
Utilization of Health Services Among the Elderly in Medan City
Putranto Manalu
1,* a
, Ermi Girsang
1b
, Santy Deasy Siregar
2c
, Naomi Enzeli Manullang
3
and Nisa Apriyani Ginting
3
1
Departement of Public Health and Preventive Medicine, Universitas Prima Indonesia, Jl. Sampul No.3, Medan City,
Indonesia
2
Departement of Occupational Health and Safety, Universitas Prima Indonesia, Jl. Sampul No.3, Medan City, Indonesia
3
Departement of Healthcare Management, Universitas Prima Indonesia, Jl. Sampul No.3, Medan City, Indonesia
Keywords: Healthcare Utilization, Elderly, Distance.
Abstract: The low utilization of health services is a prevalent global issue, particularly in low- and middle-income
countries. As the elderly experience a decline in their overall body function and ability, they become more
vulnerable to degenerative diseases, which increases the demand for health services and the risk of mortality.
The present study aimed to analyze the determinants of health service utilization at the primary level. This
cross-sectional study was conducted at 41 community health center in Medan City, North Sumatra Province.
A proportional random sampling technique was used to select 485 participants. A structured questionnaire
was administered to collect the data. The data were analyzed using the chi-square test and logistic regression.
The findings revealed that health service utilization was affected by knowledge (0.002), insurance ownership
(0.006), distance (0.004), and family support (0.002). The logistic regression test demonstrates that distance
is the most influential factor (PR=10.067 (2.797-22.714)). Hence, it can be inferred that the utilization of
health services by older adults is affected by their knowledge, insurance ownership, distance, and family
support. Stakeholders are advised to guarantee convenient transportation access to overcome the challenge of
distance to healthcare centers.
1 INTRODUCTION
The increasing elderly population requires special
attention because their healthcare needs tend to rise
along with the growing risks of degenerative diseases
and healthcare costs (Abdi et al., 2019;
Sambamoorthi et al., 2015). The cumulative chronic
pathological processes in the elderly make it
challenging to recover from disease, and the growing
symptoms remaining from disease progression
contribute to the severity of other illnesses (Fan et al.,
2021). Declining memory, reduced hearing ability
(presbycusis), and vision impairment (presbyopia)
can limit physical mobility in older adults (Amarya et
al., 2018). Furthermore, psychological disturbances,
such as the loss of a life partner, can exacerbate the
above conditions, often leading to fatal outcomes
(Stahl et al., 2016).
a
https://orcid.org/0000-0002-2397-1067
b
https://orcid.org/0000-0003-4313-4941
c
https://orcid.org/0000-0003-0472-0331
The increase in the elderly population is occurring
globally as a consequence of technological and
healthcare advancements as well as improved
socioeconomic levels. It is estimated that by 2050, the
elderly population will double to 2.1 billion, with
80% residing in low- and middle-income countries
(WHO, 2022). Data from SUSENAS 2022 indicate
that the elderly population in Indonesia constitutes
10.48% of the total population with a dependency
ratio of 16.09 ((BPS, 2022). The demographic shift
among the elderly requires special attention from the
government, particularly regarding access to both
physical and mental healthcare (Chen et al., 2023).
The WHO mandated reforms in healthcare and long-
term care systems for the elderly in 2016, aiming to
enable them to optimize physical and mental health
throughout their lifetimes (WHO, 2016). Therefore,
efforts are needed to enhance the access and
Manalu, P., Girsang, E., Siregar, S. D., Manullang, N. E. and Ginting, N. A.
Utilization of Health Services Among the Elderly in Medan City.
DOI: 10.5220/0013666600003873
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Medical Science and Health (ICOMESH 2023), pages 101-106
ISBN: 978-989-758-740-5
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
101

affordability of healthcare services for the elderly and
address existing barriers.
Ease of access to healthcare is crucial for
improving healthcare service quality. Understanding
the factors with significant impacts is essential to
formulate effective strategies to overcome barriers to
accessing healthcare among the elderly. The
interactions among individuals, families, the
environment, and the healthcare system can be
explained by the concept of access to healthcare (Din
et al., 2014). Elderly people have specific needs in
terms of both the physical and psychological aspects
of daily activities. Limitations such as declining
physical abilities, income, and therapy needs can
affect the quality of life and self-actualization (Putri
& Lestari, 2018). Reduced physical capabilities in the
elderly can lead to decreased economic capacity,
subsequently limiting their social mobility (Quinn &
Cahill, 2016). Various factors influence healthcare
service utilization among the elderly, including
individual, family, community, and healthcare system
factors (Hlaing et al., 2020; Lin et al., 2020; Zeng et
al., 2022).
Previous studies have emphasized the importance
of knowledge in shaping health behavior changes and
health-seeking behavior (He et al., 2016; Teo et al.,
2021). Health insurance ownership has also been
reported as a predictor of healthcare service
utilization and can reduce inequality in the elderly
population (Dalinjong et al., 2017; Laksono et al.,
2023; Siongco et al., 2020). Healthcare service
disparities due to distance from healthcare facilities
have been reported in studies conducted in Yangon
and Texas ((Hlaing et al., 2020; Smith et al., 2019).
Research in Indonesia and China has concluded that
both financial and non-financial family support is a
crucial factor in encouraging the elderly to access
healthcare services (Cahyawati et al., 2020; Yuan et
al., 2022).
Medan is the third largest city in Indonesia and the
largest city on the island of Sumatra. Data gathered
from routine reports by the Medan City Health
Department indicate that the elderly population in the
city will amount to 186,196 people in 2022. Several
previous studies only involved one community health
center, thus having limitations in representing the
elderly population in the city of Medan as a whole
(Nasution, 2019; Siregar et al., 2015; Yollanda &
Zulfendri, 2018). This study will provide a more
comprehensive and representative overview of the
primary healthcare access challenges faced by the
elderly in the city of Medan. Therefore, the results of
this study can provide a deeper and more relevant
understanding in designing policies and intervention
programs that are in line with the real needs of the
elderly population in Medan. This study aimed to
analyze the relationship between knowledge, health
insurance ownership, distance to healthcare facilities,
family support, and healthcare service utilization
among the elderly in Medan
2 METHODS
2.1 Study Design
This cross-sectional study was conducted at 41
community health centers in Medan. This research
was conducted from June 2023 to August 2023.
2.2 Participant
The sample for this study consisted of 485 elderly
individuals obtained using the Lemeshow formula. In
recruiting research subjects, proportional random
sampling techniques were used to ensure that the
number of subjects was aligned with the population
size at each health center. The study included elderly
individuals aged ≥ 60 years, proficient in reading, and
willing to provide informed consent.
2.3 Data Collection
Data were collected using structured questionnaires
and observational sheets. The questionnaire was
divided into six sections: The first section contained
questions about the subjects' sociodemographic
information. The second section consisted of nine
questions on knowledge, and the third section
contained questions on health insurance ownership.
In the fourth section, the researcher inquired about the
distance (in kilometers) from the subjects' homes to
the community health center. The fifth section
comprises six questions about family support in
accessing healthcare. The sixth section included the
question: "Has the elderly person visited the
community health center in the last three months?".
All questionnaires were directly distributed to the
participants, and during data collection, the
researcher was accompanied by healthcare or local
officers to ensure the participants’ residential
addresses.
2.4 Data Analysis
All completed questionnaires were processed using
SPSS software version 26. The total scores of the
responses on each questionnaire were grouped into
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
102
several categories relevant to the operational
definition of the variables. Data were statistically
analyzed using the chi-squared test and logistic
regression analysis. The test results are presented in
tables and in narrative form.
2.5 Ethical Consideration
Ethical clearance for this study was obtained from the
Research Ethics Commission of Universitas Prima
Indonesia with registration number:
090/KEPK/UNPRI/VII/2023.
3 RESULTS
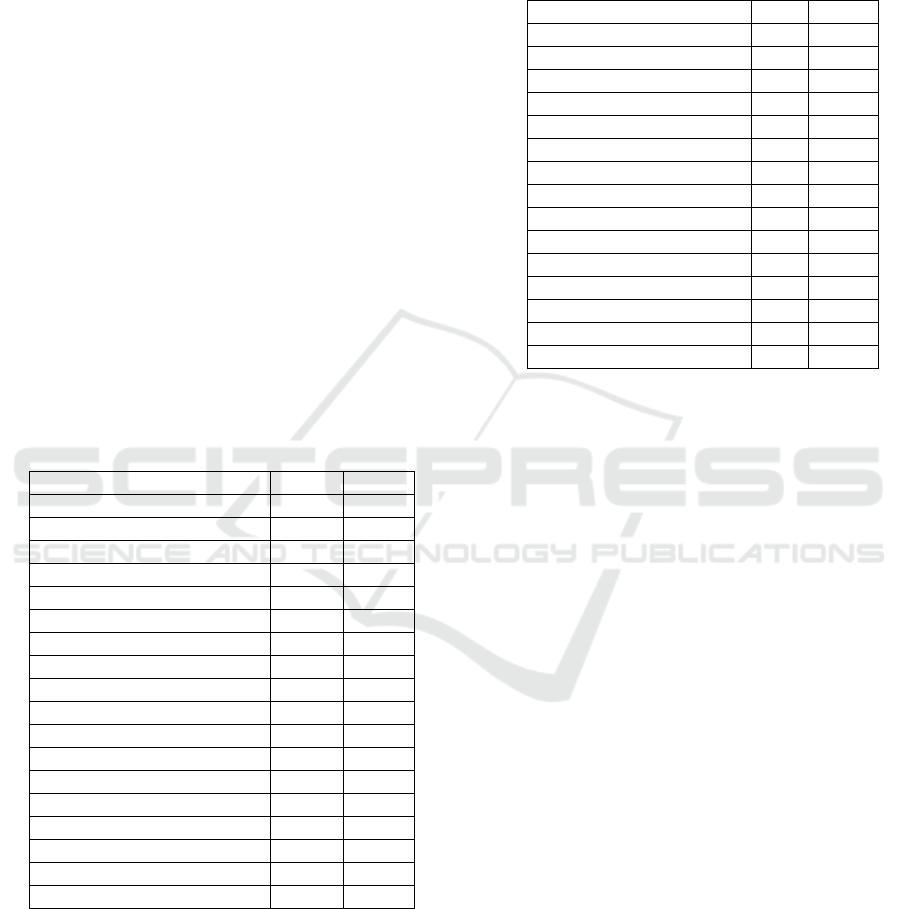
In Table 1, it can be observed that the majority of the
elderly fell within the age range of 60-65 years
(47.58%), and over half of them were female
(67.22%). Only 16.08% of the elderly pursued higher
education, while 2.27% did not attend school. More
than half of the elderly did not have a monthly income
(61.03%), and only 18.76% still had an income
exceeding 1.5 million rupiahs per month.
Table 1: Elderly sociodemographic data (n=485)
Characteristic n %
Age
60-64 226 47.58
65-69 170 35.79
≥70 79 16.63
Sex
Male 159 32.78
Female 326 67.22
Education Status
No school 11 2.27
Primary school 92 18.97
Middle school 143 29.48
High school 161 33.20
College/Degree 78 16.08
Income per month (Rupiah)
Nil 296 61.03
< 750.000 31 6.39
750.000 – 1.500.000 67 13.81
>1.500.000 91 18.76
Table 2 shows the frequency distribution based on
knowledge, health insurance ownership, distance to
healthcare facilities, family support, and healthcare
service utilization. The majority of the subjects had
insufficient knowledge (75.26%) and possessed
health insurance (85.36%). More than half of the
respondents indicated that the distance to healthcare
facilities was quite far, exceeding 5 km (67.42%). A
total of 314 individuals stated that they had received
support from their families (64.74%). Only 17.94%
had utilized healthcare services in the last 3 months
Table 2: Frequency distribution of research variables
Variable n %
Knowledge
Less 365 75.26
Good 120 24.74
Insurance ownership
No 71 14.64
Yes 414 85.36
Distance
Far (>5 km) 327 67.42
Near (≤ 5 km) 158 32.58
Family support
No 171 35.26
Yes 314 64.74
Health service utilization
No 398 82.06
Yes 87 17.94
Furthermore, the researcher conducted a chi-
square test to determine the significance of the
relationship between the predictors and healthcare
service utilization (Table 3). Among subjects with
poor knowledge, 60.82% did not utilize healthcare
services, and only 14.43% did so. In contrast, among
respondents with good knowledge, 21.24% did not
use healthcare services. The test results indicated a
significant relationship between knowledge and
healthcare service utilization (0.002). Similarly,
concerning health insurance, the statistical test results
show a significant relationship between insurance
ownership and healthcare service utilization (0.006).
Of 71 elderly individuals without health insurance, 50
did not utilize healthcare services. By contrast, among
those with insurance, only 13.61% utilized healthcare
services.
In this study, distance to healthcare facilities was
associated with healthcare service utilization (0.004).
Of the 327 elderly individuals who indicated that their
distance to healthcare facilities was quite far, only 61
utilized healthcare services. Family support is also
related to healthcare service utilization (0.000).
Elderly individuals receiving family support are more
likely to utilize health care services.
Next, a logistic regression analysis was conducted
to determine the variables or factors that most
dominantly influenced healthcare service utilization.
From the bivariate analysis, it was evident that all
predictors met the criteria for inclusion in the logistic
regression analysis (p<0.250).
Utilization of Health Services Among the Elderly in Medan City
103
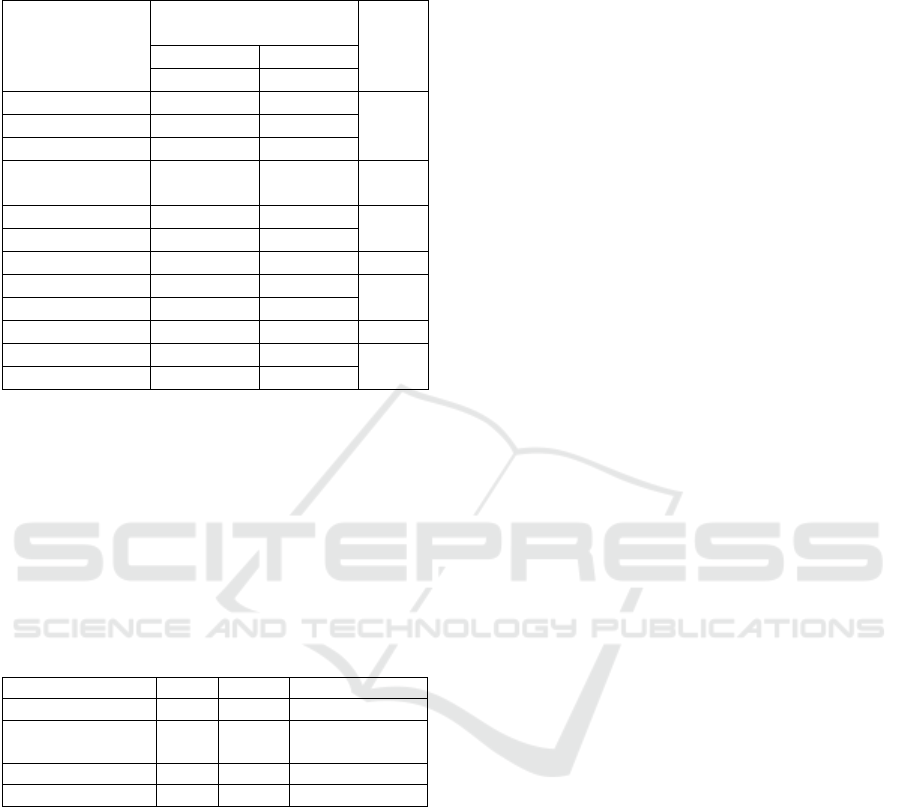
Table 3: Relationship between knowledge, insurance
ownership, distance, and family support with health service
utilization
Variable
Health service
utilization
p
No Yes
n (%) n (%)
Knowledge
0.002 Less 295 (60.82) 70 (14.43)
Good 103 (21.24) 17 (3.51)
Insurance
ownership
No 50 (10.31) 21 (4.33)
0.006
Yes 348 (71.75) 66 (13.61)
Distance
Far (>5 km) 266 (54.85) 61 (12.58)
0.004
Near (≤ 5 km) 132 (27.22) 26 (5.36)
Family support
No 146 (30.10) 25 (5.15)
0.000
Yes 252 (51.96) 62 (12.78)
The results of the analysis indicate that the most
dominant predictor influencing the utilization of
community health center services by the elderly in
Medan was distance. With a PR value of 10.067, it
can be projected that elderly individuals with a long
distance to healthcare facilities have a tendency to not
utilize healthcare services 10.067 times. This finding
underscores the significance of accessibility to
healthcare services.
Table 4: Dominant factor for health service utilization
Variable
p
PR 95% CI
Knowled
g
e 0.242 1.415 1.034
–
2.545
Insurance
ownership
0.007 8.469 2.797 – 22.714
Distance 0.002 10.067 2.455
–
44.714
Famil
y
su
pp
ort 0.124 0.668 1.956
–
3.341
4 DISCUSSION
The utilization of health services by the elderly is an
important and complex topic. Ideally, primary
healthcare facilities such as community health centers
should provide comprehensive services for the
elderly. Beyond focusing on primary treatment and
rehabilitation, these centers need to offer both
physical and mental health education services as a
form of promotive and preventive care to enable the
elderly to manage their health independently.
Numerous factors can influence the elderly's
utilization of available health services. This study
focused on several aspects, such as the elderly's
knowledge about health services, health insurance
ownership, distance from their residence to health
facilities, and family support.
The results indicate that knowledge significantly
predicts health-service utilization. In this study,
elderly individuals with limited knowledge were less
likely to use health services. Knowledge is crucial for
motivating the elderly to explore and access health
information. This finding aligns with those of several
previous studies (Mosadeghrad, 2014; Rahmadani et
al., 2022; Vorrapittayaporn et al., 2021). Limited
information receipt may lead the elderly to lack
interest in visiting health facilities, even for medical
checkups. One study reported infrequent health
check-ups due to insufficient information (Chien et
al., 2020). Additionally, most older people in this
study had high school education. A study in the
Philippines reported an association between
education level and health knowledge (Hoffmann &
Lutz, 2019).
The elderly also need adequate health insurance to
cover health service costs. Statistically, there was a
significant relationship between health insurance
ownership and health service utilization. Although
most elderly individuals have health insurance, only
a few use health services. This is possibly due to
public concerns about disparities in medical services
provided by community health centers for patients
with social insurance (JKN). A study in Manado
reported community reluctance to use JKN for
treatment because of negative perceptions
(Rumengan et al., 2015). Another study mentioned
that patients with JKN complained about short
examination and consultation durations, giving a
rushed impression (Rochmah et al., 2020). The study
results also indicate that family support significantly
encourages the elderly to access health services.
Families can assist the elderly in various ways such
as escorting them to health facilities, helping them
understand medical information, and providing
emotional support(Schulz et al., 2020). Additionally,
families can engage in discussions with health care
professionals and make informed decisions about
elderly care, especially in managing chronic diseases
(Alqahtani & Alqahtani, 2022).
In this study, the distance to health facilities was
also significantly associated and was the most
dominant predictor of elderly health services
utilization. This finding is consistent with that of a
study conducted in Ethiopia (Girma et al., 2011).
Elderly individuals from health facilities find it
challenging to travel, especially if they have mobility
limitations or lack access to reliable and friendly
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
104

transportation. Moreover, if transportation costs are
perceived as high, it becomes a consideration for the
elderly to seek health services. A study in China
reported barriers faced by the elderly despite the
reasonable distance to health facilities. Traffic
congestion, public transportation inconvenience, and
fare issues are the reasons for their lack of access to
health services (Li et al., 2022). Steps that can be
taken include encouraging the government to make
changes in an elderly friendly environment,
especially in public spaces and transportation
facilities, thus making them easily accessible.
Increasing the number of health facilities could be an
additional option, particularly in urban areas with
inadequate public transportation.
5 CONCLUSIONS
The results indicate that knowledge, health insurance,
distance, and family support are significantly
associated with the utilization of health services by
the elderly. Space emerged as the most dominant
predictor influencing the elderly to seek healthcare
services at health facilities. Elderly individuals with
good knowledge, health insurance, proximity, and
strong family support are more likely to use health
services than those without these factors. Community
health centers are recommended to enhance the
quality and availability of healthcare services for the
elderly, especially in terms of health information, and
promote family involvement in healthcare.
Additionally, the government is encouraged to
provide elderly friendly and cost-effective
transportation facilities.
REFERENCES
Abdi, S., Spann, A., Borilovic, J., de Witte, L., & Hawley,
M. (2019). Understanding the care and support needs of
older people: a scoping review and categorisation using
the WHO international classification of functioning,
disability and health framework (ICF). BMC
Geriatrics, 19(1), 195. https://doi.org/10.1186/s12877-
019-1189-9
Alqahtani, J., & Alqahtani, I. (2022). Self-care in the older
adult population with chronic disease: concept analysis.
Heliyon, 8(7), e09991.
https://doi.org/10.1016/j.heliyon.2022.e09991
Amarya, S., Singh, K., & Sabharwal, M. (2018). Ageing
Process and Physiological Changes. In Gerontology.
InTech. https://doi.org/10.5772/intechopen.76249
BPS. (2022). Statistik Penduduk Lanjut Usia 2022. BPS.
Cahyawati, S., Rumaolat, W., Jalaludin Rumi, N. S., &
Rumaolat, W. (2020). Factors Related to the Utilization
of the Integrated Health Services Center for the Elderly.
Jurnal Ners, 15(1), 63–66.
https://doi.org/10.20473/jn.v15i1Sp.18945
Chen, C., Ding, S., & Wang, J. (2023). Digital health for
aging populations. Nature Medicine, 29(7), 1623–1630.
https://doi.org/10.1038/s41591-023-02391-8
Chien, S.-Y., Chuang, M.-C., & Chen, I.-P. (2020). Why
People Do Not Attend Health Screenings: Factors That
Influence Willingness to Participate in Health
Screenings for Chronic Diseases. International Journal
of Environmental Research and Public Health, 17(10),
3495. https://doi.org/10.3390/ijerph17103495
Dalinjong, P. A., Welaga, P., Akazili, J., Kwarteng, A.,
Bangha, M., Oduro, A., Sankoh, O., & Goudge, J.
(2017). The association between health insurance status
and utilization of health services in rural Northern
Ghana: evidence from the introduction of the National
Health Insurance Scheme. Journal of Health,
Population and Nutrition, 36(1), 42.
https://doi.org/10.1186/s41043-017-0128-7
Din, N. C., Ghazali, S. E., Ibrahim, N., Ahmad, M., Said,
Z., Ghazali, A. R., Razali, R., & Shahar, S. (2014).
Health Needs Assessment of Older People in an
Agricultural Plantation. International Journal of
Gerontology, 8(3), 120–126.
https://doi.org/10.1016/j.ijge.2013.12.003
Fan, Z.-Y., Yang, Y., Zhang, C.-H., Yin, R.-Y., Tang, L.,
& Zhang, F. (2021). Prevalence and Patterns of
Comorbidity Among Middle-Aged and Elderly People
in China: A Cross-Sectional Study Based on CHARLS
Data. International Journal of General Medicine, 14,
1449–1455. https://doi.org/10.2147/IJGM.S309783
Girma, F., Jira, C., & Girma, B. (2011). Health services
utilization and associated factors in jimma zone, South
west ethiopia. Ethiopian Journal of Health Sciences,
21(Suppl 1), 85–94.
He, Z., Cheng, Z., Shao, T., Liu, C., Shao, P., Bishwajit, G.,
Feng, D., & Feng, Z. (2016). Factors Influencing Health
Knowledge and Behaviors among the Elderly in Rural
China. International Journal of Environmental
Research and Public Health, 13(10), 975.
https://doi.org/10.3390/ijerph13100975
Hlaing, S. M. M., Clara, N., & Han, A. N. (2020). Factors
influencing health service utilization among the elderly
in Insein Township, Yangon Region. Makara Journal
of Health Research, 24(3), 208−215.
https://doi.org/10.7454/msk.v24i3.1223
Hoffmann, R., & Lutz, S. U. (2019). The health knowledge
mechanism: evidence on the link between education
and health lifestyle in the Philippines. The European
Journal of Health Economics, 20(1), 27–43.
https://doi.org/10.1007/s10198-017-0950-2
Laksono, A. D., Nugraheni, W. P., Ipa, M., Rohmah, N., &
Wulandari, R. D. (2023). The Role of Government-run
Insurance in Primary Health Care Utilization: A Cross-
Sectional Study in Papua Region, Indonesia, in 2018.
International Journal of Social Determinants of Health
Utilization of Health Services Among the Elderly in Medan City
105

and Health Services, 53(1), 85–93.
https://doi.org/10.1177/00207314221129055
Li, Z., Gao, Y., Yu, L., Choguill, C. L., & Cui, W. (2022).
Analysis of the Elderly’s Preferences for Choosing
Medical Service Facilities from the Perspective of
Accessibility: A Case Study of Tertiary General
Hospitals in Hefei, China. International Journal of
Environmental Research and Public Health, 19(15),
9432. https://doi.org/10.3390/ijerph19159432
Lin, Y., Chu, C., Chen, Q., Xiao, J., & Wan, C. (2020).
Factors influencing utilization of primary health care by
elderly internal migrants in China: the role of social
contacts. BMC Public Health, 20(1), 1054.
https://doi.org/10.1186/s12889-020-09178-3
Mosadeghrad, A. M. (2014). Factors Influencing
Healthcare Service Quality. International Journal of
Health Policy and Management, 3(2), 77–89.
https://doi.org/10.15171/ijhpm.2014.65
Nasution, F. A. (2019). Analisis Pemanfaatan Posyandu
Lansia di Wilayah Kerja Puskesmas Amplas Tahun
2019. Universitas Islam Negeri Sumatera Utara.
Putri, A. A., & Lestari, C. N. (2018). The Ability to Meet
the Elderly’s Basic Needs for Healthy Ageing in Low-
and Middle-Income Countries. KnE Life Sciences, 4(1),
39. https://doi.org/10.18502/kls.v4i1.1364
Quinn, J. F., & Cahill, K. E. (2016). The new world of
retirement income security in America. American
Psychologist, 71(4), 321–333.
https://doi.org/10.1037/a0040276
Rahmadani, S., Lasari, H. H. D., Hamka, N. A., & Rahma,
A. N. (2022). Determinants of the Utilization of Elderly
Integrated Healthcare Center Services in the Kassi
Kassi Health Center Working Area of Makassar City.
Jurnal Publikasi Kesehatan Masyarakat Indonesia,
9(3), 129–139.
Rochmah, T. N., Chalidyanto, D., Ernawaty, & Suhanda, R.
(2020). National Health Insurance Participants
Satisfaction in General Polyclinic Services at First
Level Healthcare Facilities. Indian Journal of Forensic
Medicine & Toxicology, 14(4), 3531–3537.
https://doi.org/10.37506/ijfmt.v14i4.12174
Rumengan, D. S. S., Umboh, J. M. L., & Kandou, G. D.
(2015). Faktor-Faktor yang Berhubungan dengan
Pemanfaatan Pelayanan Kesehatan Pada Peserta BPJS
Kesehatan di Puskesmas Paniki Bawah Kecamatan
Mapanget Kota Manado. Jurnal Ilmu Kesehatan
Masyarakat, 5(1), 88–100.
https://doi.org/10.1016/j.psychres.2014.11.019
Sambamoorthi, U., Tan, X., & Deb, A. (2015). Multiple
chronic conditions and healthcare costs among adults.
Expert Review of Pharmacoeconomics & Outcomes
Research, 15(5), 823–832.
https://doi.org/10.1586/14737167.2015.1091730
Schulz, R., Beach, S. R., Czaja, S. J., Martire, L. M., &
Monin, J. K. (2020). Family Caregiving for Older
Adults.
Annual Review of Psychology, 71(1), 635–659.
https://doi.org/10.1146/annurev-psych-010419-050754
Siongco, K. L. L., Nakamura, K., & Seino, K. (2020).
Reduction in inequalities in health insurance coverage
and healthcare utilization among older adults in the
Philippines after mandatory national health insurance
coverage: trend analysis for 2003–2017. Environmental
Health and Preventive Medicine, 25(1), 17.
https://doi.org/10.1186/s12199-020-00854-9
Siregar, R., Siagian, A., & Lubis, H. S. (2015). Faktor-
Faktor yang Berhubungan dengan Pemanfaatan
Pelayanan Posyandu Lansia di Wilayah Kerja
Puskesmas Suka Surya Medan Kelurahan Suka Maju
Kecamatan Medan Johor. Universitas Sumatera Utara.
Smith, M., Towne Jr, S., Bergeron, C., Zhang, D., McCord,
C., Mier, N., & Goltz, H. (2019). Geographic disparities
associated with travel to medical care and attendance in
programs to prevent/manage chronic illness among
middle-aged and older adults in Texas. Rural and
Remote Health, 19(4), 5147.
https://doi.org/10.22605/RRH5147
Stahl, S. T., Arnold, A. M., Chen, J.-Y., Anderson, S., &
Schulz, R. (2016). Mortality After Bereavement: The
Role of Cardiovascular Disease and Depression.
Psychosomatic Medicine, 78(6), 697–703.
https://doi.org/10.1097/PSY.0000000000000317
Teo, K., Churchill, R., Riadi, I., Kervin, L., & Cosco, T.
(2021). Help-seeking behaviours among older adults: a
scoping review protocol. BMJ Open, 11(2), e043554.
https://doi.org/10.1136/bmjopen-2020-043554
Vorrapittayaporn, C., Malathum, P., & Phinitkhajorndech,
N. (2021). Relationships among Knowledge, Health
Literacy, and Health Behavior in Older Persons with
Chronic Kidney Disease. Nursing Research and
Innovation Journal, 27(1), 77–91.
WHO. (2016). Multisectoral action for a life course
approach to healthy ageing: draft global strategy and
plan of action on ageing and health.
http://apps.who.int/gb/ebwha/pdf_files/WHA69/A69_
17-en.pdf
WHO. (2022). Ageing and health.
https://www.who.int/news-room/fact-
sheets/detail/ageing-and-health
Yollanda, Y. E., & Zulfendri. (2018). Beberapa Faktor
yang Mempengaruhi Pemanfaatan Pelayanan
Kesehatan Puskesmas oleh Masyarakat di Wilayah
Kerja Puskesmas Medan Labuhan Tahun 2018.
Universitas Sumatera Utara.
Yuan, B., Zhang, T., & Li, J. (2022). Family support and
transport cost: understanding health service among
older people from the perspective of social-ecological
model. Archives of Public Health, 80(1), 173.
https://doi.org/10.1186/s13690-022-00923-1
Zeng, Y., Xu, W., & Tao, X. (2022). What factors are
associated with utilisation of health services for the
poor elderly? Evidence from a nationally representative
longitudinal survey in China. BMJ Open, 12(6),
e059758. https://doi.org/10.1136/bmjopen-2021-
059758
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
106
