
Evaluating COVID-19 Treatment Among Infected COVID-19
Patients at a Private Hospital in North Jakarta in 2021
Dini Permata Sari and Siti Saidatus S.
Faculty of Pharmacy, Universitas 17 Agustus 1945, Jakarta, Indonesia
Keywords: COVID-19, COVID-19 Treatment, Evaluation.
Abstract: Coronavirus Disease 2019 (COVID-19) is a newly discovered infectious respiratory disease caused by severe
acute respiratory syndrome, coronavirus 2 (SARS CoV-2). This study purpose evaluation of handling on the
treatment of COVID-19 patients at a private hospital in North Jakarta. This study an observational method
with a sample of 109 people selected using purposive sampling. The instrument of this study used patient
medical record data. The result of this study was from 109 patients, 58.45% of them w male with 78.90%
without comorbidities in the study. The treatment were given antiviral (oseltamivir, favipiravir, remdesivir),
antibiotics (azithromycin, levofloxacin), symptomatic drugs (mucolytics/expectorants, fever, pain, etc.),
comorbidity drugs (such as DM drugs, hypertension drugs, and other comorbidities drugs), and therapeutic
additives such as heparin. Most of those patient received oseltamivir and azitromycin for COVID-19 treatment
at the private hospital in north Jakarta.
1 INTRODUCTION
The coronavirus disease 2019 (COVID-19) is a major
health concern today. COVID-19 was caused by the
SARS-CoV-2 virus. An outbreak of viral pneumonia
of unknown etiology was found introduced in Wuhan,
China on December 12, 2019 (Ji et al, 2020).
Indonesia has announced a case of COVID-19 to
be precise in March 2020 (WHO,2020). The data on
March 31, 2020, showed that there were 1,528
confirmed cases and 136 deaths ((Ministry of Health,
2021).
Infection occurs when particles containing the
virus exhaled by an infected person, either as
respiratory droplets or aerosols, enter the mouth,
nose, or eyes of another person who is in close contact
(Zhai et al., 2020)
Symptoms of coronavirus disease often vary, but
most people experience fever, cough, difficulty
breathing, fatigue, and loss of smell and taste. In
severe cases of renal failure, high fever, organ failure,
dyspnea, and hypoxia, are observed (Lata et al.,
2021).
No specific treatment for coronavirus infection
has been prescribed to date, except for careful
supportive care. Management of the source of
infection, minimizing personal protective procedures,
risk of transmission, and early identification,
isolation, and supportive care for infected patients are
the solutions to this disease. There is no adequate
antibacterial agent (Rahmatillah &Isnaini, 2021).
Based on the references above, an exploration
about the treatment given among COVID-19 patients
was needed to be conducted.
2 METHODS
This study used observational methods. Using
retrospective cohort studies, by collecting secondary
data on patient medical records in 2021. The sample
used was 109 people who were COVID-19 patients at
A Private Hospital in North Jakarta, which was
selected using Purposive sampling in accordance with
existing inclusion criteria. Data collection using
tables created in excel. Inclusion Criteria:
a. Confirmed positive for COVID-19 based on
Swab or Antigen.
b. Patients over 18 years of age.
c. Completed medical records.
d. COVID-19- positive patients with and without
comorbidities.
Sari, D. and S., S.
Evaluating COVID-19 Treatment Among Infected COVID-19 Patients at a Private Hospital in North Jakarta in 2021.
DOI: 10.5220/0011979000003582
In Proceedings of the 3rd International Seminar and Call for Paper (ISCP) UTA â
˘
A
´
Z45 Jakarta (ISCP UTA’45 Jakarta 2022), pages 219-224
ISBN: 978-989-758-654-5; ISSN: 2828-853X
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
219
3 RESULT AND DISCUSSION
Based on research that has been carried out at a
Private Hospital in North Jakarta, COVID-19 among
patients hospitalized during the 2021 period who met
the inclusion and exclusion criteria, was 109 patients.
Medical records with complete data based on patient
characteristics including gender, age, weight,
comorbid diseases, and patient treatment therapy.
3.1 Profile Based on Patient
Characteristics
3.1.1 Gender
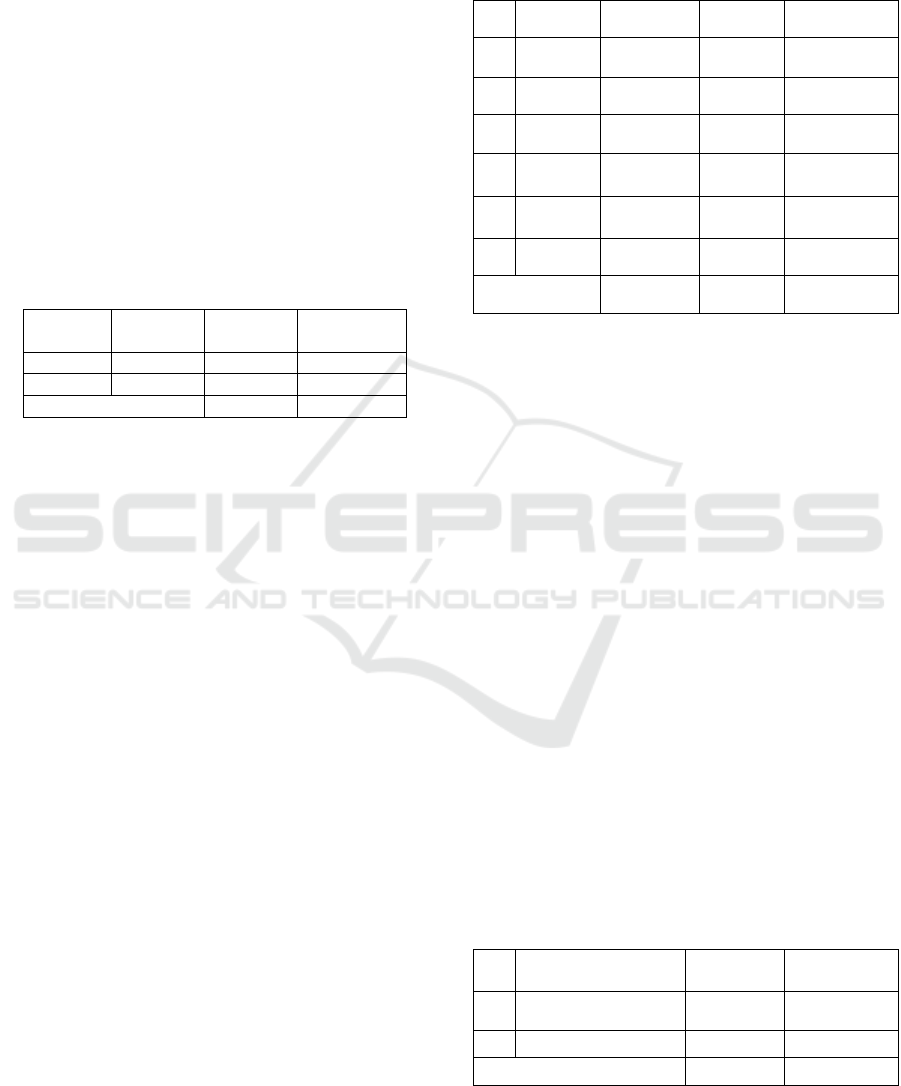
Table 1: Percentage of COVID-19 patients based on
gender.
No Type Sex Amount Percentage
%
1 Man 64 58,71%
2 Woman 45 41,29%
Total 109 100%
Based on table 1, it can be seen that the number of
patients diagnosed positive for COVID-19 with or
without comorbid diseases among patients at a
Private Hospital in North Jakarta, was 109 patients
based on gender with male 64 patients with a
percentage of 58.71%, while female patients were 45
patients with a percentage of 41.29% (Table 1). The
research data obtained, it shows that the COVID-19
disease in Private Hospitals in North Jakarta occurs
more in males.
There are more male patients than females
infected with COVID-19 (Zhai et al., 2020). Found
that, due to the patient's weak immune function,
SARS-CoV-2 was more likely to infect older adult
males with chronic comorbidities (Zhai et al., 2020).
Gender has been shown to be is a risk factor for
mortality in COVID-19 patients, where males die
more than women. This is due to fundamental
differences in the immunological systems of males
and women, differences in lifestyle, and the
prevalence of smoking (Wenham, et al. 2020).
Fewer males recovered than the group who died.
Higher mortality rates are associated with higher
chronic comorbidities in males, cardiovascular
disease, hypertension, pulmonary disease, and
smoking (Jean et al., 2020).
3.1.2 Age
From the results of research that has been carried out
based on the age characteristics of among patient
COVID-19 patients at a Private Hospital in North
Jakarta, it can be seen in table 2, as follows:
Table 2: Percentage of COVID-19 patients based on age.
No Age Category Amount Percentage %
1 17-25 Late Teen 10 9.17%
2 26-35 Early Adult 17 16.00%
3 36-45 Late Adult 28 25.69%
4 46-55
Early
Elderl
y
26 23.85%
5 56-65
Late
Elderl
y
16 14.67%
6 >65 seniors 12 11.00%
TOTAL 109 100%
Based on table 2, it can be seen that the number of
patients diagnosed as positive for COVID-19 with or
without comorbid diseases at a Private Hospital in
North Jakarta was 109 patients. Based on the age
characteristics of COVID-19-positive patients, most
in the late adult category with ages 36-45 years as
many as 28 patients with a percentage of 25.68%
(Table 2).
Elderly patients have long-term health problems
so they are more at risk when exposed to the virus, a
person's immune system decreases when they reach
old age, making it difficult to fight infection.
These results are reinforced by research, which
shows data that Covid-19 mortality increases with age
with a percentage of CFR of 1.3% in patients aged 50-
59 years, 3.6% in patients aged 60-69 years, 8% in
patients aged 70-79 years, and 14.8% in patients aged
≥80 years (Wiliam et al, 2021).
The percentage of COVID-19 mortality is
increasing due to age increase, with the youngest
patients aged 5% to the oldest at 55% ((Zhou et al,
2020).
3.1.3 Patients with or without Comorbidities
Table 3: Percentage of COVID-19 patients based on with
or without comorbid
No Disease
Comorbidities
Amount Percentage %
1 With comorbid 23 21,10%
2 Without comorbid 86 78.90 %
TOTAL 109 100
Based on table 3, it can be seen that the number of
patients diagnosed as positive for COVID-19 who
ISCP UTA’45 Jakarta 2022 - International Seminar and Call for Paper Universitas 17 Agustus 1945 Jakarta
220
underwent hospitalization at A Private Hospital in
North Jakarta in 2021 as many as 109 patients based
on the characteristics of patients with or without
comorbidities, namely patients with comorbidities.
patients with comorbidities were 23 patients with a
percentage of 21.10%, and patients without
comorbidities 86 patients with a percentage of
78.90% (Table 3).
The presence of comorbidities can determine the
prognosis of COVID-19 patients. This is presumably
because previous health conditions affect the severity
of COVID-19 sufferers. Thus, the presence of
comorbidities will exacerbate COVID-19 infection
and can even become the pathogenesis of COVID-19
infection.
3.1.4 Patients by Type of Comorbid Disease
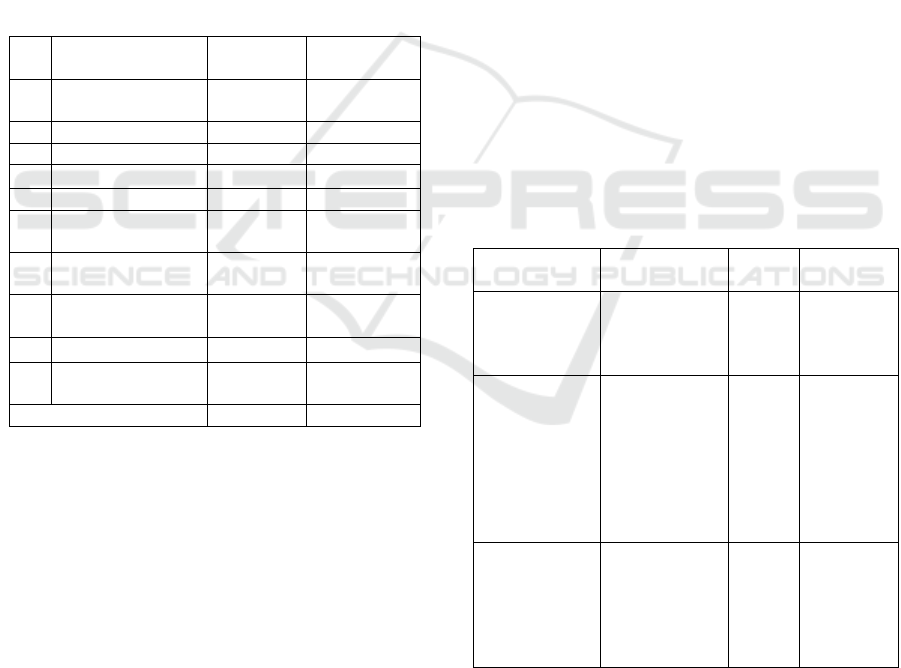
Table 4: Percentage of COVID-19 Patients based on the
type of comorbid disease.
No
Type Disease
Participant
Amount Percentage %
1
Hypertension &
DM
4 17.40%
2 DM 3 13.04 %
3 Kidne
y
/ CKD 3 13.04 %
4 Hypertension 6 26.08%
5 Broncho
p
neumonia 1 4.35%
6
Pulmonary TB &
Anemia
1 4.35%
7
Hypertension &
Thrombocytopenia
1 4.35%
8
Post Stroke &
H
yp
ertension
1 4.35%
9 Dyspepsia 1 4.35%
10
Hypertension &
Kidne
y
2 8.69%
TOTAL 23 100%
Based on table 4, it can be seen that the number of
patients diagnosed as positive for COVID-19 patients
at a Private Hospital in North Jakarta in 2021 was 109
patients. Characteristics of patients based on the type
of comorbidities as many as 23 patients. Patients who
had the most comorbidities were hypertension as
many as 6 patients with a percentage of 26.08%, and
comorbid complications of hypertension & diabetes
mellitus as many as 4 patients with a percentage of
17.40% (Table 4).
The most common comorbidities reported in
COVID-19 patients are hypertension, cardiovascular
diseases, and diabetes (Jarahzadeh et al., 2021).
Chronic heart and metabolic disease, the
presence of acute inflammation, and decreased organ
function (heart, kidney, liver, and hematology)
experienced by patients at the beginning of treatment
can increase the risk of death due to COVID-19
infection (Yang & Yan, 2020).
Meanwhile, a UK study showed that patients
with heart, kidney and lung disease, cancer, dementia,
and obesity, had a higher risk of death (Docherty et
al., 2020).
3.2 Therapeutic Profile of COVID-19
Patients Treatment
The data obtained were classified into descriptions of
the treatment of COVID-19 patients including all
drugs (whether single or combination drug use) used
for the treatment of hospitalized COVID-19 patients
with a total sample of 109. The use of drugs for the
treatment of hospitalized suspected Covid-19 patients
in private Hospitals in North Jakarta includes
antibiotics, antiviral drugs, vitamins, multivitamins
and supplements, symptomatic drugs to reduce
symptoms, and comorbid drugs to treat comorbidities
in confirmed COVID-19 patients. Then it is analyzed
trough numbers and percentages and presented in the
form of a table.
3.2.1 The Use of Drugs as the Main Therapy
for Covid-19
Table 5: Percentage of the use of drugs as the main therapy
for Covid-19.
group Type Drug
Amount
use
Percentage
%
Antiviral
Oseltamivir
Remdesivir
favipirafir
Iso
p
rinosine
71
12
16
63
43.83%
7.40%
9.88%
38.89%
Antibiotics
Azithromycin
Levofloxacin
Fradiomicin -
Gramicidin
Metronidazole
Ceftriaxone
Cefotaxime
cefadroxil
83
62
2
2
1
2
1
54.25%
40.52%
1.31%
1.31%
0.65%
1.31%
0.65%
Multivitamins/
Supplements
Vit C
Vit D
Zink
Vit K
Mecobalamin
Folic Aci
d
108
107
86
1
3
2
35.18%
34.85%
28.01%
0.33%
0.98%
0.65%
Based on table 1, it shows the use of drugs used as
main therapy in COVID-19 patients among patients
at a Private Hospital in, North Jakarta in 2021,
including multivitamins / supplements, antivirals, and
antibiotics.
Evaluating COVID-19 Treatment Among Infected COVID-19 Patients at a Private Hospital in North Jakarta in 2021
221
Drug use therapy as the main therapy used is with
antiviral drugs such as oseltamivir, isoprinosine,
remdesivir, and favipiravir. In the study data, patients
were given more oseltamivir antivirals as many as 71
with a presentase 3,83% (Table 1).
Oseltamivir has also been used in clinical trials in
various combinations with chloroquine and
favipiravir, nucleoside analogues known as broad-
spectrum antiviral drug that have follow-up in male,
those in the older age groups with chronic kidney
disease, and those whose therapy is Oseltamivir +
Chloroquine, 16 people (57.1%) recovered clinically.
Four were shown EC50 61.88 M against SARS-CoV-
2 and low toxicity (CC50>400 M) ((Zhai et al., 2020).
Furthermore, drug therapy as the main therapy
used was Multivitamins/Supplements. In this study,
the most widely used multivitamins/supplements
were vitamin D, vitamin C, and zinc. The use of
Vitamin C either orally or intravenously is effective
in reducing the severity, reducing the risk of
complications, overcoming symptoms and improving
the prognosis of COVID-19 patients.
The administration of vitamin C can significantly
reduce pneumonia caused by coronavirus by
increasing the expression of IFR 3 (Interferon
regulatory factor 3) which functions to cause an
innate antiviral response, inhibit nuclear factor kappa-
B (NFkB), and play an important role in immunity by
regulating chemokines, cytokines, adhesion
molecules, inflammatory mediators and inhibiting
apoptosis (Cai et al., 2015).
In this study, vitamins were prescribed to all
patients. The number of studies also shows the same
pattern. Vitamins other than to restore the deficiency
has a role as an antioxidant. Most studies also show
the same pattern ((Lata et al., 2021)).
COVID-19 disease is characterized by
pneumonia, so the use of antibiotics is needed to be
able to prevent bacterial co-infection. The most
widely used antibiotics in this study are levofloxacin
and azithromycin. Azithromycin can strengthen the
effect of hydroxychloroquine in lowering viral load in
COVID-19 patients. Azithromycin, in addition to its
macrolide antibacterial activity, also has antiviral and
immunomodulating properties. This action makes
azithromycin often an option in the management of
inflammatory manifestations of coronavirus
involving the lungs ((Lata et al., 2021).
3.2.2 The Use of Drugs as Symptomatic
Therapy of COVID-19
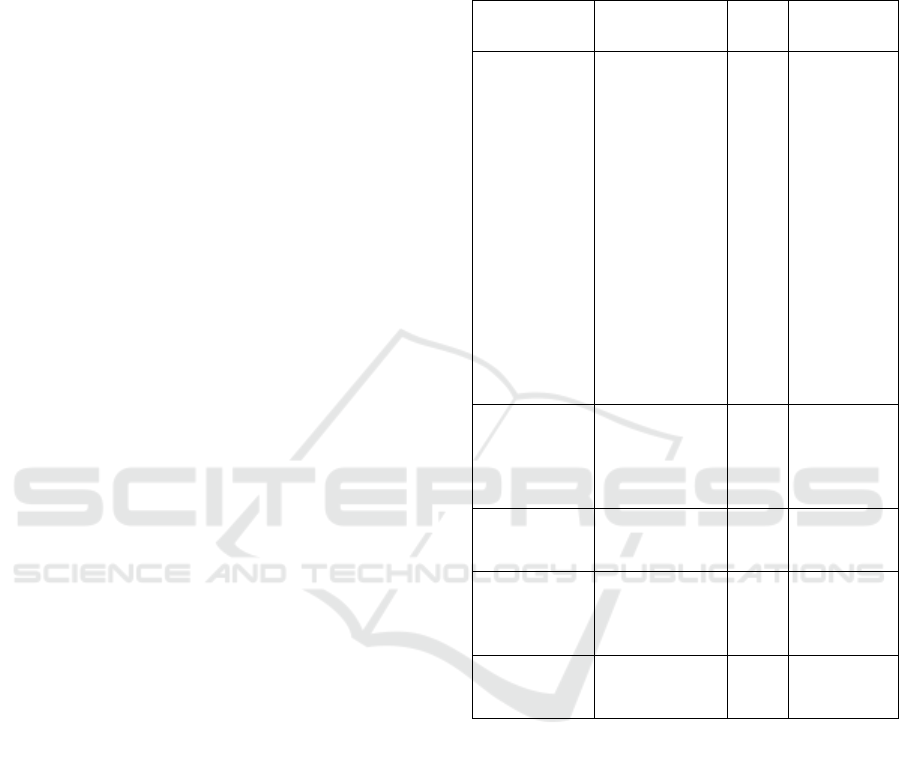
Table 6: Percentage of the use of drugs as symptomatic
therapy of COVID-19.
group Type of
medicine
Total
Usage
Percentage
%
Gastrointestina
l drugs (gastric
ulcers, gastritis
and
antiemetics)
Histamine H2
Receptor
Antagonists
(Ranitidine)
Proton Pump
Inhibitor PPI
(Omeprazole,
lansoprazole)
Antacids and
Antireflux
(Sucralfate,
strocaine, and
rebamipide)
Antiemetics
(ondancentron
and
domperidone)
38
18
17
40
33.63%
15.93%
15.04%
35.40%
Mucolytic &
expectorant
Ambroxol
Acetyl cysteine
Loratadine &
pseudoephedrine
OBH
1
70
2
16
1.12%
78.65%
2.25%
17.98%
Antidiarrhea
and
consti
p
ation
Attapulgit
Loperamide
Laxadine
4
5
4
30.77%
38.46%
30.77%
NSAID Paracetamol
Dexamethasone
US. Mefenamate
Ketorolac
54
33
1
1
60.68%
37.08%
1.12%
1.12%
Antihistamines Betahistine
Flunarizine
CTM
7
1
2
70%
10%
20%
Based on table 2, it shows that the use of drugs used
as symptomatic therapy in COVID-19 patients treated
at a Private Hospital in North Jakarta in 2021. The
administration of these drugs aims to overcome the
clinical symptoms experienced by COVID-19
patients. that can worsen the situation, condition and
support the success of therapy. The use of
symptomatic therapy drugs is intended to reduce the
symptoms felt by the patient, such as fever, cough,
sore throat, nausea, diarrhea, and so on.
Based on research conducted on treatment for
symptomatic therapy in COVID-19 patients at A
Private Hospital in North Jakarta in accordance with
the guildelines for the management of COVID-19
patients according to the Indonesian Lung Doctors
Association (PDPI) and the Ministry of Health.
Symptomatic therapy is given according to the
ISCP UTA’45 Jakarta 2022 - International Seminar and Call for Paper Universitas 17 Agustus 1945 Jakarta
222
symptoms experienced by COVID-19 patients to
reduce the symptoms experienced.
3.2.3 The Use of Drugs by Type of
Comorbid Disease Class
Table 7: Percentage of the use of drugs by type of comorbid
disease class.
group Amount
use
Percentage %
Drug Comorbid
Hypertension :
Amlodipine
Losartan
Captropil
Bisoprolol
Simvastatin
Kandesartan
33
21
2
5
2
1
2
78.58%
Drug CKD
comorbid :
Furosemide
1 2.38%
Dru
g
Heart : ISDN 4 9.52%
Drug Comorbid
DM:
Metformin
Insulin Lispro
4
3
1
9.52%
TOTAL 42 100%
Based on table 3, it shows the use of comorbid disease
drug classes in COVID-19 patients who are
hospitalized at A Private Hospital in North Jakarta in
2021. The table above shows data on 42 patients
confirmed COVID-19 patients, there are 33 patients
with comorbid hypertension who use hypertension
drug therapy with a percentage of 78.90%. With the
most use of hypertension drugs, namely amlodipine
by 50% (Table 3).
Patients with cardiac comorbidities were patients,
and the drug used was ISDN with a percentage of
2.38%. Patients with the use of diuretic drug classes
for patients with comorbid renal failure and heart
failure with a percentage of 2.38% using furosemide.
The use of comorbid DM drugs was 4 patients with a
percentage of 9.52%. The most widely used drug use
in COVID-19 patients with comorbid DM is
metforfin with a percentage of 7.15% (Table 3).
3.2.4 The Use of Drugs as Adjunctive
Therapy
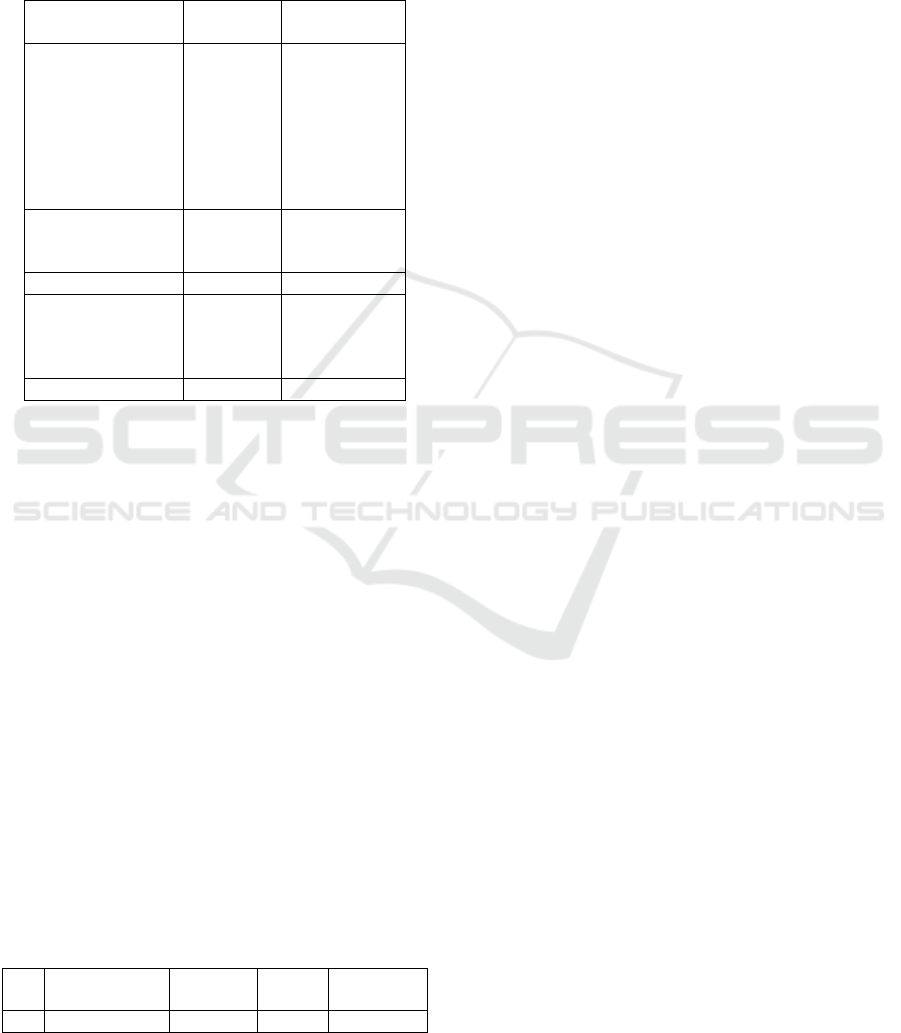
Table 8: Percentage of the use of drugs as adjunctive
therapy.
No group
Drug
Type
Usage
amount
Percentage
%
1 Anticoagulants Heparin 53 48.62%
Based on table 4, it shows the use of drugs as
additional therapy for Covid-19 among patient at A
Private Hospital in North Jakarta in 2021. The
provision of additional therapy for Covid-19 aims to
support the success of the therapy carried out.
Additional therapy used for Covid-19 patients is an
anticoagulant drug class, the type of drug used is
heparin. Giving anticoagulants aims to prevent
coagulation which can result in thrombosis and
thromboembolism.
Therapeutic use of anticoagulant drugs in Covid-
19 patients provides a good prognosis. Coagulation
disorders, especially increased values of D-dimer and
Fibrinogen-degradation product (FDP) were found in
high levels in pneumonia patients due to Covid-19
who died. Based on the guidelines for the treatment
of Covid-19, the provision of anticoagulants is seen
based on the evaluation of the DPJP (see explanation
on severe / critical degrees) (Ministry of Health,
2021).
4 CONCLUSION
The average age among those patients was 36-45 with
only less than 25,69% of them had hypertension and
diabetic. Most of those patients oseltamivir as an
antiviral and azitromycin as an antibiotic.
REFERENCES
Bhagat RK, Linden PF. Displacement ventilation: A viable
ventilation strategy for emergency hospitals and public
buildings to contain COVID-19 and other airborne
diseases. R Soc Open Sci 2020;7:200680.
Cai, Y., Li, Y., Tang, L., Tsoi, B., Chen, M., Chen, H.,
Chen, X., Tan, R., Kurihara, H., & He, R. (2015). A
New Mechanism of Vitamin C Effects on A / FM / 1 / 47
( H1N1 ) Virus-Induced Pneumonia in Restraint-
Stressed Mice. 2015.
Docherty, A. B., Harrison, E. M., Green, C. A., Hardwick,
H. E., Pius, R., Norman, L., Holden, K. A., Read, J. M.,
Dondelinger, F., Carson, G., Merson, L., Lee, J.,
Plotkin, D., Sigfrid, L., Halpin, S., Jackson, C., Gamble,
C., Horby, P. W., Nguyen-Van-Tam, J. S., … Semple,
M. G. (2020). Features of 20 133 UK patients in
hospital with covid-19 using the ISARIC WHO Clinical
Characterisation Protocol: Prospective observational
cohort study. The BMJ, 369(March), 1–12.
https://doi.org/10.1136/bmj.m1985.
Doctor, P., & Indonesia, P. (n.d.). COVID-19 Pneumonia
Diagnosis & Amplifics In Indonesia.
Huang C, Wang Y, Li X, et al. Clinical picture of patients
infected with novel coronavirus 2019 in 2020.100719
PMID: 32717568 PLOS ONE |
Evaluating COVID-19 Treatment Among Infected COVID-19 Patients at a Private Hospital in North Jakarta in 2021
223

https://doi.org/10.1371/journal.pone.0250147 April 16,
2021 Wuhan, China. Lanceolate. 2020;
395(10223):497–506. https://doi.org/10.1016/S0140-
6736(20)30183-5 PMID: 31986264
Jarahzadeh, M. H., Asadian, F., Farbod, M., Meibodi, B.,
Abbasi, H., Jafari, M., Raee-Ezzabadi, A., Bahrami, R.,
& Neamatzadeh, H. (2021). Cancer and Coronavirus
Disease (COVID-19): Comorbidity, Mechanical
Ventilation, and Death Risk. Journal of
Gastrointestinal Cancer, 52(1), 80–84.
https://doi.org/10.1007/s12029-020-00529-2.
Jean, S. S., Lee, P. I., & Hsueh, P. R. (2020). Treatment
options for COVID-19: The reality and challenges.
Journal of Microbiology, Immunology and Infection,
53(3), 436–443.
https://doi.org/10.1016/j.jmii.2020.03.034.
Ji, W., Wang, W., Zhao, X., Zai, J., & Li, X. (2020). Cross-
Species Transmission of the Newly Identified
Coronavirus 2019-nCoV. Journal of Medical Virology,
92(4), 433– 440. https://doi.org/10.1002/jmv.25682.
Lata, S., Khajuria, V., & Sawhney, V. (2021). Machine
Translated by Google POLA PENGOBATAN PASIEN
COVID-19 DI RUMAH SAKIT PERAWATAN TERSIR
Machine Translated by Google. 14, 9–12.
LATA, S., KHAJURIA, V., & SAWHNEY, V. (2021).
Treatment Pattern of Covid-19 Patients in a Tertiary
Care Teaching Hospital of Northern India. Asian
Journal of Pharmaceutical and Clinical Research,
14(11), 48–51.
https://doi.org/10.22159/ajpcr.2021.v14i11.42345.
Ministry of Health of the Republic of Indonesia. (2021).
Clinical Management of Corona Virus Disease 2019
(COVID-19) Management in Health Service Facilities.
Ministry of Health of the Republic of Indonesia, 2019,
1–360.
https://covid19.go.id/storage/app/media/Regulasi/2021
/Agustus/kmk-no-hk0107-menkes-5671-2021-ttg-
manajemen-klinis-tata-laksana-covid-19-di-fasilitas-
pelayanan-kesehatan-signed-1.pdf.
Ministry of health of the Republic of Indonesia. (2021,
August). The current situation of the development of
corona virus. Ministry of Health of the Republic of
Indonesia. Retrieved
darihttps://covid19.kemkes.go.id/situasi-infeksi-
emerging/ accessed 02 August 2021.
Rahmatillah & Suri Isnaini. (2021). Treatment Profiles and
Clinical Outcome of COVID-19 Patients at Private
Hospital in Jakarta. Jakarta. April, 1–11.
Yang, W., & Yan, F. (2020). Patients with RT-PCR-
Confirmed COVID-19 and Normal Chest CT.
Radiology, 41(1), 43–43.
https://doi.org/10.1177/030802267804100122.
Wenham, C., Smith, J., & Morgan, R. (2020). COVID-19:
the Gendered Impacts of the Outbreak. In The Lancet
(Vol. 395, Issue 10227, pp. 846–848).
https://doi.org/10.1016/S0140-6736(20)30526-2.
Wiliam, Herick A., Ketaren, Infan, & Supit, Alice I. (2020).
Impact of coronavirus disease 2019 on the
kardiovascular system. E-CliniC,8(2).
World Health Organization. (2021, August). Coronavirus
Disease 2019 (Covid-19) situation report. WHO.
Retrieved from
https://covid19.who.int/table?tableDay=yesterday&tab
leChartType=heatdiakses 02 August 2021. 5.
Zhai, P., Dinga, Y., Wub, X., Longc, J., Zhong, Y., & Li,
Y. (2020). Jurnal Internasional Agen Antimikroba
Machine Translated by Google. 55.
Zhang, M.; Jativa, D.F. Vitamin C supplementation in
critically ill people: a systematic review and meta-
analysis. SAGE Open Med. 2018, 6. [CrossRef].
Zhou, F., Yu, T., Du, R., Fan, G., Liu, Y., Liu, Z., Xiang,
J., Wang, Y., Song, B., Gu, X., Guan, L., Wei, Y., Li,
H., Wu, X., Xu, J., Tu, S., Zhang, Y., Chen, H., & Cao,
B. (2020). Clinical Course and Risk Factors for
Mortality of Adult Inpatients with COVID-19 in
Wuhan, China: a retrospective cohort study. The
Lancet, 395(10229), 1054–1062.
https://doi.org/10.1016/S0140-6736(20)30566-3.
ISCP UTA’45 Jakarta 2022 - International Seminar and Call for Paper Universitas 17 Agustus 1945 Jakarta
224
