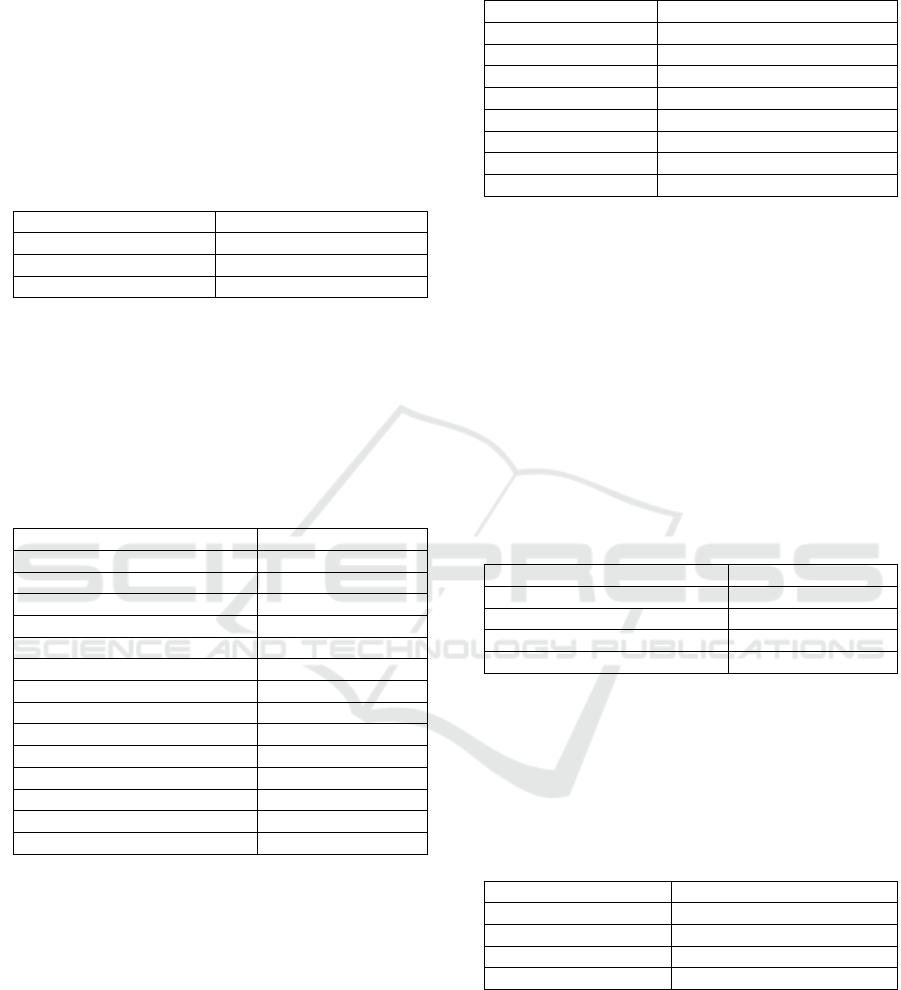
Based on the research data provided, it's evident
that the ICU at Dr. H. Abdul Moeloek Regional
General Hospital had a total of 89 patients as research
subjects. The patients' ages displayed a considerable
range, spanning from a minimum of 18 years to a
maximum of 94 years. The average age of patients
treated in the ICU is approximately 56.49 years.
These results depict the diversity of ages among
patients requiring intensive care in this hospital.
Table 2: Distribution Frequency of Patients Gender.
Data Criteria Patients Gende
r
Men 42
Women 47
Total 89
Based on the research data provided, it is
observed that in the ICU of Dr. H. Abdul Moeloek
Regional General Hospital, out of a total of 89
research subjects, there were 42 male patients and 47
female patients. These results depict an insignificant
difference between the number of male and female
patients.
Table 3: Distribution Frequency of Primer Diagnoses.
Data Criteria Primer Diagnoses
Neurological Disorders 19
Cardiovascular System 15
Res
p
iration S
y
ste
m
1
Gastrointestinal S
y
stem 2
Endocrine Disorders 4
Infection 1
Postoperative Management 25
Liver Disorders 3
Kidne
y
Disorders 6
Mali
g
nanc
y
8
Sensory Syte
m
2
Hematological Disorders 2
Reproduction Syste
m
1
Total 89
Based on the distribution of primary diagnoses,
it was found that out of the total 89 research subjects,
the three most common primary diagnoses were
patients undergoing postoperative care, neurological
system disorders, followed by cardiovascular system
issues. Patients undergoing postoperative care
included those after a laparotomy. The most prevalent
neurological diseases were patients with brain
hemorrhage and stroke. As for cardiovascular
diseases, the most frequently encountered were
patients with heart failure and coronary artery
disease.
Table 4: Distribution Frequency of Number of
Comorbidities.
Data Criteria Number of Comorbidities
0 17
1 21
2 18
37
4 18
54
64
Total 89
Based on the distribution of data on the number
of patient comorbidities, it was found that the
majority of patients undergoing treatment in the ICU
at Dr. H. Abdul Moeloek Regional General Hospital
had comorbidities, varying from a minimum of 1 to a
maximum of 6 comorbidities. Patients without
comorbidities amounted to 17 individuals. The
presence of comorbidities in patients, whether
acquired before or during their treatment, becomes a
factor that worsens the patient's condition and poses a
higher risk of mortality. The most commonly found
comorbidities were electrolyte imbalance and
infections.
Table 5: Distribution Frequency of SOFA Score.
Data Criteria SOFA Score
N 89
Minimu
m
3
Maximu
m
14
Mean 7.44
Based on table 5, the Sequential Organ Failure
Assessment (SOFA) Score among patients varied
between a minimum score of 3 and a maximum score
of 14. The mean SOFA score was around 7.44. A
higher SOFA score indicates a greater severity of
organ dysfunction experienced by the patient.
Table 6: Distribution Frequency of Length Hospitalization.
Data Criteria Len
g
th Hos
p
italization
N 89
Minimu
m
0
Maximu
m
25
Mean 5.61
According to table 6, the length of stay varied
between 0 days as the minimum and 25 days as the
maximum. The average length of stay in this ICU was
approximately 5.61 days. The varied length of stay
from 0 to 25 days reflects the diversity in patient
conditions, with some patients possibly requiring
shorter treatment durations while others may need
lengther care.
Analysis of Sequential Organ Failure Assessment (SOFA) Score Profile in Relation to Length of Stay and Patient Outcome in the ICU of
Abdul Moeloek Regional General Hospital
205
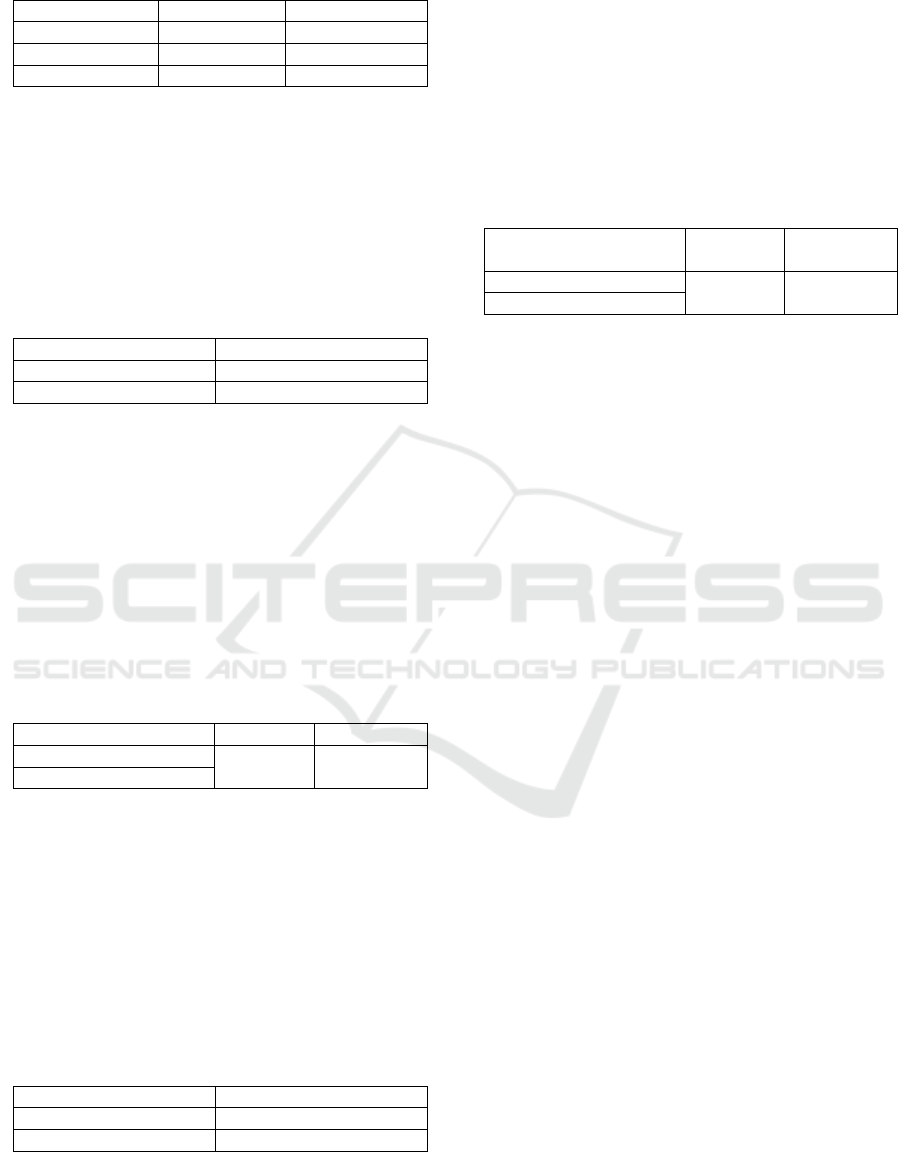
Table 7: Distribution Frequency of Final Condition.
Final Condition Fre
q
uenc
y
Percenta
g
e
(
%
)
Life 12 13.5
Dea
d
77 86.5
Total 89 100
Based on the above table 4, out of the total 89
patients who were subjects of the study,
approximately 13.5% of them successfully recovered
and survived after undergoing treatment in the ICU.
The most notable data is that around 86.5% of
patients experienced death during or after ICU
treatment.
Table 8: SOFA Score Normality Test Results with Length
of Hospitalization.
Variable P-Value
SOFA 0.008
Len
g
th Hos
p
italization 0.000
Based on the normality test using Kolmogorov-
Smirnov in the table above, it is known that the
probability values (p-values) or Asymp. Sig. (2-
tailed) for the variables SOFA Score and Length of
Stay are 0.008 and 0.000, respectively. As the
probability values are smaller than the significance
level of 0.05, it indicates that the normality
assumption is not met. Therefore, the correlation test
between SOFA Score and Length of Stay will be
conducted using Spearman Correlation.
Table 9: Correlation Test Results of SOFA Score with
Length of Hospitalization.
Variable Person (r) P-Value
SOFA
0.097
0.367
Length Hospitalization
From the table 9, it is revealed that concerning the
relationship between the SOFA Score and Length of
Stay yielded a significance value of 0.367. Since this
value is >0.05, H0 is accepted, and H1 is rejected,
indicating no relationship between the SOFA Score
and Length of Stay. With a correlation coefficient of
0.097, it signifies a very low level of association
(correlation) between the SOFA Score and Length of
Stay.
Table 10: SOFA Score Normality Test Results with
Patient’s Final Condition.
Variable P-Value
SOFA 0.008
Final Condition 0.000
Based on the normality test using Kolmogorov-
Smirnov in the table above, it is noted that the
probability values (p-values) or Asymp. Sig. (2-
tailed) for the variables SOFA Score and Patient
Outcome are 0.008 and 0.000, respectively. As the
probability values are smaller than the significance
level of 0.05, it indicates that the normality
assumption is not met. Therefore, the correlation test
between the SOFA Score and Patient Outcome will
be conducted using Spearman Correlation.
Table 11: Correlation Test Results of SOFA Score with
Patient’s Final Condition.
Variable Pearson
(r)
P-Value
SOFA
0.592
0.000
Kondisi Akhir Pasien
From the table 11, it's clear that in relation to the
connection between the SOFA Score and the patient's
outcome, a significance value of 0.000 was obtained.
As this value is <0.05, H0 is declined, and H1 is
acknowledged, signifying an association between the
SOFA Score and the Patient's Outcome. With a
correlation coefficient of 0.592, it signifies a
moderately strong level of association (correlation)
between the SOFA Score and the Patient's Outcome.
As the correlation coefficient is positive, it indicates
a direct relationship between the two variables.
Therefore, it can be concluded that as the SOFA
Score increases, the patient's outcome deteriorates.
4 DISCUSSION
The SOFA score is a reliable scoring method utilized
to illustrate organ failure or dysfunction, typically
measured in patients undergoing intensive care unit
(ICU) treatment. However, based on the findings of
this research, there was no correlation found between
the SOFA score and the duration of stay. The
correlation test revealed a weak correlation between
these two variables. Factors influencing ICU patient
length of stay include age, primary diagnosis, and the
patient's initial condition upon admission. In this
study, the subjects encompassed all patients receiving
ICU care, resulting in diverse patient ages and
primary diagnoses, hence no significant relationships
were found due to the variability in patient
backgrounds. This highlights the need for more
specific research in subsequent studies.
The SOFA score serves as an indication of the
quantity and severity of organ dysfunction in ICU
patients. A higher SOFA score indicates increased
organ dysfunction severity, elevating the risk of
mortality (Sari et al., 2021). SOFA score
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
206

measurements indicated that the majority of patients
with a fatal outcome experienced multi-organ
dysfunction, notably in the respiratory system, as
observed from PaO2/FiO2 data. Patients
experiencing respiratory distress exhibited decreased
lung compliance and hypoxemia, leading to
inadequate oxygen reaching body tissues.
Another indicator of multi-organ dysfunction seen
in SOFA score measurements is the neurological
system through a decrease in the Glasgow Coma
Scale (GCS), signifying reduced patient
consciousness levels. This serves as an indication of
potential brain injury worsening due to infection,
masses, or other inflammatory processes. The
cardiovascular system is also assessable via the
SOFA score, with Mean Arterial Pressure (MAP) as
an indicator. The initial MAP target for patients
receiving vasopressor therapy is 65 mmHg to achieve
optimal tissue perfusion. Prolengthed hypotension is
associated with increased patient mortality risk.
Serum creatinine levels serve as an indicator for
monitoring kidney function and are included in SOFA
score evaluations. Patients with acute kidney injury
exhibit increased serum creatinine levels, indicating
weakened filtration and elimination over several
hours to days. Elevated serum creatinine levels
correlate with worse patient outcomes.
The research findings indicate a connection
between the SOFA score and the final condition of
ICU patients. Correlation tests showed that higher
SOFA scores correspond to an increased risk of the
patient's final condition worsening. This aligns with
previous studies where a SOFA score ≥7 had a
mortality rate of 72.6% (Sari et al., 2021). Iskandar
and Siska (2020) mentioned that individuals having a
SOFA score of ≥7 faced a mortality risk 2.8 times
higher than those with a SOFA score of <7. Other
studies, such as Bale et al. (2013), also highlighted the
use of the SOFA score as a predictor of the patient's
final condition.
5 CONCLUSION
The SOFA score does not have a significant
relationship with the length of stay of patients
undergoing intensive care treatment in the ICU at
RSUD Dr. H. Abdul Moeloek. However, the SOFA
score does have a significant relationship with patient
mortality, thus serving as a reasonably good predictor
in predicting the patient's final condition.
REFERENCES
Ascharya, S., Pradhan, B., and Marhatta, M., 2007.
Application of the Sequential Organ Failure
Assessment (SOFA) Score in Predicting Outcome in
ICU Patients with SIRS. Kathmandu University
Medical Journal. Vol.5, No.4, pp.475-483.
Darwis I amd Probosuseno., 2019. Hubungan Neutorphyl
Lymphocyte dengan Outcome Pasien Sepsis pada
Geriatri. JK Unila. Vol.3, No.1, pp.147-153.
Dirgantoro, Z., 2018. Tesis : Hubungan antara Red Cell
Distribution Width (RDW), neutrofil-Limfosit Rasio
(NLR), Mean Platelet Volume (MPV) dengan skor
SOFA sebagai Prediktor Keparahan pada Sepsis di
RSUD Dr. Moewardi Surakarta. Surakarta :
digilib.uac.id.
Ferreira, F., Giuseppe, D., Giovanni, B., Fransescoc, D.,
and Pasquale, P., 2017. Sepsis dan Septic Shock: New
Definitions, New Diagnostic and Therapeutic
Approaches. Journal of Global Antimicrobial
Resistance. Vol.10, pp.204-212.
Iskandar A and Siska F., 2020. Analisis Hubungan SOFA
Score dengan Mortalitas Pasien Sepsis. Jurnal
Kesehatan Andalas. Vol. 9, No.2, pp.168-173.
Kemenkes., 2017. Pedoman Nasional Pelayanan
Kedokteran Tata Laksana Sepsis. Jakarta : Kementerian
Kesehatan RI.
Marik P dan Taeb A., 2017. SIRS, qSOFA, and new sepsis
definition. J Thorac Dis. Vol.9, No.4, pp.943-945.
McLymont dan Glover G., 2016. Scoring systems for the
characterization of sepsis and associated outcomes.
Ann TransI Med. Vol.4, No.24, pp.527.
Sari, E., Hayati, Y., and Rokhmawati, N., 2021. Hubungan
Skor Sofa dengan Mortalitas pada Pasien Sakit Kritis.
Majalah Kesehatan. Vol.8, No.3, p.149-155.
Seymourl, W., Vincent, C., Theodore, J., Frank, M,,
Thomas, D., et al., 2016. Assessment of clinical criteria
for sepsis : For the third international consensus
definitions for sepsis and septic shock (Sepsis-3).
JAMA. Vol.315, pp.762-774.
Shapiro, N., Zimmer, G., and Barkin, A., 2010. Sepsis
Syndromes. In: Marx et al. Rosen’s Emergency
Medicine Concepts and Clinical Practice. 7th Ed.
Philadelphia : Mosby Elsevier.
Singer, M., Deutschman, C., Seymour, C., Shankar, H.,
Annanne D, et al., 2016. The Third International
Consensus Definitions for Sepsis and Septic Shock
(Sepsis-3). JAMA. Vol.315, No.8, pp.801-810.
Sugiman, T., 2011. Sistem Skor di Intensive Care Unit.
Majalah Kedokteran Terapi Intensif. Vol.1, No.2,
pp.76-88.
Tavare A and Oflynn N., 2017. Recognition, Diagnosis, and
Early Management of Sepsis : NICE Guideline. British
Journal of General Practice. Vol.67, pp.185-186.
WHO., 2017. Improving the Prevention, Diagnosis, and
Clinical Management of Sepsis. World Health
Organizations.
Analysis of Sequential Organ Failure Assessment (SOFA) Score Profile in Relation to Length of Stay and Patient Outcome in the ICU of
Abdul Moeloek Regional General Hospital
207
