
Designing a Digital Personal Coach to Promote a Healthy Diet and
Physical Activity Among Patients After Cardiothoracic Surgery
Ana Martins
1,3 a
, Isabel Nunes
3 b
, Lu
´
ıs Velez Lap
˜
ao
2,3 c
and Ana Londral
1,2 d
1
Value for Health CoLAB, Lisboa, Portugal
2
Comprehensive Health Research Center, Nova Medical School, Nova University of Lisbon, Lisboa, Portugal
3
Department of Mechanical and Industrial Engineering, NOVA School of Science and Technology, Nova University of
Lisbon, Lisboa, Portugal
Keywords:
Digital Coach, Text-Message Intervention, Conversational Agents, Behavior Change Theory, Cardiothoracic
Surgery.
Abstract:
This position paper describes the design of a text-message intervention that uses behavior change theory to
help design the intervention to improve patients’ diet and physical activity. The text-message intervention aims
to guide patients to improve their self-efficacy in managing their disease to reduce complications and hospital
readmissions and improve health-related outcomes, well-being, and quality of life. Design Science Research
methodology is used to support problem definition, design, development, and evaluation of a sustainable,
useful, and valuable artifact.
1 INTRODUCTION
A healthy lifestyle can reduce the burden associated
with chronic diseases by preventing their appearance,
and promoting health maintenance. Protective behav-
iors should be taught to chronic patients to improve
their quality of life and long-term well-being. This
can reduce the workload of healthcare professionals
by making patients active agents in their health (Bauer
et al., 2014; Kontis et al., 2014). Behavior change in-
terventions can guide the process of change and help
maintain a healthy behavior (Grimmett et al., 2019).
The use of conversational agents can be an afford-
able and efficient way to personalize care by deliv-
ering personalized content based on what is reported
and needed by the patient (Chaix et al., 2019; Fitz-
patrick et al., 2017; Stephens et al., 2019; Ghandehar-
ioun et al., 2019).
Cardiovascular disease (CVD) is the biggest cause
of mortality and morbidity worldwide (WHO, 2021).
A prospective cohort study found that cardiovascular
disease events are caused by modifiable risk factors.
The predominant factors were hypertension, high
a
https://orcid.org/0000-0002-4890-3941
b
https://orcid.org/0000-0002-0428-0930
c
https://orcid.org/0000-0003-0506-1294
d
https://orcid.org/0000-0002-8002-6790
low-density lipoprotein (LDL) cholesterol, household
pollution, and tobacco use (Yusuf et al., 2020).
Cardiothoracic surgery has decreased mortality
and morbidity of cardiovascular patients, allowing pa-
tient’s to live longer. However, because surgery is
a stressful event (Gardner et al., 2005; Pinto et al.,
2016; Tadas et al., 2021), it may result in a failure
to fully understand the medical information provided
and compromise health outcomes. These facts have
led researchers to focus on ways to increase patients’
awareness of their disease to improve their well-being
and quality of life and prevent further events from oc-
curring (Tully, 2013). Pervasive technology might be
used to improve modifying risk factors and quality of
life.
Behavior change interventions (BCIs) systemati-
cally organize actions that target specific behaviors
with the intent to improve a target behavior in a tar-
get population (Michie et al., 2011). Interventions
to change behavior are complex due to the interact-
ing components they are composed of. In the design
phase, specifications must be understandable to en-
sure proper evaluation of effectiveness.
The Behavior Change Wheel (BCW) summarizes
19 behavior change frameworks and was developed
using expert consensus and validation (Michie et al.,
2011) to guide researchers in the design and evalua-
tion phases. The framework divides intervention de-
Martins, A., Nunes, I., Lapão, L. and Londral, A.
Designing a Digital Personal Coach to Promote a Healthy Diet and Physical Activity Among Patients After Cardiothoracic Surgery.
DOI: 10.5220/0011776800003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 5: HEALTHINF, pages 595-602
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
595

sign into three phases: (1) understanding the behav-
ior, (2) identifying intervention options, and (3) iden-
tifying content and implementation options. In the
first phase, the definition of the problem in behav-
ioral terms is specified, the target behavior is selected
and specified, and a needs assessment is performed.
The behavioral analysis is performed using the model
of capacity, opportunity, and motivation (COM-B).
Capability stands for the psychological and physical
ability to perform a certain activity. Opportunity is
characterized as the external factors that could trig-
ger/enable a particular behavior, and motivation is the
conscious and unconscious cognitive processes that
lead the agent to perform a particular behavior in-
tuitively or rationally. Phase 2 establishes the in-
tervention functions and policy categories are iden-
tified. Education, persuasion, incentivization, coer-
cion, training, restriction, environmental structuring,
modeling, and enablement are intervention functions
that can be used to achieve a specific target behavior
(Michie et al., 2011). In the last phase, the content
and implementation options are clarified. Behavior
change techniques (BCTs) should be defined in this
phase.
BCTs are observable, replicable, and irreducible
components that aim to redirect causal processes that
regulate target behavior. They can give us cues about
how the content delivered by the conversational agent
influences the receiver (Michie et al., 2013). Mecha-
nisms of action (MoAs) give us a better understand-
ing of how BCTs act on individuals to produce the
expected effects. Based on the studies published to
date, the Human Behavior Change Project has devel-
oped a tool that maps BCTs to MoAs. This allows the
MoA underlying the change to be identified (Carey
et al., 2018; Johnston et al., 2021).
In this position paper, we describe the methodol-
ogy we used to develop a pilot study aimed at inte-
grating behavior change theory into a digital solution
to promote healthy eating and regular physical activ-
ity. Future work is also explained.
2 METHODS
Design Science Research Methodology (DSRM) is
used to ensure that a successful artifact created to ad-
dress a problem that meets the interests of all stake-
holders is produced (Hevner et al., 2004). A suc-
cessful DSRM cycle draws on previous literature and
lends itself as a solution to a specific problem whose
utility, quality, and effectiveness will be rigorously
evaluated (Hevner et al., 2004). The development
of the artifact should uphold on existing theories and
knowledge to a specific problem (Peffers et al., 2007).
We followed a nominal process based on previous re-
search involving 6 steps (Peffers et al., 2007) as de-
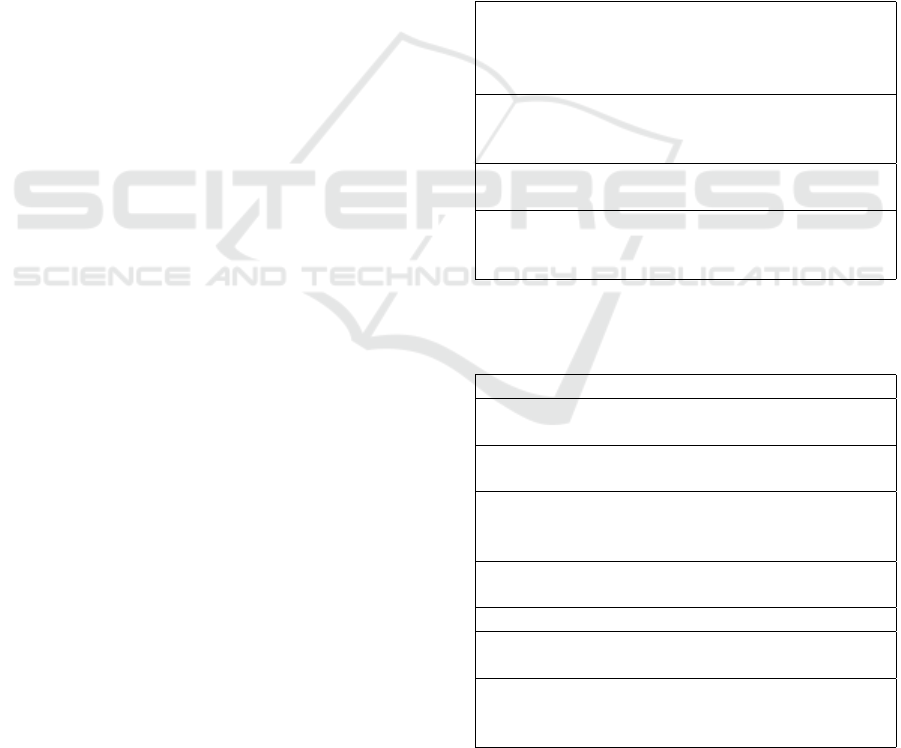
picted in Figure 1.
2.1 Problem Identification, Context
Characterization, and Motivation
Consistent with the DSRM, problem identification
and motivation definition are critical to the sustain-
ability of the artifact. This step was divided into 4
activities, namely context characterization, data anal-
ysis, literature review, and semi-structured interview
with clinical team.
We obtained an initial description of the context
in which the artifact would be used during a meet-
ing with the researchers involved in an earlier research
project to develop a telemonitoring service to monitor
patients undergoing cardiothoracic surgery (Londral
et al., 2022). An additional meeting with the clini-
cal team helped understanding how the follow-up af-
ter the telemonitorization period was done and what
were the major concerns of the clinical team after the
telemonitorization period.
Following the context characterization, data anal-
ysis of electronic health records (EHR) was con-
ducted to better understand the demographic charac-
teristics of the study population, such as age, gen-
der, income, education, occupation, and additional
medical information on pre-existing conditions to
surgery and type of procedure. In addition, patient-
reported outcomes (PROMs) collected by nurses dur-
ing follow-up interviews were also analyzed.
At this point qualitative studies regarding experi-
ences after surgery (Gardner et al., 2005; Pinto et al.,
2016; Tadas et al., 2021) where studied to understand
what are patient’s experiences after surgery. Addi-
tionally, risk modifying factors of cardiovascular dis-
ease were assessed (Yusuf et al., 2020).
After data analysis and discussion of findings with
the research team, semi-structured interviews were
conducted with 7 healthcare providers to understand
(1) what are risk modifying factors for the population
considered important to the clinical team, (2) what is
important for patients to have a better quality of life,
(3) what are the barriers and facilitators to activities
relevant to increasing patient well-being, (4) whether
there are personality traits in this population that with
better health outcomes, (5) how the follow-up service
works, (6) how information is communicated to pa-
tients (literacy strategies used), and (7) how this ser-
vice can be improved. Interviews were performed us-
ing LimeSurvey (Schmitz, 2012).
Scale-IT-up 2023 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
596

Figure 1: Methodology for developing a valuable artifact for follow-up in the cardiothoracic surgery service.
2.2 Define the Objectives for a Solution
The specification of the target behaviors for the in-
tervention focused on understanding which behaviors
can have a broader impact in the modifying risk fac-
tors for cardiovascular disease.
Ten patients who had participated in the telemon-
itoring pilot project mentioned earlier (Londral et al.,
2022) were interviewed a year and a half after surgery
to collect their experiences during the recovery pe-
riod. The semi-structured interview consisted of 8
questions, according to the recommendations of the
clinical team, who advised us to ask only a few ques-
tions, otherwise, the patient would lose interest. In
this interview, the COM -B model is used to identify
barriers and facilitators to healthy eating and physi-
cal activity. So the questions focused on finding out
how the surgery changed their lives, what their quality
of life is like today, what motivates them to maintain
healthy habits and follow the clinical team’s recom-
mendations, whether they adhere to diet and physical
activity recommendations. We also asked patients if
they could recommend changes to the service. In this
way, we were able to conduct a behavioral analysis
of the patients who participated in the telemonitoring
project in accordance with the phase 1 of the BCW
framework. The main barriers and motivators for ini-
tiating and maintaining a particular behavior were as-
signed to the intervention function layer of the BCW.
The objectives were set after 2 meetings with the
researchers involved in the study (engineers, medical
doctors, and nurses) where all the information gath-
ered and a possible objective for a solution were pre-
sented. We foresee the need to redefine the objective
after each iteration of the study.
A systematic literature review was conducted to
determine how to develop conversational agents that
deliver personalized and automated content to pa-
tients with chronic diseases.
2.3 Design and Development
In designing and developing the solution, we focused
on integrating the results of the previously defined
target behavior with the intervention functions previ-
ously identified by the clinical team and the results of
the systematic literature review.
2.4 Demonstration
The first iteration of the DSRM will be completed
with a pilot study of 5 patients who agree to partic-
ipate.
2.5 Evaluation
The evaluation process was defined based on the tar-
get behavior previously established in the goal defini-
tion phase. Our goal was to define methods currently
used in the service to assess patient recovery in or-
der to increase the feasibility of the artifact. We also
wanted to measure engagement, acceptance, and sat-
isfaction.
3 RESULTS
3.1 Problem Identification and
Motivation
The cardiothoracic surgery service follows patients
for one year after surgery. During this time, nurses
conduct follow-up visits to assess patients’ recovery
based on physical activity, pain, diet, body mass in-
dex, medications, health monitoring, social support,
tobacco use, and quality of life. Regular appointments
are also scheduled with the patient’s assigned medical
doctor. In addition, patients who are willing to partic-
ipate in the telemonitoring study, if selected for the
intervention group, can benefit from the telemonitor-
ing service three months after surgery, as shown in
Figure 2.
EHRs provided by the hospital showed that only
1% of patients had no preexisting condition before
surgery. Pre-existing conditions or risk factors were
arterial hypertension (17.7%), hypercholesterolemia
(14.6%), diabetes (6.9%), persistent atrial fibrillation
(3.8%), previous myocardial infarction (3.2%), smok-
ing (3.1%), and more. According to the clinical team,
Designing a Digital Personal Coach to Promote a Healthy Diet and Physical Activity Among Patients After Cardiothoracic Surgery
597

most patients are treated as having a chronic dis-
ease after surgery and there is a high risk of read-
mission 1 year after surgery. Therefore, the service
provides specialist appointments, uses various tech-
niques to improve patients’ literacy, conducts tele-
monitoring, does regular follow-up interviews, and
distributes brochures on nutrition and physical activ-
ity to help patients properly manage their condition.
The semi-structured interviews with the clinical
team revealed that risk factors are important to im-
prove health-related outcomes. Managing chronic
conditions such as diabetes, hypertension, LDL, a
healthy diet, regular physical activity, good mental
health, and a social role are factors that positively
influence recovery. Barriers to implementing protec-
tive behaviors include poor health literacy skills, lack
of motivation, lack of support and specialized help,
employment, anxiety, fear, pain, and physical capa-
bility. The clinical team was unable to identify any
unique personality traits in this population. The clin-
ical team suggested developing an automated system
that would not increase the workload of the clinical
team, predict what the patient’s needs would be at
home after the telemonitoring period, and send per-
sonalized messages to encourage healthy behaviors.
Doctors also say that it is very common for pa-
tients to come back to the hospital after 1 year of
surgery due to complications. This might be cause
by lack of self-management skills and distress at that
moment.
For what was said, we hypothesized that a prob-
lem could be associated with the lack self-efficacy in
self-managing the disease. Thus, the use of pervasive
technology could be important to provide support,
and valuable information for managing their disease
(Halldorsdottir et al., 2020; Akinosun et al., 2021).
3.2 Define the Objectives for a Solution
The target behaviors for the intervention were identi-
fied by first analyzing all the modifying risk factors
to the target population, which can be split into three
types of factors: (1) behavioral factors (ie, tobacco
use, alcohol, diet, physical activity, and sodium in-
take), (2) metabolic factors (ie, lipids, blood pressure,
diabetes, obesity), (3) socioeconomic and psychoso-
cial factors (ie, education, symptoms of depression),
(3) grip strength, and household and ambient pollu-
tion (Yusuf et al., 2020). We chose diet and physical
activity as target behaviors for the intervention since
they have a great impact in other factors, such as to-
bacco use, sodium intake, lipids, blood pressure, dia-
betes, obesity, and symptoms of depression (Warbur-
ton and Bredin, 2017; Cena and Calder, 2020).
The semi-structured interviews with patients re-
vealed that personalized advice on physical activity
and healthy eating could increase their well-being and
help them recover. The main barriers to engaging
in these behaviors were occupation, lack of motiva-
tion and physical capability, health status, medication,
weight, weather, and mental health. The main pro-
moters were social support, health beliefs, identifica-
tion with the behavior, pets, and the presence of mon-
itoring devices to track activity. We focused in the
results of the semi-structured interviews and results
from two studies to identify the determinants of hav-
ing a healthy diet and being physically active (Brug,
2008; Sherwood and Jeffery, 2000). We found that the
most important determinants for physical activity are
self-efficacy, health-related outcomes, social interac-
tion, stage of change, and social support. While, for
having a healthy diet, the most important were moni-
toring, personal satisfaction, social comparison, stage
of change, and social support.
The systematic literature review showed that to
carry out a fully-automated BCI it is necessary to set
up a data management platform and a communica-
tion system, incorporate algorithms that can automate
content delivery, specify the intended personalization
features, and find proper instruments to evaluate the
intervention. Previous studies carried out BCI to im-
prove physical activity, diet, enhance disease moni-
toring, and self-management (Mayberry et al., 2021;
Kelly et al., 2020; Polgreen et al., 2018; Cadilhac
et al., 2020; Chokshi et al., 2018; Horner et al., 2017;
Thiengwittayaporn et al., 2021). Three of those de-
veloped their own data management platforms (Pol-
green et al., 2018; Thiengwittayaporn et al., 2021;
Cadilhac et al., 2020), while the remaining used com-
mercially available platforms (Mayberry et al., 2021;
Kelly et al., 2020; Horner et al., 2017; Chokshi et al.,
2018). Every study used rule-based models to au-
tomate content delivery. Personalization features in-
cluded patient-centered goals (Mayberry et al., 2021;
Kelly et al., 2020; Cadilhac et al., 2020), barriers to
behavior change (Kelly et al., 2020), timing (May-
berry et al., 2021; Kelly et al., 2020; Cadilhac et al.,
2020) and frequency (Kelly et al., 2020) of message
delivery, functional ability (Cadilhac et al., 2020),
disease stage (Thiengwittayaporn et al., 2021), com-
munication channel (Mayberry et al., 2021; Chokshi
et al., 2018; Cadilhac et al., 2020), feedback based
on activity (Polgreen et al., 2018; Chokshi et al.,
2018; Horner et al., 2017), baseline demographic data
(Horner et al., 2017), and stage of behavior change
(Horner et al., 2017). Nevertheless, personalization
algorithms are not well documented and could be en-
hanced using other approaches that automatically un-
Scale-IT-up 2023 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
598
derstand what are the patient’s needs and adjust con-
tent.
Based on the above, we have the following objec-
tives for the solution:
• The end users are healthcare providers and pa-
tients after telemonitoring or surgery who want to
receive messages to improve their ability to self-
manage their condition.
• There should be no additional burden on health-
care providers.
• A ”virtual coach” CA sends text messages to
improve self-efficacy and help patients maintain
healthy behaviors (diet and physical activity).
• Intervention functions will include education, per-
suasion, training, and enablement.
• The language used should be encouraging, posi-
tive, friendly, polite, and lighthearted.
• Messages should be written using behavior
change techniques to allow for replicability.
• Content, communication channel, and dose
should be personalized.
• The follow-up questionnaire already used by the
clinical team should be used to measure the effec-
tiveness of the artifact.
• Improve self-management skills and prepare pa-
tients for the time when they are not supported by
the team (1 year after surgery).
• A platform should be developed that allows
healthcare professionals to select messages sug-
gested by an automation algorithm.
• This platform should be modular and reusable for
evidence-based behavior change interventions.
3.3 Design and Development
The patient journey in cardiothoracic surgery after the
integration of this artifact is shown in Figure 2. Typ-
ically, patients are admitted to the hospital one day
before surgery (preoperative). There, they receive
instructions to facilitate their postoperative recovery.
After surgery, the patient stays in the hospital for 5-7
days, depending on how the surgical procedure went
(hospitalization). After discharge from the hospital,
study participants are selected by a risk assessment
model to use a remote patient monitoring kit (home
telemonitoring). After 3 months of telemonitoring,
patients are asked if they would like to receive text
messages to help them engage in healthy behaviors
(text message intervention).
The text messages were developed using a text
message bank that has already been used with patients
with diabetes and developed with BCTs (MacPherson
et al., 2021). Therefore, we used these messages as
a reference to create a text message bank. The text
message bank was translated into Portuguese, adapted
to the population of the study, and validated by the
nurses to ensure the reliability of the content. This
database may grow as we determine the need for
more messages, which should happen iteratively as
the study progresses.
A platform is being developed to automate the
conversational agent to be used during the pilot study.
During the pilot study, we will use a fixed-frame
dialog to send content to the patient. An example of
the weekly dialog flow can be found in Table 1.
Table 1: Example of a weekly dialog flow.
(Monday) Getting rid of old habits is difficult,
start with simple things: try to eat fruit when you
feel like something sweet or drink water instead of
juice.
(Tuesday) The small steps can lead to big changes
in your health. Every step you take this week is a
step towards a healthier you.
(Wednesday) Think where, when and how you
will exercise today!
(Thursday) Try swapping refined carbohydrates
(eg white bread) for whole grain equivalents (eg
whole wheat bread).
Table 2: Example of a weekly status questionnaire [MoA -
mechanisms of action] UX - user experience).
.
[MoA/UX] Message (expected answer)
[Knowledge] A balanced diet means eating all
foods in the same amount. (T/F)
[Attitudes towards behavior] I don’t like the taste
of healthy food. (T/F)
[Attitudes towards behavior] I would have more
energy for my family and friends if I exercised
regularly. (T/F)
[Beliefs about consequences] Personally, I exer-
cise to improve my health. (T/F)
[Intention] I intend to eat more fruit. (T/F)
[UX] Do you consider the information sent to you
this week to be relevant?
[UX] Would you like to maintain the frequency
with which we send you messages? If not, indi-
cate the number of times per week.
Designing a Digital Personal Coach to Promote a Healthy Diet and Physical Activity Among Patients After Cardiothoracic Surgery
599
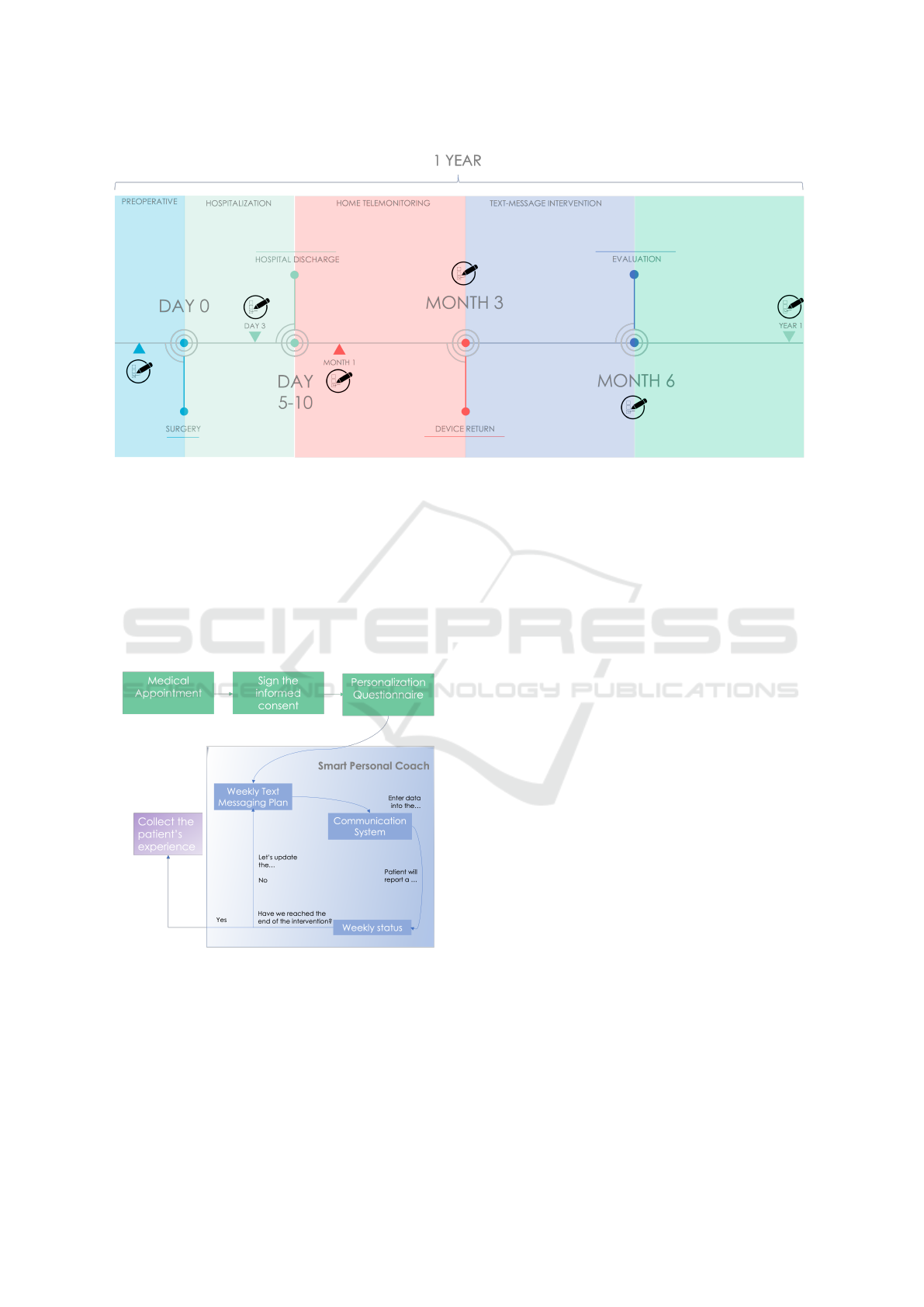
Figure 2: The patient journey at Santa Marta’s hospital will comprise 5 stages: (a) preoperative, (b) hospitalization, (c) home
telemonitoring, (d) text-message intervention, (e) regular follow-up.
3.4 Demonstration
The demonstration of the solution will be firstly be
done with a small pilot study with 5 patients and dur-
ing a month. The main goal is to understand the
usability, the engagement, and the satisfaction with
the intervention. The text-intervention diagram is de-
picted in Figure 3.
Figure 3: Text-intervention diagram.
3.5 Evaluation
Questionnaires will be used to improve patient expe-
rience (dose, timing, and relevance will be assessed
weekly). An example of a weekly questionnaire is
shown in Table 2. Patient progress will be evaluated
using data from the follow-up questionnaire already
used by the clinical team to assess the patient’s recov-
ery.
4 DISCUSSION AND
CONCLUSION
This paper focuses on explaining the methodology
that led to the development of a text messaging inter-
vention. DSRM was used to ensure the sustainability
and usability of solutions developed to address real-
world problems, such as the one we identified: lack
of self-efficacy in managing a cardiovascular disease
after cardiothoracic surgery. To do this, it is essential
to engage with all stakeholders involved. Behavior
change theory is used to guide the design of the inter-
vention by guiding a behavior analysis, and help de-
fine the target behavior, developing message content,
and personalize the intervention.
The goal of this work is to help patients improve
their quality of life and well-being and take control of
their disease after the follow-up period in the hospital.
The platform to be developed will be designed to be
reusable for future interventions and ensure usability
by paying attention to the user experience. This text
messaging intervention has not yet been evaluated and
no preliminary results are available.
Currently, we are focusing on developing algo-
rithms to personalize content selection. Unsupervised
algorithms will be used to understand patient needs
using data from previous patients. The next step will
be to develop a modular platform that will allow the
clinical team to monitor the diet and physical activity
Scale-IT-up 2023 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
600

of patients enrolled in the study and send text mes-
sages to patients who are not enrolled in the study.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the cardio-
thoracic service of the Santa Marta Hospital for their
contributions to carry out the study. This research has
been supported by the project DSAIPA/AI/0094/2020
from the Fundac¸
˜
ao para a Ci
ˆ
encia e Tecnologia AI 4
COVID-19 Program.
REFERENCES
Akinosun, A. S., Polson, R., Diaz Skeete, Y., De Kock,
J. H., Carragher, L., Leslie, S., Grindle, M., and
Gorely, T. (2021). Digital technology interventions
for risk factor modification in patients with cardiovas-
cular disease: Systematic review and meta-analysis.
JMIR mHealth and uHealth, 9(3):e21061.
Bauer, U. E., Briss, P. A., Goodman, R. A., and Bowman,
B. A. (2014). Prevention of chronic disease in the 21st
century: elimination of the leading preventable causes
of premature death and disability in the USA. The
Lancet, 384(9937):45–52.
Brug, J. (2008). Determinants of healthy eating: motiva-
tion, abilities and environmental opportunities. Family
Practice, 25:i50–i55.
Cadilhac, D. A., Andrew, N. E., Busingye, D., Cameron,
J., Thrift, A. G., Purvis, T., Li, J. C., Kneebone, I.,
Thijs, V., Hackett, M. L., Lannin, N. A., Kilkenny,
M. F., and on behalf of the ReCAPS investigators
(2020). Pilot randomised clinical trial of an eHealth,
self-management support intervention (iVERVE) for
stroke: feasibility assessment in survivors 12–24
months post-event. Pilot and Feasibility Studies,
6(1):172.
Carey, R. N., Connell, L. E., Johnston, M., Rothman, A. J.,
de Bruin, M., Kelly, M. P., and Michie, S. (2018). Be-
havior change techniques and their mechanisms of ac-
tion: A synthesis of links described in published inter-
vention literature. Annals of Behavioral Medicine.
Cena, H. and Calder, P. C. (2020). Defining a healthy diet:
Evidence for the role of contemporary dietary patterns
in health and disease. Nutrients, 12(2):334.
Chaix, B., Bibault, J.-E., Pienkowski, A., Delamon, G.,
Guillemass
´
e, A., Nectoux, P., and Brouard, B. (2019).
When chatbots meet patients: One-year prospective
study of conversations between patients with breast
cancer and a chatbot. JMIR Cancer, 5(1):e12856.
Chokshi, N. P., Adusumalli, S., Small, D. S., Morris, A.,
Feingold, J., Ha, Y. P., Lynch, M. D., Rareshide, C.
A. L., Hilbert, V., and Patel, M. S. (2018). Loss-
framed financial incentives and personalized goal-
setting to increase physical activity among ischemic
heart disease patients using wearable devices: The
ACTIVE REWARD randomized trial. Journal of the
American Heart Association, 7(12):e009173.
Fitzpatrick, K. K., Darcy, A., and Vierhile, M. (2017). De-
livering cognitive behavior therapy to young adults
with symptoms of depression and anxiety using a fully
automated conversational agent (woebot): A random-
ized controlled trial. JMIR Mental Health, 4(2):e19.
Gardner, G., Elliott, D., Gill, J., Griffin, M., and Crawford,
M. (2005). Patient experiences following cardiotho-
racic surgery: An interview study. European Journal
of Cardiovascular Nursing, 4(3):242–250.
Ghandeharioun, A., McDuff, D., Czerwinski, M., and
Rowan, K. (2019). EMMA: An emotion-aware well-
being chatbot. In 2019 8th International Confer-
ence on Affective Computing and Intelligent Interac-
tion (ACII), pages 1–7. IEEE.
Grimmett, C., Corbett, T., Brunet, J., Shepherd, J., Pinto,
B. M., May, C. R., and Foster, C. (2019). Systematic
review and meta-analysis of maintenance of physical
activity behaviour change in cancer survivors. Inter-
national Journal of Behavioral Nutrition and Physical
Activity, 16(1):37.
Halldorsdottir, H., Thoroddsen, A., and Ingadottir, B.
(2020). Impact of technology-based patient education
on modifiable cardiovascular risk factors of people
with coronary heart disease: A systematic review. Pa-
tient Education and Counseling, 103(10):2018–2028.
Hevner, March, Park, and Ram (2004). Design science
in information systems research. MIS Quarterly,
28(1):75.
Horner, G. N., Agboola, S., Jethwani, K., Tan-McGrory, A.,
and Lopez, L. (2017). Designing patient-centered text
messaging interventions for increasing physical activ-
ity among participants with type 2 diabetes: Qualita-
tive results from the text to move intervention. JMIR
mHealth and uHealth, 5(4):e54.
Johnston, M., Carey, R. N., Connell Bohlen, L. E., John-
ston, D. W., Rothman, A. J., de Bruin, M., Kelly,
M. P., Groarke, H., and Michie, S. (2021). Devel-
opment of an online tool for linking behavior change
techniques and mechanisms of action based on trian-
gulation of findings from literature synthesis and ex-
pert consensus. Translational Behavioral Medicine,
11(5):1049–1065.
Kelly, J. T., Conley, M., Hoffmann, T., Craig, J. C., Tong,
A., Reidlinger, D. P., Reeves, M. M., Howard, K., Kr-
ishnasamy, R., Kurtkoti, J., Palmer, S. C., Johnson,
D. W., and Campbell, K. L. (2020). A coaching pro-
gram to improve dietary intake of patients with CKD:
ENTICE-CKD. Clinical Journal of the American So-
ciety of Nephrology, 15(3):330–340.
Kontis, V., Mathers, C. D., Rehm, J., Stevens, G. A., Shield,
K. D., Bonita, R., Riley, L. M., Poznyak, V., Beagle-
hole, R., and Ezzati, M. (2014). Contribution of six
risk factors to achieving the 25x25 non-communicable
disease mortality reduction target: a modelling study.
The Lancet, 384(9941):427–437.
Londral, A., Azevedo, S., Dias, P., Ramos, C., Santos, J.,
Martins, F., Silva, R., Semedo, H., Vital, C., Gualdino,
A., Falc
˜
ao, J., Lap
˜
ao, L. V., Coelho, P., and Fragata,
Designing a Digital Personal Coach to Promote a Healthy Diet and Physical Activity Among Patients After Cardiothoracic Surgery
601

J. G. (2022). Developing and validating high-value pa-
tient digital follow-up services: a pilot study in cardiac
surgery. BMC health services research, 22(1):680.
MacPherson, M., Cranston, K., Johnston, C., Locke, S.,
and Jung, M. E. (2021). Evaluation and refinement
of a bank of SMS text messages to promote behav-
ior change adherence following a diabetes prevention
program: Survey study. JMIR Formative Research,
5(8):e28163.
Mayberry, L. S., Berg, C. A., Greevy, R. A., Nelson,
L. A., Bergner, E. M., Wallston, K. A., Harper, K. J.,
and Elasy, T. A. (2021). Mixed-methods random-
ized evaluation of FAMS: A mobile phone-delivered
intervention to improve family/friend involvement in
adults’ type 2 diabetes self-care. Annals of Behavioral
Medicine, 55(2):165–178.
Michie, S., Richardson, M., Johnston, M., Abraham, C.,
Francis, J., Hardeman, W., Eccles, M. P., Cane, J.,
and Wood, C. E. (2013). The behavior change tech-
nique taxonomy (v1) of 93 hierarchically clustered
techniques: Building an international consensus for
the reporting of behavior change interventions. An-
nals of Behavioral Medicine, 46(1):81–95.
Michie, S., van Stralen, M. M., and West, R. (2011). The
behaviour change wheel: A new method for character-
ising and designing behaviour change interventions.
Implementation Science, 6(1):42.
Peffers, K., Tuunanen, T., Rothenberger, M. A., and Chat-
terjee, S. (2007). A design science research method-
ology for information systems research. Journal of
Management Information Systems, 24(3):45–77.
Pinto, A., Faiz, O., Davis, R., Almoudaris, A., and Vincent,
C. (2016). Surgical complications and their impact
on patients’ psychosocial well-being: a systematic re-
view and meta-analysis. BMJ Open, 6(2):e007224.
Polgreen, L. A., Anthony, C., Carr, L., Simmering, J. E.,
Evans, N. J., Foster, E. D., Segre, A. M., Cremer,
J. F., and Polgreen, P. M. (2018). The effect of au-
tomated text messaging and goal setting on pedome-
ter adherence and physical activity in patients with di-
abetes: A randomized controlled trial. PLOS ONE,
13(5):e0195797.
Schmitz, C. (2012). LimeSurvey: An Open Source survey
tool. LimeSurvey Project, Hamburg, Germany.
Sherwood, N. E. and Jeffery, R. W. (2000). The behav-
ioral determinants of exercise: implications for physi-
cal activity interventions. Annual Review of Nutrition,
20:21–44.
Stephens, T. N., Joerin, A., Rauws, M., and Werk, L. N.
(2019). Feasibility of pediatric obesity and predi-
abetes treatment support through tess, the AI be-
havioral coaching chatbot. Translational Behavioral
Medicine, 9(3):440–447.
Tadas, S., Pretorius, C., Foster, E. J., Gorely, T., Leslie,
S. J., and Coyle, D. (2021). Transitions in technology-
mediated cardiac rehabilitation and self-management:
Qualitative study using the theoretical domains frame-
work. JMIR Cardio, 5(2):e30428.
Thiengwittayaporn, S., Wattanapreechanon, P., Sakon, P.,
Peethong, A., Ratisoontorn, N., Charoenphandhu, N.,
and Charoensiriwath, S. (2021). Development of a
mobile application to improve exercise accuracy and
quality of life in knee osteoarthritis patients: a ran-
domized controlled trial. Archives of Orthopaedic and
Trauma Surgery.
Tully, P. J. (2013). Quality-of-life measures for cardiac
surgery practice and research: a review and primer.
The Journal of Extra-Corporeal Technology, 45(1):8–
15.
Warburton, D. E. and Bredin, S. S. (2017). Health bene-
fits of physical activity: a systematic review of current
systematic reviews. Current Opinion in Cardiology,
32(5):541–556.
WHO (2021). Cardiovascular diseases (CVDs).
Yusuf, S., Joseph, P., Rangarajan, S., Islam, S., Mente, A.,
Hystad, P., Brauer, M., Kutty, V. R., Gupta, R., Wiel-
gosz, A., AlHabib, K. F., Dans, A., Lopez-Jaramillo,
P., Avezum, A., Lanas, F., Oguz, A., Kruger, I. M.,
Diaz, R., Yusoff, K., Mony, P., Chifamba, J., Yeates,
K., Kelishadi, R., Yusufali, A., Khatib, R., Rahman,
O., Zatonska, K., Iqbal, R., Wei, L., Bo, H., Rosen-
gren, A., Kaur, M., Mohan, V., Lear, S. A., Teo, K. K.,
Leong, D., O’Donnell, M., McKee, M., and Dagenais,
G. (2020). Modifiable risk factors, cardiovascular dis-
ease, and mortality in 155 722 individuals from 21
high-income, middle-income, and low-income coun-
tries (PURE): a prospective cohort study. The Lancet,
395(10226):795–808.
Scale-IT-up 2023 - Workshop on Best Practices for Scaling-Up Digital Innovations in Healthcare
602
