
Evaluation of Correlation Between Severity and Laboratory Data for
COVID-19 Patients at Jakarta Private Hospital
Nona Ainah
1
, Diana Laila Ramatillah
2
and Michael
1a
1
Faculty of Pharmacy, Universitas 17 Agustus 1945, Jakarta 14350, Indonesia
2
Clinical Pharmacy, Universiti Sains Malaysia, Malaysia
Keywords: Evaluation, Correlation, COVID-19, Severity, Laboratory Data.
Abstract: As of June 29, 2022, the COVID-19 outbreak has caused around 6 million confirmed cases, with the deaths
of around 156.000 patients in Indonesia. The purpose of this study was to clarify the correlation between
severity and laboratory data for COVID-19 patients at Jakarta Private Hospital. A retrospective cohort study
with convenience sampling was applied in this study. The study was conducted from March to June 2021.
There were 980 patients, but only 320 patients were eligible for inclutions criteria. The gender of the majority
of patients as the sample was male, 165 (52%) and 155 (48%) female patients. The results of this study showed
that almost all non-ICU patients had moderate severity, totaling 261 (91%). Meanwhile, patients admitted to
the ICU had a critical severity level of 32 (97%). In COVID-19 patients, severity correlated with ICU or non-
ICU (P-value <0.05). Laboratory data that show a correlation with the severity of COVID-19 infection are
leukocytes (P=0.001), platelets (P=0.006), urea (P=0.003), and creatinine (P=0.021). The conclusion in this
study shows that there is a significant correlation between laboratory data and the severity of COVID-19
patients (P-value <0.05).
1 INTRODUCTION
In December 2019, an outbreak of an unknown
pneumonia was reported. A virus called SARS-
CoV2, which is characterized as a highly contagious
and deadly disease, was discovered (Chen et al.,
2020). SARS-CoV-2 is a new type of coronavirus that
has never been identified in humans. At least two
types of coronavirus are known to cause illnesses that
can lead to severe symptoms, including Middle East
Respiratory Syndrome (MERS) and Severe Acute
Respiratory Syndrome (SARS) (Dirjen P2P
Kemenkes R1, 2020) (WHO, 2020).
The COVID-19 outbreak has caused around 6
million confirmed cases, with the deaths of around
156,000 patients in Indonesia as of June 29, 2022
(Worldometers, 2022). According to the Minister of
Health of the Republic of Indonesia, there are 4
categories of severity of COVID-19 patients: [1]
asymptomatic, [2] moderate symptoms (patients with
pneumonia symptoms and SpO2 93-95%), [3] severe
symptoms (patients with pneumonia and
SpO2<93%), and [4] critical illness (patients with
a
https://orcid.org/0000-0003-0207-0275
ARDS, sepsis, and septic shock) (Michael &
Ramatillah, 2022).
Some studies have shown that mild or
asymptomatic COVID-19 has low levels of SARS-
CoV, develops two specific antibodies, or cannot
detect them at all levels. However, severely ill patients
are at a higher level. This data raises questions with
the protective ability of antibodies and the
involvement of specific antibodies in the cause of
COVID-19 (a new coronavirus infection) (Goudouris,
2021).
The consequences of SARS-CoV-2 infection with
severe acute respiratory syndrome are very different,
and it is clear that the majority of young people
suffers from mild illness (Brodin, 2021). In patients
with severe illness, men are overestimated, probably
due to differences in evoked immune responses.
Comorbidities such as obesity, hypertension, chronic
obstructive pulmonary disease, and cardiovascular
disease are all associated with severe COVID-19
infections (Brodin, 2021). SARS-CoV-2 copies at
diagnosis were reported to be higher in patients with
severe COVID-19 than in patients with mild COVID-
Ainah, N., Ramatillah, D. and Michael, .
Evaluation of Correlation Between Severity and Laboratory Data for COVID-19 Patients at Jakarta Private Hospital.
DOI: 10.5220/0011978500003582
In Proceedings of the 3rd International Seminar and Call for Paper (ISCP) UTA â
˘
A
´
Z45 Jakarta (ISCP UTA’45 Jakarta 2022), pages 193-196
ISBN: 978-989-758-654-5; ISSN: 2828-853X
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
193

19. Smoking is another risk factor. Cigarette smoke
induces the expression of angiotensin-converting
enzyme 2 (ACE2). This can allow SARS-CoV-2 to
invade cells and affect viral entry beyond adverse
effects on overall lung function (Brodin, 2021).
2 METHOD
This study used a retrospective cohort study with
convenience sampling conducted from March to June
2021 on COVID-19 patients treated at the Jakarta
Private Hospital.
2.1 Selection Criteria
2.1.1 Inclusion Criteria
▪ Patients are >18 years old;
▪ Patients who have complete medical records;
▪ COVID-19 positive patients with and without
comorbidities.
2.1.2 Exclusion Criteria
▪ Patients with advanced cancer;
▪ SLE sufferers;
▪ Pregnant women;
▪ HIV/AIDS sufferers.
2.2 Ethical Approval
The research received approval from the ethical
community by the Health Research Ethics Committee
at the University of 17 August 1945 Jakarta, based on
a certificate of ethical feasibility (Ethical Clearance).
2.3 Data Analysis
Before collecting data, the researcher first asked for
ethical approval. The process of data collection and
recording of medical record data for COVID-19
patients undergoing laboratory examinations. There
were 980 patients but only 320 patients met the
inclusion criteria. The gender of the majority of
patients in the sample were male 165 and 155 female
patients. Then the data was analyzed descriptively
with the Kruskal wallis method and Fisher's exact test
using SPSS version 25 software. In this study the
distribution was not normal or there was a significant
correlation indicated by P-value<0.05 (error rate of
5%).
3 RESULT AND DISCUSSION
3.1 Correlation Between Severity with
ICU / non-ICU of Covid-19 Patients
Almost all non-ICU patients had moderate severity,
with 261 (91%) patients. Meanwhile, patients
admitted to the ICU had a critical severity level of 32
(97%) patients. From table 1, it can be seen that there
is a correlation between severity and patients
admitted to ICU or non-ICU (p=0.001).
Based on research by Hockova et al. Up to a
quarter of hospitalized COVID-19 patients require
intensive care unit (ICU) treatment, revealing
epidemiological evidence that patients admitted to the
intensive care unit are susceptible to the following
illnesses: secondary pneumonia, heart injury, kidney
injury, and neurological disorders (Hocková et al.,
2021).
3.1 Correlation Between Severity with
Laboratory Data of COVID-19
Patients
In Table 2, it can be seen that most of the leukocytes
of COVID-19 patients had moderate severity in 262
(82%) patients. Leukocytes were found to be
correlated to patient severity (p=0.001). According to
the guidelines for interpreting clinical data in
Indonesia, the main functions of leukocytes are to
fight infection, protect the body by attracting foreign
organisms and produce or distribute antibodies.
Leukocytes have a normal value of 3200-
10,000/mm3 (Kemenkes RI, 2011).
Table 1: Correlation Between Severity and ICU/non-ICU.
Facto
r
Severit
y
Total Sig.
(P-Value)*
Mild
n (%)
Moderate
n (%)
Severe
n (%)
Critical Illness
n (%)
Non ICU 16 (5.5) 261 (91) 10 (3.48) 0 (0) 287 0.000
ICU 0 (0) 1 (3.0) 0 (0) 32 (97) 33
16 (5.0) 262 (81.9) 10 (3.1) 32 (10) 320
*Fisher`s Exact Test
ISCP UTA’45 Jakarta 2022 - International Seminar and Call for Paper Universitas 17 Agustus 1945 Jakarta
194
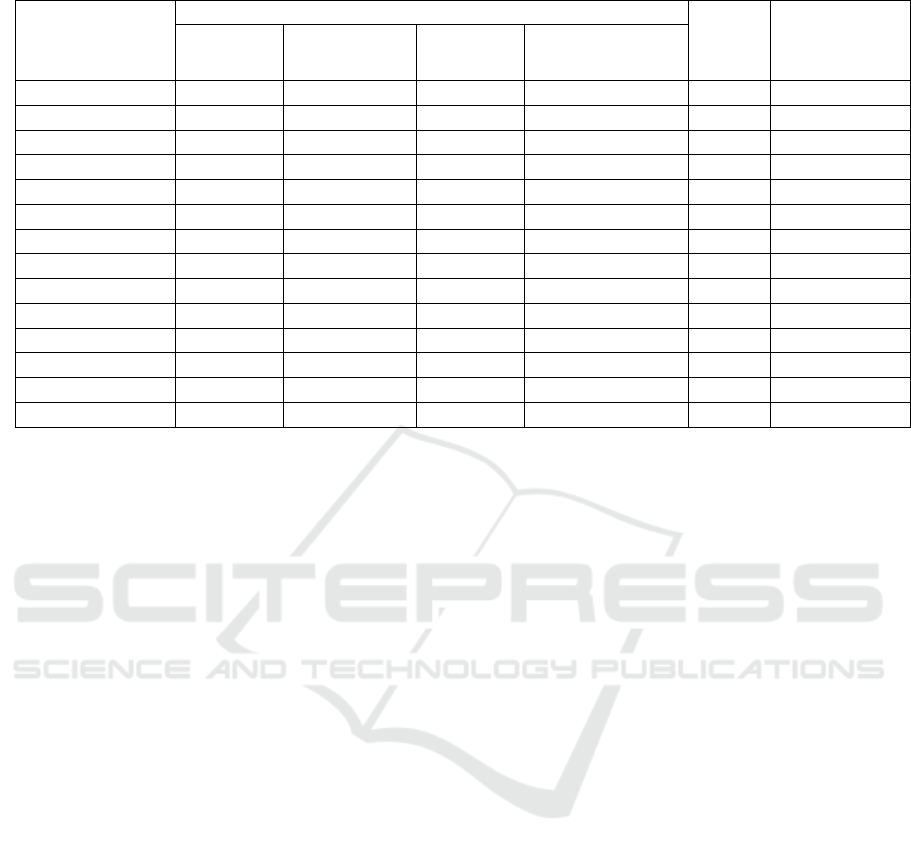
Table 2: Correlation Severity and Laboratory data.
Facto
r
Severit
y
Total Sig.
(P-Value)*
Mild
n (%)
Moderate
n (%)
Severe
n (%)
Critical illness
n (%)
ESR 16 (5) 262 (82) 10 (3) 32 (10) 320 0.870
Hb 16 (5) 262 (82) 10 (3) 32 (10) 320 0.952
RBC 16 (5) 262 (82) 10 (3) 32 (10) 320 0.601
WBC 16 (5) 262 (82) 10 (3) 32 (10) 320 0.001
Hematocrit 16 (5) 262 (82) 10 (3) 32 (10) 320 0.894
Platelets 16 (5) 261 (82) 10 (3) 32 (10) 319 0.006
MCV 16 (5) 262 (82) 10 (3) 32 (10) 320 0.782
MCH 16 (5) 262 (82) 10 (3) 32 (10) 320 0.914
MCHC 16 (5) 262 (82) 10 (3) 32 (10) 320 0.811
Kaliu
m
13 (4.4) 245 (82.4) 10 (3.4) 29 (9.8) 297 0.052
Natriu
m
13 (4.4) 245 (82.4) 10 (3.4) 29 (9.8) 297 0.212
Chloride 13 (4.4) 245 (82.4) 10 (3.4) 29 (9.8) 297 0.079
Urea 2 (2) 68 (75.8) 4 (4.4) 16 (17.8) 90 0.003
Creatinine 15 (5.4) 219 (81) 9 (3.3) 28 (10.3) 271 0.021
*Kruskal-Wallis Test
Platelets correlate with the severity of COVID-19
patiens (p=0.006) (table 2). According to the
guidelines for interpreting clinical data in Indonesia,
the normal value for platelets is 170-380. 103/mm3
(Kemenkes RI, 2011). Research by Dawood et al.,
2020, showed the occurrence of thrombocytosis in
6.26% of patients with a platelet count
>400,000/mm3 and thrombocytopenia in 5.36%
of patients with a platelet count <150,000/mm3 in
COVID-19 patients (Dawood et al., 2020).
Based on table 2, the highest creatinine in patients
with moderate severity was about 219 (80.8%), so
creatinine correlates with severity (p=0.021). Based
on the research of Cheng et al. (2020), 710 COVID-
19 patients were reported to have a prevalence of
15.5% increase in serum creatinine (Fadillah et al.,
2020)(Y. Cheng et al., 2020).
According to a study by Brian et al., creatinine
clearance values are determined by measuring the
concentration of endogenous creatinine (produced in
the body) in plasma and urine. The reference range
for men is generally in the range of 97-137 ml/min
and for women, 88-128 ml/min (Vesselaldo &
Ramatillah, 2022)(Nankivell, 2001). According to the
guidelines for interpretation of clinical data in
Indonesia, normal creatinine is 0.6-1.3 mg/dL
(Kemenkes RI, 2011).
Based on table 2, urea correlated with severity
(p=0.003). According to the guidelines for
interpreting clinical data in Indonesia, the normal
urea value in adult women is 6-21 mg/dL and adult
men, 8-24 mg/dL (Kemenkes RI, 2011). Blood urea
nitrogen (BUN) is the final nitrogen product of
protein metabolism and has been observed to be
associated with mortality from a variety of diseases
(Cheng et al., 2020). BUN is a surrogate marker that
predicts persistent organ failure after 48 hours of
hospitalization, in addition to its role in assessing
renal function (Cheng et al., 2020).
4 CONCLUSIONS
This study shows that there was a significant
correlation between laboratory data from leukocytes,
platelets, urea, and creatinine with the severity of
COVID-19 patients (P-value <0.05).
REFERENCES
Brodin, P. (2021). Immune determinants of COVID-19
disease presentation and severity. Nature Medicine,
27(1), 28–33. https://doi.org/10.1038/s41591-020-
01202-8
Chen, W., Zheng, K. I., Liu, S., Yan, Z., Xu, C., & Qiao, Z.
(2020). Plasma CRP level is positively associated with
the severity of COVID-19. Annals of Clinical
Microbiology and Antimicrobials, 19, 1–7.
https://doi.org/10.1186/s12941-020-00362-2
Cheng, A., Hu, L., Wang, Y., Huang, L., Zhao, L., Zhang,
C., … Liu, Q. (2020). Diagnostic performance of initial
blood urea nitrogen combined with D-dimer levels for
predicting in-hospital mortality in COVID- 19 patients.
Evaluation of Correlation Between Severity and Laboratory Data for COVID-19 Patients at Jakarta Private Hospital
195

International Journal of Antimicrobial Agents, 56(3).
https://doi.org/10.1016/j.ijantimicag.2020.106110
Cheng, Y., Luo, R., Wang, K., Zhang, M., Wang, Z., Dong,
L., … Xu, G. (2020). Kidney disease is associated with
in-hospital death of patients with COVID-19. Kidney
International, 97(5), 829–838.
https://doi.org/10.1016/j.kint.2020.03.005
Dawood, Q., Al-Hashim, Z., Al Hijaj, B. A., Jaber, R., &
Khalaf, A. (2020). Study of hematological parameters
in patients with coronavirus disease 2019 in Basra.
Iraqi Journal of Hematology, 9(2), 160.
https://doi.org/10.4103/ijh.ijh_49_20
Fadillah, R., Nasrul, E., & Prihandani, T. (2020). Research
Article Overview of Examination of SGOT, SGPT, and
Urea levels, 10(2).
Goudouris, E. S. (2021). Laboratory diagnosis of COVID-
19. Jornal de Pediatria, 97(1), 7–12.
https://doi.org/10.1016/j.jped.2020.08.001
Hocková, B., Riad, A., Valky, J., Šulajová, Z., Stebel, A.,
Slávik, R., … Klugar, M. (2021). Oral complications of
ICU patients with COVID-19: Case-series and review
of two hundred ten cases. Journal of Clinical Medicine,
10(4), 1–
13. https://doi.org/10.3390/jcm10040581
Indonesia, D. J. P. dan P. P. K. K. R. (2021). Guidelines for
the Prevention and Control of Coronavirus Disease
(COVID-19), March 2020. Retrieved from
https://www.kemkes.go.id/resources/download/info-
terkini/COVID-Universitas Sumatera Utara 119 19
dokumen resmi/2 Pedoman Pencegahan dan P
engendalian Coronavirus Disease (COVID-19).pdf
Kemenkes RI. (2011). Clinical Data Interpretation
Guidelines. Kementrian Kesehatan RI, (January), 1–
83.
Michael & Ramatillah. (2022). TREATMENT PROFILE
AND SURVIVAL ANALYSIS ACUTE
RESPIRATORY DISTRESS SYNDROME (ARDS)
COVID-19 PATIENTS. International Journal of
Applied Pharmaceutics, 14(2), 54–56.
https://doi.org/10.22159/ijap.2022.v14s2.44750
Nankivell, B. J. (2001). Creatinine clearance and the
assessment of renal function. Australian Prescriber,
24(1), 15–
17. https://doi.org/10.18773/austprescr.2001.009
Vesselaldo, M., & Ramatillah, D. L. (2022).
EVALUATION OF BMI RELATIONSHIP WITH
INCREASED D-DIMER IN COVID-19 PATIENTS
AT A JAKARTA PRIVATE HOSPITAL, 14(2), 1– 5.
https://doi.org/https://dx.doi.org/10.22159/ijap.2022.v
14s2..
WHO. (2020). Naming the Coronavirus disease (COVID-
19) and the virus that causes it. Coronavirus disease
2019: Technical guidance. Retrieved from
https://www.who.int/emergencies/diseases/novel-
coronavirus-2019/technical-guidance/naming-the-
coronavirus-disease-(covid-2019)- and-the-virus- that-
causes-it
Worldometers. (2022). Coronavirus Pandemic. Retrieved
fromhttps://www.worldometers.info/coronavirus/count
ry/indonesia/
ISCP UTA’45 Jakarta 2022 - International Seminar and Call for Paper Universitas 17 Agustus 1945 Jakarta
196
