
Monitoring of Vital Signs in the Home Environment: A Review of
Current Technologies and Solutions
Nerea Arandia
1 a
, Jose Ignacio Garate
2 b
and Jon Mabe
1 c
1
TEKNIKER, Basque Research and Technology Alliance (BRTA), 20600 Eibar, Spain
2
Department of Electronics Technology, University of the Basque Country (UPV/EHU), 48080 Bilbao, Spain
Keywords:
Monitoring, Vital Signs, Wearable, Medical Device, Sensors.
Abstract:
Vital signs measurement is key for monitoring and controlling the health of patients in the home environment.
Parameters such as body temperature, heart rate, blood pressure, respiratory rate, oxygen saturation or blood
glucose reflect the state of essential functions of the human body. Deviations of some of these parameters
may indicate illness or worsening of the patient’s condition. Nowadays there are different devices that allow
the measurement of the main vital signs, in this article the measurement technologies as well as the main
medical devices are reviewed. Many of these devices are not suitable for simultaneous monitoring of several
vital signs so the patient is required to handle a multitude of devices. Therefore, a review of new monitoring
device concepts that combine more than one vital sign and do not interfere with the day-to-day life of patients
is carried out.
1 INTRODUCTION
This article aims to review the current state of sensori-
sation and monitoring technologies used in biomedi-
cal applications for the diagnosis and treatment of pa-
tients at home. To this end, firstly, the monitoring
of the patient’s vital signs has been addressed. Then,
the monitored physiological characteristics have been
defined and the technologies and medical equipment
established or likely to be used in their measure-
ment/monitoring have been summarised.
This review has shown how advances in micro-
electronics, communications, sensors and data pro-
cessing have led to the development of wearable sen-
sors for monitoring, both at research and commer-
cial levels. Despite this, there are still challenges of
adapted functionality and usability to bring together
in a single device all the parameters for comprehen-
sive care, such as the need for multiple sensors in dif-
ferent areas of the body or accuracy limitations for
healthcare use.
In this sense, existing commercial developments
have been presented and the advantages and limita-
tions of their operation have been shown. Finally, a
review of portable developments in the literature for
monitoring vital signs at home has been made.
a
https://orcid.org/0000-0003-2679-8068
b
https://orcid.org/0000-0003-0343-6320
c
https://orcid.org/0000-0002-0211-842X
2 MONITORING OF VITAL
SIGNS
Monitoring systems aim to obtain continuous infor-
mation on the state of a patient to enable diagnosis
and treatment. Theses systems can be use in a home
context to achieve detailed characterization of the pa-
tient status. Typically, the indicators measured for this
are vital signs.
Vital signs are a series of parameters that show
body’s most basic functions such as the haemody-
namic status of a patient. They reflect the state of the
organism and are the first sign of alarm in the event
of a malfunction or defect in the organism. There are
four main vital signs that physicians and other health
professionals routinely examine in clinical practice
(Rose and Clarke, 2010), (Lockwood et al., 2004):
body temperature, heart rate, blood pressure and res-
piratory rate.
In this context, two groups of potential patient
monitoring solutions can be identified. On the one
hand, there are non-intrusive sensing solutions in the
patient’s home environment. On the other hand, so-
lutions based on highly portable devices, wearables.
Currently, technology allows the integration of sev-
eral sensors together with the information processing
units, which makes it possible to build very compact
and accurate wearables.
In an ageing society with the increasing preva-
lence of chronic diseases such as neurological dis-
108
Arandia, N., Garate, J. and Mabe, J.
Monitoring of Vital Signs in the Home Environment: A Review of Current Technologies and Solutions.
DOI: 10.5220/0011646700003414
In Proceedings of the 16th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2023) - Volume 1: BIODEVICES, pages 108-115
ISBN: 978-989-758-631-6; ISSN: 2184-4305
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
eases, cardiovascular diseases, diabetes, respiratory
disorders. . . the demand for continuous monitoring
will lead to a growing sector of wearable devices.
This will provide greater patient comfort and more
meaningful data to perform diagnostics. As an indica-
tion of the financial size of the wearable health mar-
ket, in the US it accounted for spending in the years
2017, 2018 and 2019 of $7 billion, $10 billion and
$25 billion, respectively. In other words, spending
has almost quadrupled in two years (Fortune Business
Insights, 2020).
2.1 Body Temperature
Body temperature is a measure of the body’s ability to
generate and eliminate heat. Depending on where it
is measured, three types of temperature can be distin-
guished. Core body temperature, when measured rec-
tally, orally or tympanically. Proximal skin tempera-
ture if taken near the central axis of the body such as
the groin or armpit. And distal skin temperature when
measured in the regions furthest from the central axis
of the body, typically the hands and legs.
Depending on the place where the measurement
is taken, different results are obtained. Likewise, as-
pects such as stress can vary body temperature. In
(Vinkers et al., 2013), the author states that stress
causes a decrease in body and distal temperature, but
an increase in proximal temperature. Likewise, (Coif-
fard et al., 2021) shows how the body temperature
presents a circadian rhythm, increasing its value dur-
ing the day and decreasing during the night. In addi-
tion, age, sex of the patient or different diseases can
also affect the measurement. In Alzheimer’s patients
the core body temperature rises by up to 0.2 degrees
Celsius (Sixsmith et al., 2005). A rise in body tem-
perature is the first symptom of infection or inflam-
mation somewhere in the body. When the proximal
skin temperature value is below 35.8ºC, it is called
hypothermia. If the value is high, it is called febrile
(up to 37.5ºC) or fever (above 38ºC) (Marion, 2003).
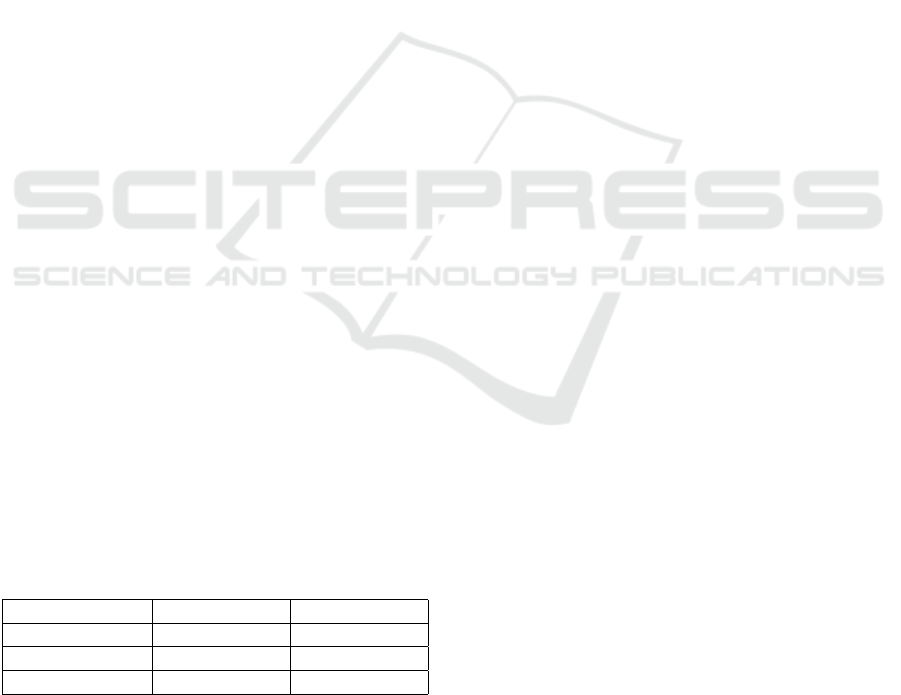
Table 1: Normal body temperature ranges according to
reading type and gender.
Type of reading Female Male
Oral 33,2 – 38,1 ºC 35,7 – 37,7 ºC
Rectal 36,8 – 37,1 ºC 36,7 – 37,5 ºC
Tympanic 35,7 – 37,8 ºC 35,5 – 37,8 ºC
2.2 Pulse or Heart Rate
It refers to the number of heart beats or contractions
per minute. It can change throughout the day or in a
given situation. However, it is quickly reversed in the
event of a specific triggering situation. The standard
values are considered between 60 and 100 beats per
minute (bpm). Tachycardia is defined as a state when
the heartbeat is greater than 100 bpm and bradycardia
when it is less than 60 bpm. The heartbeat is also sub-
jected to natural variations that show how our nervous
system adapts to sudden challenges (Spodick et al.,
1992).
2.3 Blood Pressure
Blood pressure is the force applied against the walls
of the arteries when the heart pumps blood through
the body. It is a parameter that can change through-
out the day. It is measured in millimetres of mer-
cury (mmHg). Two different blood pressure values
can be distinguished, Systolic blood pressure (SBP)
and Diastolic blood pressure (DBT). SBP reflects the
pressure in blood vessels when heart contracts (stan-
dard values between 110 and 140 mmHg). DBT is
the pressure of the blood on the walls of the arteries
when the heart rests between beats (standard values
are between 70 and 90 mmHg). A patient is said to be
hypertensive when their SBP is above 140 mmHg and
their DBT is above 90 mmHg (Organization, 2022).
2.4 Respiratory Rate
It quantifies the number of breaths taken in a specified
period of time, usually one minute. In adults, 12 to
20 breaths per minute is considered a standard value.
When the value is higher, the patient has lack of oxy-
gen, this status is called tachypnoea. If it is less, it is
bradypnea (Lovett et al., 2005).
2.5 Non-Universal Vital Signs
Several additional vital signs have been proposed, al-
though they have not been officially or universally
adopted. These additional parameters include the
oxygen saturation and blood glucose.
2.5.1 Oxygen Saturation
Oxygen saturation, reflects the amount of oxygen
available in the blood; a critical parameter in patients
with respiratory pathology. The standard oxygen sat-
uration value is between 95% and 100% and indicates
that cells are receiving enough oxygen to preserve
their function. A saturation value below 90%, called
hypoxaemia, is considered insufficient and is mani-
fested by shortness of breath and a compensatory in-
crease in respiratory rate. Values below 80% are con-
sidered severe hypoxaemias (Subhi et al., 2009).
Monitoring of Vital Signs in the Home Environment: A Review of Current Technologies and Solutions
109

2.5.2 Blood Glucose
The sugar ingested with food is converted by
metabolism into glucose, which travels through the
bloodstream to reach cells of different tissue types
providing the energy they need to function. Blood
glucose levels, clinically referred to as blood glucose,
vary throughout the day. When insulin metabolism is
not working properly, glucose is no longer properly
assimilated by tissue cells, and it is accumulated in
the blood. The standard value of glucose before eat-
ing are between 70 - 100 mg/dl (Gunst and Van den
Berghe, 2010).
3 MEASUREMENT
TECHNOLOGIES AND
PRINCIPLES
This section reviews the specific medical technologies
and equipment already established for the measure-
ment of vital signs. Although in certain cases there
may be variants based on more precise methods, this
summary prioritises those devices that can carry out
the measurement in a automated non-invasive way.
3.1 Clinical Thermometers
They are used to measure body temperature. There is
a wide variety, and they can be classified according
to the area of the body where they are designed to
measure (oral, axillary, rectal, tympanic or temporal)
or the type of technology on which they are based.
In terms of technology they use, the most common
clinical thermometers are those based on liquid, liquid
crystal, electronic contact and infrared.
3.1.1 Liquid Thermometers
Liquid thermometers are based on the thermal expan-
sion of a liquid inside a graduated glass tube. The
traditional solution used mercury, although it is no
longer used due to its toxicity. Now, coloured alcohol
or gallium is used as an alternative. Due to their op-
eration principle, it is necessary to wait for about 3 to
10 minutes (depending on the area of the body) so that
the device can perform a reliable measurement. They
are commonly used for measurements in the armpit,
mouth or rectum. Due to their fragility, measurement
time and the ban on mercury variants, their use has
been largely displaced by digital alternatives, espe-
cially outside the hospital environment.
In addition, there are liquid crystal thermometers,
It consists of heat-sensitive liquid crystals that are
integrated in a plastic strip. These crystals change
their colour to indicate different temperatures. They
are usually placed on the forehead and are disposable
(Rodr
´
ıguez et al., 2008).
3.1.2 Electronic Contact Thermometers
They are made up of temperature dependent transduc-
ers that vary the output voltage depending on the tem-
perature of the patient. This voltage variation is trans-
lated into degrees and displayed on a small screen.
Some of their advantages are that they are easy to read
and quick to respond, so their use has spread both in-
side and outside the hospital setting. Many of them
employ predictive algorithms to provide a reading in
a few seconds rather than a minute. They are com-
monly used for measurement in the armpit, mouth,
rectum or ear. In the case of predictive devices, the
algorithms used must take into account the area of
placement in order to provide an accurate temperature
reading (Habibian et al., 2009).
3.1.3 Infrared Thermometers
They do not require physical contact to carry out the
measurement and it is usually performed on the fore-
head, although there are specific developments for ear
measurements. As they do not require contact, they
can reduce the risk of infection transmission. Mea-
surement times are low, in the order of seconds. As
these devices are based on optical sensors, readings
can be affected by the state of the surface on which
the measurement is made (cleanliness, humidity, po-
sition, movement, etc.). Also, the level of ambient
light, external heat sources or the use of clothing or
cosmetic products can vary the measurement. There-
fore, it is more prone to measurement errors than con-
tact alternatives (Khan et al., 2021).
3.2 Heart Rate Monitor
Heart rate monitor allows real-time measurement of
a patient’s heart rate. Modern wearable devices typi-
cally use electrocardiography or photoplethysmogra-
phy method to record heart rate signals.
3.2.1 Electrocardiograph
Electrocardiograph or ECG electrical can record the
electrical activity of the heart. That is, the bio-
potential generated by the electrical signals that con-
trol the expansion and contraction of the heart. In
other words, it captures, records, and magnifies the
electrical activity of the heart. Different types of
ECGs can be distinguished according to the number
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
110

of used electrodes: 1, 2, 6 or 12 leads or channels,
where each lead will measure the electrical potential
difference between two electrodes. A 1-lead ECG
provides only basic monitoring of the heart. In con-
trast, a 12-lead ECG provides a complete picture of
cardiac activity. ECG is widely used to detect almost
any cardiac pathology (Bansal and Joshi, 2018).
There are different algorithms to extract the pulse
from the ECG. The basis of this measurement is the
detection of QRS complex. This parameter is formed
by three vectors: the Q wave, the first wave of the
complex with negative values; the R wave, which
follows the Q wave, is positive and the largest one;
and finally, the S wave, any negative wave that fol-
lows the R wave. Based on the duration, amplitude
and shape of QRS complex it is possible to detect
heart rate, arrhythmia, infarcts and other disorders.
In (Parak and Havlik, 2011) authors discuss differ-
ent algorithms and methods of heart rate frequency
estimation based on auto-correlation of energy signal,
thresholding of energy signal and peak detection in
energy signal envelope.
3.2.2 Photoplethysmography
Photoplethysmography or PPG optical determines the
heart rate using a light source of a specific length that
emits a beam on the skin to illuminate the subcuta-
neous vessels. The subcutaneous vessels reflect part
of the beam depending on the amount of red blood
cells they contain. (Saquib et al., 2015) The reflected
light hits on a photosensor which converts it into an
equivalent voltage. The cardiac cycle can be obtained
by measuring the interval between each voltage peak.
Its principle of operation is the same as that of the
oximeter, hence there are pulse oximeters that offer
both measurements.
3.3 Blood Pressure Monitor
It is a medical device used for indirect measurement
of blood pressure through SBP and DBT values. It
consists of a manometer and a cuff that is inflated un-
til it squeezes the measurement area so that, by occlu-
sion, the transit of blood is temporarily stopped for
measurement. It is used in conjunction with a stetho-
scope to auscultate the audible intervals of the Ko-
rotkoff arterial sounds while the cuff is being deflated
in a controlled manner.
For home use the digital ones are the most ap-
propriate as the whole process to be automatic, in-
cluding inflation. However, they require periodic cal-
ibration as they use sensors placed in the cuff to de-
tect Korotkoff sounds (Babbs, 2015). These sensors
can be auscultatory or oscillometric. The auscultation
is based on microphones capable of interpreting the
sounds of the measurement process (Beevers et al.,
2001). The Oscillometer relies on deformable mem-
branes whose variation in piezo-resistance or capaci-
tance allows the analysis of the vibration transmission
of the arterial wall (Mostafa et al., 2021). Most ven-
dors use the oscillometric procedure, displacing the
auscultatory procedure, which makes these devices
particularly suitable for noisy environments.
3.4 Respiratory Rate Monitor
Respiratory rate is usually measured manually by ob-
servation, palpation or using a stethoscope. There is,
however, equipment for automatic monitoring. For
example, fibre optic sensors can be used during Mag-
netic Resonance Imaging (MRI) scans to monitor res-
piratory rate (Nedoma et al., 2018).
3.4.1 Respiratory Inductance Plethysmography
This is a device that records respiratory movements
using an inflatable coil that surrounds the thorax.
These signals are connected to a monitoring device
that transforms the inductance of these coils into sig-
nals relative to the rib cabe and abdomen strains (Mas-
saroni et al., 2021). This measurement technique is
widely used in the hospital environment.
3.4.2 Impedance Pneumography
Another technique is based on impedance pneumog-
raphy. This is done by using 2 or 4 electrodes on the
thorax. A high-frequency, low-amplitude current is
flowed through the chest cavity and the variation in
resistance is used to estimate respiratory rate (Charl-
ton et al., 2021). The variation in resistance is due to
the impedance of the body and its respiratory cycle.
3.4.3 Spirometry
By using spirometers it is also possible to record the
amount of inhaled and exhaled air during a certain
time. Modern spirometers are able to graphically rep-
resent these curves. Based on a test of at least 60 sec-
onds, it is possible to measure the breathing rate. To
do this, it is sufficient to count the number of peaks
or troughs that are represented on the breathing graph
(Miller et al., 2005).
3.4.4 Capnography
Capnography is used to measure the concentration of
carbon dioxide in the airway of a patient during the
respiratory cycle. From the time evolution of this con-
centration, it is possible to determine the value of the
Monitoring of Vital Signs in the Home Environment: A Review of Current Technologies and Solutions
111

respiratory rate. Their operation is generally based on
the principle of absorption of infrared light by carbon
dioxide (Bergese et al., 2017).
3.5 Pulse Oximeter
This is a medical device that can determine the per-
centage of oxygen saturation of haemoglobin us-
ing photoelectric methods in a non-intrusive man-
ner. The pulse oximeter is placed on a part of
the body that is relatively translucent and has good
blood flow: the fingers, toes, earlobe or wrist.
The equipment emits light at specific wavelengths
(green/red/infrared) which pass sequentially from an
emitter to a photodetector through the patient (Moc¸o
and Verkruysse, 2021). The absorbance of each wave-
length caused by arterial blood (pulsatile component)
is measured, excluding venous blood, skin, bone,
muscle, fat. With this data it is possible to calculate
the blood oxygen saturation.
3.6 Glucometer
It is a device in which a test strip impregnated with a
drop of blood. It provides the result of the patient’s
blood glucose levels automatically in just a few sec-
onds and its use is not complex for the patient him-
self. However, it is an invasive method (Wang, 2008).
As an alternative, there are developments aimed at
achieving continuous monitoring of glucose concen-
tration, usually in interstitial or tissue fluid (McKinlay
et al., 2017).
4 MULTI-MONITORING
SOLUTIONS
The current scenario of technology applied to health
services does not free us from a series of challenges
that arise when considering the possibility, and even
the need, to use technologies suitable for home use.
The technologies required for this are evolving and
are making remarkable advances, such as develop-
ments in micro and nano electronics and SoC (System
on Chip) integration. As these developments are pro-
grammable and have a large memory capacity, they
have created the basis for very small systems with var-
ious integrated sensors and a large information pro-
cessing capacity. This, together with the constant
evolution in the field of electronic communications,
makes it possible for these systems to be connected to
distant information repositories, or even to be inter-
connected with each other.
This scenario is perfectly compatible with the in-
troduction and use of highly portable, increasingly
usable and interconnected devices in the field of
health and personal care. These principles tie in with
concepts that are at the epicentre of the evolution:
eHealth, Internet of Things (IoT) and its combina-
tion IomT (Internet of Medical Things) (Sudana and
Emanuel, 2019).
Thus, advances in microelectronics, communica-
tions, sensors and data processing have made possible
a great scope in the development of new technologies
and devices to support healthcare. Wearable sensor
devices for monitoring are an example of these ad-
vances (Li et al., 2018). There are a large number of
wearable devices that, due to their design and built-
in sensors, are functionally adapted to obtain health-
related information from non-hospital settings. They
can enable continuous monitoring of parameters such
as body temperature, position or bio-electrical signals
(Garc
´
ıa et al., 2019).
However, the development of wearable devices,
with high usability and medical use, still offer a num-
ber of challenges. Despite major developments, it is
still not possible to bring together in a single device
the ability to monitor all the parameters necessary for
comprehensive care. The proper placement of the
sensors, as part of the wearables, is a critical point
for the correct functioning and obtaining the measure-
ment of the corresponding vital sign.
There is a wide variety of systems proposed in the
literature for monitoring patients’ vital signs at home
(Lin et al., 2017), (Rashidi and Mihailidis, 2013).
However, many of these monitoring systems are de-
signed to monitor one or two specific parameters only
(Shivakumar and Sasikala, 2014). Among the multi-
measurement systems, the most important ones in-
clude smartwatch-based systems, smart furniture, and
textiles with integrated sensors.
4.1 Smartwatches
The role played by smartwatches and their use should
also be mentioned. Some of them, at the high
end of the price range, are starting to offer quite
advanced monitoring of health parameters, includ-
ing ECG-correlated measurements. However, these
smartwatches must be certified as medical devices to
be used for this intended use. The regulatory barrier
limits their availability in certain markets.
A representative example is the Apple Watch, the
first smartwatch approved by the US Food and Drug
Administration (FDA) for the incorporation of algo-
rithms for detecting atrial fibrillation and performing
ECGs (Isakadze and Martin, 2020). A similar autho-
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
112

risation was granted by the European Commission in
2019 for 19 countries. For this purpose, the watch
incorporates electrodes on its back and crown. Plac-
ing a finger on the crown closes the circuit with the
back electrodes providing data to the ECG applica-
tion. A measurement takes about 30 seconds and of-
fers the option of four possible results: sinus rhythm,
atrial fibrillation, high or low heart rate or inconclu-
sive. However, it is necessary to remark the limita-
tions of the Apple Watch’s single-lead system com-
pared to a traditional holter, a small electronic device
that records and stores the patient’s electrocardiogram
for at least 24 hours on an ambulatory basis (De As-
mundis et al., 2014). This limitation makes the Apple
smartwatch unable to detect heart attacks, cardiovas-
cular accidents or other heart conditions.
In the case of other vital signs, the technology
available for wearables is still far from the healthcare
related purposes. For example, several smartwatch
manufacturers such as Apple, Samsung or Amazfit
are planning to incorporate in their products the pos-
sibility of estimate blood pressure using different al-
gorithms. This is possible due to the optical sensors
that watches incorporate for heart rate measurement.
As with the Apple Watch ECG, such capabilities re-
quire the approval of specific regulatory affairs. In
terms of blood pressure monitoring, the Omron Heart-
guide wristband (Liang and Chapa-Martell, 2021), is
the only smartwatch with FDA clearance. This device
is an ultra-portable wrist sphygmomanometer.
Likewise, there are more and more references in
which different smartbands or smartwatches are used
to estimate body temperature. For example, (Kwak
et al., 2019) presents a statistical approach to estimate
body temperature based on skin temperature mea-
sured with a smartband.
4.2 Smart Furniture
Smart beds or chairs equipped with vital signs sen-
sors, can also be an interesting option for non-
intrusive monitoring of various vital signs.
In (Popescu and Mahnot, 2012) a set of pneumatic
sensors placed on a bed is presented to carry out heart
rate and respiratory rate measurements. In (Klack
et al., 2011), temperature measurement is carried out
using a high-precision IR camera. (Grace et al., 2017)
use different types of external sensors to measure res-
piratory rate in bed by integrating accelerometers in
the blanket, heart rate while sitting or standing using
electrodes on the floor in contact with the feet. The
use of a ballistocardiograph using pressure sensors in-
stalled on chairs or on the bed to estimate blood pres-
sure is also tested.
4.3 Textiles with Sensors
Another alternative is to incorporate monitoring ca-
pabilities into everyday items or accessories that the
patient carries with them on a regular basis, such as
socks, shoes, T-shirts, waistcoats, wristbands (Avgeri-
nakis et al., 2013)... One example is the Smart Vest,
a wearable monitoring system for parameters such as
heart rate, blood pressure, axillary temperature and
ECG (Pandian et al., 2008). There are other exper-
imental designs with promising preliminary results
that incorporate measurement capabilities (heart rate,
respiratory rate) into conventional T-shirts rather than
more bulky garments (Sardini and Serpelloni, 2014).
(Pigini et al., 2017) describe the pilot development
of a commercial home telemonitoring system. The
system is capable of performing ECG measurements
(1-lead) by means of a smart patch that can be placed
as a stand-alone sticker on the chest or can be inte-
grated into a garment or an elastic band. The sys-
tem also employs a commercial multi-purpose non-
wearable device to measure several constants: Heart
rate, blood pressure, and blood oxygen saturation.
The same system also performs a glycaemia measure-
ment.
(Pham et al., 2016) describe a system that uses a
smart garment with ECG textile electrodes and a chest
strap to measure respiration using an inductive trans-
ducer that measures changes in chest or abdominal
circumference.
An example of a commercial development of a
wearable for vital signs monitoring is the Hexoskin
smart garment (Villar et al., 2015). It is an elastic T-
shirt that provides, among other data, continuous in-
formation on heart and lung activity: ECG (1-lead),
heart rate, heart rhythm, breathing rate, etc. Another
example is the Philips wearable biosensor (Li et al.,
2019) in the form of a patch with, among other things,
a temperature sensor (thermistor) and ECG (1-lead).
5 CONCLUSIONS
This article reviews vital signs, measurement tech-
nologies and principles, and monitoring systems. The
review shows the limited number of wearable devices
that can be considered medical devices and highlights
their drawbacks for diagnosis. That is, wearables that
have been certified according to medical device regu-
lations. There is also a lack of wearables capable of
simultaneously monitoring several vital signs at home
environment.
Monitoring of Vital Signs in the Home Environment: A Review of Current Technologies and Solutions
113

ACKNOWLEDGEMENTS
Activity developed within the framework of the
IBERUS project. Technological Network of Biomed-
ical Engineering applied to degenerative patholo-
gies of the neuromusculoskeletal system in clinical
and outpatient settings (CER-20211003), CERVERA
Network financed by the Spain Ministry of Science
and Innovation through the Center for Industrial Tech-
nological Development (CDTI).
REFERENCES
Avgerinakis, K., Briassouli, A., and Kompatsiaris, I. (2013).
Recognition of activities of daily living for smart
home environments. Proceedings - 9th International
Conference on Intelligent Environments, IE 2013,
pages 173–180.
Babbs, C. F. (2015). The origin of Korotkoff sounds and
the accuracy of auscultatory blood pressure measure-
ments. Journal of the American Society of Hyperten-
sion, 9(12):935–950.e3.
Bansal, A. and Joshi, R. (2018). Portable out-of-hospital
electrocardiography: A review of current technolo-
gies. Journal of arrhythmia, 34(2):129–138.
Beevers, G., Lip, G. Y., and O’brien, E. (2001). Blood pres-
sure measurement. BMJ, 322(7293):1043–1047.
Bergese, S. D., Mestek, M. L., Kelley, S. D., McIntyre,
R., Uribe, A. A., Sethi, R., Watson, J. N., and Addi-
son, P. S. (2017). Multicenter Study Validating Ac-
curacy of a Continuous Respiratory Rate Measure-
ment Derived From Pulse Oximetry: A Compari-
son With Capnography. Anesthesia and Analgesia,
124(4):1153.
Charlton, P. H., Bonnici, T., Tarassenko, L., Clifton, D. A.,
Beale, R., Watkinson, P. J., and Alastruey, J. (2021).
An impedance pneumography signal quality index:
Design, assessment and application to respiratory rate
monitoring. Biomedical Signal Processing and Con-
trol, 65:102339.
Coiffard, B., Diallo, A. B., Mezouar, S., Leone, M., and
Mege, J. L. (2021). A Tangled Threesome: Circa-
dian Rhythm, Body Temperature Variations, and the
Immune System. Biology, 10(1):65.
De Asmundis, C., Conte, G., Sieira, J., Chierchia, G. B.,
Rodriguez-Manero, M., Di Giovanni, G., Ciconte, G.,
Levinstein, M., Baltogiannis, G., Saitoh, Y., Casado-
Arroyo, R., and Brugada, P. (2014). Comparison of
the patient-activated event recording system vs. tradi-
tional 24 h Holter electrocardiography in individuals
with paroxysmal palpitations or dizziness. EP Eu-
ropace, 16(8):1231–1235.
Fortune Business Insights (2020). mHealth Market mHealth
Market Size, Share & Industry Analysis, By Category
(By Apps Disease & Treatment Management, Well-
ness Management, By Wearable Body & Temperature
Monitors, Glucose Monitors). Technical report, For-
tune Business Insights.
Garc
´
ıa, L., Tom
´
as, J., Parra, L., and Lloret, J. (2019). An
m-health application for cerebral stroke detection and
monitoring using cloud services. International Jour-
nal of Information Management, 45:319–327.
Grace, S. L., Taherzadeh, G., Jae Chang, I. S., Boger, J.,
Arcelus, A., Mak, S., Chessex, C., and Mihailidis, A.
(2017). Perceptions of seniors with heart failure re-
garding autonomous zero-effort monitoring of phys-
iological parameters in the smart-home environment.
Heart & Lung, 46(4):313–319.
Gunst, J. and Van den Berghe, G. (2010). Blood Glucose
Control in the Intensive Care Unit: Benefits and Risks.
Seminars in Dialysis, 23(2):157–162.
Habibian, R., Salehi, S., Imani, R., Sadeghi, B., and
Hatamipou, K. (2009). Comparative study of mea-
suring body temperature by mercury and digital ther-
mometer. Iran Journal of Nursing.
Isakadze, N. and Martin, S. S. (2020). How useful is
the smartwatch ECG? Trends in Cardiovascular
Medicine, 30(7):442–448.
Khan, S., Saultry, B., Adams, S., Kouzani, A. Z., Decker,
K., Digby, R., and Bucknall, T. (2021). Comparative
accuracy testing of non-contact infrared thermometers
and temporal artery thermometers in an adult hospi-
tal setting. American Journal of Infection Control,
49(5):597–602.
Klack, L., Schmitz-Rode, T., Wilkowska, W., Kasugai, K.,
Heidrich, F., and Ziefle, M. (2011). Integrated home
monitoring and compliance optimization for patients
with mechanical circulatory support devices. Annals
of biomedical engineering, 39(12):2911–2921.
Kwak, Y.-T., Lee, Y., and You, Y. (2019). Statistical es-
timation of body temperature from skin temperature
for smart band. In 2019 International Conference on
Information and Communication Technology Conver-
gence (ICTC), pages 1477–1481.
Li, H., Shrestha, A., Heidari, H., Kernec, J. L., and Fio-
ranelli, F. (2018). A Multisensory Approach for
Remote Health Monitoring of Older People. IEEE
Journal of Electromagnetics, RF and Microwaves in
Medicine and Biology, 2(2):102–108.
Li, T., Divatia, S., McKittrick, J., Moss, J., Hijnen, N. M.,
and Becker, L. B. (2019). A pilot study of respiratory
rate derived from a wearable biosensor compared with
capnography in emergency department patients. Open
Access Emergency Medicine : OAEM, 11:103.
Liang, Z. and Chapa-Martell, M. A. (2021). Validation
of Omron Wearable Blood Pressure Monitor Heart-
GuideTM in Free-Living Environments. Lecture
Notes of the Institute for Computer Sciences, Social-
Informatics and Telecommunications Engineering,
LNICST, 362 LNICST:339–350.
Lin, M. H., Yuan, W. L., Huang, T. C., Zhang, H. F., Mai,
J. T., and Wang, J. F. (2017). Clinical effectiveness
of telemedicine for chronic heart failure: a system-
atic review and meta-analysis. Journal of investiga-
tive medicine : the official publication of the American
Federation for Clinical Research, 65(5):899–911.
Lockwood, C., Conroy-Hiller, T., and Page, T. (2004). Vital
signs. JBI Reports, 2(6):207–230.
BIODEVICES 2023 - 16th International Conference on Biomedical Electronics and Devices
114

Lovett, P. B., Buchwald, J. M., St
¨
urmann, K., and Bijur, P.
(2005). The vexatious vital: Neither clinical measure-
ments by nurses nor an electronic monitor provides
accurate measurements of respiratory rate in triage.
Annals of Emergency Medicine, 45(1):68–76.
Marion, D. W. (2003). Therapeutic Moderate Hypothermia
and Fever. Cerebral Blood Flow, pages 272–276.
Massaroni, C., Nicol
`
o, A., Sacchetti, M., and Schena,
E. (2021). Contactless methods for measuring res-
piratory rate: A review. IEEE Sensors Journal,
21(11):12821–12839.
McKinlay, C. J., Chase, J. G., Dickson, J., Harris, D. L.,
Alsweiler, J. M., and Harding, J. E. (2017). Continu-
ous glucose monitoring in neonates: a review. Mater-
nal Health, Neonatology and Perinatology 2017 3:1,
3(1):1–9.
Miller, M. R., Hankinson, J., Brusasco, V., Burgos, F.,
Casaburi, R., Coates, A., Crapo, R., Enright, P.,
van der Grinten, C. P. M., Gustafsson, P., Jensen, R.,
Johnson, D. C., MacIntyre, N., McKay, R., Navajas,
D., Pedersen, O. F., Pellegrino, R., Viegi, G., and
Wanger, J. (2005). Standardisation of spirometry. Eu-
ropean Respiratory Journal, 26(2):319–338.
Moc¸o, A. and Verkruysse, W. (2021). Pulse oximetry based
on photoplethysmography imaging with red and green
light: Calibratability and challenges. Journal of Clin-
ical Monitoring and Computing, 35(1):123–133.
Mostafa, M., Hasanin, A. M., Elsayed, O. S., Mostafa,
M. M., and Sarhan, K. (2021). Accuracy of oscillo-
metric blood pressure measurement at both arms in
the lateral position. Blood Pressure Monitoring, pages
364–372.
Nedoma, J., Kepak, S., Fajkus, M., Cubik, J., Siska, P., Mar-
tinek, R., and Krupa, P. (2018). Magnetic Resonance
Imaging Compatible Non-Invasive Fibre-Optic Sen-
sors Based on the Bragg Gratings and Interferometers
in the Application of Monitoring Heart and Respira-
tion Rate of the Human Body: A Comparative Study.
Sensors 2018, Vol. 18, Page 3713, 18(11):3713.
Organization, W. H. (2022). Hypertension.
Pandian, P. S., Mohanavelu, K., Safeer, K. P., Kotresh,
T. M., Shakunthala, D. T., Gopal, P., and Padaki, V. C.
(2008). Smart Vest: Wearable multi-parameter remote
physiological monitoring system. Medical Engineer-
ing & Physics, 30(4):466–477.
Parak, J. and Havlik, J. (2011). ECG signal processing and
heart rate frequency detection methods. In Proceed-
ings of Technical Computing Prague.
Pham, M., Mengistu, Y., Do, H. M., and Sheng, W.
(2016). Cloud-Based Smart Home Environment
(CoSHE) for home healthcare. IEEE International
Conference on Automation Science and Engineering,
2016-November:483–488.
Pigini, L., Bovi, G., Panzarino, C., Gower, V., Ferratini,
M., Andreoni, G., Sassi, R., Rivolta, M. W., and Fer-
rarin, M. (2017). Pilot Test of a New Personal Health
System Integrating Environmental and Wearable Sen-
sors for Telemonitoring and Care of Elderly People at
Home (SMARTA Project). Gerontology, 63(3):281–
286.
Popescu, M. and Mahnot, A. (2012). Early illness recog-
nition using in-home monitoring sensors and mul-
tiple instance learning. Methods of information in
medicine, 51(4):359–367.
Rashidi, P. and Mihailidis, A. (2013). A survey on ambient-
assisted living tools for older adults. IEEE Journal of
Biomedical and Health Informatics, 17(3):579–590.
Rodr
´
ıguez, H., Williams, M., Wilkes, J. S., and Rogers,
R. D. (2008). Ionic liquids for liquid-in-glass ther-
mometers. Green Chemistry, 10(5):501–507.
Rose, L. and Clarke, S. P. (2010). Vital Signs. American
Journal of Nursing, 110(5):11.
Saquib, N., Papon, M. T. I., Ahmad, I., and Rahman,
A. (2015). Measurement of heart rate using pho-
toplethysmography. Proceedings of 2015 Interna-
tional Conference on Networking Systems and Secu-
rity, NSysS 2015.
Sardini, E. and Serpelloni, M. (2014). T-shirt for vital pa-
rameter monitoring. Lecture Notes in Electrical Engi-
neering, 162 LNEE:201–205.
Shivakumar, N. S. and Sasikala, M. (2014). Design of vital
sign monitor based on wireless sensor networks and
telemedicine technology. Proceeding of the IEEE In-
ternational Conference on Green Computing, Com-
munication and Electrical Engineering, ICGCCEE
2014.
Sixsmith, A., Johnson, N., and Whatmore, R. (2005). Pyro-
electric IR sensor arrays for fall detection in the older
population. Journal De Physique. IV : JP, 128:153–
160.
Spodick, D. H., Raju, P., Bishop, R. L., and Rifkin,
R. D. (1992). Operational definition of normal si-
nus heart rate. The American Journal of Cardiology,
69(14):1245–1246.
Subhi, R., Smith, K., and Duke, T. (2009). When should
oxygen be given to children at high altitude? A sys-
tematic review to define altitude-specific hypoxaemia.
Archives of Disease in Childhood, 94(1):6–10.
Sudana, D. and Emanuel, A. W. (2019). How Big Data
in Health 4.0 Helps Prevent the Spread of Tuberculo-
sis. Proceedings - 2019 2nd International Conference
on Bioinformatics, Biotechnology and Biomedical En-
gineering - Bioinformatics and Biomedical Engineer-
ing, BioMIC 2019.
Villar, R., Beltrame, T., and Hughson, R. L. (2015).
Validation of the Hexoskin wearable vest dur-
ing lying, sitting, standing, and walking ac-
tivities. https://doi.org/10.1139/apnm-2015-0140,
40(10):1019–1024.
Vinkers, C. H., Penning, R., Hellhammer, J., Verster, J. C.,
Klaessens, J. H., Olivier, B., and Kalkman, C. J.
(2013). The effect of stress on core and peripheral
body temperature in humans. The International Jour-
nal on the Biology of Stress, 16(5):520–530.
Wang, J. (2008). Electrochemical glucose biosensors.
Chemical Reviews, 108(2):814–825.
Monitoring of Vital Signs in the Home Environment: A Review of Current Technologies and Solutions
115
