
A Survey on Technologies Used During out of Hospital Cardiac Arrest
Gaurav Rao
1 a
, David W. Savage
2 b
, Vijay Mago
3 c
and Pawan Lingras
1
1
Saint Mary’s University, Halifax, Nova Scotia, Canada
2
Northern Ontario School of Medicine, Thunder Bay, Ontario, Canada
3
Lakehead University, Thunder Bay, Ontario, Canada
Keywords:
Out of Hospital Cardiac Arrest (OHCA), Automated External Defibrillator, Cardiopulmonary Resuscitation
(CPR), CPR Feedback, Fall Detection, Agonal Breathing, OHCA Workflow, Responder Network System.
Abstract:
Out of hospital cardiac arrest (OHCA) causes close to 400,000 deaths every year in North America, and
it is also a leading cause of death among young athletes. OHCA is a treatable medical condition, and the
patient’s survival chances can be increased if immediate treatment is provided to the patient. However, non-
treatment of the patient leads to a dramatic decline in survival chances at 10% per minute. Currently, various
technologies are being used, and many more are being researched to reduce the time to provide early treatment
to the patient. This survey focuses on summarizing various available technologies for use during OHCA. This
survey focuses on evaluating technologies used in each step of the OHCA process. In this survey, articles were
searched using the term “ohca” on Google Scholar and more than 18,000 articles were found. The articles
were further filtered using keywords for each stage of the OHCA process, finally, 112 articles were used in
this survey. The technologies that exist today work independently and are not linked with the other steps of the
OHCA process. Integration between these technologies could help in reducing time and increase the survival
chances of the patient.
1 INTRODUCTION
Sudden Cardiac Arrest (SCA) is a medical condi-
tion in which a patient’s heart either stops or beats
irregularly with little or no cardiac perfusion (Med-
lineplus.gov, 2021). Every year more than 350,000
deaths occur in the U.S. due to out of hospital car-
diac arrest (OHCA), and more than 40,000 deaths in
Canada (Heart.org, 2021a; Research, 2019). OHCA
is the leading cause of death among young athletes,
which means that SCA can occur to anyone irrespec-
tive of their health or age (Landry et al., 2017). Dur-
ing OHCA, the patient collapses and the blood circu-
lation to organs either stops or is insufficient to pre-
vent damage to organs (Medlineplus.gov, 2021). In
this condition, the patient’s survival rate decreases at
a significant rate of 10% per minute (Heart.org, 2014;
Valenzuela et al., 1997). With the rapid decline in
survival after each minute, early identification and re-
sponse by both bystanders and emergency medical
services (EMS) is required. The recommended treat-
a
https://orcid.org/0000-0003-1092-9617
b
https://orcid.org/0000-0003-2837-3127
c
https://orcid.org/0000-0002-9741-3463
ment with the greatest evidence for improving sur-
vival in OHCA is performing cardiopulmonary resus-
citation (CPR) and the application of the automated
external defibrillator (AED) (Heart.org, 2014; Nord
et al., 2017; Folke et al., 2021). Studies confirm that
the survival rate of the patient increases if the recom-
mended treatment is started within the first few min-
utes of the OHCA occurrence (Sanko et al., 2020; Pi-
jls et al., 2016).
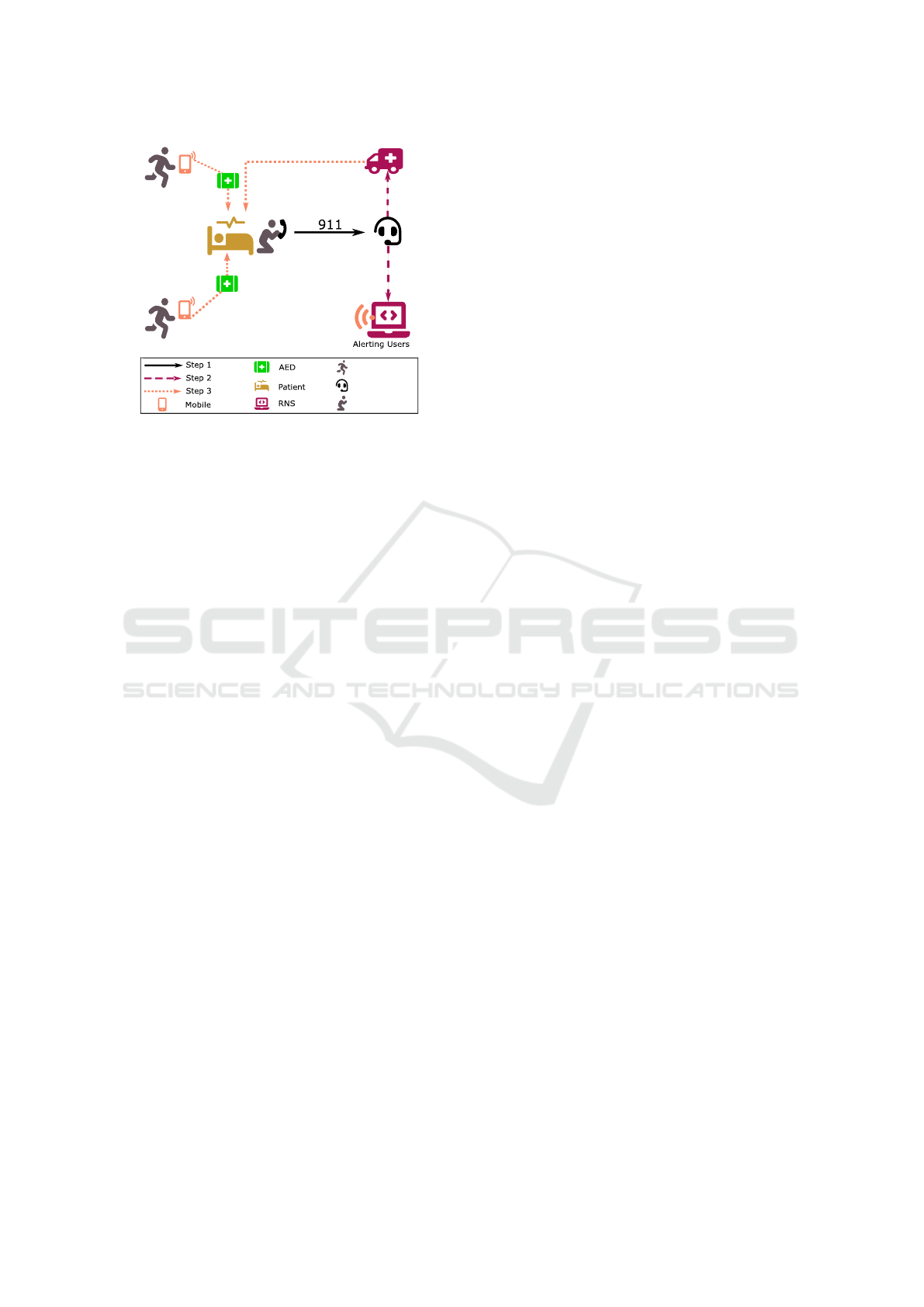
During an OHCA, several steps are performed
prior to the arrival of the EMS and if executed swiftly,
the survival chances of the patient increases. Figure 1
shows the workflow followed during the emergency.
The OHCA workflow includes steps taken by either
the bystanders or the dispatcher to assist the patient
until the emergency medical services arrive at the pa-
tient’s location. Figure 1, shows a graphical represen-
tation of the workflow. The first step of the OHCA
workflow is when a patient collapses or losses of con-
sciousness. This step can be observed by a bystander
or an intelligent device such as a smartphone, smart-
watch, or camera. The witnessing of the patient’s col-
lapse is essential as a delay in identifying the patient
suffering an OHCA delays the workflow and rapidly
Rao, G., Savage, D., Mago, V. and Lingras, P.
A Survey on Technologies Used During out of Hospital Cardiac Arrest.
DOI: 10.5220/0011749800003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 5: HEALTHINF, pages 477-488
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
477
RNS Responder
Dispatcher
Bystander
Figure 1: Emergency workflow.
decreases the patient’s survival chances (Chan et al.,
2019; Rea et al., 2021; Lu et al., 2019). The second
step in the OHCA workflow is to alert the emergency
services, the bystander can perform this by calling the
emergency services through a telephone. Depending
on the smart device, this step can be performed in var-
ious ways: 1) Send an alert to the patient’s emergency
contact and then they call the emergency services. 2)
The smart device sends an alert to its service provider
and then the service provider calls the emergency ser-
vices (Rao et al., 2020; Berglund et al., 2018). 3) The
smart device itself sends an alert to the emergency ser-
vices. The workflow’s third step includes dispatching
the emergency resources to the patient’s location, the
dispatcher performs this action. The emergency re-
sources activated for the patient depend on the ser-
vices available at the emergency center. The services
include: 1) dispatching emergency medical services,
2) dispatching fire and police units, and 3) activating
a Responder Network System (RNS) (Stieglis et al.,
2020; Rao et al., 2020). The fourth step is to re-
suscitate the patient by performing CPR. This step is
performed by either a bystander who witnessed the
OHCA or by a bystander who is responding after re-
ceiving the alert from RNS. At this step, the bystander
can be assisted by a feedback device or the dispatcher
to perform high-quality CPR (White et al., 2017; Plata
et al., 2019).
This survey is structured based on the steps fol-
lowed in the OHCA workflow and the technologies
used within each step of the workflow. Section 2 de-
scribes the search criteria used to select articles for
the survey. Section 3 explains the technologies used
for identifying a patient experiencing an OHCA. The
techniques used to confirm cardiac arrest in the pa-
tient are discussed in Section 4. Section 5 details
technologies used to assist a bystander to perform
high-quality CPR. In Section 6 technologies related
to AED assistance are discussed. Section 7 provides
a summary and discussion of all the technologies used
during the OHCA.
2 METHODOLOGY
OHCA is a broad topic for research as it includes top-
ics such as: 1) the training of the general public and
medical professionals in the use of technologies for
the management of cardiac arrest patients; 2) proto-
cols, procedures and technologies used by bystanders,
emergency dispatch centres, and emergency medical
services during cardiac arrest; 3) the treatment and
protocols used by the doctors and nurses at the hos-
pital after the arrival of the patient. The focus of this
survey is to summarize the technologies used by by-
standers or dispatch centres during an OHCA event.
The OHCA event can be divided into four steps: 1)
witness OHCA, 2) confirm OHCA, 3) CPR assis-
tance, and 4) AED assistance. The search strategy for
article selection for each of these steps is discussed
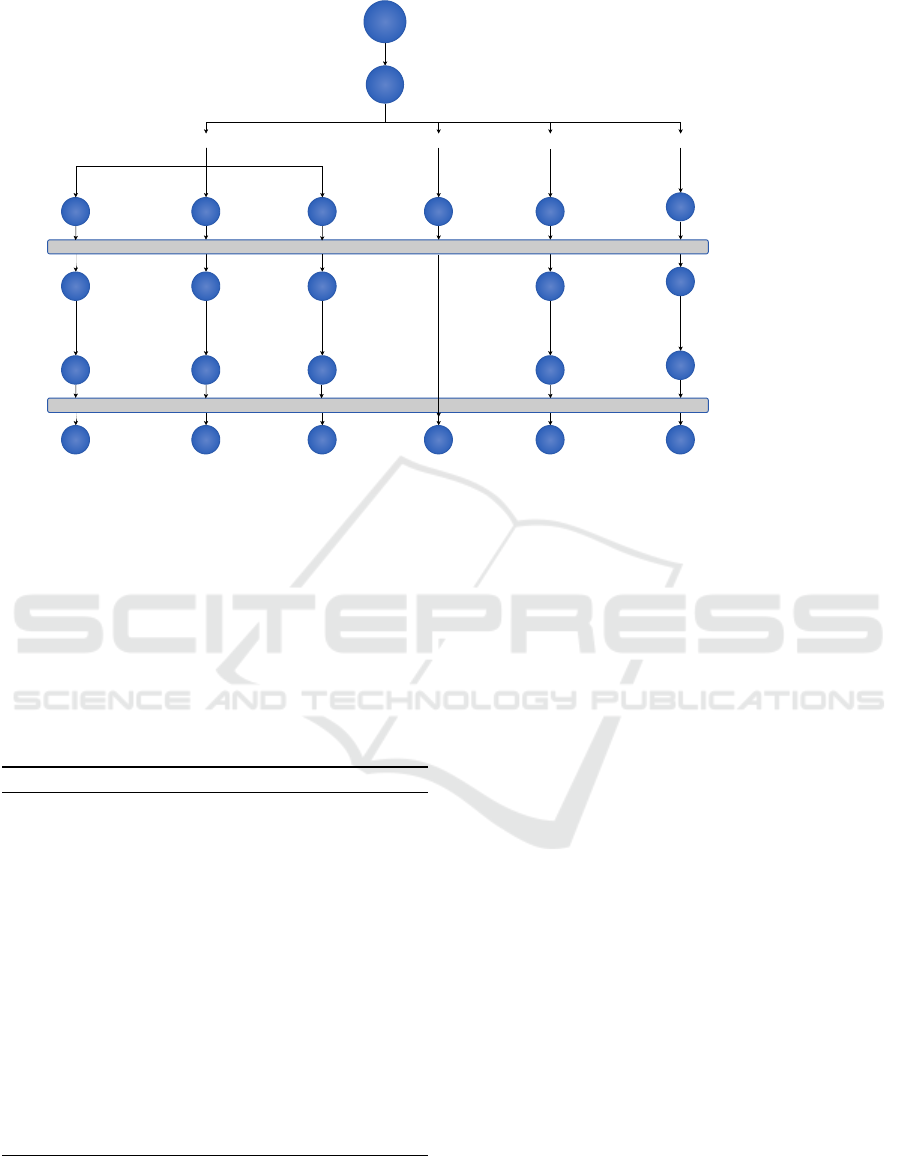
below and also shown in Figure 2.
To obtain the articles for this survey, a search was
performed with the term “OHCA” on Google Scholar
and PubMed, the query resulted in 8,950 and 1,937
matches, respectively (LLC, 2021; NIH, 2022). A
further comparison was performed on the results and
it was found that the Google Scholar results cov-
ered more than 90% of the articles found on Pubmed.
Therefore, all search queries for this survey were per-
formed on Google Scholar. For each step of the
OHCA workflow, a more comprehensive search query
was generated using a publication date filter set to find
articles from 2017 onward to review the latest tech-
nologies. The results from these queries were filtered
using a semi-automated filtering process to select only
the relevant article for each step.
Witness OHCA: To select articles for this section,
three different searches were aggregated, which are:
a) “OHCA detection smart watch”, b) “OHCA ago-
nal breathing identification”, and c) “OHCA fall de-
tection”. The filter of publishing date since 2017 was
also applied, and these queries resulted in 93, 276, and
367 articles, respectively. The number of duplicate
articles in each of these queries were 8, 7, 10, respec-
tively, and were removed from further analysis. The
next step for filtration was performed using a python
script called “QuickSearcher” or “QS”, pesudocode is
presented in Algorithm 1. The authors developed QS
to search for keywords with logical operations (AND,
OR) in the title or abstract of the article. For each
of the three queries, the following filtering query was
HEALTHINF 2023 - 16th International Conference on Health Informatics
478
Manual filtering
Removing duplicates
18,000+
8,950
93 276 367
85
18
7
705
62364
Google Scholar search query “ohca”
Filter since 2017
Witnessing OHCA CPR Assistance AED Assistance
"ohca detection
smart watch"
Confirming OHCA
QS filter : (smartwatch)
AND (identify OR
recognize OR detect)
"ohca agonal breathing
identification”
269
42
QS filter : (agonal)
AND (identify OR
recognize or detect)
9
"ohca fall detection”
357
53
5
QS filter: (fall AND
detect AND cardiac)
"ohca agonal
breathing call taker”
20
"ohca cpr feedback
technology”
603
142
37
QS filter :
(cpr or
compression)
"ohca aed AND find
OR locate”
689
84
34
QS filter: (aed OR aeds) AND (locate
OR search OR find OR near OR
close OR deliver OR transport OR
carry OR bring)
QS filter refers to the filtering performed using the “QuickSearcher”.
Figure 2: The method of selection and filtering of articles used in this survey, along with the count of articles selected at each
step.
made to QS, respectively: 1) smartwatch AND (iden-
tify OR recognize OR detect) 2) agonal AND (iden-
tify OR recognize OR detect) 3) fall AND detect AND
cardiac. A manual review was performed on the QS
results to identify articles relevant to this survey. The
authors performed the manual review and identified a
total of 21 articles from all three queries performed in
this section.
Algorithm 1: Pseudocode for Quick Searcher.
Input:
AllData = List of titles and abstract of the articles
AllSearch =List of combinations to search
Output:
List of articles matching search criteria
Process:
for data IN AllData do
AllMatchFound = True
newText = Join title and abstract in data
for search IN AllSearch do
if search Does Not match newText then
SET AllMatchFound = False
end if
end for
if AllMatchFound is True then
ADD article to output
end if
end for
Confirm OHCA: The initial query performed in
Google Scholar for this section was “ohca agonal
breathing call taker”, and articles published since
2017, resulting in 64 articles. Due to a small num-
ber of articles found, the authors performed a manual
review of the articles’ abstracts and selected 20 most
relevant articles.
CPR Assistance: In order to find articles for this sec-
tion, a Google Scholar search was performed using
the terms “ohca cpr feedback technology” for articles
published since 2017, which resulted in 623 articles
out of which 20 were duplicates. QS was used to fil-
ter the results further by using the query “compression
OR cpr”, which narrowed the results to 142. The au-
thors then performed a manual review of the title and
abstracts and selected 37 articles.
AED Assistance: The query was performed using
Google Scholar for this section using the terms “ohca
aed AND find OR locate”, for articles published since
2017. The query resulted in 705 articles which in-
cluded 16 duplicates. The results were further filtered
using the QS query “(aed OR aeds) AND (locate OR
search OR find OR near OR close OR deliver OR
transport OR carry OR bring)”. The QS algorithm
further reduced the number of articles to 84. A man-
ual review by authors resulted in a selection of 34 ar-
ticles for this section.
Exclusions: This survey discusses technologies cur-
rently being used during OHCA events, along with
the technologies under development for future use.
However, other technologies are being used during
OHCA workflow, such as mechanical CPR initi-
ated by first responders and healthcare profession-
A Survey on Technologies Used During out of Hospital Cardiac Arrest
479

als, advanced traffic light controls that allow ambu-
lances an unobstructed path to the emergency loca-
tion, advanced AED algorithms for early detection of
a shockable rhythm, and the use of audio and video
feedback in CPR training (Nguyen, 2019). These
technologies have been excluded as this survey fo-
cuses on technologies that directly affect the OHCA
workflow before the arrival of the emergency medical
services.
3 WITNESSING OHCA
A crucial part of the OHCA process is to witness the
occurence of OHCA event, which implies that there
should be a bystander nearby the patient who ob-
serves the patient experience OHCA symptoms and
reports the event to the emergency services. There
are a significant number of OHCA events that remain
unwitnessed as they occur in private dwellings or in
less crowded public places such as parking lots (Chan
et al., 2019). Patients who experience an unwitnessed
OHCA, experience a delayed response and treatment,
and with each minute delay, their survival chances
are reduced by 10% per minute (Ko et al., 2018;
Heart.org, 2021c). Multiple studies have confirmed
that early detection of the OHCA event increases the
survival chances of the patient (Chan et al., 2019;
Kiyohara et al., 2021). Thus, it is crucial to detect
the OHCA in the first few minutes of its occurrence,
such that the patient can be treated immediately. Vari-
ous technologies are being developed for the early de-
tection of the OHCA event, including smartwatches,
smart wristbands, radar detection, and fall detection.
These technologies are explained in detail below.
Body Sensors: Smartwatches and wristbands are
playing an important role in the health monitoring in-
dustry (Plata et al., 2019; Lu et al., 2019). These de-
vices are small and can be worn continuously with-
out interrupting day-to-day activities. Depending on
the device, they are equipped with sensors to capture
the user’s physical activity, ECG data, blood oxygen
levels, heart rate, and are capable of detecting falls
(Jesus, 2018; Chan et al., 2019). The information
collected on the device can synchronize with other
devices such as smartphones and tablets or even to
the cloud server via a cellular or Wi-Fi connection.
Some of these devices can detect medical conditions
such as irregular heart rhythms and low oxygen levels.
These devices can be programmed to send an emer-
gency alert to emergency services or to a designated
user specified in the emergency contacts upon detect-
ing an emergency (Fakhrulddin et al., 2019; Tanaka
et al., 2017).
Fall Detection: The patients collapse is the first ob-
served sign that a sudden cardiac arrest is occuring.
It is not always possible to have bystanders witness
and assist the patient; therefore, researchers have pro-
posed solutions to detect falls using smart devices.
Fall detection is a highly researched topic, a Google
Scholar search found over 233,000 articles using the
term “fall detection system” since 2017. A major-
ity of these proposed technologies use smartphones,
smartwatches, cameras, radar, and other IoT devices
to detect the fall (Bhattacharya and Vaughan, 2020;
King and Sarrafzadeh, 2018). Most of these systems
can send an alert when the user collapses to the reg-
istered emergency contact. Some of these devices
may use another device to send the alert, such as a
smartwatch using the paired smartphone to send the
alert. Additionally, security cameras are widely used
in offices, warehouses, parking lots, and especially in
isolated parts of a building, to address security con-
cerns. Artificial intelligence (AI) and machine learn-
ing (ML) algorithms can use the video from secu-
rity cameras to detect a person collapsing. For in-
stance, Scquizzato proposed an algorithm that can de-
tect OHCA from a security camera feed (Scquizzato,
2018).
Agonal Breathing Agonal breathing is a type of
“gasping” commonly seen in approximately half of
patients experiencing cardiac arrest (Chan et al.,
2019; Riou et al., 2018b). A recent study confirms
that if a patient experiences agonal breathing dur-
ing CPR, then the patient’s survival chances are 17%
higher than a cardiac arrest patient without agonal
breathing (Adams et al., 2017). A bystander can
quickly identify agonal breathing in a patient; in cases
when a bystander is not present, researchers have pro-
posed solutions that can detect agonal breathing us-
ing microphones built-in smart devices such as mo-
bile phones and smart speakers (Jesus, 2018; Rea
et al., 2021). Studies confirm that a significant num-
ber of SCA occur in the home environment (Chan
et al., 2019; Tsukigase et al., 2019). Agonal breathing
detection solutions work optimally in quiet environ-
ments, as these solutions require minimal background
noise so that the device can record the agonal breath-
ing.
4 CONFIRMATION OF CARDIAC
ARREST
Once the emergency dispatcher receives a call about
an emergency, they need to determine if the patient
is experiencing cardiac arrest or not. If the OHCA is
confirmed, the dispatcher then advises the bystander
HEALTHINF 2023 - 16th International Conference on Health Informatics
480

to perform CPR and communicate the confirmation
information to the dispatched ambulance. The time
taken by the dispatcher to confirm cardiac arrest may
cause a substantial delay in the patient’s treatment (Ko
et al., 2018; Fukushima and Bolstad, 2020). Studies
confirm that if the time taken by the dispatchers to
confirm OHCA is reduced, then the survival chances
of the patient increases (Adams et al., 2017; Sanko
et al., 2021). The early confirmation is also benefi-
cial as the dispatcher can dispatch other emergency
services (e.g., police and fire services) who can ar-
rive prior to the ambulance (Heart.org, 2021b). This
issue has been recognized in the literature and multi-
ple solutions have been proposed which are discussed
in this section (Riou et al., 2018b; Breckwoldt et al.,
2020).
When OHCA incidents occur in residential loca-
tions, the caller is generally known to the patient and
is emotionally distressed. In such situations, the dis-
patcher has to spend time calming the caller first be-
fore they can ask the caller to provide the patient’s in-
formation (Fukushima and Bolstad, 2020). When an
OHCA occurs in a public location, the caller some-
times steps away from the patient to call the emer-
gency services. The stepping away from the patient
may be due to overcrowding near the patient, cellular
reception or environmental noise (Case et al., 2018).
In such situations, when the dispatcher requests the
caller to check and provide the medical information of
the patient, the caller needs to go back to the patient
and then analyze the condition, causing the delay in
assessment (Fukushima and Bolstad, 2020).
Two significant recommendations from various
studies related to agonal breathing and OHCA are
1) overcoming the language and linguistic issues be-
tween the caller and dispatcher will improve out-
comes (Riou et al., 2017; Fukushima and Bolstad,
2020) and 2) if the dispatcher has confusion in de-
tecting agonal breathing, then CPR should be advised
(Adams et al., 2017; Leong et al., 2020). Overall,
early confirmation of cardiac arrest can help in reduc-
ing the time to resuscitate the patient.
5 ASSISTED CPR
After the dispatcher confirms that the patient is expe-
riencing cardiac arrest, the next step is to guide the
caller to perform CPR. CPR performed by bystanders
plays a vital role in increasing the patient’s survival
chances (White et al., 2018; Ng et al., 2021). By-
stander CPR is necessary because the ambulance dis-
patched to the patient’s location takes approximately
8-10 minutes, depending on the site of dispatch vehi-
cles (Van de Voorde et al., 2017; Chien et al., 2020).
The estimated time from the start of the emergency
to the arrival of the emergency services is estimated
to be between 8 and 15 minutes, leading to almost
100% mortality for patients who do not receive chest
compressions (Ko et al., 2018; Heart.org, 2021c; An-
delius et al., 2019). Figure 3, shows an estimate of the
time required at each step of the SCA workflow.
Figure 3: Figure showing an estimated timeline graph of the
steps performed during an OHCA.
The CPR quality directly affects the patient’s sur-
vival chances; high quality CPR increases a patients
chances of survival (Ng et al., 2021; Estabrooks,
2018). Medical agencies have defined CPR per-
formance metrics; for instance, the American Heart
Association (AHA) defines that high-quality CPR
should have a chest compression depth between 2
and 2.4 inches at a rate of 100-120 compressions per
minute (Heart.org, 2015). The European Resusci-
tation Council recommends that chest compressions
should have a depth of 5–6 cm with a rate of 100–
120 compressions per minute (Perkins et al., 2015).
These standards are likely unknown to bystanders un-
less they are trained in CPR. Also, it is not easy for
the bystander to measure the compression depth and
the frequency during a stressful emergency scenario.
Researchers have proposed various solutions to over-
come this issue, such as guiding the bystander over
the phone, real-time CPR feedback devices to im-
prove performance, and mechanical devices to per-
form CPR automatically (Riou et al., 2018a; Case
et al., 2018). These technologies are discussed in the
following subsections.
Telephone Assisted CPR: Telephone assisted CPR
is also known as “Tele CPR”, “TCPR”, or “DA-CPR”
(Dispatcher Assisted CPR) (Hardeland et al., 2017;
Al Hasan et al., 2019). In this CPR assistance method,
the dispatcher advises the caller to perform CPR and
guides them on performing high-quality CPR (Sanko
et al., 2021; Al Hasan et al., 2019). This type of
assisted CPR is the most commonly used since it
does not require any additional hardware or software.
A Survey on Technologies Used During out of Hospital Cardiac Arrest
481
Also, the dispatcher can modify their instructions as
per the caller to help them understand and perform
high-quality CPR (Riou et al., 2018a). Assisted CPR
can encounter challenges caused by the communica-
tion between the two parties. One significant con-
cern is the refusal by the caller to perform CPR ei-
ther due to their physical ability, emotional barriers,
or legal concerns. The patient needs to be placed on a
hard flat surface such as a floor for performing CPR.
The physical movement of the patient might be chal-
lenging for the caller due to their own physical abil-
ity. Another concern is the refusal by the caller to
perform CPR, which may be due to their low confi-
dence level, emotional anxiety, or legal concern that
they might hurt the patient (Fukushima and Bolstad,
2020; Takahashi et al., 2018). Linguistic differences
between the dispatcher and the caller are also a con-
cern as they may affect the delivery of the instruction
and their feedback (Sanko et al., 2021; Case et al.,
2018). Researchers have also proposed training the
dispatcher to improve communication with the caller
(Al Hasan et al., 2019; Michiels et al., 2020). Studies
have shown that the dispatchers were able to convince
38% more callers to perform CPR after receiving the
specialized training (Riou et al., 2018b). Tele CPR
is dependent on the communication between the dis-
patcher and the caller. There will be situations where
the dispatcher’s instructions are not accurately heard
and understood by the caller due to the surrounding
noise or linguistic challenges, ultimately affecting the
CPR quality and patient’s survival chances (Leong
et al., 2020; Gram et al., 2021).
Video-Assisted CPR: Video-assisted CPR (V-CPR)
technology allows the dispatcher to view the CPR
performed by the caller over video and provide real-
time feedback to the CPR provider (Lee et al., 2021a;
Meinich-Bache et al., 2018). This technology is one
of the latest methods proposed for dispatchers but
it has not been implemented widely. Once the dis-
patcher confirms that the patient is experiencing car-
diac arrest and another bystander can hold the phone,
the dispatcher switches the audio call to a video call
(Lee et al., 2021a). The second bystander holds the
device such that the dispatcher can view the CPR be-
ing performed and provides real-time feedback to the
bystander to perform high-quality CPR (Kim et al.,
2020). Studies confirm that CPR quality improved
when video feedback was provided (Ali et al., 2019;
Lee et al., 2021b). Studies have also confirmed that
the time spent explaining hand placement on the chest
was reduced during V-CPR with subsequent feedback
able to make quick corrections to improve CPR qual-
ity. (Lin et al., 2018; Ecker et al., 2020). V-CPR
technology has some limitations, implementing this
system in existing dispatch centres will require signif-
icant cost. The cost will include adding a high-speed,
secure network for streaming videos, and a software
upgrade to switch audio calls to video calls. Also,
another uncontrollable factor is that the bystander
should have a cellphone that allows video calling.
These requirements may be fulfilled in major cities,
but the overhead cost may be too high for rural areas
(Hambly and Rajabiun, 2021; Durish, 2020).
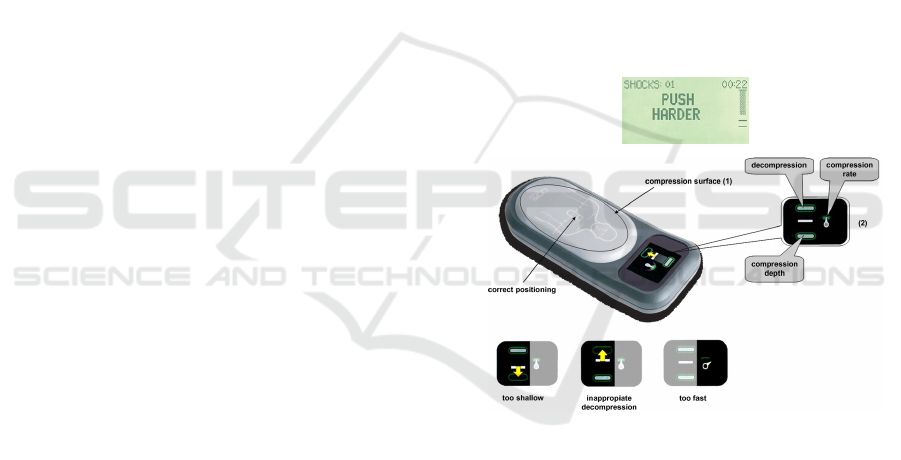
CPR Feedback Devices: CPR feedback devices are
designed to provide real-time feedback to the CPR
performer to provide high-quality CPR. CPR feed-
back devices are external hardware devices encapsu-
lated with various sensors to analyze current CPR per-
formance and compare it with high-quality CPR stan-
dards (i.e., compression depth of 5-6 cm and compres-
sion rate from 100-120 per minute). After compar-
ing actual CPR performing metrics with high-quality
CPR standards, these devices provide audio, visual, or
both feedback to the user for achieving high-quality
CPR.
Figure 4: Image showing Visual Feedback indications on
CPR feedback devices. Top image: Zoll Real CPR Help,
Source: https://www.zoll.com/. Bottom image: Laerdal
feedback device, Source: Skorning et al., Resuscitation
(2010).
Many CPR feedback devices are available on the
market, such as Real CPR Help and CPRmeter 2
(Zoll, 2021; Laerdal, 2021). These devices are placed
on the patient’s chest and the CPR performer places
their hands on the device and performs CPR. Most of
these devices consist of two sensors, one measuring
acceleration and another measuring force. Based on
the data collected from these sensors, the device an-
alyzes the CPR performance and provides feedback.
Depending on the device, the feedback can be visual,
showing if the parameter is in optimal range or not,
shown in Figure 4. However, these devices are ex-
HEALTHINF 2023 - 16th International Conference on Health Informatics
482

Table 1: A comparison of technologies used to perform CPR during an OHCA.
Technologies Availability
during
OHCA
Additional
person
required
Ease of use Time to
setup
Hardware re-
quirement
Cost Can
cause
harm
Market
avail-
ability
Tele CPR Easy No Hard None None None Yes Yes
Camera Easy Yes Easy Little Camera phone None Minor Yes
Smart
watch
Easy No Easy None Smartwatch None None Yes
Feedback
devices
Hard No Hard Hard Special device High None Yes
AR Hard No No Little Special device High None No
VR Hard No No Little Special device High None No
pensive and are not publicly available for help dur-
ing OHCA incidents. Some researchers are propos-
ing smaller devices similar to the size of a credit
card, which will help portability but still limit the use
of these devices in an actual incident (White et al.,
2018). Another type of CPR feedback device on the
market are contained in smartphone and smartwatch
devices (Sevil et al., 2021; Plata et al., 2019). As
the degree of portability increases, the probability of
these devices being used during an emergency also
increases. These devices use the built-in sensors like
accelerometer and gyroscope to evaluate the perfor-
mance of the CPR and can provide audio, visual and
haptic feedback for improving CPR performance in
real-time (Jeon et al., 2021). With technology con-
tinually improving, the number of CPR feedback de-
vices continues to expand with the latest technologies
being Virtual Reality (VR) and Augmented Reality
(AR) (Vaughan et al., 2019; Higashi et al., 2017).
At the time of writing this review, the authors are not
aware of any application of these technologies in ac-
tual OHCA. Overall, many CPR feedback devices are
available for OHCA usage and studies confirm that
these devices improve CPR performance. However,
due to their high cost and limited availability, these
devices are often used for CPR training but not dur-
ing OHCA. Table 1 compares the different CPR assis-
tance technologies used during OHCA and highlights
the drawbacks of each technology.
6 AED ASSISTANCE
The American Heart Association and the European
Resuscitation Council recommend that in addition to
providing high quality CPR, the patient should also
be defibrillated using an AED device if they have the
appropriate heart rhythm (Sondergaard et al., 2018;
Heart.org, 2021b). Multiple studies have confirmed
an increased rate of survival for patients when AEDs
were used during an OHCA (Heart.org, 2014). AEDs
are an electronic device consisting of a central unit
and two electrode pads. For portable AEDs used dur-
ing OHCA, the central unit consists of a battery and a
mini-computer to capture and interpret the ECG and
other information needed by the AED. The electrode
pads are placed on the patient’s body to collect the
ECG information and delivers an electric shock if
needed. When a bystander calls the emergency ser-
vices during a SCA emergency, the dispatcher sends
an ambulance and provides instructions to the caller
to perform CPR on the patient. At this stage of the
SCA workflow, it becomes vital to apply an AED
to the patient to increase their chances of survival.
Finding an AED nearby and bringing it to the patient
are the two biggest challenges faced at this stage of
SCA workflow. These challenges are recognized and
have been investigated by several researchers (Murata
et al., 2021; Telec et al., 2018). The following subsec-
tions detail the various technological solutions pro-
posed by researchers for finding and getting the AED
to the patient during OHCA.
Finding AED: AEDs are small devices, generally
placed in corridors, on shelves, in cabinets and other
places. Studies show that the existing AEDs are un-
derutilized because bystanders are unable to find them
during an emergency since many are placed in areas
with restricted access or in unmarked locations (Fred-
man, 2018; Cunningham et al., 2019). Another sig-
nificant issue found in the studies is that the AEDs
are not optimally placed compared to the OHCA oc-
currence, which results in low availability of AEDs
in high OHCA prone geographical locations (Srini-
vasan et al., 2017; Leung et al., 2021). The follow-
ing solutions proposed in the literature to find AEDs
are: 1) Mobile-based Applications, 2) Dispatcher As-
sisted, and 3) RNS. There are currently many free mo-
bile applications available on the Google Play Store
and the Apple App Store that can help the user to
find a nearby AED, such as AED Quebec, Staying
Alive, and PulsePoint AED (Champlain, 2021; As-
sociation RMC-BFM and AEDMAP, 2021; Founda-
tion, 2021). These mobile applications generally use
crowdsourcing techniques to collect AED informa-
A Survey on Technologies Used During out of Hospital Cardiac Arrest
483

Table 2: A comparison between the technologies used to find nearby AED devices during an OHCA event.
Finding AED using Mobile Appli-
cation
Finding AED using Dis-
patcher Assisted
Finding AED using RNS
Action by Bystander Dispatcher RNS system
Requirements Mobile App 911 system with AED listing 911 RNS integration
Advantage Can be used when 911 or RNS is
not available
Bystander can focus on CPR,
dispatcher helps finding AED
Fully automatic and con-
sider various situations
Disadvantage Pre-installed mobile application.
Latest AED information on app.
May distract dispatcher in help-
ing the bystander perform CPR.
RNS responder should
agree carrying the AED
Data Reliability Low High High
tion (Neves Briard et al., 2019; Chua et al., 2020).
In a dispatcher assisted AED location system, the dis-
patcher has access to a particular platform integrated
within the existing emergency services system to find
the available AEDs near the patient’s location (Per-
era et al., 2020; Tsukigase et al., 2019). This sys-
tem offloads the work of finding an AED from the by-
stander to the dispatcher. The RNS system can help in
finding AEDs during an emergency and is controlled
and activated by the dispatcher (Berglund et al., 2018;
Stieglis et al., 2020). RNS are automated systems that
find and alert registered users near the emergency to
assist the patient by finding an AED or performing
CPR. RNS have access to the AED location informa-
tion and can find the nearest AEDs to the emergency
(Rao et al., 2019; Smith et al., 2020; Rao et al., 2020).
Table 2 summarizes various technologies used in find-
ing the nearby AEDs during an OHCA emergency.
Delivering the AED: Once the nearest AED is found
by the methods described above, the next challenge
is to quickly bring the AED to the patient. The de-
livery mechanisms are linked to the technology used
to find an AED. For example, if a mobile applica-
tion is used to find the AED, then another bystander
must bring the AED to the patient (Neves Briard et al.,
2019; Chua et al., 2020). In this scenario, another by-
stander is required because the first bystander should
not stop performing CPR to get an AED according
to the AHA guidelines (Heart.org, 2014; Heart.org,
2021c). Therefore, this technique may not work in
situations when another bystander is not available.
The second way of AED delivery is dispatcher as-
sisted, and this method is very similar to the mo-
bile application method of delivery discussed above
(Perera et al., 2020; Tsukigase et al., 2019). The
critical difference between the two methods is that
the dispatcher provides the location of the nearest
AED in this method. In this situation, there is a
high probability that the location of the AED is cor-
rect. However, this method shares the identical draw-
back: one bystander must make a round trip to attain
the AED while another bystander performs CPR. The
third method of AED delivery discussed is via RNS.
In this method, the dispatcher activates the RNS sys-
tem, which then finds AEDs and responders in close
proximity to the patient and provides instructions to
either carry an AED or reach the emergency to as-
sist the patient depending on their locations (Stieglis
et al., 2020; Smith et al., 2020). These systems have
been implemented in limited geographical locations
in the world due to their significant cost of setup
(Stieglis et al., 2020; Berglund et al., 2018). Another
innovative and advanced technology proposed by re-
searchers for the delivery of the AED is by drones
(Fredman, 2018; Shirane, 2020). These devices have
been tested in simulated OHCA incidents, with mul-
tiple studies confirming that they can be used during
OHCA and can deliver AEDs faster than any existing
method of delivery (Sanfridsson et al., 2019; Nguyen,
2019). Table 3 summarizes various technologies used
in delivering the AEDs to the patient. Yet another way
to deliver an AED faster is to optimize their placement
such that AEDs can be accessed more quickly in loca-
tions that cover a larger geographical area. This issue
and its solutions are discussed in the following sub-
section.
AED Placement: Existing AEDs have been under-
used during OHCA incidents and one significant rea-
son for their under utilization is the distance be-
tween the emergency and the AED (Deakin et al.,
2018; Sondergaard et al., 2018; Cunningham et al.,
2019). Multiple studies show that if the placement
of the AEDs is optimized, then their use will in-
crease and ultimately the patient’s chances of survival
will improve (Cunningham et al., 2019; Srinivasan
et al., 2017). Researchers have proposed mathemati-
cal models to determine the optimized locations of the
AEDs (Leung et al., 2021; Derevitskii et al., 2020).
These models include a mathematical formulation to
identify high-risk OHCA zones, positioning based on
historical OHCA incidents, and equally distributing
the units across levels of socioeconomic deprivation.
HEALTHINF 2023 - 16th International Conference on Health Informatics
484
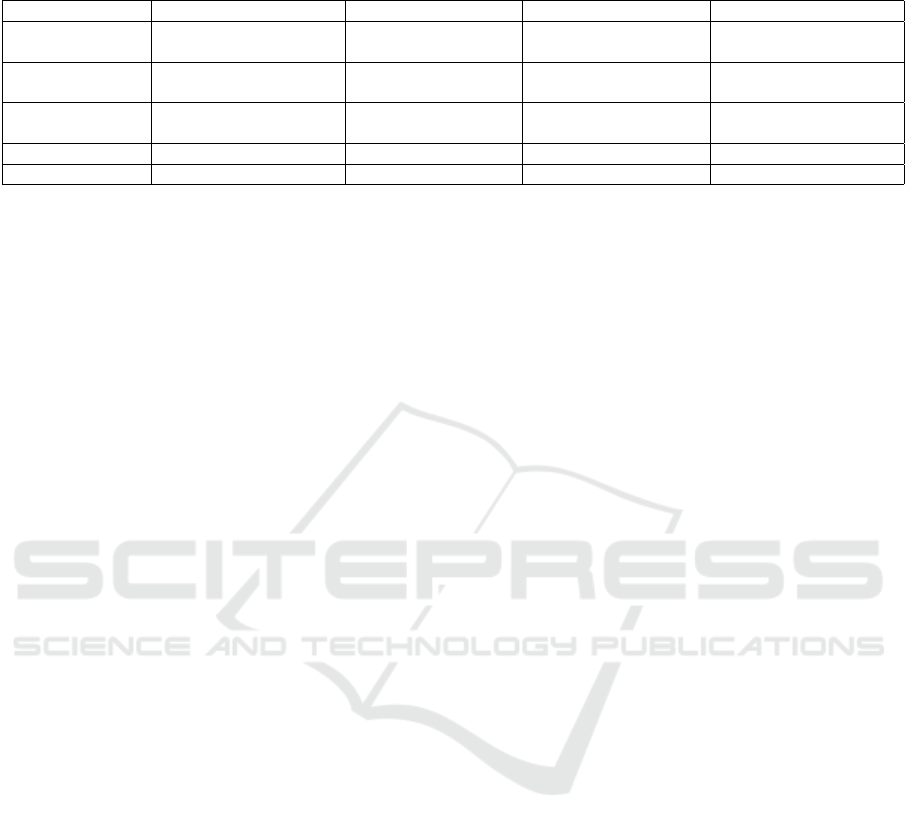
Table 3: A comparison between the technologies used to deliver AED devices to the emergency location during an OHCA
event.
Mobile Application Dispatcher Assisted RNS Drone
Time to delivery Two way trip, going
and getting it
Two way trip, going
and getting it
One way trip, getting
the AED enroute
One way trip, getting
the AED enroute via air
Constraints Requries another by-
stander
Requries another by-
stander
Requires RNS respon-
der to bring the AED
Requires a nearby
drone station.
Advantage Bystander can search
for AED
Bystander focuses on
getting AED
Multiple responders
get different AEDs
Time to delivery is low-
est
Cost Low Low Low High
Currently Used Yes Yes Yes In trial
7 DISCUSSION AND
CONCLUSION
SCA patient’s survival chances depended on the by-
stander, their CPR knowledge, past CPR training, and
CPR performance. We are in a new era, various tech-
nologies have been developed to assist the patient in
receiving early resuscitation and increasing their sur-
vival chances.
Currently, technologies assist bystanders in pro-
viding early resuscitation to the patient. One of the
primary reasons for delays in response to OHCA or
no assistance being provided to the patient relates to
the location of the cardiac arrest. A large number
of OHCAs occur at home, in parking lots, or other
private locations, where bystanders are not available
to assist the patient. Researchers have proposed fall
detection, agonal breathing and camera monitoring
as solutions for detecting OHCA occurrence in these
places. The fall detection method uses sensors such
as an accelerometer, gyroscope, heart rate sensor, or
ECG sensor that are available on smartwatches, smart
bands, and smartphones. Furthermore, these devices
can also monitor heart rhythm to confirm cardiac ar-
rest using advanced algorithms depending on the de-
vice. This method of OHCA detection can be used
in the community and is effective since many of the
smart devices are now part of people’s day-to-day life.
The technological solutions described in this re-
view have the potential to improve mortality for those
patients experiencing an OHCA. The feasibility of
these proposed solutions depends on the technologies
adopted either by the bystander or the dispatch cen-
ter. The use of smart devices such as smartphones
and smartwatches is one of the most practical solu-
tions as they are widely used and have become part
of the day-to-day life of people. There are indirect
ways that can help to increase the survival chances of
the SCA patient, such as better AED placement and
better CPR training. Researchers have proposed solu-
tions for these issues as well. This survey provides
an overview of the current and future technologies
that can be used during an OHCA event. This sur-
vey provides a good foundation for researchers who
intend to develop or advance technologies used dur-
ing OHCA, it will also help them integrate their own
solutions within the OHCA workflow.
REFERENCES
Adams, D., Debaty, G., Labarere, J., Frascone, R. J.,
Wayne, M. A., Swor, R. A., Mahoney, B. D., Domeier,
R. M., Olinger, M. L., O’Neil, B. J., Yannopou-
los, D., Aufderheide, T. P., and Lurie, K. G. (2017).
Long-term prognostic value of gasping during out-of-
hospital cardiac arrest. Journal of the American Col-
lege of Cardiology, 70(12):1467–1476.
Al Hasan, D., Drennan, J., Monger, E., Mahmid, S. A., Ah-
mad, H., Ameen, M., and El Sayed, M. (2019). Dis-
patcher assisted cardiopulmonary resuscitation imple-
mentation in kuwait a before and after study examin-
ing the impact on outcomes of out of hospital cardiac
arrest victims. Medicine (United States), 98(44).
Ali, S., Athar, M., and Ahmed, S. (2019). A randomised
controlled comparison of video versus instructor-
based compression only life support training. Indian
Journal of Anaesthesia, 63(3):188–193.
Andelius, L., Hansen, C., Lippert, F., Karlsson, L.,
Torp-Pedersen, C., Gislason, G., and Folke, F.
(2019). 40 long ambulance response time is associ-
ated with higher incidence of cardiopulmonary resus-
citation and defibrillation by dispatched citizen first-
responders. BMJ Open, 9(Suppl 2):A15—-A15.
Association RMC-BFM and AEDMAP (2021). Staying
alive - apps on google play.
Berglund, E., Claesson, A., Nordberg, P., Dj
¨
arv, T., Lund-
gren, P., Folke, F., Forsberg, S., Riva, G., and Ringh,
M. (2018). A smartphone application for dispatch of
lay responders to out-of-hospital cardiac arrests. Re-
suscitation, 126:160–165.
Bhattacharya, A. and Vaughan, R. (2020). Deep learning
radar design for breathing and fall detection. IEEE
Sensors Journal, 20(9):5072–5085.
Breckwoldt, I. R. D., Geri, G., Brooks, S., Couper, K.,
Hatanaka, T., Kudenchuk, P., Olasveengen, T., Pel-
A Survey on Technologies Used During out of Hospital Cardiac Arrest
485

legrino, J., Schexnayder, S. M., Morley, P., Mancini,
M. B., Travers, A., and Cast, M. (2020). Diagnosis of
out-of-hospital cardiac arrest by emergency medical
dispatch: a diagnostic systematic review. Resuscita-
tion.
Case, R., Cartledge, S., Siedenburg, J., Smith, K., Straney,
L., Barger, B., Finn, J., and Bray, J. E. (2018). Identi-
fying barriers to the provision of bystander cardiopul-
monary resuscitation (cpr) in high-risk regions: A
qualitative review of emergency calls. Resuscitation,
129:43–47.
Champlain, F. J.-d. (2021). Aed - quebec - apps on google
play.
Chan, J., Rea, T., Gollakota, S., and Sunshine, J. E. (2019).
Contactless cardiac arrest detection using smart de-
vices. npj Digital Medicine, 2(1).
Chien, C. Y., Tsai, S. L., Tsai, L. H., Chen, C. B., Seak,
C. J., Weng, Y. M., Lin, C. C., Ng, C. J., Chien, W. C.,
Huang, C. H., Lin, C. Y., Chaou, C. H., Liu, P. H.,
Tseng, H. J., and Fang, C. T. (2020). Impact of trans-
port time and cardiac arrest centers on the neurolog-
ical outcome after out-of-hospital cardiac arrest: A
retrospective cohort study. Journal of the American
Heart Association, 9(11).
Chua, S. Y. I., Ng, Y. Y., and Ong, M. E. H. (2020). Getting
r-aedi to save lives in singapore. Singapore Medical
Journal, 61(2):60–62.
Cunningham, C. J., Lowe, J., Johnson, A., Carter, W.,
Whited, W. M., Shofer, F. F., Brice, J. H., and
Williams, J. G. (2019). Public access defibrillation:
Utilisation and missed opportunities. Australasian
Journal of Paramedicine, 16.
Deakin, C. D., Anfield, S., and Hodgetts, G. A. (2018). Un-
derutilisation of public access defibrillation is related
to retrieval distance and time-dependent availability.
Heart, 104(16):1339–1343.
Derevitskii, I., Kogtikov, N., Lees, M. H., Cai, W., and Ong,
M. E. (2020). Risk-based aed placement - singapore
case. Lecture Notes in Computer Science (including
subseries Lecture Notes in Artificial Intelligence and
Lecture Notes in Bioinformatics), 12140 LNCS:577–
590.
Durish, N. (2020). A Case Study in the Design and Develop-
ment of a Community-Based Internet Assessment Ini-
tiative in Rigolet, Nunatsiavut, Canada. PhD thesis,
University of Guelph.
Ecker, H., Lindacher, F., Adams, N., Hamacher, S., Win-
gen, S., Schier, R., B
¨
ottiger, B. W., and Wetsch, W. A.
(2020). Video-assisted cardiopulmonary resuscita-
tion via smartphone improves quality of resuscitation:
A randomised controlled simulation trial. European
Journal of Anaesthesiology, 37(4):294–302.
Estabrooks, A. G. (2018). an Analysis of Certified Athletic
Trainers’ Ability To Provide High-Quality Cardiopul-
monary Resuscitation (Cpr) Over Hockey Shoulder
Pads. search.proquest.com.
Fakhrulddin, S. S., Gharghan, S. K., Al-Naji, A., and Chahl,
J. (2019). An advanced first aid system based on an
unmanned aerial vehicles and a wireless body area
sensor network for elderly persons in outdoor envi-
ronments. Sensors (Switzerland), 19(13).
Folke, F., Andelius, L., Gregers, M. T., and Hansen, C. M.
(2021). Activation of citizen responders to out-of-
hospital cardiac arrest. Current opinion in critical
care, 27(3):209–215.
Foundation, P. (2021). Pulsepoint aed - apps on google play.
Fredman, D. (2018). Placement of automated external de-
fibrillators and logistics to facilitate early defibrilla-
tion in sudden cardiac arrest. PhD thesis, Karolinska
Institutet.
Fukushima, H. and Bolstad, F. (2020). Telephone cpr: cur-
rent status, challenges, and future perspectives. Open
Access Emergency Medicine.
Gram, K. H., Præst, M., Laulund, O., and Mikkelsen, S.
(2021). Assessment of a quality improvement pro-
gramme to improve telephone dispatchers’ accuracy
in identifying out-of-hospital cardiac arrest. Resusci-
tation Plus, 6:100096.
Hambly, H. and Rajabiun, R. (2021). Rural broadband:
Gaps, maps and challenges. Telematics and Informat-
ics, 60:101565.
Hardeland, C., Sk
˚
are, C., Kramer-Johansen, J., Birkenes,
T. S., Myklebust, H., Hansen, A. E., Sunde, K., and
Olasveengen, T. M. (2017). Targeted simulation and
education to improve cardiac arrest recognition and
telephone assisted cpr in an emergency medical com-
munication centre. Resuscitation, 114:21–26.
Heart.org (2014). Every second counts aed fact sheet 2014.
Heart.org (2015). New resuscitation guidelines update cpr
chest pushes.
Heart.org (2021a). 2021 Heart Disease and Stroke Statistics
Update Fact Sheet At-a-Glance.
Heart.org (2021b). Emergency treatment of cardiac arrest
— american heart association.
Heart.org (2021c). What is cpr?
Higashi, E., Fukagawa, K., Kasimura, R., Kanamori, Y.,
Minazuki, A., and Hayashi, H. (2017). Development
and evaluation of a corrective feedback system us-
ing augmented reality for the high-quality cardiopul-
monary resuscitation training. 2017 IEEE Interna-
tional Conference on Systems, Man, and Cybernetics,
SMC 2017, 2017-Janua:716–721.
Jeon, S. A., Chang, H., Yoon, S. Y., Hwang, N., Kim, K.,
Yoon, H., Hwang, S. Y., Shin, T. G., Cha, W. C., and
Kim, T. (2021). Effectiveness of smartwatch guidance
for high-quality infant cardiopulmonary resuscitation:
A simulation study. Medicina (Lithuania), 57(3):1–
10.
Jesus, D. A. B. (2018). Accelerometer signals for detection
of pulse presence and blood pressure inference. PhD
thesis, Universidade D CIMBRA.
Kim, G. W., Lee, D. K., Kang, B. R., Jeong, W. J., Lee,
C. A., Oh, Y. T., Kim, Y. J., and Park, S. M. (2020). A
multidisciplinary approach for improving the outcome
of out-of-hospital cardiac arrest in south korea. Euro-
pean Journal of Emergency Medicine, 27(1):46–53.
King, C. E. and Sarrafzadeh, M. (2018). A survey of
smartwatches in remote health monitoring. Journal
of Healthcare Informatics Research, 2(1-2):1–24.
Kiyohara, K., Okubo, M., Komukai, S., Izawa, J., Gibo, K.,
Matsuyama, T., Kiguchi, T., Iwami, T., and Kitamura,
HEALTHINF 2023 - 16th International Conference on Health Informatics
486

T. (2021). Association between resuscitative time on
the scene and survival after pediatric out-of-hospital
cardiac arrest. Circulation Reports, 3(4):211–216.
Ko, S. Y., Ro, Y. S., Shin, S. D., Song, K. J., Hong, K. J.,
and Kong, S. Y. (2018). Effect of a first responder on
survival outcomes after out-of-hospital cardiac arrest
occurs during a period of exercise in a public place.
PLoS ONE, 13(2).
Laerdal (2021). Cprmeter 2 — laerdal medical.
Landry, C. H., Allan, K. S., Connelly, K. A., Cunningham,
K., Morrison, L. J., and Dorian, P. (2017). Sudden car-
diac arrest during participation in competitive sports.
New England Journal of Medicine, 377(20):1943–
1953.
Lee, H. S., You, K., Jeon, J. P., Kim, C., and Kim, S.
(2021a). The effect of video-instructed versus audio-
instructed dispatcher-assisted cardiopulmonary resus-
citation on patient outcomes following out of hospital
cardiac arrest in seoul. Scientific Reports.
Lee, S. G. W., Kim, T. H., Lee, H. S., Shin, S. D.,
Song, K. J., Hong, K. J., Kim, J. H., and Park, Y. J.
(2021b). Efficacy of a new dispatcher-assisted car-
diopulmonary resuscitation protocol with audio call-
to-video call transition. American Journal of Emer-
gency Medicine, 44:26–32.
Leong, W. K., Leong, S. H., Arulanandam, S., Ng, M., Ng,
Y. Y., Ong, M. E. H., and Mao, R. H. (2020). Simpli-
fied instructional phrasing in dispatcher-assisted car-
diopulmonary resuscitation – when ‘less is more’. Sin-
gapore Medical Journal.
Leung, K. B., Brooks, S. C., Clegg, G. R., and Chan, T. C.
(2021). Socioeconomically equitable public defibril-
lator placement using mathematical optimization. Re-
suscitation, 166:14–20.
Lin, Y. Y., Chiang, W. C., Hsieh, M. J., Sun, J. T.,
Chang, Y. C., and Ma, M. H. M. (2018). Qual-
ity of audio-assisted versus video-assisted dispatcher-
instructed bystander cardiopulmonary resuscitation:
A systematic review and meta-analysis. Resuscitation,
123:77–85.
LLC, G. (2021). Google scholar.
Lu, T. C., Chang, Y. T., Ho, T. W., Chen, Y., Lee, Y. T.,
Wang, Y. S., Chen, Y. P., Tsai, C. L., Ma, M. H. M.,
Fang, C. C., Lai, F., Meischke, H. W., and Turner,
A. M. (2019). Using a smartwatch with real-time feed-
back improves the delivery of high-quality cardiopul-
monary resuscitation by healthcare professionals. Re-
suscitation, 140:16–22.
Medlineplus.gov (2021). Sudden Cardiac Arrest — Sudden
Cardiac Death — MedlinePlus.
Meinich-Bache, Ø., Engan, K., Birkenes, T. S., and Myk-
lebust, H. (2018). Real-time chest compression qual-
ity measurements by smartphone camera. Journal of
Healthcare Engineering, 2018.
Michiels, C., Clinckaert, C., Wauters, L., and Dewolf, P.
(2020). Phone cpr and barriers affecting life-saving
seconds. Acta Clinica Belgica: International Journal
of Clinical and Laboratory Medicine.
Murata, T., Fukushima, A., Harada, T., and Sasaki, M.
(2021). Social awareness from analysis of available
time for automated external defibrillators in a city.
2021 5th IEEE International Conference on Cybernet-
ics, pages 045–049.
Neves Briard, J., Grou-Boileau, F., El Bashtaly, A., Spe-
nard, C., de Champlain, F., and Homier, V. (2019).
Automated external defibrillator geolocalization with
a mobile application, verbal assistance or no assis-
tance: A pilot randomized simulation (aed g-map).
Prehospital Emergency Care, 23(3):420–429.
Ng, Q. X., Han, M. X., Lim, Y. L., and Arulanandam,
S. (2021). A systematic review and meta-analysis
of the implementation of high-performance cardiopul-
monary resuscitation on out-of-hospital cardiac arrest
outcomes. Journal of Clinical Medicine, 10(10):2098.
Nguyen, V. (2019). Time to delivery of an automated
external defibrillator (AED) using a drone to im-
prove out-of-hospital cardiac arrest (OHCA) mortal-
ity. core.ac.uk.
NIH (2022). Pubmed.
Nord, A., Svensson, L., Karlsson, T., Claesson, A., Herlitz,
J., and Nilsson, L. (2017). Increased survival from
out-of-hospital cardiac arrest when off duty medically
educated personnel perform cpr compared with lay-
men. Resuscitation, 120:88–94.
Perera, N., Ball, S., Birnie, T., Morgan, A., Riou, M.,
Whiteside, A., Perkins, G. D., Bray, J., Fatovich,
D. M., Cameron, P., Brink, D., Bailey, P., and Finn,
J. (2020). “sorry, what did you say?” communicating
defibrillator retrieval and use in ohca emergency calls.
Resuscitation, 156:182–189.
Perkins, G. D., Handley, A. J., Koster, R. W., Castr
´
en, M.,
Smyth, M. A., Olasveengen, T., Monsieurs, K. G.,
Raffay, V., Gr
¨
asner, J.-T., Wenzel, V., Ristagno, G.,
Soar, J., Bossaert, L. L., Caballero, A., Cassan, P.,
Granja, C., Sandroni, C., Zideman, D. A., Nolan, J. P.,
Maconochie, I., and Greif, R. (2015). European re-
suscitation council guidelines for resuscitation 2015.
Resuscitation, 95:81–99.
Pijls, R. W., Nelemans, P. J., Rahel, B. M., and Gorgels,
A. P. (2016). A text message alert system for trained
volunteers improves out-of-hospital cardiac arrest sur-
vival. Resuscitation, 105:182–187.
Plata, C., Stolz, M., Warnecke, T., Steinhauser, S., Hinkel-
bein, J., Wetsch, W. A., B
¨
ottiger, B. W., and Spel-
ten, O. (2019). Using a smartphone application (pock-
etcpr) to determine cpr quality in a bystander cpr sce-
nario — a manikin trial. Resuscitation, 137:87–93.
Rao, G., Choudhury, S., Lingras, P., Savage, D., and Mago,
V. (2020). Surf: identifying and allocating resources
during out-of-hospital cardiac arrest. BMC Medical
Informatics and Decision Making, 20(11):1–15.
Rao, G., Mago, V., Savage, D. W., and Beyer, R. (2019).
Identifying and allocating resources during out of hos-
pital cardiac arrest. Proceedings - 2019 IEEE Inter-
national Congress on Cybermatics: 12th IEEE In-
ternational Conference on Internet of Things, 15th
IEEE International Conference on Green Computing
and Communications, 12th IEEE International Con-
ference on Cyber, Physical and So, pages 959–966.
Rea, T., Kudenchuk, P. J., Sayre, M. R., Doll, A., and Eisen-
berg, M. (2021). Out of hospital cardiac arrest: Past,
A Survey on Technologies Used During out of Hospital Cardiac Arrest
487

present, and future. Resuscitation, 165(May):101–
109.
Research, C. I. o. H. (2019). Research program intended to
help canadians survive sudden cardiac arrest expands
to all 10 canadian provinces - CIHR.
Riou, M., Ball, S., O’Halloran, K. L., Whiteside, A.,
Williams, T. A., Finn, J., O’Halloran, K. L., White-
side, A., Williams, T. A., and Finn, J. (2018a). Hi-
jacking the dispatch protocol: When callers pre-empt
their reason-for-the-call in emergency calls about car-
diac arrest. Discourse Studies, 20(5):666–687.
Riou, M., Ball, S., Williams, T. A., Whiteside, A., Cameron,
P., Fatovich, D. M., Perkins, G. D., Smith, K., Bray,
J., Inoue, M., O’Halloran, K. L., Bailey, P., Brink, D.,
and Finn, J. (2018b). ‘she’s sort of breathing’: What
linguistic factors determine call-taker recognition of
agonal breathing in emergency calls for cardiac arrest?
Resuscitation, 122:92–98.
Riou, M., Ball, S., Williams, T. A., Whiteside, A.,
O’Halloran, K. L., Bray, J., Perkins, G. D., Smith,
K., Cameron, P., Fatovich, D. M., Inoue, M., Bailey,
P., Brink, D., and Finn, J. (2017). ‘tell me exactly
what’s happened’: When linguistic choices affect the
efficiency of emergency calls for cardiac arrest. Re-
suscitation, 117:58–65.
Sanfridsson, J., Sparrevik, J., Hollenberg, J., Nordberg,
P., Dj
¨
arv, T., Ringh, M., Svensson, L., Forsberg, S.,
Nord, A., Andersson-Hagiwara, M., and Claesson, A.
(2019). Drone delivery of an automated external de-
fibrillator - a mixed method simulation study of by-
stander experience. Scandinavian Journal of Trauma,
Resuscitation and Emergency Medicine, 27(1).
Sanko, S., Feng, S., Lane, C., and Eckstein, M. (2021).
Comparison of emergency medical dispatch systems
for performance of telecommunicator-assisted car-
diopulmonary resuscitation among 9-1-1 callers with
limited english proficiency. JAMA Network Open,
4(6).
Sanko, S., Kashani, S., Lane, C., and Eckstein, M.
(2020). Implementation of the los angeles tiered
dispatch system is associated with an increase
in telecommunicator-assisted cpr. Resuscitation,
155:74–81.
Scquizzato, T. (2018). Cardiac arrest detection through arti-
ficial intelligence-based surveillance camera: A work-
ing prototype. Resuscitation, 130:e114.
Sevil, H., Bastan, V., G
¨
ult
¨
urk, E., El Majzoub, I., and
G
¨
oksu, E. (2021). Effect of smartphone applications
on cardiopulmonary resuscitation quality metrics in a
mannequin study: A randomized trial. Turkish Jour-
nal of Emergency Medicine, 21(2):56–61.
Shirane, T. (2020). A systematic review of effectiveness of
automated external defibrillators delivered by drones.
Global Journal of Health Science, 12(12):101.
Smith, C. M., Griffiths, F., Fothergill, R. T., Vlaev, I.,
and Perkins, G. D. (2020). Identifying and over-
coming barriers to automated external defibrillator
use by goodsam volunteer first responders in out-of-
hospital cardiac arrest using the theoretical domains
framework and behaviour change wheel: A qualita-
tive study. BMJ Open, 10(3).
Sondergaard, K. B., Hansen, S. M., Pallisgaard, J. L., Gerds,
T. A., Wissenberg, M., Karlsson, L., Lippert, F. K.,
Gislason, G. H., Torp-Pedersen, C., and Folke, F.
(2018). Out-of-hospital cardiac arrest: Probability of
bystander defibrillation relative to distance to near-
est automated external defibrillator. Resuscitation,
124:138–144.
Srinivasan, S., Salerno, J., Hajari, H., Weiss, L. S., and Sal-
cido, D. D. (2017). Modeling a novel hypothetical use
of postal collection boxes as automated external defib-
rillator access points. Resuscitation, 120:26–30.
Stieglis, R., Zijlstra, J. A., Riedijk, F., Smeekes, M., van der
Worp, W. E., and Koster, R. W. (2020). Aed and text
message responders density in residential areas for
rapid response in out-of-hospital cardiac arrest. Re-
suscitation, 150:170–177.
Takahashi, H., Sagisaka, R., Natsume, Y., Tanaka, S.,
Takyu, H., and Tanaka, H. (2018). Does dispatcher-
assisted cpr generate the same outcomes as sponta-
neously delivered bystander cpr in japan? American
Journal of Emergency Medicine, 36(3):384–391.
Tanaka, S., Rodrigues, W., Sotir, S., Sagisaka, R., and
Tanaka, H. (2017). Cpr performance in the presence of
audiovisual feedback or football shoulder pads. BMJ
Open Sport and Exercise Medicine, 3(1).
Telec, W., Baszko, A., Da¸browski, M., Da¸browska, A., Sip,
M., Puslecki, M., Kłosiewicz, T., Potyrala, P., Jurczyk,
W., Maciejewski, A., Zalewski, R., Witt, M., Ladny,
J. R., and Szarpak, Ł. (2018). Automated external de-
fibrillator use in public places: A study of acquisition
time. Kardiologia Polska, 76(1):181–185.
Tsukigase, K., Takyu, H., Inoue, H., and Tanaka, H. (2019).
‘where and who” did deliver public access defibrilla-
tions for ohca in japan. Resuscitation, 142:e50–e51.
Valenzuela, T. D., Roe, D. J., Cretin, S., Spaite, D. W., and
Larsen, M. P. (1997). Estimating effectiveness of car-
diac arrest interventions. Circulation, 96(10):3308–
3313.
Van de Voorde, P., Gautama, S., Momont, A., Ionescu,
C. M., De Paepe, P., and Fraeyman, N. (2017). The
drone ambulance [A-UAS]: golden bullet or just a
blank? Resuscitation, 116:46–48.
Vaughan, N., John, N., and Rees, N. (2019). Cpr virtual
reality training simulator for schools. Proceedings -
2019 International Conference on Cyberworlds, CW
2019, pages 25–28.
White, A., Wah, W., Jalil, N., Lum, N., EKX, N., Kua,
P., and Ong, M. (2018). 11 Quality of bystander
CPR by lay first responders: training versus real-
world use of a novel CPR feedback device in singa-
pore. bmjopen.bmj.com.
White, A. E., Ng, H. X., Ng, W. Y., Ng, E. K. X., Fook-
Chong, S., Kua, P. H. J., and Ong, M. E. H. (2017).
Measuring the effectiveness of a novel cprcard
TM
feedback device during simulated chest compressions
by non-healthcare workers. Singapore Medical Jour-
nal, 58(7):438–445.
Zoll (2021). Real cpr help
R
: Quality technology to im-
prove cpr - zoll medical.
HEALTHINF 2023 - 16th International Conference on Health Informatics
488
