
Short-Term and Long-Term Readmission Prediction in Uncontrolled
Diabetic Patients using Machine Learning Techniques
Monira Mahmoud
1
, Mohamed Bader
1
and James McNicholas
1,2
1
University of Portsmouth, Buckingham Building, Lion Terrace, Portsmouth PO1 3HE, U.K.
2
Queen Alexandra Hospital, Portsmouth Hospitals NHS Trust, U.K.
Keywords: Machine Learning, Data Mining, Diabetes, Uncontrolled Diabetes, Readmission.
Abstract: Diabetes is a chronic disease and major health problem which leads to many complications if not managed
probably. Hyperglycemia, or raised blood sugar, is a common effect of Uncontrolled diabetes that may leads
overtime to serious complications, especially in the nerves and blood vessels. As well as leads to repeated
hospital admission. The main purpose of this study is to help clinicians to improve healthcare of uncontrolled
diabetic patients through using machine learning as a tool in decision making, consequently this will improve
patient care and reduce the readmission which considered a medical quality measurement and cost reduction
objective. This study aims to predict the hospital readmission of the uncontrolled diabetic patient who is
considered more susceptible to developing life-threatening diabetes complications and based on the Diabetes
130-US hospitals dataset. Several machine learning employed to predict the short term (within 30 days), and
both short and long-term readmission (within or after 30 days) of uncontrolled diabetic patient. As expected,
the results are in line with other research in the literature. For the first scenario of whole readmission
prediction, our model achieved a better accuracy of 64.5 % with SVM and attribute selection and for the
second scenario, RF achieved the highest accuracy of 86.38 % which still come in context with other research
in the literature.
1
INTRODUCTION
Diabetes Mellitus (DM) is a major public health
problem, Worldwide, 415 million adults—or one in
every eleven—are projected to have diabetes. By
2040, there will likely be 642 million individuals
living with diabetes worldwide. (diabetes UK
organization). According to the world health
organization, the number of people with diabetes rose
from 108 million in 1980 to 422 million in 2014.
Also, within the UK, there are 3.5 million diabetics,
up from 1.4 million in 2000. Hospital readmission is
an episode when a patient who has been discharged
from the hospital is readmitted again within a
specified period. Indeed, the burdens of inpatient
diabetes is huge, growing, and expensive, and
readmission can greatly increase these burdens.
Hospital readmission is used as a measure of a
hospital’s ability to provide quality service and
patient care. Also, hospital readmission is often used
as a benchmark, since a high proportion of
readmission is likely to be preventable if the hospital
provided adequate care. Thus, the reduction of
readmission is a medical quality measurement and
cost reduction objective (Battineni et al, 2020). In
particular, uncontrolled diabetes implies high blood
sugar levels over a prolonged time even if the patient
on treatment, it is diagnosed when HbA1c is higher
than 6.5. According to Diabetes UK Organization,
HbA1c is one of the tests used to diagnose and
monitor the diabetic patient, known as glycated
hemoglobin, and refers to average blood glucose
levels for the last two to three months. For a diabetic
patient, an ideal HbA1c level is 48mmol/mol (6.5).
Uncontrolled diabetes can result in hyperglycemia,
which damages many of the body’s systems,
particularly the nerves and blood vessels, over time.
Nearly every organ in an uncontrolled diabetic
patient’s body can suffer a toll from diabetes,
including, the eyes, kidneys, nerves, heart, blood
vessels, gastrointestinal tract, teeth, and gum.
Interestingly, on a daily basis, hospitals generate a
great deal of data, but that information usually
remains as data that is not always converted into
knowledge. Through the application of ML
techniques, it is possible to uncover hidden
relationships or patterns among the data and convert
them into knowledge that can be used by healthcare
680
Mahmoud, M., Bader, M. and McNicholas, J.
Short-Term and Long-Term Readmission Prediction in Uncontrolled Diabetic Patients using Machine Learning Techniques.
DOI: 10.5220/0011926000003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 5: HEALTHINF, pages 680-688
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)

professionals to make better decisions. Prediction of
readmission could play a role in early intervention for
the management of the uncontrolled diabetic patient
who is considered a host of complications if not
managed properly. Hence, this study aims to apply a
set of machine learning techniques to predict
uncontrolled patient readmission. Therefore,
predicting readmission will ultimately allow hospitals
to better calculate and assess the quality of care.
This study applies machine learning prediction
tools for a specific group of diabetic patients
(uncontrolled patients), based on UCI diabetes
dataset. Moreover, it considers different scenarios for
prediction (i.e. short-term or short- and long-term
readmission prediction) with feature selection. Six
supervised ML technique used for the prediction (RF,
NB, KNN, Ada-Boost, SVM, bagging, and NN) of
readmission. The study benefits from two scenarios.
The first scenario (i.e. using the first subset of data)
predicts the readmission event, while the second
scenario (using subset data two) predicts of the early
readmission (readmission within 30 days).
Experiments employed for both sub data sets with and
without attribute selection. Results shows that, in the
first scenario (all readmission events), SVM achieved
the highest accuracy of 64 % and NB achieved the
best AUROC area of 0.65. In the second scenario
(early readmission only), RF achieved the highest
accuracy of 86 % and the best AUROC area of 0.63.
Our goal within the healthcare prospective is to
use data mining, data analytical and ML to predict If
the uncontrolled diabetic patient will be readmitted at
any time point, as a first scenario or If will be
readmitted in a short-term time (within 30 days), as a
second scenario.
This research aims to develop a model that can
accurately predict the readmission of uncontrolled
diabetic patient. Also, to provide a better
understanding of the readmitted patient
characteristics through descriptive analysis.
Therefore, using ML for prediction of uncontrolled
diabetics readmission will boost early intervention,
and consequently lead to better disease management
and cost reduction
The paper is structured as follows: Section 2
presents the literature review on machine learning
(ML) and diabetes. Section 3 discusses the material
and methods. Section 4 provides the results, and
Section 5 provides conclusion.
2
LITERATURE SURVEY
A large and growing body of literature has
investigated the application of machine learning
algorithms in the healthcare domain ((Battineni et al,
2020), (Kumar et al, 2018), (Kohli et al, 2018)), (Ali
et al, 2020). In particular, a stream of research
examines the accuracy of machine learning
algorithms in predicting hospital readmission of
diabetic patients. The following section discuss the
existing literature related to this paper.
2.1 Diabetes and Machine Learning
Diabetes is linked to micro and macrovascular
diseases such as heart disease, kidney failure, eye
disease, and amputation, which also leads to a high
rate of repeated admission of diabetic patients.
Moreover, it is fast becoming a key instrument in
complicating other unrelated medical conditions like
infections, accidents, and surgery. For instance, the
United States (US) health system endures a
significant economic burden for diabetes care. This
cost reached about 327 billion dollars in 2017
(Kavakiotis et al 2017). Nevertheless, the cost of
diabetes is not directly related to the diagnosis and
management of diabetes itself but also costs
generated by long-term complications and their
economic and social consequences (Alamer et al,
2019).
Furthermore, uncontrolled diabetes, if not
managed properly, often leads to biochemical
imbalances that can cause acute life-threatening
events and hospitalizations. Evidently, the
uncontrolled diabetic patient is nine times higher risk
of admission (Boutayeb et al, 2004), three times more
susceptible to developing severe periodontitis (Hu et
al ,2019), much greater risk for presenting with later
stages of diabetic retinopathy, other rare diabetic
ocular complications, including glaucoma, cataract,
and dry eye disease (Eldarrat et al ,2011). Extent
research links uncontrolled diabetes with substantial
mortality and cardiovascular disease burden (Alamer
et al, 2019) and increases the risk of peroperative
complication (Threatt et al ,2013).
Therefore, predicting readmission will ultimately
allow hospitals to better calculate and assess the
quality of care they provide to their patients (Navarro-
Pérez et al ,2018). The readmission of an individual
with uncontrolled diabetes falls into the Potentially
Preventable Readmission (PPRs) category. Since
ambulatory care (outpatient care) plays an
important
role in diabetes management, most hospitalizations
with uncontrolled diabetes are a direct reflection of
the quality of primary health care received outside of
hospitals (Kim et al, 2010). Accordingly, the Agency
for Healthcare Research and Quality (AHRQ)
Short-Term and Long-Term Readmission Prediction in Uncontrolled Diabetic Patients using Machine Learning Techniques
681

selected uncontrolled diabetes as a prevention quality
indicator (PQI) where hospitalization would be
decreased through timely and appropriate ambulatory
care ((Pujianto et al ,2019), (Kim et al, 2007)).
Machine learning (ML) is a subclass of artificial
intelligence technology, where algorithms process
large data sets to detect patterns, learn from them, and
execute tasks autonomously without being instructed
on exactly how to address the problem. There is
ample evidence on the rapid increase in Machine
learning applications in disease prediction and
diagnosis ((Battineni et al,2020), (Kumar et al,2018),
(Kohli et al, 2018) and (Ali et al,2020)). Thus, using
machine learning to predict the readmission of
diabetic patients will play a role in improving the
healthcare system by decreasing the negative
consequences related to diabetes readmission.
In the context of diabetes, ML methods have been
used to detect, predict, and diagnose i.e. bio-marker
Prediction and Diagnosis in DM (Farajollahi etal
,2021), Diabetic Complications (Dagliati et al,2018),
Drugs and Therapies (Donsa et al, 2015), Genetic
Background and Environment (Urban et al, 2018),
and Health Care Management which includes the
readmission prediction (Sharma et al ,2019). An
example, Chaki et. al (2020) surveyed 107 papers that
addressed the application of machine learning and
artificial intelligence techniques in DM detection,
diagnosis, and self-management. Likewise, Dagliati
et. al (Dagliati et al., 2018) provides empirical
evidence on the importance of ML in predicting the
complications of diabetes.
2.2 Related Work
Several studies used the UCI diabetes dataset for the
purpose of diabetic patient readmission prediction.
However, the results are mixed due to the variation in
the data prepossessing and the used ML algorisms.
Bhuvan et. al studies both short-term and long-term
readmission as two scenarios (Bhuvan et. al,2016).
The first scenario considered the short-term
readmission versus all readmission cases. The second
scenario combined all the readmission cases versus
non-readmitted cases. They found that RF was
optimal for this task, compared to NB, Ada-Boost,
and NN. Moreover, they employed an ablation study
to identify risk factors and association rule mining to
identify the association across critical risk factors.
They found that the number of inpatient visits,
discharge disposition, and admission type are the
most important for identifying the high risk patient.
Proposing an ensemble model and cluster
analysis, Pham et al (Pham et al,2019), investigate the
whole readmission events. the final ensemble model
was created using the five best models, which were
chosen from a pool of 15 models. The final ensemble
reaches a 56 % sensitivity while maintaining a 63.5
% accuracy. Using cluster analysis, they identified
four unique patient groupings. Their results suggest
that patients who have had previous in-patient visits
or who received a large amount of treatment during
their most recent visit were shown to be more likely
to be readmitted.
Addressing short-term readmission, Al-Ars et al
(Al-Ars et al, 2022), Farajollahi et al (Farajollahi et
al,2021), Sharma et al (Sharma et al ,2019) and Neto
et al (Neto et al,2021) explored the accuracy of
alternative predictors and the attributes selections for
predicting rea mission of diabetic patients.
Sharma et al (Sharma et al ,2019) investigate the
prediction of short-term readmission using RF, LR,
XGBoost, Adaboost and DT. They concluded that
random forest achieved t highest accuracy of 94. They
also pointed out the most important 10 attributes
which contribute mostly to the hospital readmission
of a diabetes patient in case of using RF an DT
algorisms, However, the handling out of the
prediction attribute not defined.
Furthermore, Al-Ars et al (Al-Ars et al, 2022)
studies prediction of the short-term readmission
based on the measurement of HbA1c and the primary
diagnosis using LR, NB, J8 and comparing the results
with and without using t discretization step. They
found that the discretization o numerical attributes
step improves the performance of N into 93.51.
Applying principal component analysis (PCA) for
feature selection, Farajollahi et al (Farajollahi et
al,2021) identified three scenarios of attribute
selection. In This paper, they employed RF, DT,
XGBoost, KNN, AdaBoost, and Deep learning to
predict the short-term readmission and found that dee
learning achieved the highest accuracy of 86.8%.
However, the handling out of the prediction attribute
not defined. the study showed that a machine learning
model’s effectiveness depends on the choice of the
prediction model, the numb of selected features, and
the number” k” for k-fold validation.
Furthermore, using six different scenarios based
on attribute selection, Neto et al (Neto et al,2021)
considered the short-term readmission, using RF, J48,
NB, IBK, and MLP algorithms. Comparing
alternative scenarios, they documented that the best
performance is for the RF with an accuracy of 0,898
in the case of the scenarios with the highest number
of attributes.
CCH 2023 - Special Session on Machine Learning and Deep Learning for Preventive Healthcare and Clinical Decision Support
682
3
MATERIALS AND METHODS
3.1
Materials
This study is based on a dataset obtained from the
UCI machine learning repository about diabetic
patients (Dua and Graff,2019). The data set contains
about 100,000 instances and it includes 55 features
from 130 hospitals in the United States for10 years
(1999-2008). the attributes describing the diabetic
encounters, including demographics, diagnoses,
diabetic medications, number of visits in the year
preceding the encounter, and payer information.
3.2 Methodology
This research will follow The CRoss Industry
Standard Process for Data Mining (CRISP-DM)
methodology. The CRISP-DM steps will be
described in details next. For the data preparation
phase of this study, Excel used for data preparation
and WEKA for the Modelling and Evaluation.
Excel’s usability and the number of classifiers
available by WEKA made it the ideal tool for this
analysis.
A. Business Understanding
As a measure of a hospital’s ability to provide quality
service and care, readmissions are often used as a
benchmark since most readmissions can be prevented
if patients receive adequate treatment. In addition to
being a quality indicator of healthcare systems,
readmissions are also a financial burden, about 3.3
million readmissions were reported in the United
States after 30 days, according to the Agency for
Healthcare Research and Quality (AHRQ). The
burden of inpatient diabetes is huge, growing, and
expensive, and readmission can greatly increase this
burden. Nevertheless, reducing readmission rates for
diabetics could significantly reduce medical costs
while improving care outcomes. The reduction of
readmission is a medical quality measurement and
cost reduction objective (Battineni et al,2020). As
well as the uncontrolled diabetic patent is considered
a host of diabetes complications which is considered
a cost burden as well. As a result, predicting cases of
uncontrolled diabetes patients who are likely to have
hospital readmission is the project’s commercial goal
in order to help decrease the readmission rate.
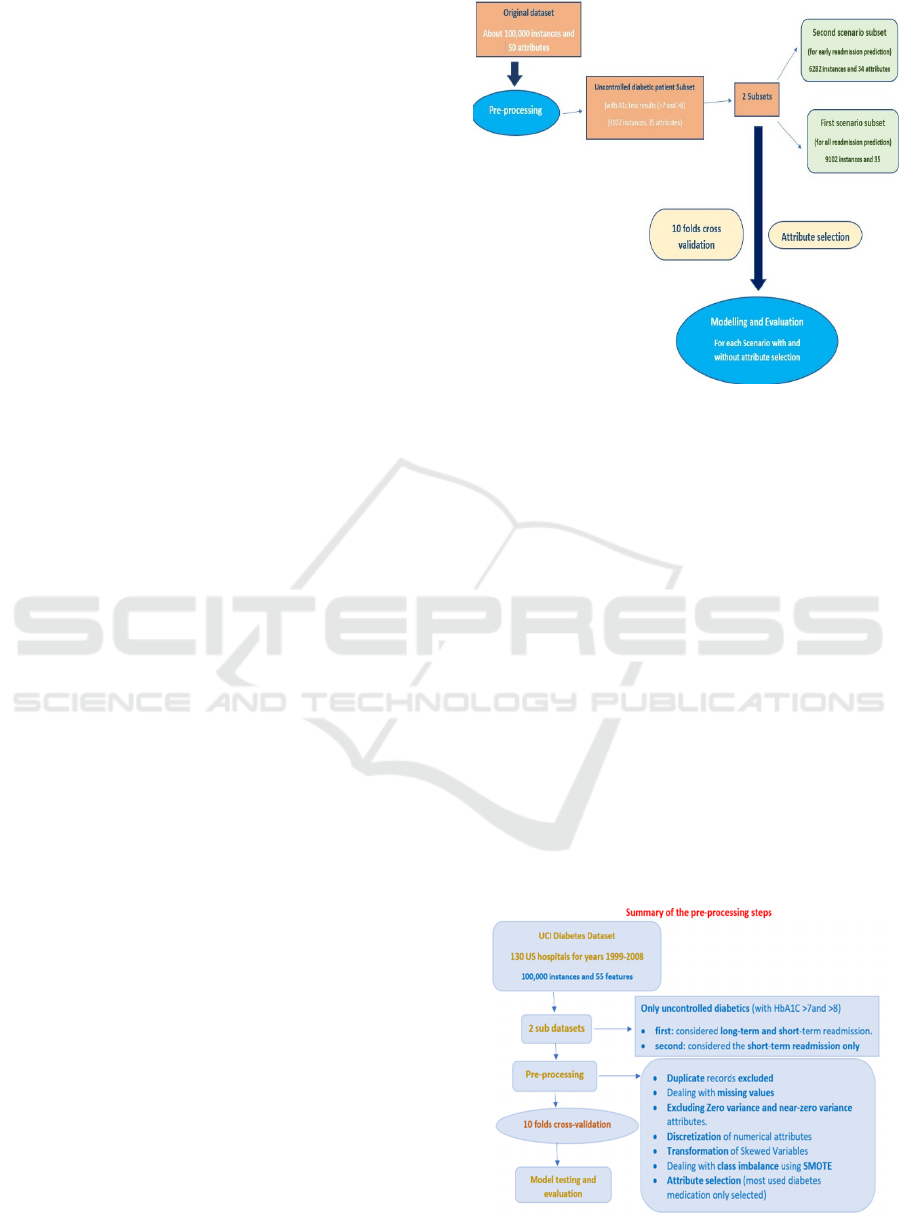
This graph shows the summary of this research
methodology.
Figure 1: Methodology.
B. Data Understanding
This study is based on a data set obtained from the
UCI machine learning repository about diabetic
patients (Dua and Graff,2019). The dataset contains
about 100,000 instances and it includes 50 features
from 130 hospitals in the United States for 10 years
(1999-2008). the attributes describing the diabetic
encounters, including demographics, diagnoses,
diabetic medications, number of visits in the year
preceding the encounter, and payer information. The
full list of the features and their description is
provided in Table1 (
Strack
et al, 2014).
C. Data Preparation
To ensure that the data is suitable to be used in the
various models, the following data prepossessing
methods are applied. Figure 2 shows a summary of
the prepossessing steps.
Figure 2: Summary of the prepossessing steps.
Short-Term and Long-Term Readmission Prediction in Uncontrolled Diabetic Patients using Machine Learning Techniques
683
Table 1: Data description.
Feature name Type Description and Values %
missing
Encounter ID Numeric Unique identifier of an encounter 0%
Patient number Numeric Unique identifier of a patient 0%
Race Nominal Values: Caucasian, Asian, African American, Hispanic, and other 2%
Gender Nominal Values: male, female, and unknown/invalid 0%
Age Nominal Grouped in 10-year intervals: 0, 10), 10, 20), …, 90, 100) 0%
Weight Numeric Weight in pounds. 97%
Admission type Nominal Integer identifier corresponding to 9 distinct values, for example, emergency, urgent,
elective, newborn, and not available
0%
Discharge disposition Nominal Integer identifier corresponding to 29 distinct values, for example, discharged to
home, expired, and not available
0%
Admission source Nominal Integer identifier corresponding to 21 distinct values, for example, physician referral,
emergency room, and transfer from a hospital
0%
Time in hospital Numeric Integer number of days between admission and discharge 0%
Payer code Nominal Integer identifier corresponding to 23 distinct values, for example,Blue Cross/Blue
Shield, Medicare, and self-pay
52%
Medical specialty Nominal Integer identifier of a specialty of the admitting physician, corresponding to 84
distinct values, for example, cardiology, internal medicine, family/general practice,
and surgeon
53%
Number of lab procedures Numeric Number of lab tests performed during the encounter 0%
Number of procedures Numeric Number of procedures (other than lab tests) performed during the encounter 0%
Number of medications Numeric Number of distinct generic names administered during the encounter 0%
Number of outpatient visits Numeric Number of outpatient visits of the patient in the year preceding the encounter 0%
Number of emergency visits Numeric Number of emergency visits of the patient in the year preceding the encounter 0%
Number of inpatient visits Numeric Number of inpatient visits of the patient in the year preceding the encounter 0%
Diagnosis 1 Nominal The primary diagnosis (coded as first three digits of ICD9); 848 distinct values 0%
Diagnosis 2 Nominal Secondary diagnosis (coded as first three digits of ICD9); 923 distinct values 0%
Diagnosis 3 Nominal Additional secondary diagnosis (coded as first three digits of ICD9); 954 distinct
values
1%
Number of diagnoses Numeric Number of diagnoses entered to the system
0%
Glucose serum test result Nominal Indicates the range of the result or if the test was not taken. Values: “>200,” “>300,”
“normal,” and “none” if not measured
0%
A1c test result Nominal Indicates the range of the result or if the test was not taken. Values: “>8” if the result
was greater than 8%, “>7” if the result was greater than 7% but less than 8%,
“normal” if the result was less than 7%, and “none” if not measured.
0%
Change of medications Nominal Indicates if there was a change in diabetic medications (either dosage or generic
name). Values: “change” and “no change”
0%
Diabetes medications Nominal Indicates if there was any diabetic medication prescribed.Values: “yes” and “no” 0%
24 features for medications Nominal For the generic names: metformin, repaglinide, nateglinide, chlorpropamide,
glimepiride, acetohexamide, glipizide, glyburide, tolbutamide, pioglitazone,
rosiglitazone, acarbose, miglitol, troglitazone, tolazamide, examide, sitagliptin,
insulin, glyburide-metformin, glipizide-metformin, glimepiride-pioglitazone,
metformin-rosiglitazone, and metformin-pioglitazone, the feature indicates whether
the drug was prescribed or there was a change in the dosage. Values: “up” if the
dosage was increased during the encounter “down” if the dosage was decreased,
“steady” if the dosage did not change, and “no” if the drug was not prescribed
0%
Readmitted Nominal Days to inpatient readmission. Values: “<30” if the patient was readmitted in less than
30 days, “>30” if the patient was readmitted in more than 30 days, and “No” for no
record of readmission.
0%
•Missing Data:
weight attribute (97 % missing) was considered to be
too sparse and it was not included in further analysis.
Furthermore, the payer code attribute is considered
irrelevant to the outcome as well as it has a high
percentage of missing values so it is excluded too.
“medical specialty” refers to the specialty of
CCH 2023 - Special Session on Machine Learning and Deep Learning for Preventive Healthcare and Clinical Decision Support
684
attending physician which has some missing data so
we fill “Missing” in the missing place as this is an
important feature for analysis.
•Zero Variance Attributes:
Troglitazone, acetohexamide,citoglipton,glimepirie
pioglitazone,metformin pioglitazone, and examide
were excluded as no patients on these drugs.
•Near Zero Variance Attributes:
metformin rosiglitazone, glipizide-metformin,
tolazamide, tolbutamide, chlorpropamide, and
miglitol were excluded as there are only very few
cases with steady doses (less than 10 instances).
•Transformation of Skewed Variables:
Age attribute is categorised into 3 distinct groups
based on trends proposed by Beata Strack et al (Strack
et al,2014). Admission Type id, admission source,
and discharge disposition id attribute are categorised
with similar categories merged.
•Discretization:
The three diagnosis results are given in icd-9 coding
discretized into 9 groups. As well as discretization
applied to the numerical attributes (time in hospital,
number medications, number lab procedures, number
procedures, number outpatient, number emergency
and number inpatient) discretized in to 5 pins, using
unsupervised splitting technique based on a specified
number of bins.
•Class Imbalance:
SMOTE is used to balance the prediction variable
classes. For the purpose of uncontrolled diabetic
patient readmission prediction.
At the end ,2 sub data sets were extracted from the
original one. The first subset for the prediction of all
readmission cases (within 30 days or after 30 days
counted as yes). The second subset for the prediction
of the early readmission cases (excluding all
readmission after 30 days).
This ended with 35 attributes in the first subset
(long- term and short-term readmission) and 9102
instances. A 6282 instances and 34 attributes in the
second subset (short- term readmission only).
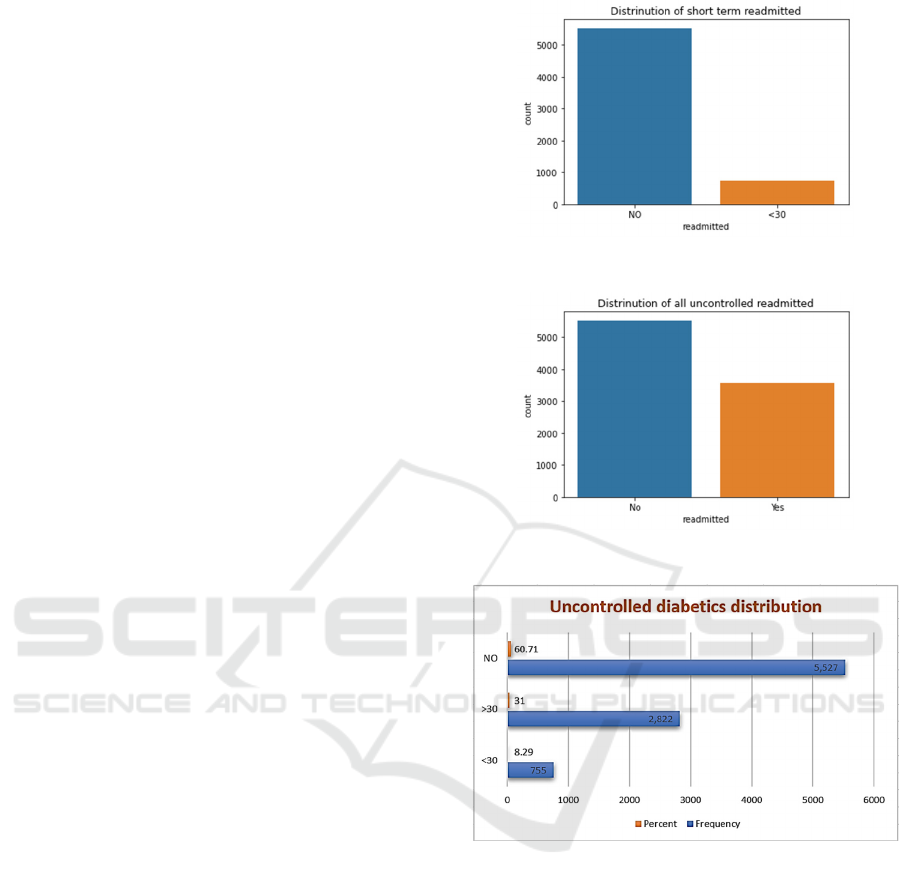
The following charts shows the distribution of the
prediction variable (readmission) in the data set and
the two sub sets. Chart 1 and 2 shows the distribution
of the readmission through the subsets. Chart 3 shows
the distribution of the excluded data set for
uncontrolled diabetics.
Chart 1: Distribution of short-term readmission.
Chart 2: Distribution of uncontrolled diabetic patient.
Chart 3: distribution of the excluded data set for
uncontrolled diabetics.
D. Modelling
WEKA was the tool that has been chosen for this step
because of its variety of classification methods, this
study used a tree-based Algorithm (RF), a Bayesian
learning algorithms (NB), a function algorithm
(SVM, NN), a meta algorithm (Ad boost), and a lazy
algorithm (KNN). After choosing the algorithms,
Sampling been done with
10 folds cross validation while 30 % used for the
test set and 70 % used for the training set. Cross
validation has been used to give the model an
opportunity to be trained on multiple (10) train test
splits as well as it reduces over fitting. Also, all these
Short-Term and Long-Term Readmission Prediction in Uncontrolled Diabetic Patients using Machine Learning Techniques
685
algorithms used through the filtered classifier
algorism in WEKA to apply the over sampling for the
training set only not on both training and test sets.
Finally, two prediction scenarios have been
developed to compare the results. The first scenario
for the prediction of all readmission cases (within 30
days or after 30 days). The second scenario for the
prediction of the early readmission cases (excluding
all readmission after 30 days). the output of this step
were 2 sub data sets one for the early readmission
prediction and the second for the readmission
prediction.
E. Evaluation
The basic performance parameters this study
considers are the model accuracy and AUROC (Area
Under curve for the ROC). While AUROC is the
measure of the ability of a classifier to distinguish
between classes, the accuracy is the fraction of
predictions our model got right.
4
RESULTS
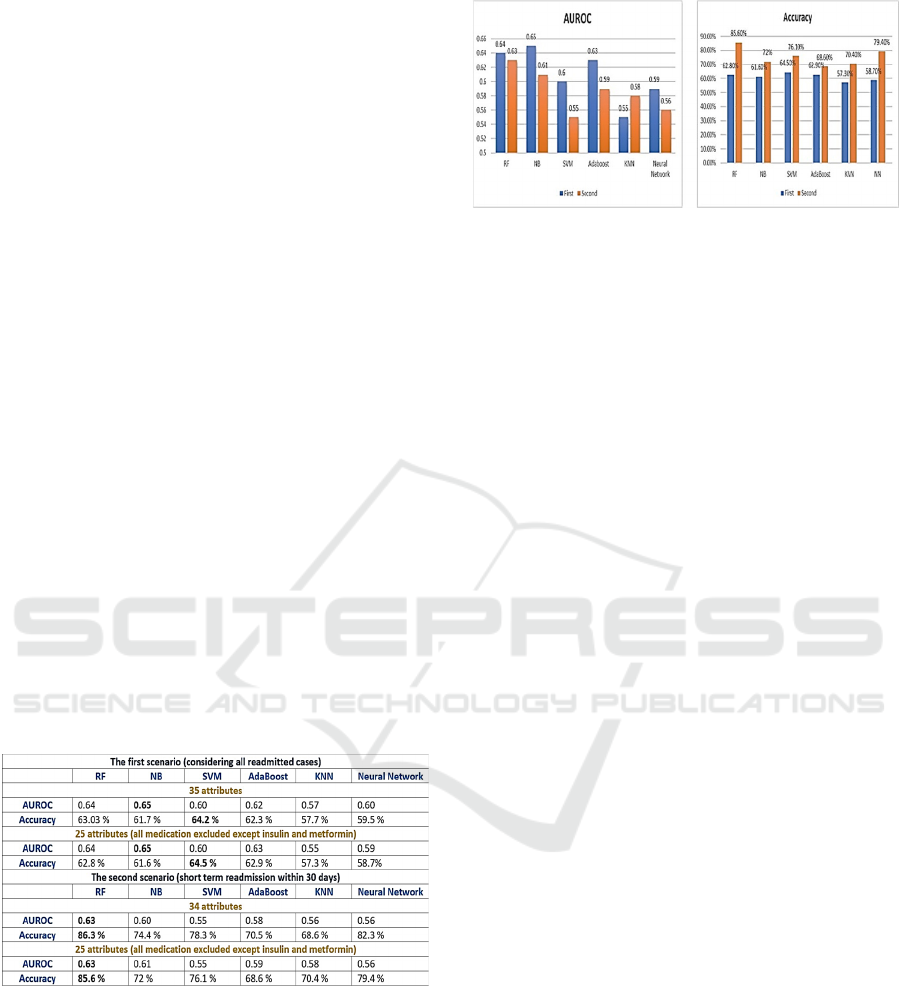
For the first scenario, SVM achieved the highest
accuracy of 64.2 % and NB achieved the best
AUROC area of 0.65. For the second scenario, RF
achieved the highest accuracy of 86.38 % and the best
AUROC area of 0.63. Table 2 summarizes the results:
Table 2: Results summary.
Also, as noticed from the results, the second scenario
shows a much better accuracy of 86 %, but the first
scenario shows a little better AUROC (.65). This
figure compares the AUROC and accuracy for each
algorithm in both scenarios.
Chart 4: Results graph.
5
DISCUSSION
Although this research targets uncontrolled diabetics
and all research in literature targets all diabetic
patients. The results comes, as expected, in context
with other research in literature, especially the whole
readmission predictions as example ,Pham et al
ensemble model achieved an accuracy of 63 %
accuracy , our model achieved a better accuracy of
64.5 % with SVM and attribute selection .For the
second scenario for the short term uncontrolled
diabetic readmission prediction, although, Sharma et
al RF model achieved 94 % accuracy and Alars et al
NB model achieved 93.5 % ,our model is still in
context with other research in literature, as example
Neto et al RF model achieved 89.8 % and Farajollahi
et al achieved 86.8 % using deep learning. the
difference in the data sample used in this research
(uncontrolled diabetic patient may explain the
difference in accuracy with other researchers.
6
CONCLUSION
In this study, several machinebased methods were
proposed to predict short-term and long-term
uncontrolled diabetic readmission. SMOTE-based
data pre-processing is introduced to address the
imbalanced data. In addition, comparisons have been
done between Random forest, Neural network, KNN,
Naïve Bayes, SVM, and Adaboost. The experimental
results indicate that in the first scenario, SVM
outperforms other methods in the prediction of short-
term and long-term readmission with an accuracy of
64 % but NB achieved a better AUROC 0.65 in both
cases with and without attribute selection. Also, In the
second scenario, the prediction of early readmission
with Random forest outperforms other methods with
an accuracy of 86,38 % and an AUROC of 0.63 in
both experiments with and without attribute selection.
CCH 2023 - Special Session on Machine Learning and Deep Learning for Preventive Healthcare and Clinical Decision Support
686

In this study, uncontrolled diabetic patients are
targeted; nevertheless, we expect that this early study
will pave the way for future research that can improve
the accuracy of readmission risk estimates for other
health conditions like heart and kidney diseases. Also,
an improved data set, including other important
features such as age, weight, and laboratory values,
could prove valuable and warrant further study.
REFERENCES
Alamer, A. A., Patanwala, A. E., Aldayyen, A. M., & Fazel,
M. T. (2019). Validation and comparison of two 30-day
re-admission prediction models in patients with
diabetes. Endocrine Practice, 25(11), 1151-1157.
Al-Ars, Z. T., & Aldabbagh, A. M. (2021). Predicting the
Early Re-admission of Diabetic Patients Using
Different Data Mining Techinques. In 2021 Fourth
International Conference on Electrical, Computer and
Communication Technologies (ICECCT) (pp. 1-8).
IEEE.
Ali, F., El-Sappagh, S., Islam, S. R., Kwak, D., Ali, A.,
Imran, M., & Kwak, K. S. (2020). A smart healthcare
monitoring system for heart disease prediction based on
ensemble deep learning and feature fusion. Information
Fusion, 63, 208-222.
Battineni, G., Sagaro, G. G., Chinatalapudi, N., & Amenta,
F. (2020). Applications of machine learning predictive
models in the chronic disease diagnosis. Journal of
personalized medicine, 10(2), 21.
Bhuvan, M. S., Kumar, A., Zafar, A., & Kishore, V. (2016).
Identifying diabetic patients with high risk of
readmission. arXiv preprint arXiv:1602.04257.
Boutayeb, A., Twizell, E. H., Achouayb, K., & Chetouani,
A. (2004). A mathematical model for the burden of
diabetes and its complications. Biomedical engineering
online, 3(1), 1-8.
Dagliati, A., Marini, S., Sacchi, L., Cogni, G., Teliti, M.,
Tibollo, V., & Bellazzi, R. (2018). Machine learning
methods to predict diabetes complications. Journal of
diabetes science and technology, 12(2), 295-302.
Donsa, K., Spat, S., Beck, P., Pieber, T. R., & Holzinger, A.
(2015). Towards personalization of diabetes therapy
using computerized decision support and machine
learning: some open problems and challenges. In Smart
Health (pp. 237-260). Springer, Cham.
Dua, D. and Graff, C. (2019). UCI Machine Learning
Repository [http://archive.ics.uci.edu/ml]. Irvine, CA:
University of California, School of Information and
Computer Science
Eldarrat, A. H. (2011). Diabetic patients: their knowledge
and perception of oral health. Libyan Journal of
Medicine, 6(1), 5691.
Farajollahi, B., Mehmannavaz, M., Mehrjoo, H., Moghbeli,
F., & Sayadi, M. J. (2021). Diabetes diagnosis using
machine learning. Frontiers in Health Informatics,
10(1), 65.
Farajollahi, B., Mehmannavaz, M., Mehrjoo, H., Moghbeli,
F., & Sayadi, M. J. (2021). Predicting hospital
readmission of diabetic patients using machine
learning. Frontiers in Health Informatics, 10(1), 74.
Hu, P., Li, S., Huang, Y. A., & Hu, L. (2019, June).
Predicting hospital readmission of diabetics using deep
forest. In 2019 IEEE International Conference on
Healthcare Informatics (ICHI) (pp. 1-2). IEEE.
Kavakiotis, I., Tsave, O., Salifoglou, A., Maglaveras, N.,
Vlahavas, I., & Chouvarda, I. (2017). Machine learning
and data mining methods in diabetes research.
Computational and structural biotechnology journal,
15, 104-116.
Kim, H., Ross, J. S., Melkus, G. D., Zhao, Z., & Boockvar,
K. (2010). Scheduled and unscheduled hospital
readmissions among diabetes patients. The American
journal of managed care, 16(10), 760.
Kim, S. (2007). Burden of hospitalizations primarily due to
uncontrolled diabetes: implications of inadequate
primary health care in the United States. Diabetes care,
30(5), 1281-1282.
Kohli, P. S., & Arora, S. (2018, December). Application of
machine learning in disease prediction. In 2018 4th
International conference on computing communication
and automation (ICCCA) (pp. 1-4). IEEE.
"Kumar, P. M1. Battineni, G., Sagaro, G. G.,
Chinatalapudi, N., & Amenta, F. (2020). Applications
of machine learning predictive models in the chronic
disease diagnosis. Journal of personalized medicine,
10(2), 21.., Lokesh, S., Varatharajan, R., Babu, G. C.,
& Parthasarathy, P. (2018). Cloud and IoT based
disease prediction and diagnosis system for healthcare
using Fuzzy neural classifier. Future Generation
Computer Systems, 86, 527-534."
Navarro-Pérez, J., Orozco-Beltran, D., Gil-Guillen, V.,
Pallares, V., Valls, F., Fernandez, A., & Tellez-Plaza,
M. (2018). Mortality and cardiovascular disease burden
of uncontrolled diabetes in a registry-based cohort: the
ESCARVAL-risk study. BMC cardiovascular
disorders, 18(1), 1-9.
Neto, C., Senra, F., Leite, J., Rei, N., Rodrigues, R.,
Ferreira, D., & Machado, J. (2021). Different scenarios
for the prediction of hospital readmission of diabetic
patients. Journal of Medical Systems, 45(1), 1-9.
Pham, H. N., Chatterjee, A., Narasimhan, B., Lee, C. W.,
Jha, D. K., Wong, E. Y. F., & Chua, M. C. (2019, July).
Predicting hospital readmission patterns of diabetic
patients using ensemble model and cluster analysis. In
2019 International Conference on System Science and
Engineering (ICSSE) (pp. 273-278). IEEE.
Pujianto, U., Setiawan, A. L., Rosyid, H. A., & Salah, A.
M. M. (2019). Comparison of Naïve Bayes Algorithm
and Decision Tree C4. 5 for Hospital Readmission
Diabetes Patients using HbA1c Measurement. Knowl.
Eng. Data Sci., 2(2), 58-71.
Sharma, A., Agrawal, P., Madaan, V., & Goyal, S. (2019,
June). Prediction on diabetes patient's hospital
readmission rates. In Proceedings of the Third
International Conference on Advanced Informatics for
Computing Research (pp. 1-5).
Short-Term and Long-Term Readmission Prediction in Uncontrolled Diabetic Patients using Machine Learning Techniques
687

Sharma, A., Agrawal, P., Madaan, V., & Goyal, S. (2019,
June). Prediction on diabetes patient's hospital
readmission rates. In Proceedings of the Third
International Conference on Advanced Informatics for
Computing Research (pp. 1-5).
Strack, B., DeShazo, J. P., Gennings, C., Olmo, J. L.,
Ventura, S., Cios, K. J., & Clore, J. N. (2014). Impact
of HbA1c measurement on hospital readmission rates:
analysis of 70,000 clinical database patient records.
BioMed research international, 2014.
Threatt, J., Williamson, J. F., Huynh, K., Davis, R. M., &
Hermayer, K. (2013). Ocular disease, knowledge and
technology applications in patients with diabetes. The
American journal of the medical sciences, 345(4), 266-
270.
Urban, G., Tripathi, P., Alkayali, T., Mittal, M., Jalali, F.,
Karnes, W., & Baldi, P. (2018). Deep learning localizes
and identifies polyps in real time with 96% accuracy in
screening colonoscopy. Gastroenterology, 155(4),
1069-1078.
CCH 2023 - Special Session on Machine Learning and Deep Learning for Preventive Healthcare and Clinical Decision Support
688
