
Social Security for People Affected by Drug-Resistant TB
Ninik Annisa
1
, Ahmad Imam Mujaddid Rais
2
, Dena Sundari Alief
3
, Deni Wahyudi Kurniawan
4
,
Uga Pratama Gunawan
5
, Indro Laksono
6
and Nurliyanti
6
1
Central Board of ‘Aisyiyah, Jakarta, Indonesia
2
Bureau for International Relation and Cooperation International Relations, Central Board of Muhammadiyah,
Jakarta, Indonesia
3
Magister Student on Social Welfare at the University of Indonesia, Jakarta, Indonesia
4
Faculty of Health Sciences, Muhammadiyah University of Prof. Dr. Hamka, Jakarta, Indonesia
5
Department of Social Welfare Pasundan University, Bandung, Indonesia
6
Stop TB Partnership Indonesia, Jakarta, Indonesia
uga.pratama111194@gmail.com, indro.l@stoptbindonesia.org, nurliyanti@stoptbindonesia.org
Keywords: Social Security, Drug Resistance TB.
Abstract: The high incidence of Drug Resistance Tuberculosis (DR TB) and the low number of people with DR TB
who get treatment shows that the prevention of DR TB in Indonesia requires serious attention. Need about 24
months for treatment and healing and requires huge financing and adherence. Although the government has
facilitated treatment for people affected by DR TB through National Health Insurance (JKN), and enabler
support from the TB Control program funded by the Global Fund, however not all people with DR TB
received that assistance. This study focuses on examining the importance of social security for people with
DR TB and analyzing the adequacy of policies so that social security can be implemented for people with DR
TB. This study finds that DR TB is a catastrophic disease that brings about poverty to patients with multi-
dimension impacts including physiological, psychological, social, and economic. The integration of DR TB
into social security is feasible in Indonesia. Finally, this study looks at the issuance of Presidential Decree No.
67 in the year 2021 about TB control becoming a very strong base for the integration of TB-affected people
into social protection programs.
1 INTRODUCTION
Currently, Indonesia is ranked third in the world with
the most TB cases in the world after India and China.
According to the Global TB Report 2021 data, the
estimated TB cases in Indonesia are 824,000, but
notifications currently only reach 443,235 (53.79%)
cases per year. Of the number that was notified, 8,268
(1.86%) of them confirmed TBC RO.
The spread of TB RO is a challenge, the data on
the Indonesian TB enrollment rate or the number of
people starting TB treatment for TB is only around
45%. There are still around 55% (1,819) of people
with TB RO who do not get treatment and have the
potential to infect others around them (Ministry of
Health, 2022).
The government has borne the direct medical
costs of TB RO treatment (direct medical costs)
through the National Health Insurance (JKN).
However, in practice in certain conditions and areas,
people with RO TB need to spend money on other
costs such as radiology, laboratory tests, and anti-TB
RO drugs (if they are found to be out of stock at the
health facilities). In addition, people affected by TB
RO currently receive enabler fees, from the TB
control program funded by the Global Fund, to
address direct non-medical costs such as
transportation costs. However, in its implementation,
not everyone affected by TB RO has received this
enabler fund (STPI, 2022).
Likewise, some people affected by TB RO have
also received social security schemes such as PKH
(Program Keluarga Harapan), Basic Food Assistance,
assistance from local governments, and others.
However, the allocation of the social security scheme
is not specific, partial, and incidental (the scheme is
not clear), and only considers the condition of
poverty. Therefore, the government needs to provide
social security for people affected by TB RO by
180
Annisa, N., Rais, A., Alief, D., Kurniawan, D., Gunawan, U., Laksono, I. and Nurlianti, .
Social Security for People Affected by Drug-Resistant TB.
DOI: 10.5220/0011662200003608
In Proceedings of the 4th International Conference on Social Determinants of Health (ICSDH 2022), pages 180-185
ISBN: 978-989-758-621-7; ISSN: 2975-8297
Copyright
c
2023 by SCITEPRESS – Science and Technology Publications, Lda. Under CC license (CC BY-NC-ND 4.0)
compiling rules and mechanisms as well as better
monitored implementation. One of the social security
programs for people with TB RO is the CCT model;
namely a conditional cash transfer program aimed at
poor households, by requiring these households to
make long-term investments in Human Resources
(HR) such as improving education, health, and
improving nutrition. This program is noted as an
important component of social protection systems
and poverty reduction in many countries, especially
developing countries (World Bank, 2009). The CCT
model is considered relevant in TB RO to help TB RO
patients increase family income to prevent
catastrophic costs. In addition, because the CCT
approach requires conditionality adherence to
treatment for TB RO patients can be monitored.
Previous research conducted by Fuady (2018),
Estro (2021), and WHO (2022) showed catastrophic
costs faced by TB RO sufferers. However, there is a
research gap in aspects that analyze the condition of
people affected by TB RO, available social security
policies, and the urgency of implementing social
security. Based on these things, STPI conducted a
study on Social Security for People Affected by TB
RO which aims to see a description of the condition
of people affected by TB RO including the needs and
constraints experienced, as well as analyzing policy
opportunities that exist in Indonesia regarding the
urgency of social security for affected people. TB
RO. With the presence of policies that are more
supportive of TB RO, it is hoped that the recovery of
people affected by TB RO will increase to achieve TB
elimination in Indonesia.
2 METHODOLOGIES
This research was conducted using a mixed method
with a convergent parallel design (that is, the use of
quantitative and qualitative research at the same time
or phase) to answer the formulation of the research
problem. The methods used include literature review,
surveys, interviews with people with TB RO and TBC
RO stakeholders both from government agencies and
CSOs, FGDs with TB stakeholders from government
agencies and CSOs, policy analysis, and mapping of
key stakeholders.
Sampling in the survey was determined by the
purposive sampling method with criteria for people
affected by TB RO who had started second-line
treatment and were in 10 areas (North Sumatra, South
Sumatra, Lampung, DKI Jakarta, Banten, West Java,
Central Java, DI Yogyakarta, East Java, and South
Sulawesi) assisted by PR of the STPI Penabulu
Community Consortium. The survey was conducted
by Case Managers as enumerators of 332 people with
TB RO which was conducted in the period December
2021 to February 2022.
3 DISCUSSIONS
3.1 Multidimensional Impact on People
with TB RO
Physical impact. People with TB RO who undergo
treatment for 9-20 months with a very large number
of treatment regimens will experience several side
effects, such as dizziness/headache, chest pain,
diarrhea, muscle and bone pain, nausea to vomiting,
and tingling (Ministry of Health, 2020). ). All these
side effects then have implications for suffering and a
sense of helplessness that is inevitable for patients
(STPI, 2022).
Psychological impacts for people with TB RO
include excessive anxiety, stress, and even
depression. In some cases, people with TB RO
experience hallucinations and attempt suicide
(Ministry of Health, 2020). Social impact. Exclusion
from family and environment and even being
expelled from work or quitting school is not
uncommon for them to experience (Morris, 2013).
People with TB RO often get stigma internal (feeling
inferior) and external (other people). Not
infrequently, external stigma also comes from health
workers (STPI, 2022).
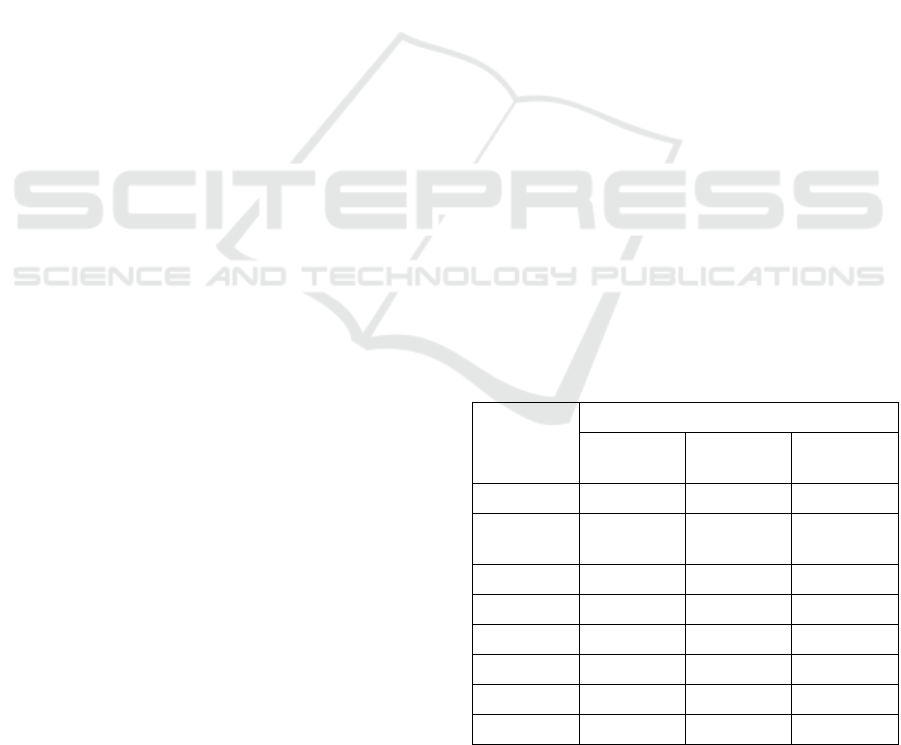
Table 1: Income Levels and Respondents' Status by
Participation in PKH.
Income
Level
Status in PKH Program
Not
Participant
Participant Total
<Rp 500K
53 (16%) 18 (5%) 71 (21%)
Rp 500K –
1M
22 (7%) 16 (5%) 38 (11%)
Rp 1 – 2M 52 (16%) 21 (6%) 73 (22%)
Rp 2 – 3M 65 (20%) 13 (4%) 78 (23%)
Rp 3 – 4M 30 (9%) 5 (2%) 35 (11%)
Rp 4 – 5M 23 (7%) 2 (1%) 25 (8%)
> Rp 5M 12 (4%) 0 (0%) 12 (4%)
Total 257 (77%) 75 (23%) 332 (100%)
K=thousands, M=Million
Financial impact. For the sake of recovery treatment,
it is not uncommon for people with TB RO to have to
Social Security for People Affected by Drug-Resistant TB
181
bear direct non-medical costs such as transportation
costs and consumption during treatment; indirect
costs, namely the loss of productive time which
results in income loss (Ahmad, et al. 2021).
Compared to the needs of people with TB RO, the
assistance received are still Limited.
The STPI study found that most of the
respondents were poor families with an income of
fewer than 2 million rupiahs (54%) and vulnerable
poor families with an income below 3 million rupiahs
(23%).
In terms of household expenditure, STPI's
research also found that 79% of household
respondents affected by TB RO bear expenses that
exceed their monthly income where the average
household expenditure is between 1-4 million per
month with four family members.
This high expenditure creates a catastrophic
burden on the families of people with TB RO. Table
of Income Levels and Respondents' Status by
Participation in PKH.
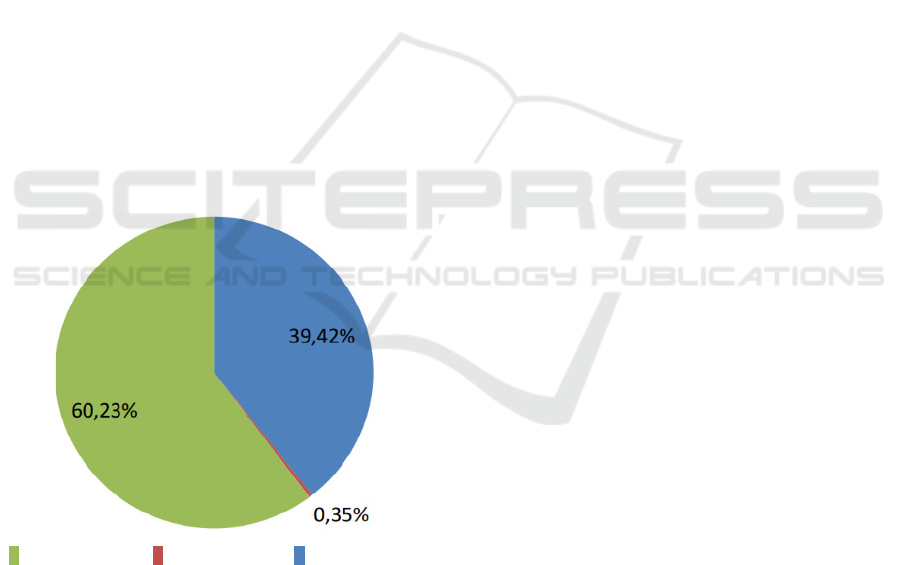
Another study by Estro et.al (2021) showed that
81% of people affected by TB RO experienced
catastrophic discharge. The largest proportion of
expenses for people with TB RO are indirect costs or
lost income/jobs (60.23%), followed by non-medical
costs (39.42%) and the lowest is medical costs
(0.35%).
Indirect
cost/lost
income
Total medical
cost
Total non-
medical cost
Figure 1: The proportion of total medical expenses, non-
medical costs, and indirect costs
STPI's research also found that several social
security mechanisms have been received by people
with TB RO, including assistance for treatment and
living expenses with different schemes.
Most of these aids were provided through
government channels. However, this social security
assistance is still provided with various, uneven and
non-specific frequencies targeting people affected by
TB RO. One of them, from the STPI study, showed
that only 23% of TB RO respondents received the
PKH program, whereas 77% of respondents earned
less than 3 million rupiahs (STPI, 2022). Even 21%
of them live with an income of less than 500 thousand
per month. Many respondents are eligible to receive
assistance from the PKH program but are not served
by this program.
This situation shows that the provision of social
assistance for people affected by TB RO is still based
on poverty data, not their health status. People
affected by TB RO have a vulnerability to being poor
due to the catastrophic conditions they experience.
Thus, the scope of providing social support received
by TB RO patients is very limited.
3.2 Existing Social Security Has Not
Specifically Targeted People
Affected by TB RO Even Though
the Policy Basis Already Exists
3.2.1 Title
Of the government's social security programs that
have the potential to support the needs and success of
treatment for TB RO patients, none specifically
targets people affected by TB RO as recipients. Until
now, the government has at least 25 social security
programs, with 5 programs that have the potential to
support the fulfillment of the treatment needs of
people affected by TB RO. Social security programs
that have the potential to support TB RO patients are
the Healthy Indonesia Program (Healthy Indonesia
Card/BPJS Kesehatan), PKH, the Basic Food
Program, the Social Entrepreneurship Program
(ProKus), and the Social Rehabilitation of
Uninhabitable Homes (RS-RTLH).
People affected by TB were once a health
component in the Family Hope Program at the end of
2020 based on the Decree of the Director General of
Social Protection and Security, Ministry of Social
Affairs. However, the policy was later discontinued
due to the lack of a strong legal basis and studies for
its implementation.
Based on the National TB Elimination Strategy,
the integration of programs to support people affected
by TB should be a concern because it encourages the
strengthening of commitment and leadership at all
levels of government through the provision of
adequate budgets for TB control (Article 5 paragraph
2 (a) and Article 7 point b ). The Central Government,
Regional Government, and non-government are also
ICSDH 2022 - The International Conference on Social Determinants of Health
182

asked to ensure the mitigation of psychological,
social, and economic support for the continuation of
treatment until completion [Article 12 paragraph
8(b)], one of which is by providing health insurance
and social protection [Article 24 Paragraph 3 (a) )].
Further Presidential Regulation No. 67 of 2021
concerning the Prevention of Tuberculosis is an
opportunity and momentum to encourage the
provision of social security for people with TB RO.
As stated in Chapter IV Article 24 Paragraph 1 it is
stated that in the implementation of TB control, the
Central Government is responsible for mitigating the
psychosocial and economic impacts faced by people
affected by TB and their families (point d) and
carrying out social protection and empowerment
efforts for people affected by TB and the community.
affected by tuberculosis (point e).
The Roadmap for the Elimination of Tuberculosis
in Indonesia 2020-2030 by the Ministry of Health
targets a reduction in the incidence of TB by 2030
using 6 strategies and interventions. Specifically, by
optimizing the supporting procedures for the
diagnosis and treatment of Drug Sensitive
Tuberculosis (TB SO) and TB RO in an integrated
manner by increasing psychosocial and economic
support for people affected by tuberculosis, including
ensuring justice in work (at point 2.3) and
strengthening the financing system for tuberculosis
(point 2). 6.3). The strategies and policies above
clearly support the availability of social security for
people with TB RO.
3.3 Lack of Synergy between Ministries
and Institutions in Combating TB
RO and Integration of Social
Security
The government's initiative to provide social security
for people affected by TB RO is still constrained. In
the regulatory aspect, there is no specific
nomenclature for people affected by TB RO as
beneficiaries of social security. In the context of its
application, social security for people with TB RO
requires complex data integration.
Judging from the opportunities, synergies across
key ministries (Ministry of Health and Ministry of
Social Affairs) for social security for people affected
by TB RO are already open. From the aspect of data
availability, at least each of these ministries already
has a database (SITB/Tuberculosis Information
System and DTKS/Social Welfare Integrated Data)
so they only need to integrate and regulate technical
matters and management mechanisms. From the
aspect of the regulatory base for synergies between
ministries and institutions in TB control, there has
also been legal strengthening, namely Presidential
Regulation no. 67 of 2021 concerning the Prevention
of Tuberculosis. Even in the Presidential Regulation,
it has also been mandated to both central and regional
governments to mitigate the psychosocial and
economic impacts faced by TB patients and their
families.
In addition, the National Tuberculosis Strategy
document 2020-2024 states that one of the
interventions that need to be carried out is multi-
stakeholder and cross-program collaboration to
increase the number of people with TB RO who start
treatment, including through financial protection for
people affected by TB by integrating psychosocial
and social security systems. the economy of people
affected by TB RO into protection schemes in other
ministries such as programs at the Ministry of Social
Affairs.
3.4 CCT as a Social Security Model for
People Affected by TB RO
The provision of social security is a solution to
mitigate the psychosocial and economic burdens that
must be borne by people affected by TB RO and their
families. A modeling analysis conducted by Carter
(2018), shows that the global incidence of TB will
decrease by 84.3% if poverty is eliminated and all
individuals are enrolled in social protection programs,
while if only social protection is applied, TB cases
will decrease by 76.1%. Oliosi (2019) concluded that
TB patients who are integrated into the social security
or protection system have an 88% greater chance of
recovering compared to TB patients who do not have
a social security program.
Several countries have succeeded in reducing the
catastrophic burden as well as having a positive
impact on reducing TB morbidity through policies
and implementation of providing social security for
people with TB RO. Among these countries are
Brazil, India, Argentina, and South Africa. The model
of providing social security for people with
tuberculosis that has been implemented in these
countries is based on CCT, namely a conditional cash
transfer program. CCT beneficiaries are bound by an
agreement made together to support the smooth
process of treatment until recovery. Indonesia
adopted a CCT-based social security program in 2007
namely PKH. PKH participants or recipients are
eligible, that is, they are categorized as poor and
vulnerable families. The program is also an entry
point for other social assistance programs for
beneficiary families. However, the drawback of PKH
is that it is distributed every three months, and is
Social Security for People Affected by Drug-Resistant TB
183

considered quite long by people with TB RO.
Therefore, the application of social security support
to people affected by TB RO is very important
considering the duration of the distribution of aid.
4 CONCLUSIONS
From the studies that have been conducted, it can be
concluded that:
Drug-resistant TB is a disease with a multi-
dimensional impact and has a catastrophic cost.
The support needed by people affected by TB RO
consists of medical support, non-medical support,
and indirect costs.
The policy basis for the implementation of social
security support for people affected by TB RO
already exists, namely Presidential Regulation
No. 67 the year 2021
The challenge lies in lowering policy and
implementation because it involves cross-
Ministry/Agency
The model of providing support can be in the form
of Conditional Cash Transfer (CCT) because it is
proven to be able to anticipate poverty while
increasing the recovery of TB patients.
5 RECOMMENDATIONS
By understanding and exploring the importance of
comprehensive support and assistance for TBC RO,
seeing the existence of policy gaps on the one hand
and on the other hand opening up policy opportunities
to fulfill the needs of TBC RO. Several things are
recommended from this study to fill opportunities for
the creation of better policy spaces and research
developments in the future, this study recommends
the following:
5.1 Recommendations for the
Government
(1) It is urgent to develop a policy that provides social
security support for people affected by TB RO.
Considering that TB RO is a condition that
impoverishes the economy of the affected people
and their families, and reduces the productivity
and quality of society and the nation at large. The
treatment period for TB RO is 24 months, which
is a very difficult challenge both in terms of time
and the side effects of the drugs experienced. The
impact is felt both by people with TB RO and their
families. With the integration of social security for
people affected by TB RO, it is hoped that they
will be able to ease their socio-economic burden,
support assistance and supervision of treatment to
complete and recover, change the behavior of
people affected by TB RO to be healthier until the
2030 TB elimination target is achieved.
(2) Policies that will come later can be following
needs and strategies based on their conditionality
and TB elimination targets.
(3) Supporting the government to integrate people
affected by TB RO as one of the recipients of the
Family Hope Program (PKH) as a relevant and
appropriate CCT-based social security program to
support the treatment process until they recover.
(4) Encouraging the government to immediately
follow up Presidential Regulation No. 67 of 2021
concerning TB Control into the Technical
Guidelines/Juknis so that it can be immediately
used by Ministries, Institutions, and local
governments.
(5) The policy on social security for people affected
by TB RO can be in the form of a Joint Regulation
of the Minister of Social Affairs and the Minister
of Health or a Regulation of the Coordinating
Ministry for Human Development and Culture.
5.2 Recommendations for the
Academics
(1) Encouraging studies and research, evaluation,
and learning on social security and protection
programs that have been carried out by the
government, both in terms of effectiveness, the
efficiency of governance, as well as the impact
on target groups and accountability and
accountability.
(2) Increase research on social security that covers
the needs and protection of people affected by
TB.
(3) Encourage studies related to social protection
and social welfare with a comprehensive
approach.
ACKNOWLEDGEMENTS
Thank you to Stop TB Partnership Indonesia for
supporting this study.
ICSDH 2022 - The International Conference on Social Determinants of Health
184

REFERENCES
Ahmad, Riris Andono, et al. (2021). Indonesia National TB
Patient Cost Survey 2020. UGM: Yogyakarta
Carter, Daniel J., et.al., (2018). The impact of a cash
transfer program on tuberculosis treatment success
rate: a quasi-experimental study in Brazil. BMJ Global
Health: doi:10.1136/bmjgh-2018-001029
Estro DS, Donny H, Nurul DN., Stop TB Partnership
Indonesia (2021). Laporan Kajian biaya katastropik
dan kemiskinan bagi orang terdampak TBC RO.
Kementerian Kesehatan Republik Indonesia. (2020).
Strategi Nasional Penanggulangan Tuberkulosis di
Indonesia 2020-2024.
Kementerian Kesehatan Republik Indonesia. (2020).
Buletin Eliminasi Tuberkulosis Vol.1 https://tbind
onesia.or.id/wp-content/uploads/2020/11/Buletin-TBC
-Vol-1-Tahun-2020-Final.pdf.
Morris MD, Quezada L, Bhat P, Moser K, Smith J, Perez
H, Laniado-Laborin R, Estrada-Guzman J, Rodwell
TC. Social, economic, and psychological impacts of
MDR-TB treatment in Tijuana, Mexico: a patient's
perspective. Int J Tuberc Lung Dis. 2013 Jul;17(7):954-
60. doi: 10.5588/ijtld.12.0480. PMID: 23743315;
PMCID: PMC3769163.
Ninik A, et. al., Stop TB Partnership Indonesia (2022).
Laporan Penelitian Jaminan Sosial bagi Orang
Terdampak TBC RO.
Oliosi, J.G.N., et.al., (2019). Effect of the Bolsa Familia
Programme on the outcome of tuberculosis treatment:
a prospective cohort study. Lancet Global Health.
http://dx.doi.org/10.1016/S2214-109X(18)30478-9
Social Security for People Affected by Drug-Resistant TB
185
