
Clinical Features, Surveillance and Determinant Factors of Malaria
Outbreak in Usili Village, Southwest Papua, Indonesia
Andrew Ivan Humonobe
*
a
, Nadiyah Kamilia
b
and Sintong Halomoan Sianturi
c
Faculty of Medicine, University of Papua, Aimas-Klamono Street Km.28, Sorong Regency, Indonesia
Keywords: Malaria, Risk Factor, Surveillance.
Abstract: Malaria is a global health concern including in Indonesia. In early 2023, Sorong Regency Health Office
reported that there was a malaria outbreak in Usili Village, Southwest Papua, Indonesia. A total of 38 cases
were confirmed positive by rapid diagnostic test (RDT) and microscopic examination. This study aimed to
describe clinical features, surveillance system and determinant factors that contributed to the outbreak. A mix-
method study was conducted. Clinical features and surveillance were designed with qualitative descriptive,
while determinant factors of malaria used case control design. A total of 144 individuals were participated in
this study. Results showed that 68.7% of the case was uncomplicated malaria. Risk factor analysis illustrated
that working status (OR 2.1; 95% CI 1.005-2.765), night outdoor activities (OR 1.6; 95% CI 0.650 - 1.805),
using mosquito net (OR 1.9; 95% CI 0.005-2.765) were contributed to the case. Surveillance variables
revealed incomplete data reporting, unreliable data collection, and a postponed epidemiology investigation.
We draw conclusion that the majority cases of this outbreak were clinically uncomplicated malaria. The
outbreak was linked to determinant factors like outdoor activities, mosquito net use, and working status. This
study also emphasizes the shortcomings of the surveillance system in preventing malaria.
1 INTRODUCTION
Malaria is one of infectious disease affects globally
which lead to increasing morbidity and mortality.
World Malaria Report 2022 released by WHO states
that there were 247 million cases of malaria in 2021,
which resulted in 619,000 deaths (WHO, 2022). Nine
countries in South-East Asia are endemic for malaria,
which accounts for 22% of malaria deaths and 15.6%
of cases in the region. With an estimated 811,636
cases, Indonesia has the second-highest number of
malaria cases in this region. (WHO, 2022, 2021b).
Annual malaria report showed that there was an
increasing malaria incidence in 2021 roughly up to
thirty percent giving escalated number from 304,607
to 400,253 positive cases in 2022, dominantly
occurred in Papua region which contributed to 90%
of national total cases (Indonesian Ministry of Health,
2023).
a
https://orcid.org/0009-0008-3043-5466
b
https://orcid.org/0009-0003-1964-1203
c
https://orcid.org/0009-0004-4049-7290
Malaria is a parasitic infection of Plasmodium sp
in human. This parasite is transmitted by the
Anopheline mosquito that leads to acute-life
threatening disease (Buck and Finnigan, 2023).
Human infection is known to occur in five
Plasmodium species including P. vivax, P.
falciparum, P. ovale, P. knowlesi, and P. malariae
(Buck and Finnigan, 2023; Tangpukdee et al., 2009).
Furthermore, P. falciparum and P. vivax were the
most prevalent species in Indonesia (Bria et al.,
2021). Malaria transmission is a complex web of
interactions exists between human hosts, Anopheline
mosquitoes, Plasmodium parasites, and local socio-
ecological conditions (Dhewantara et al., 2019).
Malaria risk factors include the use of mosquito nets,
spraying insecticide, age, home construction
conditions, altitude and weather conditions (Mosha et
al., 2020; Sulistyawati et al., 2020).
Typical malaria symptoms are chills, fever and
sweating. Other additional manifestation include
headache, dizziness, vomiting, diarrhea, muscle pain,
Humonobe, A. I., Kamilia, N. and Sianturi, S. H.
Clinical Features, Surveillance and Determinant Factors of Malaria Outbreak in Usili Village, Southwest Papua, Indonesia.
DOI: 10.5220/0013660400003873
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Medical Science and Health (ICOMESH 2023), pages 55-61
ISBN: 978-989-758-740-5
Proceedings Copyright © 2025 by SCITEPRESS – Science and Technology Publications, Lda.
55

lack of appetite, weakness, jaundice and even
impaired consciousness. Malaria can, however,
occasionally present with no symptoms (Bartoloni
and Zammarchi, 2012; Bria et al., 2021).
The primary method for identifying malaria is by
examining microscopic findings, which is considered
the gold standard. However, there are instances where
misdiagnosis can occur, particularly when the level of
parasites in the blood is low or if the identification of
the specific species is incorrect (Kang et al., 2017;
Tangpukdee et al., 2009). To address this issue, rapid
diagnostic testing (RDT) is frequently employed in
isolated locations with limited access to microscopic
examination expertise (Diallo et al., 2017;
Tangpukdee et al., 2009).
Indonesia's malaria control program goal is to
completely eradicate malaria by 2030, achieving
malaria-free status gradually. Three primary actions
were to raise annual blood examination rate (ABER)
and decrease the annual parasite incidence (API) and
positivity rate (PR). The actions done are to certify
each region for malaria, beginning at the district or
city and moving up to the province, region, and
national levels. These indicate that the following
conditions must be met in order: (1) no indigenous
cases for three years in a row; (2) PR of less than 5%;
and (3) API of less than 1 per 100,000 (Herawati et
al., 2023).
Malaria surveillance program starts with patient
registration and data collection at Public Health
Center (PHC). Next, PHC generates monthly reports
on malaria based on the disease's cases it has
identified and its outpatient services. PHC is in charge
of data analysis and the production of a report on the
trends and distribution of the disease for the local
area. PHCs notify the district malaria control officer
of any malaria-related issues, and the officer compiles
the data into district health profile. Details regarding
the annual and monthly cases of malaria reported at
village level are included in the health profile. Then,
sub-directorate of malaria control at directorate of
vector-borne diseases in Indonesian Ministry of
Health receives aggregated malaria reports from the
district health office, which then forwards them to the
provincial health office three times a year (Elyazar et
al., 2011).
In early 2023, unpublished data from Sorong
Regency Health Office reported that there was a
malaria outbreak in Usili Village as many as 38
positive cases, whereas previously there had been no
history of malaria infection in the region. The
transmission scheme was indigenous. Usili Village is
located in Aimas District, Sorong Regency,
Southwest Papua Province and positioned in the
working area of Malawili PHC under Sorong
Regency Health Office supervision. This study aimed
to describe clinical aspects, implementation of
surveillance system and other risk factors that play
role in the emergence of malaria outbreaks in Usili
Village, Southwest Papua.
2 METHOD
This study was designed with a mixed method.
Clinical features and surveillance variables were
observed with qualitative descriptive design using
interview and secondary data analysis. Surveillance
data was collected from Malawili PHC and Sorong
Regency Health Office. In order to depicting
determinant factors of malaria, an analytical study
with a case-control design with a ratio of 1:2 was
used. Data collection was carried out from primary
and secondary source. Secondary data was taken from
Malawili PHC medical record. Meanwhile, primary
data was obtained by using questionnaire. A total of
144 participants from Usili Village was recruited in
this study, 48 people were grouped as positive malaria
(confirmed through microscopic finding or RDT from
medical record) while 96 people were control.
Samples were selected using the stratified random
sampling.
3 RESULT
3.1 Clinical Features
Malaria can present with a range of clinical
manifestations, from mild to potentially fatal. During
the interviews with all of the positively confirmed
participants, symptoms such as fever, chills,
headache, muscle soreness, nausea, vomiting,
diarrhea, weakness, jaundice, and seizures were
reported. In Figure 1, it is clear that all (100%)
responders who tested positive for malaria had fever.
Additionally, a majority of these individuals
experienced chills (93.75%) and nausea (87.5%).
Other reported symptoms included headache
(68.75%), muscle pain (41.67%), weakness
(35.42%), vomiting (25%), diarrhea (20.83%),
seizures (22.92%), and jaundice (8.33%). By
considering the last set of clinical symptoms, it is
reasonable to assume that approximately 31.25%
(corresponding to 15 individuals) had severe malaria,
while the remaining 68.75% (33 individuals)
exhibited uncomplicated malaria.
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
56
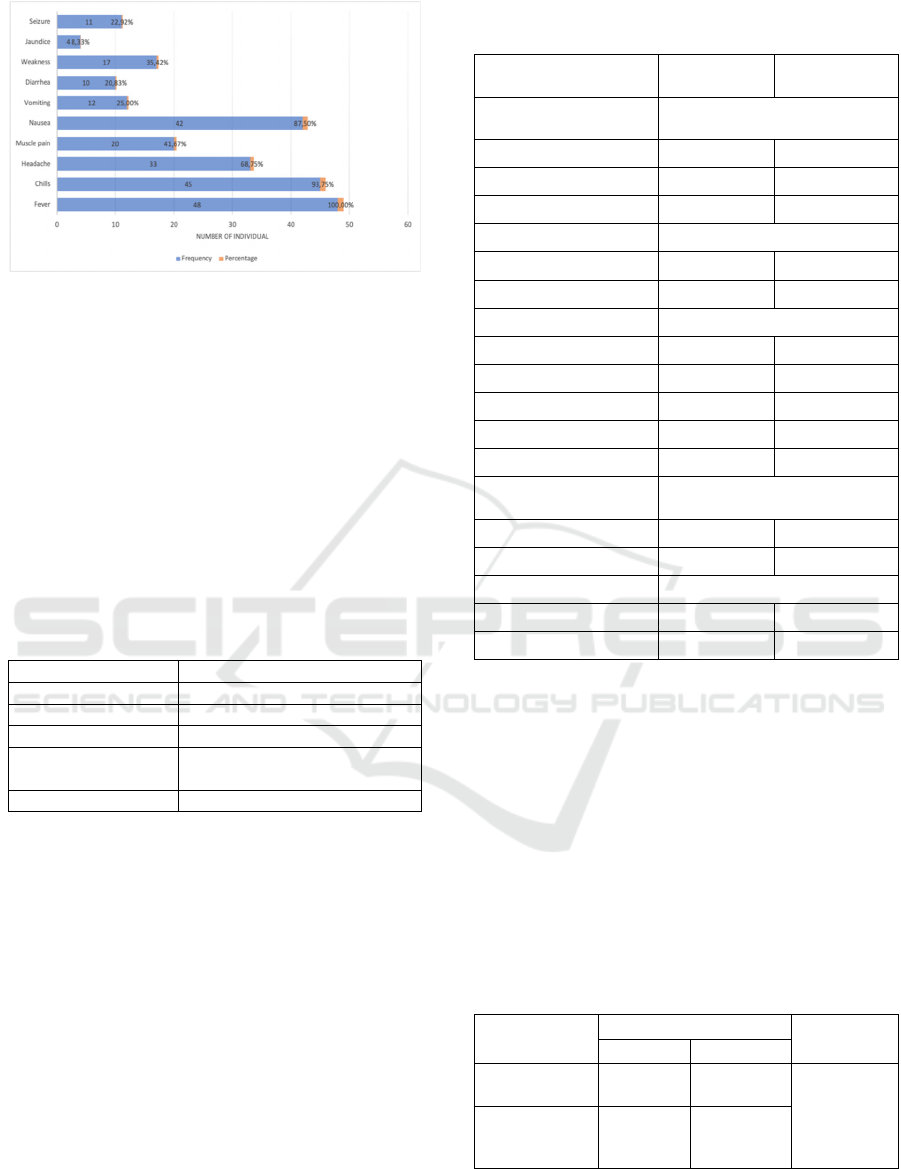
Figure 1: Clinical symptoms of malaria positive
respondents
3.2 Surveillance System Management
Planning, implementing, and evaluating public health
practices are all part of public health surveillance,
which is reliant on ongoing, systematic data
collection, analysis, and interpretation (Centers for
Disease Prevention and Control, 2022).
Although Malawi PHC has carried out malaria
surveillance in accordance with national guidelines,
there are some inconsistencies in the way it has been
carried out. Table 1 shows this in the following.
Table 1: Surveillance data taken from Malawili PHC.
Surveillance data Result
Data simplicit
y
Easy to get
Data
q
ualit
y
Incom
p
lete data
Data stabilit
y
Unreliable
System
representation
Distributed over all
p
opulation
Re
p
ortin
g
schedule Dela
y
ed investi
g
ation
3.3 Analysis of Malaria Determinant
Factors
Table 2 shows the characteristics of respondents and
the type of infection in the people of Usili Village. In
total, 144 people were included in the study. The type
of infection that occurs is mostly by P. vivax
(45.83%), P. falciparum (37.5%) and mixed malaria
(16.67%). Based on the characteristics of the
respondents, the most (70.83%) are those who are
actively working, 36.11% are not in school, 63.89%
have nighttime activities outside the home, and
51.39% do not use mosquito nets while sleeping.
Table 2: Type of malaria and characteristic of participants
in Usili Village.
Characteristics
Frequency
(
n
)
Percentage
(
%
)
Type of malaria
infection
P. falciparum 18 37.50
P. vivax 22 45.83
Mixed malaria 8 16.67
Working
Yes 102 70.83
No 42 29.17
Education level
Not joining school 52 36.11
Primary school 40 27.78
Middle school 15 10.42
High school 20 13.89
University 17 11.81
Night outdoor
activities
Yes 92 63.89
No 52 36.11
Use of mosquito nets
Yes 70 48.61
No 74 51.39
Table 3 presents working status factor and the
occurrence of malaria. Out of the 48 individuals who
have malaria, 50% of them are engaged in some form
of work, while the remaining 50% are not employed.
Interestingly, among those who work, 81.91% do not
have a malaria infection. Statistical results indicate a
significant association between people who do not
work and experience malaria (p = <0.001; OR CI 95%
= 2.1 (1.005-2.765). These findings indicate that the
risk of contracting malaria is 2.1 times higher in non-
working individuals than in working individuals.
Table 3: Bivariate analysis of working status and malaria
incidence.
Working Malaria infection p
Positive Negative
Yes
24
(
50.0%
)
78
(
81.91%
)
<0.001
OR 2.1
95%
CI(1.005-
2.765)*
No
24
(50.0%)
18
(18.11%)
*chi-square analysis
Clinical Features, Surveillance and Determinant Factors of Malaria Outbreak in Usili Village, Southwest Papua, Indonesia
57
Table 4 describes education level factor and
malaria incidence in Usili Village. Based on the data
of respondents who are positive for malaria, 18.75%
are individuals who are not in school, 27.08% are
only up to primary education, 41.67% are only up to
secondary education, 6.25% are high school and
6.25% are up to higher education. There was no
significant result displayed in the statistical analysis
(p=0.114; OR 1.308 95% CI=(1.005-1.702)) although
the odds ratio showed that people with low education
level were at risk 1.308 times higher than individuals
with high levels of education.
Table 4: Bivariate analysis of education level with malaria
incidence.
Education level Malaria infection p
Positive Negative
Not joining
school
9
(
18.75%
)
43
(
44.79%
)
0.114
OR 1.308
95%
CI(1.005-
1.702)*
Primary school
13
(27.08%)
27
(28.12%)
Middle school
20
(41.67%)
12
(12.5%)
High school
3
(
6.25%
)
17
(
17.7%
)
University
3
(
6.25%
)
4
(
4.16%
)
*chi-square analysis
According to the data shown on Table 5, up to
52.08% (25 persons) of those who engage in
nighttime activities outside of their homes suffer from
malaria, compared to 47.91% (23 people) of those
who do not. There is a statistically significant
correlation (p<0.05) between malaria incidence and
activity during the night. These findings also indicate
that there is a 1.6-fold increase in the risk of malaria
infection in individuals who are active at night.
Table 5: Bivariate analysis of night outdoor activities with
the incidence of malaria.
Night outdoor
activities
Malaria infection p
Positive Negative
Yes
25
(52.08%)
67
(69.79%)
0.037
OR 1.6
95%
CI(0.650-
1.805)*
No
23
(47.91%)
29
(30.20%)
*chi-square analysis
The chance of contracting malaria while using
mosquito nets is shown in Table 6. Considering the
findings of this research, 70.83% of the population
who do not use mosquito nets are at risk of
developing malaria, while 29.16% of people who use
less mosquito nets are affected by malaria. Significant
findings from statistical analysis indicated a
relationship between the prevalence of malaria and
the use of mosquito nets (p=0.001). This research also
shows that sleeping without a mosquito net increases
the risk of malaria by 1.9 times compared to sleeping
with one.
Table 6: Bivariate analysis of mosquito net use activities
and malaria incidence.
Mosquito
net usage
Malaria infection
p
Positive Negative
Yes
14
(29.16%)
56
(58.33%)
0.001
OR 1.9
95%CI(0.005-
2.765)*
No
34
(70.83%)
40
(41.67%)
*chi-square analysis
4 DISCUSSION
The objectives of this study were to look into a
malaria outbreak, characterize clinical characteristics,
identify risk factors, and look into health centers'
malaria surveillance.
Diagnosing malaria can be challenging. In this
study it appears that all patients experienced common
symptom such as fever. Based on WHO guidelines all
patients who have a fever or a history of fever can be
suspected of being infected with malaria.
Nevertheless, diagnosis based only on clinical
symptoms has low specificity and can lead to
overtreatment. To get a definite diagnosis should be
carried out further examination of microscopic blood
smear examination or with RDT (WHO, 2023). It was
discovered that the majority of the malaria outbreaks
in Usili Village were caused by P. vivax infection,
with P. falciparum infections coming in second and
mixed malaria making up the least. According to the
clinical symptoms reported, the majority of cases of
malaria experienced by residents of Usili Village in
this study are uncomplicated cases with a lesser
number of severe cases. This finding is in accordance
with the results that appear that most malaria
infections that occur in the village is caused by
P.vivax (45.83%). Additionally, P. vivax tends to
cause less parasitemia and is less severe than P.
falciparum, according to the study (Baird, 2013;
Menkin-Smith and Winders, 2023). Although no
additional laboratory tests were performed in these
cases, the severe malaria cases in this study were
based on those who experienced symptoms such as
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
58

jaundice and seizures (Bartoloni and Zammarchi,
2012).
In this study, we use five attributes—data quality,
data stability, system representativeness, timeliness,
and surveillance system simplicity—to evaluate the
surveillance success indicators based on WHO
guidelines (Centers for Disease Prevention and
Control, 2022; Nsubuga et al., 2006). System
simplicity can be assessed by looking at indicators
such as ease of defining cases, collecting, recording
and reporting data. The case definition used by the
Malawili PHC is in accordance with the national
guidelines for malaria management, where case
enforcement is based on anamesis and laboratory
diagnosis. It is necessary to underline the importance
of correct diagnosis in establishing the definition of
malaria cases (Indonesian Ministry of Health, 2019;
WHO, 2023). Malawili PHC is already good at
screening and confirmation activities.
The validity and completeness of the data entered
into the epidemiological surveillance system can be
used to assess the quality of the data. Data is said to
be complete if the confirmation case is filled in
completely and validates to health facilities that
report confirmed cases of malaria (Centers for
Disease Prevention and Control, 2022). The data
available in the Malawili PHC surveillance are
monthly situation monitoring, individual basic data
reports, monthly reports by summing patients/deaths
including some basic eradication/countermeasures
activities every month to the Sorong Regency Health
Office. However, the weakness in the presentation of
the data is made data stratification determination of
malaria endemicity sub-district level by making the
sub-district table by summing malaria patients. This
is similar to the results of other studies in the Kupang
area which found that PHC in Kupang regency had
not made an endemicity map of the area, so it was
considered incompatible with the role of PHC as a
work unit in the surveillance system to carry out
malaria in the working area by village (stratification)
annually where the dissemination of information by
the health office and PHC was only in the form of
reports, and did not publish malaria
bulletins/magazines. Cross-organizational meetings
have also not been conducted by the health office.
This is not in accordance with the role of the
district/city health office as a work unit in the
surveillance system, namely distributing malaria
information across programs and across sectors
(Desita et al., 2021).
Data stability relates to the reliability and
availability of surveillance system. The capacity to
accurately gather, arrange, and deliver data is known
as reliability. Conversely, availability is the capacity
to function when called upon (Centers for Disease
Prevention and Control, 2022). The Malawili PHC
does not report weekly and monthly cases to the
Sorong Regency Health Office. Data is received if
there are cases from outbreak reports and new cases
resulting from epidemiological investigations in the
field. The Sorong Regency Health Office does not
receive individual case data directly from Malawili
PHC unless the PHC diagnoses individual data from
referral health facilities. This is related to the absence
of cross-sector involvement to carry out laboratory
and RDT examinations in primary care facilities
around the Aimas district. Surveillance data stability
refers to the consistency and reliability of data
collected through a health surveillance system.
Reporting consistency factors influencing the
stability of surveillance data at the Malawili PHC are
consistency in reporting data to responsible entities,
such as health office, ensuring that information is
available and can be used for decision making and
then related to officer training where officers must
know that one of their duties is to improve networking
with health service facilities.
Timeliness of surveillance refers to the extent to
which surveillance data is collected, analyzed and
reported according to a predetermined schedule. This
timeliness has a pivotal role in surveillance system
effectiveness and response to public health issues.
Case reporting confirm malaria according to
agreement that is less than 24 hours, while reporting
case recaps per sub-district by the public health center
that is the 4th of every month and agreed to require a
maximum of 24 hours to immediately carry out an
epidemiological investigation (Centers for Disease
Prevention and Control, 2022; Indonesian Ministry of
Health, 2019). However, when the observation was
carried out there was a delay in the report from the
hospital and more than 24 hours was needed to carry
out an epidemiological investigation.
The risk factors most associated with malaria
cases in Usili Village are night outdoor activities,
working status and using mosquito nets. Outdoor
activities at night can have implications for the risk of
malaria transmission, especially since the Anopheles
mosquito, which is a vector of the disease, is
generally active at night, especially at dusk and early
morning. A person's chance of contracting malaria is
increased if they spend a lot of time outside at night
in an area where Anopheles mosquito vectors are
common (Sulistyawati et al., 2020). This result is in
line with other studies conducted at the Remu PHC in
Sorong City with a sample of 84 people where it was
found that there was a significant relationship
Clinical Features, Surveillance and Determinant Factors of Malaria Outbreak in Usili Village, Southwest Papua, Indonesia
59

between nighttime activities outside the home with
the risk of malaria infection (OR 3.411 95% CI
(1.363-8.542)). This is due to the activities of people
who often go out of the house at night, namely people
who have a lot of work so they come home at night,
as students who study at night, as motorbike taxi
drivers, mothers who do social gatherings or who
worship at night. and most groups of young people,
even children, who often hang out, walk around and
date at night, without wearing protective clothing
such as jackets/long sleeves/trousers/sarongs can be
at risk of contracting malaria (Papilaya et al., 2015).
The factor of not using mosquito nets also
contributed to the malaria
outbreak in Usili Village. This result is in line with
research observed at Remu PHC Sorong City, where
based on bivariate analysis conducted, there is a
connection between the risk of getting malaria and the
use of mosquito nets. (p=0.042; OR 2.562 95% CI =
1.025-6.406)) (Papilaya et al., 2015). Based on
interviews with respondents in the positive malaria
group and the control group said that although they
had been given mosquito nets from health workers
from the Malawili PHC, they did not use them
because they felt uncomfortable and the room became
hot when using mosquito nets at night and there were
even those who sold and discarded mosquito nets that
had been given.
This study also found that working status have a
relationship with malaria incidence. We observed that
people who do not work typically spend their time
doing household chores and running the risk of
contracting malaria. People who are less active for a
long time at home have a high chance of exposure to
Anopheles mosquitoes. This is because the houses of
Usili Village residents are located in a swamp area
which is a suitable condition for the breeding of
anopheles mosquitoes as malaria vectors (Munthe et
al., 2022).
5 CONCLUSIONS
The first malaria outbreak in Usili Village, Southwest
Papua was contributed by several weaknesses in the
surveillance system and malaria prevention
programs, including: shortcomings of surveillance
system at the Malawili PHC in recording and
reporting incomplete cases, unreliable data collection
and management, furthermore receiving and sending
case reports was not on time. In addition, there are
still many residents who are not aware of malaria
prevention that are seen in the sub-optimal use of
mosquito nets, high outdoor activity at night and
passive activities in the house also become risk
factors in this malaria outbreak.
In an effort to improve malaria control so that
similar outbreaks do not occur in Sorong regency, the
quality of reporting must be supported by effort to
strengthen networks that are integrated with health
offices and health facilities. Vector control programs
also need careful supervision such as submitting
procedures and circulars on clear duties related to the
implementation of health promotion on intensive
malaria prevention.
ACKNOWLEDGEMENTS
We are grateful for the research grant from Lembaga
Penelitian dan Pengabdian kepada Masyarakat
(LPPM) University of Papua.
REFERENCES
Baird, J. K. 2013. Evidence and Implications of Mortality
Associated with Acute Plasmodium vivax Malaria.
Clinical Microbiology Reviews, 26(1), 36–57.
https://doi.org/10.1128/CMR.00074-12
Bartoloni, A., and Zammarchi, L. 2012. Clinical Aspects of
Uncomplicated and Severe Malaria. Mediterranean
Journal of Hematology and Infectious Diseases, 4(1).
https://doi.org/10.4084/MJHID.2012.026
Bria, Y. P., Yeh, C.-H., and Bedingfield, S. 2021.
Significant symptoms and nonsymptom-related factors
for malaria diagnosis in endemic regions of Indonesia.
International Journal of Infectious Diseases, 103, 194–
200. https://doi.org/10.1016/j.ijid.2020.11.177
Buck, E., and Finnigan, N. A. 2023. Malaria. In StatPearls.
StatPearls Publishing.
http://www.ncbi.nlm.nih.gov/books/NBK551711/
Centers for Disease Prevention and Control. 2022..
Introduction to Public Health Surveillance.
https://www.cdc.gov/training/publichealth101/surveill
ance.html
Desita, M. Y., Riwu, Y. R., and Limbu, R. 2021. Evaluasi
Pelaksanaan Kegiatan Surveilans Malaria dalam
Mendukung Eliminasi Penyakit Malaria di Kabupaten
Kupang. Media Kesehatan Masyarakat, 3(2), 165–174.
https://doi.org/10.35508/mkm.v3i2.3199
Dhewantara, P. W., Ipa, M., and Widawati, M. 2019.
Individual and contextual factors predicting self-
reported malaria among adults in eastern Indonesia:
Findings from Indonesian community-based survey.
Malaria Journal, 18(1), 118.
https://doi.org/10.1186/s12936-019-2758-2
Diallo, M. A., Diongue, K., Ndiaye, M., Gaye, A., Deme,
A., Badiane, A. S., and Ndiaye, D. 2017. Evaluation of
ICOMESH 2023 - INTERNATIONAL CONFERENCE ON MEDICAL SCIENCE AND HEALTH
60

CareStart
TM
Malaria HRP2/pLDH (Pf/pan) Combo
Test in a malaria low transmission region of Senegal.
Malaria Journal, 16(1), 328.
https://doi.org/10.1186/s12936-017-1980-z
Directorate of Surveillance and Health Quarantine. 2023.
Pedoman Sistem Kewaspadaan Dini dan Respon
(SKDR) Penyakit Potensial KLB/Wabah. Indonesian
Ministry of Health. https://p2p.kemkes.go.id/pedoman-
sistem-kewaspadaan-dini-dan-respon-skdr-penyakit-
potensial-klb-wabah/
Elyazar, I. R. F., Hay, S. I., and Baird, J. K. 2011. Malaria
Distribution, Prevalence, Drug Resistance and Control
in Indonesia. Advances in Parasitology, 74, 41.
https://doi.org/10.1016/B978-0-12-385897-9.00002-1
Herawati, M. H., Besral, Lolong, D. B., Pracoyo, N. E.,
Sukoco, N. E. W., Supratikta, H., Veruswati, M., and
Asyary, A. 2023. Service availability and readiness of
malaria surveillance information systems
implementation at primary health centers in Indonesia.
PLOS ONE, 18(4), e0284162.
https://doi.org/10.1371/journal.pone.0284162
Indonesian Ministry of Health. 2019. Pedoman Nasional
Pelayanan Kedokteran Tatalaksana Malaria.
Indonesian Ministry of Health.
https://yankes.kemkes.go.id/unduhan/fileunduhan_161
0416186_13796.pdf
Indonesian Ministry of Health. 2023. Laporan Kinerja
Semester I Tahun 2023 Ditjen P2P. Indonesian
Ministry of Health. http://p2p.kemkes.go.id/wp-
content/uploads/2023/08/Final-LAKIP-Ditjen-P2P-
Semester-I-Tahun-2023.pdf
Kang, J.-M., Cho, P.-Y., Moe, M., Lee, J., Jun, H., Lee, H.-
W., Ahn, S. K., Kim, T. I., Pak, J. H., Myint, M. K.,
Lin, K., Kim, T.-S., and Na, B.-K. 2017. Comparison
of the diagnostic performance of microscopic
examination with nested polymerase chain reaction for
optimum malaria diagnosis in Upper Myanmar.
Malaria Journal, 16(1), 119.
https://doi.org/10.1186/s12936-017-1765-4
Menkin-Smith, L., and Winders, W. T. 2023. Plasmodium
vivax Malaria. In StatPearls [Internet]. StatPearls
Publishing.
https://www.ncbi.nlm.nih.gov/books/NBK538333/
Mosha, J. F., Lukole, E., Charlwood, J. D., Wright, A.,
Rowland, M., Bullock, O., Manjurano, A., Kisinza, W.,
Mosha, F. W., Kleinschmidt, I., and Protopopoff, N.
2020. Risk factors for malaria infection prevalence and
household vector density between mass distribution
campaigns of long-lasting insecticidal nets in North-
western Tanzania. Malaria Journal, 19(1), 297.
https://doi.org/10.1186/s12936-020-03369-4
Munthe, G. M., Nugraha, D., Mudjianto, G. P., Rohmah, E.
A., Weni, A. D. D., Salma, Z., Rossyanti, L., Fitriah,
Pusarawati, S., Utomo, B., Basuki, U., and Uemura, H.
2022. Breeding Preference and Bionomics of
Anopheles spp. At the Malarial Endemic Area, Runut
Village, East Nusa Tenggara Province, Indonesia.
Biomolecular and Health Science Journal, 5(1), 19–24.
https://doi.org/10.20473/bhsj.v5i1.35278
Nsubuga, P., White, M. E., Thacker, S. B., Anderson, M.
A., Blount, S. B., Broome, C. V., Chiller, T. M., Espitia,
V., Imtiaz, R., Sosin, D., Stroup, D. F., Tauxe, R. V.,
Vijayaraghavan, M., and Trostle, M. 2006. Public
Health Surveillance: A Tool for Targeting and
Monitoring Interventions. In Disease Control Priorities
in Developing Countries. 2nd edition. The International
Bank for Reconstruction and Development / The World
Bank.
https://www.ncbi.nlm.nih.gov/books/NBK11770/
Papilaya, M. L., Ratag, B. T., and Joseph, W. B. S. 2015.
Hubungan antara faktor perilaku dengan kejadian
malaria di wilayah kerja Puskesmas Remu Kota
Sorong. 4(2).
https://ejournal.unsrat.ac.id/index.php/kesmas/article/v
iew/12689
Sulistyawati, S., Fitriani, I., and Fitriani, I. 2020. Risk
Factor and Cluster Analysis to Identify Malaria Hot
Spot for Control Strategy in Samigaluh Sub-District,
Kulon Progo, Indonesia. Iranian Journal of Public
Health. https://doi.org/10.18502/ijph.v48i9.3024
Tangpukdee, N., Duangdee, C., Wilairatana, P., and
Krudsood, S. 2009. Malaria Diagnosis: A Brief Review.
The Korean Journal of Parasitology, 47(2), 93.
https://doi.org/10.3347/kjp.2009.47.2.93
WHO. 2021a. Global technical strategy for malaria 2016–
2030, 2021 update. WHO.
https://iris.who.int/handle/10665/342995
WHO. 2022. World Malaria Report 2022 (p. 293)
[Electronic]. World Health Organization.
https://www.who.int/teams/global-malaria-programme
WHO. 2023. WHO Guidelines for Malaria. WHO.
https://www.who.int/teams/global-malaria-programme
WHO. 2021b. Evidence-informed action to eliminate
malaria in Indonesia.
https://www.who.int/about/accountability/results/who-
results-report-2020-mtr/country-story/2021/indonesia
Clinical Features, Surveillance and Determinant Factors of Malaria Outbreak in Usili Village, Southwest Papua, Indonesia
61
