
Digital Therapeutics for Healthy Longevity: A Roadmap
Tim Leistner
1a
and Tobias Kowatsch
1,2,3 b
1
School of Medicine, University of St. Gallen, St. Gallen, Switzerland
2
Institute for Implementation Science in Health Care, University of Zurich, Zurich, Switzerland
3
Centre for Digital Health Interventions, Department of Management, Technology, and Economics,
ETH Zürich, Zurich, Switzerland
Keywords: Healthy Longevity, Digital Therapeutics, Scalability, Platform Business Model, Innovation, mHealth.
Abstract: Non-communicable diseases (NCDs), including common mental disorders, not only impose an enormous
health burden on individuals but also lead to substantial economic burdens for healthcare systems. Especially
individuals with lower socioeconomic status are affected by NCDs. Digital therapeutics (DTx) have the
potential to offer low-cost personalized interventions easing the burden of NCDs and addressing inequalities
in health. This position paper highlights the importance of preventive care and offers a roadmap toward DTx
for healthy longevity.
1 INTRODUCTION
Non-communicable diseases (NCDs) such as cancer,
cardiovascular diseases or diabetes, and common
mental disorders (CMDs) such as depression or
anxiety not only pose an enormous health burden on
individuals but also lead to substantial health
economic challenges for healthcare systems
(Jacobson et al., 2023; Vandenberghe & Albrecht,
2020). In 2012 NCDs were the leading cause of death
(WHO, 2014). Numbers increased to approximately
73% of all deaths by 2017 (Roth et al., 2018). NCDs
also lead to a major economic burden for NCD
households. Especially the population in lower-
income countries and China is affected by costs
associated with NCDs (Murphy et al., 2020). Also, in
developed countries like Switzerland NCDs account
for about 80% of the health costs (Wieser et al.,
2014). Unmodifiable risk factors for the development
of NCDs are age, genetics, and environmental factors.
Modifiable factors primarily relate to aspects of
lifestyle, for example, tobacco and excessive alcohol
consumption, low daily activity, food choices, and
lack of resilience. Especially individuals with low
socioeconomic status are substantially affected by
NCDs (Mackenbach et al., 2008), a highly relevant
socioeconomic inequity (Federal Office of Public
a
https://orcid.org/0000-0003-2808-8123
b
https://orcid.org/0000-0001-5939-4145
Health, 2016). At the same time, this group is
underrepresented in clinical trials (Davis et al., 2019;
Sharrocks et al., 2014). This fact leads to an important
problem as clinical trials that aim at developing novel
digital therapeutics (DTx), i.e., evidence-based
software for the prevention, management, and
treatment of disease (Digital Therapeutics Alliance,
2019), may not work for those individuals with a
lower socioeconomic status. Thus, DTx may not at all
lower the socioeconomic inequalities in health and
thus, will also not reduce the health and economic
burden of NCDs and CMDs (Carrilero et al., 2021;
Kowatsch, 2023).
To this end, we recommend a paradigm shift
where healthcare systems depart from curative care
and incentivize primary, secondary, and tertiary
prevention. We, therefore, highlight the importance
of scalable DTx for healthy longevity and that these
DTx are also effective in vulnerable individuals with
lower socioeconomic status.
Next, we outline a roadmap toward DTx for
healthy longevity. We provide a list of stakeholders
that may be important in pushing forward innovation
in this area with substantial societal impact. Then, the
building blocks of DTx and potential business
opportunities are discussed. Here, we provide two
examples of corresponding initiatives in Switzerland
616
Leistner, T. and Kowatsch, T.
Digital Therapeutics for Healthy Longevity: A Roadmap.
DOI: 10.5220/0011778500003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 5: HEALTHINF, pages 616-622
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
and Singapore. We close this position paper with a
discussion and outline of future work.
2 ROADMAP
The WHO defines healthy aging as “the process of
developing and maintaining the functional ability that
enables well-being in older age” (WHO, 2015, p.
228). Healthy longevity extends this definition to all
stages of life: “Health is a state of complete physical,
mental and social well-being and not merely the
absence of disease or infirmity” (WHO, 2006, p. 1).
Therefore, a holistic approach to DTx is required, an
approach that does not neglect social or psychological
well-being. DTx for healthy longevity are defined as
DTx for primary, secondary, and tertiary prevention.
DTx for healthy longevity have, therefore, the overall
goal to maximize the average quality of life and
ensure that the increased lifespan is accompanied by
an increased health span (Beard et al., 2016; Chen et
al., 2018). For such DTx to be successfully deployed,
healthcare systems must support innovative
ecosystems, the development of novel DTx, and
business models.
2.1 Innovative Ecosystem
Developing DTx for healthy longevity requires an
innovative ecosystem of stakeholders that combine
complementary expertise from various disciplines.
We conducted expert interviews with medical
doctors, DTx experts, payers (health insurers), as well
as technology and innovation managers from both
academia and the healthcare industry.
The following stakeholders were identified to be
essential for such an innovative ecosystem:
policymakers, regulatory and public health bodies,
experts in biomedical ethics, public and private
hospitals, healthy and patient populations, patient
organizations, academic health institutions (e.g.,
medical and public health schools), digital health
start-ups, biomedical laboratories, physiotherapists,
nursing facilities, health and stress management
coaches, diet and nutrition experts, hospitality
facilities, and corporate health care units. These
stakeholders together can establish new DTx with a
holistic focus on mental, physical, and social health.
We also identified local initiatives and
educational programs at universities, like executive
education, to promote innovation in DTx for healthy
longevity and dedicated DTx innovation and
accelerator programs (e.g., the Dartmouth Innovation
Accelerator for Digital Health). Moreover, DTx
design and trial platforms are required, such as
Ethicadata.com, Mahalo.health, or MobileCoach.eu.
2.2 Digital Therapeutics
DTx for healthy longevity can trigger personalized
preventive care support at opportune moments
(receptive states) in case a vulnerable state is detected
or predicted (Nahum-Shani et al., 2023; Keller et al.,
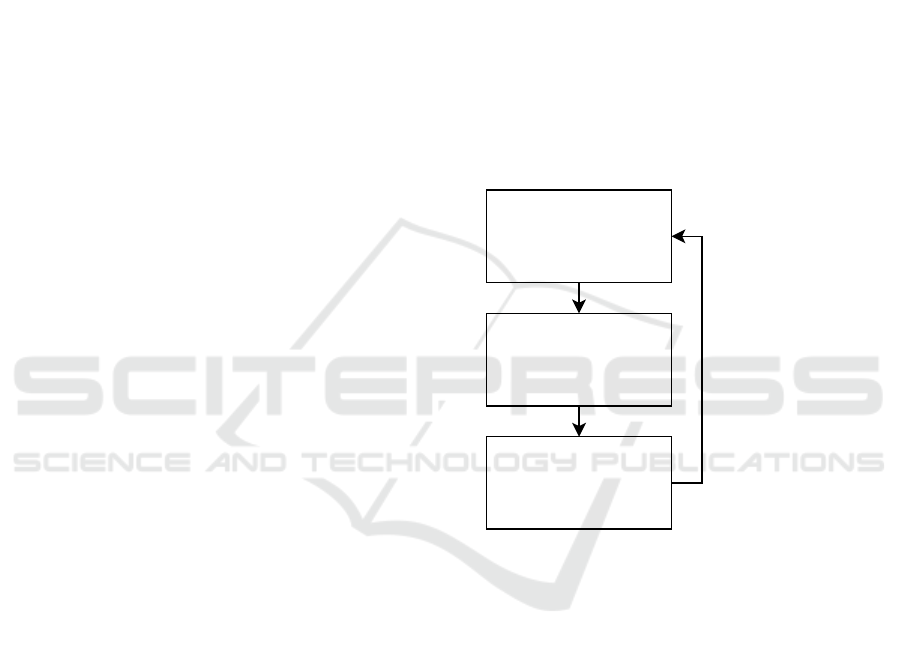
2023). To this end, the three building blocks of DTx
cover states of vulnerability, states of receptivity, and
personalized support as depicted in Fig. 1. Moreover,
DTx also have the potential to improve themselves
with every human-DTx interaction, for example,
through reinforcement learning algorithms (Liao et
al., 2020). Each of the three building blocks is
discussed in the following sections, as well as a
design and evaluation framework for DTx.
Figure 1: Building blocks of a DTx (adapted from Keller et
al. 2023, Fig. 6.1, p. 67).
2.2.1 State of Vulnerability
First, for a DTx to decide on personalized support, a
specific state of vulnerability must be measured or
predicted. A vulnerable state is a ”person’s transient
tendency to experience adverse health outcomes or to
engage in maladaptive behaviors” (Nahum-Shani et
al., 2015, p. 3). Therefore, the first step in developing
an effective DTx is to measure or – if possible – even
predict adverse health outcomes or maladaptive
behaviors by using relevant sensor data streams or
patient-reported outcome data. Examples are the
measurement of nocturnal breathing signals for early
detection of Parkinson’s disease (Yang et al., 2022)
or acoustic cough detection to assess asthma control
or predict attacks (Tinschert et al., 2020). Digital
biomarkers can also be used in primary prevention.
State of vulnerability
e.g. stress at work via mouse
movements, high heart rate or
nocturnal breathing signals
State of receptivity
e.g. getting ready for bed
information based on contextual
factors of location and time
Personalized support
e.g. via conversational agents,
smart speakers or healthcare
robots
A learning system that adapts to
interpersonal differences and
optimizes the support
Digital Therapeutics for Healthy Longevity: A Roadmap
617

For example, it has been shown that stress at the
workplace can be measured via computer mouse
movements (Banholzer et al., 2021). More basic
biomarkers include step count, heart rate, and average
sleep duration and quality per night.
Recent improvements in consumer technology
(e.g., wearables, smartphones, smart speakers, or
smart TVs) further increase the quality of sensor data.
Accordingly, “mobile health technologies are
evolving from descriptive monitoring tools to digital
diagnostics and therapeutics” (Sim, 2019, p. 965);
this evolution of data streams requires more work
before digital biomarkers can improve patient
outcomes (Carovos et al., 2019).
2.2.2 State of Receptivity
New technologies also enable more effective means
of how and when to deliver support by DTx. Context-
aware notification management systems on
smartphones or smartwatches can increase the
response rate to notifications (Künzler et al., 2017,
2019; Mishra et al., 2021). For example, support is
better perceived when engaged in working, studying
or when getting ready for bed (Choi et al., 2019).
Contextual factors, such as geolocation or time, can
therefore influence states of receptivity. To this end,
effective DTx deliver personalized support at the
right time, i.e., the target is in a state of receptivity,
after a vulnerable state was measured or predicted.
However, such context-aware DTx may also raise
privacy and data security concerns which, in turn, can
represent substantial adoption barriers. It is, therefore,
of utmost importance to comply with any legal,
ethical, and regulatory requirements.
2.2.3 Personalized Support
Virtual or augmented reality, healthcare robots, or
smart speakers allow for a new way of delivering
personalized support with conversational agents
(CAs) such as chatbots or virtual assistants like
Amazon’s Alexa or Apple’s Siri (Kowatsch and
Fleisch, 2021). CAs are computer programs that
mimic human conversation via voice or text chat
(Bickmore & O’Leary, 2023). Humans can perceive
CAs as social actors (e.g., digital health assistants)
and build a working alliance (Kaveladze & Schueller,
2023). The latter is an important relationship quality
robustly linked to treatment outcomes (Del Re et al.,
2021). DTx that use conversational agents can reach
and engage individuals in a highly scalable manner
(Kowatsch et al., 2021). Barriers of implementing
CAs can be liability issues (Schlieter et al., 2022), for
example, patient safety was often overlooked in prior
work (Laranjo et al., 2018). Recent technological
advances in large language models for healthcare
promise safer and more accurate CAs in the future
(Singhal et al., 2022).
2.2.4 Design & Eval. Framework for DTx
As for the design of scalable and evidence-based
DTx, digital health companies, researchers, and/or
clinicians have the responsibility to validate and
evaluate the effectiveness of the DTx’ individual
building blocks (Kowatsch et al., 2019, Coravos et al.,
2019). Therefore, a design and evaluation framework
for DTx has been proposed (DEDHI) to support both
researchers and practitioners (Kowatsch et al., 2019).
DEDHI consists of four phases. Preparation,
optimization, evaluation, and implementation. It was
derived from the Multiphase Optimization Strategy
(Collins, 2018) and several other frameworks, e.g.,
Campbell et al. (2007). DEDHI specifies the goals
and tasks, technical maturity, evaluation criteria, and
implementation barriers for each phase.
2.3 Novel Business Models
Digital health companies that focus on prevention and
disease detection are underrepresented on the health
continuum with most businesses focused on disease
management (Cohen et al., 2020). And even though it
is “far better to prevent disease than to treat people
after they get sick” (Levine et al., 2019), only 3% of
total US healthcare expenditures are spent on
prevention (Pryor and Volpp, 2018). Against this
background and the health and economic burden of
NCDs and CMDs, there is a substantial need for
successful business models for prevention and aging
society (Coughlin, 2017). An exchange platform for
DTx may be a viable business model in this regard
(Wortmann et al., 2022). DTx for healthy longevity,
blended with various other online or online
preventive care services, can be offered and bought
by different types of consumers. For example, there
could be offerings like “Healthy Longevity Holidays”
with a blended DTx approach, were a target person
(or family) uses a DTx before and after the holidays
while getting personalized on-site coaching sessions
based on the data collected via the DTx during the
holiday period. In another, secondary prevention
example, national screening programs like Donna are
offered. Donna is a program for early detection of
breast cancer for women over 50. Women are
automatically scheduled for a mammography and
questionnaire every two years which significantly
reduces mortality (Warner, 2011). Finally,
Scale-IT-up 2023 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
618

Germany’s DIGA concept represents an example for
tertiary prevention with DTx (FIDMD, 2020).
Doctors can prescribe this class of DTx while health
insurance companies take over the reimbursement.
The DTx deprexis, for example, can be prescribed as
an adjunctive treatment for people with depression. It
has been shown that this DTx results in better
treatment outcomes than human-delivered
psychotherapy alone (Berger et al., 2018). Another
example is the DTx zanadio for individuals with
obesity (Forkmann et al., 2022). The estimated
revenue of DIGAs in Germany was around 55 million
EUR in 2022 (McKinsey & Company, 2022). A
search in the PitchBook database for privately held
venture capital-backed companies in “longevity”
shows a rising number of deals and total capital raised
from 14 (€62.83 M) in 2017 to 49 (€333.57 M) in
2022 indicating the potential of DTx for healthy
longevity.
3 EXAMPLES
With two specific initiatives in Switzerland and
Singapore, we would like to illustrate the potential of
DTx for healthy longevity according to the roadmap
outlined above.
3.1 Switzerland
First, Switzerland was recently ranked as the most
innovative country (WIPO, 2022). The key to
innovation is university-industry collaboration and
matching preconditions (Rajalo et al., 2017). The
Switzerland Innovation initiative was invented to
improve collaboration by opening innovation parks, a
cluster for specific industries, e.g., in Basel for life
sciences. In 2022, the Switzerland Innovation Park
OST (SIP-OST) was founded in the canton of
St.Gallen to focus on health, industrial engineering,
and digitalization. This focus area enables
opportunities for innovation in DTx. With respect to
this position paper, SIP-OST is currently developing
a strategy for a DTx ecosystem with a focus on
healthy longevity. The region has access to clinical
and non-clinical populations with the cantonal
hospital of St.Gallen, the children's hospital, the
geriatric clinic, the rehabilitation clinic in Gais, and
the Hirslanden Clinic. For the development of
minimally invasive biosensors, SIP-OST can foster
the expertise of the Swiss Federal Laboratories for
Material Science and Technology (EMPA). For
example, EMPA developed textile-based ECG
electrodes for long-term monitoring (Weder et. Al,
2015) which is now the spin-off Nahtlos. Also, this
region is one of Switzerland's biggest IT hubs, and
has the infrastructure to build and scale DTx for
healthy longevity. The Center for Laboratory
Medicine, Labor Dr. Riesch, Labor Team W, or
Microsynth are some examples of laboratories
focusing on biomedical analyses. Synergies with
established organizations and competence centers
(e.g., the cantonal hospital and the Centre for Digital
Health Interventions) and the recently founded HSG
School of Medicine and HSG Institute of Computer
Science allow the development of scalable DTx. The
HSG Chairs of Information, Technology, and
Innovation Management, Entrepreneurship, Digital
Health Interventions, International Business Law and
Health Care Management enable the development of
new business models to bring new DTx for healthy
longevity to the market. A healthy start-up culture is
built with initiatives like Startfeld, START Global, or
Startup@HSG. In addition to the dovetailing of
technological, medical, and health-economic
expertise in Eastern Switzerland, it has a
geographically unique location between Lake
Constance and the Alps. This is particularly relevant
for primary, secondary, and tertiary prevention of
NCDs and CMDs, as a walk or a hike in nature
promotes physical and mental health (Hansen et al.,
2017). The rural areas also enable the development of
DTx projects and services with a strong focus on
remote monitoring and virtual clinics. The digital
health company OnlineDoctor, for example, connects
patients and dermatologists. Eastern Switzerland,
therefore, harbors a promising ecosystem to develop
innovative DTx for healthy longevity.
3.2 Singapore
Singapore will likely be the fifth oldest country
worldwide by 2050 by median age (United Nations,
2015). The recent adaptation to their aging society
will probably be an example for other nations on how
to transform the healthcare system to meet the need
of the global demographic shift. Healthier SG is a
healthcare transformation program that addresses the
aging of its population (Healthier SG, 2022). All
relevant stakeholders were involved in the
development of Healthier SG. At the center of
Healthier SG lies the challenge of changing personal
health-seeking behavior (Knittle et al., 2020) and
greater emphasis on preventive care instead of
curative care. Healthier SG designed a five-step
process to reach the program’s goals. First, everyone
in Singapore will choose a family doctor, who can
educate them on improving their health and who will
Digital Therapeutics for Healthy Longevity: A Roadmap
619

build a relationship with them. Second, personal
health plans will be developed depending on lifestyle
and screening. Annual check-ins as primary
prevention will be implemented. Third, local partners
help people to stay on track with their health plans
and, at the same time, promote social well-being.
Fourth, a national family doctor health program will
be implemented for over 60-year-olds in 2023. And
finally, and most importantly, policies will
incentivize preventive care, IT systems will be
developed to ensure a seamless sharing of data, and
healthcare manpower will be equipped with the
corresponding skills. Additionally, DTx like H365
promote daily activity by rewarding health points
which can be exchanged for vouchers.
4 DISCUSSION AND FUTURE
WORK
It is of utmost importance to lower social inequalities
in health. DTx for healthy longevity offer scalable
means to reach and engage vulnerable individuals. To
ensure the effectiveness of such DTx, principal
investigators of clinical studies should, therefore,
especially target and consider individuals with a
lower socioeconomic status. This can be achieved,
among other approaches, with the help of community
partnerships (Bonevski et al., 2014). It is now time to
give forethought to strong incentive structures and
evaluation methods to promote high-quality and
equitable DTx for healthy longevity. Clinicians,
(business) organizations, public bodies, and
regulators have the joint responsibility to design an
ecosystem where innovative DTx for an aging society
can strive. To come to these solutions, one must first
conduct iterative, interdisciplinary, and user-centered
healthy longevity studies. Feasibility, optimization,
evaluation, and implementation studies must be
conducted from a technical, medical, behavioral, and
health economic perspective. The resources required
depend strongly on which application scenario lies in
focus (e.g., a healthy vs. patient population).
Depending on that focus, appropriate partnerships
and funding sources can be selected.
As a next step, we will work on a globally
scalable DTx design and trial service based on
MobileCoach.eu. The objective of this service is to
accelerate the design of evidence-based DTx for
healthy longevity and with it, to reduce the
inequalities in health.
5 CONFLICT OF INTEREST
TK is affiliated with the Centre for Digital Health
Interventions (CDHI), a joint initiative of the Institute
for Implementation Science in Health Care,
University of Zurich; the Department of
Management, Technology, and Economics at Swiss
Federal Institute of Technology in Zürich; and the
Institute of Technology Management and School of
Medicine at the University of St Gallen. CDHI is
funded in part by the Swiss health insurer CSS. CSS
was not involved in this research. TK is also a co-
founder of Pathmate Technologies, a university spin-
off company that creates and delivers digital clinical
pathways. However, Pathmate Technologies was not
involved in this research.
REFERENCES
Banholzer, N., Feuerriegel, S., Fleisch, E., Bauer, G. F., &
Kowatsch, T. (2021). Computer mouse movements as
an indicator of work stress: longitudinal observational
field study. Journal of medical Internet
research, 23(4), e27121.
Beard, J. R., Officer, A., De Carvalho, I. A., Sadana, R.,
Pot, A. M., Michel, J. P., Lloyd-Sherlock, P., Epping-
Jordan, J. E., Peeters, G., Mahanani, W. R.,
Thiyyagarajan, J. A., & Chatterji, S. (2016). The World
report on ageing and health: a policy framework for
healthy ageing. The lancet, 387(10033), 2145-2154.
Berger, T., Krieger, T., Sude, K., Meyer, B., & Maercker,
A. (2018). Evaluating an e-mental health program
(“deprexis”) as adjunctive treatment tool in
psychotherapy for depression: Results of a pragmatic
randomized controlled trial. Journal of affective
disorders, 227, 455-462.
Bickmore, T., & O'Leary, T. (2023). Conversational agents
on smartphones and the web. In Digital Therapeutics
for Mental Health and Addiction (pp. 99-112).
Academic Press.
Bonevski, B., Randell, M., Paul, C., Chapman, K.,
Twyman, L., Bryant, J., Brozek, I., & Hughes, C.
(2014). Reaching the hard-to-reach: a systematic
review of strategies for improving health and medical
research with socially disadvantaged groups. BMC
medical research methodology, 14(1), 1-29.
Campbell, N. C., Murray, E., Darbyshire, J., Emery, J.,
Farmer, A., Griffiths, F., Guthrie, B, Lester, H., Wilson,
P. & Kinmonth, A. L. (2007). Designing and evaluating
complex interventions to improve health
care. Bmj, 334(7591), 455-459.
Carrilero, N., García‐Altés, A., Mendicuti, V. M., & Ruiz
García, B. (2021). Do governments care about
socioeconomic inequalities in health? Narrative review
of reports of EU‐15 countries. European Policy
Analysis, 7(2), 521-536.
Scale-IT-up 2023 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
620

Chen, S., Kuhn, M., Prettner, K., & Bloom, D. E. (2018).
The macroeconomic burden of noncommunicable
diseases in the United States: Estimates and
projections. PloS one, 13(11), e0206702.
Choi, W., Park, S., Kim, D., Lim, Y. K., & Lee, U. (2019).
Multi-stage receptivity model for mobile just-in-time
health intervention. Proceedings of the ACM on
interactive, mobile, wearable and ubiquitous
technologies, 3(2), 1-26.
Cohen, A. B., Dorsey, E., Mathews, S. C., Bates, D. W., &
Safavi, K. (2020). A digital health industry cohort
across the health continuum. NPJ digital
medicine, 3(1), 1-10.
Collins, L. (2018). Optimization of behavioral,
biobehavioral, and biomedical interventions. Cham:
Springer International Publishing, 10(1007), 978-973.
Coravos, A., Khozin, S., & Mandl, K. D. (2019).
Developing and adopting safe and effective digital
biomarkers to improve patient outcomes. NPJ digital
medicine, 2(1), 1-5.
Coughlin, J. F. (2017). The longevity economy: Unlocking
the world's fastest-growing, most misunderstood
market. Hachette UK.
Davis, T. C., Arnold, C. L., Mills, G., & Miele, L. (2019).
A qualitative study exploring barriers and facilitators of
enrolling underrepresented populations in clinical trials
and biobanking. Frontiers in Cell and Developmental
Biology, 7, 74.
Del Re, A. C., Flückiger, C., Horvath, A. O., & Wampold,
B. E. (2021). Examining therapist effects in the
alliance–outcome relationship: A multilevel meta-
analysis. Journal of Consulting and Clinical
Psychology, 89(5), 371.
Digital Therapeutics Alliance. (2019). Digital Therapeutics
Definition and Core Principles. Digital Therapeutics
Alliance Fact Sheet.
Federal Office of Public Health. (2016). National Strategy
for the Prevention of Non-communicable Diseases
(NCD strategy). Federal Office of Public Health.
FIDMD. (2020). The Fast-Track Process for Digital Health
Applications (DiGA) according to Section 139e SGB V:
A Guide for Manufacturers, Service Providers and
Users. F. I. f. D. a. M. Devices.
Forkmann, K., Roth, L., & Mehl, N. (2022). Introducing
zanadio—A Digitalized, Multimodal Program to Treat
Obesity. Nutrients, 14(15), 3172.
Hansen, M. M., Jones, R., & Tocchini, K. (2017). Shinrin-
yoku (forest bathing) and nature therapy: A state-of-
the-art review. International journal of environmental
research and public health, 14(8), 851.
Healthier SG. (2022). White Paper on Healthier SG.
Forward SG.
Jacobson, N. C., Kowatsch, T., & Marsch, L. A. (Eds.).
(2023). Digital Therapeutics for Mental Health and
Addiction: The State of the Science and Vision for the
Future. Academic Press.
Kaveladze, B., & Schueller, S. M. (2023). A digital
therapeutic alliance in digital mental health. In Digital
Therapeutics for Mental Health and Addiction (pp. 87-
98). Academic Press.
Keller, R., v. Wangenheim, F., Mair, J. & Kowatsch, T.
(2023). Chapter 6 – Receptivity to mobile health
interventions. Academic Press.
Knittle, K., Heino, M., Marques, M. M., Stenius, M.,
Beattie, M., Ehbrecht, F., Hagger, S., Hardeman, W. &
Hankonen, N. (2020). The compendium of self-
enactable techniques to change and self-manage
motivation and behaviour v. 1.0. Nature Human
Behaviour, 4(2), 215-223.
Kowatsch T. (2023). How to Lower Socioeconomic
Inequalities in Health with Digital Therapeutics?
Healthification – A Short Animation. Workshop on Best
Practices for Scaling-Up Digital Innovations in
Healthcare - Scale-IT-up 2023, co-located with the
16th International Joint Conference on Biomedical
Engineering Systems and Technologies, 16-18
February 2023, Lisbon, Portugal.
Kowatsch, T., & Fleisch, E. (2021). Digital Health
Interventions. In Connected Business (pp. 71-95).
Springer, Cham.
Kowatsch, T., Otto, L., Harperink, S., Cotti, A., & Schlieter,
H. (2019). A design and evaluation framework
for digital health interventions. IT-Information
Technology, 61(5-6), 253-263.
Kowatsch, T., Schachner, T., Harperink, S., Barata, F.,
Dittler, U., Xiao, G., Stanger, C., v Wangenheim, F.,
Fleisch, E., Oswald, H. & Möller, A. (2021).
Conversational agents as mediating social actors in
chronic disease management involving health care
professionals, patients, and family members: multisite
single-arm feasibility study. Journal of medical
Internet research, 23(2), e25060.
Künzler, F., Kramer, J. N., & Kowatsch, T. (2017). Efficacy
of mobile context-aware notification management
systems: A systematic literature review and meta-
analysis. In 2017 IEEE 13th International Conference
on Wireless and Mobile Computing, Networking and
Communications (WiMob)(pp. 131-138). IEEE.
Künzler, F., Mishra, V., Kramer, J. N., Kotz, D., Fleisch,
E., & Kowatsch, T. (2019). Exploring the state-of-
receptivity for mhealth interventions. Proceedings of
the ACM on Interactive, Mobile, Wearable and
Ubiquitous Technologies, 3(4), 1-27.
Laranjo, L., Dunn, A. G., Tong, H. L., Kocaballi, A. B.,
Chen, J., Bashir, R., Surian, D., Gallego, B., Magrabi,
F., Lau, A. Y. S. & Coiera, E. (2018). Conversational
agents in healthcare: a systematic review. Journal of the
American Medical Informatics Association, 25(9),
1248-1258.
Levine, S., Malone, E., Lekiachvili, A., & Briss, P. (2019).
Health care industry insights: why the use of preventive
services is still low. Preventing chronic disease, 16.
Liao, P., Greenewald, K., Klasnja, P., & Murphy, S. (2020).
Personalized heartsteps: A reinforcement learning
algorithm for optimizing physical activity. Proceedings
of the ACM on Interactive, Mobile, Wearable and
Ubiquitous Technologies, 4(1), 1-22.
Mackenbach, J. P., Stirbu, I., Roskam, A. J. R., Schaap, M.
M., Menvielle, G., Leinsalu, M., & Kunst, A. E. (2008).
Socioeconomic inequalities in health in 22 European
Digital Therapeutics for Healthy Longevity: A Roadmap
621

countries. New England journal of medicine, 358(23),
2468-2481.
McKinsey & Company. (2022). E-Health Monitor 2022
Deutschlands Weg in die digitale
Gesundheitsversorgung – Status quo und Perspektiven.
Medizinische Wissenschaftliche Verlagsgesellschaft.
Mishra, V., Künzler, F., Kramer, J. N., Fleisch, E.,
Kowatsch, T., & Kotz, D. (2021). Detecting receptivity
for mHealth interventions in the natural environment.
Proceedings of the ACM on interactive, mobile,
wearable and ubiquitous technologies, 5(2), 1-24.
Murphy, A., Palafox, B., Walli-Attaei, M., Powell-Jackson,
T., Rangarajan, S., Alhabib, K. F., Avezum, A., Calik,
K. B. T., Chifamba, J., Choudhury, T., Dagenais, G., L
Dans, A. , Gupta, R., Iqbal, R., Kaur, M., Kelishadi, R.,
Khatib, R., Kruger, I. M., Kutty, V. R., … & McKee,
M. (2020). The household economic burden of non-
communicable diseases in 18 countries. BMJ global
health, 5(2), e002040.
Nahum-Shani, I., Hekler, E. B., & Spruijt-Metz, D. (2015).
Building health behavior models to guide the
development of just-in-time adaptive interventions: A
pragmatic framework. Health psychology, 34(S), 1209.
Nahum-Shani, I., Wetter, D. W., & Murphy, S. A. (2023).
Adapting just-in-time interventions to vulnerability
and receptivity: Conceptual and methodological
considerations. In Digital Therapeutics for Mental
Health and Addiction (pp. 77-87). Academic Press.
Pryor, K., & Volpp, K. (2018). Deployment of preventive
interventions—time for a paradigm shift. N Engl J
Med, 378(19), 1761-1763.
Rajalo, S., & Vadi, M. (2017). University-industry
innovation collaboration: Reconceptualization.
Technovation, 62, 42-54.
Roth, G. A., Abate, D., Abate, K. H., Abay, S. M., Abbafati,
C., Abbasi, N., Abbastabar, H., Abd-Allah, F., Abdela,
J., Abdelalim, A., Abdollahpour, I., Abdulkader, R. S.,
Abebe, H. T., Abebe, M., Abebe, Z., Abejie, A. N.,
Abera, S. F., Abil, O. Z., Abraha, H. N., … &
Borschmann, R. (2018). Global, regional, and national
age-sex-specific mortality for 282 causes of death in
195 countries and territories, 1980–2017: a systematic
analysis for the Global Burden of Disease Study
2017. The Lancet, 392(10159), 1736-1788.
Schlieter, H., Marsch, L. A., Whitehouse, D., Otto, L.,
Londral, A. R., Teepe, G. W., ... & Kowatsch, T.
(2022). Scale-up of Digital Innovations in Health Care:
Expert Commentary on Enablers and Barriers. Journal
of Medical Internet Research, 24(3), e24582.
Sharrocks, K., Spicer, J., Camidge, D. R., & Papa, S.
(2014). The impact of socioeconomic status on access
to cancer clinical trials. British journal of
cancer, 111(9), 1684-1687.
Sim, I. (2019). Mobile devices and health. New England
Journal of Medicine, 381(10), 956-968.
Singhal, K., Azizi, S., Tu, T., Mahdavi, S. S., Wei, J.,
Chung, H. W., Scales, N., Tanwani, A., Cole-Lewis, H.,
Pfohl, S., Payne, P., Seneviratne, M., Gamble, P., Kelly,
C., Scharli, N., Chowdhery, A., Mansfield, A., Aguera
y Arcas, B. & Natarajan, V. (2022). Large Language
Models Encode Clinical Knowledge. arXiv preprint
arXiv:2212.13138.
Tinschert, P., Rassouli, F., Barata, F., Steurer-Stey, C.,
Fleisch, E., Puhan, M. A., Kowatsch T. & Brutsche, M.
H. (2020). Nocturnal cough and sleep quality to assess
asthma control and predict attacks. Journal of asthma
and allergy, 13, 669.
United Nations. (2015). Word population ageing Economic
& Social Affairs.
Vandenberghe, D., & Albrecht, J. (2020). The financial
burden of non-communicable diseases in the European
Union: a systematic review. European Journal of
Public Health, 30(4), 833-839.
Warner, E. (2011). Breast-cancer screening. New England
Journal of Medicine, 365(11), 1025-1032.
Weder, M., Hegemann, D., Amberg, M., Hess, M., Boesel,
L. F., Abächerli, R., Meyer, V. R. & Rossi, R. M.
(2015). Embroidered electrode with silver/titanium
coating for long-term ECG monitoring. Sensors, 15(1),
1750-1759.
WHO. (2006). Constitution of the World Health
Organization, Basic Documents. Forty.
WHO. (2014). Global status report on noncommunicable
diseases 2014. Word Health Organization.
WHO. (2015). World report on ageing and health. World
Health Organization.
Wieser, S. (2014). Die Kosten der nichtübertragbaren
Krankheiten in der Schweiz: Schlussbericht. Federal
Office of Public Health.
WIPO. (2022). Global Innovation Index 2022 World
Intellectual Property Organization. Geneva, 15
th
edition.
Wortmann, F., Jung, S., Bronner, W., & Gassmann, O.
(2022). The Platform Navigator: 88 Patterns to Design
and Implement Platform Business Models.
Yang, Y., Yuan, Y., Zhang, G., Wang, H., Chen, Y. C., Liu,
Y., Tarolli, G., Crepeau, D., Bukaryk, J., Junna, M. R.,
Videnovic, A., Ellis, T. D., Lipford, M. C., Dorsey, R.
& Katabi, D. (2022). Artificial intelligence-enabled
detection and assessment of Parkinson’s disease using
nocturnal breathing signals. Nature medicine, 28(10),
2207-2215.
Scale-IT-up 2023 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
622
