
Towards an IoHT Platform to Monitor QoL Indicators
Pedro Almir M. Oliveira
1 a
, Rossana M. C. Andrade
1 b
,
Pedro A. Santos Neto
2 c
and Breno S. Oliveira
1 d
1
Group of Computer Networks, Software Engineering and Systems (GREat), Federal University of Cear
´
a, Cear
´
a, Brazil
2
Laboratory of Software Optimization and Testing (LOST), Federal University of Piau
´
ı, Piau
´
ı, Brazil
Keywords:
Internet of Health Things, Smart Quality of Life, Automated Monitoring.
Abstract:
The Quality of Life has been studied for a long time, and the World Health Organization defines it as the indi-
vidual perception about life regarding four major domains: physical, psychological, social, and environmental.
The relevance to study QoL lies in the search for strategies able to measure a patient’s well-being. Without
these strategies, treatments, and technological solutions that aim to improve people’s QoL would be restricted
to physicians’ implicit and subjective perceptions. Thus, there are many instruments for formal QoL assess-
ment (usually questionnaires). However, the use of these instruments is time-consuming, non-transparent, and
error-prone. Considering this problem, in this work, we discuss the proposal to use the Internet of Health
Things (IoHT) to collect data from smart environments and apply machine learning techniques to infer QoL
measures. To achieve this goal, we designed an IoHT platform inspired by the MAPE-K loop. Our literature
review has shown that this idea is promising and that there are many open challenges to be addressed.
1 INTRODUCTION
Over the past few years, the use of technologies in
healthcare and medical care has grown (Oliveira et al.,
2021b). For example, years ago, it was practically un-
feasible to continuously monitor a patient without the
intrusive need of a robust hospital infrastructure (Is-
lam et al., 2015). However, advances in the Internet of
Things (IoT) such as sensors miniaturization, efficient
communication protocols, expansion in data process-
ing capacity, application of intelligent algorithms, and
even more secure approaches to guarantee the pri-
vacy of patients have made possible a revolution in
the healthcare area (Mesk
´
o, 2014).
In this way, the Internet of Health Things (IoHT)
emerges from the application of IoT in healthcare
(Rodrigues et al., 2018) and it is possible to cite many
examples of IoHT solutions. For example, there are
non-invasive glucose sensing (Istepanian et al., 2011),
electrocardiogram monitoring (Agu et al., 2013), el-
derly fall detection (Almeida et al., 2016), and many
others.
a
https://orcid.org/0000-0002-3067-3076
b
https://orcid.org/0000-0002-0186-2994
c
https://orcid.org/0000-0002-1554-8445
d
https://orcid.org/0000-0003-0079-8799
In general, these solutions have been proposed to
achieve i) individual benefits, by increasing safety
and well-being; ii) economic benefits, by improving
the cost-effectiveness of limited healthcare resources;
and, finally, iii) social benefits by promoting better
living conditions (Dohr et al., 2010).
Regarding the cost-effectiveness of healthcare
systems, world society has experienced a phe-
nomenon that has put much pressure on them: pop-
ulation aging (Nations, 2019). The United Nations
(UN) projected that, in 2050, there will be 1.5 bil-
lion of older persons. The population aging process is
highly positive since it indicates that we are progress-
ing as a society. However, this new scenario brings
new challenges. Among them, we can highlight the
need for a healthcare system focused on preventive
care (Gmeinder et al., 2017). Today, it is common to
act only when the patient becomes ill (Marvasti and
Stafford, 2012).
The Organization for Economic Co-operation and
Development (OECD) pointed out that only 2.8% of
health spending goes on prevention, and only 7% of
this part was focused on early disease detection (Fig-
ure 1) (Gmeinder et al., 2017). Furthermore, the last
World Health Organization (WHO) report indicates
that this percentage grew only to 5% in 2020 (Vri-
jburg and Hern
´
andez-Pe
˜
na, 2020).
438
Oliveira, P., Andrade, R., Neto, P. and Oliveira, B.
Towards an IoHT Platform to Monitor QoL Indicators.
DOI: 10.5220/0010823500003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 438-445
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

Figure 1: Fraction of health expenditure applied in preven-
tive health strategies (Gmeinder et al., 2017).
Thus, one of the strategies that can improve the
effectiveness of healthcare systems is the continuous
monitoring of people’s Quality of Life (QoL) in order
to anticipate the development of health issues related
to physical, psychological, social, and environmental
aspects. According to the WHO, it is crucial to mea-
sure the QoL because it has a close relationship with
the health status, and it provides valuable data to med-
ical practice (Estrada-Galinanes and Wac, 2018).
Nevertheless, given the available techniques and
tools, it is possible to state that seamless Quality of
Life (QoL) monitoring is complex, expensive, non-
transparent, and error-prone. It is complex because
there are at least 150 strategies to measure QoL (Gill
and Feinstein, 1994), and it remains difficult to firmly
define QoL (Karimi and Brazier, 2016). It is ex-
pensive and non-transparent because these strategies
(usually questionnaires) should be self-rated by the
patient or should be applied by a healthcare profes-
sional (Bowling, 2005). Furthermore, it is error-prone
since an active answer to a questionnaire can add a
bias in the outcomes (Crane et al., 2016).
Thus, this work presents ongoing research that
aims to create an IoHT platform able to support the
development of self-adaptive applications (Vansyckel
et al., 2013) focused on monitoring and improving
users’ Quality of Life. This study is part of a larger
STIC-AmSud
1
project - called Angel - which aims
to provide a robust Internet of Things (IoT) platform
to Ambient Assisted Living, offering support to the
improvement of Quality of Life (QoL), especially for
persons with chronic diseases, older adults and per-
sons with acute diseases under medical monitoring.
The idea is to use the Internet of Things (IoT) to ob-
tain and enrich environmental data in order to infer
QoL levels, monitor health vital signs, and identify
atypical situations such as falls and nocturia.
In this paper, we discussed the advances in our
data collection module. The following sections dis-
cuss our background, proposal, ongoing proof of con-
cept, and final remarks.
1
STIC-AmSud: sticmathamsud.org/stic/proyectos.
2 BACKGROUND
Before any formal definition, having a better Quality
of Life is probably the greatest desire of humankind.
Naturally, this desire has driven the development of
studies focused on improving people’s QoL (Baker
et al., 2017), mainly because there is a close relation-
ship between health and QoL (Guyatt et al., 1993).
However, despite being discussed for a long time
(Elkinton, 1966), the term Quality of Life is con-
fusing and can be observed from many perspectives
(Karimi and Brazier, 2016). The QoL can be related
to the absence of chronic diseases, perception of lone-
liness, physical well-being, and understanding of the
aging/death process. In this work, the WHO defi-
nition for Quality of Life was considered the main
reference. For WHO, QoL can be described as the
individual perception of life in a sociocultural con-
text and concerning goals, expectations, and personal
standards (WHOQoL Group, 1994).
From this definition, many mechanisms to evalu-
ate QoL have been proposed. One of the most cited
is the WHOQOL-BREF questionnaire (Skevington
et al., 2004) due to its reliability and cross-cultural
validity. The WHOQOL-BREF was evaluated in 23
countries (including Brazil), and it is available in 19
different languages. It has twenty-six (26) questions
distributed into four domains: physical, psychologi-
cal, social, and environment.
The “Physical” domain assesses motor facets such
as daily living activities, medicines’ dependence, mo-
bility, sleep quality, and work capacity. The “Psycho-
logical” domain is related to the bodily image, neg-
ative and positive feelings, self-esteem, spirituality,
and other mental health aspects. The “Social” do-
main observes personal relationships, social support,
and sexual activity. Finally, the “Environment” do-
main aims to evaluate the environmental facets such
as freedom, safety, security, participation in leisure
activities, pollution, noise, traffic, and climate.
Unfortunately, the continuous application of
this kind of instrument is tedious and bothersome
(Sanchez et al., 2015), which makes it challenging
to engage the participants. Therefore, the QoL con-
tinuous monitoring is still an open problem due to
the complexity of the measurement instruments and
the invasive approaches that do not preserve privacy
(Oliveira et al., 2021b). The relevance of this problem
emerges from the health benefits that can be achieved
from up-to-date and accurate QoL information (e.g.,
early interventions). Due to this, some studies have
been conducted to find strategies to use the Internet
of Things for seamless QoL monitoring.
Towards an IoHT Platform to Monitor QoL Indicators
439

3 RELATED WORK
In order to compose our related work, a literature re-
view was performed on papers indexed on Elsevier’s
Scopus database. Our search string was composed of
the following terms and their synonyms: “smart qual-
ity of life, passive sensing, internet of health things,
platform and machine learning”. The first two terms
were included to ensure the retrieval of three con-
trol papers (previously identified by the authors). The
other terms are directly associated with our final goal:
to build a platform to support the development of
IoHT systems that use Machine Learning to monitor
and improve users’ QoL.
The Scopus database was selected based on its
coverage
2
of software engineering venues and rele-
vant digital libraries such as ACM, IEEExplorer, Sci-
ence Direct, and Springer. Thus, the selected papers
represent a suitable sample to describe this study area.
Furthermore, it is also important to note that we did
not include any date restriction.
Initially, 122 papers were recovered, but only 13
were chosen after full reading. The eligibility criteria
were: be a primary study, written in English, fully
available on the Web, and with more than 5 pages;
be published in conferences or journals; and discuss
IoHT solutions to monitor QoL automatically.
Table 1 summarizes the 13 selected papers and
our work. However, before starting the discussion of
these works, we would like to highlight the difficulty
in building a search string capable of differentiating
studies focused on strategies to automate QoL mea-
surements or that seek to correlate data collected by
IoHT systems with measurements made by QoL ques-
tionnaires; from the studies that bring a specific pro-
posal for a health problem. In general, both kinds of
these studies use the terms Quality of Life, monitor-
ing, and improvement. Thus, we argue that the term
“Smart Quality of Life” is a suitable candidate to rep-
resent this research area. Within this context, the first
authors
3
to use this expression were (Qiu et al., 2020).
Unfortunately, the authors did not provide a formal
definition for this term. Therefore, we present here a
formal definition inspired by the WHO statement.
Smart QoL can be described as the perception of
a person’s Quality of Life from individual and contex-
tual data acquired in Smart Environments using ubiq-
uitous technologies. Usually, this perception is built
through intelligent algorithms, and, over time, it can
be used to detect health issues. Now, in light of this
definition, it is possible to discuss our related work.
2
Scopus Coverage: elsevier.com/?a=69451.
3
Other authors have used this term, but in the context of
smart cities.
We decided to group on the top of Table 1 case
studies. Thus, the criteria “Deal with heterogene-
ity?”, “Use any semantic model?”, “Provide AI for
data analysis?”, and “Allow strategies to adapt user’s
environment” were filled with a dash because they are
not applicable for them.
The studies presented by (Bade et al., 2018),
(Kim et al., 2019), (Lee et al., 2019), (Angthong and
Veljkovic, 2019), (Oliveira et al., 2021a), and (Brudy
et al., 2021) were classified as longitudinal studies
because they involve analyzing the participants data
through an extended period in order to prove the cor-
relation between health data and the patients’ QoL.
Although these studies do not present software arti-
facts as the main contribution, their discussion is rele-
vant to indicate strategies for evaluating solutions that
use health data to infer the quality of life of their users.
All these works (excluding only the study conducted
by (Lee et al., 2019)) used commercial smart bands
and their native applications. This decision is prob-
ably related to the costs of these devices (values be-
tween $15 and $60 dollars). In general, devices with
higher processing power that allow the development
of native apps for their platforms are expensive (val-
ues above $300 dollars). Another difficulty observed
in these studies is the absence of APIs for data extrac-
tion, which makes this extraction an arduous process.
Regarding the data analysis, all of these longitu-
dinal studies present statistical analyzes to validate
their hypotheses. (Bade et al., 2018) and (Oliveira
et al., 2021a) proved that there is a correlation be-
tween physical activity data and the QoL of people
with cancer. Similarly, (Kim et al., 2019) shown this
correlation for hospitalized patients with spinal is-
sues; (Lee et al., 2019) for patients with fibromyalgia;
(Angthong and Veljkovic, 2019) for adults with foot-
ankle condition, and (Brudy et al., 2021) for children
with congenital heart disease. The results of these
studies can be generalized to state that it is possi-
ble to use data collected by smart objects to mea-
sure the Quality of Life of patients even with dif-
ferent QoL questionnaires and for different health
conditions. This opportunity has also been rein-
forced in renowned medical journals (Huckvale et al.,
2019). Unfortunately, none of these studies made
their datasets available, which hinders the advance-
ment in this study area. Currently, there are many data
silos without a semantic representation that allows its
use in further investigations.
To conclude this first group of works, (Concheiro-
Moscoso et al., 2021) brings a protocol to assess the
impact of stress in workers’ QoL. Their main contri-
bution is to present a guide on conducting studies that
seek to correlate health data with QoL facets.
HEALTHINF 2022 - 15th International Conference on Health Informatics
440
Table 1: Papers selected in the literature review compared with our proposal.
Work Contribution
Deal with
hetero-
geneity?
Use any
semantic
model?
Provide
AI for
data
analysis?
Allow
strategies
to adapt
user’s
environ-
ment?
Domains Profile # of Part. Env. Devices Analysis
(Bade et al.,
2018)
Longitudinal
study
- - - - Physical
Patients with
Lung Cancer
30
Not
specified
Fitbit Zip and Smartphone
Spearman rank
correlation
(Kim et al.,
2019)
Longitudinal
study
- - - - Physical
People with
spinal issues
22 Hospital Fitbit Charge
Pearson
correlation and
regression
analysis
(Lee et al.,
2019)
Longitudinal
study
- - - - Physical
Fibromyalgia
patients
14
Not
specified
Specific wearable built for
this study
Statistical
analysis
(Angthong
and
Veljkovic,
2019)
Longitudinal
study
- - - - All
Adults with
foot- and
ankle-related
conditions
52
Not
specified
Foot pod (Garmin)
Pearson’s
correlation
(Oliveira
et al., 2021a)
Longitudinal
study
- - - - All
Lymphoma
patients
16
Not
specified
Microsoft Band 2
Statistical
analysis
(Concheiro-
Moscoso
et al., 2021)
Study
Protocol
- - - - Physical Adults 11 Work Xiaomi Mi Band 3
Statistical
analysis
(Brudy et al.,
2021)
Longitudinal
study
- - - - All
Children with
congential
heart disease
343
Not
specified
Garmin vivofit Jr
Logistic
regression
(Merilahti
et al., 2012)
Model No No Yes No Physical Older adults 19
Not
specified
Actigraphy, Bed sensor,
Omron Walking Style II
pedometer and Omron
705IT
Spearman
correlation and
k-means
clustering
(Vargiu et al.,
2014)
Methodology Yes No Yes No All
People with
disabilities
Not
informed
Home
Brain/Neural Computer
Interface (BNCI), inertial
sensors, environmental
sensors, smart home devices
C4.5 and k-NN
(Bono-Nuez
et al., 2014)
System No No Yes No Physical Older adults
Not
informed
Smart
Kitchen
Kitchen appliances, Zigbee
sensors, RFID and portable
devices
Self-organizing
maps (SOM)
(De Masi
et al., 2016)
Platform No No Yes No All Generic
Not
informed
Indoor
and
outdoor
Smartphone and Wearables
User data
timeline
(Dobre et al.,
2019)
Architecture Yes No No No All Older adults
Not
informed
Indoor
and
outdoor
Smartwatch, smart shoes,
camera
Statistical
Analysis
(R
˘
adulescu
et al., 2019)
Framework No No No No All Older adults 17
Not
specified
Not specified
Spearman
correlation
Our work Platform Yes Yes Yes Yes
Physical
and Psy-
chological
Adults
In
progress
Indoor
and
Outdoor
Smartphones, Amazfit Bip,
and Smart Home Devices
Machine
Learning
The second group brings methods, frameworks,
systems, and platforms as their main contribution.
In (Merilahti et al., 2012), the authors present
a study about the performance of health monitor-
ing technologies to estimate the physical function of
older adults. They present a hypothesis that health
data would predict pre-clinical measures. Thus, 19
older adults were analyzed through 84 days using
wrist-worn activity monitors, bed sensors, pedome-
ters, weight scales, and blood pressure monitors. The
acquired raw data were transformed into 16 features,
and they were analyzed using statistical correlation
and clustering methods. Unfortunately, the results
were not promising, indicating only a correction with
the daily steps. However, this work brings interesting
insights about which features can be used in this type
of investigation and points out issues in data collec-
tion. Compared to our proposal, this paper presents
only a specific model for the physical domain, which
does not consider self-assessment questionnaires and
does not concern itself with other aspects of IoHT
(such as heterogeneity, semantic model, and environ-
mental adaptation).
(Vargiu et al., 2014) propose a context-aware
methodology to telemonitor QoL concerning the
physical and social autonomy of people with disabili-
ties. Thus, they adapted the EQ-5D-5L questionnaire
to assess mood, health status, mobility, self-care,
usual activities, and pain/discomfort. On the other
hand, health data were collected by Brain/Neural
Computer Interface (BNCI), inertial and environmen-
tal sensors, and smart home devices. Finally, the au-
thors achieved good results using the C4.5 and k-NN
algorithms. Nonetheless, due to the lack of real data,
synthetic data was used.
(Bono-Nuez et al., 2014) focused their contri-
bution in creating a QoL evaluation system to sup-
port the work of caregivers. The idea is to provide
QoL assessments of older adults periodically to help
decision-making of caring actions. Unlike other stud-
ies, the authors did not choose a QoL questionnaire
as a reference. Instead, they decided to cluster the
data using self-organizing maps (SOM). Neverthe-
less, their proposal was focused on smart kitchens,
and it requires the analysis of a domain expert to in-
terpret the results obtained by the SOM.
Towards an IoHT Platform to Monitor QoL Indicators
441
The work proposed by (De Masi et al., 2016) is
probably the most related to our proposal. The signifi-
cant difference is that the authors proposed a platform
to support interdisciplinary studies related to Quality
of Life. In contrast, we are focused on helping the
development of IoHT systems capable of using data
from Smart Environments to provide a closed adapta-
tion loop. The authors present the first version of the
mQoL Living Lab and the requirements for the sec-
ond version in their paper. Unfortunately, this plat-
form is not publicly available, and it was not possible
to conduct a more in-depth test.
(Dobre et al., 2019) propose an IoT architecture
to deliver non-intrusive monitoring and support older
adults’ healthcare. One of the most interesting points
of this work lies in the authors’ concern about inher-
ent Internet of Things challenges, such as interoper-
ability. The architecture was designed with a mod-
ular structure and, similar to the work proposed by
(De Masi et al., 2016), the data analysis module is
aimed at conducting scientific studies. However, this
work did not address semantic models for QoL data,
intelligent techniques to infer QoL, and strategies to
act in the environment.
The work proposed by (R
˘
adulescu et al., 2019)
brings a framework to find a correlation of health pa-
rameters with QoL questionnaires. The authors deal
with this problem using mathematical models. They
selected the Technique for Order Preference by Sim-
ilarity to an Ideal Solution (TOPSIS), which uses the
concept of “ideal” and “anti-ideal” solutions and com-
putes the Euclidean distance to find an overall health
index for the elderly. Nonetheless, the method was
evaluated only with synthetic data, and its complexity
makes its adoption in several contexts difficult.
Finally, the analysis of these papers highlights that
there are still opportunities in developing platforms
that enable the collection of health data, the pro-
cessing of these data using intelligent algorithms, the
planning of interventions in case of risky situations,
and the environment adaptation. In other words, a
closed loop of health care that seeks to identify health
issues before they become a reality.
4 OUR PROPOSAL
This investigation has the final goal to develop an
IoHT solution to collect data from smart environ-
ments and apply machine learning to infer QoL mea-
sures. Moreover, this solution should allow high-level
health interventions to adapt the user’s environment.
To achieve this goal, we are proposing a platform
to support the development of this kind of system.
The rationale for building a platform lies in the bene-
fits obtained by software reuse since other researchers
or practitioners can use it to implement solutions for
specific contexts (Ara
´
ujo et al., 2018). In addition,
the platform is being designed to address challenges
such as lack of interoperability, high volatility, high
development cost when it involves AI, absence of
a semantic model for QoL data, and difficulties to
bring healthcare professionals closer to the develop-
ment process (Oliveira et al., 2021b).
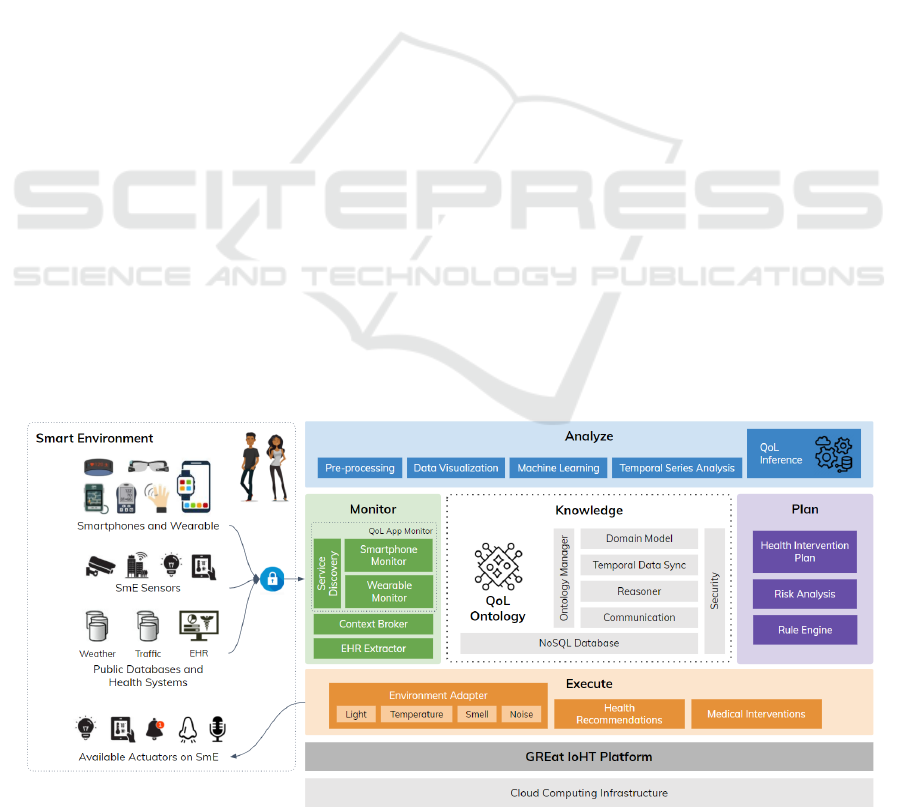
Figure 2 presents an overview of this proposal. We
decided to organize the platform modules following
the MAPE-K loop framework (IBM, 2005). Hence,
the platform will support collecting and analyzing
data, plan what actions should be taken based on the
analysis result, and adjust the environment. Further-
Figure 2: IoHT platform design inspired on the MAPE-K loop.
HEALTHINF 2022 - 15th International Conference on Health Informatics
442
more, it will be possible to represent the knowledge
using a QoL ontology.
In the monitor are the modules responsible for ob-
taining user data. These data can be collected from
mobile devices (e.g., smartphones), context brokers,
or EHR (Electronic Health Record) systems. As dis-
cussed in our related work, the literature already has
evidence that data collected from wearables can infer
QoL aspects. In this way, this proposal argues that an
expanded view of devices present in smart environ-
ments allows a broad and accurate QoL inference.
Additionally, it will be integrated a previous work
called LoCCAM-IoT (Andrade et al., 2020), which is
a multifaceted infrastructure to support the develop-
ment of self-adaptive IoT systems. This infrastructure
has three major modules: i) CoAP-CTX, an extension
of the CoAP protocol for context-awareness device
discovery; ii) LoCCAM, a middleware for acquisition
and context management that uses smartphones as a
decision center; and iii) SUCCEEd, which was cre-
ated to support the self-adaptation using workflows.
In the analysis area, the platform will provide ma-
chine learning techniques adapting the Athena tool,
which is a visual, customizable, cloud-based tool to
support the development of systems that require Com-
putational Intelligence (CI) techniques. It uses the ab-
straction of visual modules to encapsulate the CI al-
gorithms allowing their interconnection to solve com-
plex problems (Oliveira et al., 2018). All these tech-
niques should support the creation of an intelligent
model to infer QoL.
Monitoring and data analysis will provide a QoL
profile for the user. With this profile, it will be pos-
sible to identify risk situations and plan health inter-
ventions. These interventions - defined by health pro-
fessionals - can be recommendations for changes in
habits; or even the execution of adaptations in the en-
vironment. In critical cases, it will be possible to re-
quest medical interventions.
Finally, the execution of this loop generates a vast
amount of data, which represents the knowledge ac-
quired in that context. Thus, the platform also pro-
vides an ontology for representing and storing data.
5 PROOF-OF-CONCEPT
A Proof-of-Concept (PoC) is in progress in order to
validate our proposal. This PoC aims to anticipate
the best strategies for collecting data from users and
which machine learning algorithms are suitable for
the inference process.
For this, we developed an Android application –
called QoL Monitor – to collect contextual and health
data from users. In this version, we collect sociode-
mographic and anthropometric data, sleep duration,
daily steps, calories spent, physical activities, heart
rate, location, apps usage time, and the number of
calls made or received. To do that, it was necessary to
integrate our app with the Google Fit API. Thus, users
who participate in this study can use different wear-
ables as long as they are integrated with the Google
Fit account.
Since we are looking to validate the creation of
intelligent models to infer users’ QoL, it will be nec-
essary for them to answer questionnaires informing
their QoL perception periodically. We are working
to reduce the use of these questionnaires. However,
today, they are our best alternative to calibrate our
machine learning models, as they have been validated
with many participants in different countries.
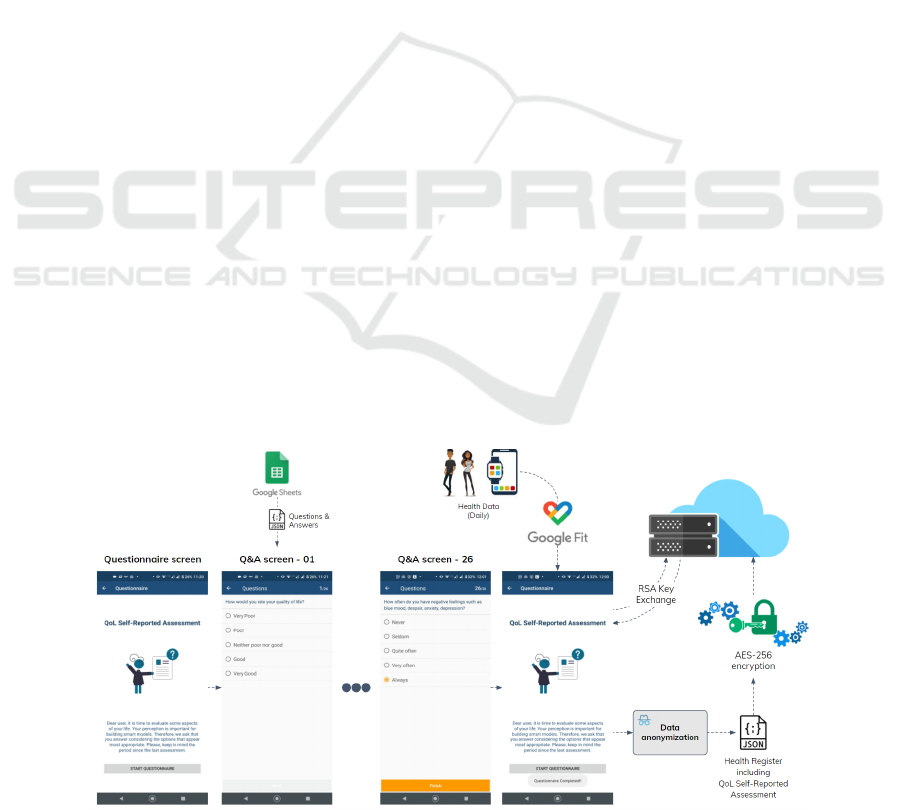
Figure 3 presents the QoL Monitor data collec-
tion workflow. It is possible to observe some impor-
Figure 3: QoL Monitor data collection workflow.
Towards an IoHT Platform to Monitor QoL Indicators
443

tant points: i) the questionnaire can be externally cus-
tomized, making easier changes throughout the study
or even the validation of another questionnaire; ii)
historical health data is obtained via Google Fit API;
and iii) before sending the data to the server, they are
anonymized and encrypted using AES-256 algorithm,
in addition to the exchange of RSA keys for secure
communication with the server.
Currently, the QoL Monitor has been finished and
internally validated by the researchers. Thus, our next
step is to request permission for the ethics commit-
tee to start a pilot study with a larger number of par-
ticipants. Our purpose is also to create a public and
anonymous database to improve QoL inference mod-
els. Unfortunately, to the best of our knowledge, no
databases were found able to correlate contextual and
health data with self-report QoL questionnaires.
6 FINAL REMARKS
This work is just beginning, and there are many points
to be defined. However, we argue that this paper dis-
cusses an interesting research topic to guide the scien-
tific community towards an IoHT platform to monitor
and improve people’s Quality of Life.
In this paper, we present the platform’s design in-
spired by the MAPE-K loop. Using this approach, it is
possible to support IoHT applications able to monitor
and analyze user data and plan and execute interven-
tions in the environment.
Furthermore, we state that there is a growing need
for investments in solutions capable of anticipating
health issues. This kind of solution has the poten-
tial to move our healthcare system from passive care
to active care, increasing its cost-benefit. Due to this,
we also discussed 13 related works and proposed a
definition for the term Smart Quality of Life.
As our future work, we highlight the conclusion
of our PoC; the investigation of which health issues
can be early detected by analyzing QoL over time; the
development of the first version of our IoHT platform;
and the conduction studies to validate the platform.
ACKNOWLEDGMENTS
We would like to thank CNPQ for the Productiv-
ity Scholarship of Rossana M. C. Andrade DT-2 (N
o
315543 / 2018-3), for the Productivity Scholarship of
Pedro A. dos Santos Neto DT-2 (N
o
315198 / 2018-4).
REFERENCES
Agu, E., Pedersen, P., Strong, D., Tulu, B., He, Q., Wang,
L., and Li, Y. (2013). The smartphone as a medical de-
vice: Assessing enablers, benefits and challenges. In
IEEE Int. Workshop of Internet-of-Things Networking
and Control, pages 48–52. IEEE.
Almeida, R. L., Macedo, A. A., de Ara
´
ujo,
´
I. L., Aguilar,
P. A., and Andrade, R. M. (2016). Watchalert: An
evolution of the falert app for detecting falls on smart-
watches. In Extended Proceedings of the XXII Brazil-
ian Symp. on Multimedia and Web Systems, pages
124–127. SBC.
Andrade, R. M., Junior, B. R. A., Oliveira, P. A. M., Maia,
M. E., Viana, W., and Nogueira, T. P. (2020). Mul-
tifaceted infrastructure for self-adaptive iot systems.
Information and Software Technology, page 106505.
Angthong, C. and Veljkovic, A. (2019). Relationships
among subjective patient-reported outcome, quality of
life, and objective gait characteristics using wearable
foot inertial-sensor assessment in foot–ankle patients.
European Journal of Orthopaedic Surgery & Trauma-
tology, 29(3):683–687.
Ara
´
ujo, t., Andrade, R., and Aguilar, P. (2018). Artefatos de
Reuso para Internet das Coisas: Arquiteturas, Middle-
wares, Frameworks e Padr
˜
oes. Thesis report, Federal
University of Cear
´
a.
Bade, B. C., Brooks, M. C., Nietert, S. B., Ulmer, A.,
Thomas, D. D., Nietert, P. J., Scott, J. B., and Silvestri,
G. A. (2018). Assessing the correlation between phys-
ical activity and quality of life in advanced lung can-
cer. Integrative cancer therapies, 17(1):73–79.
Baker, S. B., Xiang, W., and Atkinson, I. (2017). Internet of
things for smart healthcare: Technologies, challenges,
and opportunities. IEEE Access, 5:26521–26544.
Bono-Nuez, A., Blasco, R., Casas, R., and Mart
´
ın-del Br
´
ıo,
B. (2014). Ambient intelligence for quality of life as-
sessment. Journal of Ambient Intelligence and Smart
Environments, 6(1):57–70.
Bowling, A. (2005). Just one question: If one question
works, why ask several?
Brudy, L., Meyer, M., Oberhoffer, R., Ewert, P., and M
¨
uller,
J. (2021). Move more–be happier? physical activ-
ity and health-related quality of life in children with
congenital heart disease. American Heart Journal,
241:68–73.
Concheiro-Moscoso, P., Groba, B., Mart
´
ınez-Mart
´
ınez,
F. J., Miranda-Duro, M. d. C., Nieto-Riveiro, L., Pou-
sada, T., Queir
´
os, C., and Pereira, J. (2021). Study for
the design of a protocol to assess the impact of stress
in the quality of life of workers. Int. journal of envi-
ronmental research and public health, 18(4):1413.
Crane, M., Rissel, C., Greaves, S., and Gebel, K. (2016).
Correcting bias in self-rated quality of life: an ap-
plication of anchoring vignettes and ordinal regres-
sion models to better understand qol differences
across commuting modes. Quality of life research,
25(2):257–266.
De Masi, A., Ciman, M., Gustarini, M., and Wac, K. (2016).
mqol smart lab: quality of life living lab for interdisci-
HEALTHINF 2022 - 15th International Conference on Health Informatics
444

plinary experiments. In Proceedings of the 2016 ACM
Int. Joint Conf. on Pervasive and Ubiquitous Comput-
ing: Adjunct, pages 635–640.
Dobre, C., Bajenaru, L., Marinescu, I. A., and Tomescu, M.
(2019). Improving the quality of life for older people:
From smart sensors to distributed platforms. In 2019
22nd Int. Conf.on Control Systems and Computer Sci-
ence (CSCS), pages 636–642. IEEE.
Dohr, A., Modre-Opsrian, R., Drobics, M., Hayn, D., and
Schreier, G. (2010). The internet of things for am-
bient assisted living. In 7th int. conf. on information
technology: new generations, pages 804–809. IEEE.
Elkinton, J. R. (1966). Medicine and the quality of life.
Annals of Internal Medicine, 64:711–714.
Estrada-Galinanes, V. and Wac, K. (2018). Visions and
challenges in managing and preserving data to mea-
sure quality of life. In 3rd Int. Work. on Foundations
and Applications of Self Systems, pages 92–99. IEEE.
Gill, T. M. and Feinstein, A. R. (1994). A critical appraisal
of the quality of quality-of-life measurements. Jama,
272(8):619–626.
Gmeinder, M., Morgan, D., and Mueller, M. (2017). How
much do oecd countries spend on prevention?
Guyatt, G. H., Feeny, D. H., and Patrick, D. L. (1993). Mea-
suring health-related quality of life. Annals of internal
medicine, 118(8):622–629.
Huckvale, K., Venkatesh, S., and Christensen, H. (2019).
Toward clinical digital phenotyping: a timely oppor-
tunity to consider purpose, quality, and safety. NPJ
digital medicine, 2(1):1–11.
IBM (2005). An architectural blueprint for autonomic com-
puting.
Islam, S. R., Kwak, D., Kabir, M. H., Hossain, M., and
Kwak, K.-S. (2015). The internet of things for health
care: a comprehensive survey. IEEE access, 3:678–
708.
Istepanian, R. S., Hu, S., Philip, N. Y., and Sungoor, A.
(2011). The potential of internet of m-health things
“m-iot” for non-invasive glucose level sensing. In An-
nual Int. Conf. of the IEEE Engineering in Medicine
and Biology Society, pages 5264–5266. IEEE.
Karimi, M. and Brazier, J. (2016). Health, health-related
quality of life, and quality of life: what is the differ-
ence? Pharmacoeconomics, 34(7):645–649.
Kim, D. H., Nam, K. H., Choi, B. K., Han, I. H., Jeon, T. J.,
and Park, S. Y. (2019). The usefulness of a wear-
able device in daily physical activity monitoring for
the hospitalized patients undergoing lumbar surgery.
Journal of Korean Neurosurgical Society, 62(5):561.
Lee, J., Park, S.-H., Ju, J. H., and Cho, J. H. (2019). Appli-
cation of a real-time pain monitoring system in korean
fibromyalgia patients: A pilot study. International
journal of rheumatic diseases, 22(5):934–939.
Marvasti, F. F. and Stafford, R. S. (2012). From “sick
care” to health care: reengineering prevention into the
us system. The New England journal of medicine,
367(10):889.
Merilahti, J., P
¨
arkk
¨
a, J., and Korhonen, I. (2012). Esti-
mating older people’s physical functioning with au-
tomated health monitoring technologies at home: fea-
ture correlations and multivariate analysis. In Interna-
tional Conference on Grid and Pervasive Computing,
pages 94–104. Springer.
Mesk
´
o, B. (2014). The guide to the future of medicine: tech-
nology and the human touch. Webicina kft.
Nations, U. (2019). World population prospects: the 2019
revision. United Nations, Department of Economic
and Social Affairs, Population Division.
Oliveira, A., Silva, E., Aguiar, J., Faria, B. M., Reis, L. P.,
Cardoso, H., Gonc¸alves, J., Oliveira e S
´
a, J., Carvalho,
V., and Marques, H. (2021a). Biometrics and quality
of life of lymphoma patients: A longitudinal mixed-
model approach. Expert Systems, 38(4):e12640.
Oliveira, P., Neto, P. S., Britto, R., Rabelo, R., Braga, R.,
and Souza, M. (2018). Ciaas-computational intelli-
gence as a service with athena. Computer Languages,
Systems & Structures, 54:95–118.
Oliveira, P. A. M., Andrade, R. M. C., and Neto, P. S. N.
(2021b). Iot-health platform to monitor and improve
quality of life in smart environments. In 8th IEEE Int.
Workshop on Medical Computing. IEEE.
Qiu, L., Tong, Y., Yang, Q., Sun, N., Gong, Y., and Yin,
X. (2020). Reliability and validity of a smart quality
of life scale for patients with tuberculosis. Journal of
Public Health, 28(5):575–582.
R
˘
adulescu, C. Z., Alexandru, A., and B
˘
ajenaru, L. (2019).
Health parameters correlation in an iot monitoring,
evaluation and analysis framework for elderly. In 2019
23rd International Conf. on System Theory, Control
and Computing (ICSTCC), pages 531–536. IEEE.
Rodrigues, J. J., Segundo, D. B. D. R., Junqueira, H. A.,
Sabino, M. H., Prince, R. M., Al-Muhtadi, J., and
De Albuquerque, V. H. C. (2018). Enabling tech-
nologies for the internet of health things. Ieee Access,
6:13129–13141.
Sanchez, W., Martinez, A., Campos, W., Estrada, H., and
Pelechano, V. (2015). Inferring loneliness levels in
older adults from smartphones. Journal of Ambient
Intelligence and Smart Environments, 7(1):85–98.
Skevington, S. M., Lotfy, M., and O’Connell, K. A. (2004).
The world health organization’s whoqol-bref quality
of life assessment: psychometric properties and re-
sults of the international field trial. Quality of life Re-
search, 13(2):299–310.
Vansyckel, S., Sch
¨
afer, D., Schiele, G., and Becker, C.
(2013). Configuration management for proactive
adaptation in pervasive environments. In 2013 IEEE
7th International Conference on Self-Adaptive and
Self-Organizing Systems, pages 131–140. IEEE.
Vargiu, E., Fern
´
andez, J. M., and Miralles, F. (2014).
Context-aware based quality of life telemonitoring. In
Distributed Systems and Applications of Information
Filtering and Retrieval, pages 1–23. Springer.
Vrijburg, K. and Hern
´
andez-Pe
˜
na, P. (2020). Global spend-
ing on health: Weathering the storm 2020. World
Health Organization Working paper, (19.4).
WHOQoL Group (1994). The development of the world
health organization quality of life assessment instru-
ment (the whoqol). In Quality of life assessment: In-
ternational perspectives, pages 41–57. Springer.
Towards an IoHT Platform to Monitor QoL Indicators
445
