
Comparative Analysis and Prediction of Malignant Tumor Mortality
in China Based on LSTM Models
Fan Yang
School of Computer Science and Engineering, Central South University, Nan Chang, China
Keywords: Malignant Tumor, LSTM Model, Mortality Rate.
Abstract: The prediction and analysis of the mortality rate of malignant tumors is a hot topic of great importance and
urgency in the world. However, the dynamic mortality prediction model commonly used in the medical field
still has some limitations in the nonlinear structure of mortality research. Therefore, based on the survey data
of "Mortality rate of major diseases in selected urban/rural areas of China" from 2008 to 2021, this research
will utilize the Long and short-term memory networks (LSTM) model to validate the model and predict the
mortality rate in 2022. This research will also quantitatively analyze and explore the reasons for the mortality
rate differences arising from regional differences and gender differences. The prediction results show that the
mortality rate in urban areas in 2022 may increase compared with the value in 2021, while the mortality rate
in rural areas will decrease, and the difference in the trend is only reflected in the regional differences.
Furthermore, the trends in mortality rates over the years show a general decline in urban areas and an increase
in rural areas, with the urban mortality rate being lower than the rural rate after 2020, and the male mortality
rate being much higher than the female mortality rate.
1 INTRODUCTION
Malignant tumors, one of the most dangerous diseases
nowadays, always occupy the first place on the list of
causes of death in many countries (Sung et al. 2021).
Rapid economic development, increasing
environmental pollution, and changes in people's
lifestyles have increased the incidence of malignant
tumors. China National Cancer Center released a new
report on malignant tumor statistics, which reveals
that the number of new cases of malignant tumors in
China reached 4,064,000 in 2016, and the total
number of deaths reached 2,414,000 (Rongshou et al.
2022). The development of society and the economy
are now seriously hampered by malignant tumors,
which also pose a serious threat to people's lives and
health. The importance and urgency of malignant
tumor-related research have become self-evident. The
mortality rate is an important index in malignant
tumor-related research, and the prediction and analysis
of malignant tumor mortality rate is also a hot topic.
Commonly used mortality prediction models are static
and dynamic mortality prediction models. Currently,
the dynamic mortality prediction model represented by
the Lee-Carter model is commonly used in the medical
field. However, the dynamic mortality prediction
model can only portray the linear relationship between
the influencing factors and the mortality rate, and there
are some limitations in the nonlinear structure of the
mortality rate research (Gang et al. 2022). When it
comes to machine learning algorithms, the nonlinearity
of the kernel function and activation function can
realize the nonlinear mapping of the data, which
enables machine learning algorithms to have excellent
nonlinear learning ability. Moreover, for the time series
data, the Long and short-term memory networks
(LSTM) model always performs excellently. In this
research, the prediction of malignant tumor mortality
and the analysis of regional and gender differences will
help understand and predict the development trend of
malignant tumors in China, explore the sore points of
malignant tumor deaths in China, and provide targeted
preventive suggestions to the public from a multi-level
perspective.
Based on the data from the "Mortality rate of major
diseases in selected urban/rural areas of China" from
2008 to 2021, this research will validate the model and
predict the mortality rate of malignant tumors in
selected urban/rural areas of China in 2022 with the
LSTM model. The paper will also analyze the
178
Yang, F.
Comparative Analysis and Prediction of Malignant Tumor Mortality in China Based on LSTM Models.
DOI: 10.5220/0012816200003885
Paper published under CC license (CC BY-NC-ND 4.0)
In Proceedings of the 1st International Conference on Data Analysis and Machine Learning (DAML 2023), pages 178-183
ISBN: 978-989-758-705-4
Proceedings Copyright © 2024 by SCITEPRESS – Science and Technology Publications, Lda.
differences in mortality rate by region and gender and
the reasons for these differences. This study might be
helpful for the Chinese public and medical institutions
to understand and treat malignant tumors. This
research will first use the data of the previous 12 years
to predict the mortality rate in 2020 and 2021, thus
verifying the LSTM model's applicability. Then, the
LSTM model will be used to predict the total mortality
rate in urban and rural areas and the mortality rate of
each gender in 2022. Furthermore, the differences in
mortality rate due to regional and gender differences
will be quantitatively analyzed and the reasons for
these differences will be investigated.
2 METHOD
2.1 Data Source
The data for this research come from a survey
"Mortality rate of major diseases in selected
urban/rural areas of China", published in the China
Statistical Yearbook by the National Bureau of
Statistics of the People's Republic of China (NBS).
The survey utilized a stratified probability sampling
method proportional to population size. Several large
cities and small and medium-sized cities were selected
as urban respondents, and several municipalities and
county-level cities were selected as rural respondents.
The survey conducted gender-specific mortality rate
and death cause statistics on the top 10 major diseases
among Chinese residents in recent years according to
the International Classification and Statistics
Standard-10 (ICD-10) for Diseases. Based on the
theme of this study and the distribution of causes of
death, this study excluded diseases that were not
continuously listed as the top 10 major diseases in the
survey, as well as diseases with small mortality values
ranging from 0.01% to 1%. This study will use the
mortality rate value in selected urban/rural areas from
2008 to 2021 as research data. Since malignant tumors
account for the highest proportion of causes of death
among the ten major diseases throughout the year, and
the mortality rate is also relatively high, it is of great
research significance and representativeness.
The data of this study include six indicators,
including the total mortality rate of malignant tumors,
male mortality rate, and female mortality rate in urban
and rural areas, etc.
2.2 Model
Long and short-term memory networks are a specific
kind of recurrent neural network (RNN). RNN is the
most natural architecture for sequential data due to the
chaining feature. However, since the same function
will be combined with itself many times, RNN will
face the problem of gradient vanishing or gradient
explosion and long-term dependency during training.
The long-term dependence issue brought on by RNN
will be partially resolved by Hochreiter’s unique unit
design of the LSTM model, which also effectively
realizes the modeling of time-series data (Hochreiter
and Schmidhuber 1997). RNN models all have some
repeating neural network modules, the traditional RNN
only simply repeats a single neural network layer,
while the LSTM repeats module comprises four
interacting layers, including three sigmoid layers and
one tanh layer, whose interactions tend to be very
specific.
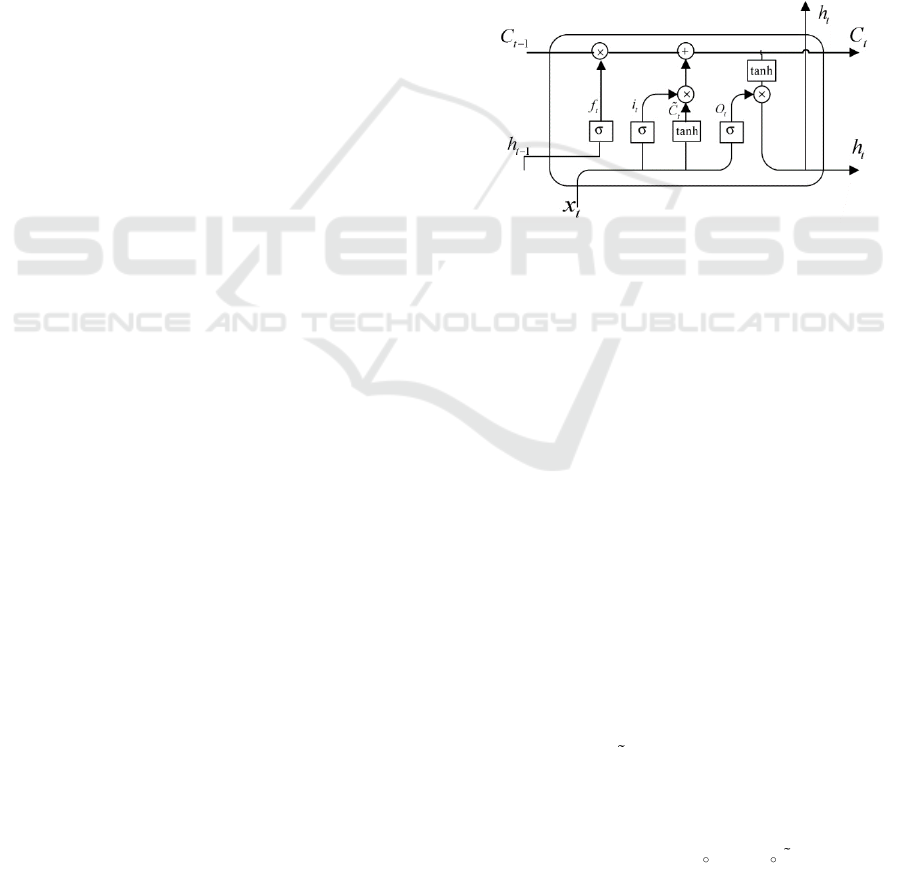
Figure 1: Cell of LSTM model.
As shown in Fig. 1, each LSTM cell contains three
gate structures, the forgetting gate(f
t
), the input gate(i
t
),
and the output gate(o
t
), as well as a cell state to
maintain and update the state (Han et al 2021). Where
the forget gate is used to choose which information
from the cell state to discard, the structure reads the
previous output h
t-1
and the current input x
t
, then
conducts a Sigmoid nonlinear mapping and outputs a
vector f
t
, which can be described as:
( )
1t fh t fx t f
f W h W x b
−
= + +
()
where W denotes the weights and b denotes the bias.
What information will remain in the cell state is
determined by the input gate. It is divided into two
sections. The sigmoid layer will first determine which
values to update; the tanh layer will then generate a
new vector of candidate values C
t
and add it to the cell
state. The relationship is stated as follows:
( )
1t ih t ix t i
i W h W x b
−
= + +
()
( )
1
tanh
t ch t cx t c
C W h W x b
−
= + +
()
Next, the cell state will be updated from C
t-1
to C
t
as an input to the next cell, and the relationship can be
expressed as:
1t t t t t
C f C i C
−
=+
()
Comparative Analysis and Prediction of Malignant Tumor Mortality in China Based on LSTM Models
179
where
denotes the Hadamard product.
The output gate is in charge of calculating the
output value depending on the cell state. To begin, use
a sigmoid layer to determine which part of the cell
state will be output. Simultaneously, the cell state is
processed by the tanh layer and multiplied by the
output of the sigmoid gate, generating the value h
t
,
which is important for the computation of the
following cell. This relationship can be stated as
follows:
( )
1t oh t ox t o
o W h W x b
−
= + +
()
( )
tanh
t t t
h o C=
()
3 RESULT
3.1 Verification
To validate the LSTM model's applicability for
forecasting malignant tumor mortality, this research
will use the malignant tumor mortality data of urban
areas from 2008 to 2019 to predict the corresponding
mortality rates in 2020 and 2021. The predictions will
also be compared with the true values to evaluate and
validate the model's applicability based on Mean
Squared Error (MSE). The models for applicability
validation will include five mainstream regression
prediction models: random forest, linear regression,
decision tree, support vector machines (SVM), and
LSTM. The prediction results are shown in Table 1:
Table 1: Mse of the Models.
Mode
l
Rando
m
Forest
Linear
Regressio
n
Decisio
n
Tree
SVM
LST
M
MSE
7.012
9.179
1.542
8.32
1
0.813
The MSE obtained by the LSTM model is 0.813,
whose magnitude is much smaller than the range of
prediction values from 150 to 180, indicating good
accuracy. Meanwhile, the MSE value of the LSTM
model is much smaller than the corresponding values
of the other four mainstream regression prediction
models, which also indicates that the LSTM model
has a more excellent performance than the other
models in this research topic. Thus, it can be verified
that the LSTM model is appropriate for the following
prediction of malignant tumor mortality.
3.2 Prediction
3.2.1 Prediction of Urban and Rural Total
Mortality Rates in 2022
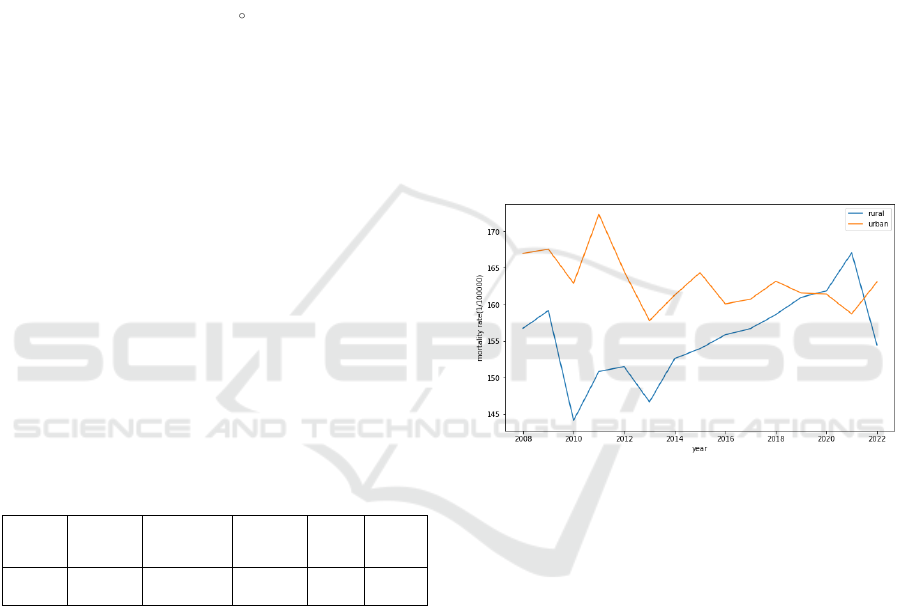
In this research, the mortality rate of malignant
tumors in urban and rural areas in 2022 will be
predicted using the LSTM model. The predicted
value of the total malignant tumor mortality rate in
the urban region is 163.076, which is an increase of
2.76% compared to 2021. The predicted value of the
total mortality rate for rural regions in 2022 is
154.456, which is a decrease of 7.54% compared to
2021. At the same time, urban regions' forecasts are
5.5% higher than rural regions' forecasts. The trend of
the total mortality rate of malignant tumors in urban
and rural regions from 2008 to 2022 is shown in Fig.
1, where the horizontal coordinate indicates the year
and the vertical coordinate is the mortality rate
(1/100,000):
Figure 2: Overall urban and rural mortality rates (Picture
credit: Original).
Urban areas show a general downward trend in the
total mortality rate, with a predicted decrease of 2.33%
in 2022 compared to 2008. Rural areas show a more
mixed picture, with a 1.45% decrease in 2022
compared to 2008. Comparing the mortality rate of
urban areas with the rural ones, the mortality rate of
urban areas was higher than the rural areas until 2020,
after which it reversed. Furthermore, between 2021
and 2022, urban and rural regions are expected to
follow opposing trends, with urban areas rising and
rural areas falling.
3.2.2 Predictions of Male/Female Mortality
Rates in Urban and Rural Areas in
2022
Urban Area: The predicted male mortality rate for the
urban area is 204.753, an increase of 2.33% from
2021. While the female mortality rate for the urban
DAML 2023 - International Conference on Data Analysis and Machine Learning
180
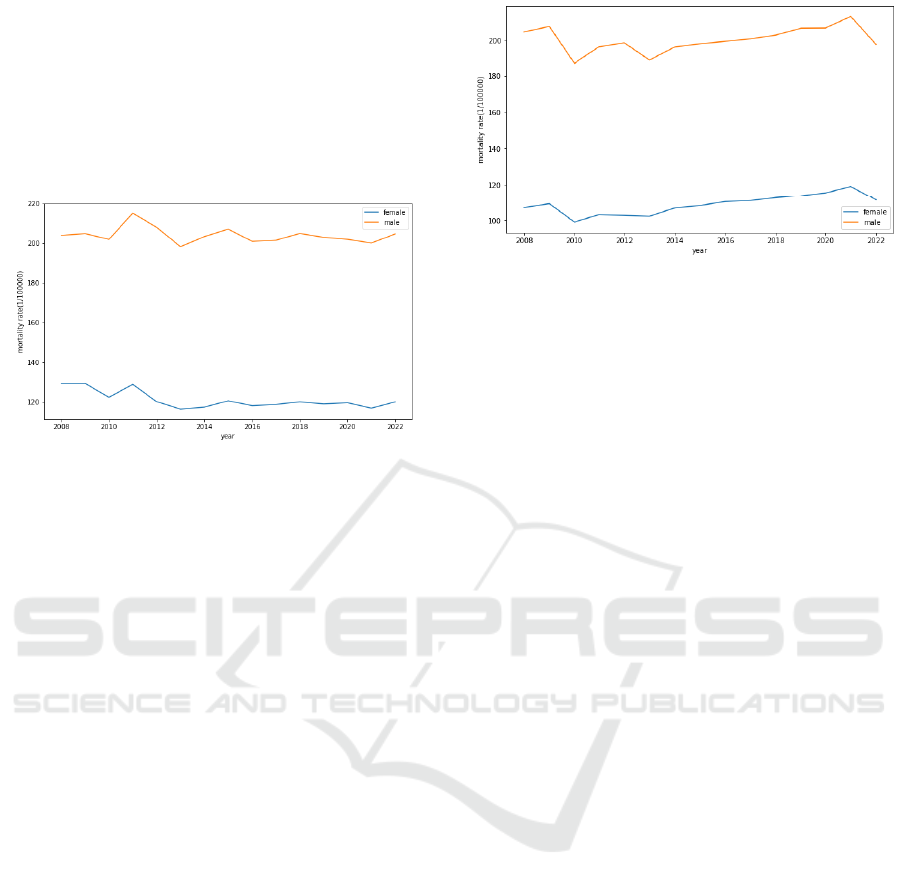
area in 2022 is predicted to be 119.984, an increase of
2.76% from 2021. At the same time, the predicted
value of the male mortality rate is 70.65% higher than
the predicted value of the female mortality rate. The
trend of male and female mortality rates in the urban
area from 2008 to 2022 is shown in Figure 2, where
the horizontal coordinate indicates the year and the
vertical coordinate is the mortality rate (1/100,000):
Figure 3: Male/female mortality rates in urban areas
(Picture credit: Original).
Trends in male mortality rates are generally
consistent with those of female mortality rates, both
of which are on a downward trend. In the case of men,
the predicted value of the mortality rate in 2022 is
0.37% lower than in 2008. The predicted value of the
female mortality rate in 2022 is 7.15% lower than that
in 2008. Male mortality is much greater than female
mortality, and both are predicted to follow a similar
upward trend between 2021 and 2022.
Rural Area: The predicted male mortality rate in
rural areas is 197.797, which is 7.19% lower than the
value in 2021. The predicted female mortality rate in
rural areas in 2022 is 111.543, which is 6.35% lower
than that in 2021. At the same time, the predicted
value of the male mortality rate is 77.33% higher than
the predicted value of the female mortality rate. The
trend of male and female mortality rates in rural areas
from 2008 to 2022 is shown in Figure 3, where the
horizontal coordinate indicates the year and the
vertical coordinate is the mortality rate (1/100,000).
Trends in male mortality rates are generally
consistent with those of female mortality rates, both of
which are on an upward trend. In the case of males,
the predicted value of the mortality rate in 2022 is
3.32% lower than in 2008. The female mortality rate
is predicted to increase by 4.19% in 2022 compared to
2008. The male mortality rate is much higher than the
female mortality rate, and both are predicted to follow
a similar downward trend between 2021 and 2022.
Figure 4: Male/female mortality rates in rural areas (Picture
credit: Original).
4 DISCUSSION
The predicted trends in mortality rates for males and
females in the different regions are consistent with the
predicted trends of the total mortality rates in the
corresponding regions, and the differences in the
trends are only related to the differences in regional
distribution, and not so much to the differences in
gender. In general, the mortality rate in urban areas is
decreasing, probably due to the development of
medicine and increased health awareness. In rural
areas, the mortality rate is on the rise, probably
because the rural population aging problem is very
serious (Rongshou et al 2018). Until 2020, the total
mortality rate in urban regions was greater than in
rural regions, but this trend reversed after 2020. This
might be associated with the Human Development
Index (HDI), a comprehensive assessment of regional
human development in terms of health, education,
and income, with free human development as the core
concept (UNDP 1990). Research has shown that the
HDI index is closely related to malignant tumors, and
Khazaei discovered a positive correlation between the
incidence of prostate cancer and the HDI index, and a
negative correlation between the standardized death
rate and the HDI index (Khzazei et al 2016). The HDI
index in urban areas is higher than the value in rural
areas, and rural areas lack medical services and
cancer preventive understanding. All these factors
can lead to the reversal of the mortality rate in rural
areas and urban areas. The government can publicize
cancer prevention in rural areas and promote
healthcare reform to alleviate the imbalance of
healthcare resources.
As for gender differences, the mortality rate of
men is much higher than that of women, which may
be due to the following reasons: (1) males and women
have distinct physiological structures, and women
Comparative Analysis and Prediction of Malignant Tumor Mortality in China Based on LSTM Models
181

have greater estrogen levels than males, which may
be a preventive factor for the development of some
malignancies (Xiyi 2017); (2) the awareness of tumor
prevention of women is stronger than that of men (Ni
et al2019); (3) the level of exposure to risk factors of
men is higher than that of women. For example,
tobacco consumption and alcoholism are higher in
men than in women. Chronic disorders such as
hypertension and diabetes mellitus are also more
prevalent in males than in women (Ye et al 2016 &
Zengwu et l 2018). Moreover, there are differences in
the cancer spectrum of different genders, for example,
breast cancer and thyroid cancer are highly prevalent
in women but have a better prognosis, whereas
digestive tract cancers are highly prevalent in men but
have a poorer prognosis, which may lead to a higher
burden of malignant tumors in men than in women
(Wei et al 2021). Therefore, men should raise their
awareness of cancer protection and reduce their
exposure to harmful substances such as tobacco and
alcohol, which can effectively prevent cancer.
This research still has some limitations. First, the
LSTM model requires a large amount of training data
for training and prediction. Still, this research only
studied the mortality-related data of malignant tumors
during the 14-year period from 2008 to 2021, which
is a small amount of data, and it may lead to
inaccurate predictions. Second, the focus of the
analysis in this research was mainly on regional and
gender differences, and many other influencing
factors were not taken into account, such as age,
cancer spectrum distribution, and other factors. In the
future, the model and analysis can be further refined
in the above aspects and more detailed data are also
indispensable to facilitate in-depth research on this
topic.
5 CONCLUSION
The predictions in this research indicate that the total
mortality rate and the male and female mortality rates
in urban areas are likely to increase in 2022, whereas
the corresponding mortality rates in rural areas are
likely to decrease, and the differences in the trends are
only related to regional differences. Second, the
research analyzed the differences in the mortality rate
by region and gender. For regional differences, the
mortality rate in urban is declining, while the
mortality rate in rural regions is growing, and after
2020, the value of the mortality rate in urban began to
be lower than the corresponding mortality rate in rural
areas. Possible explanations for the difference include
a higher HDI index in urban regions, a deeper
understanding of tumor prevention in urban areas
than in rural ones, and a more serious population
aging problem in rural areas. The difference by
gender is reflected in the fact that the mortality rate
for men is much higher than that for women. The
reasons for this difference may include the different
physiological structures of men and women, the
higher awareness of tumor prevention in women than
in males, the higher level of exposure to risk factors
in men than in women, and the difference in the
cancer spectrum. The analysis of the malignant tumor
mortality rate, regional differences, and gender
differences in this study can help to understand and
predict the development trend of malignant tumors in
China, uncover the pain points of malignant tumor
deaths, and provide targeted preventive advice to the
public from a multi-level perspective. However, this
study also suffers from the limitations of too little data
and not enough comprehensive investigation of
factors. In the future, this research should make use
of more sufficient data and improved models to
include more factors into the investigation and
conduct a multi-factor comprehensive analysis.
REFERENCES
H. Sung, J. Ferlay, R. L. Siegel, et al., “Global cancer
statistics 2020: GLOBOCAN estimates of incidence
and mortality worldwide for 36 cancers in 185
countries,” CA: a cancer journal for clinicians, vol. 71,
pp. 209-249, 2021.
Z. Rongshou, Z. Siwei, Z. Hongmei, et al., “Cancer
incidence and mortality in China, 2016,” Journal of the
National Cancer Center, vol. 2, pp. 1-9, 2022.
Y. Gang, Y. Yanping, S. Chao, “Prediction of Mortality of
Elderly Population with an Improved AE-LSTM
Model,” Mathematical Theory and Applications, vol.
42, pp. 100, 2022.
S. Hochreiter, J. Schmidhuber, “Long short-term memory,”
Neural computation, vol. 9, pp. 1735-1780, 1997.
G. Han, S. Renju, M. Li, L. Wenyu, “A heart failure
mortality prediction model based on AB-CNN-
BILSTM,” Computer Applications and Software, vol.
38, pp. 37-42, 2021.
Z. Rongshou, G. Xiuying, L. Xueting, et al., “Analysis on
the trend of cancer incidence and age change in cancer
registry areas of China, 2000 to 2014,” Chinese journal
of preventive medicine, vol. 52, pp. 593-600, 2018.
UNDP, “Human development report 1990,” New York and
Oxford: Oxford University Press, pp. 10, 1990.
S. Khazaei, S. Rezaeian, E. Ayubi, et al., “Global prostate
cancer incidence and mortality rates according to the
human development index,” Asian Pacific Journal of
Cancer Prevention, vol. 17, pp. 3791-3794, 2016.
J. Xiyi, H. Yunqing, Y. Ding, L. Qilong, C. Kun, J.
Mingjuan, “Disparities of sex on cancer incidence and
DAML 2023 - International Conference on Data Analysis and Machine Learning
182

mortality in Jiashan county, Zhejiang province, 1990-
2014,” Chinese journal of Epidemiology, vol. 38, pp.
772-778, 2017.
W.Ni, H. KaiYong, Y. Li, “Analysis on health literacy and
its influencing factors about cancer prevention and
control among urban residents in Guangxi,” Chinese
Journal of Disease Control & Prevention, vol.23, pp.
711-716, 2019.
R. Ye, Y. Qinghua, X. Jiying, et al., “Epidemiology of
diabetes in adults aged 35 and older from Shanghai,
China.” Biomedical and Environmental Sciences, vol.
29, pp. 408-416, 2016.
W. Zengwu, C. Zuo, Z. Linfeng, et al., “Status of
hypertension in China: results from the China
hypertension survey, 2012–2015,” Circulation, vol. 137,
pp. 2344-2356, 2018.
C. Wei, C. Hongda, Y. Yiwen, L. Ni, C. Wanqing,
“Changing profiles of cancer burden worldwide and in
China: a secondary analysis of the global cancer
statistics 2020,” Chinese medical journal, vol. 134, pp.
783-791, 2021.
Comparative Analysis and Prediction of Malignant Tumor Mortality in China Based on LSTM Models
183
