
An Analysis of IoMT Vital Signs Measurement Devices for Practical
and Secure Remote Clinical Monitoring
Kerry Y. Fang
1a
, Quoc Lap Trieu
1b
, Heidi Bjering
1c
, Steven Thomas
2d
, Jim Basilakis
1e
,
and Jeewani Anupama Ginige
1f
1
School of Computer, Data and Mathematical Sciences, Western Sydney University, Sydney, Australia
2
South Western Sydney Local Health District, Sydney, Australia
Keywords: Vital Signs Measurement, Internet of Medical Things (IoMT), Remote Monitoring, Security, Interoperability.
Abstract: The increasing need to provide care outside of hospitals necessitates remote monitoring of basic vital signs of
patients from places such as private homes and aged care facilities. While much exploratory research has been
done on using Internet of Medical Things (IoMT) devices for remote monitoring, there is a requirement to
examine the practicality associated with the mass use of affordable off-the-shelf devices in terms of usability,
secure access to data, and integration into hospital-based information systems. This paper investigates various
security aspects in nine vital signs sensor devices that can be purchased and used for homecare monitoring in
Australia. Specifically, the security and privacy aspects of these devices and associated software, regulatory
compliance, interoperability, and formats of the accessible data streams were investigated. It was found that
the devices were not entirely secure, as personal health information could be accessed using appropriate tools.
Only one vendor enabled encryption during data transmission and provided an API to access data. While the
clinical use of these devices with integration into hospital systems for practical remote monitoring is not easily
achievable, it is possible to use devices for day-to-day vital signs monitoring purposes in a home setting.
1 INTRODUCTION
With the continuous advancement in technologies
such as the Internet of Medical Things (IoMT), cloud
computing and sensor devices, the remote monitoring
of health and well-being is becoming more common
and convenient worldwide, especially in developed
countries. In addition, integrating innovative
technologies into smart homes and smart healthcare
is positively changing how people live. However,
security and privacy issues are still a major concern
surrounding the adoption of IoMT devices in the
health sector (Chacko & Hayajneh, 2018).
Threats of the network layer, support layer and
application layer on IoT devices remain challenging
when integrating IoMT devices (Pahlevanzadeh et al.,
2021). Data tampering, eavesdropping, DoS (Denial-
a
https://orcid.org/0000-0001-6989-4485
b
https://orcid.org/0000-0003-0678-374X
c
https://orcid.org/0000-0001-5925-3510
d
https://orcid.org/0000-0002-2416-0020
e
https://orcid.org/0000-0002-7440-1320
f
https://orcid.org/0000-0002-6695-6983
of-Service) attack, unauthorised access, DDoS
(Distributed Denial-of-Service) and sniffers are all
examples of the three perception layer attacks
(Leloglu, 2016). Furthermore, security risks increase
with the growing number of IoMT devices connected
to the Internet (Talwana & Hua, 2016).
This exploratory research aims to investigate
regulatory compliance, interoperability, data format,
security and privacy issues associated with a selected
set of off-the-shelf Bluetooth-enabled vital signs
sensor devices in the context of using the devices for
homecare monitoring in Australia. The sensor devices
investigated are designed for the remote measuring
and monitoring of five vital signs measurements:
body temperature, blood oxygen saturation, heart
rate/electrocardiogram, blood pressure, and body
weight. The selected devices ranged from low-cost to
Fang, K., Trieu, Q., Bjering, H., Thomas, S., Basilakis, J. and Ginige, J.
An Analysis of IoMT Vital Signs Measurement Devices for Practical and Secure Remote Clinical Monitoring.
DOI: 10.5220/0011887100003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 1: BIODEVICES, pages 85-95
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
85

expensive off-the-shelf products and included
regulated and unregulated medical devices according
to federal agencies such as the FDA (Food and Drug
Administration of the USA) and TGA (Therapeutic
Goods Administration in Australia). In addition, the
mobile apps corresponding to these sensor devices
were also investigated to ascertain the ease of setup,
security and privacy of the patient data and
measurement data stored and shared within the apps.
The security and privacy aspects of these sensor
devices were inspected and compared using Node-
RED
1
and ESP32
2
devices. Hence this paper aims to
answer the following research question:
“In the Australian context, is it practical to use
off-the-shelf vital signs measurement products for
remote clinical monitoring of patients securely?”
There are several highlighted keywords in the
above question that requires some contextual
explanations as follows:
1. Practicality – practical usage of these off-the-
shelf products has several aspects. Firstly,
considering the potential mass use, these
products should be affordable, user-friendly and
easy to set up by an average consumer, including
older adults. In addition, it should be possible to
remotely integrate these devices to pull the data
into clinical information management systems
housed in the healthcare networks. In other
words, the implementation should not depend on
IT professionals visiting every household to set
up. It should be doable by the average end-users
with some guidance.
2. Clinical monitoring – In the clinical setting, it is
imperative to use devices approved by regulatory
authorities, such as TGA or FDA, to ensure that
these devices comply with the standards
expected in healthcare. When exploring the off-
the-shelf vital sign measurement device market,
it is unclear whether the available products are
suitable for clinical use in this sense. Also,
certain words used in marketing (e.g., FDA
cleared vs approved) around regulatory
compliance can be ambiguous and confusing for
the average user.
3. Security – The ability to easily integrate devices
into healthcare information systems essentially
means sharing the data via Bluetooth/Wi-Fi and
through the internet to locations beyond the
patient's home setting. This can be a double-
edged sword as it is likely that other motivated
1
https://nodered.org/
2
https://en.wikipedia.org/wiki/ESP32
yet uninvited parties (e.g., hackers) would also be
interested in having access to such data when
exposed through these technologies.
The major contribution of this paper is the
evaluation of the possible security vulnerabilities of
popular Bluetooth-enabled sensor devices used for
vital sign measurements using third-party software
(Node-RED
71
) and instruments (ESP32
2
).
The remainder of this paper is organised as
follows. First, the background section summarises the
current research on security IoMT devices used in
healthcare and followed by that, our methods in
device selection and testing procedures are presented.
The next section discusses the findings from four
dimensions – usability and regulatory compliance;
security and privacy at the end-user and mobile app
level; data accessibility and integration; and sensor
device data extraction, followed by a brief conclusion
with an outline of possible future works.
2 BACKGROUND
Health care is moving beyond the hospital and into
patients' homes with the aging population increase.
This change is one of the main drivers behind the
growth of innovative and smart healthcare IoMT
devices. The word “smart” implies the combination
of software, hardware, cloud, and sensor technologies
to collect and share real-time health data, which can
then be used to monitor health and aid decision-
making (Papa et al., 2020). The IoMT environment
supports this process through the creation and linkage
of a network of smart devices, and it is estimated that
the number of connected devices worldwide will
reach 75 billion by the year 2025 (Nick, 2022). Smart
healthcare is therefore considered an application of
IoMT. The sensor technology used in smart
healthcare is gradually being embedded into the daily
lives of many people, especially the elderly and
people with chronic diseases. Wearable sensors are
devices patients can wear, and measurements can be
transmitted to the smartphone via Bluetooth or Wi-Fi
technology. It offers significant advantages to
healthcare as it provides the ability for remote health
monitoring, such as the monitoring of various vital
signs.
The main challenges with IoMTs are security and
privacy issues. Many of the existing IoMT devices in
the market require connections from the sensor to a
mobile app for displaying and storing results and
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
86

personal data. Bluetooth is one of the preferred ways
of data communication, as it is economical and
suitable for use in compact devices (Zubair et al.,
2019). Bluetooth 4.0 is known as Bluetooth Low
Energy (BLE), a low-energy variation widely used in
IoMTs (Kandhare, 2019). However, when Bluetooth
is used to connect and transfer results to an app, it can
act as an attack surface, that may potentially
compromise the integrity, availability and
confidentiality of the transmitted clinical data. In
addition, although people's health data privacy
awareness is increasing, many still need to secure
their smartphones (Grindrod et al., 2017). This can be
an issue when the smartphone is lost or taken by
others without consent, and all the valuable personal
app data and phone data are at risk of malicious
attack.
Some existing research looked at the security and
privacy concerns of home monitoring technologies
such as medical sensor devices. Gerke and colleagues
(2020) discussed the security and privacy issue of
home monitoring technologies during the COVID-19
pandemic. Another study conducted by Sivaraman
and colleagues (2017) looked at the security and
privacy threats for smart home IoMT devices,
including smart switches, smart cameras, Amazon
Echo, and smart light bulbs. Within the study, 20
IoMT devices were tested in total using data
capturing and mock server techniques. The result
showed that most devices were vulnerable to some
malicious attack. The authors also provided some
recommendations to manage these potential risks,
which range from user education to regulation and
legislation (Sivaraman et al., 2017). Another study
looked at the significant security and privacy features
of health tracker devices, including Fitbit, Jawbone
and Google Glass, by investigating the devices’
strength, communication methods, and Bluetooth
pairing processes (Zhang et al., 2020).
Figure 1: Points of security vulnerabilities adapted from
Kim et al (2020).
Kim et al. (2020) present a model for security
evaluation in telemedicine, in which they identify
areas where telemedicine security could be
vulnerable to attacks. Based on Kim et al.’s (2020)
Figure 1 summarises the areas of concern according
to the architectural elements (in rounded rectangular
boxes) and various layers – user, software, device and
communication (separated by dotted lines).
However, none of the existing research utilised
technologies and tools for data access to physically
check/test the security and privacy of medical vital
signs measurement devices and applications. In this
paper, the security concerns related to end-user or
patient, IoMT devices and Mobile Apps points of
view (highlighted in red fonts in Figure 1) are
discussed with respect to vital sign measurement
devices used in homecare implementations. As
previous examples show, most existing research
discussed the overall security and privacy of health
devices or sensors for general wellbeing and fitness,
e.g., Fitbit or smart watches, thus not specific to vital
medical signs measurement devices for clinical use.
Moreover, most existing research focuses on health
sensors and devices for managing certain health
conditions or is limited to certain health devices or
applications. For example, Hendricks-Sturrup (2022)
investigated the privacy of multiple pulse oximeter
apps during the COVID-19 pandemic. Another study
by Knorr and colleagues (2015) used a novel method
that studied the files stored in the APK package of
various Blood pressure and diabetes apps, the
dynamic behaviour of the app and the app’s privacy
policy. Lastly, as far as the authors are aware, existing
research could not be found on the security and
privacy of vital medical signs measurement devices
from both the device and mobile application (app)
dimensions. The security and privacy aspects of the
sensor devices and the related mobile applications can
be especially crucial to the users, as both can be used
to collect, store, and transfer sensitive personal
health-related data. This means either one can
become vulnerable to malicious attacks or privacy
leaks, ultimately leading to patient risks. Therefore,
our research aims to fill these gaps by utilising
hardware and software solutions for examining more
closely the processes and data involved in sensor
information exchange, with tools such as Node-red
and ESP32. These technologies allow us to analyse
and compare the security and privacy aspects of
existing medical vital signs measurement devices and
their corresponding mobile applications.
3 METHODS
This study mainly consisted of four steps:
(A) Vital signs measurement device selection;
An Analysis of IoMT Vital Signs Measurement Devices for Practical and Secure Remote Clinical Monitoring
87
(B) Privacy policy inspection of the
corresponding mobile applications;
(C) Regulatory compliance investigation of the
selected devices;
(D) Checking the accessibility to low-level
sensor data via Node-red and ESP32.
A total of nine (9) Bluetooth-enabled vital signs
measurement devices were selected and tested; these
consisted of three (3) oximeters, two (2) digital
thermometers, two (2) blood pressure monitors, two
(2) portable ECG/EKGs, and two (2) digital weight
scales.
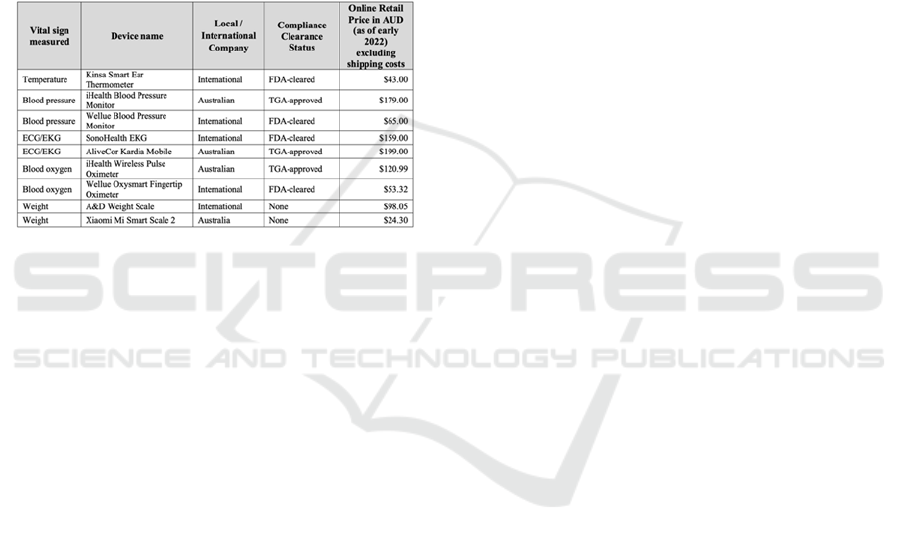
Table 1: Device list.
(A) Vital Signs Measurement Device Selection.
Vital signs are the measurements of the human body’s
basic functions and can be particularly useful in
detecting or monitoring health issues. Four crucial
vital signs are body temperature, blood oxygen
saturation, heart rate/electrocardiogram, and blood
pressure. In addition to the four crucial vital signs,
body weight is an important measurement as it
provides supporting information regarding a patient’s
overall health and physical condition
(NursingAnswers.net, 2018). Moreover, most
treatment decisions and dosages depend on body
weight measurement. These vital signs and body
weight measurements are often measured through
sensor technologies, which can be used in a variety of
clinical settings, for instance in-home and hospitals.
Results from the sensor devices are displayed almost
immediately and can be sent to healthcare
professionals or stored in the cloud for future
reference.
A range of vital signs measurement devices was
researched based on their price, functionality, and
regulatory compliance clearance perspectives. Where
possible, the authors made efforts to include at least
one product from an Australian company. Table 1
lists the selected vital signs measurement devices for
this research.
(B) Privacy Policy Inspection of the Corresponding
Mobile Applications.
With the increased use of mobile devices worldwide,
mobile applications have become popular for
smartphone users as a platform for entertainment and
personal use. mHealth (Mobile Health) uses apps,
devices, and other wireless technology in medical
care (Holman, 2022). mHealth apps are health
applications available on mobile devices, offering
users a wide range of medical and health-related
services. This means various health data will be
collected, analysed, and shared through the
applications. As a result, mHealth apps accounted for
the largest revenue share of 75.4% in the mHealth
market in 2021 (Grand View Research, 2022). The
innovation in mHealth apps brings many health and
clinical benefits, such as real-time analysis and
transmission of health data, remote health
monitoring, promoting self-management, and
promote health awareness. However, at the same
time, mHealth apps also open up a portal to new
privacy and security risks.
The corresponding mHealth apps to the sensor
devices used in this research were inspected by
examining the device organisations’ privacy policies,
terms and services, and inspection of the mobile
traffic using Fiddler Everywhere. Fiddler Everywhere
is a secure web debugging proxy (Fiddler
Everywhere, 2022). For this research, Fiddler
Everywhere were used to inspect the traffic from the
mHealth apps used on iOS mobile devices.
(C) Regulatory Compliance Investigation of the
Selected Devices.
Various Acts and regulations exist to protect the
collection and transmission of these sensitive health
data, such as the Health Insurance Portability and
Accountability Act (HIPAA) in the US and the
Personal Information Protection and Electronic
Documents Act (PIPEDA) in Canada. It is also
important for IoMT device manufacturers to clarify
the secondary use of data to the users (Muzny et al.,
2020), either through the product manual or the
company website. Gerke and colleagues (2020)
further explored the regulatory aspect of medical
technologies, such as the emergency use
authorisations for medical devices in the USA and
Europe. Healthcare professionals and medical device
companies in the US should ensure that they comply
with HIPAA in order to protect the privacy of the
patient’s data. A similar regulation in Europe is the
General Data Protection Regulation (GDPR), which
prohibits using and processing of personal health and
genetic data (Gerke et al., 2020). Besides issues with
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
88

privacy and security of health-related data, there are
concerns regarding the accuracy and safety of
medical IoMT devices and sensors. Regulations
helped to govern medical devices sold in the market.
However, many devices that can be bought online are
still largely unregulated. In the US, for a medical
device to be sold legally, it must be approved by the
Food and Drug Administration (FDA) to prove that
the device is safe to use. Similar regulation exists in
Australia, where the Therapeutic Goods
Administration (TGA) uses a four-tiered
classification system to govern the supply and usage
of medical devices in Australia. Nowadays, buyers
are becoming more aware of various medical device
regulations. Therefore, formal approvals from these
regulatory bodies will give the buyers a sense of
security.
In this study, the authors closely inspected the
regulatory compliance status of the devices and
various data collected and transmitted using the
devices and associated software.
(D) Checking the Accessibility to Low-level Sensor
Data via NODE-RED and ESP32
Sensor data from the chosen health sensor devices
were gathered and analysed using Node-RED and
ESP32. Node-RED is a browser-based visual tool for
programming a device. It is used for wiring different
hardware devices, APIs and online services. It is a
mature framework that’s been around for about nine
years and can be applied on any machine or platform
running Node.js. Furthermore, node-RED is simple to
understand with the easy-to-use drag-and-drop
components user interface, which makes it ideal to
represent the flow of communication compared to
many other frameworks such as Eclipse Kura.
ESP32 is a dual-core microcontroller with WiFi
and Bluetooth communication and is a simplified
version of what the industry has been using for years.
In addition, ESP32 provides stability and reliability
with its powerful dual-core CPU. Regarding
connectivity, the Bluetooth and WiFi capabilities
make ESP32 a more suitable microcontroller for
IoMT projects compared to other microcontrollers in
the market, such as the Arduino development boards.
It is also less costly and can achieve ultra-low power
consumption with its power-saving features.
Experimental Setup
There are two types of Bluetooth communication
protocols: BLE (Bluetooth Low Energy) and Classic
Bluetooth. Only iHealth Blood Pressure (BP5) uses
Classic Bluetooth. The rest of the devices use the
BLE Bluetooth protocol. In order to handle these
Bluetooth protocols, Node-RED uses two Bluetooth
modules. The first module is node-red-contrib-
generic-ble to handle BLE protocol and the second
module is node-red-contrib-bluetooth-serial-port to
handle Classic Bluetooth protocol. The authors used
Node-RED v2.1.6 for the testing environment, which
is installed on MacBook Pro (16-inch, 2019), 16 GB
2667 MHz DDR4, 2.3 GHz 8-Core Intel Core i9,
running macOS Big Sur 11.5.2 (20G95). The
MacBook Pro uses the Bluetooth chipset 4364B3
from Broadcom with firmware version v65 c4188.
For testing on ESP32, MicroPython
(MicroPython, 2022) was used, which is an
implementation of Python3 and is optimised for
microcontrollers. Moreover, it has a Python library
aioble to work on both types of Bluetooth protocols
(Github, 2022).
It is important to identify the service and
characteristic UUIDs of the sensor device. They are
unique strings representing the information the sensor
can provide. There are various ways to identify the
service and its characteristics. Node-RED module
node-red-contrib-generic-ble has the method for
scanning the Bluetooth devices and provides the
information related to the connection, such as
services, characteristics, name, manufacturer, and
peripheral identifier of the device. In macOS, an
application named BlueSee was also used, which
allowed users to scan and obtain similar information.
After obtaining UUIDs, the Bluetooth connection
to the device were established by specifying the
service UUID. It was essential to determine the
attributes of the characteristics to be use. It was a read
attribute or notify attribute in our case. The former
allowed the client to read the data from the connected
sensor device. The latter allowed the client to
subscribe to the characteristic and be notified
whenever data was available.
After connecting and subscribing to the sensor
device, the data that was transmitted were able to be
retrieved. However, some sensor devices, such as
iHealth devices and EKGraph from SonoHealth,
require extra steps before the devices can send the
data over. In that case, it was necessary to understand
the authentication process for each device to get the
data from those sensor devices. For example, each
iHealth device requires a key to encrypt and decrypt
the buffer string sent over by the device when the
connection was initiated. EKGrapth device required
the client to initiate the connection by sending a static
buffer array.
It was necessary to understand the data structure
stored in the buffer data of each sensor device in order
to read the data received by the sensors. Some devices
An Analysis of IoMT Vital Signs Measurement Devices for Practical and Secure Remote Clinical Monitoring
89

can store lots of information in the buffer data,
including timestamps, user values and more. The
relevant information was extracted from the data by
understanding the parsing structure and then
converting the hex numbers with different character
lengths to meaningful numbers.
4 FINDINGS/RESULTS
The apps corresponding to the chosen sensor devices
were carefully researched and tested to identify the
various privacy and security features that have been
incorporated to protect personal and health-related
information. Section 4.1 to Section 4.3 provides a
detailed summary of the usability, security,
accessibility and integration of the apps and devices.
The Apps were tested on iOS smartphones, and the
individual researchers tested the devices in real-life
scenarios. Section 4.4 explained the back-end testing
done using Node-Red and ESP32. Furthermore,
section 4.5 provides an overall discussion of the
findings.
4.1 Usability and Regulatory
Compliance
As shown in Table 1, Section 3, most of the devices
tested were either FDA or TGA approved/cleared for
clinical use. This provides a certain level of assurance
that these devices have undergone standard
development and testing and may provide more
accurate results compared to those that were not
approved by such regulatory bodies. Within the list of
devices selected for this research, only the Kardia
TGA-approved), Kinsa (FDA-cleared), and iHealth
(TGA-approved) devices require a password when
setting up the device through the app.
All the devices were relatively easy to set up and
use. The devices required either insertion of batteries
or charging via the provided charging cord before use.
Clear instructions are given in the user manuals that
are supplied with the devices. Three of the devices
required installation and set-up of a mobile app before
the devices could be used. These included the two
iHealth devices and the Karida mobile ECG/EKG
monitor. Both the iHealth devices connect to the same
app. Although the remaining devices could be used
without first connecting to the app, all the devices did
have the ability to connect to apps. The apps had good
usability overall, with user interfaces that are simple
to understand.
4.2 Security and Privacy at the
End-User and Mobile App Level
There are several points of concern regarding the
security and privacy of remote patient care. As shown
in Figure 1, the security and privacy concerns
associated with this testing are presented under three
sub-headings: Patient/User level, Device-level and
Mobile app Level.
4.2.1 Data Privacy Policies
Australian regulations mandate that all digital data
collection products (e.g., Apps and websites) should
have a laid out privacy policy associated with the
product that details the collection, usage,
management and disclosure of personal information
collected through the products (OAIC, 2022b). In
addition, there are special provisions made for the
collection, primary & secondary usage, and
management of health-related data (OAIC, 2022a).
The main requirement is that apps have a clearly laid
out privacy policy on usage, storage and sharing of
the collected information, in particular with parties
outside Australia – for which the end user's explicit
consent is required.
All apps analysed in this study had a set of Terms
and Conditions (T&C) that the users had to agree to
at the setup stage. These T&C statements included
clauses around privacy, use of the collected
information, conditions on access to services and
applications, and any disclaimers surrounding
diagnoses or other medically related matters.
Our analysis found that Kardia, SonoHealth,
Oxysart and Wellue provided the most detailed
privacy policies regarding data collection and usage.
Since iHealth provides a platform to cater for a range
of products, their privacy policy is set an overarching
policy that apply to all devices and cloud accounts
that link to the device. There were no specific details
provided on the collection, usage and dissemination
of the data on the iHealth thermometer app. However,
iHealth provided terms and conditions around data
privacy for their blood pressure monitor and pulse
oximeter. The other entities, Kinsa and A&D,
provided low-level details about the data collection
and usage in their privacy policies.
The types of data collected varied between
devices. However, email, date of birth, name, and sex
details were collected by almost all Apps in addition
to the intended measurements (e.g., blood pressure,
weight) collected through the device. In addition to
these, height and weight were collected by iHealth
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
90

pulse oximeter & blood pressure monitor and Kardia
ECG monitor.
4.2.2 Data Security
The Australian Signals Directorate (ASD) provides
an Information Security Manual, in accordance with
the Intelligent Services Act 2001
83
, that is to be
followed by any software vendor
4
. The security
principles outlined in this manual mandate that all
software vendors take adequate measures to
safeguard the data collected, stored and
communicated through their platforms. In this regard,
the authors explored the measures taken by the
selected vendors of the off-shelf vital sign
measurement devices analysed in this study. The
findings are detailed below:
• Cloud Set-Up -
Most modern mobile applications use cloud locations
to store and process data collected via the devices. In
the analysis of the set of devices and the associated
applications, the authors investigated which vendor
saved the data on cloud locations.
Among the vendors studied Kinsa, Wellue, and
A&D did not send the data to a cloud location but
provided the capability to link to Apple Health
5
, which
essentially transferred the data to the Apple cloud. The
vendors iHealth and Kardia had their own cloud
locations on which data was saved and processed.
While the iHealth cloud was included as part of the
device purchase, KardiaCare cloud required users to
pay a monthly or equivalent annual subscription fee to
have their data stored on the cloud for future usage.
• Connection Security -
Most devices connected to the App via Bluetooth,
except for Kardia which used audio signals to push
the measurement data onto the mobile device.
Information on the mechanisms to ensure secure
connectivity were only provided by SonoHealth and
Kardia. SonoHealth detailed what data is
communicated and stored in server environments,
while Kardia explained the encryption techniques
deployed to assure connection security. The other
vendors did not mention any aspect concerning
connection security.
• Password Policy (App security) –
A weak password length can open up security
vulnerabilities in any application setting. Therefore,
3
https://www.legislation.gov.au/Series/C2004A00928
4
https://www.cyber.gov.au/acsc/view-all-content/ism
5
https://www.apple.com/au/ios/health/
the password policies used by the vendors concerning
App security were explored. In this exploration, it
was found that Kardia has the most comprehensive
password requirements of 8-20 characters (no space)
length, at least one upper case letter, one lower case
letter, and one number. Kinsa, iHealth, Wellue, and
SonoHealth had only password length requirements
of 6 characters or more. A&D did not require a
password to access the App.
Forgotten password recovery methods also can
create a security loophole if not properly managed. In
exploring this aspect, it was found that all vendors
sent emails to the nominated email address to recover
the passwords.
• Login Attempts (App security) –
In best security practices, it is recommended to
restrict login attempts if the right credentials are not
provided, as this will eliminate brute-force attacks.
However, none of the vendors had implemented any
restrictions on login attempts, and users could make
any number of attempts.
• Two-Factor Authentication (App security) -
Two-factor authentication was invented in 1967 and
used as early as 1986. Google popularised it in 2010
in response to China’s attacks on Gmail accounts
(Petsas et al., 2015). Since then, many vendors have
adopted the use of this technology. However, none of
the vendors in the focus of this study did use two-
factor authentication in their app implementation,
possibly due to the perceived non-sensitivity of the
collected data.
4.3 Data Accessibility and Integration
Personal data relating to the users are collected and
stored in the apps that are linked to the sensor devices.
For example, personal data such as first name, last
name, date of birth (DOB), gender, email address and
phone number are required and collected when first
registering for an account in most apps. Two
exceptions are the apps for the A&D weight scale and
Wellue blood pressure monitor, where entering these
personal data is optional. In addition, the iHealth app
requires more personal data, such as the users’ weight
and height information.
The results taken by the sensor devices are
transmitted to the mobile apps via Bluetooth.
However, some devices can work without the app by
displaying the results on the LCD screen, which
An Analysis of IoMT Vital Signs Measurement Devices for Practical and Secure Remote Clinical Monitoring
91
means these results will not be transmitted and stored
in the app. Data accessibility is the degree to which
other people can access and use the data stored in the
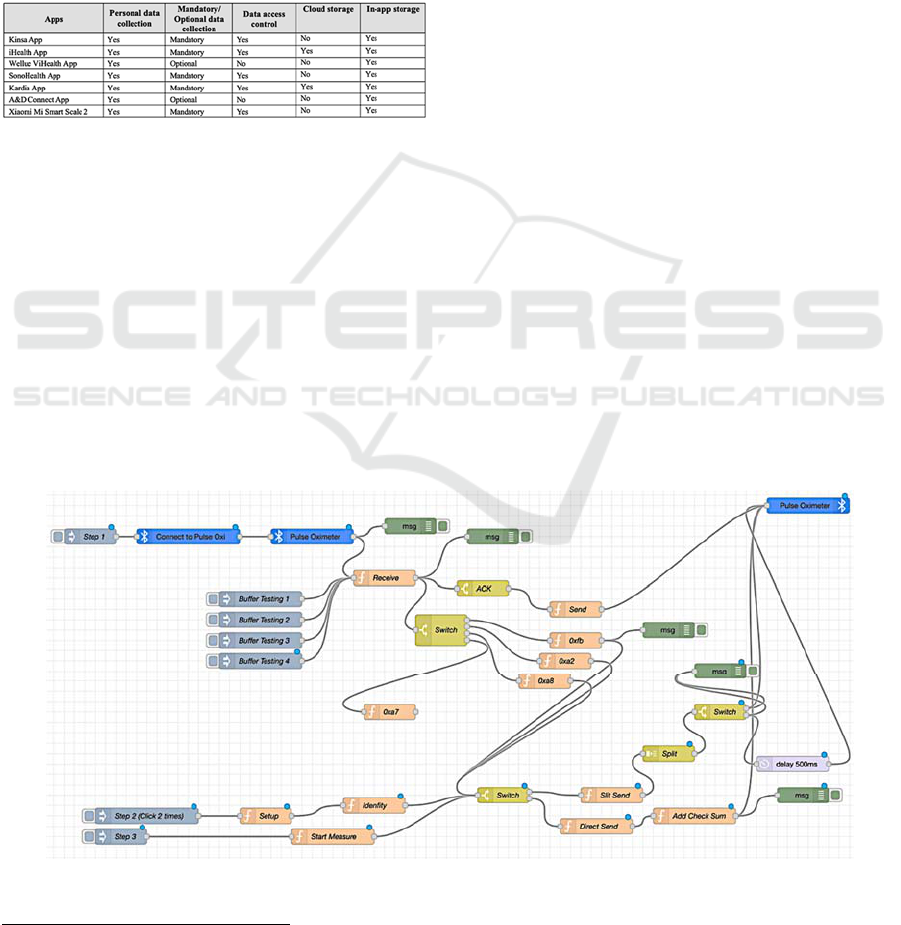
device or the app. As shown in Table 2, most apps
have integrated access control in the form of
username and password during the device and app
setup process. This protects personal health data from
unauthorised access. However, no access control was
in place for the apps where the collection of personal
data is optional.
Table 2: Summary of the data collection requirements and
access control for the apps.
All apps provide in-app storage of results, with a
few also providing cloud storage. Wellue’s ViHealth
App and Kardia App enable connection to Apple
Health, where they transfer and sync the data and
results. For example, Kardia’s app allows connection
to Apple Health to sync health metrics automatically,
and users can send Apple Watch ECGs for review by
a clinician.
4.4 Sensor Device Data Extraction
This section briefly explains the process of accessing
the considered sensor devices. One of the important
steps to gaining access to the Bluetooth device is
understanding the Bluetooth communication
protocol. Depending on the manufacturer, each
device can have a different communication protocol.
It could either require a key to authenticate like
iHealth devices or trigger the communication by
sending over a unique command. Data could also be
captured directly from some sensor devices without
authentication.
Figure 2 shows the Node-RED diagram of the
communication between the client and the iHealth
Pulse Oximeter PO3 device using Bluetooth BLE
protocol. From the diagram, the first step (Step 1) for
communication is to initialise the Bluetooth
connection from the client by scanning and
connecting to the sensor.
After connecting to the sensor, the next process is
to determine whether the device needs to
authenticate. By using the Wireshark
6
tool, the
authors were able to identify the characteristic value
and the overall protocol to determine what the sensor
device requires to communicate. In Step 2, to get the
buffer key for authentication, reverse engineering the
iHealth Android app allowed extraction of the static
buffer key for each type of iHealth device from the
iHealth Android SDK library. A buffer string can then
be sent with a timestamp to the PO3 device to
authenticate. Another buffer string can then be sent
back for authentication. The authors used the key to
decrypt that string and sent it back to the sensor
device. Once successfully authenticated through the
light on the sensor device, real-time data can be
received through subscription to services. The
received data is parsed depending on each type of
device. At the end of the process, all received data are
converted to a hexadecimal format for consistency.
Figure 2: Node-RED diagram of iHealth Pulse Oximeter (PO3).
6
https://www.wireshark.org/
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
92
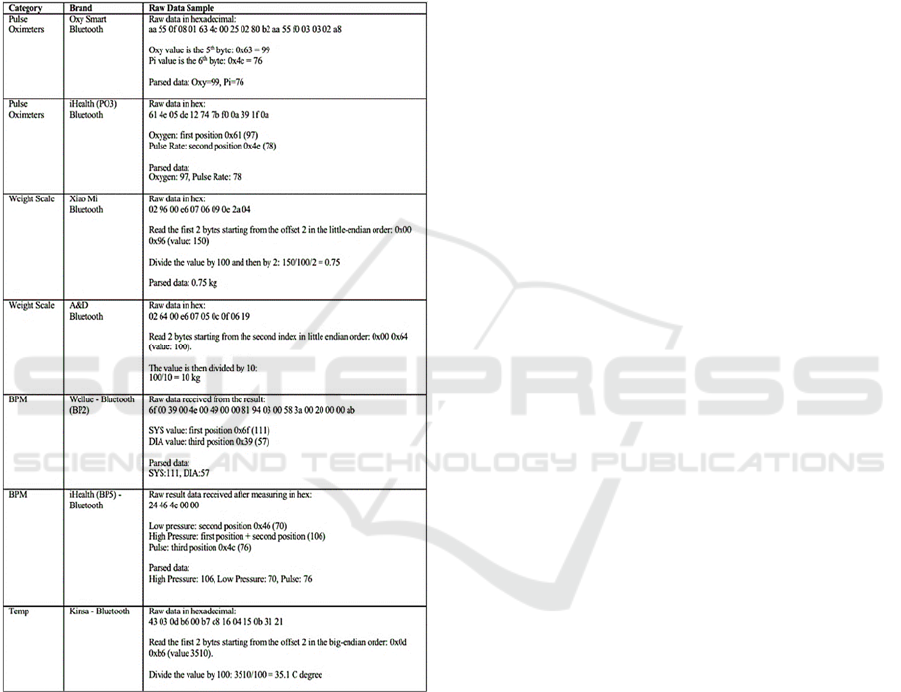
Table 3 shows examples of parsing the samples of
raw data received from different sensor devices. Each
device has a different method of parsing raw data to
actual values. For example, the iHealth Pulse
Oximeter PO3 device represents blood oxygen level
using the first hexadecimal value and pulse rate
measure with the second hexadecimal value in the
received data transmission.
Table 3: Examples of parsing raw data samples.
5 DISCUSSION
Vital signs measurement devices are becoming more
commonly used in people's homes. In this study, the
authors aim to find out the practicality of using these
devices in remote clinical monitoring in a secure
manner. In this regard, 9 devices that could be
purchased in Australia, including online, were
investigated. These devices could measure four vital
signs: body temperature, blood oxygen saturation,
heart rate/electrocardiogram, and blood pressure, plus
body weight as an additional measure. An overall
summary of the privacy- and security-related features
examined for all 9 sensor devices, together with their
associated apps and online platforms, can be found
within the link: ‘https://tinyurl.com/5n87x9ht’.
Based on the findings, it was identified that most
devices could be used for clinical purposes, as these
devices had regulatory clearances. However, it was
unclear whether the associated software (mobile App)
had clearance under 'software as a medical device'
(Therapeutic Goods Administration, 2022). When
selecting devices, the authors found that the non-
regulated devices were relatively cheaper than those
with regulatory clearances. Sometimes the regulated
devices were $100 (AUD) or more expensive than the
non-cleared devices. These high prices may create
access inequalities in implementing remote
monitoring solutions.
It was relatively easy for the end-users to set up
and use the devices. In that regard, most devices were
suitable for practical use. However, integrating the
data collected from these devices in hospital-based
information systems would be difficult as most of
these systems are closed systems that work with their
own App and cloud solutions. Hence, the practical
implementation of remote clinical monitoring would
require medical device vendors and healthcare
information system providers to work together - in
other words, these were not simple 'plug and play'
devices that could be used for implementing practical
integrated solutions with other clinical information
systems. However, it is worth noting that one vendor
organisation, iHealth, provided a promising API in
building interoperability between healthcare software
systems and devices. Significant effort would be
required to link individual patient readings correctly
into their medical records and to overcome the
appropriate authentication and validation measures.
The most alarming finding of this research is that
despite the lack of legitimate access to collected data
through an API, data stream transfers could still be
intercepted through Bluetooth using either Node-
RED, ESP32 or both. This may pose some privacy
risk to individuals who have concerns about their
sensor information and metadata being intercepted
and leaked. In addition, most devices transmit data in
clear formats. iHealth is the only vendor that provided
encryption of the transmitted data, but an individual
static key was used to access the transmitted data of
each of the two iHealth devices tested. Overall,
iHealth devices had the most promising results
regarding practical and secure use.
An Analysis of IoMT Vital Signs Measurement Devices for Practical and Secure Remote Clinical Monitoring
93

6 CONCLUSIONS AND FUTURE
WORK
Motivated by the increasing need for remote
monitoring of patients, in this paper, the authors
investigate whether it is practically possible to use
off-the-shelf vital sign measurement devices for
remote clinical use in a secure manner. A set of
devices (9 in total) were selected to measure the four
vital signs and weight. The devices and software
associated with them (Apps) were examined in detail.
In addition, usage terms and conditions and
regulatory compliance status were explored. With the
help of Node-Red and ESP32, the authors attempted
to intercept the data streams that were communicated
through Bluetooth.
Following review of the selected medical devices
in this paper, the practical use off-the-shelf vital signs
measurement products for remote clinical monitoring
of patients securely appears to be a difficult prospect
to achieve. This is due the fact that the reviewed
products are predominantly closed systems that have
regulatory challenges in terms of integration with
other clinical information systems. Despite this fact,
data from these sensor devices were able to be
intercepted relatively easily, thereby posing some risk
to individual privacy. The authors note there are
promising products in the market, but these still
require significant efforts to achieve practical
solutions.
As for future work, there is the plan to investigate
Bluetooth range testing to measure how far the
devices can maintain connectivity with Node-RED or
ESP32, providing a clearer indication of the
proximity requirements of these sensor devices in
their susceptibility to data interception or other
attacks.
REFERENCES
Chacko, A., & Hayajneh, T. (2018). Security and privacy
issues with IoT in healthcare. EAI Endorsed
Transactions on Pervasive Health and Technology,
4(14), e2-e2.
Fiddler Everywhere. (2022). https://www.telerik.com/
fiddler/fiddler-everywhere
Gerke, S., Shachar, C., Chai, P. R., & Cohen, I. G. (2020).
Regulatory, safety, and privacy concerns of home
monitoring technologies during COVID-19. Nature
medicine, 26(8), 1176-1182.
Github. (2022). Github - Micropython. https://github.
com/micropython/micropython-
lib/tree/master/micropython/bluetooth/aioble
Grand View Research. (2022). mHealth Market Size, Share
& Trends Analysis Report By Component, By Services
(Monitoring Services, Diagnosis Services), By
Participants (Mobile Operators, Devices Vendors), By
Region, And Segment Forecasts, 2022 - 2030.
https://www.grandviewresearch.com/industry-analysis
/mhealth-market
Grindrod, K., Boersema, J., Waked, K., Smith, V., Yang, J.,
& Gebotys, C. (2017). Locking it down: The privacy
and security of mobile medication apps. Canadian
Pharmacists Journal/Revue Des Pharmaciens Du
Canada, 150(1), 60-66.
Hendricks-Sturrup, R. (2022). Pulse Oximeter App Privacy
Policies During COVID-19: Scoping Assessment.
JMIR mHealth and uHealth, 10(1), e30361.
Holman, T. (2022). mHealth (mobile health). https://
www.techtarget.com/searchhealthit/definition/mHealth
Kandhare, A. (2019). Bluetooth Vs. Bluetooth Low
Energy: What’s The Difference? https://medium.
com/@akash.kandhare/bluetooth-vs-bluetooth-low-en
ergy-whats-the-difference-74687afcedb1
Kim, D.-w., Choi, J.-y., & Han, K.-h. (2020). Risk
management-based security evaluation model for
telemedicine systems. BMC Medical Informatics and
Decision Making, 20(1), 1-14.
Knorr, K., Aspinall, D., & Wolters, M. (2015). On the
privacy, security and safety of blood pressure and
diabetes apps. IFIP International Information Security
and Privacy Conference,
Leloglu, E. (2016). A review of security concerns in
Internet of Things. Journal of Computer and
Communications, 5(1), 121-136.
MicroPython. (2022). MicroPython.
https://micropython.org/
Muzny, M., Henriksen, A., Giordanengo, A., Muzik, J.,
Grøttland, A., Blixgård, H., Hartvigsen, G., & Årsand,
E. (2020). Wearable sensors with possibilities for data
exchange: Analyzing status and needs of different
actors in mobile health monitoring systems.
International journal of medical informatics, 133,
104017.
Nick, G. (2022). How Many IoT Devices Are There in
2022? [All You Need To Know]. Tech Jury.
https://techjury.net/blog/how-many-iot-devices-are-
there/#gref
NursingAnswers.net. (2018). Health Observation Lecture:
Measuring and Recording the Vital Signs.
https://nursinganswers.net/lectures/nursing/health-
observation/3-detailed.php
OAIC. (2022a). Health and medical research.
https://www.oaic.gov.au/privacy/the-privacy-
act/health-and-medical-research
OAIC. (2022b). Read the Australian Privacy Principles.
https://www.oaic.gov.au/privacy/australian-privacy-
principles/read-the-australian-privacy-principles
Pahlevanzadeh, B., Koleini, S., & Fadilah, S. I. (2021).
Security in IOT: Threats and vulnerabilities, layered
architecture, encryption mechanisms, challenges and
solutions. International Conference on Advances in
Cyber Security,
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
94

Papa, A., Mital, M., Pisano, P., & Del Giudice, M. (2020).
E-health and wellbeing monitoring using smart
healthcare devices: An empirical investigation.
Technological Forecasting and Social Change, 153,
119226.
Petsas, T., Tsirantonakis, G., Athanasopoulos, E., &
Ioannidis, S. (2015). Two-factor authentication: is the
world ready? Quantifying 2FA adoption. Proceedings
of the eighth european workshop on system security,
Sivaraman, V., Gharakheili, H., & Fernandes, C. (2017).
Inside Job: Security and privacy threats for smart-home
IoT devices. Australian Communications Consumer
Action Network, Sydney.
Talwana, J. C., & Hua, H. J. (2016). Smart world of Internet
of Things (IoT) and its security concerns. 2016 IEEE
international conference on internet of things (iThings)
and IEEE green computing and communications
(GreenCom) and IEEE cyber, physical and social
computing (CPSCom) and IEEE smart data
(SmartData),
Therapeutic Goods Administration. (2022). Regulation of
software based medical devices. https://www.tga.
gov.au/how-we-regulate/manufacturing/medical-devic
es/manufacturer-guidance-specific-types-medical-devi
ces/regulation-software-based-medical-devices
Zhang, C., Shahriar, H., & Riad, A. K. (2020). Security and
Privacy Analysis of Wearable Health Device. 2020
IEEE 44th Annual Computers, Software, and
Applications Conference (COMPSAC),
Zubair, M., Unal, D., Al-Ali, A., & Shikfa, A. (2019).
Exploiting bluetooth vulnerabilities in e-health IoT
devices. Proceedings of the 3rd international
conference on future networks and distributed systems,
An Analysis of IoMT Vital Signs Measurement Devices for Practical and Secure Remote Clinical Monitoring
95
