
Enhancing Men’s Health Management at Home with an Easy-to-Use,
App-Connected Prostate Self-Testing Device
Elisabeth Benke
1a
, Simone Gschaidmeier
2
, Olivier Gentsch
3
, Hannes Deittert
1
,
Sina Martin
1b
, Alexander Preis
1c
and Jörg Franke
1d
1
Institute for Factory Automation and Production Systems, Friedrich-Alexander-Universität Erlangen-Nürnberg, Germany
2
Earliebirdie, Kolbermoor, Germany
3
Digmesa AG, Ipsach, Switzerland
info@digmesa.com, hannes.deittert@fau.de
Keywords: Urology, Uroflowmetry, Benign Prostatic Hyperplasia, Prostate Conditions, Men’s Health.
Abstract: A fundamental problem in men's health is that large groups of men shy away from visiting the doctor, and
specifically, often do not take part in early screening tests if they do not have complaints yet. This is
particularly evident in the sensitive field of urology. Benign prostatic hyperplasia (BPH) is one of the most
widespread disorders in ageing men and is associated with an increasing burden on healthcare systems. It is
often underdiagnosed and undertreated and has a substantial impact on the patients’ quality of life. An altered
urine flow curve can be a first clue to BPH. A new developed, easy-to-use prostate self-testing device based
on a Swiss high-precision flowmeter enables men to check their urine flow at home in familiar surroundings.
Via a Bluetooth connection, the results can be transmitted wirelessly and stored in a digital diary so that long-
term developments can be tracked. The self-testing device not only provides men with the opportunity to deal
with their health with low effort and in a discreet way, but also gives them certainty about their prostate health
status.
1 INTRODUCTION
Benign prostatic hyperplasia (BPH) is one of the most
widespread disorders in ageing men (Madersbacher et
al., 2019) and even argued to be one of the most
common diseases of mankind (Vuichoud & Loughlin,
2015). It is associated with high medical and societal
costs and can have an extremely negative impact on
the quality of life of those affected, as they often
suffer from symptoms such as nocturia that affect
their daily lives and those of their partners. Due to the
ageing society, the disorder may become a rising
socio-economic challenge. (Speakman et al., 2015)
BPH is characterised by a change in the size of the
prostate and is often associated with lower urinary
tract symptoms (LUTS), such as urinary incon-
tinence, reduced flow or feeling of incomplete
emptying, which then usually lead to medical
a
https://orcid.org/0000-0002-6610-4430
b
https://orcid.org/0000-0002-2146-8265
c
https://orcid.org/0000-0003-3469-5982
d
https://orcid.org/0000-0003-0700-2028
consultation (Langan, 2019; Madersbacher et al.,
2019).
A challenge is not only the treatment, but also the
early detection of changes in the prostate. Despite the
distressing symptoms, BPH/LUTS is often under-
diagnosed and undertreated (Speakman et al., 2015)
as large groups of men shy away from going to the
urologist and have insufficient information about
their health status (Müller, 2021). During the
COVID-19 pandemic this problem has further
increased as doctors are visited even less often and
screening services are used less (Nossiter et al.,
2022). It is therefore all the more important to provide
men with an option to assess their urological health
status easily at home.
One of the possible diagnostic methods for the
detection of prostatic disorders is uroflowmetry,
which is non-invasive and by which conditions can be
182
Benke, E., Gschaidmeier, S., Gentsch, O., Deittert, H., Martin, S., Preis, A. and Franke, J.
Enhancing Men’s Health Management at Home with an Easy-to-Use, App-Connected Prostate Self-Testing Device.
DOI: 10.5220/0011778800003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 1: BIODEVICES, pages 182-189
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)

detected based on the urine flow curve. With
Kormoran11, an innovative, handy prostate self-
testing device is developed for practical use in private
environment. It is based on a Swiss high-precision
flowmeter and is currently expanded to include a
Bluetooth-based app connection, which enables the
wireless transfer and storage of flow information in a
digital diary. The device is developed to give men the
opportunity to deal with their own health with a low
hurdle at home and to give them orientation and
security about this sensitive topic. Deliberately, the
focus is on a simple, intuitive and comprehensible
design without overwhelming the user with
information.
This paper will first provide an overview of BPH
and the increasing socio-economic challenges
associated with it, before introducing the
Kormoran11 device, its functionality and its testing.
1.1 BPH: Prevalence, Symptoms and
Diagnosis
BPH affects 30-40% of men over the age of 30 and
the prevalence increases almost linearly with age to
70-80% in men over 80 years (Madersbacher et al.,
2019). Also the prevalence of LUTS increases with
age: while around 50% of men over the age of 60
suffer from BPH-caused symptoms, the rate is
already 80% for men over 80 (Miernik & Gratzke,
2020). The symptoms can be divided into different
categories, e.g. storage symptoms such as increased
urination frequency, urination at night or urinary
incontinence, or voiding symptoms such as a slow,
reduced or intermitted stream or terminal dribble
(Gravas & Melekos, 2009; Miernik & Gratzke, 2020).
For BPH diagnosis and in order to assess the
severity of LUTS, the American Urological Associ-
ation (AUA) created the International Prostate Sym-
ptom Score (IPSS), a screening tool consisting of
eight questions. This procedure has also been adopted
by the World Health Organization (WHO). The
questionnaire refers to BPH-related symptoms such
as nocturia, weak urinary stream or incomplete
emptying as well as the patient’s quality of life. Each
answer given by the patient is scored from 0 to 5
points. The total score correlates with the severity of
the symptoms, up to ‘severely symptomatic’ (20 to 35
points). (Barry et al., 1992; Cockett, 1991)
1.2 Socio-Economic Challenges
Due to the high prevalence in the ageing population,
BPH not only presents a medical but also a growing
socio-economic challenge. The economic burden of a
disease is not only composed of direct costs for the
affected patients, such as medication or interventions,
but essentially also of indirect costs to be shouldered
by society, as workforce or participation in public life
may be decreased. According to an estimate by
(Welliver et al., 2022), the cost of treating all men
over 40 in the United States was at least $1.9 billion
in 2013. It is emphasised that these costs are a
minimum due to few non-covered populations and do
not include indirect costs. The authors also found a
steady increase in expenditures by age group, which
is consistent with the age-related increase in the
prevalence of LUTS/BPH. A 2005 study states that
the cost associated with a BPH diagnosis in the US
was $1,536 per year. The authors found that the
average employee with BPH missed 7.3 hours of
work per year, with about 10% of the considered
group reporting some missed work related to BPH
health care encounter. The sum of direct and indirect
BPH-related costs was estimated to be $3.9 billion
annually. (Saigal & Joyce, 2005) Several studies
assessed the LUTS/BPH-related burden for patients
and society and suspect that these will potentially
increase as the proportion of older men in the
population increases. (Devlin et al., 2021; Speakman
et al., 2015; van Exel et al., 2006)
1.3 Early Urological Screenings –
Situation in Germany and
Influence of the COVID-19
Pandemic
Early detection of changes in the size of the prostate
volume enable early observation and treatment of
symptoms. Studies show that only a few men suffer
from LUTS that can be directly attributed to prostate
cancer. However, a change in the prostate size is not
always benign and if a nodular abnormality is present
there is a chance that biopsy will result in a diagnosis
of prostate cancer. (Chang et al., 2012)
For early detection of changes in the prostate,
there is therefore the possibility of in-office
screenings by the urologist. In Germany, an annual
inspection of the external genitalia and palpation of
the prostate are reimbursed by health insurance funds
for all men over the age of 45. However, a 2022 health
insurance research report states that this examination
was only claimed by 21.7% of eligible men in 2020.
(Grobe et al., 2022) Prostatahilfe Deutschland
(Prostate Aid Germany) assumes various causes for
this: shame about unpleasant examinations, fear of a
drastic diagnosis or the understanding of many men
that a doctor is only necessary when they actually
have a health problem and do not seek health care
Enhancing Men’s Health Management at Home with an Easy-to-Use, App-Connected Prostate Self-Testing Device
183

without complaints. In addition, some men are simply
not used to talking about their physical or mental
sensitivities. (Müller, 2021) Figures in the report in
(Grobe et al., 2022) further suggest that the COVID-
19 pandemic may have led to even fewer people
taking advantage of early prostate screenings.
Compared to 2019, the number of men undergoing
the examination has decreased by 7.7%.
This connection with the COVID-19 pandemic is
underlined by further recent studies. Nossiter et al.
found that the number of men newly diagnosed with
prostate cancer in 2020 after the first lockdown
decreased by 30.8% in England compared to the same
period in 2019, while those diagnosed were at a more
advanced stage of disease. (Nossiter et al., 2022) A
Swedish study by Fallara et al. comes to a similar
conclusion. During the period of March - June 2020
36% fewer cases of prostate cancer were registered
compared to the corresponding periods in 2017 -
2019. The greatest decrease of 51% was seen in men
aged 75 and older. In contrast, there was no decrease
in the numbers of patients receiving cancer curative
treatments. (Fallara et al., 2021) There is a strong
presumption that there is a link between habits
changed by the COVID-19 pandemic and the use of
health services, which has a particular impact on older
people.
2 PROSTATE SELF-TESTING
DEVICE FOR DISCREET USE
AT HOME
Since large proportions of men shy away from
professional urological in-office examinations, a need
arises for options to discreetly deal with the health of
their prostate at home. With Kormoran11, an
innovative, handy flowmeter is developed for
practical use in private environment. The self-testing
device evaluates the urine flow curve and thus gives
clues to the impairment of it by an enlarged prostate.
The latest research approaches also deal with the
extension to wireless evaluation and storage of the
data in an app application. The device is patented
under DE Patent No. 10 2014 008 760 B4 (Beck-
Gschaidmeier & Simmons, 2014).
A challenge with regard to BPH diagnosis is that
the patient self-assesses the severity of his LUTS
when using the IPSS tool described in 1.1. An
objective assessment of the severity of his symptoms
is hardly possible with this procedure; moreover, the
patient has to remember all micturition situations of
the last month and several pages of paper have to be
filled out by hand. The Kormoran11 is supposed to
offer a better alternative for this procedure that is
quicker and less complicated. Especially with regard
to question 5 of the IPSS (Barry et al., 1992) the
device can be a suitable substitute:
Over the past month, how often have you had a weak
urinary stream?
o Not at all (0 points)
o Less than 1 time in 5 (1 point)
o Less than half the time (2 points)
o About have the time (3 points)
o More than half the time (4 points)
o Almost always (5 points)
2.1 Basics of Uroflowmetry
Uroflowmetry is a recognised procedure to confirm
the suspicion of bladder emptying disorders in men.
It records the volume of urine leaving the urethra per
unit time during a micturition. The result is the urine
flow rate measured in mL/sec, which can be displayed
as urine flow curve. Uroflowmetry has the advantage
of being non-invasive and does not require the use of
a catheter. It can therefore be used in almost all
patient groups with suspected bladder emptying
disorders. The measured maximum urine flow rate
Q
max
is the parameter that plays the most important
role in clinical observation and is considered reliable
and easily comparable regarding prognostic and post-
therapeutic assessments. It is, however, important to
ensure that the micturition volume is at least 150 mL,
otherwise the validity of the measurement is limited.
(Hautmann & Gschwend, 2014; Schultz-Lampel et
al., 2012)
The normal urinary flow curve is bell-shaped and
may be slightly flatter on the right side. The urine
flow increases continuously to reach a peak and then
decreases. Figure 1 shows the typical course of a flow
curve.
Figure 1: Schematic representation of a normal urinary flow
curve. (Schultz-Lampel et al., 2012).
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
184
Some subsequent dripping, as shown in Figure 1
by the two posterior maxima, may occur and is not
necessarily a pathological symptom.
A maximum flow rate of more than 20 mL/sec is
often considered normal. However, this rough
guideline is subject to restrictions and cannot be
generalised as the flow rate depends on the voiding
volume, age and sex. According to the ‘Liverpool
nomogram’ by Haylen et al. which aims to better
distinguish normal urine flow values from
pathological values for different population groups,
the curve of the 25th percentile of men > 50 years
shows a maximum flow rate of approx. 11 mL/sec at
a voiding volume of 150 mL. As the voiding volume
increases, the flow rate of the considered group
increases to about 15 mL/sec at 500 mL. (Haylen et
al., 1989) In the guideline on therapy of benign
prostatic syndrome, published by the association of
German urologists, a flow rate with Q
max
< 10 mL/sec
is considered ‘reduced’ and may indicate an
obstruction of the urine flow. (Dreikorn & Höfner,
2014) In general, Q
max
> 12…15 mL/sec is
considered 'normal' in the literature, even though it
must be mentioned that parameters in uroflowmetry
are subject to great variation and a definitive normal
range cannot be defined. (Jarvis et al., 2012)
2.2 Home Uroflowmetry
The idea of home uroflowmetry was first suggested
by Blaivas in 1988 to counter disadvantages of single-
episode office uroflowmetry (Boci et al., 1999).
Literature indicates that the latter procedure may not
be sufficiently reliable to detect certain BPH-related
voiding dysfunctions since many patients are unable
to relax and void urine in a normal way in clinical
environment. In addition, possible variations between
consecutive flow measurements and circadian
changes may have an impact on various voiding
parameters, specifically on the peak flow rate.
(Golomb et al., 1992)
Boci et al. conducted a study in 1999 to
compare home uroflowmetry to conventional, free
office uroflowmetry. 25 male patients at a mean age
of 67 years with symptomatic BPH performed both
free and home uroflowmetry. It was found that 80%
of the investigated patient group considered home
uroflowmetry simpler and more acceptable. 60% of
the patient group felt psychologically better using
home uroflowmetry. However, the crucial restriction
was found that the device to be used at home must be
explained to the patient in an understandable way.
(Boci et al., 1999)
2.3 Device Architecture and
Functionality
The aim was to develop a device with which the urine
flow can be checked at home in familiar surroundings
to give men certainty about their health status. From
the literature and clinical feedback, the self-testing
device should be easy to use and understand by non-
professionals. The Kormoran11 is intended to serve
for self-monitoring in case of a suspected new
decrease in urine flow, to observe the consequences
of medication treatment or after surgical intervention
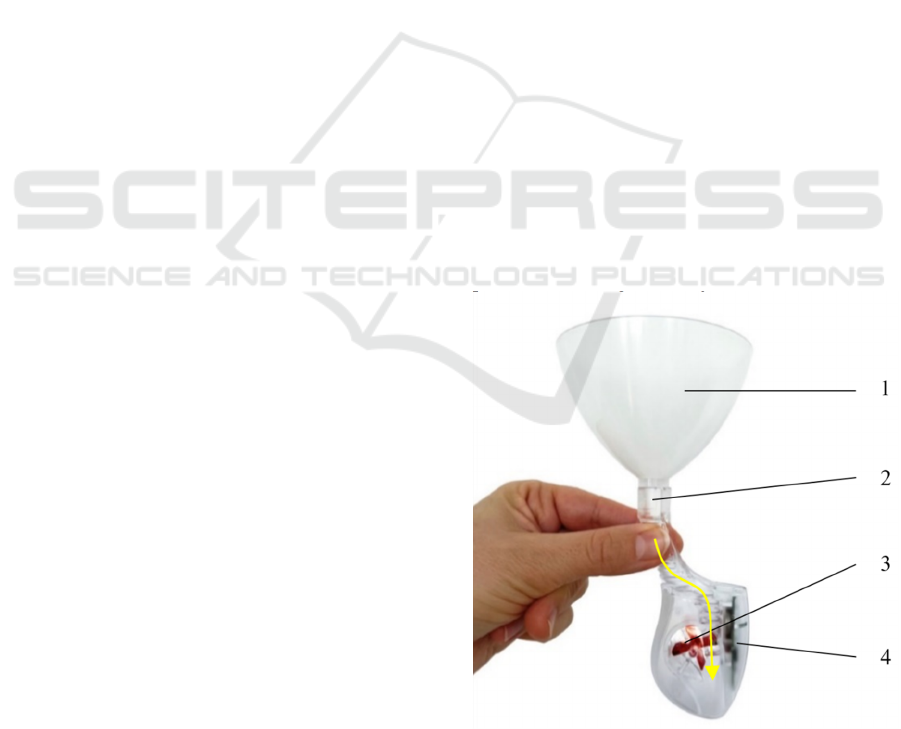
on the urethra or prostate. As pictured in Figure 2, the
device consists of a funnel and a measuring unit in
which the flow rate is evaluated. A high precision
turbine-based flow measurement method (Digmesa
AG, Ipsach, Switzerland) is used for this purpose. The
sensor system consists of a reed switch, which is
integrated in the circuit board, and permanent
magnets, with which 2 of the 4 turbine blades are
equipped. To set the turbine in rotation, the outer area
of the rotor blades is exposed to the flow, as indicated
in Figure 2. When the user urinates into the funnel,
the flow is directed through the measuring unit and
leaves it at the outlet. To assess the urine flow, the
measured peak value of the flow curve is compared
with the maximum flow rate of Q
max
=11 mL/sec. If
the critical value is exceeded, a green led lights up on
the device when the measurement is completed;
otherwise, there is a red led signal. The housing of the
pictured measuring unit is injection moulded.
Figure 2: Prostate Self-Testing-Device Kormoran11,
consisting of a funnel (1) into which urine is passed, a flow
channel (2), the flow measuring unit (3) and a circuit board
with microcontroller, reed switch, battery and LED lights (4).
The yellow arrow indicates the course of the flow channel.
Enhancing Men’s Health Management at Home with an Easy-to-Use, App-Connected Prostate Self-Testing Device
185
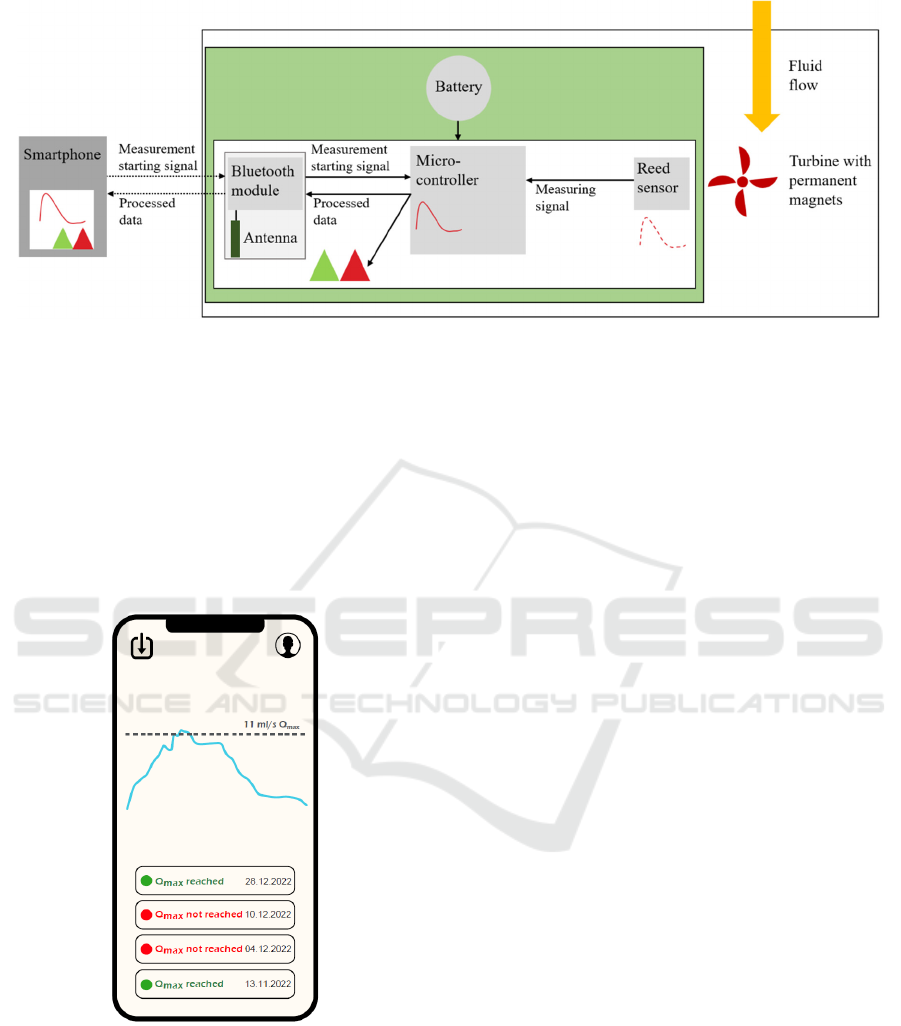
Figure 3: Schematic diagram of the device architecture and the integrated circuit board. The outer white box represents the
Kormoran11 device, the circuit board is shown in green. It is equipped with the nRF52832 Bluetooth Low Energy Module
by Adafruit. The processing of the measurement data takes place on the circuit board so that information can be provided also
directly on the device via the red and green led lights (indicated by the red and green triangles).
A digital version of the device contains a Bluetooth
module, which allows the wireless transmission of the
results to a smartphone. There the measured data can
be stored in a flow rate diary in order to track long-
term developments, which can give the user and
urologist indications of possible pathological
changes.
Figure 4: Prototyped user interface of the flow rate diary.
Green and red dots indicate whether the target value
Q
max
=11 mL/sec has been reached or not.
Figure 3 shows a schematic diagram of the device
architecture. For the Bluetooth connection, the
integrated circuit board is equipped with the
nRF52832 Bluetooth Low Energy Module by
Adafruit (New York, United States). It has a BLE
radio (Nordic Semiconductor, Trondheim, Norway),
the supporting circuit and a Bluetooth antenna already
integrated and measures only 10 x 16 mm. The
processing of the measurement data takes place on the
board so that it can provide information also directly
on the device via the red and green led lights. For app
connected use, the device is placed next to a
Bluetooth-enabled smartphone and the recording can
be started in the app. The flow data is then transmitted
continuously during the measurement, followed by
the red or green indicator. In the app the result of the
measurement is provided with the date and time, so
that the flowmetry results can be observed over a
longer period. Figure 4 shows the prototyped user
interface. Green and red dots indicate whether the
target value of Q
max
=11 mL/sec has been reached on
certain days or not.
2.4 Testing of the Device
Functionality and accuracy of the Kormoran11 were
determined in laboratory in various flowmetry tests
on a test bench. Water was used as the test liquid. A
measuring programme with 13 measurement points
was carried out for each test. On the test bench, which
is pictured in Figure 5, the flow rate is varied with the
aid of a controllable flow regulator. To determine the
average flow rate, a valve is opened for a
measurement period of 7 seconds and the amount of
liquid passed is measured using digital scales. As
water passes through the measuring unit of the device,
it causes the turbine to rotate. The rotation of the
turbine blades is detected magnetically and converted
into electric pulses. The sensor pulse frequency is
directly related to the turbine speed and thus to the
flow velocity.
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
186
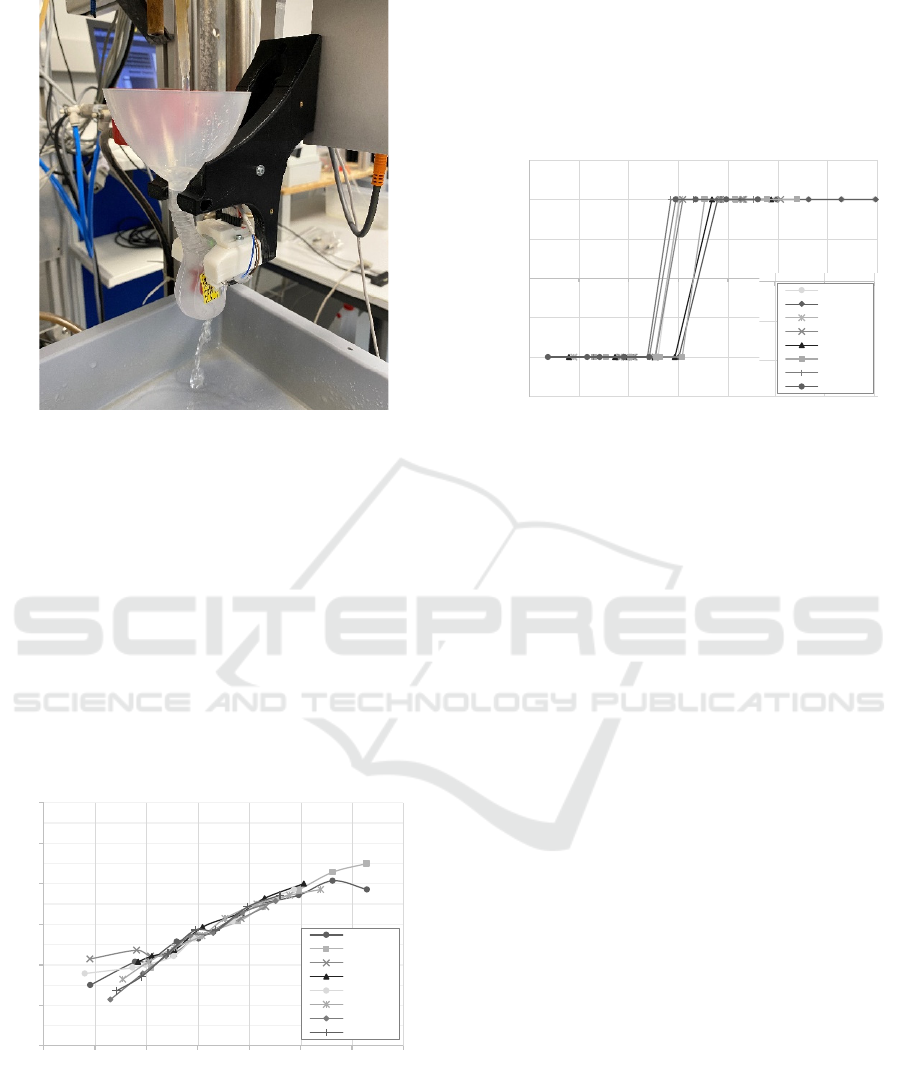
Figure 5: Laboratory testing of the Kormoran11 device on
a test bench. The flow rate can be varied using a
controllable flow regulator; the amount of liquid passed is
measured using digital scales.
Figure 6 shows the relationship between the
frequency of detected sensor pulses and the flow rate
around the critical range of the switching point over a
measurement series consisting of eight single measur-
ements. This gives information about the
performance of the sensor over the flow rate. The
resulting curve is used to calibrate the device and
requires repeatability and linearity. It can be seen that
from about 580 mL/min the curves lie well together
on almost a straight line, which shows good repetition
over the test series.
Figure 6: Detected sensor pulses as a function of the flow
rate around the critical range of the desired switching point
of 0.66 L/min.
In order to show the accuracy and reliability of the
sensor unit, the LED switching points from RED to
GREEN were also examined in various tests. Figure 7
shows the results of an exemplary series with eight
single measurements. A value of −1 corresponds to
RED and +1 corresponds to GREEN. This allows the
display of the flow rate at which the transition from
RED to GREEN was indicated for each test in the
series.
Figure 7: Switching point from RED to GREEN for a
measurement series of eight tests. A value of -1 corresponds
to RED and +1 corresponds to GREEN.
From Figure 7 it can be observed that below
588 mL/min the sensors in all tests indicate RED, the
first sensor indicating GREEN does so at
635 mL/min. The last sensor to indicate RED is at
658 mL/min. At 729 mL/min, all sensors indicate
GREEN. The aim was to reliably determine the value
of 660 mL/min (equals Q
max
=11 mL/sec) with a band
of +/-10%, i.e. from 594 to 726 mL/min. This can be
confirmed by this series of measurements.
3 CONCLUSIONS
In this paper, the newly developed, easy-to-use
prostate self-testing device Kormoran11 is presented,
which enables men to assess their urine flow simply
and discreetly in the familiar surroundings of their
own home. The application of the device represents
not only a low hurdle when men do not want to go to
the urologist or first approach the sensitive subject
themselves. It also enables repeated and regular
measurement to obtain as much certainty as possible
despite fluctuating parameters that have an influence
on urine flow, such as circadian changes. The
Kormoran11 signals whether normal urine flow is
ensured and indicates possible changes in the
prostate, bladder or urethra. The device has been
shown to operate accurately and to have high
repeatability in detecting the set Q
max
value of
11 mL/sec. The operation is simple and the indication
with a red and green led light is easy to understand.
6
8
10
12
14
16
18
350 450 550 650 750 850 950 1050
Pulses (sec
-
1
)
Flow rate (mL/min)
Sample 1
Sample 2
Sample 3
Sample 4
Sample 5
Sample 6
Sample 7
Sample 8
-1,5
-1
-0,5
0
0,5
1
1,5
3504505506507508509501050
LED signal (+1 GREEN, -1 RED)
Flow rate (mL/min)
Sample 1
Sample 2
Sample 3
Sample 4
Sample 5
Sample 6
Sample 7
Sample 8
Enhancing Men’s Health Management at Home with an Easy-to-Use, App-Connected Prostate Self-Testing Device
187

In a version without app connection, the Kormoran11
is already approved as a medical device and available
on the market.
The digital functions and the app connection were
introduced specifically at the suggestion of the
urologists accompanying the project. It is expected
that the possibility of observing the long-term
development of measurements will enable a better
medical assessment and that the device will also be
accepted and used by younger users. However, with
regard to the older target group, it should be noted that
a digital connection is not necessary to fulfil the
function of Kormoran11.
It must be emphasised that the self-test result can
only be a first indication and that the final diagnosis
by a urologist is essential. The device is intentionally
not a measuring instrument, but serves to introduce
men to the sensitive subject in a simple way and to
familiarise themselves with their prostate health
status. The user is educated that a red light means that
the current flow is too weak. He is instructed to repeat
the measurement on other days at other times in that
case. If the signal is predominantly red, a visit to the
doctor is advised.
In conclusion, the authors are convinced that this
work can make a great contribution to men's health.
However, future studies need to test the willingness
of men to purchase and use the Kormoran11 device
and further development work is needed to make the
app-connected version ready for series production. In
addition to home use, it is also conceivable that the
device could be used in day care, nursing homes and
general practitioners’ offices.
ACKNOWLEDGEMENTS
This project was partly funded by the Bavarian
Ministry of Economic Affairs, Regional Develop-
ment and Energy. The patent process was funded by
the Federal Ministry for Economic Affairs and
Energy as part of the SIGNO initiative. The authors
would further like to express their gratitude for the
medical support provided to the project by
Prof. Thomas Ebert, Head of the Prostate Centre of
the Nuremberg Metropolitan Region, St. Theresien
Hospital Nuremberg.
REFERENCES
Barry, M. J., Fowler, F. J., O’Leary, M. P., Bruskewitz, R.
C., Holtgrewe, H. L., Mebust, W. K., & Cockett, A. T.K.
(1992). The American Urological Association
Symptom Index for Benign Prostatic Hyperplasia. The
Journal of Urology, 148(5 Part 1), 1549–1557.
https://doi.org/10.1016/S0022-5347(17)36966-5
Beck-Gschaidmeier, S., & Simmons, C. T. (2014).
Harnflussmessgerät,(DE Patent, 10 2014 008 760 B4).
Boci, R., Fall, M., Waldn, M., Knutson, T., & Dahlstrand,
C. (1999). Home uroflowmetry: Improved accuracy in
outflow assessment. Neurourology and Urodynamics,
18(1), 25–32. https://doi.org/10.1002/(SICI)1520-
6777(1999)18:1<25::AID-NAU5>3.0.CO;2-O
Chang, R. T. M., Kirby, R., & Challacombe, B. J. (2012).
Is there a link between BPH and prostate cancer? The
Practitioner, 256(1750), 13-6, 2.
Cockett, A. T. K. (1991). The international consultation on
benign prostatic hyperplasia (BPH): Proceedings,
Paris, June 26-27, 1991. International Scientific
Committee.
Devlin, C. M., Simms, M. S., & Maitland, N. J. (2021).
Benign prostatic hyperplasia - what do we know? BJU
International, 127(4), 389–399. https://doi.org/
10.1111/bju.15229
Dreikorn, K., & Höfner, K. (2014, November 16). S2e
Leitlinie „Therapie des Benignen Prostatasyndroms
(BPS)“ (Leitlinienreport AWMF-Register-Nummer
(043-035)).
Fallara, G., Sandin, F., Styrke, J., Carlsson, S., Lissbrant, I.
F., Ahlgren, J., Bratt, O., Lambe, M., & Stattin, P.
(2021). Prostate cancer diagnosis, staging, and
treatment in Sweden during the first phase of the
COVID-19 pandemic. Scandinavian Journal of
Urology, 55(3), 184–191. https://doi.org/10.1080/
21681805.2021.1910341
Golomb, J., Lindner, A., Siegel, Y., & Korczak, D. (1992).
Variability and Circadian Changes in Home
Uroflowmetry in Patients with Benign Prostatic
Hyperplasia Compared to Normal Controls. The
Journal of Urology, 147(4), 1044–1047. https://doi.org/
10.1016/S0022-5347(17)37462-1
Gravas, S., & Melekos, M. D. (2009). Male lower urinary
tract symptoms: How do symptoms guide our choice of
treatment? Current Opinion in Urology, 19(1), 49–54.
https://doi.org/10.1097/MOU.0b013e32831505fe
Grobe, T. G., Braun, A., & Szecsenyi, J. (2022). BARMER
Arztreport 2022: Coronapandemie - Auswirkungen auf
Gesundheit und Versorgung. Berlin.
Hautmann, R., & Gschwend, J. E. (Eds.). (2014). Springer-
Lehrbuch. Urologie (5. Aufl. 2014). Springer Berlin
Heidelberg. http://nbn-resolving.org/urn:nbn:de:bsz:
31-epflicht-1544725
Haylen, B. T., Ashby, D., Sutherst, J. R., Frazer, M. I., &
West, C. R. (1989). Maximum and average urine flow
rates in normal male and female populations--the
Liverpool nomograms. British Journal of Urology,
64
(1), 30–38. https://doi.org/10.1111/j.1464-410x.
1989.tb05518.x
Jarvis, T. R., Chan, L., & Tse, V. (2012). Practical
uroflowmetry. BJU International, 110 Suppl 4, 28–29.
https://doi.org/10.1111/bju.11617
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
188

Langan, R. C. (2019). Benign Prostatic Hyperplasia.
Primary Care, 46(2), 223–232. https://doi.org/10.
1016/j.pop.2019.02.003
Madersbacher, S., Sampson, N., & Culig, Z. (2019).
Pathophysiology of Benign Prostatic Hyperplasia and
Benign Prostatic Enlargement: A Mini-Review.
Gerontology, 65(5), 458–464. https://doi.org/10.1159/
000496289
Miernik, A., & Gratzke, C. (2020). Current Treatment for
Benign Prostatic Hyperplasia. Deutsches Arzteblatt
International, 117(49), 843–854. https://doi.org/
10.3238/arztebl.2020.0843
Müller, I. (2021). Früherkennung von Prostatakrebs:
Männer gehen weiterhin nicht hin. https://www.
prostata-hilfe-deutschland.de/prostata-news/frueherke
nnung-prostatakrebs-maenner-gehen-nicht-hin
Nossiter, J., Morris, M., Parry, M. G., Sujenthiran, A.,
Cathcart, P., van der Meulen, J., Aggarwal, A., Payne,
H., & Clarke, N. W. (2022). Impact of the COVID-19
pandemic on the diagnosis and treatment of men with
prostate cancer. BJU International, 130(2), 262–270.
https://doi.org/10.1111/bju.15699
Saigal, C. S., & Joyce, G. (2005). Economic costs of benign
prostatic hyperplasia in the private sector. The Journal
of Urology, 173(4), 1309–1313. https://doi.org/
10.1097/01.ju.0000152318.79184.6f
Schultz-Lampel, D., Goepel, M., & Haferkamp, A. (Eds.).
(2012). Urodynamik: Akademie der Deutschen
Urologen (3. Aufl. 2012). Springer Berlin Heidelberg.
http://nbn-resolving.org/urn:nbn:de:bsz:31-epflicht-15
30263
Speakman, M., Kirby, R., Doyle, S., & Ioannou, C. (2015).
Burden of male lower urinary tract symptoms (LUTS)
suggestive of benign prostatic hyperplasia (BPH) -
focus on the UK. BJU International, 115(4), 508–519.
https://doi.org/10.1111/bju.12745
Statistisches Bundesamt. (2021). Number of people aged 67
or over will grow 22% by 2035: Press release No. 459
of 30 September 2021 [Press release].
https://www.destatis.de/EN/Press/2021/09/PE21_459_
12411.html
van Exel, N. J. A., Koopmanschap, M. A., McDonnell, J.,
Chapple, C. R., Berges, R., & Rutten, F. F. H. (2006).
Medical consumption and costs during a one-year
follow-up of patients with LUTS suggestive of BPH in
six european countries: Report of the TRIUMPH study.
European Urology, 49(1), 92–102. https://doi.org/10.
1016/j.eururo.2005.09.016
Vuichoud, C., & Loughlin, K. R. (2015). Benign prostatic
hyperplasia: Epidemiology, economics and evaluation.
The Canadian Journal of Urology, 22 Suppl 1, 1–6.
Welliver, C., Feinstein, L., Ward, J. B., Kirkali, Z.,
Martinez-Miller, E., Matlaga, B. R., & McVary, K.
(2022). Evolution of healthcare costs for lower urinary
tract symptoms associated with benign prostatic
hyperplasia. International Urology and Nephrology,
54(11), 2797–2803. https://doi.org/10.1007/s11255-
022-03296-0.
Enhancing Men’s Health Management at Home with an Easy-to-Use, App-Connected Prostate Self-Testing Device
189
