
From Wearable Device to OpenEMR: 5G Edge Centered Telemedicine
and Decision Support System
Ying Wang
1,2
, Patricia Tran
1,2
and Janusz Wojtusiak
1,2
1
School of Systems and Enterprises, Stevens Institute of Technology, Hoboken, NJ, U.S.A.
2
Health Informatics Department, George Mason University, Fairfax, U.S.A.
Keywords:
IoT, 5G, Wearable Communication, Mobile Edge Computing, Cloud/Edge, Artificial Intelligence, OpenEMR,
Atrial Fibrillation.
Abstract:
The Internet of Things (IoT) is developing rapidly, with applications across various fields and industries. In
healthcare, wearable devices and the Internet of Medical Things (IoMT) have tremendous potential for im-
provements in the quality of telemedicine and producing medical insights and discoveries. Massive Machine
Type of Communication (mMTC) in 5G further reduces latency and enhances connectivity in supporting
wearables and IoMT, which provides a promising infrastructure for telemedicine. Although cloud computing
reduced the computation and storage load on wearable devices significantly, the massive amounts of data pro-
duced by wearable devices and IoMT introduce challenges for latency and storage in the cloud. Additionally,
applications will need to navigate the regulation and compliance laws related to handling sensitive and private
health data, adding complexity to the accessibility and distribution of such innovations. This study first exam-
ined the current frameworks for wearable devices in 5G telemedicine implementation and discussed existing
challenges. We then proposed a multi-layer 5G mobile edge computing (MEC) centered telemedicine design
that dynamically integrates wearable devices with OpenEMR electronic health records system. The multi-
layer design includes the IoT layer, MEC layer, Network layer, and Application layer. Near-real-time artificial
intelligence (AI) components and electronic health record (EHR) instances are automatically deployed to and
removed from the MEC layer to keep cloud computing capabilities closest to the infrastructure edge when a
user is associating and disassociating with a 5G bases station, respectively. Lastly, we demonstrate a proof
of concept by designing and implementing a system for detecting atrial fibrillation (Afib) over the design we
proposed. Afib detection has the character of predictable trending, random occurrence of adverse events, and
urgent care needed when happening. These characters requires a low latency, large range coverage and high
throughput infrastructure. The proposed approach provides a distributed solution addressing the requirements
for Afib detection. This approach can be used for other applications in telemedicine beyond Afib detection.
1 INTRODUCTION
The Internet of Medical Things (IoMT) improves
multiple aspects in healthcare, including asset man-
agement in hospitals, patients’ vitals remote monitor-
ing, treatment compliance monitoring, smarter med-
ication, assisted living, and telemedicine, etc. In
IoMT, various medical devices or sensors, smart-
phones, imaging devices, personal digital assistants,
and electronic health records (EHR) integrate and
act as core parts of the system (Latif et al., 2017).
At present, wearable biomedical/health devices are
developing rapidly, offering advantages such as the
continuity of medical services and real-time capture
of health data. Wearable devices consist of sen-
sors placed on the body to capture and monitor data.
Ranging from fitness trackers and smartwatches to
augmented reality (AR)/virtual reality (VR) glasses,
wearable devices in healthcare collect data on a vari-
ety of measures such as heart rates, sleeping cycles,
locations, and steps, etc. (Haghi et al., 2017). Wear-
able devices offer easier access, mobility, and conve-
nience for users and medical personnel and have al-
ready demonstrated applications in fall identification
and prevention, physical activity monitoring, sports
medicine, patient education, diabetes care manage-
ment, and more (Min Wu and Jake Luo, 2020). The
emerging and integration of artificial intelligence (AI)
and machine learning (ML), big data, and IoT has en-
hanced the degree of intelligence of wearable devices
Wang, Y., Tran, P. and Wojtusiak, J.
From Wearable Device to OpenEMR: 5G Edge Centered Telemedicine and Decision Support System.
DOI: 10.5220/0010837600003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 491-498
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved
491

(Zhang et al., 2020). Combined with 5G technology,
these technologies have the potential to revolutionize
the healthcare industry, facilitating exciting research
and development towards this direction in the field of
telemedicine (Latif et al., 2017).
In current implementations of telemedicine over
the IoMT monitoring in the both Long Term Evolu-
tion (LTE) and Wi-Fi system, three different types of
operation exist. The first category is wearable de-
vices to collect health data and connect to the cloud
in the data network. In the cloud, AI may take place
to provide diagnostic or predictive analysis for physi-
cians or patients, and decision-making support for
treatment or management (Zhang et al., 2020). The
second category is for IoMT devices to run in an ac-
cessory mode and tether to a local connected mobile
device for data storage and processing. An IoMT in
the accessory mode is connected to a mobile phone
through Wi-Fi or Bluetooth for raw data transmis-
sion, and most of the data analysis is processed on
the mobile phone. The limitation of this model is
the requirement of mobile phone presence within Wi-
Fi/Bluetooth coverage, which is usually within 10 me-
ters. The third category is for wearable devices to
perform in standalone mode. For IoT in standalone
mode, the connection to a base station is through cel-
lular technology directly, and local data analysis oc-
curs without any connection to the cloud. However,
computing and energy limitations continue to hinder
these devices’ ability to process data locally. Addi-
tionally, there are limitations in hardware cost, size,
and the number of devices able to connect to the base
station at a given time.
Wearable devices are limited by power and stor-
age constraints, hardware size, and computing capa-
bility and are subject to high hardware costs. Thus,
most current IoMT devices adopted the second and
third category model by sending their data to mobile
devices with more computation power or further con-
necting to the clouds for processing (Sun et al., 2018).
Existing technology such as LTE-Advanced and Wi-
Fi are gradually evolving to fit the needs of wearable
communication in telemedicine. However, besides
the aforementioned limitations, telemedicine over the
IoT will generate an unprecedented amount of data
requiring transmission, analysis, and storage and face
challenges such as security, latency, and connectivity
under the current LTE infrastructure.
Furthermore, IoMT devices handles sensitive and
private data, but the current regulations and policy
of data generated by wearable data are not sufficient.
Unlike traditional health or medical data required to
comply with HIPAA regulations, HIPAA protection
does not extend to wearables and Apps. Integrat-
ing wearable devices with regulated EHR systems
like OpenEMR offers advantages of HIPPA protec-
tion and the creation of new applications. The cy-
ber security of healthcare data is more stringent than
other areas, and health data is frequently the target
of cybercriminals. Despite several digital transforma-
tions, the ”healthcare industry remains highly suscep-
tible to compromises of valuable health information”
(Chernyshev et al., 2019). Security breaches and data
leakage not only result in reputation and/or financial
harm for the healthcare provider/facility but may also
threaten patients’ well-being or health. Weak health
data protection and security measures may result in
detrimental and costly consequences, such as identity
theft, fraudulent insurance claims, ordering drugs for
resale, or even harmful or fatal patient care.
According to a study by Shahriar et al., EHR
applications in general ”suffer from implementation
level vulnerabilities impacting HIPAA requirements,”
and open-source EHR systems are not excluded from
such vulnerabilities (file manipulation, SQL injection,
possible flow control, etc.) (Shahriar et al., 2021).
However, open-source solutions (OSS) have already
been gaining traction in the scientific hardware com-
munity for their evidence of cost-effectiveness, and
technological sophistication (Pearce, 2017). In the
healthcare industry, open-source EHR systems are
gaining more attention as adoption rates are increas-
ing, helping to overcome barriers such as excessive
cost and lack of interoperability (Latif et al., 2017).
Besides its cost-effectiveness, open-source EHR sys-
tems offer more flexibility, less vendor lock, and in-
creased control over data; customers utilizing OSS
have more say and control in how data is stored and
used, as compared to proprietary systems. OpenEMR
is a popular and widely used open-sourced EHR sys-
tem and one of the few OSS EHR systems certified by
the Office of the National Coordinator (ONC) of the
US Department of Health and Human Services.
An important application area of the wearable de-
vice is cardiology disease detection. Atrial fibrillation
(Afib) is a quivering or irregular heartbeat (arrhyth-
mia) that can lead to blood clots, stroke, heart failure,
and other heart-related complications. At least 2.7
million Americans are living with Afib. Its prevalence
is 1- 2% of the general population, and it is associated
with increased risk of mortality and morbidity (Behar
et al., 2017). Physicians’ review of the patient’s signs
and symptoms, medical history, and physical exam-
ination including Electrocardiogram (ECG), Holter
monitor, Event Recorder, Echocardiogram, Blood
tests, Stress test, and Chest X-ray are required for Afib
diagonisis. Asymptomatic Afib is more difficult to de-
tect and can go undiagnosed for extended periods of
HEALTHINF 2022 - 15th International Conference on Health Informatics
492
time. Undetected Afib poses more risk to the patient
and may have devastating consequences if diagnosed
too late. Wearable devices are a non-invasive, conve-
nient way to monitor cardiac rhythms, possibly aiding
in the earlier detection of asymptomatic Afib. Afib
detection through wearable devices has the characters
of temporal based trending, adverse event random oc-
currences, and urgent care needed when it happens.
These three characters determine stringent require-
ments of a desired solution: seamless geographic cov-
erage, complex computation support, and low latency,
secure connection. Our proposed 5G edge-centered
telemedicine and decision support system fits the use
case scenario and provides a reliable and scalable so-
lution. Thus, as the proof of concept, we have de-
signed and implemented an Afib detection model de-
ployed to the 5G edge-centered system built and con-
nected to an OpenEMR system. An extension to other
medical models can easily be added to it.
2 SYSTEM DESIGN
2.1 5G Network Framework for
Telemedicine
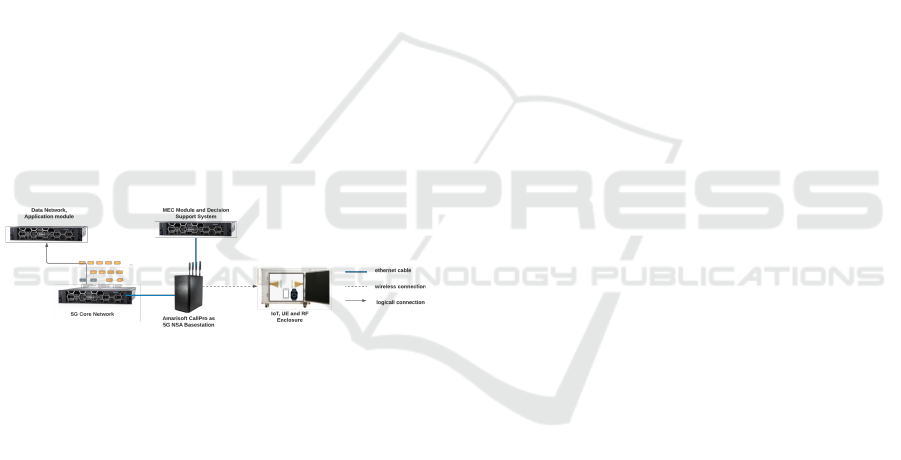
Figure 1: Hardware Implementation.
Despite the fact that the advantages on physi-
cal coverage of cellular network, IoMT devices in
telemedicine generates a massive amount of data,
some of which may require rapid analysis - such im-
mense and diverse data needs are not supported by the
current 4G/LTE infrastructure (Li, 2019). Latency,
bandwidth, quality of service (QoS), reliability, and
a massive number of connectivity are just some of
the challenges associated with IoT on the current in-
frastructure. Moving forward, telemedicine will need
support for a massive number of devices, standard-
ization, energy-efficiency, device density, and secu-
rity (Ahad et al., 2020). To build effective alarm
or decision support models, secure exchange of data
across various platforms is required. The 5G network
is highly attractive in these regards due to its high
speed, massive number connection characteristic, low
latency, flexibility in Radio Area Network (RAN),
and security enhancement due to network slicing for
verticals. Especially, mMTC networks enable the
long battery life,low latency, and high coverage den-
sity with support up to a million devices in a square
kilometer which are crucially for massive scale, ultra-
low-cost hardware.
The implemented hardware platform depicted in
Fig.1 consists of a User Equipment (UE), Base Sta-
tion (BS), Core Network (CN), MEC. The detailed
information for the setup can be referred to at (Wang
et al., 2021).
2.2 MEC Centered Design
Due to wearable devices’ computing and energy con-
straints, telemedicine applications based on IoMT
cannot be executed locally on the terminals, nor
should all health data be uploaded to the cloud for
analysis either. Deploying cloud computing in the
current framework with massive amounts of data gen-
erated by IoT will introduce high data analysis latency
and storage costs, placing tremendous pressure on the
cloud and causing challenges to the network band-
width and end-to-end delay (Zhang et al., 2020). IoT
devices and cloud computing alone cannot fulfill the
demands of wearable communication. Instead, mo-
bile edge computing (MEC) should be utilized in tan-
dem with IoT technology, artificial intelligence, and
cloud computing components.
MEC has characteristics of decentralization, data
localization, and low latency. MEC allows real-time
intelligent decision-making by reducing network de-
lay and transmission costs during the classification
and assignment of QoS. By removing most of the
computing needs of the IoT devices, IoT devices be-
come ’lighter,’ essentially only collecting and trans-
mitting data and performing simple computations.
This may save on hardware costs and improve the bat-
tery usage and performance speed of the wearable de-
vice. Utilizing a MEC layer also reduces strain on the
cloud. The MEC Edge layer does not eliminate the
need for a cloud computing layer, but rather the two
layers communicate and work together to enhance the
capabilities of the proposed system. MEC layer han-
dles the pre-processing of data and data analysis be-
fore transmitting data to the cloud for storage and fur-
ther management. The cloud computing layer per-
forms big data analysis, mining, and sharing to train
and upgrade the AI algorithm model that gets pushed
to the edge nodes.
From Wearable Device to OpenEMR: 5G Edge Centered Telemedicine and Decision Support System
493
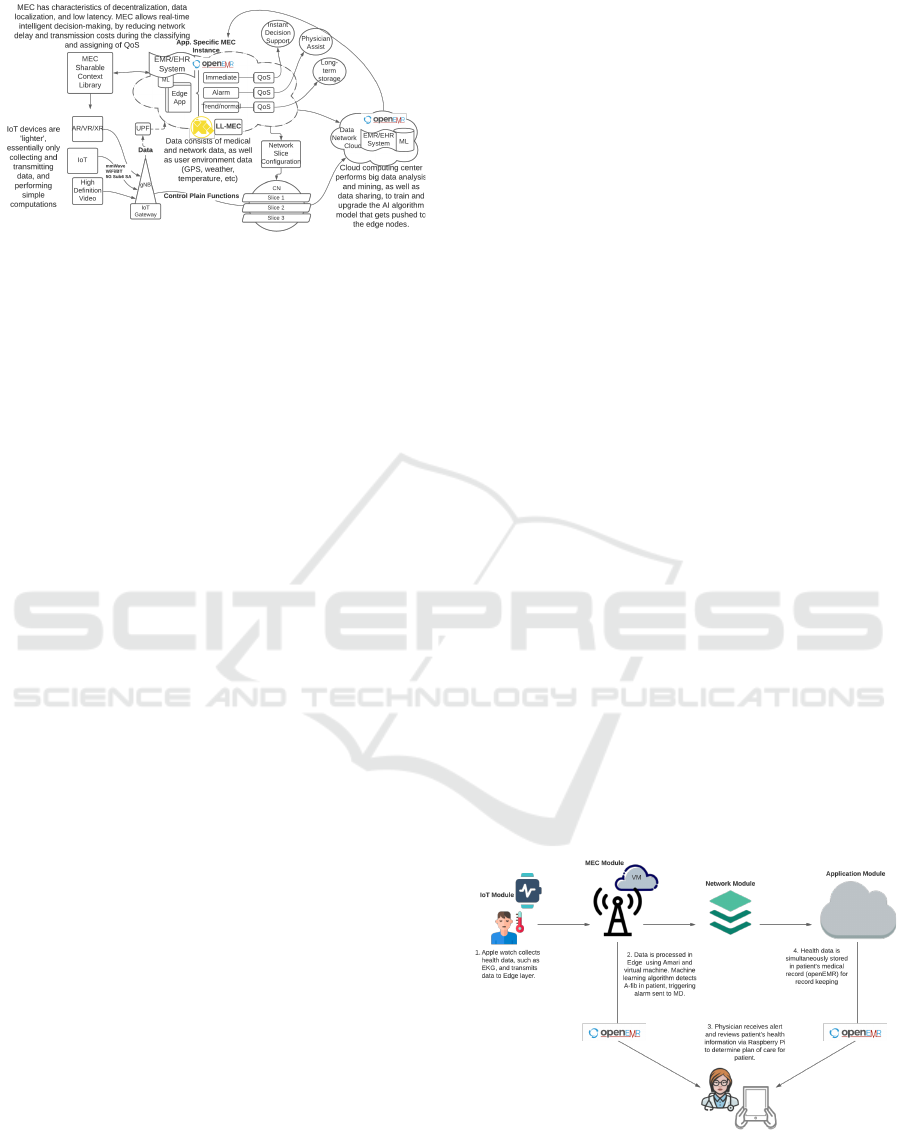
Figure 2: Proposed Telemedicine System Design.
2.3 OpenEMR-based Distributed
System
A primary concern related to wearable device usage
relates to the security and governance of data sharing.
IoMT generated medical data storing in the central-
ized storage system leads to a single point of failure,
privacy, and security concern (Kumar and Tripathi,
2021). HIPAA protection not extending to wearables
and Apps creates another area of concerns for per-
sonal health data privacy and security. Wearable data
should be stored in secure, regulated personal health
clouds or electronic health records with opt-in sys-
tems, advance security measures, and transparent pri-
vacy policies in place (Bayoumy et al., 2021) in the
desired scenario. In the proposed system design, the
data storage challenges are addressed by a distributed
open source EMR based architecture.
OpenEMR is a widely used open-sourced soft-
ware for electronic health records and medical prac-
tice management solutions, utilized in more than
100 countries worldwide with an estimated usage by
100,000 medical providers serving greater than 90
million patients internationally. OpenEMR leverages
one of the largest communities of users, volunteers,
and contributors dedicated to developing and main-
taining its software, making it a superior alternative
to proprietary counterparts and more comprehensive
than emerging applications. OpenEMR is ONC Cer-
tified as a Complete EHR, having achieved complete
Meaningful Use certification with Release 5.0 and be-
yond. Compared to other popular open-sourced EHR
systems like GNU Health, OpenMRS, and OSHERA
VistA, OpenEMR has the highest functionality and is
among the top for performance (Purkayastha et al.,
2019). Utilizing OpenEMR supports interoperabil-
ity and industry standards and reduces the burden of
seeking new regulation compliance and additional se-
curity measures by making use of a popular exist-
ing electronic health records platform. According to
its website, it offers HIPAA-friendly security features
such as database connection encryption support, fine
grained access control objects, the ability to encrypt
patient documents, and industry-standard password
hashing.
As with other open-sourced software, one of the
most significant benefits of OpenEMR in the health-
care industry is that it is free and can easily be down-
loaded from one of the repositories (Syzdykova et al.,
2017). Unlike proprietary electronic medical records
systems, smaller health settings can utilize and adapt
OpenEMR to their needs. Open-sourced systems
are flexible, cost-efficient, offer freedom to try be-
fore buying and avoid vendor lock-in. These ad-
vantages help relieve health disparities by allowing
for greater distribution and accessibility of electronic
health records worldwide.
2.4 Proposed System Architecture
Our proposed system integrates 5G technology with
wearable devices to capture physiological indicators
in real-time and send them to the edge and cloud.
Physiological indicators may include EKG data, heart
rate, oxygen saturation, and other measures captured
via wearable devices. As shown in Figure 2, four
modules constitute the system: IoT module, MEC
module, Network module, and Application module.
Protocols of communications between the modules
are defined. A layer structure is used for the mod-
ule design. Each module is an abstract virtual ma-
chine that provides a cohesive set of services through
a managed interface (Bass et al., 2013). With this de-
sign, layers imbue a system with portability through
the ability to change the underlying computing plat-
form, network, hardware, or application update. The
connection among the four modules is shown in Fig-
ure 3.
Figure 3: System Component Connection.
The IoT Module is responsible for the acquisition
of health-based data and relative ambient data. It is
also responsible for transmitting the data to the in-
HEALTHINF 2022 - 15th International Conference on Health Informatics
494
frastructure, defined by the modules’ protocol. The
category of data acquisition affects the selection of
data transmission. The physical layer data transmis-
sion attribution data is also recorded for security and
acquisition anomaly detection.
The MEC Module is the main component for
deploying OpenEMR instances, anomaly detection,
real-time decision support, long-term data storage,
and data merging to centerized data storage in the
cloud. When a user is an associate with a gNodeB,
the OpenEMR instance will be deployed on MEC
with user customization and relevant user data sync
up from the center OpenEMR location. Acquisition
data from these patients will be transmitted to and an-
alyzed at the MEC in real-time manners. The system
will perform instant decision support, physician assis-
tant alarm, and plan for long-term data backup based
on the results and resources requested. When a user
disassociate with the base station, a clearing up pro-
cess will be launched to release the resources in the
MEC and hand over to the next base station. This
edge based design significantly reduce the latency by
bring the data analysis closer to users and avoiding
the routing to core network and enables the real-time
decision support. Firewall and security features lo-
cated on the MEC provide security enhancement to
all instances.
The Network Module includes data transmission
from gNB/MEC to the core network. Traffic security
and efficiency is the primary responsibility for net-
work module. The network data are also used for
anomaly detection combined with acquisition data.
Network slicing are used for directing the traffic, iso-
lating context, and enhance network performance.
The Application Module is responsible for cen-
tralized application data management in the cloud.
Long-term analysis and trending, non-real-time ma-
chine learning models are running in the application
module.
2.5 System Implementation and
Automation
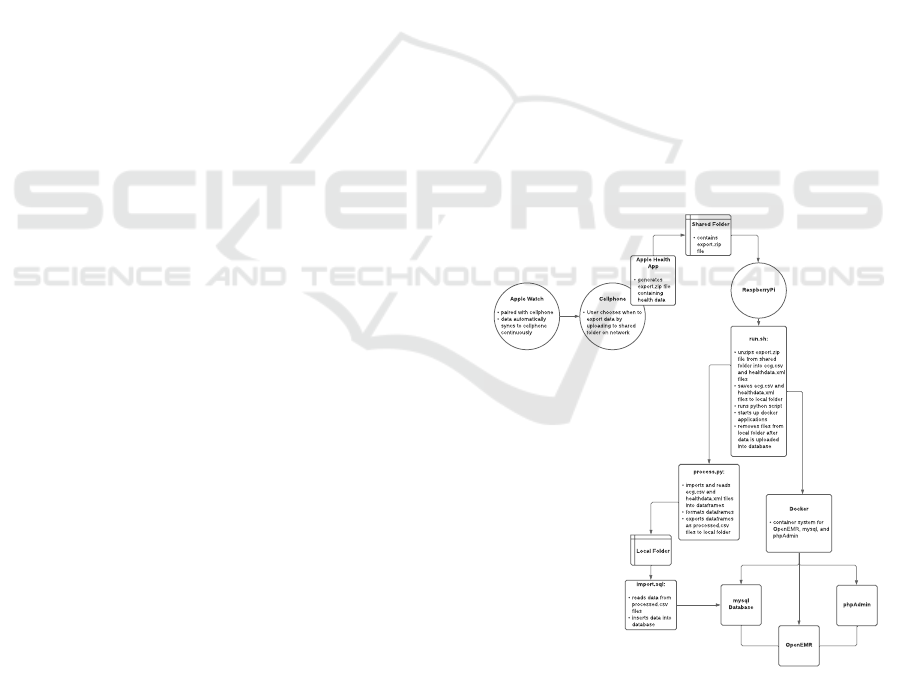
To test the system design and implementation, a Ap-
ple Watch Series 6 was selected as the wearable de-
vice during the implementation. ECG, heart rate, and
blood oxygen data were collected. This data from
the Apple Watch is sent via 5G technology to the
MEC layer, where pre-processing and analysis oc-
cur to detect atrial fibrillation. Studies suggest wear-
able devices, like the Apple Watch, may be effec-
tive and convenient tools to diagnose asymptomatic
or symptomatic atrial fibrillation and/or other arrhyth-
mia (Bayoumy et al., 2021). Using artificial intel-
ligence, MEC determines the classification of health
data as either ’trend/normal,’ ’alarm,’ or ’immediate’
and assigns the appropriate QoS resources. If abnor-
malities are detected, and ’immediate’ or ’alarm’ clas-
sifications are triggered, MEC can quickly alert 911
services or medical personnel and the user; this is
the benefit of edge computing - tasks are performed
at the edge of the network, reducing both the dis-
tance of data transmission and communication delay.
Therefore, critical decision-making tasks can occur in
a real-time manner. OpenEMR software was installed
on a Raspberry Pi device and handles the cloud’s stor-
age and management of health data. Raspberry Pi
is a low-cost computer that acts as the server in this
design, continuously running script to handle Apple
Health files and pre-process then process data for in-
sertion into the OpenEMR database. The MEC layer
works alongside the cloud, pulling relevant data from
existing records in OpenEMR to enhance its artifi-
cial intelligence and pushing data to the OpenEMR
database in the cloud for long-term storage and fur-
ther management. The transmission of data between
the Apple Watch and the MEC layer and to and from
the cloud is performed via 5G technology to ensure
high QoS, low latency, massive connectivity and en-
hanced security. In Figure 4, the flowgraph of the sys-
tem implementation is shown.
Docker
- container system for
OpenEMR, mysql, and
phpAdmin
OpenEMR
process.py:
- imports and reads
ecg.csv and
healthdata.xml files
into dataframes
- formats dataframes
- exports dataframes
as processed.csv
files to local folder
run.sh:
- unzips export.zip
file from shared
folder into ecg.csv
and healthdata.xml
files
- saves ecg.csv and
healthdata.xml
files to local folder
- runs python script
- starts up docker
applications
- removes files from
local folder after
data is uploaded
into database
phpAdmin
mysql
Database
Shared Folder
- contains
export.zip
file
Local Folder
Apple Watch
- paired with cellphone
- data automatically
syncs to cellphone
continuously
RaspberryPi
import.sql:
- reads data from
processed.csv
files
- inserts data into
database
Cellphone
- User chooses when to
export data by
uploading to shared
folder on network
Apple Health
App
- generates
export.zip file
containing
health data
Figure 4: Apple Watch Based IOT connecting to 5G Edge
System Automation.
From Wearable Device to OpenEMR: 5G Edge Centered Telemedicine and Decision Support System
495
3 SYSTEM PROOF OF CONCEPT:
ATRIAL FIBRILLATION
DETECTION IN 5G
TELEMEDICINE NETWORK
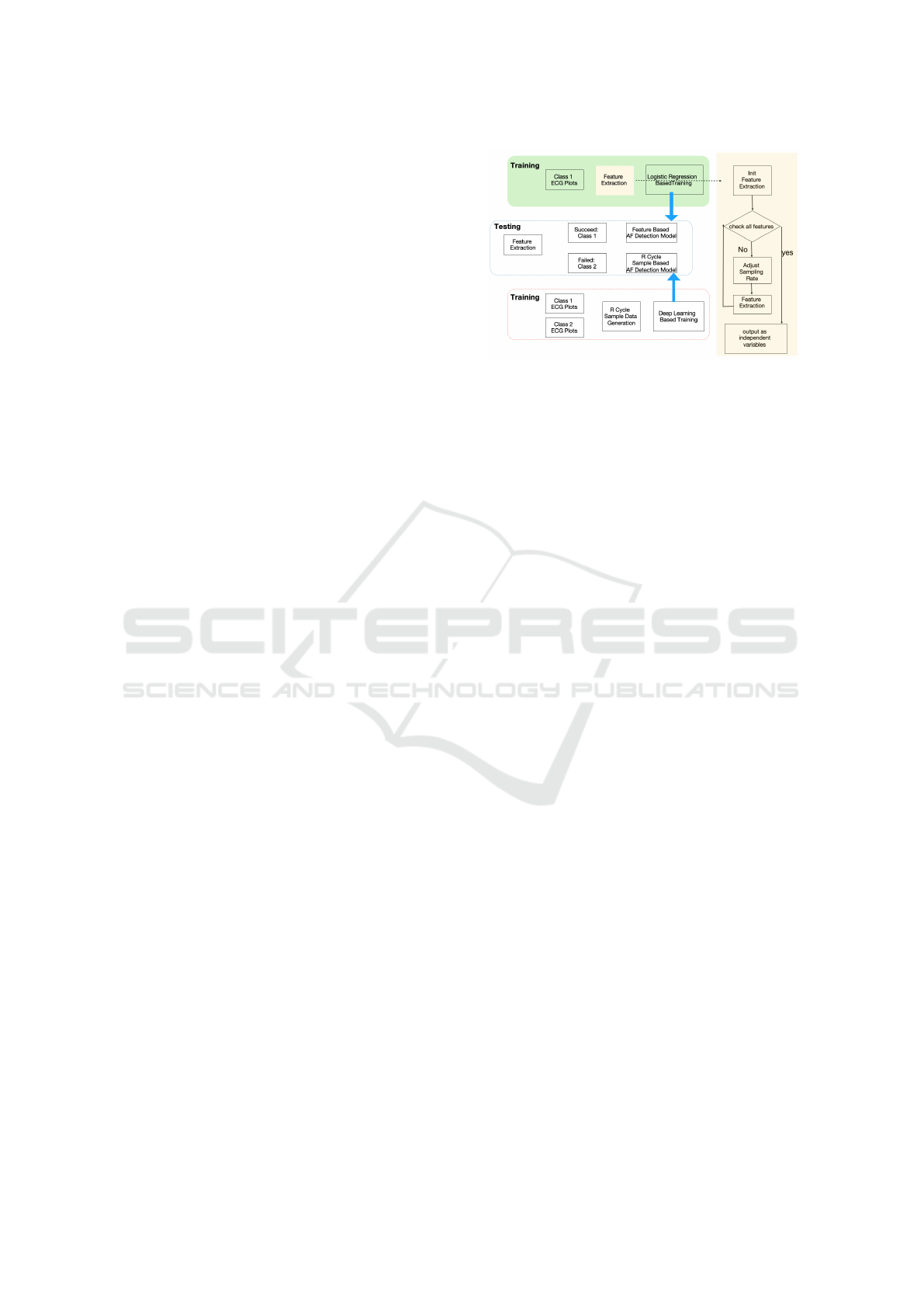
In this session, we have designed and implemented
Atrial fibrillation (AF) detection system based on
the previously discussed framework. The model is
trained using data from single-lead ECG plots gener-
ated by AliveCor devices. ECG recordings were col-
lected using the AliveCor device and made available
in (Clifford et al., 2017). A database of 8528 single-
lead ECG and their annotations were used for training
and testing. Four categories of ECG recordings were
present in the databases: atrial fibrillation (A), nor-
mal sinus rhythm (N), other rhythms (O), and noisy
recordings. Using this as proof of concept in the pro-
posed system, we focused on the detection of type A:
atrial fibrillation detection.
This is a proof of concept for the 5G Edge Cen-
tered Decision Support System with OpenEMR For
Wearable Devices. Figure 5 shows the flowgraph of
the Afib detection system itself. Figure 6 offers the
integration and deployment of the system shown in
Figure 5 to the 5G Edge Centered Telemedicine and
Decision Support System. When a user device asso-
ciates to the 5G network, the gNB that the device is
associated with or in the process of handing over to
will start creating the OpenEMR instance with the as-
sociated patient records and the Edge App instance.
Relevant trained non-near-real time models are trans-
ferred from the data network to MEC on Edge App.
As shown in Figure.6, Feature extraction, feature-
based Afib detection model, R Cycle sample-based
Afib detection model will be transmitted to the Edge
app from the data network to MEC. Context data, in-
cluding location, weather, road condition, etc., will
also be accessible by the Edge App. As patient data
are transmitted to the gNB and MEC, the data will be
instantly processed by feature extraction, Afib model
detection, and generating the results. One of the three
potential types of results will be generated, Afib De-
tected, Low Detection Confidence, and normal result.
The Afit detected result needs immediate attention,
with an alarm being sent with the highest QoS. The
low detection confidants need a physician’s decision
and assist with the second level of QoS. The normal
results will be saved for long-term monitoring. As
the patients disassociate with the current gNB(A) or
handover to the next gNB(B), the process will be re-
launched in the next gNB(B); meanwhile, the existing
patient data and Edge App will be removed from the
current gNB(A).
Figure 5: Flowgraph of Afib Detection.
Preprocessing is needed to extract features from
ECG plots. The cardinal features of atrial fibrilla-
tion are an absence of coordinated depolarization of
the atria (absence of P waves on the ECG) and unpre-
dictable depolarization of the ventricles (no pattern to
R wave occurrence on the ECG). As shown in Figure
1, The P wave represents the depolarization of the left
and right atrium and corresponds to atrial contraction,
and the QRS complex includes the Q wave, R wave,
and S wave.
In general, some features are used to describe
ECG medically. The commonly used features are
ECG Signal quality, Heart Beats / Cardiac Cycles,
and Heart Rate Variability (HRV). In HRV, there are
a set of parameters used to describe the ECG sig-
nal, including CVSD, HF, LF, RMSSD, Shannon,
Power, Triang, ULF, VHF, VLF, cvNN, madNN,
mcvNN, meanNN, medianNN, pNN20, pNN50 and
dNN. These are the basic features we used in our
model.
8528 data samples are used for analysis. The
length of each data sample is 9,000 to 18,000, record-
ing 30 seconds to 60 seconds of ECG. Figure 7 shows
an element overlap illustration of when aligning with
the peak of the R wave of a normal ECG. Figure 8
shows an element overlap illustration of when align-
ing with the peak of the R wave with AF detected.
For the data processing part, we first categorize
ECG plots by extracting essential Cardio and HRV
features from the ECG. If we can extract them, the
ECG plots are categorized as class 1. If the features
are not extractable due to the low quality or abnormal
ECG, then the plots are categorized as class 2. Here,
we use a python library called NeuroKit (Dominique
Makowski, ) for the feature extraction.
Results show that there are 1.2% class 2 ECG
plots and 98.8% class 1 ECG plots. For class 1 ECG,
we use 27 features extracted from Table 1 to prepare
for the data. We can reach an F1 score of 0.76.
For class 2 ECG plots, we need to take a closer
look at them. Among the 104 ECG plots, there are
HEALTHINF 2022 - 15th International Conference on Health Informatics
496
Figure 6: Flowgraph of Afib Detection Over the Proposed Telemedicine System.
Figure 7: Normal ECG R Wave Overlap Illustration.
Figure 8: ECG with AF R Wave Overlap Illustration.
5% normal ECG, 13% AF, 66% Other Abnormal, and
15% noise. 95% of them are abnormal ECG plots.
This will explain the reason why the features can be
extracted. For the 5% normal ECG, the quality of
the ECG plots also shows low. The experimental re-
sults are shown in Figure 10. The real-time AFib de-
Figure 9: Result of The AFib Detection Model.
tection from the apple watch is validated in our sys-
tem. Depending on the watchOS version, two types of
data sources are supported - a pdf format image and
the raw data file. As shown in Figure 10, when the
available data source is a pdf image, our system con-
verted it into an accepted data format for the detection
model.
4 CONCLUSIONS
This study proposed a 5G mobile edge computing
(MEC) based telemedicine design integrating wear-
able devices with an Open-EMR electronic health
records system. This design has multiple modules:
the IoT module, MEC module, Network module, and
Application module. A near-real-time artificial intel-
ligence (AI) components and electronic health record
From Wearable Device to OpenEMR: 5G Edge Centered Telemedicine and Decision Support System
497

Figure 10: Result of Apple Watch ECG image detection.
(EHR) instances are deployed to the MEC layer, en-
abling cloud computing capabilities on the network
edge. 5G technology further improves the latency
and connectivity necessary to support wearables and
IoMT in telemedicine. A proof of concept imple-
mentation of atrial fibrillation (Afib) detection with
frequency predictable by trending, adverse event ran-
dom occurrence, and urgent care needed when hap-
pens are evaluated. Future work includes applications
in telemedicine beyond Afib detection and further de-
velopment of the telemedicine work with mmWave
and integration with other technologies.
ACKNOWLEDGEMENTS
This work was funded by the Commonwealth Cyber
Initiative (CCI), research, innovation, and workforce
initiative of the Commonwealth of Virginia.
REFERENCES
Ahad, A., Tahir, M., Sheikh, M. A., Ahmed, K. I., Mughees,
A., and Numani, A. (2020). Technologies trend to-
wards 5g network for smart health-care using iot: A
review. Sensors (Switzerland), 20(14).
Bass, L., Clements, P., and Kazman, R. (2013). Software
Architecture in Practice Second Edition Third Edition.
Bayoumy, K., Gaber, M., Elshafeey, A., Mhaimeed, O.,
Dineen, E. H., Marvel, F. A., Martin, S. S., Muse,
E. D., Turakhia, M. P., Tarakji, K. G., and Elshazly,
M. B. (2021). Smart wearable devices in cardiovas-
cular care: where we are and how to move forward.
Nature Reviews Cardiology.
Behar, J. A., Rosenberg, A. A., Yaniv, Y., and Oster, J.
(2017). Rhythm and quality classification from short
ECGs recorded using a mobile device. In Computing
in Cardiology, volume 44.
Chernyshev, M., Zeadally, S., and Baig, Z. (2019). Health-
care Data Breaches: Implications for Digital Forensic
Readiness. Journal of Medical Systems, 43(1).
Clifford, G. D., Liu, C., Moody, B., Lehman, L. H., Silva,
I., Li, Q., Johnson, A. E., and Mark, R. G. (2017).
AF classification from a short single lead ECG record-
ing: The PhysioNet/computing in cardiology chal-
lenge 2017. In Computing in Cardiology, volume 44.
Dominique Makowski. NeuroKit.
Haghi, M., Thurow, K., and Stoll, R. (2017). Wearable
Devices in Medical Internet of Things: Scientific Re-
search and Commercially Available Devices. Health-
care Informatics Research, 23(1).
Kumar, R. and Tripathi, R. (2021). Towards design and
implementation of security and privacy framework
for Internet of Medical Things (IoMT) by leveraging
blockchain and IPFS technology. The Journal of Su-
percomputing, 77(8).
Latif, S., Qadir, J., Farooq, S., and Imran, M. (2017). How
5G Wireless (and Concomitant Technologies) Will
Revolutionize Healthcare? Future Internet, 9(4).
Li, D. (2019). 5G and intelligence medicine–how the
next generation of wireless technology will recon-
struct healthcare?. Precision Clinical Medicine, 2(4).
Min Wu and Jake Luo (2020).
https://www.himss.org/resources/wearable-
technology-applications-healthcare-literature-review.
Pearce, J. M. (2017). Emerging Business Models for Open
Source Hardware. Journal of Open Hardware, 1(1).
Purkayastha, S., Allam, R., Maity, P., and Gichoya, J. W.
(2019). Comparison of Open-Source Electronic
Health Record Systems Based on Functional and User
Performance Criteria. Healthcare Informatics Re-
search, 25(2).
Shahriar, H., Haddad, H. M., and Farhadi, M. (2021). As-
sessing HIPAA Compliance of Open Source Elec-
tronic Health Record Applications. International
Journal of Information Security and Privacy, 15(2).
Sun, H., Zhang, Z., Hu, R. Q., and Qian, Y. (2018). Wear-
able communications in 5g: Challenges and enabling
technologies. IEEE Vehicular Technology Magazine,
13(3).
Syzdykova, A., Malta, A., Zolfo, M., Diro, E., and Oliveira,
J. L. (2017). Open-Source Electronic Health Record
Systems for Low-Resource Settings: Systematic Re-
view. JMIR Medical Informatics, 5(4).
Wang, Y., Gorski, A., and da Silva, A. (2021). Development
of a Data-Driven Mobile 5G Testbed: Platform for Ex-
perimental Research. In IEEE International Mediter-
ranean Conference on Communications and Network-
ing.
Zhang, Y., Chen, G., Du, H., Yuan, X., Cheriet, M., and
Kadoch, M. (2020). Real-time remote health moni-
toring system driven by 5G MEC-IOT. Electronics
(Switzerland), 9(11).
HEALTHINF 2022 - 15th International Conference on Health Informatics
498
