
Remote Patient Monitoring Systems based on Conversational Agents for
Health Data Collection
Pedro Dias
1,2 a
, Miguel Cardoso
1 b
, Federico Guede-Fernandez
1 c
, Ana Martins
1 d
and Ana Londral
1,2 e
1
Value for Health CoLAB, Lisboa, Portugal
2
Comprehensive Health Research Center, Nova Medical School, Nova University of Lisbon, Lisboa, Portugal
Keywords:
Healthcare, Chatbot, Conversational Agents, Cardio-thoracic Surgery, Hypocoagulability, Telemonitorization,
Patient-reported Outcomes.
Abstract:
The pursue of digital health has been increasing in the past years and the COVID-19 pandemic promoted it fur-
ther. Remote monitoring health care allows patients to report health outcomes and receive a proper follow-up
from home and personalized health care by preventing unnecessary trips to hospitals. The design, development
and use of two rule-based chatbots for data collection and guidance providing in two health telemonitoring
contexts, post-cardiothoracic surgery for derived-complications control and patients with hypocoagulation, is
described in this paper. The designed chatbots have the goal of being simple, modular and human guided.
The first chatbot was used to collect photos from the surgical wound and the second was used to collect the
INR value (from a coagulometer) and six related questions, following a measurement plan. In both use cases
the clinical team could analyze the collected data and interact with patients using a web application. This
chatbot may contribute to the increase of the safety perception of the patient and their engagement with their
health status. The inclusion of the clinical team in the development was key to identify the requirements and
to improve the user experience.
1 INTRODUCTION
The pursue of digital health increased during the past
years and the COVID-19 pandemic promoted it fur-
ther. Preventing unnecessary trips to hospitals by con-
stantly monitoring patients through Internet of Things
(IoT) devices, mobile apps, or simply through mes-
sages shows promising results. Severe acute respi-
ratory syndrome corona-virus 2 (SARS-CoV-2) is a
highly contagious corona-virus which has put at risk
human health since 2019. Due to its high conta-
gious rate and severity, it spread all over the world
and caused difficult prognosis or even death to elderly
individuals and individuals with non-communicable
diseases (NCDs) (P
´
ecout et al., 2021). NCDs are
long-term and in some cases life-long pathologies and
include cardiovascular diseases, cancer, chronic respi-
a
https://orcid.org/0000-0002-8875-2228
b
https://orcid.org/0000-0002-6290-9098
c
https://orcid.org/0000-0003-2762-0333
d
https://orcid.org/0000-0002-4890-3941
e
https://orcid.org/0000-0002-8002-6790
ratory diseases, diabetes and neurological disorders.
Patients living with NCDs require constant care to
delay disease progression. This leads to both health
and economic consequences due to the growing age
of the worldwide population (Vandenberghe and Al-
brecht, 2020). During the pandemics, patients have
been avoiding hospitals to prevent contagion which
might lead to an increased disease severity and higher
costs to the healthcare system (Kardas et al., 2021).
Remote monitoring healthcare allows patients to
receive a proper follow-up from home and personal-
ized health care, which has been revealed especially
important since the Covid-19 outbreak (Mantena and
Keshavjee, 2021). In the healthcare context, IoT-
enabled devices can be defined as any device, includ-
ing computers, mobile phones, and wearable sensors
that may allow data collection, transfer and storage.
These devices can be used to monitor patients’ symp-
toms in real time (Mamdiwar et al., 2021). Point-
of-care (POC) testing devices are particularly useful
during telemonitorization because relevant parame-
ters can be measured and reported from home. In
the case of people on long-term oral anticoagulation,
812
Dias, P., Cardoso, M., Guede-Fernandez, F., Martins, A. and Londral, A.
Remote Patient Monitoring Systems based on Conversational Agents for Health Data Collection.
DOI: 10.5220/0011011000003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 812-820
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

these tests can be used to measure the international
normalized ratio (INR) and adjust accordingly the
medication dose (Heneghan et al., 2016).
Conversational agents (CAs) are software tools
that mimic a human-like entity during a conversation
using, text, voice, images or a mixture of all (Laranjo
et al., 2018). CAs are usually deployed on messag-
ing apps, websites or mobile-phone applications, as
well as multimodal platforms. They have been used
in a wide range of domains such as customer service,
technical support, marketing, education and health-
care. Several authors have demonstrated that humans
tend to attribute human-like attributes to non-human
agents. Due to this trait about human-machine inter-
action, CAs are perceived as social interaction part-
ners, capable of establishing a meaningful relation-
ship (Bickmore and Cassell, 2001; Epley et al., 2007).
Therefore, a CA can be perceived by the patient as a
health counselor that is available to provide continu-
ous guidance. This continued support can be given by
providing reminders or information about medication
or treatment plan, assisting on self-monitoring tasks,
or by interacting with healthcare professionals report-
ing the results of monitorization.
POC testing alone can be used to do self-
monitoring and self-management. In this case, the
patient is responsible for managing her/his treatment
plan and does not have a proper feedback about
her/his recovery. IoT have changed this paradigm by
allowing healthcare professionals to monitor in real-
time the state of the patient and intervene if there is an
abnormality, which increases patient’s safety. A CA
interacts directly with the patient and can be used to
increase the patient’s literacy, help managing medica-
tion doses and treatment based on the patient’s mea-
surements and prognosis. A system that integrates
all of these technologies might promote patient’s self-
care.
The aim of the present study is to demonstrate
the applicability of ruled-based chatbots on two dif-
ferent clinical follow-up services: post-cardiothoracic
surgery and patients with hypocoagulation. In both
cases, a telemonitoring system capable of collecting
and reporting data and provide support to the patient
was developed. The principles followed to design
both chatbots as well as the technology used to de-
velop them are described in Section 3. The applica-
tion, data collection procedure, implementation and
results for each chatbot are further explained in Sec-
tion 4.2 and 4.3. In Section 6, conclusions and future
work are presented.
2 STATE OF THE ART
In 1966, the first rule-based chatbot was developed
by Joseph Weizenbaum at MIT Intelligence labora-
tory and it was named ELIZA. ELIZA was designed
to mimic a patient-centered Rogerian psychotherapist
and answer based on the identification of keywords
in a sentence using pattern matching (Weizenbaum,
1966). In 1972, PARRY was developed by psychia-
trist Kenneth Colby to simulate the behavior of a pa-
tient with schizophrenia (Colby et al., 1971). Psyx-
pert was an expert on disease diagnosis developed in
1987 and used to aid psychiatrists in diagnosing psy-
chotic disorders (Overby, 1987). SESAM-DIABETE
was developed in 1989 to be an interactive educa-
tional expert and provide support to insulin-requiring
diabetic patients by giving personalised guidance and
therapeutic support (Levy et al., 1989). In 1995, AL-
ICE (Artificial Linguistic Internet Computer Entity)
was the first computer program to use Natural Lan-
guage Process (NLP) to interpret user input (Wallace,
2009).
Nowadays, CAs can be delivered using smart-
phone, web or computer-based apps (Chaix et al.,
2019; Denecke et al., 2018; Kamita et al., 2019),
smartphone embedded software (Griol and Callejas,
2016) or any other messaging app, such as Telegram
or Facebook Messenger (van Heerden et al., 2017;
Fitzpatrick et al., 2017; Casas et al., 2018). It was
shown that the use of apps that need to be regularly
updated leads to high dropout rates and non-usage
(Lee et al., 2018). Messaging applications are the
preferable mean to convey a conversation since most
of the population is used to use them in the daily life
(Tudor Car et al., 2020).
In healthcare, CAs have been used as a mean of
conveying information between healthcare providers
and patients. CAs have been applied to many health
care sectors such as mental health (Vaidyam et al.,
2019; Luo et al., 2021), physical activity (Schachner
et al., 2020), HIV prevention (Marcus et al., 2020),
oncology (Abd-Alrazaq et al., 2021), nutritional dis-
orders (Pereira and D
´
ıaz, 2019), neurological disor-
ders (Pereira and D
´
ıaz, 2019) and chronic diseases
(Schachner et al., 2020; B
´
erub
´
e et al., 2021).
Personal patient data and data collected during a
conversation that might change the patient behavior
can be used to customize the output messages and im-
prove the user experience (Abashev et al., 2017). Ad-
ditionally, in cases where the CA has medical knowl-
edge provided by a secure source, such as medical
databases, helpful context can be automatically gener-
ated through the CA which is particularly relevant for
educational chatbots (Bickmore et al., 2016). An ex-
Remote Patient Monitoring Systems based on Conversational Agents for Health Data Collection
813

ample of educational chatbot is the electronic medica-
tion management assistant (eMMA). eMMA was de-
veloped to empower patients by giving them the max-
imum information about their treatment. Reminders,
interactive medication plans with information about
each medicine and food interaction data are provided
to the user (Tschanz et al., 2018).
Human-like communicative behaviors that can
have positive effects on this therapeutic relationship
have been largely studied (Van Pinxteren et al., 2020).
Potts et al. (2021) studied the preferred human-like
characteristics that would be desired for a chatbot to
help support a mental health service. They found that
the desired chatbot would have a positive outlook, ac-
cessible for any person and be able to support while
recalling previous conversations (Potts et al., 2021).
During the interaction, CAs must endure a relation-
ship with the user. Moore et al. (2017) mentioned that
it is important to ensure that the user is engaged: (1)
the dialogue is tailored to match the user’s level of un-
derstanding, (2) interactions are simple and synthetic
and (3) rephrasing when the user does not understand
the message (Moore et al., 2017).
NCDs are hard to manage for patients recently di-
agnosed, who need to learn how to adapt their lives
and to this new normality. CAs were identified as im-
portant factors in mitigating knowledge gaps and as
supportive agents since a closer relationship between
the patient and the healthcare provider might be en-
dorsed and, additionally, might be used as a mean to
increase literacy and signalling high-risk situations by
monitoring vital parameters (Heneghan et al., 2016;
Guhl et al., 2020; Echeazarra et al., 2021; Bian et al.,
2020; de Pennington et al., 2021).
Long-term oral anti-coagulation monitorization
has been used to estimate the dosage of anticoagu-
lant given the international normalized ratio (INR)
test. At first, the patient would need to provide to
her/his healthcare provider the INR and accordingly
to its value the doctor or nurse would be responsi-
ble for choosing the right anti-coagulation dose. Self-
management would be required to trained patients. In
this case, given the INR test, they would be responsi-
ble for interpreting the results and adjusting the med-
ication (Heneghan et al., 2016). This was particularly
relevant on increasing medication adherence.
In 2020, a randomized controlled trial (RCT)
aimed on increasing the adherence to medication by
sending reminders and the quality of life of patients
with atrial fibrillation. An embodied CA was used
to improve communication, prevent hospital readmis-
sion, and educate patients. This study revealed im-
provements in patient’s quality of life, daily activity
and a self-reported adherence to anticoagulation ther-
apy (Guhl et al., 2020).
A RCT using a Telegram based chatbot assistant,
TensionBot, was performed to monitor patients with
high blood pressure (BP). Its main functionalities
are sending reminders to patients to ensure that BP
is measured, storing measurements and letting data
available to healthcare professional and, giving addi-
tional support about how to measure BP (Echeazarra
et al., 2021). This study revealed that patients using
this CA were able to improve their ability to properly
measure BP and diminish the paperwork for health-
care providers (Echeazarra et al., 2021).
A postoperative follow-up system of orthopedic
patients was performed in an exploratory quantita-
tive and qualitative study in 2020. This system was
based on a CA that would perform a series of ques-
tions through a cellphone call based on a template
given by the medical staff and patient’s personal data.
Patient’s responses would be processed using speech
recognition and spoken language understanding tech-
niques. This dialogue was about patient’s satisfaction
regarding the hospital service, health education and
wound recovery. Doctors and nurses would have ac-
cess to the feedback report and be able to intervene
when needed. They found that AI-assisted follow-up
could replace traditional follow-up (Bian et al., 2020).
In 2021, a proposal project that aimed to evalu-
ate the effectiveness, usability, and acceptability of
a CA named Dora. This conversation model would
integrate speech recognition and generation to per-
form telephone follow-up by asking questions regard-
ing patient’s recovery (de Pennington et al., 2021).
3 DESIGN OF CHATBOT
The designed chatbot can be categorized as a rule-
based task-oriented chatbot which has the goal of be-
ing clear, modular and human guided. Safi et al.
(2020) identified four stages that should be considered
during CA design to facilitate user engagement: text
understanding, dialog management, data management
and text generation (Safi et al., 2020). The design
of the proposed chatbot has considered the aforemen-
tioned four stages:
• Text understanding: it refers to the process of fig-
uring out what is the meaning or intention of the
user’s input. This process can be done by using
pattern matching (keyword or string matching) or
intelligent models using NLP or Machine Learn-
ing (ML) models (Safi et al., 2020). Some stud-
ies revealed the embryonic stage of NLP mod-
els in healthcare due to their lack of consistent
methodology and evaluation methods (Schachner
Scale-IT-up 2022 - Workshop on Scaling-Up Health-IT
814

et al., 2020). The proposed chatbot is used for
telemonitoring purposes and vital signs gathering,
thus it exists in a structured and organized context
which opposes to conversational agents that work
directly with free-text.
• Dialog management: it is the process of establish-
ing a link between user’s input and the CAs re-
sponse. This can be handled using finite, frame
or agent-based dialogue system. A finite-based
dialogue is a state transition network that can be
defined by a sequence of pre-determined interac-
tions between the user and the CA. In this case,
user’s dialogue is limited to a set of options and
the dialog flow is fixed. A frame-based dialogue
is characterized by a dialog flow determined by
the content of the user’s input and the CAs data.
The answer given by the user will be used to fill
the missing data from the task. Agent-based di-
alogue is defined as a dynamic dialogue between
two agents that have enough intelligence to pur-
sue a conversation based on reasoning and the
sequence of arguments discussed during the di-
alogue (McTear et al., 2016; Safi et al., 2020).
In this study, a finite-state dialogue machine was
developed to increase the simplicity of the inter-
action with the user while offering the necessary
modularity to give support during the follow-up.
• Data management: the proposed CA was de-
signed to collect patient’s data to generate a daily
report to the healthcare professional for further
analysis. Additionally, health-related information
is led available to users, in order to improve their
health literacy.
• Text generation: it is responsible for answering
the user. This answer can be fixed or generated
in case the output is built on top of intelligent
models that use NLP or DL (Safi et al., 2020).
Systems that give fixed responses can be tedious
and frustrating to the user due to their inflexi-
bility (Williams et al., 2018; Irfan et al., 2020).
Intelligent agent might increase user engagement
(Schumaker et al., 2007), the lack of robust eval-
uation methods together with the black box effect
related to machine learning models (Tudor Car
et al., 2020) might result in adverse consequences
to the patient (Laranjo et al., 2018). Therefore, the
text generation of the proposed chatbot is based on
pre-defined and fixed text.
That being said, following the proposed design we
implemented two distinct chatbots for two use cases
using Django, a Python-based framework as their
backbone and Twilio as the cloud communication
platform to send and receive text messages through
Short Message Service (SMS) and WhatsApp mes-
sages. What is more, to handle data management we
leverage the open-source database management sys-
tem PostgreSQL. Finally, to host both of our applica-
tions we use the platform as a service (PaaS) Heroku.
4 APPLICATIONS
In this section we will describe two applications de-
veloped under a multidisciplinar team of healthcare
professionals, engineers and linguists: CardioFollow
and HemoControlBot. These applications aimed at
improving the follow-up of post-surgery (CardioFol-
low) and patients with hypocoagulation (HemoCon-
trolBot) by giving them support and additional in-
formation. Both use cases had the objective of col-
lecting patient reported outcomes measures (PROM)
and to display this data on a web application to the
pertinent clinical staff (doctors and nurses), follow-
ing the human computer interaction principles. The
chatbot and the web application were developed in a
co-creation environment, meaning that the members
of the clinical staff had a pivotal role in their design
and improvement. The target population for both use
cases were patients that were recovering from a car-
diothoracic surgery. What is more, the chatbots im-
plemented for the introduced use cases leverage either
SMS or Whatsapp. In this section, we define the com-
mon web application that sustained both use cases,
specifying the details of each use case. Afterwards
we explain the functionality of each developed chat-
bot.
4.1 Clinical Team’s Web Application
The web application is the bridge that connects pa-
tients with the clinical team. Whilst patients inter-
act through the chatbot, the clinical staff monitors the
patients’ health closely through the developed appli-
cation. The application goal is to show patients data
through different formats and layouts which were de-
signed side by side with the clinical team - through
icons, tables and interactive graphics. The use of
icons allow a quick understanding of a patient’s health
status, namely changing colors according to specific
events - a sudden alteration in any collected measure
or value outside of a specified range. The graphics
were used to display the data overtime, giving the
clinical team the ability to compare the last reported
value with the previous ones.
A screenshot of the web application is depicted in
Fig. 1. This figure provides information regarding all
patients and offers an overview of their health status
Remote Patient Monitoring Systems based on Conversational Agents for Health Data Collection
815

with the goal of being easily readable to the clinical
team: all measurements are identified with a specific
icon and their values are displayed in the same rectan-
gle. When the values outbound the predefined healthy
range, the color will change to properly identify the
high-risk situations. Thus, allowing the clinical team
to prioritize the patients according to the number of
alerts.
Figure 1: List of telemonitored patients with the respective
outcomes and alerts. Measure that are outside of the normal
range are represented with the color yellow. The names of
the participants were hidden with a grey box.
Furthermore, the web application also has direct
access to the dialogues within the chatbot which can
be used for the clinical team to communicate directly
to the patient, through the developed web application.
4.2 CardioFollow
This chatbot was used in a pilot that consisted of the
telemonitoring of patients that underwent cardiotho-
racic surgery. Complications during surgery or hos-
pitalization are common (Crawford et al., 2017), but
risk also extends to the postoperative period, lead-
ing to hospital readmission of around 15-20% of pa-
tients during the first month and 30% in the first year
(Efthymiou and O’Regan, 2011; McElroy et al., 2016;
Khoury et al., 2020). This pilot had the participation
of 35 patients so far, as depicted in Table 1. These
patients, after the hospital discharge, were telemoni-
tored for 1 month.
Table 1: Overview of both use cases. TD - Telemonitoring
Duration; PTP - Previously Telemonitored Patients; PTF -
Patients to be Telemonitored in the Future.
Use Case TD PTP PCT PTF
CardioFollow 1 month 35 0 150
HemoControlBot 6 months 0 1 29
During this period, the patients had a daily rou-
tine where they would report their blood pressure,
weight, number of steps, heart rate and answer six
questions, using IoT devices connected to a mobile
application (Lopes et al., 2019). Whereas, the de-
veloped chatbot was used to collect daily photos of
the patients’ surgical wounds. That being said, we
needed only a subset of the design defined above.
Namely, dialog management, text generation and data
management. More specifically, when the patient
sends the photo of his/her surgical wound, the chat-
bot needs to be able to understand it, respond with
clinically approved messages, and store the picture
for further analysis by the clinical team. The chat-
bot text generation feature can be divided into two
parts. The first part consists of an appreciation mes-
sage that was used to engage the patient and to cre-
ate some kind of empathy with him/her. The second
part consists of a set of day-dependent literacy mes-
sages used to provide guidance during the patient’s
recovery/telemonitoring. This message calendar was
developed with the clinical team based on leaflets that
were given to patients after hospital discharge. The
message was sent right after the photo was sent be-
cause it is at that moment that the patient has his/her
attention focused on the smartphone.
This specific use case is going to be expanded to
more 150 patients, as depicted in Table 1 and evalu-
ated throughout a larger span of time where more im-
provements resulting from the clinical staff require-
ments will be developed.
4.3 HemoControlBot
This use case albeit developed in a similar context
that Cardiofollow, was targeted specifically to as-
sess hypocoagulation, through the International Nor-
malized Ratio (INR) and additional health outcomes,
through multiple-choice questions with the goal of
evaluating if the use of a coagulometer allowed the
patient a longer and better stay in the therapeutic
range, when compared to standard clinical follow-up.
That being said, the entirety of the interaction of the
patient occurs through the chatbot, which is respon-
sible for delivering the multi-step questionnaires, val-
idating and storing the data. The patients are given
a coagulometer (used to measure the INR), the chat-
bot’s phone number and a code representing a mea-
surement plan defined by the clinical staff. A mea-
surement plan is a set of measures with a certain pe-
riodicity. In this specific use case the periodicity is
set to 7 days and consists of 7 items: INR value and
6 questions, related to medication, bruise, bleeding,
feces, nausea and trips to the hospital/health center.
This chatbot is currently being tested with one patient
and 29 more will enter the program, as depicted in Ta-
ble 1. Each patient will report his/her outcomes to the
chatbot for 6 months.
The chatbot implemented for this use case used
all the four features defined in Section 3. Namely, in
order for the patient to register into the chatbot we
Scale-IT-up 2022 - Workshop on Scaling-Up Health-IT
816
make use of the four features since we offer a self-
enroll approach. That being said, the interaction is
triggered by a patient’s message saying ”hello”. The
chatbot initiates the enrollment process requesting the
measurement plan code, name, birth date and gender,
step by step. Thus, the chatbot needs to understand,
store, manage and validate the entirety of the interac-
tion. Furthermore, the chatbot validates the user input
accepting only valid answers, that are measurement
dependent and in turn are defined by regular expres-
sions. Moreover, by leveraging the dialog manage-
ment and text generation capabilities of the chatbot,
we display the expected input format and give proper
feedback if the input does not match with the expected
format. Furthermore, if the measurement is a ques-
tion, we showcase the possible answers to the user.
All the answers are preceded with a number that al-
lows the user to answer with the respective number.
This way, the answering process is faster and easier to
the patient. In addition, due to the data management
capability, we can store all the measures and user-
defined thresholds for each measurement, which then
permits the chatbot to send an alert (for the patient and
the clinical staff) whenever any measure goes outside
of the expected ranges, defined by the clinical team.
Finally, with the goal of allowing the patient to vali-
date his/her answers, the chatbot always asks for con-
firmation before storing the reported outcomes. If the
patient does not validate the answers, the chatbot re-
sets to the beginning of the measurement plan. The
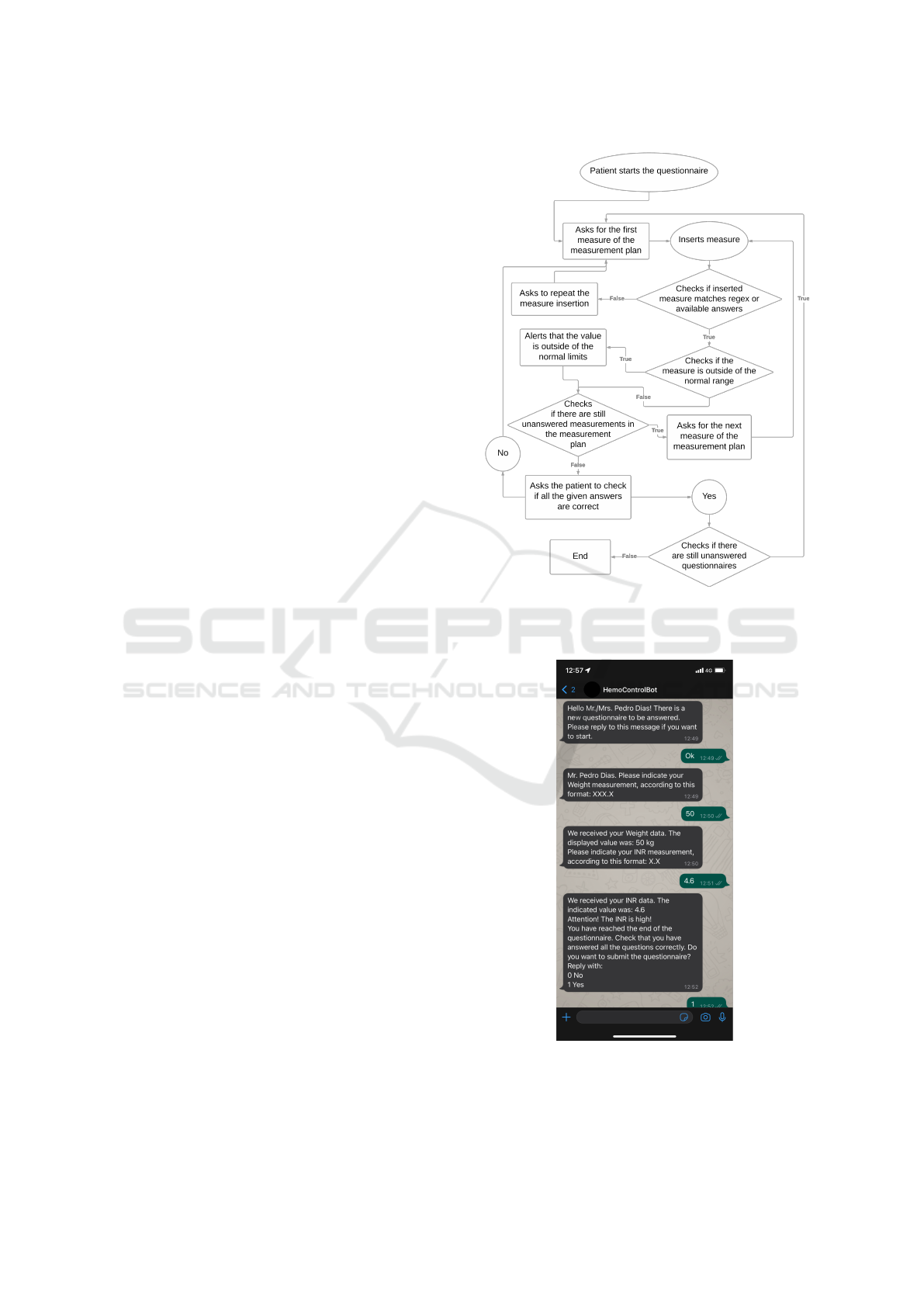
flow behind this chatbot is depicted in Fig.2.
An example of a conversation between a patient
and the chatbot is depicted in Fig. 3. The green
speech bubbles represent the patient and the black
speech bubbles represent the chatbot.
In this use case, the requirements were trans-
lated into new features to the web application.
Namely, manage measurement plans specific for a
given service, in this case there is only the cardio-
thoracic service. Nevertheless, multiple services
from multiple hospitals could use the developed soft-
ware/solution/application. A measurement plan is
used within two contexts: periodic reporting as noted
previously, and on-demand reporting, which is trig-
gered by the clinical staff. Thus, our web application
was extended to be able to create and manage mea-
surement plans, as well as their periodicity and allow-
ing the clinical staff to request specific measures if de-
sired. Intuitively, we offer a easy to use interface for
the clinical staff to manage all the features described
above.
Figure 2: Measure collection flow. The circle represents the
patient, the diamond represents the finite state machine and
the rectangle represents the chatbot.
Figure 3: Example of a conversation between a patient and
the chabot.
Remote Patient Monitoring Systems based on Conversational Agents for Health Data Collection
817

5 DISCUSSION
As it is mentioned in subsections 4.2 and 4.3, two CAs
were developed to provide support to patients after
discharge from the hospital. The information deliv-
ered to the patient was defined after several meetings
with the clinical team and it contains guidelines to im-
prove recovery. These chatbots are specially impor-
tant due to the huge amount of information provided
to the patient after diagnosis, which usually lets the
patient overwhelmed and might be difficult to remem-
ber when away from the hospital. Thus, with these
solutions we aim at providing health literacy, solve
the issue regarding the lack of understanding of med-
ications regimens, monitor vital signs while targeting
high-risk situations, and equip the clinical team with
an easy to use web application to communicate and
understand the patient’s recovery.
The CAs design aimed at the development of a
system adapted to most patients. Not all patients
could be included due to the exclusion criteria of the
two use cases. These criteria were illiteracy and the
inability to manage a cellphone. However, if the pa-
tient spends his/her recovery period with a capable in-
formal caregiver, the telemonitoring can still occur,
which happened with some patients from CardioFol-
low.
The user experience of the selected patients might
be improved by attending to the degree of patient’s
literacy and adjusting the dialogue to improve the en-
gagement with the CA. This could be done by having
different dialogue-frames given the patient’s literacy
level.
Patients mentioned the importance of having a
non-invasive tool that at specific timings can provide
support when needed. After diagnosis, patients tend
to look for adapted normality. A supportive tool that
empowers patients by capacitating them to take their
own decisions and feel safe from home, might be the
key to giving them this adapted normality.
6 CONCLUSIONS
In this work, we successfully defined a generalized
design of a rule-based task-oriented chatbot, which
we then applied to two different use cases. Our initial
experiments showed that offering a conversational-
based interface to collect PROMs is an efficient way
to keep the end-users - the patients - engaged. Mo-
bile phones are ubiquitous, so most of the popula-
tion can benefit from this way of outcome collection.
Using SMS or Whatsapp as an outcomes collection
channel is a good way to interact with patients be-
cause nowadays anyone carries their cell phone with
them, thus being able to respond quickly to what is re-
quested. Although the interface is simple and easy-to-
use, managing a mobile phone requires some level of
digital literacy, thus not being useful for every type of
patient. Both use cases described in this paper, were
developed with the objective of being extended to col-
lect outcomes from patients with other health condi-
tions.
From our experience, telemonitored patients feel
safer and more engaged regarding their health status,
so this work is a starting point to pose remote patient
monitoring as a way of preventing clinical complica-
tions, due to its close follow-up, and of leading to an
increase of the patients health literacy level. More-
over, from the clinical team point of view, having
the possibility to analyze more outcomes will help to
make better clinical decisions and adopt a more per-
sonalized treatment for each patient.
Finally, regarding the chatbot and web applica-
tion development, including the clinical team in the
process is of the utmost importance for two reasons.
First, they are the domain experts with the necessary
knowledge to identify the requirements for such sys-
tems to be of any use. Second, they are the end-users,
and user experience is extremely important within
this context. Ultimately, the developed systems must
serve the clinical team, not the opposite.
7 FUTURE WORK
Both of the use cases described above took place
within the context of cardiothoracic surgery in Por-
tugal. Thus, intuitively, future work lies in expanding
these conversational agents to other contexts, which
will require further development to adapt to specific
requirements that might arise. However, these two
use cases are still undergoing as depicted in Table 1.
There is currently no way to show to the patient a
summary of his/her latest measurements, so develop-
ing a way of showcasing this data is a priority in the
near future. Regarding user interaction, increasing the
intelligence of the chatbot might be a way of decreas-
ing input errors and giving advice. This can be done
by suggesting, predicting or correcting the user’s in-
put.
ACKNOWLEDGEMENTS
The authors would like to acknowledge the Roche Di-
agnostics and the cardiothoracic service of the Hos-
pital de Santa Marta for their contributions to car-
Scale-IT-up 2022 - Workshop on Scaling-Up Health-IT
818

rying out the study. This research has been sup-
ported by the project DSAIPA/AI/0094/2020 from the
Fundac¸
˜
ao para a Ci
ˆ
encia e Tecnologia AI 4 COVID-
19 Program.
REFERENCES
Abashev, A., Grigoryev, R., Grigorian, K., and Boyko,
V. (2017). Programming Tools for Messenger-Based
Chatbot System Organization: Implication for Outpa-
tient and Translational Medicines. BioNanoScience,
7(2):403–407.
Abd-Alrazaq, A. A., Alajlani, M., Ali, N., Denecke, K.,
Bewick, B. M., and Househ, M. (2021). Perceptions
and Opinions of Patients About Mental Health Chat-
bots: Scoping Review. Journal of Medical Internet
Research, 23(1):e17828.
Bian, Y., Xiang, Y., Tong, B., Feng, B., and Weng, X.
(2020). Artificial Intelligence–Assisted System in
Postoperative Follow-up of Orthopedic Patients: Ex-
ploratory Quantitative and Qualitative Study. Journal
of Medical Internet Research, 22(5):e16896.
Bickmore, T. and Cassell, J. (2001). Relational Agents:
A Model and Implementation of Building User Trust.
In Proceedings of the SIGCHI conference on Human
factors in computing systems, pages 396–403, Seattle,
WA, USA.
Bickmore, T. W., Utami, D., Matsuyama, R., and Paasche-
Orlow, M. K. (2016). Improving Access to Online
Health Information With Conversational Agents: A
Randomized Controlled Experiment. Journal of Med-
ical Internet Research, 18(1):e1.
B
´
erub
´
e, C., Schachner, T., Keller, R., Fleisch, E., V Wan-
genheim, F., Barata, F., and Kowatsch, T. (2021).
Voice-Based Conversational Agents for the Preven-
tion and Management of Chronic and Mental Health
Conditions: Systematic Literature Review. Journal of
Medical Internet Research, 23(3):e25933.
Casas, J., Mugellini, E., and Khaled, O. A. (2018). Food
Diary Coaching Chatbot. In Proceedings of the 2018
ACM International Joint Conference and 2018 In-
ternational Symposium on Pervasive and Ubiquitous
Computing and Wearable Computers, pages 1676–
1680, Singapore Singapore. ACM.
Chaix, B., Bibault, J.-E., Pienkowski, A., Delamon, G.,
Guillemass
´
e, A., Nectoux, P., and Brouard, B. (2019).
When Chatbots Meet Patients: One-Year Prospective
Study of Conversations Between Patients With Breast
Cancer and a Chatbot. JMIR Cancer, 5(1):e12856.
Colby, K. M., Weber, S., and Hilf, F. D. (1971). Artificial
Paranoia. Artificial Intelligence, 2(1):1–25.
Crawford, T. C., Magruder, J. T., Grimm, J. C., Suarez-
Pierre, A., Sciortino, C. M., Mandal, K., Zehr, K. J.,
Conte, J. V., Higgins, R. S., Cameron, D. E., and
Whitman, G. J. (2017). Complications After Cardiac
Operations: All Are Not Created Equal. The Annals
of Thoracic Surgery, 103(1):32–40.
de Pennington, N., Mole, G., Lim, E., Milne-Ives, M., Nor-
mando, E., Xue, K., and Meinert, E. (2021). Safety
and Acceptability of a Natural Language Artificial In-
telligence Assistant to Deliver Clinical Follow-up to
Cataract Surgery Patients: Proposal. JMIR Research
Protocols, 10(7):e27227.
Denecke, K., Hochreutener, S., P
¨
opel, A., and May, R.
(2018). Self-Anamnesis with a Conversational User
Interface: Concept and Usability Study. Methods of
Information in Medicine, 57(05/06):243–252.
Echeazarra, L., Pereira, J., and Saracho, R. (2021). Ten-
sioBot: a Chatbot Assistant for Self-Managed in-
House Blood Pressure Checking. Journal of Medical
Systems, 45(4):54.
Efthymiou, C. A. and O’Regan, D. J. (2011). Postdischarge
complications: what exactly happens when the patient
goes home? Interactive CardioVascular and Thoracic
Surgery, 12(2):130–134.
Epley, N., Waytz, A., and Cacioppo, J. T. (2007). On seeing
human: a three-factor theory of anthropomorphism.
Psychological review, 114(4):864–886.
Fitzpatrick, K. K., Darcy, A., and Vierhile, M. (2017). De-
livering Cognitive Behavior Therapy to Young Adults
With Symptoms of Depression and Anxiety Using a
Fully Automated Conversational Agent (Woebot): A
Randomized Controlled Trial. JMIR Mental Health,
4(2):e19.
Griol, D. and Callejas, Z. (2016). Mobile Conversational
Agents for Context-Aware Care Applications. Cogni-
tive Computation, 8(2):336–356.
Guhl, E., Althouse, A. D., Pusateri, A. M., Kimani, E.,
Paasche-Orlow, M. K., Bickmore, T. W., and Mag-
nani, J. W. (2020). The Atrial Fibrillation Health Lit-
eracy Information Technology Trial: Pilot Trial of a
Mobile Health App for Atrial Fibrillation. JMIR Car-
dio, 4(1):e17162.
Heneghan, C. J., Garcia-Alamino, J. M., Spencer,
E. A., Ward, A. M., Perera, R., Bankhead, C.,
Alonso Coello, P., Fitzmaurice, D., Mahtani, K. R.,
and Onakpoya, I. J. (2016). Self-monitoring and
self-management of oral anticoagulation. Cochrane
Database of Systematic Reviews, 2021(4).
Irfan, B., Hellou, M., Mazel, A., and Belpaeme, T. (2020).
Challenges of a Real-World HRI Study with Non-
Native English Speakers: Can Personalisation Save
the Day? In Companion of the 2020 ACM/IEEE In-
ternational Conference on Human-Robot Interaction,
pages 272–274, Cambridge United Kingdom. ACM.
Kamita, T., Ito, T., Matsumoto, A., Munakata, T., and In-
oue, T. (2019). A Chatbot System for Mental Health-
care Based on SAT Counseling Method. Mobile In-
formation Systems, 2019:9517321.
Kardas, P., Boven, J. F. M. v., Pinnock, H., Menditto,
E., Wettermark, B., Tsiligianni, I., and
´
Agh, T.
(2021). Disparities in European healthcare system
approaches to maintaining continuity of medication
for non-communicable diseases during the COVID-
19 outbreak. The Lancet Regional Health - Europe,
4:100099.
Khoury, H., Ragalie, W., Sanaiha, Y., Boutros, H., Rudasill,
S., Shemin, R. J., and Benharash, P. (2020). Read-
mission After Surgical Aortic Valve Replacement in
the United States. The Annals of Thoracic Surgery,
110(3):849–855.
Laranjo, L., Dunn, A. G., Tong, H. L., Kocaballi, A. B.,
Chen, J., Bashir, R., Surian, D., Gallego, B., Magrabi,
Remote Patient Monitoring Systems based on Conversational Agents for Health Data Collection
819

F., Lau, A. Y. S., and Coiera, E. (2018). Conversa-
tional agents in healthcare: a systematic review. Jour-
nal of the American Medical Informatics Association,
25(9):1248–1258.
Lee, K., Kwon, H., Lee, B., Lee, G., Lee, J. H., Park, Y. R.,
and Shin, S.-Y. (2018). Effect of self-monitoring on
long-term patient engagement with mobile health ap-
plications. PLOS ONE, 13(7):e0201166.
Levy, M., Ferrand, P., and Chirat, V. (1989). SESAM-
DIABETE, an expert system for insulin-requiring di-
abetic patient education. Computers and Biomedical
Research, 22(5):442–453.
Lopes, I., Sousa, F., Moreira, E., and Cardoso, J. (2019).
Smartphone-Based Remote Monitoring Solution for
Heart Failure Patients. Studies in Health Technology
and Informatics, 261:109–114.
Luo, T. C., Aguilera, A., Lyles, C. R., and Figueroa, C. A.
(2021). Promoting Physical Activity Through Conver-
sational Agents: Mixed Methods Systematic Review.
Journal of Medical Internet Research, 23(9):e25486.
Mamdiwar, S. D., R, A., Shakruwala, Z., Chadha, U., Srini-
vasan, K., and Chang, C.-Y. (2021). Recent Advances
on IoT-Assisted Wearable Sensor Systems for Health-
care Monitoring. Biosensors, 11(10).
Mantena, S. and Keshavjee, S. (2021). Strengthening
healthcare delivery with remote patient monitoring in
the time of COVID-19. BMJ Health Care Informatics,
28(1):e100302.
Marcus, J. L., Sewell, W. C., Balzer, L. B., and Krakower,
D. S. (2020). Artificial Intelligence and Machine
Learning for HIV Prevention: Emerging Approaches
to Ending the Epidemic. Current HIV/AIDS reports,
17(3):171–179.
McElroy, I., Sareh, S., Zhu, A., Miranda, G., Wu, H.,
Nguyen, M., Shemin, R., and Benharash, P. (2016).
Use of digital health kits to reduce readmission af-
ter cardiac surgery. Journal of Surgical Research,
204(1):1–7.
McTear, M. F., Callejas, Z., and Griol, D. (2016). The
Conversational Interface: Talking to Smart Devices.
Springer.
Moore, R. J., Arar, R., Ren, G.-J., and Szymanski, M. H.
(2017). Conversational UX Design. In Proceedings
of the 2017 CHI Conference Extended Abstracts on
Human Factors in Computing Systems, CHI EA ’17,
pages 492–497, New York, NY, USA. Association
for Computing Machinery. event-place: Denver, Col-
orado, USA.
Overby, M. A. (1987). Psyxpert: an expert system proto-
type for aiding psychiatrists in the diagnosis of psy-
chotic disorders. Computers in biology and medicine,
17(6):383–393.
P
´
ecout, C., Pain, E., Chekroun, M., Champeix, C., Kulak,
C., Prieto, R., van Vugt, J., Gilchrist, K., and Lain
´
e-
Pellet, A.-F. (2021). Impact of the COVID-19 Pan-
demic on Patients Affected by Non-Communicable
Diseases in Europe and in the USA. Interna-
tional Journal of Environmental Research and Public
Health, 18(13).
Pereira, J. and D
´
ıaz, O. (2019). Using Health Chatbots for
Behavior Change: A Mapping Study. Journal of Med-
ical Systems, 43(5):135.
Potts, C., Ennis, E., Bond, R. B., Mulvenna, M. D., McTear,
M. F., Boyd, K., Broderick, T., Malcolm, M., Kuos-
manen, L., Nieminen, H., Vartiainen, A. K., Koste-
nius, C., Cahill, B., Vakaloudis, A., McConvey, G.,
and O’Neill, S. (2021). Chatbots to Support Mental
Wellbeing of People Living in Rural Areas: Can User
Groups Contribute to Co-design? Journal of Technol-
ogy in Behavioral Science, 6(4):652–665.
Safi, Z., Abd-Alrazaq, A., Khalifa, M., and Househ, M.
(2020). Technical Aspects of Developing Chatbots
for Medical Applications: Scoping Review. Journal
of Medical Internet Research, 22(12):e19127.
Schachner, T., Keller, R., and v Wangenheim, F. (2020). Ar-
tificial Intelligence-Based Conversational Agents for
Chronic Conditions: Systematic Literature Review.
Journal of Medical Internet Research, 22(9):e20701.
Schumaker, R. P., Ginsburg, M., Chen, H., and Liu, Y.
(2007). An evaluation of the chat and knowledge de-
livery components of a low-level dialog system:The
AZ-ALICE experiment. Decision Support Systems,
42(4):2236–2246.
Tschanz, M., Dorner, T. L., Holm, J., and Denecke, K.
(2018). Using eMMA to Manage Medication. Com-
puter, 51(8):18–25.
Tudor Car, L., Dhinagaran, D. A., Kyaw, B. M., Kowatsch,
T., Joty, S., Theng, Y.-L., and Atun, R. (2020). Con-
versational Agents in Health Care: Scoping Review
and Conceptual Analysis. Journal of Medical Internet
Research, 22(8):e17158.
Vaidyam, A. N., Wisniewski, H., Halamka, J. D., Kasha-
van, M. S., and Torous, J. B. (2019). Chatbots and
Conversational Agents in Mental Health: A Review
of the Psychiatric Landscape. The Canadian Journal
of Psychiatry, 64(7):456–464.
van Heerden, A., Ntinga, X., and Vilakazi, K. (2017). The
potential of conversational agents to provide a rapid
HIV counseling and testing services. In 2017 Inter-
national Conference on the Frontiers and Advances
in Data Science (FADS), pages 80–85, Xi’an, China.
IEEE.
Van Pinxteren, M. M., Pluymaekers, M., and Lemmink,
J. G. (2020). Human-like communication in conversa-
tional agents: a literature review and research agenda.
Journal of Service Management, 31(2):203–225.
Vandenberghe, D. and Albrecht, J. (2020). The financial
burden of non-communicable diseases in the Euro-
pean Union: a systematic review. European Journal
of Public Health, 30(4):833–839.
Wallace, R. S. (2009). The Anatomy of A.L.I.C.E. In Ep-
stein, R., Roberts, G., and Beber, G., editors, Parsing
the Turing Test, pages 181–210. Springer Netherlands,
Dordrecht.
Weizenbaum, J. (1966). ELIZA—a Computer Program for
the Study of Natural Language Communication be-
tween Man and Machine. Communications of the
ACM, 9(1):36–45.
Williams, T., Thames, D., Novakoff, J., and Scheutz, M.
(2018). ”Thank You for Sharing that Interesting
Fact!”: Effects of Capability and Context on Indi-
rect Speech Act Use in Task-Based Human-Robot Di-
alogue. In Proceedings of the 2018 ACM/IEEE In-
ternational Conference on Human-Robot Interaction,
pages 298–306, Chicago IL USA. ACM.
Scale-IT-up 2022 - Workshop on Scaling-Up Health-IT
820
