
Extracting Alarm Events from the MIMIC-III Clinical Database
Jonas Chromik
1 a
, Bjarne Pfitzner
1 b
, Nina Ihde
1 c
, Marius Michaelis
1 d
, Denise Schmidt
1 e
,
Sophie Anne Ines Klopfenstein
2 f
, Akira-Sebastian Poncette
2 g
, Felix Balzer
2 h
and Bert Arnrich
1 i
1
Hasso Plattner Institute, University of Potsdam, Germany
2
Charit
´
e – Universit
¨
atsmedizin Berlin, Berlin, Germany
Keywords:
Patient Monitor Alarm, Medical Alarm, Intensive Care Unit, Vital Parameter, Data Cleaning, Data Extraction.
Abstract:
Lack of readily available data on ICU alarm events constitutes a major obstacle to alarm fatigue research.
There are ICU databases available that aim to give a holistic picture of everything happening at the respective
ICU. However, these databases do not contain data on alarm events. We utilise the vital parameters and alarm
thresholds recorded in the MIMIC-III database in order to artificially extract alarm events from this database.
Prior to that, we uncover, investigate, and mitigate inconsistencies we found in the data. The results of this
work are an approach and an algorithm for cleaning the alarm data available in MIMIC-III and extract concrete
alarm events from them. The data set generated by this algorithm is investigated in this work and can be used
for further research into the problem of alarm fatigue.
1 INTRODUCTION
Alarm fatigue is the desensitisation of medical staff
due to an excessive number of alarms, most of them
being false or irrelevant (McCartney, 2012). This
results in a lack of response to the alarm stimulus.
The problem of alarm fatigue has been widely inves-
tigated, both qualitatively (Cvach, 2012) and quanti-
tatively (Drew et al., 2014).
However, building technical solutions for alleviat-
ing alarm fatigue is hindered by a lack of readily avail-
able data on patient monitor alarms. Public medical
databases usually provide no data on patient monitor
alarms as is the case with eICU CRD (Pollard et al.,
2018) and HiRID (Hyland et al., 2020).
The MIMIC-III database (Johnson et al., 2016)
provides alarm data. However, there are only alarm
a
https://orcid.org/0000-0002-5709-4381
b
https://orcid.org/0000-0001-7824-8872
c
https://orcid.org/0000-0001-5776-3322
d
https://orcid.org/0000-0002-6437-7152
e
https://orcid.org/0000-0002-6299-0738
f
https://orcid.org/0000-0002-8470-2258
g
https://orcid.org/0000-0003-4627-7016
h
https://orcid.org/0000-0003-1575-2056
i
https://orcid.org/0000-0001-8380-7667
thresholds recorded in the database and not the alarm
events themselves. Alarm thresholds are lower and
upper boundaries for a certain vital parameter, such
as the heart rate (HR). For example, for HR the low
alarm threshold might be set to 60 bpm and the high
alarm threshold to 120 bpm. Whenever the measured
parameter, i.e. HR, drops below the low alarm thresh-
old or exceeds the high alarm threshold, an alarm
event goes off at the patient monitor and alerts the
medical staff.
The objective of this work is to extract these alarm
events from the MIMIC-III database by taking into
account alarm thresholds and the actual parameter
value. This is done for the following vital parameters:
HR: heart rate, as measured by an electrocardiogram
(ECG) and expressed in beats per minute (bpm)
NBP
s
: non-invasively measured systolic blood pres-
sure, as measured by a sphygmomanometer and
expressed in millimeters of mercury (mmHg)
S
p
O
2
: peripheral blood oxygen saturation, as mea-
sured by a pulse oximeter (usually on the patients
finger) and expressed in %
Furthermore, we uncover and rectify inconsisten-
cies in the recorded alarm thresholds such as unrealis-
tically high or low values or instances where the high
328
Chromik, J., Pfitzner, B., Ihde, N., Michaelis, M., Schmidt, D., Klopfenstein, S., Poncette, A., Balzer, F. and Arnrich, B.
Extracting Alarm Events from the MIMIC-III Clinical Database.
DOI: 10.5220/0010767200003123
In Proceedings of the 15th International Joint Conference on Biomedical Engineering Systems and Technologies (BIOSTEC 2022) - Volume 5: HEALTHINF, pages 328-335
ISBN: 978-989-758-552-4; ISSN: 2184-4305
Copyright
c
2022 by SCITEPRESS – Science and Technology Publications, Lda. All rights reserved

alarm threshold is below the low alarm threshold.
The rest of this work is structured as follows: In
Section 2 we describe which parts of the MIMIC-III
database we are using, how we address data inconsis-
tencies through data cleaning, and finally how we ex-
tract alarm events. In Section 3 we describe the alarm
event data set that is produced as a result of this work.
Finally, in Section 4 we discuss our findings as well
as potential applications and limitations of this data
set.
2 MATERIALS & METHODS
The MIMIC-III database contains 26 tables provid-
ing a wide range of information on the events at the
intensive care units (ICUs) of Beth Israel Deaconess
Medical Center. For our use case, however, only
the CHARTEVENTS table is of interest. This table
contains, among others, measured values and alarm
thresholds of the vital parameters listed in Section 1.
The objective of this work is to extract alarm
events by comparing the measured parameter values
with the corresponding alarm thresholds. However,
before the alarm events can be extracted, we have to
deal with a number of data inconsistencies that we un-
covered. The inconsistencies and our corresponding
rectification approaches are presented in the follow-
ing.
2.1 Data Cleaning
The CHARTEVENTS table contains a multitude of
information, such as routine vital signs, ventilator set-
tings, laboratory values, and mental status.
1
For ex-
tracting alarm events, however, only a small subset of
this information is relevant, i.e. measurements of the
three vital parameters we consider in this work (HR,
NBP
s
, and S
p
O
2
) as well as their respective high and
low alarm thresholds. Hence, the first step in data
cleaning is removing all irrelevant information by re-
taining only a specific subset of ITEMIDs which are
listed in Table 1.
Invalid Value Removal. Besides removing irrele-
vant data items, we are also interested in validating
the correctness of the relevant data items. For exam-
ple, S
p
O
2
can not exceed 100% and HRs above 350
bpm are rare. For the considered vital parameters, we
found that their recorded values are not always within
clinically valid ranges. We assume that these extreme
values are either erroneous or bear a special but un-
1
https://mimic.mit.edu/iii/mimictables/chartevents/
Table 1: Complete list of ITEMIDs retained while filter-
ing the CHARTEVENTS table with their respective label
as recorded in the D ITEMS table.
ITEMID Label
220045 HR
220046 HR Alarm - High
220047 HR Alarm - Low
220179 NBP
s
223751 NBP
s
Alarm - High
223752 NBP
s
Alarm - Low
220277 S
p
O
2
223769 S
p
O
2
Alarm - High
223770 S
p
O
2
Alarm - Low
documented meaning. Therefore, we decided to re-
move values outside the clinically valid ranges listed
in Table 2.
Invalid value removal is done both for the param-
eter measurements themselves and the threshold set-
ting (both low and high) using the same ranges. The
ranges are intentionally chosen to be conservative in
order not to remove valid measurements or settings.
For measurements, this removal means that the value
at this point in time is missing afterwards but could
be reproduced by interpolating between the neigh-
bouring measurements. Concerning alarm thresholds,
only changes of these thresholds are recorded in the
MIMIC-III database. Hence, we do not have dedi-
cated threshold information for each parameter mea-
surement. Thus, for alarm threshold, invalid value re-
moval means that the threshold update is lost and the
previous threshold is carried over.
Table 2: Clinically valid ranges for the vital parameters con-
sidered in this work. Adapted from (Harutyunyan et al.,
2019).
Parameter Lower Limit Upper Limit
HR 0 350
NBP
s
0 375
S
p
O
2
0 100
To show how the cleaning steps affect the origi-
nal data set, we look at the distributions of thresholds
and measurements for NBP
s
. NBP
s
serves only as an
example here. The same cleaning steps were also per-
formed for HR and S
p
O
2
. Figure 1 shows that the
majority of threshold values and measurements are in
the valid range. However, there is still a wide range
of outliers with implausibly high values. These out-
liers are removed by the invalid value removal clean-
ing step. Figure 2 shows a rectified and more reason-
able value distribution after the outliers are removed.
Apart from values outside clinically relevant
ranges, we also found inconsistencies within the
alarm thresholds. These inconsistencies are essen-
Extracting Alarm Events from the MIMIC-III Clinical Database
329
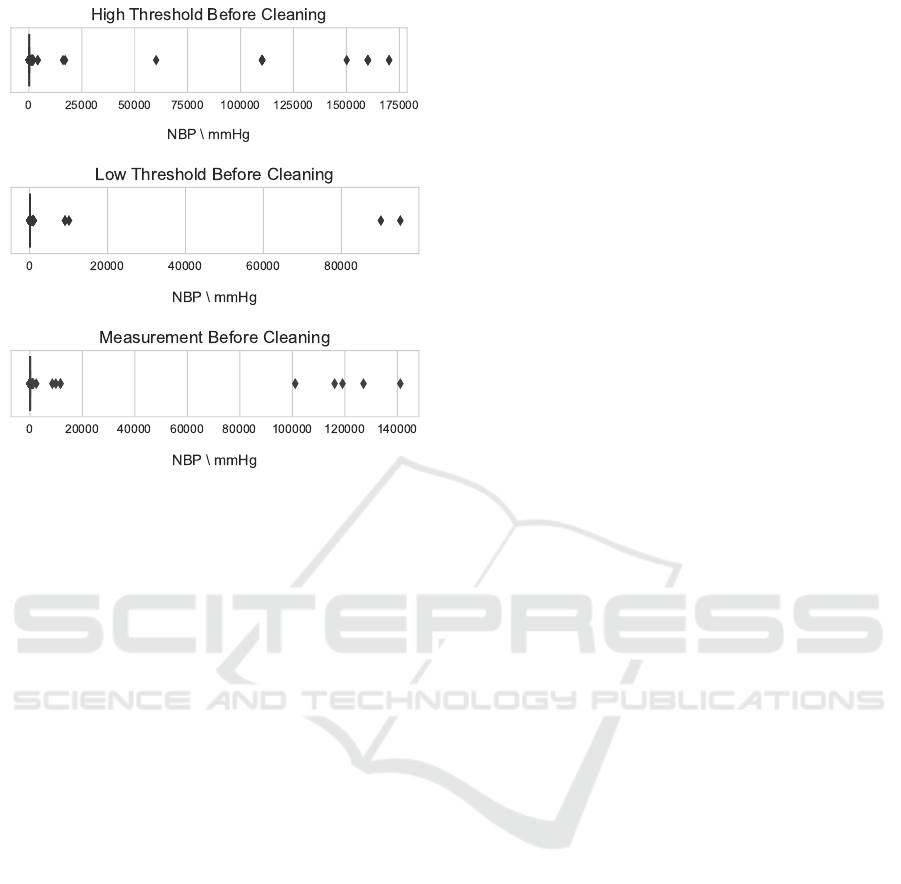
Figure 1: Boxplots showing the distribution of high alarm
thresholds, low alarm thresholds and measurements before
cleaning. The distribution is vastly skewed with the valid
range barely visible at the far left corner and a wide range
of outliers.
tially periods of time, where the high alarm threshold
is below the low alarm threshold for a vital parameter.
We further distinguish between exact threshold swaps
and threshold overlaps which we both describe in the
following.
Exact Threshold Swaps. In MIMIC-III, changes
in corresponding high and low thresholds are al-
ways recorded simultaneously. Every newly recorded
high threshold is associated with a low threshold be-
ing recorded at the same time and vice versa. At
times, these thresholds are exactly swapped, i.e., the
high thresholds taking the value of the low threshold
and vice versa as shown in Fig. 2a. This, however,
would create an alarm with every further measure-
ment which is why we consider this to be an erroneous
recording that needs rectification. Exact threshold
swaps are easily identified and corrected by swapping
the high and the low threshold as shown in Fig. 2b.
Threshold Overlaps. Besides the exact alarm
threshold swaps, there are also cases where high
and low alarm thresholds overlap but are not exactly
swapped and therefore generate an alarm too. For ex-
ample, a high alarm threshold might be set unreason-
ably low and falls below the corresponding low alarm
threshold as shown in Fig. 3a. At the same time, the
low alarm threshold continues to stay at a reasonable
value. Such an overlap is usually present for short pe-
riods only. These cases cannot be corrected by swap-
ping. Therefore, since high and low alarm thresh-
olds are always recorded pairwise in the MIMIC-III
database, both high and low alarm thresholds are re-
moved in the respective segment where they overlap.
The last clinically meaningful alarm thresholds prior
to the overlapping thresholds are chosen instead, as
shown in Fig. 3b.
2.2 Extracting Alarm Events
In Section 2.1 we described how we cleaned the
CHARTEVENTS table from out-of-range values and
inconsistencies. In this section, we show how we used
the actual measurements of the vital parameters and
their corresponding threshold setting in order to find
actual alarm events in the data. As shown in Algo-
rithm 1, we first isolated measurements and thresh-
olds for each ICU stay (single stay of a single patient
at the ICU) and each vital parameter. Then, we went
through each high threshold setting and low threshold
setting respectively and checked whether any mea-
surement within the relevant time frame exceeded
the high threshold or falls below the low thresholds.
Whenever this happened, we return either a high or
a low alarm event at the respective measurement’s
timestamp.
A shortcoming of this approach is that the num-
ber of alarms is subject to the sampling frequency of
the respective vital parameter. Higher sampling fre-
quencies produce more alarms because there are more
measurements in a period of time where the vital pa-
rameter is out of range. Figure 4 shows the differences
in the number of samples for the data items listed in
Table 1. Clearly, HR and S
p
O
2
are measured or at
least recorded more often than NBP
s
. This can result
in an over-representation of HR and S
p
O
2
alarms as
compared to NBP
s
alarms.
3 RESULTS
In Section 2 we describe methods and algorithms we
used to clean the CHARTEVENTS table and extract
concrete alarm events from it. This results in a data
set containing all patient monitor alarms as per the
MIMIC-III database in its respective observation pe-
riod. In this section, we show some descriptive statis-
tics that are made possible by the extracted data set of
alarm events.
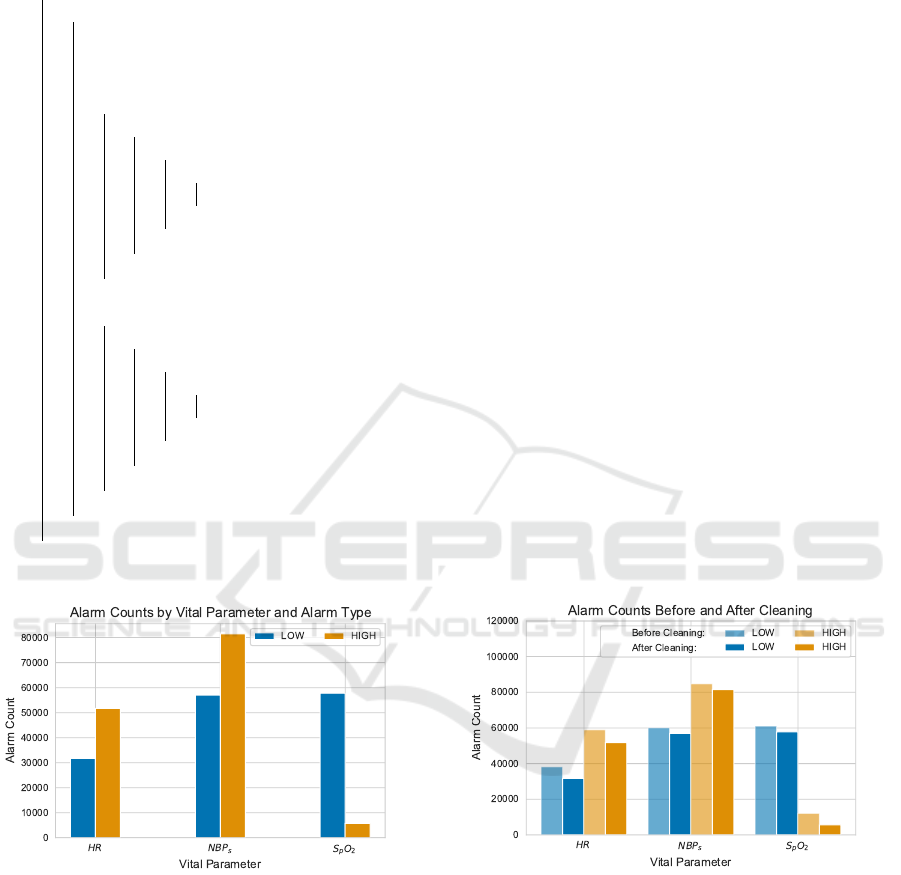
Parameters and Alarm Types. The data set gives
insight into the relative counts of alarms produced
HEALTHINF 2022 - 15th International Conference on Health Informatics
330

(a) Exactly swapped low and high thresholds before cor-
rection. Every measurement in the time period where
the thresholds are swapped would theoretically produce an
alarm.
(b) A data cleaning step removes the exact threshold swap
thus rectifying the alarm threshold. No alarm events will be
recognised in the respective time period.
Figure 2: Example for an exact threshold swap correction.
(a) In this case, the thresholds overlap without being exactly
swapped. Here, the unreasonable low value for the high
threshold would result in all measurements in the respective
period of time triggering a high threshold alarm.
(b) Threshold overlap was corrected by removing the re-
sponsible alarm threshold settings. After correction, no
high alarms are triggered in the respective period of time.
Figure 3: Example for threshold overlap correction.
Figure 4: Comparison of the number of samples for mea-
surements and thresholds for HR, NBP
s
, and S
p
O
2
. The
number of measurements is much higher than the number
of thresholds in all cases and there are distinct differences
in the number of samples for the different vital parameter
measurements.
by the different vital parameters. Comparing alarm
counts among vital parameters might yield skewed re-
sults due to the differences in sampling frequencies,
as already discussed in Section 2.2. However, com-
paring the counts of high and low threshold alarms for
a single vital parameter yields interesting results. Fig-
ure 5 shows such a comparison. For HR and NBP
s
,
violations of the high threshold seem to occur more
often than violations of the low threshold. However,
for S
p
O
2
violations of the low threshold are a lot more
common than violations of the high threshold. This is
to be expected since a high blood oxygen saturation is
rarely a problem while too low blood oxygen satura-
tion is a harmful condition (Silverthorn, 2018).
We also want to emphasise the effect of the clean-
ing steps we performed on the alarm counts. Fig-
ure 6 shows the numerical reduction of alarms for
each alarm type we considered. The alarms that are
Extracting Alarm Events from the MIMIC-III Clinical Database
331
Data: MIMIC-III CHARTEVENTS
Result: List of Alarm Events
foreach ICUSTAY do
foreach Parameter do
msmts := measurements for Parameter and ICUSTAY;
highs := high threshold settings for Parameter and ICUSTAY;
lows := low threshold settings for Parameter and ICUSTAY;
foreach high in highs do
foreach msmt in msmts do
if time(high) <= time(msmt) < time(high+1) then
if value(msmt) > value(high) then
Return a high alarm event at msmt;
end
end
end
end
foreach low in lows do
foreach msmt in msmts do
if time(low) <= time(msmt) < time(low+1 then
if value(msmt) < value(low) then
Return a low alarm event at msmt;
end
end
end
end
end
end
Algorithm 1: Algorithm for extracting alarm events from measurements and thresholds.
Figure 5: Comparison of alarm counts by vital parameter
(i.e. HR, NBP
s
, and S
p
O
2
) and alarm type (i.e. whether a
high or a low threshold was violated).
not present as a result of the cleaning steps are suppos-
edly false alarms. Hence, this shows that the clean-
ing step actually improves the quality of the generated
data set, since the alarms not included after cleaning
are supposedly false alarms.
Alarm Distribution among ICU Stays. The gen-
erated data set shows that the distribution of alarm
events among the ICU stays seems to follow a Pareto
Figure 6: Alarm counts for low and high alarms regarding
HR, NBP
s
, and S
p
O
2
. Extracted from an uncleaned and
from a cleaned data set, respectively. This figure shows that
there is a reduction in alarm count due to cleaning for each
type of alarm.
distribution. The majority of patients produce only
a low number of alarms with the interquartile range
(IQR) spanning from 3 to 16 alarms per ICU stay.
However, there are few patients that are responsible
for an excessively high number of alarms as can be
seen in Fig. 7. We considered the 1% of ICU stays
with the highest number alarms to be outliers and
hence to not show them in the plot in an attempt to
HEALTHINF 2022 - 15th International Conference on Health Informatics
332
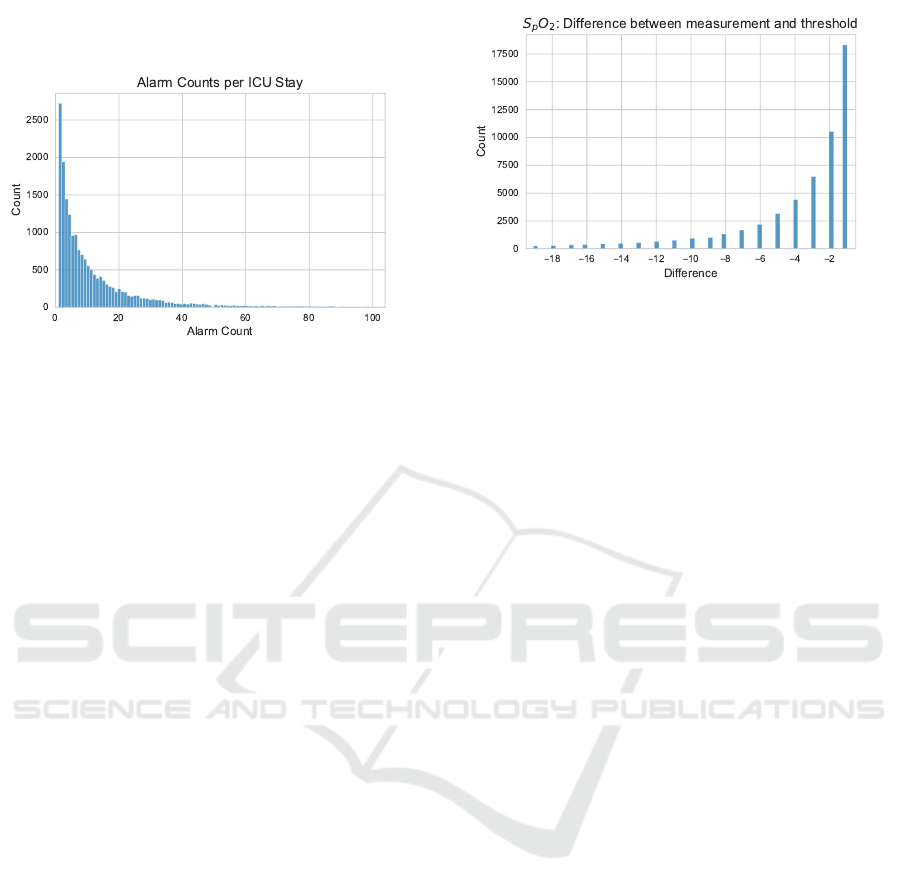
show the distribution of the remaining 99% per cent
more clearly.
Figure 7: The distribution of alarm counts (only 99%
shown) among the ICU stays follows a Pareto distribution
with few patients generating a large number of alarms and
many patients generating only few alarms.
Differences between Alarm Threshold and Mea-
surement. Patient monitor alarms do not differenti-
ate between strong and slight threshold violations. An
alarm goes off whenever the measurement exceeds a
high threshold or drops below a low threshold. For the
patient monitor, it does not matter whether the dif-
ference between measurement and threshold is high
or low. However, in clinical practice, the difference
is relevant since a parameter slightly out of range is
far less critical than a parameter that has by far left
a physiologically healthy range. Therefore, we in-
vestigated the difference between measurement and
threshold. Figure 8 shows this difference by the ex-
ample of the S
p
O
2
low threshold. Most of the alarms
are caused by only a slight drop of the measurement
below the threshold by a few per cent. On the other
hand, large drops of the S
p
O
2
parameter are rare. The
same pattern of many low differences between mea-
surement and threshold and few large differences are
also to be found when looking at the other parameters,
i.e. HR and NBP
s
.
4 DISCUSSION
The analyses we have shown in Section 3 – although
interesting – are only examples for the potential use
cases of the data set that is created by the approach
presented in this paper. Nevertheless, these results are
relevant findings that can guide further research into
alarm fatigue.
Structural Findings. On finding is that extensive
post-processing in terms of cleaning and alarm ex-
Figure 8: Histogram of the differences between alarm
threshold and actual measurement for the S
p
O
2
low thresh-
old. The majority of alarms are triggered by a slight drop of
the measurement below the threshold.
tracting is necessary to make sense from the alarm
data in MIMIC-III. This calls for guidelines prescrib-
ing on how to appropriately provide alarm data. Vital
parameters, alarm thresholds, and alarm events both
in terms of threshold alarm and in terms of other
alarms such as arrhythmia alarms need to be taken
into account. Furthermore, data inconsistencies as un-
covered in Section 2.1 need to be avoided. This can
either be avoided on a device level by designing the
interface of the patient monitor in a way that incon-
sistent thresholds are impossible to set. Or, a post-
processing step is required to rectify or remove these
inconsistencies.
Contentual Findings. Apart from findings related
to the structure and consistency of the data, we also
want to discuss the findings related to the content of
the generated data set. Figure 7 shows that the major-
ity of patients generate only a low number of alarms
while few patients generate a large number of alarms.
In order to alleviate alarm fatigue, it would be sensible
to conduct further research into what causes these pa-
tients to generate far greater numbers of alarms. Fur-
ther, we showed in Fig. 8 that the majority of alarms
are caused by minimal threshold violations. This find-
ing can be used to guide further research. For ex-
ample, patient monitors could take the difference be-
tween measurement and threshold into account in or-
der to adapt the volume of the alarm, as shown in
(Greer et al., 2018). Another option would be to sup-
press or delay alarms caused by slight threshold viola-
tions in order to help the medical staff focus on more
severe emergencies as (Schmid et al., 2013) and (Win-
ters et al., 2018) find that alarm delays are an effective
tool to reduce false alarms at the ICU.
Two design decisions are noteworthy in our ap-
proach to data cleaning. First, in the invalid value re-
moval step, we remove measurements and thresholds
Extracting Alarm Events from the MIMIC-III Clinical Database
333

if and only if their values are outside the correspond-
ing valid range. One result of this is that threshold up-
dates might be partially removed, i.e. a high threshold
update being removed while the corresponding low
threshold is retained or vice versa. This is notewor-
thy because thresholds update originally occur only
pairwise in the MIMIC-III database. We decided to
remove only the invalid part of the threshold update
in order to retain as much valid information as possi-
ble.
Second, when removing threshold overlaps, we
decided to always remove both parts (high and low)
of the threshold update because it is not always ob-
vious whether one threshold part remains in a sen-
sible range while the other part deviates or whether
both parts deviate. This can not be determined with-
out making strong assumptions about the nature of
threshold updates. Hence, we decided to always re-
move both parts thus reverting the effective threshold
to the last reasonable threshold update.
Limitations and Threats to Validity. The alarm
event data set we generated from the MIMIC-III
database provides some interesting insights into the
problem of alarm fatigue in medicine. However, there
are some limitations and threats to validity attached to
our approach. The data quality of the generated alarm
events data set is – apart from the cleaning steps we
performed – limited by the data quality of the data
set it is generated from. For example, the sampling
frequencies for the data in the MIMIC-III database
manifest an upper limit for the sampling frequencies
in the alarm events data set. Furthermore, all changes
in sampling frequency, missing data, etc. are also car-
ried over into the alarm events data set. For exam-
ple, higher sampling frequencies in the vital param-
eter measurements will result in a higher number of
alarms. Since the sampling frequencies vary among
vital parameters, as Fig. 4 shows, some alarm types
(e.g. HR) might be over-represented. This has to be
kept in mind when working with the data set.
Future Work. We already discussed the implica-
tions for alarm fatigue research of this work’s find-
ings as well as its limitations. Further work needs
to be done in order to validate the finding from the
MIMIC-III database. Especially, more extensive ICU
databases are needed covering not only vital param-
eters, input and output events, laboratory findings,
and hospital logistics but also providing data on ICU
alarms.
Until such a database is created, the data set gener-
ated in this work can be used for a variety of purposes,
some of them are demonstrated in Section 3. Among
others, this data set enables quantitative analyses on
alarm events, alarm forecasting, and alarm threshold
recommendation which are to be covered in future re-
search.
5 CONCLUSION
The contribution of the paper is an approach and al-
gorithm to generate alarm events from the MIMIC-
III database. Publishing the generated data set it-
self would have been more convenient for researchers
interested in data on alarm events. However, by
publishing only the algorithm we ensure compliance
with the data protection guidelines of the MIMIC-
III database. Everyone with access to the MIMIC-
III database can apply the algorithm to the database
and thus create the alarm events data set themselves.
The algorithms for data cleaning and alarm extrac-
tion are published on GitHub, see https://github.com/
HPI-CH/mimic-alarms.
ACKNOWLEDGEMENTS
This work was partially carried out within the
INALO project. INALO is a cooperation project be-
tween AICURA medical GmbH, Charit
´
e – Univer-
sit
¨
atsmedizin Berlin, idalab GmbH, and Hasso Plat-
tner Institute. INALO is funded by the German Fed-
eral Ministry of Education and Research under grant
16SV8559.
REFERENCES
Cvach, M. (2012). Monitor alarm fatigue: An integrative
review. Biomedical Instrumentation & Technology,
46(4):268–277.
Drew, B. J., Harris, P., Z
`
egre-Hemsey, J. K., Mammone,
T., Schindler, D., Salas-Boni, R., Bai, Y., Tinoco, A.,
Ding, Q., and Hu, X. (2014). Insights into the problem
of alarm fatigue with physiologic monitor devices: A
comprehensive observational study of consecutive in-
tensive care unit patients. PloS one, 9(10):e110274.
Greer, J. M., Burdick, K. J., Chowdhury, A. R., and
Schlesinger, J. J. (2018). Dynamic alarm systems for
hospitals (dash). Ergonomics in Design, 26(4):14–19.
Harutyunyan, H., Khachatrian, H., Kale, D. C., Ver Steeg,
G., and Galstyan, A. (2019). Multitask learning and
benchmarking with clinical time series data. Scientific
Data, 6(1):1–18.
Hyland, S. L., Faltys, M., H
¨
user, M., Lyu, X., Gumbsch, T.,
Esteban, C., Bock, C., Horn, M., Moor, M., Rieck, B.,
HEALTHINF 2022 - 15th International Conference on Health Informatics
334

et al. (2020). Early prediction of circulatory failure in
the intensive care unit using machine learning. Nature
Medicine, 26(3):364–373.
Johnson, A. E. W., Pollard, T. J., Shen, L., Lehman, L.-
W. H., Feng, M., Ghassemi, M., Moody, B., Szolovits,
P., Celi, L. A., and Mark, R. G. (2016). MIMIC-III,
a freely accessible critical care database. Scientific
Data, 3(1):1–9.
McCartney, P. R. (2012). Clinical alarm management.
MCN: The American Journal of Maternal/Child Nurs-
ing, 37(3):202.
Pollard, T. J., Johnson, A. E., Raffa, J. D., Celi, L. A., Mark,
R. G., and Badawi, O. (2018). The eICU collabora-
tive research database, a freely available multi-center
database for critical care research. Scientific Data,
5(1):1–13.
Schmid, F., Goepfert, M. S., and Reuter, D. A. (2013). Pa-
tient monitoring alarms in the ICU and in the operat-
ing room. Annual Update in Intensive Care and Emer-
gency Medicine 2013, pages 359–371.
Silverthorn, D. U. (2018). Human Physiology: An Inte-
grated Approach. Pearson, 8th edition.
Winters, B. D., Cvach, M. M., Bonafide, C. P., Hu, X.,
Konkani, A., O’Connor, M. F., Rothschild, J. M.,
Selby, N. M., Pelter, M. M., McLean, B., and Kane-
Gill, S. (2018). Technological distractions (part 2):
A summary of approaches to manage clinical alarms
with intent to reduce alarm fatigue. Critical Care
Medicine, 46(1):130–137.
Extracting Alarm Events from the MIMIC-III Clinical Database
335
