
LifeSeniorProfile: A Multisensor Dataset for Elderly Real-time Activity
Track
Maicon Diogo Much
a
, Julio Alexander Sieg
b
, Ayalon Angelo de Moraes Filho
c
,
Vanessa de Moura Bartoski
d
, Guilherme Schreiber
e
and C
´
esar Marcon
f
School of Technology, Pontifical Catholic University of Rio Grande do Sul, Porto Alegre, Brazil
Keywords:
Multisensor Dataset, Real-time Activity Tracking, Elderly Motion Data, Elderly Physiological Data.
Abstract:
Real-time tracking and detection of risky situations in the elderly, such as falls and sudden changes in vital
signs, requires reliable, continuous, and automated monitoring systems based on relevant information. Wire-
less biosensors provide a great opportunity to remotely detect and monitor hazardous situations, allowing for
a fast response in an emergency. Motion data is widely used to track daily activities. Physiological data can
also be used for this exact purpose. However, there is yet to be a database available in the field of research in
which the patient’s physiological and movement information were collected simultaneously, considering daily
activities and simulation of falls. This work presents a multisensor dataset for developing real-time tracking
systems for the daily activities of older people. The data sensed refer to movement, using a triaxial accelerom-
eter, and physiology, considering blood volume pulse, electrodermal activity, heart rate, inter-beat interval,
and skin temperature. We collected these data from ten volunteers while performing 36 daily activities in a
simulated environment.
1 INTRODUCTION
Monitoring, detecting, and classifying activities of
older people through non-invasive wearable systems
is an open research area due to the similarity be-
tween movement data sensed in daily activities and
risky situations, such as falls. Recently, many ma-
chine learning algorithms, especially those that ex-
plore deep layers of neural networks (Mauldin et al.,
2018) (Li et al., 2019) (Santos et al., 2019), have
tried to search for hidden details of motion data of
accelerometers, gyroscopes, barometers, and magne-
tometers to identify features that classical algorithms
cannot identify. Despite the promising results, even
these high-performance algorithms hardly reveal a
real risk, achieving a false positive rate close to zero.
Accelerometers are the most common motion sen-
sors used to identify human activities, providing real-
a
https://orcid.org/0000-0002-1760-907X
b
https://orcid.org/0000-0003-3966-9855
c
https://orcid.org/0000-0001-7044-1504
d
https://orcid.org/0000-0001-6365-9273
e
https://orcid.org/0000-0002-1037-4853
f
https://orcid.org/0000-0002-7811-7896
time relative acceleration in a given direction, which
varies according to available freedom degrees. In the
rest state, the accelerometers share quasi-static val-
ues, and at excessive motion, they provide an accel-
eration peak. This behavior is adequate to develop a
low-precision algorithm based on peak detection sig-
nals to detect fall situations and identify elderly risk
situations. On the one hand, this algorithm is ineffec-
tive since many risk-free activities also have the same
data signature. On the other hand, the foundation is
the same for many fall detection systems developed in
various research. Over the years, many studies have
tried to improve these results by adding different mo-
tion sensors, but this problem is still an open research
area.
Our primary motivation for this work is based on
the direct correlation between accidental falls and vi-
tal signs (Naschitz and Rosner, 2007); this correla-
tion is not explored in most of the research data avail-
able to develop systems that explore risk situations
for older people. Integrating vital signs with motion
signals offers a considerable advantage for identify-
ing, detecting, and classifying daily activities and fall
risks. However, this integration is rarely addressed
in the available works (Oliver and Healy, 2009) (Vas-
Much, M., Sieg, J., Moraes Filho, A., Bartoski, V., Schreiber, G. and Marcon, C.
LifeSeniorProfile: A Multisensor Dataset for Elderly Real-time Activity Track.
DOI: 10.5220/0011730000003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 5: HEALTHINF, pages 453-460
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
453

sallo et al., 2009).
This work provides a dataset of multisensory in-
formation, which includes, in addition to traditional
motion sensors, some physiological sensors collected
during activities of daily living and risky situations.
We designed this database to analyze changes in vital
signs caused by daily activities and falls. These data
enable us to explore the fusion of physiological and
motion data and classify all sensors based on their
importance in detecting daily activities and falls, al-
lowing us to give weight to each element sensed.
2 RELATED WORK
This section describes articles encompassing datasets
of wearable sensors employed to predict falls and
daily activities, and Table 1 emphasizes the main
points of the related articles concerning the work pre-
sented here. Table 1 lets us notice the main similari-
ties and differences between this work and the others
for comparison and elaboration of some conclusions.
The first comparison in the table can be made by
evaluating the position of the sensors on the partici-
pants’ bodies. While some related works seek to use
several sensors in different body positions, like (Casi-
lari et al., 2017) and (Saleh et al., 2021a), the LifeSe-
nior dataset seeks to use a single device located on the
participants’ wrists, which is the same strategy used
by (Garcia-Ceja et al., 2021) and (Bruno et al., 2014)
datasets. This strategy is based on the idea that the
wrist is a well-accepted place to create products that
can be used daily.
Another interesting point is related to the activities
identified in each dataset. Related works that bring
daily activities simulate them starting with a lack of
movement and then the activity to be considered. Dif-
ferently from that, the LifeSenior dataset brings the
idea of executing a specific activity/risk situation to
perform some daily activity/fall. The closest to this
approach is found in the (Saleh et al., 2021a) dataset,
where the fall activities are related to a previous daily
activity, which leads to the fall.
The LifeSenior dataset contains data for 36 daily
activities, including fall situations, which is the higher
number of activity and fall data in a single dataset
compared to related work. The closest to this quantity
is the sheer number of fall types found in the FallAllD
(Saleh et al., 2021a) dataset, the diversity of daily ac-
tivities brought in HMP (Bruno et al., 2014), and even
the fusion of falls and activities brought in UMAFall
dataset (Casilari et al., 2017).
Regarding the sensors used, most of the related
works use the accelerometer as the only or one of the
motion sensors, which is the same approach as the
LifeSenior dataset. Despite this, while (Saleh et al.,
2021a) and (Casilari et al., 2017) rely on commonly
used sensors such as the gyroscope and magnetome-
ter and the smartphone that appears in some cases,
the dataset proposed in this work is based on a few
different sensors: PPG, EDA and Skin Temperature.
These sensors are located in the same body position,
the wrist, and can bring information that was previ-
ously little considered or unknown in other works.
In addition, the authors believe that using data fusion
from these sensors can bring new and unexpected re-
sults in future work.
3 SENSORS
We developed this dataset to record natural and pro-
voked human actions, such as a fall, using several sen-
sors that enable us to gather information from mul-
tiple points of view about each human action. We
planned to include a triaxial accelerometer to detect
human movement and insert sensors of temperature,
electrodermal activity (EDA), and photoplethysmog-
raphy (PPG) to extract vital signs.
3.1 Motion Sensors
All datasets evaluated presented data on daily activ-
ities and falls collected through motion sensors, pri-
marily accelerometers. The main reason to focus on
motion sensors is that most activities usually vary sig-
nificantly in the sensing signal. For example, a fall is
registered by a sequence of peaks and valleys in an
accelerometer signal.
An accelerometer is an electromechanical device
that measures the change in velocity over time (Pic-
cinno et al., 2019). Acceleration measurements can
be static, such as the force of gravity, or dynamic,
caused by motion. In general, accelerometers trans-
late an external acceleration signal into a displace-
ment of their moving mass, called inertial mass. An
accelerometer reports a drop as an abrupt change
in values, represented by peaks and valleys (Bourke
et al., 2007); a graph generated by an accelerometer
during a fall shows the pre-fall, critical, and post-fall
phases. Within the critical phase, it is still possible to
identify the free fall, impact, and adjustment (Saleh
et al., 2021b).
On the one hand, the presence of a high peak of
acceleration followed by inactivity is a solid indicator
to detect falls; on the other hand, more information
is needed to avoid false alarms. For example, lying
on a bed satisfy this accelerator sequence, making a
HEALTHINF 2023 - 16th International Conference on Health Informatics
454
Table 1: Comparisons between the related articles and our work.
Dataset Participants Sensors Sensors body position Year Activities
FallAllD 15 1, 2, 3 Neck, Wrist, Waist 2021 a
HTAD 3 1, 5 Wrist 2020 b, c, d, e, f, g, h
ShimFall&ADL 35 1 Chest 2020 a, i, j, k, l, m
HMP 16 1 Wrist 2014 e, l, m, n, r, s, t, u, v, w, x
UMAFall 17 1, 2, 3, 4 Ankle, Waist, Wrist, Chest 2017 a, k, l, m, n, p, q, r
LifeSenior 10 1, 5, 6, 7 Wrist 2022 a, l, m, o, r, y, z
Sensors: 1 - Accelerometer, 2 - Gyroscope, 3 - Magnetometer, 4 - Smartphone, 5 - PPG, 6 - EDA, 7 - Skin temperature.
Activities: a - Fall, b - Mop floor, c - Sweep the floor, d - Type on a computer keyboard, e - Brush teeth, f - Wash hands,
g - Eat chips, h - Watch TV, i - Jumping, j - Lying Down, k - Bending/Picking up, l - Sitting/Standing to/from a chair, m
- Walking, n - Climbing Stairs Down/Up, o - Loss of Motor Balance, p - Hopping, q - Light Jogging, r - Lying down (and
getting up) on (from) a bed, s - Comb hair, t - Drink from a glass, u - Eat with fork and knife, v - Eat with a spoon, w - Pour
water in a glass, x - Use telephone, y - Standing, z - Crouching and coming back
fall detection system with exclusive use of this ap-
proach somewhat limited. Therefore, we structured
this dataset by collecting vital signs to analyze how
this information can compose with motion informa-
tion to decide about a daily activity or a fall.
3.2 Vital Signs Sensors
The temperature sensor enables us to identify body
changes that may indicate simple disorders, such as
a fever crisis, or more severe disorders that can com-
promise the functioning of vital organs. If the body
temperature exceeds 42ºC, the individual is at risk of
dying, as well as when the measured body tempera-
ture drops below 30ºC (Holtzclaw, 1993). The tem-
perature sensor, combined with a motion sensor, can
help to identify the cause of a fall or fainting.
Electrodermal activity (EDA) is the term used to
define autonomous changes in the electrical proper-
ties of the skin. For this reason, the EDA sensor works
by identifying electrical changes on the surface of the
skin, allowing the monitoring of episodes of stress,
anxiety, and the neurological state of an individual
since it is much more susceptible to human emotions
than just the analysis of heart rate (Blain et al., 2008).
The photoplethysmography (PPG) sensor uses an
optical technique to identify blood volume changes
in the microvascular tissue bed under the skin due to
the pulsatile nature of the circulatory system (Kamal
et al., 1989). The sensor system consists of a light
source and a detector with a red and infrared light-
emitting diode (LED). The PPG sensor monitors light
intensity changes through reflection or tissue trans-
mission (Tamura et al., 2014). Studies report that
through PPG, it is possible to non-invasively estimate
signals such as Electrocardiogram (ECG), heart pulse
rate, saturation (Kamal et al., 1989), respiratory rate
(Jarchi et al., 2018), and blood pressure (Kurylyak
et al., 2013).
4 DATASET
LifeSeniorProfile was developed to contribute to
world research in risk situation detection in older
people based on wearable device solutions. Some
datasets are available for research in this area, but
almost all are based only on motion sensors. We
propose a novel approach bringing up important vi-
tal signs correlated with motion data during simulated
daily living activities and risk situations. We use the
E4 wristband from Empatica (McCarthy et al., 2016),
a medical-grade and trustworthy device that provides
accurate real-time signals. Figure 1 displays the de-
vice with its sensors.
Figure 1: Front and back view of Empatica E4 device
biosensor (McCarthy et al., 2016).
In addition to the pioneering nature of the pro-
posed dataset in correlating vital signs with motion
sensors, the proposal to use a device that is already
widely clinically validated for use in research and is
also certified by several regulatory agencies in the
health area makes LifeSeniorProfile dataset unique.
4.1 Data Collection Process
Once the ethics committee of Group Conceic¸
˜
ao Hos-
pital approved our experimental protocol (number
5,431,965), we started to recruit volunteers that fit
LifeSeniorProfile: A Multisensor Dataset for Elderly Real-time Activity Track
455
the eligibility criteria. All the volunteers were re-
cruited around the research laboratory; the recruiter
explained all the study details to the volunteers before
accepting them to participate.
The volunteers placed a bracelet (collection de-
vice) on the right pulse to collect and identify the vi-
tal and motion signs. The movement characterization
and performance were accompanied by a physical
therapist who recorded the movement type for each
volunteer in each situation. These records, from the
physical therapist and the collection device, known as
the gold standard, are collected to be confronted later
and related to the clinical variables of each research
subject.
All movements were performed in an area covered
by 50cm x 50cm and 20mm thick EVA plates to ab-
sorb impacts and avoid discomfort. For the fall sim-
ulations, a mattress with a fall area of 3m x 2m and
30cm thick was additionally positioned.
The movement simulation step involves executing
a previous dynamic gait, successively followed by the
unbalance or fall movement. The following dynamic
gaits were simulated prior to each specific movement:
• Walking on a level surface at normal speed for 6
meters;
• Gait with vertical head movements; Up - Down -
Forward;
• Walk around the obstacle in the format of an eight;
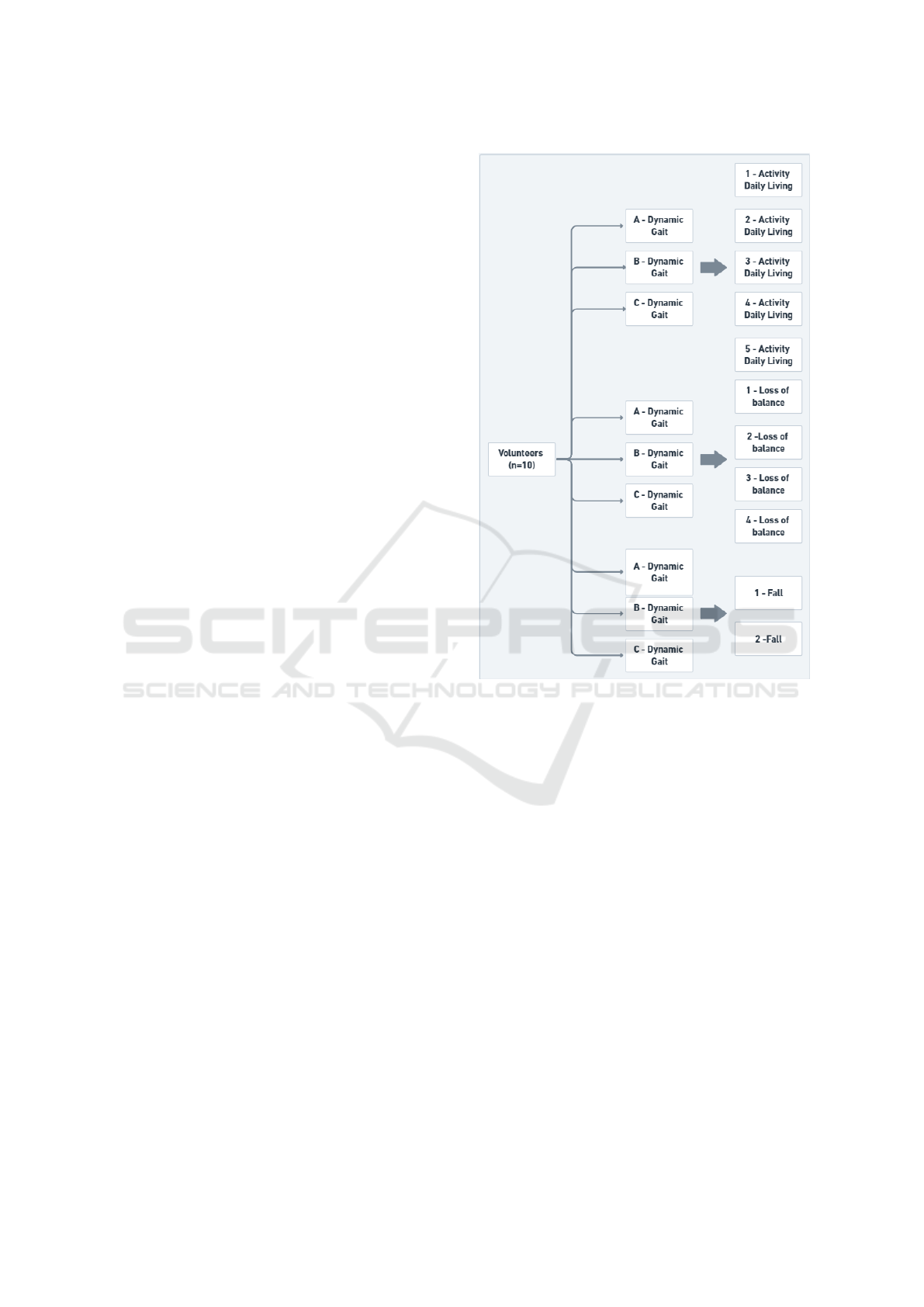
The study volunteers performed dynamic gait
prior to all movement simulations to be collected and
evaluated, including the performance of activities of
daily living (ADL), simulations of different causes of
imbalance, and simulations of different falls (Figure
2). These movements, which are described below,
were used in previous studies of drop detector wear-
ables to collect fall, non-fall, and near-fall signals
(Bourke and Lyons, 2008) (Aziz and Robinovitch,
2011):
Activity Daily Living
• Stopped - without movement;
• Walking straight for 10 meters;
• Standing up and sitting in the chair - Perform
the entire movement of sitting on a seat approx-
imately 50cm high, wait 30 seconds and get up
from the seat and stand up straight again;
• Squatting and coming back - Starting from the up-
right posture, the volunteer performs the squatting
movement until he/she rests on the heels, waits 30
seconds, and returns to the standing position;
• Lying down and getting up - the volunteer per-
forms the complete lying down movement with
Figure 2: Simulations of different causes of imbalance and
simulations of different falls.
the face-up on a bed approximately 40cm high,
waits 30 seconds, and gets out of bed, getting erect
again.
Loss of Balance
• Sitting and Standing - the volunteer completes
the entire movement of sitting on a seat approx-
imately 50cm high, waits 30 seconds, and when
standing up, simulates the loss of balance forward
and finishes the erect movement;
• Standing and sitting - the volunteer performs
the movement of sitting on a seat approximately
50cm high, simulating loss of balance due to in-
correct weight transfer to the seat and ending the
movement erect;
• Changing direction - Being initially stopped, per-
form a 180° change of direction and, in the end,
simulate the loss of balance to the side and finish
the erect movement;
• Reaching Object - Being initially stationary, the
volunteer moves to look for an object on the
HEALTHINF 2023 - 16th International Conference on Health Informatics
456

ground and, in the end, simulates the loss of for-
ward balance and finishes the upright movement.
Fall
• Obstacle - Initially walking, the volunteer sim-
ulates limb collision with an obstacle (10 cm x
15cm bulkhead) and then simulates the fall move-
ment on the mattress;
• Cadence continuity - Initially walking, the volun-
teer simulates the forward slip and then simulates
the movement of falling on the mattress;
• Syncope - Initially stopped, relax lower limbs to
simulate a fall on a mattress.
These movements were captured by the device
instrumentation, generating reference signals associ-
ated with these movement patterns, which allow train-
ing and validate different models of algorithms capa-
ble of characterizing movements and detecting falls.
4.2 Eligibility Criteria (Ethics
Committee)
Volunteers were selected following ethical principles
and with comprehensive selection criteria. Volunteers
are adults, without gender restriction, over 18 years
of age, and in total health; that is, volunteers who
presented at least one of the following characteristics
were considered unfit for the study: (i) neurological
diseases; (ii) gait disorders and musculoskeletal dis-
eases; (iii) uncorrected visual impairment; (iv) inabil-
ity to maintain orthostatism; (v) need and assistance
to get around; (vi) functional dependency; and (vii)
recent orthopedic trauma.
4.3 Characteristics of the Participants
The dataset consists of data from 10 volunteers with
an average age of 36 years; all of them meet the cri-
teria established in the 4.2 section, 60% male with
average weight and height of 85kg and 1.74m, re-
spectively. Regarding female volunteers, the average
weight and height were 72kg and 1.65m. Further in-
formation about the volunteers was preserved for con-
fidentiality reasons provided in the consent form for
participation in the research.
4.4 Experimental Protocol
We divided the experimental protocol into three
groups that simulate Daily Living Activities (DLA),
Loss of Motor Balance (LMB), and Effective Fall
(EF). In order to standardize the beginning of data col-
lection, we created three dynamic gaits: (i) on a flat
surface at normal speed for 6 meters, (ii) with vertical
head movements, and (iii) walking around an obstacle
in the shape of an 8. After performing these marches
for 30s, the collection of movements in the database
was started, as detailed in Table 2.
Altogether, we obtained 360 records identified
with the number of each individual, followed by the
initial simulation applied in the test, the type of gait,
and the effective simulation, according to the last col-
umn of Table 2.
4.4.1 Effect of Data Merging for Some Activities
The data collected by the E4 wristband is transmit-
ted to the Empatica platform and exported in CSV
(Comma-separated values) files to be manipulated in
spreadsheet and graphics software.
The sensors record data at different rates:
• Accelerometer - 32 points per second;
• PPG sensor - 64 points per second for blood vol-
ume and 1 point per second for heart rate;
• EDA sensor - 4 points per second;
• Temperature sensor - 4 points per second.
To analyze the inter-sensor correlation, we upsam-
pled the sensors with lower frequencies, using the lin-
ear interpolation method to normalize all data to 64Hz
(the highest frequency found among the sensors).
We used the accelerometer as a base sensor to
identify a volunteer’s movement, daily activities, loss
of balance, and fall. We looked for variations that
occurred in the other sensors at the points where the
events were identified on the accelerometer graph.
We noticed that the Blood Volume Parameter (BVP)
showed a strong correlation with the events recorded
by the accelerometer, as can be seen in Figure 3,
which shows the daily activity record, with gait and
vertical movements with the head, and getting up and
sitting down from the chair.
In this same record, when analyzing the normal-
ized data of heart rate, temperature, and electroder-
mal activity, large variations are not highlighted, ei-
ther null or very small, as shown in Figure 4. How-
ever, it is not possible to say that these signals are not
influenced by the movement of the volunteer, as it is
necessary to consider that they have a lower frequency
of records. What can be seen in Figure 4 is that the
Heart Rate (HR) has its records interrupted before the
end of the collection at the 6000 points of the graph.
These same characteristics, peaks in the ac-
celerometer and the synchronized blood volume sig-
nals, could be observed in the records of loss of bal-
ance activities and falls.
LifeSeniorProfile: A Multisensor Dataset for Elderly Real-time Activity Track
457
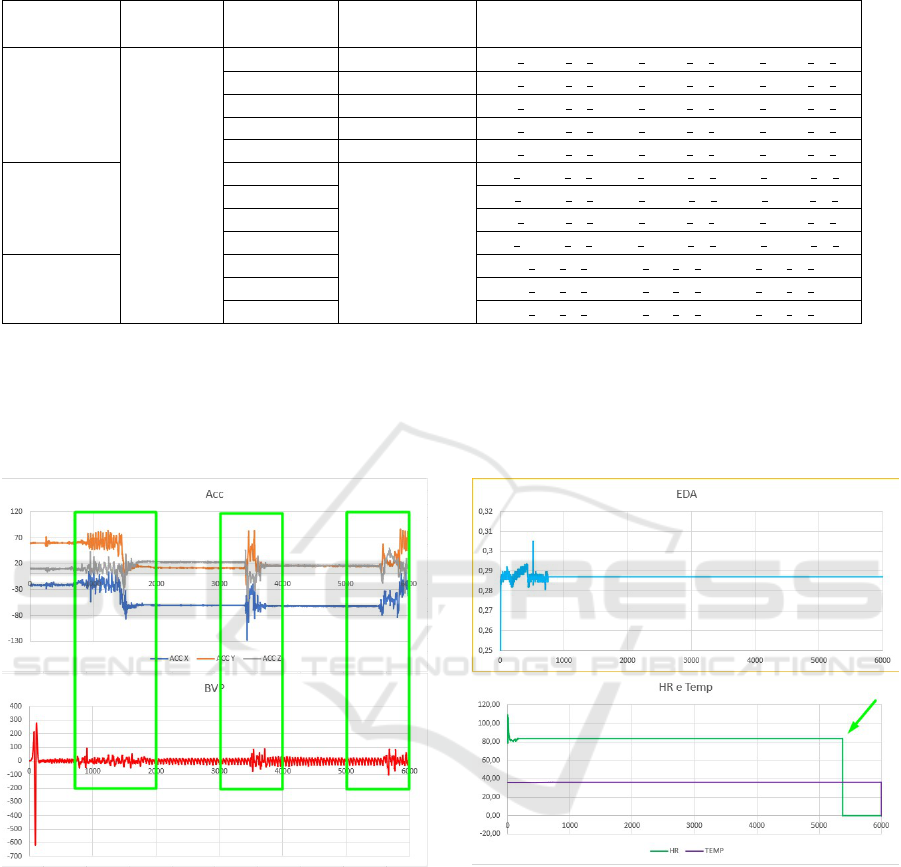
Table 2: Details of the movements present in the database.
Simulation
Dynamic
gait (30s)
Movement
simulation
Time
File name
DLA
A, D e G
1 10s V1 DLA A 1, V1 DLA D 1, V1 DLA G 1
2 The necessary V1 DLA A 2, V1 DLA D 2, V1 DLA G 2
3 2 repetitions V1 DLA A 3, V1 DLA D 3, V1 DLA G 3
4 2 repetitions V1 DLA A 4, V1 DLA D 4, V1 DLA G 4
5 2 repetitions V1 DLA A 5, V1 DLA D 5, V1 DLA G 5
LMB
6
The necessary
V1 LMB A 6, V1 LMB D 6, V1 LMB G 6
7 V1 LMB A 7, V1 LMB D 7, V1 DLA G 7
8 V1 DLA A 8, V1 DLA D 8, V1 DLA G 8
9 V1 LMB A 9, V1 LMB D 9, V1 LMB G 9
EF
10 V1 EF A 10, V1 EF D 10, V1 EF G 10
11 V1 EF A 11, V1 EF D 11, V1 EF G 11
12 V1 EF A 12, V1 EF D 12, V1 EF G 12
Simulation: DLA - Daily Living Activities, LMB - Loss of Motor Balance, EF - Effective Fall
Dynamic Walking: A - Walking on a flat surface at normal speed for 6 meters, D - Walking with vertical head movements:
Up – Down – Forward, G – Walking around an obstacle in figure eight.
Motion simulation: 1 – Standing, 2 – Walking, 3 – Standing up and sitting in the chair, 4 – Crouching and coming back, 5
– Lying down and standing up, 6 – Sitting down and standing up, 7 – From standing and sitting, 8 – Changing direction, 9 –
Reaching object, 10 – Obstacle, 11 – Cadence continuity, 12 – Syncope.
Figure 3: Accelerometer and PPG sensor signals.
The data collection of the Empatica platform pro-
vides a graphical view of the data with native lin-
ear interpolation for data normalization. This facility
enables us to verify the influence of the volunteer’s
movement also on the EDA and temperature sensors,
as shown in Figure 5 - recording a gait simulation
around obstacles in eight, followed by a fall simulat-
ing a syncope.
Figure 5 shows the last 10 seconds of the collec-
tion, where the accelerometer data are unified, with
no significant variation. However, the EDA sensor
and BVP variations are quite different. Nevertheless,
the temperature undergoes a small drop that slightly
Figure 4: Signals from heart rate (PPG) and EDA and tem-
perature sensors.
changes the graphic.
Machine learning algorithms see data raw without
the need for graphics. Thus, these slight variations in
the sensors and the accelerometer serve as points of
differentiation that can make a big difference in de-
ciding whether an event can be classified as a fall or
just a movement of an individual purposefully lower-
ing himself, for example.
HEALTHINF 2023 - 16th International Conference on Health Informatics
458

Figure 5: Signals of accelerometer, BVP, EDA, and temper-
ature sensors.
4.5 Dataset Characteristics
Each LifeSeniorProfile dataset file encompasses a dy-
namic gait simulation followed by a motion simu-
lation that can be a daily activity, loss of balance,
or a fall. Preceding the movement simulation with
a dynamic gait makes the collected data closer to a
real event, where some previous situation of normal-
ity will always precede a specific movement situation.
This procedure is another differential of the proposed
model concerning those currently available.
We separated data according to the sensor used
to perform the measurement; therefore, all participant
files were unified and separated by the sensors in the
wearable. To avoid losing the references present in
each simulation and to allow the individual analysis
of the curves, a “Label” file was created containing
the information of the last column of the previous ta-
ble. This process resulted in the following files:
• ACC-X.csv - Containing the accelerometer data
referring to the X axis;
• ACC-Y.csv - Containing the accelerometer data
referring to the Y axis;
• ACC-Z.csv - Containing the accelerometer data
referring to the Z axis;
• BVP.csv - Containing blood volume pulse data;
• EDA.csv - Containing electrodermal activity data;
• HR.csv - Containing heart rate values;
• TEMP.csv - Containing temperature data;
• LABEL.csv - Containing the characteristics of the
experimental protocol.
For convenience, the entire dataset was split into
the train and test sets. Seven subjects were included in
the train set and three in the test set. This procedure
helps develop algorithms that use the training set to
learn the characteristics, and the developed model is
not seen as data (test set).
4.6 Dataset Limitations
This dataset has some limitations that need to be taken
into consideration:
• Limited number of volunteers - as the number of
volunteers performing the simulated movements
is not higher than other datasets, the researcher
needs to consider specific algorithms; some in-
sights can be the product of a poor number of col-
lections and not from the algorithm performance.
• Age of volunteers - the average age of volun-
teers is lower than that of the elderly, generating a
loss of specific characteristics found only in older
adults. This choice prevents older adults from get-
ting injured, even with the falls being controlled
and assisted by a medical team.
5 CONCLUSION
Different methods of detection and monitoring of
daily activities performed by the human body have
already been developed and explored by numerous
scientific articles in the literature. Each method has
its peculiarities, but there is a consensus that motion
sensors are the ones that present the most acceptable
result within a feasible scenario in wearable devices.
Despite this good performance, these types of sensors
also present a high rate of false positives, like detect-
ing an activity that was not executed. This fact occurs
due to the motion signal characteristics that can be
easily confused with normal daily movements.
This article displays that the association of physi-
ological sensors to the usual movement provides rele-
vant information for reducing the number of false pos-
itive detections, given the evident correlation between
the different behavior of the vital signs in a real de-
tectable activity and a mistakenly detected one. This
dataset enables the researchers to explore in detail the
behavior associated with falls and daily living activi-
ties, thanks to a long time of data collection for each
simulated movement and the context available; there-
fore, providing a way to consider not only the exact
movement but also what occurred before and after
it. Algorithms that consider movement context, like
a fall, can find important information about the vital
sign status before the fall, what the user was doing be-
fore the fall, and also how is the motion characteristics
after the fall, enabling us to detect if it was senseless
or moving.
Our proposed dataset is an essential new tool to
improve the results of activity detector algorithms
based on non-invasive wearable sensors. It is now
LifeSeniorProfile: A Multisensor Dataset for Elderly Real-time Activity Track
459

available for new researchers and can be downloaded
at https://github.com/lifeseniorproject/profile.
For future work, we plan to collect more data from
users and include more older people, which was not
included in this article due to the difficulty of recruit-
ing them. Increasing this dataset enables us to use
deep learning algorithms.
ACKNOWLEDGMENT
This study was financed in part by the Coordina-
tion for the Improvement of Higher Education Per-
sonnel - Brazil (CAPES) - Finance Code 001, Na-
tional Council for Scientific and Technological Devel-
opment (CNPq) and Financier of Studies and Projects
(FINEP).
REFERENCES
Aziz, O. and Robinovitch, S. N. (2011). An analy-
sis of the accuracy of wearable sensors for classify-
ing the causes of falls in humans. IEEE transac-
tions on neural systems and rehabilitation engineer-
ing, 19(6):670–676.
Blain, S., Mihailidis, A., and Chau, T. (2008). Assessing
the potential of electrodermal activity as an alterna-
tive access pathway. Medical Engineering & Physics,
30(4):498–505.
Bourke, A., O’Brien, J., and Lyons, G. (2007). Evaluation
of a threshold-based tri-axial accelerometer fall detec-
tion algorithm. Gait & Posture, 26(2):194–199.
Bourke, A. K. and Lyons, G. M. (2008). A threshold-based
fall-detection algorithm using a bi-axial gyroscope
sensor. Medical engineering & physics, 30(1):84–90.
Bruno, B., Mastrogiovanni, F., and Sgorbissa, A. (2014). A
public domain dataset for adl recognition using wrist-
placed accelerometers. In The 23rd IEEE Interna-
tional Symposium on Robot and Human Interactive
Communication, pages 738–743.
Casilari, E., Santoyo-Ram
´
on, J. A., and Cano-Garc
´
ıa, J. M.
(2017). Umafall: A multisensor dataset for the re-
search on automatic fall detection. Procedia Com-
puter Science, 110:32–39. 14th International Con-
ference on Mobile Systems and Pervasive Computing
(MobiSPC 2017) / 12th International Conference on
Future Networks and Communications (FNC 2017) /
Affiliated Workshops.
Garcia-Ceja, E., Thambawita, V., Hicks, S. A., Jha, D.,
Jakobsen, P., Hammer, H. L., Halvorsen, P., and
Riegler, M. A. (2021). Htad: A home-tasks activities
dataset with wrist-accelerometer and audio features.
In Loko
ˇ
c, J., Skopal, T., Schoeffmann, K., Mezaris,
V., Li, X., Vrochidis, S., and Patras, I., editors, Multi-
Media Modeling, pages 196–205, Cham. Springer In-
ternational Publishing.
Holtzclaw, B. J. (1993). Monitoring body temperature. Ad-
vances in cardiac care limiting care, 4(1):44–55.
Jarchi, D., Salvi, D., Tarassenko, L., and Clifton, D. A.
(2018). Validation of instantaneous respiratory rate
using reflectance ppg from different body positions.
Sensors.
Kamal, A., Harness, J., Irving, G., and Mearns, A. (1989).
Skin photoplethysmography — a review. Computer
Methods and Programs in Biomedicine, 28(4):257–
269.
Kurylyak, Y., Lamonaca, F., and Grimaldi, D. (2013). A
neural network-based method for continuous blood
pressure estimation from a ppg signal. 2013 IEEE In-
ternational Instrumentation and Measurement Tech-
nology Conference (I2MTC), pages 280–283.
Li, H., Shrestha, A., Heidari, H., Le Kernec, J., and Fio-
ranelli, F. (2019). Bi-lstm network for multimodal
continuous human activity recognition and fall detec-
tion. IEEE Sensors Journal, 20(3):1191–1201.
Mauldin, T. R., Canby, M. E., Metsis, V., Ngu, A. H., and
Rivera, C. C. (2018). Smartfall: A smartwatch-based
fall detection system using deep learning. Sensors,
18(10):3363.
McCarthy, C., Pradhan, N., Redpath, C., and Adler, A.
(2016). Validation of the empatica e4 wristband. In
2016 IEEE EMBS international student conference
(ISC), pages 1–4. IEEE.
Naschitz, J. E. and Rosner, I. (2007). Orthostatic hypoten-
sion: framework of the syndrome. Postgraduate med-
ical journal, 83(983):568–574.
Oliver, D. and Healy, F. (2009). Falls risk prediction tools
for hospital inpatients: do they work? Nursing Times,
105(7):18–21.
Piccinno, A., Hemmatpour, M., Ferrero, R., Montrucchio,
B., and Rebaudengo, M. (2019). A review on fall pre-
diction and prevention system for personal devices:
Evaluation and experimental results. Advances in
Human-Computer Interaction.
Saleh, M., Abbas, M., and Le Jeann
`
es, R. B. (2021a). Fal-
lalld: An open dataset of human falls and activities
of daily living for classical and deep learning applica-
tions. IEEE Sensors Journal, 21(2):1849–1858.
Saleh, M., Abbas, M., Prudhomm, J., Somme, D., and
Le Bouquin Jeann
`
es, R. (2021b). A reliable fall de-
tection system based on analyzing the physical activ-
ities of older adults living in long-term care facilities.
IEEE Transactions on Neural Systems and Rehabili-
tation Engineering, PP:1–1.
Santos, G. L., Endo, P. T., Monteiro, K. H. d. C., Rocha, E.
d. S., Silva, I., and Lynn, T. (2019). Accelerometer-
based human fall detection using convolutional neural
networks. Sensors, 19(7):1644.
Tamura, T., Maeda, Y., Sekine, M., and Yoshida, M. (2014).
Wearable photoplethysmographic sensors—past and
present. Electronics, 3(2):282–302.
Vassallo, M., Mallela, S. K., Williams, A., Kwan, J., Allen,
S., and Sharma, J. C. (2009). Fall risk factors in el-
derly patients with cognitive impairment on rehabili-
tation wards. Geriatrics & gerontology international,
9(1):41–46.
HEALTHINF 2023 - 16th International Conference on Health Informatics
460
